Abstract
Non-human primates (NHP) have played a crucial rule in the history of morbillivirus research. Although NHPs are naturally susceptible to morbillivirus infections, outbreaks are rare among monkeys and apes living in their natural habitat. However, introduction of a highly contagious morbillivirus in a high-density population or captive colony seronegative for morbilliviruses can easily lead to an efficient transmission chain in which all animals become infected. Secondary infections due to morbillivirus-induced immune suppression can subsequently yield complications, leading to outbreaks with high morbidity and mortality. In this chapter, we provide an overview of morbillivirus outbreaks that have occurred in different monkey species, and we discuss morbillivirus epidemiology in different target species. Furthermore, differences in infection course and severity in various species are discussed. In addition to discussing natural infection of NHP with morbilliviruses, this chapter provides an overview of experimental infections of NHP with wildtype or genetically engineered morbilliviruses. These studies have contributed significantly to a more complete understanding of measles pathogenesis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
In 1911 measles virus (MV) was identified as the causative agent of measles when inoculation of macaques with filtered respiratory tract secretions from measles patients caused measles-like symptoms in these animals (Goldberger and Anderson 1911). Interestingly, this was well before isolation of the virus in 1954 (Enders and Peebles 1954). Since then, early measles studies in monkeys were performed and reported variable susceptibility of different NHP species to MV infection, complicating the initial measles pathogenesis, pathology, and vaccination studies and questioning the utility of NHPs as a model for measles research. Retrospectively, the low susceptibility of some animals to experimental MV infection was likely due to prior exposure to MV-infected humans, resulting in the development of MV-specific antibodies and rendering them immune.
Peebles et al. were the first to demonstrate that healthy laboratory macaques frequently possessed MV-specific antibodies (Peebles et al. 1957). At that time, it was postulated that measles in NHP and humans was the same disease caused by the same agent and that NHPs living in captivity potentially contracted measles by direct contact with MV-infected humans (Peebles et al. 1957). This was suggested by the fact that monkeys captured in the wild rarely had MV-specific antibodies, whereas these were frequently demonstrated in macaques living in captivity (Meyer et al. 1962). It was shown that many NHP species are naturally susceptible to infection with MV as well as other morbilliviruses such as canine distemper virus (CDV) and many outbreaks among captive NHPs have been reported in literature. Several species have since been used to elucidate measles pathogenesis by experimental infections; however, macaques have been studied most extensively and display a similar pathogenesis as observed in measles in humans.
In this chapter, we provide a background on MV and other morbilliviruses that can naturally cause disease in NHPs , discuss morbillivirus epidemiology in different host species, and report on morbillivirus outbreaks that occurred in captive NHPs . Furthermore, we discuss how experimental infections of NHPs helped elucidate mechanisms of MV entry, pathogenesis, transmission, and immune suppression and can be used to evaluate the efficacy and safety of novel generations of measles vaccines. Finally, we offer a discussion on infections of NHPs as an incentive for continued measles vaccination in the future.
9.2 Morbilliviruses
Morbilliviruses are enveloped viruses with a non-segmented negative-sense RNA genome and belong to the family Paramyxoviridae. Morbilliviruses are highly infectious, are spread via the respiratory route, cause a profound immune suppression, and have the propensity to cause large disease outbreaks in previously unexposed populations. Secondary opportunistic infections resulting from immune suppression, but also infection of the central nervous system (CNS), can lead to high morbidity and mortality. The genus Morbillivirus contains multiple viruses, including MV , rinderpest virus (RPV), peste des petits ruminants virus (PPRV), canine distemper virus (CDV), phocine distemper virus (PDV), and cetacean morbillivirus (CeMV). Each morbillivirus targets a different host species: MV is regarded the prototype morbillivirus and the only virus that normally infects (non-human) primates.
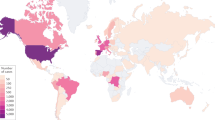
Measles, caused by MV , is a significant cause of childhood morbidity and mortality in humans and is characterized by fever, rash, cough, conjunctivitis, and a generalized immune suppression (Griffin 2013; Rota et al. 2016). Availability of safe and effective live-attenuated vaccines has led to a substantial reduction in measles morbidity and mortality (Durrheim et al. 2014), with the number of measles fatalities currently at an all-time low (below 100,000 deaths per year, (WHO 2017)). However, reduced vaccine acceptance in the industrialized world and budget deficits to maintain vaccination coverage in developing countries threaten the success of ongoing measles control programs (Strebel et al. 2011; Durrheim and Crowcroft 2017). Distemper, caused by CDV , is mainly described as an infectious disease of dogs and free-ranging carnivores like raccoons, foxes, wolves, and mustelids but has the capacity to infect a wide range of mammalian hosts. CDV infections are associated with high morbidity and mortality (Beineke et al. 2009), since the virus can virtually obliterate all lymphocytes within a host and easily invades the CNS.
Normally, morbilliviruses are restricted to natural infection of their respective host species. This is due to the fact that infection with a morbillivirus is initiated by a specific interaction between the hemagglutinin (H) protein and at least one of two proteinaceous cellular receptors: CD150 (Tatsuo et al. 2000), mainly expressed on subsets of immune cells, and nectin-4 (Noyce et al. 2011; Muhlebach et al. 2011), mainly expressed on the basolateral side (within the adherens junction) of epithelial cells. Phylogenetically, evolution of morbilliviruses largely parallels that of their host species (Visser et al. 1993; Barrett 1999). The different morbilliviruses most likely evolved from a common ancestral virus that adapted to a specific host, proving that morbilliviruses intrinsically have the ability to adapt to novel host species and measles has a zoonotic origin. For example, it has been postulated that RPV or a closely related virus crossed the species barrier from cattle into humans thousands of years ago (Barrett 1999), leading to the emergence of MV . Currently, although CDV is mainly regarded an infectious agent of carnivores, recent spread of CDV into NHPs suggests that this virus has zoonotic potential and could be devastating for humans (Qiu et al. 2011; Sakai et al. 2013a). Receptor adaptation is a crucial step for morbilliviruses like CDV to be able to cross the species barrier and infect a “non-natural” host species.
9.3 Morbillivirus Epidemiology
In general, seronegative NHPs and humans are equally susceptible to morbillivirus infections. However, since morbilliviruses are highly infectious and infections are short-lived, endemic circulation can only be sustained in a target species that lives in high-density populations of sufficient size to allow for a continuous chain of virus transmission. This explains why measles outbreaks occur frequently among morbillivirus-seronegative human populations but are rare among NHPs living in their natural habitat (Meyer et al. 1962). Therefore, while NHPs can readily be infected with a morbillivirus upon exposure to infected humans, and the infection can rapidly spread through a previously unexposed high-density colony, population sizes of NHP species are generally too small for the infection to be maintained.
9.3.1 Measles Outbreaks in Captive NHP Colonies
An initial study performed in the 1960s proved that wild NHPs in their natural habitat were indeed predominantly MV-seronegative. In this study, most NHPs showed clinical signs related to measles rapidly after trapping, and 84% of the animals seroconverted within 14 weeks after capture and transport (Meyer et al. 1962). Measles was globally endemic among humans in the 1960s, probably facilitating rapid virus transmission to monkeys. However, this study demonstrated the natural susceptibility of monkeys to MV infection and the risk of bidirectional virus transmission at the human-monkey interface. Although outbreaks were frequently reported among NHP species thereafter, it was possible, through appropriate biosecurity measures, to keep several closed populations of NHPs free of MV for decades (Andrade et al. 2003).
9.3.1.1 Measles Outbreaks in Rhesus Macaques (Macaca mulatta)
An epidemic of measles in rhesus macaques occurred in a shipment of 100 animals from India to the USA in 1966 and was meticulously described. Fifty-eight cases, including one fatal case, were reported in this study (Potkay et al. 1966). A smaller outbreak was reported in 21 rhesus macaques transported from India to the UK, including 5 lethal cases (Remfry 1976), followed by a larger outbreak in 72 imported rhesus macaques with 7 fatalities in 1979 (MacArthur et al. 1979). Diagnosis of measles in these animals was based on clinical signs (appearance of rash [illustrated in Fig. 9.1a, b], loss of appetite, conjunctivitis, respiratory symptoms) combined with the appearance of MV-specific antibodies. In addition, in some cases necropsies were performed and led to the observation of characteristic large multinucleated giant cells (illustrated in Fig. 9.2h) in the lungs (Warthin 1931; Finkeldey 1931), with or without inclusion bodies. The source of MV was not identified in either of these studies. At that time and since then, many other outbreaks of measles in free-ranging and captive rhesus macaques have been reported (Shishido 1966; Hall et al. 1971; Kessler et al. 1989; Willy et al. 1999; Jones-Engel et al. 2006).
Macroscopic images from macaques experimentally infected with (a, b) wild-type MV or a (c, d) recombinant MV expressing a fluorescent reporter protein. Figure illustrates rash on the (a) face and (b) trunk of a rhesus macaque , and less obvious on the (c1) face and (d1) trunk of a cynomolgus macaque. (c2 and d2) Anatomical locations of MV replication were visualized with a UV lamp when recombinant MV strains expressing a fluorescent reporter protein were used, and these co-localized with the appearance of rash. Panels a and b are reprinted from El Mubarak et al., J Gen Virol 2007
Images collected from experimentally infected NHPs , illustrating mechanisms underlying MV entry (a, b), dissemination (c, d), transmission (e, f), and immune suppression (g, h). MV-infected cells were detected by immunohistochemical staining (a, c, d, f), by immunofluorescent double-staining (b, e, h) or macroscopic detection (g). (a) infection of a single cell (arrow, presumably an alveolar macrophage) in the alveolar lumen at 3 days post inoculation (d.p.i.); (b) infection of epithelial cells in the trachea at 5 d.p.i. (arrow in insert points at green cilia), green = MV , red = epithelial cells, blue = nuclei; (c) infection of myeloid and lymphoid cells in bronchus-associated lymphoid tissue (arrow) at 4 d.p.i., BL = bronchial lumen; (d) low-magnification image of a lymph node at 9 d.p.i., with many B-cell follicles containing large concentrations of MV-infected lymphocytes; (e) MV-infected epithelial cells in the trachea at 9 d.p.i. (green = MV , red = epithelial cells, blue = nuclei, TL = tracheal lumen); (f) Disruption of the epithelium (arrow) of tonsillar tissue containing many MV-infected lymphocytes at 9 d.p.i.; (g) MV infection of Peyer’s patches in the small intestine at 9 d.p.i.; (h) MV-infected B-lymphocytes (including Warthin-Finkeldey syncytia, arrows) in a B-cell follicle at 9 d.p.i. (green = MV , red = B-lymphocytes, blue = nuclei). Panels a–f are reprinted from Laksono et al., Viruses 8: 2010 (2016). https://doi.org/10.3390/v8080210. Panel g is reprinted from De Vries et al., PLoS Pathog 2012
9.3.1.2 Measles Outbreaks in Other Macaque Species
In addition to rhesus macaques, measles outbreaks have also been reported in colonies of other macaque species, including cynomolgus macaques (Macaca fascicularis) (Willy et al. 1999; Welshman 1989), pig-tailed macaques (Macaca nemestrina) (Willy et al. 1999), and Japanese macaques (Macaca fuscata) (Choi et al. 1999).
Welshman et al. reported an outbreak of respiratory symptoms in 65 cynomolgus macaques in a colony of 87 animals. Interestingly, only seven of these animals developed a skin rash (illustrated in Fig. 9.1c1, d1). This is in contrast to rhesus macaques, which often develop a characteristic rash upon symptomatic MV infection (Auwaerter et al. 1999; El Mubarak et al. 2007). Conjunctivitis was not observed in this outbreak, but all animals in the colony seroconverted to MV (Welshman 1989). In general, clinical signs commonly observed in human measles patients are reproduced more accurately in rhesus macaques, compared to cynomolgus macaques (El Mubarak et al. 2007). In addition to outbreaks in cynomolgus macaque colonies, MV-seropositivity was also shown in so-called performing cynomolgus macaques living at markets in Indonesia, indicating that MV can directly spread from humans to cynomolgus macaques (Schillaci et al. 2006).
There is a particularly well-described measles outbreak among Japanese macaques; it concerns an unvaccinated colony, which lived for 20 years in outdoor exhibits of a Korean zoo before suffering an outbreak with 21% mortality. Although the source of MV was not accurately determined in this outbreak, no new monkeys had been brought into the colony and the colony had no contact with other NHP species. The authors speculate about a MV transmission event from an infected visitor to the colony while the colony was in the outdoor exhibit. Mortality in these macaques was mainly due to complicating secondary infections, in accordance with the immune suppression associated with measles. Diagnosis of measles was made on basis of histopathology, immunohistochemistry, in situ hybridization and electron microscopy, and observation of measles-associated clinical signs (Choi et al. 1999).
9.3.1.3 Measles Outbreaks in Other NHP Species
Epidemic infections in NHPs during captivity have frequently been reported in macaques but are not restricted to these species. Outbreaks of MV have also been reported in other captive Old World monkeys (colobus monkeys [Colobus guereza] and talapoins [Cercopithecus talapoin]). Captive New World monkeys (spider monkeys [Ateles spp.], marmosets and tamarins [Callithrix jacchus, Saguinus oedipus, and Saguinus fuscicollis]), and apes (chimpanzees [Pan troglodytes]) also proved to be susceptible. Outbreaks have been confirmed by the sudden appearance of MV-specific antibodies in serum and presence of multinucleated giant cells in the lungs of several fatal cases (MacArthur et al. 1979; Levy and Mirkovic 1971; van Binnendijk et al. 1995; Drewe et al. 2012).
A small measles outbreak was described among colobus monkeys; 11 animals were caught in Tanzania and transported to the UK. Within days to weeks after arrival, monkeys started to display characteristic clinical symptoms of measles (respiratory symptoms and conjunctivitis), except for the appearance of rash. Mortality was unusually high in this outbreak (100%) and a probable diagnosis of measles was based on microscopic examination of respiratory and lymphoid tissues, and the appearance of large multinucleated giant cells (illustrated in Fig. 9.2h). Measles diagnosis was confirmed by isolation of MV from one of the MV-infected colobus monkeys (Hime et al. 1975; Scott and Keymer 1975).
A natural outbreak among multiple captive marmoset and tamarin species (Callithrix jacchus, Saguinus oedipus, and Saguinus fuscicollis) was reported in 1971. These animals were housed in separate cages, spread out over separate rooms. In this outbreak, an initial fatality due to pneumonia with presence of large multinucleated giant cells was rapidly followed by the death of 57 other marmosets in the same month and another 268 fatalities in the subsequent months. Measles was identified as the probable cause on basis of histology, and MV was isolated from a moribund marmoset. Interestingly, death occurred rapidly, within 8–18 h of the initial appearance of clinical signs, significantly faster than the clinical course of measles observed in other monkey species and humans. Pneumonia was regarded as the main cause of death (Levy and Mirkovic 1971). A similar outbreak with an unidentified morbillivirus in marmosets was reported in 1978 (Fraser et al. 1978). In general, pathogenesis and disease severity in New World monkeys seems to differ from Old World monkeys, with high morbidity and mortality and rapid progression from initial clinical signs to death (Delpeut et al. 2017). CNS involvement seems to be reported more frequently in New World monkeys, confirmed by experimental intracerebral infections of these animals (Albrecht et al. 1981).
An experimental transmission study was performed with two species of tamarins (Saguinus mystax and Saguinus labiatus). In this study, tamarins were infected with two different strains of MV and housed (in separate cages) together with MV-seronegative and MV-seropositive tamarins. MV rapidly spread to the separately housed MV-seronegative tamarins (probably through airborne transmission, also the main mechanism of MV transmission in humans), confirming the natural susceptibility of these New World monkeys to MV infection. In contrast to the MV-seronegative animals, MV-seropositive animals (with the exception of 1) survived the outbreak (Lorenz and Albrecht 1980).
9.3.1.4 Measles Severity in NHPs
Although several outbreaks of MV in different species of NHPs have been well documented, it seems that mortality rates are considerably different among different outbreaks. Furthermore, in non-lethal cases, MV causes disease with variable severity in NHPs , which actually accurately parallels measles in humans. In general, New World monkeys seem more at risk of severe disease and have higher mortality rates due to measles compared to Old World monkeys (Delpeut et al. 2017), which more accurately reflect the natural course of measles in humans. Although it is likely that there are inherent species-specific differences in susceptibility to disease from MV , disease severity is probably also dependent on co-factors like the condition of monkeys during housing, or during and shortly following transport, and whether bacterial, viral, or fungal co-infections are present.
9.3.2 Ecotourism Endangering Wild NHPs
As an alternative to mass tourism, tourists increasingly enjoy visiting relatively undisturbed natural and rural areas while maintaining and conserving the natural environment. This form of tourism, known as ecotourism, provides necessary funds for local ecological conservation. However, at the same time, ecotourism frequently leads to interaction between tourists and animals naturally living in that environment, i.e., a close animal-human interface. Anthropozoonotic transmission of viruses at this interface poses a significant threat to wildlife, especially threatening endangered species like the great apes (Muehlenbein et al. 2008; Kondgen et al. 2008). In addition to ecotourists, researchers or poachers form an additional source of viruses. Mainly in areas where anthropozoonotic transmission is likely to occur, the necessary resources to identify outbreaks and their causative agents are often absent (Epstein and Price 2009), limiting the possibility for interrupting outbreaks. Since potential MV transmission from human to NHP could lead to a large measles outbreak with high mortality rates in endangered ape species, vaccination against measles of free-ranging NHP populations in areas frequently visited by ecotourists could be warranted (Epstein and Price 2009).
Besides this being a hypothetical threat, actual anthropozoonotic transmission of MV from humans to mountain gorillas (Gorilla beringei beringei) and subsequent mortality were observed in a national park in Rwanda, in 1988 (Byers and Hastings 1991; Hastings et al. 1991; Spelman et al. 2013). Initially, respiratory symptoms were observed in gorillas leading to six fatal cases. Upon necropsy, multinucleated giant cells were observed in the lungs and spleens of these fatalities. Seroconversion to measles was only observed in a single animal; however the authors speculate that this was due to early sampling during clinical signs, probably prior to seroconversion. More recently, Kaur et al. speculate on measles being the potential causative agent responsible for acute and fatal respiratory illness in wild chimpanzees (Pan troglodytes) in Tanzania (Kaur et al. 2008). In some of the outbreaks among chimpanzees in Tanzania, a paramyxovirus was identified as the causative agent. Although the paramyxovirus was not identified, the authors speculate that it is human in origin. Similar observations were made in outbreak situations in Côte d’Ivoire (Kondgen et al. 2008).
9.3.3 Distemper Outbreaks in Captive Monkey Colonies
Although CDV has originally been described as a morbillivirus of dogs, it is regarded the most species-promiscuous morbillivirus that naturally infects a wide range of carnivores and has a relatively high propensity to cross the species barrier. Disease caused by CDV infection has been reported in members of the families of Ailuridae (e.g., red pandas), Felidae (e.g., lions), Hyenidae (hyenas), Mustelidae (e.g., weasels and martens), Procyonidae (e.g., raccoons), Ursidae (black bears), Viverridae (civet cats), Megalonychidae (sloths), and Phocidae (seals) (Ludlow et al. 2014; Sheldon et al. 2017). In addition, CDV has been reported to infect javelinas (Appel et al. 1991) and was detected in rodents (Origgi et al. 2013). Although it was known that monkeys were susceptible to CDV after experimental intracerebral inoculation since the 1970s (Yamanouchi et al. 1977; Matsubara et al. 1985; Nagata et al. 1990), several natural outbreaks with CDV in NHPs have also been reported recently.
9.3.3.1 Distemper Outbreaks in Macaques
An outbreak with CDV infection in NHPs was initially reported in 1989 when a single Japanese macaque died of encephalitis. Upon necropsy, multinucleated giant cells with inclusion bodies were observed in lesions in the brain that stained positive with a CDV-specific monoclonal antibody. This subsequently led to serological testing of all the macaques in the same group. Seroconversion of all 22 animals to CDV , in the absence of antibodies to MV , was observed and proved that a CDV outbreak had occurred in these macaques (Yoshikawa et al. 1989).
More recently, larger outbreaks with higher mortality rates were reported in breeding colonies of both rhesus and cynomolgus macaques in China and Japan. Sun et al. reported a small CDV outbreak in 20 rhesus macaques in China, with 12 lethal cases (Sun et al. 2010). CDV diagnosis was made on basis of clinical signs (respiratory symptoms, anorexia, fever, thickened footpads, and rash), accompanied by electron microscopy and sequencing. From the 12 lethal cases, 11 macaques died of severe pneumonia, and a single macaque showed neurological symptoms. Whether pneumonia was caused by CDV infection itself or caused by secondary infections was not investigated. Since the sequence isolated from these macaques was identical to CDV circulating in dogs, foxes, and raccoon dogs in several regions in China, the authors speculate on spread from stray animals to macaques. Subsequently, in 2011, a full-blown epidemic was reported in a breeding farm from which the 20 animals described above originated. In this outbreak, approximately 10,000 rhesus macaques were infected with CDV ; 5–30% mortality rates were reported (Qiu et al. 2011). Diagnosis was made on basis of measles-like symptoms, seroconversion, CDV isolation, and sequencing. Again, the CDV sequence isolated from these macaques was unique, and the authors speculate on contact between colony monkeys and wild monkeys or stray dogs as cause of initial introduction into the colony. The epidemic was controlled by vaccination.
Following the two outbreaks in China, a large CDV outbreak occurred in cynomolgus macaques in Japan in 2008. This outbreak occurred in macaques imported from China and caused 46 fatalities with severe pneumonia as the main cause of death (Sakai et al. 2013a). Virus isolation, sequencing, and phylogeny indicated that the CDV strain isolated was very closely related to CDV strains associated with the outbreaks in China (Qiu et al. 2011; Sun et al. 2010). Distemper in these macaques was diagnosed on basis of clinical signs, CDV staining, and sequence analysis. Interestingly, the authors performed additional sequence analysis on macaque variants of the morbillivirus receptors and found homology between macaque CD150 and human CD150, and between human, macaque , and dog nectin-4. Notably, the CDV isolated from a moribund monkey efficiently used macaque and dog variants of receptors, but not the human variants (Sakai et al. 2013a). Adaptation of CDV to human CD150, however, appeared relatively easy (Sakai et al. 2013b).
9.3.3.2 Distemper Mortality in Macaques
CDV in its natural host is considered to be neurotropic as well as lymphotropic, whereas MV in its natural host rarely causes CNS complications. However, neurotropism was rarely observed in the few reports on CDV macaque outbreaks. Rather, the main cause of death in these outbreaks was pneumonia, and only a few animals displayed neurological signs. Frequent detection of alternative pathogens suggests that the high case fatality rates were probably related to opportunistic infections resulting from CDV-induced immune suppression and not CDV spreading into the CNS. This fits with observations made in cynomolgus macaques experimentally inoculated with CDV , rapid infection of lymphocytes and lymphopenia, while CDV was not detected in the CNS (de Vries et al. 2014).
9.4 Macaque Model for Measles Pathogenesis
Studies in NHPs have been crucial for our understanding of measles pathology and pathogenesis in humans. After initial macaque studies with filtered respiratory secretions from measles patients in the beginning of the twentieth century identified MV as the causative agent of measles (Goldberger and Anderson 1911), studies in the 1960s with measles virus isolates passaged in vitro provided the basis for currently used live-attenuated measles vaccines. More recently, measles pathogenesis was elucidated by performing experimental infections of different NHP species – mainly cynomolgus and rhesus macaques – with recombinant MV expressing a fluorescent reporter protein. These viruses allow for sensitive detection of morbillivirus-infected cells, which can be visualized macroscopically (Figs. 9.1c, d and 14.2g) and microscopically (Figs. 9.2 and 14.3). These experiments have provided critical contributions to our understanding of MV entry of a host, dissemination throughout a host, and transmission to a subsequent host.
9.4.1 Alternative Measles Animal Models
A variety of animal species has been considered in models of MV infection. Although small laboratory animals seem most attractive, these do not recapitulate the complex pathogenesis of measles as seen in NHPs and humans. Therefore, two options for animal models remain: experimental infections with animal morbilliviruses in their natural host species (e.g., CDV infection of ferrets (von Messling et al. 2003; Ludlow et al. 2012; de Vries et al. 2017)) or experimental infection of NHPs with MV (de Swart 2009; 2017).
9.4.2 Measles Pathogenesis
9.4.2.1 MV Receptors In Vivo
MV is regarded one of the most infectious human pathogens that efficiently spreads through airborne transmission (Herfst et al. 2017). Although initial infection with MV indeed occurs in the respiratory tract, it is not epithelial cells that are initially targeted rather, after host entry measles becomes a systemic disease involving infection of various cell types. Infection of the various cell types is mainly governed by expression of one of the two cellular entry receptors identified to play a role in wild-type MV infections, CD150 (Tatsuo et al. 2000), and nectin-4 (Noyce et al. 2011; Muhlebach et al. 2011). The development of recombinant MV strains that express fluorescent reporter proteins, combined with the large spectrum of antibodies available for specific phenotyping of NHP cell types, have confirmed the use of these receptors in vivo.
De Swart et al. inoculated rhesus and cynomolgus macaques with recombinant MV expressing enhanced green fluorescent protein (EGFP) via the intra-tracheal route and followed infected animals in time. Blood samples were taken regularly and analyzed by flow cytometry. Co-staining of the MV-infected (or EGFP+) cells with CD150 proved that CD150+ lymphocytes and dendritic cells (DC) were predominantly infected during MV infection of macaques (de Swart et al. 2007a). The importance of interactions between MV and CD150 was subsequently confirmed by the generation of so-called “receptor-blind” viruses, viruses containing a single point mutation in the H protein and therefore poorly able to bind to CD150. When rhesus macaques were infected with a CD150-blind virus via the intranasal route, clinical symptoms were only observed in 1/6 animals. Surprisingly, all animals seroconverted so were apparently infected at a low level (Leonard et al. 2010), proving that entry occurred, albeit inefficiently.
Whereas CD150 is critical for entry and dissemination, the receptor nectin-4 plays an important role in host exit and transmission to the subsequent host. MV only spreads to the respiratory tract epithelium relatively late in infection (Ludlow et al. 2013a, b), through interactions between MV-infected lymphoid or myeloid cells with the basolateral side of epithelial cells. When cynomolgus macaques were infected with a nectin-4-blind virus, MV was cleared more rapidly from the host and could not be detected in secretions from the throat or nose. By performing immunohistochemistry, it was shown that the nectin-4-blind virus did not infect epithelial cells in the trachea, whereas wild-type MV did (Frenzke et al. 2013). Similar observations were made when a wild-type and nectin-4-blind MV were compared side-by-side in a New World monkey model, namely, squirrel monkeys (Saimiri sciureus ) (Delpeut et al. 2017).
9.4.2.2 MV Entry of the Host
Although the role of the different receptors was accurately elucidated in monkeys as described above, formal proof of the initial target cells of MV in vivo came from a study in which macaques were allowed to inhale recombinant MV expressing EGFP as an aerosol. Since most MV studies in NHPs were performed by inoculating animals with virus via the intra-tracheal or intra-nasal route, not per se reflecting the natural situation, de Vries et al. invested in setting up an aerosol inhalation model for NHPs (de Vries et al. 2010; Lemon et al. 2011; MacLoughlin et al. 2016). In a study specifically designed to identify the initial target cells of MV , which were classically believed to be epithelial cells in the respiratory tract, cynomolgus macaques were exposed to a high dose MV administered as an aerosol and sacrificed at early time points post inoculation. Interestingly, alveolar macrophages (AM) and DC in the lower respiratory tract were identified as initial target cells (Fig. 9.2a), contradictory to the literature at that time that stated that measles starts with MV infection of epithelial cells in the respiratory tract (Lemon et al. 2011). An early time course of measles pathogenesis in NHPs was established in this study, starting with MV infection of AM and DC in the lower respiratory tract, followed by spread to bronchus-associated lymphoid tissues (BALT) (Fig. 9.2c) and draining lymph nodes and local amplification, before the virus spread systemically and could be detected in the blood and all lymphoid organs (Fig. 9.2d) (Lemon et al. 2011). This time course fits completely with the presence of the different receptors on target cells.
9.4.2.3 MV Clearance from the Host
After systemic spread of MV throughout the host, a peak of virus replication in macaques is usually observed between 7 and 10 days post inoculation, followed by a rapid decline in infected cells in the blood. This rapid decline is mediated by the virus-specific immune response of the host. Although virus neutralizing antibodies are considered the main correlate of protection against MV infection (Chen et al. 1990), viral clearance is predominantly mediated by cellular immune responses. This was originally observed in “experiments of nature,” in hypogammaglobulinemic children (lacking proper antibody formation) who recover normally from MV infection (Good and Zak 1956; Nahmias et al. 1967), whereas children with deficits in cellular immune responses develop severe disease and display prolonged viral shedding (Burnet 1968; Permar et al. 2001). These observational studies were confirmed in NHPs . Permar et al. experimentally inoculated NHPs and determined the immunological drivers of viral clearance by depleting these monkeys of either CD8+ T-lymphocytes or B-lymphocytes. Similar to the observations made in children, macaques depleted of B-lymphocytes were able to normally clear virus (Permar et al. 2004), whereas CD8+ T-lymphocyte-depleted macaques presented with a more extensive rash, higher viral loads, and a longer duration of viremia (Permar et al. 2003).
9.4.2.4 MV Transmission to the Subsequent Host
MV is regarded one of the most contagious viruses infecting humans – each infected person can transmit the virus to an average of 15–20 susceptible individuals. Macaque studies have been crucial in the understanding as to how this high rate of transmission is achieved. MV is spread from host-to-host via airborne transmission. Respiratory droplets filled with virus particles are produced by sneezing and coughing and enter the respiratory tract of a susceptible host. As mentioned above, MV uses two different cellular receptors to enter different cell types, and CD150 is regarded as the important “host entry” receptor for MV . Nectin-4 is actually regarded as the “host exit” receptor for MV that facilitates host-to-host transmission. Expression of nectin-4 was shown to be widespread in both the macaque upper and lower respiratory tract (Muhlebach et al. 2011; Ludlow et al. 2013b). When macaques were experimentally infected with MV expressing a fluorescent reporter, the virus was abundantly present in the nasal cavity during the late stage of the infection (around onset of rash) (Ludlow et al. 2013b), and in experimental infections of NHPs with wild-type viruses, cell-free and cell-associated MV can readily be isolated from nose and throat swabs (Ludlow et al. 2013a).
Based on these macaque studies, and studies that were performed with a nectin-4-blind strain of MV , an “exit strategy” for MV was postulated. MV initially enters the host via DC and AM and is amplified locally before systemic spread. After systemic spread, infected cells (probably lymphocytes) return to the respiratory tract and transfer MV to epithelial cells, where it binds nectin-4 on the basolateral side of the epithelium (Fig. 9.2e). Novel virus particles are subsequently produced and released at the apical side of the epithelium, directly into the airway. Here, aerosol is produced due to coughing and sneezing, facilitating host exit and transmission (Racaniello 2011). In addition to the release of cell-free MV into the respiratory tract, there is also evidence for cell-associated spread of MV to the subsequent host. Disrupted epithelium and cell debris was frequently observed in the respiratory tract of MV-infected macaques, in addition to disruption of tonsillar epithelium (Fig. 9.2f). This epithelial disruption would lead to induction of coughing and sneezing responses, leading to expulsion of cell-free virus produced by lymphocytes, and cell debris exuding from the respiratory submucosa or tonsillar tissues (Ludlow et al. 2013a). Additionally, cell-free virus in the airways encounters relatively little receptor-expressing cells and therefore can remain present in the mucus of the respiratory tract.
9.4.2.5 Measles-Associated Immune Suppression in NHPs
One of the most important clinical sequelae of measles is immune suppression, which is the main cause of measles morbidity and mortality. Interestingly, measles normally causes lymphopenia early after inoculation of NHPs and reduces host resistance to other infections (de Vries et al. 2012) while simultaneously inducing a strong immune response to itself that results in life-long protection from measles. The mechanism behind this “measles paradox,” simultaneous immune suppression and immune activation, was elucidated by performing a comprehensive study of virological, immunological, hematological, and histopathological observations made in NHPs euthanized after MV infection via various infection routes. In NHPs , it was observed that MV preferentially infects certain subsets of T- and B-lymphocytes, namely, memory T- and follicular B-lymphocytes. Depletion of these cells was predominantly observed in the lymphoid tissues of these animals (exemplified by heavy infection of Peyer’s patches in experimentally infected animals in Fig. 9.2g) (de Vries et al. 2012). Multinucleated giant cells are abundant in all lymphoid tissues (Fig. 9.2h), and immunofluorescence staining indicated that these were of a B-lymphocyte origin (CD20-positive, while CD11c- and CD3-negative) (Fig. 9.3).
Images collected from lymphoid tissues obtained from experimentally infected NHPs at 7 days post inoculation (d.p.i.), illustrating that multinucleated giant cells are mainly from a B-lymphocyte origin. MV-infected cells were detected by immunofluorescent double staining. (a–c) Large numbers of syncytia were observed in the B-lymphocyte follicles and were stained for EGFP (green) as a marker of MV infection. Double stains were performed with a B-lymphocyte marker (CD20, red, a1 and a2), a macrophage/dendritic cell marker (CD11c, red, b1 and b2), or a T cell marker (CD3, red, c1 and c2), and DAPI was used to counterstain the nuclei (blue). Top panels only show the red and blue channels; bottom panels show the combined red, blue and green channels. Multi-nucleated giant cells were mainly of B-lymphocyte origin (panel a), and the infection was associated with significant cytopathic effects in lymphoid tissues. All panels reprinted from supplementary data of De Vries et al., PLoS Pathog 2012
In a follow-up publication, the authors described the rapid expansion of MV-specific and bystander lymphocytes following MV clearance as the cause of resolution of lymphopenia. However, the immunological repertoire at that time is still severely limited, causing what the authors termed a temporary “immunological amnesia” (de Vries and de Swart 2014). This model explains that measles immune suppression can last for several weeks to months after recovery from measles, whereas lymphopenia is normally rapidly resolved (Mina et al. 2015). Preferential infection of CD150+ lymphocyte subsets as observed in NHPs was recently confirmed in humans (Laksono et al. 2018).
9.5 Macaque Model for Vaccine Evaluation
In addition to the crucial role NHPs played in studying MV tropism and pathogenesis, these animals have also been used to evaluate new generation MV vaccines and novel routes of MV vaccination (van Binnendijk et al. 1997; Zhu et al. 1997; Polack et al. 2000; Combredet et al. 2003). Live-attenuated measles vaccines are safe and effective and have successfully interrupted endemic MV transmission in large geographical areas. Although currently used live-attenuated MV vaccines have already been in successful use for over 50 years, surprisingly little was known about the target cells that sustain vaccine virus replication in vivo, and the molecular basis for attenuation has remained elusive. It has been known for some time that vaccine viruses have the ability to use an additional cellular entry receptor in vitro, namely, CD46 (Dorig et al. 1993; Naniche et al. 1993; Buckland and Wild 1997), which is expressed on virtually all nucleated cells (Liszewski and Atkinson 1992). However, neither the extent of use of CD46 in vivo nor the tropism of vaccine viruses was known. Macaque studies have shown that after aerosol, intra-tracheal, and intra-muscular administration, vaccine viruses still predominantly replicate in CD150-expressing cells (de Vries et al. 2010; Rennick et al. 2015; de Swart et al. 2017). In the respiratory tract, CD11c+ or CD68+ myeloid cells (CD150-positive) were predominantly infected by live-attenuated MV (de Vries et al. 2010; de Swart et al. 2017), whereas DC and macrophages (CD150-positive) were identified as the predominant target cells of live-attenuated MV after intra-muscular administration (Rennick et al. 2015).
9.5.1 Alternative Measles Vaccines
Despite their success, live-attenuated MV vaccines have several limitations. These include dependency on maintaining the cold chain, requirement for trained health-care workers for administration, and the need for hypodermic needles and safe waste disposal. To address some of these issues, different vaccination platforms for MV have been investigated. Initially, vectored approaches have been evaluated in NHPs , in which macaques were vaccinated with poxviruses expressing the MV surface fusion (F) and H glycoproteins (Stittelaar et al. 2000; Zhu et al. 2000). Vaccine efficacy was demonstrated, but the macaque model was of added value in these studies, as vaccine efficacy could also be addressed in the presence of passively transferred antibodies (simulating the presence of maternal antibodies in infants) (Stittelaar et al. 2000) or in immune-suppressed macaques to evaluate safety in immunocompromised (Stittelaar et al. 2001). Furthermore, alphavirus replicons generated to express both the MV -F and MV -H protein also showed efficacy in macaques.
In addition to vectored vaccine approaches, direct DNA vaccination was evaluated as potential novel MV vaccine in macaques. In these studies, macaques could be protected from wildtype MV challenge by prior vaccination with DNA expressing the F and/or H gene (Polack et al. 2000; Lin et al. 2013). In other studies priming of cellular immune responses was observed (Stittelaar et al. 2002). Again, these novel vaccines could also be evaluated for efficacy in the presence of passively acquired antibodies in the macaque model (Premenko-Lanier et al. 2003).
9.5.2 Alternative Measles Vaccine Administration Routes
In addition to the generation of novel measles vaccines, different routes of administration were also investigated. The focus of this research was predominantly on the generation of needle-free MV vaccination regimens. Vaccine delivery via aerosol inhalation has been considered as a promising possibility (Griffin 2014). Clinical trials have already extensively demonstrated the feasibility of this administration route (Sabin et al. 1984; Dilraj et al. 2000, 2007; Low et al. 2008, 2015).
To support licensing of novel vaccine administration routes, both pre-clinical and clinical studies are required. Inhalation administration routes were extensively investigated in NHPs , comparing administration of the MV vaccine via aerosol inhalation and dry powder inhalation directly with injection (de Swart et al. 2006, 2007b; Lin et al. 2011). In general, aerosol inhalation induced similar immune responses as detected in the injection group and protected macaques from wild-type MV challenge. Variable results were obtained with dry powder. A more recent large-scale study in macaques investigated both the tropism of recombinant vaccine viruses expressing fluorescent reporter proteins and whether vaccination should target the upper or lower respiratory tract to be immunogenic. In this study, four administration routes were compared: intra-tracheal inoculation, intra-nasal instillation, aerosol inhalation, and intra-muscular injection. This study showed that delivery of vaccine virus to the lower respiratory tract is crucial in order to induce optimal immune responses and protection from challenge (de Swart et al. 2017).
In addition to needle-free vaccine administration via the respiratory route, another promising alternative for the use of hypodermic needles is to deliver live-attenuated MV via microneedle patches. Microneedle patches are micron-scale dissolvable polymeric needles that were designed to encapsidate the standard live-attenuated MV . These patches can directly be applied to the skin for intra-dermal vaccination, without the requirement of vaccine reconstitution. NHPs have again been critical to provide the proof of principle of this approach (Edens et al. 2013, 2015).
9.6 Crossing the Species Barrier
9.6.1 Measles Eradication
After the eradication of smallpox, the potential for measles eradication was first proposed in the 1980s. In this period, interruption of endemic MV circulation had not yet been achieved, and eradication of MV was considered to be premature (Henderson 1982). However, in 2001 a formal initiative was established, known as the Measles and Rubella Initiative (https://measlesrubellainitiative.org), which aimed at reduction of global measles mortality (in addition to reducing the number of congenital rubella cases) by initiating mass vaccination campaigns and two-dose vaccination regimens. An impressive reduction in measles mortality has been obtained since then, with the current measles mortality at an all-time low (WHO 2017). Eradication of MV from the globe is considered feasible, as MV is a monotypic virus that exclusively circulates in humans, and an effective live-attenuated vaccine is available (Moss and Strebel 2011). Furthermore, in 2011 rinderpest was officially declared eradicated from the globe. Since RPV is a close relative of MV , targeted eradication of MV should also be feasible (Morens et al. 2011; Roeder 2011; de Swart et al. 2012). However, there are pitfalls like waning vaccine immunity and declining vaccination coverage, as was clearly demonstrated by the by the difficult endgame of poliovirus eradication (Cochi and Linkins 2012). Furthermore, recent spread of animal morbilliviruses into NHPs illustrates that we should be aware of zoonotic morbillivirus infections in a measles post-eradication era (Qiu et al. 2011; Sakai et al. 2013a; Yoshikawa et al. 1989; Sun et al. 2010).
9.6.2 Post-measles Eradication Era and Implications for One Health
While measles eradication would save many lives, it is also likely to result in reduced compliance to MV vaccination. As a result, many children will grow up without MV-specific immunity, similar to the scenario as observed with smallpox. In the case of smallpox, vaccination was discontinued, thus creating a niche for closely related orthopoxviruses of other mammals to cross the species barrier into humans (Essbauer et al. 2010; Reynolds et al. 2012; Reynolds and Damon 2012). Since we already know that morbillivirus infections induce at least partial cross-protection from other morbilliviruses (Strating 1975), cessation of MV vaccination after eradication might also facilitate cross-species infection and subsequent adaptation of animal morbilliviruses to humans (Cosby 2012). Historically, CDV infections in humans have been described, and some humans have serological evidence for CDV infection (Nicolle 1931; Adams 1952; DeLay et al. 1965). More compelling evidence for the capacity of CDV to adapt to primates comes from outbreaks in monkey colonies, as described above (Qiu et al. 2011; Sakai et al. 2013a; Yoshikawa et al. 1989; Sun et al. 2010). These outbreaks had high mortality rates, indicating that an outbreak of an adapted CDV in MV-naive humans could have catastrophic consequences. An additional concern is that CDV is known to be neurotropic and was shown to have replicate efficiently in experimentally infected NHPs (de Vries et al. 2014).
Therefore, the potential of non-MV morbilliviruses, especially CDV , to adapt to humans should be held in mind in measles eradication scenarios. Currently, immunity in the human population due to MV infection or MV vaccination results in immunity against other morbilliviruses and restricts the possibility of animal morbilliviruses adapting to humans. However, if the envisaged measles eradication leads to a significant drop in vaccination coverage, such adaptation cannot be excluded. For this reason, MV vaccination and serological and virological surveillance of morbillivirus infections in the human population should be maintained, even in a measles post-eradication era.
9.7 Conclusions
NHPs have played a crucial rule in MV research since the beginning of the twentieth century and continue to do so. MV was initially discovered to be the causative agent of measles by transfer of filtered respiratory tract secretions from measles patients to macaques. Since then, research in NHPs with laboratory-adapted, live-attenuated, and wild-type viruses, sometimes engineered to express fluorescent proteins or to be incapable of binding cellular receptors, have further elucidated measles pathogenesis, from entry into the host to dissemination throughout the host and transmission to the subsequent host and the induction of immune suppression. Additionally, although free-ranging NHP populations are thought not to support endemic MV circulation, they are highly susceptible to natural MV infection (or infection with other morbilliviruses, like CDV ). Demographic changes, including the increasing human population size, urbanization, and deforestation, may lead to increased interactions between humans and NHPs (Gortazar et al. 2014). Introduction of a highly contagious MV in a high-density population or captive colony seronegative for MV can easily lead to an efficient transmission chain in which all animals become infected. Secondary infections due to morbillivirus-induced immune suppression can subsequently give complications, leading to outbreaks with high morbidity and mortality. Therefore, MV-seronegative captive colonies should be protected from MV introduction by vaccination or preventing contact with MV-infected individuals. Furthermore, a close interface between humans and free-living NHPs , mainly due to ecotourism and growth of the human population, increases the potential for spread of MV into susceptible monkey and ape populations and vice versa.
References
Adams JM (1952) Pathological and serological relationships between canine distemper and a respiratory tract infection of human beings. Am J Dis Child 84(4):466–468
Albrecht P, Lorenz D, Klutch MJ (1981) Encephalitogenicity of measles virus in marmosets. Infect Immun 34(2):581–587
Andrade MR, Yee J, Barry P, Spinner A, Roberts JA, Cabello PH et al (2003) Prevalence of antibodies to selected viruses in a long-term closed breeding colony of rhesus macaques (Macaca mulatta) in Brazil. Am J Primatol 59(3):123–128. https://doi.org/10.1002/ajp.10069
Appel MJ, Reggiardo C, Summers BA, Pearce-Kelling S, Mare CJ, Noon TH et al (1991) Canine distemper virus infection and encephalitis in javelinas (collared peccaries). Arch Virol 119(1–2):147–152. https://doi.org/10.1007/Bf01314331
Auwaerter PG, Rota PA, Elkins WR, Adams RJ, DeLozier T, Shi Y et al (1999) Measles virus infection in rhesus macaques: altered immune responses and comparison of the virulence of six different virus strains. J Infect Dis 180(4):950–958. https://doi.org/10.1086/314993
Barrett T (1999) Morbillivirus infections, with special emphasis on morbilliviruses of carnivores. Vet Microbiol 69(1–2):3–13. https://doi.org/10.1016/S0378-1135(99)00080-2
Beineke A, Puff C, Seehusen F, Baumgartner W (2009) Pathogenesis and immunopathology of systemic and nervous canine distemper. Vet Immunol Immunopathol 127(1–2):1–18. https://doi.org/10.1016/j.vetimm.2008.09.023
Buckland R, Wild TF (1997) Is CD46 the cellular receptor for measles virus? Virus Res 48(1):1–9
Burnet FM (1968) Measles as an index of immunological function. Lancet 2(7568):610–613
Byers AC, Hastings BE (1991) Mountain gorilla mortality in the Parc National des Volcans, Ruhengeri Prefecture, Rwanda, 1988. Possible contributing climatic factors. Mt Res Dev 11:145–151
Chen RT, Markowitz LE, Albrecht P, Stewart JA, Mofenson LM, Preblud SR et al (1990) Measles antibody: reevaluation of protective titers. J Infect Dis 162(5):1036–1042
Choi YK, Simon MA, Kim DY, Yoon BI, Kwon SW, Lee KW et al (1999) Fatal measles virus infection in Japanese macaques (Macaca fuscata). Vet Pathol 36(6):594–600. https://doi.org/10.1354/Vp.36-6-594
Cochi SL, Linkins RW (2012) The final phase of polio eradication: new vaccines and complex choices. J Infect Dis 205(2):169–171. https://doi.org/10.1093/infdis/jir727
Combredet C, Labrousse V, Mollet L, Lorin C, Delebecque F, Hurtrel B et al (2003) A molecularly cloned Schwarz strain of measles virus vaccine induces strong immune responses in macaques and transgenic mice. J Virol 77(21):11546–11554. https://doi.org/10.1128/Jvi.77.21.11546-11554-2003
Cosby SL (2012) Morbillivirus cross-species infection: is there a risk for humans? Futur Virol 7:1103–1113
de Swart RL (2009) Measles studies in the macaque model. Curr Top Microbiol Immunol 330:55–72
de Swart RL (2017) Measles: what we have learned from non-human primate models. Drug Discov Today Dis Mod 23(Special Issue: Use of non-human primate disease models):31–34
de Swart RL, Kuiken T, Fernandez-de Castro J, Papania MJ, Bennett JV, Valdespino JL et al (2006) Aerosol measles vaccination in macaques: preclinical studies of immune responses and safety. Vaccine 24(40–41):6424–6436. https://doi.org/10.1016/j.vaccine.2006.05.125
de Swart RL, Ludlow M, de Witte L, Yanagi Y, van Amerongen G, McQuaid S et al (2007a) Predominant infection of CD150+ lymphocytes and dendritic cells during measles virus infection of macaques. PLoS Pathog 3(11):e178. https://doi.org/10.1371/journal.ppat.0030178
de Swart RL, LiCalsi C, Quirk AV, van Amerongen G, Nodelman V, Alcock R et al (2007b) Measles vaccination of macaques by dry powder inhalation. Vaccine 25(7):1183–1190. https://doi.org/10.1016/j.vaccine.2006.10.019
de Swart RL, Duprex WP, Osterhaus AD (2012) Rinderpest eradication: lessons for measles eradication? Curr Opin Virol 2(3):330–334. https://doi.org/10.1016/j.coviro.2012.02.010
de Swart RL, de Vries RD, Rennick LJ, van Amerongen G, McQuaid S, Verburgh RJ et al (2017) Needle-free delivery of measles virus vaccine to the lower respiratory tract of non-human primates elicits optimal immunity and protection. NPJ Vaccines 2:22. https://doi.org/10.1038/s41541-017-0022-8
de Vries RD, de Swart RL (2014) Measles immune suppression: functional impairment or numbers game? PLoS Pathog 10(12):e1004482. https://doi.org/10.1371/journal.ppat.1004482
de Vries RD, Lemon K, Ludlow M, McQuaid S, Yuksel S, van Amerongen G et al (2010) In vivo tropism of attenuated and pathogenic measles virus expressing green fluorescent protein in macaques. J Virol 84(9):4714–4724. https://doi.org/10.1128/JVI.02633-09
de Vries RD, McQuaid S, van Amerongen G, Yuksel S, Verburgh RJ, Osterhaus AD et al (2012) Measles immune suppression: lessons from the macaque model. PLoS Pathog 8(8):e1002885. https://doi.org/10.1371/journal.ppat.1002885
de Vries RD, Ludlow M, Verburgh RJ, van Amerongen G, Yuksel S, Nguyen DT et al (2014) Measles vaccination of nonhuman primates provides partial protection against infection with canine distemper virus. J Virol 88(8):4423–4433. https://doi.org/10.1128/JVI.03676-13
de Vries RD, Ludlow M, de Jong A, Rennick LJ, Verburgh RJ, van Amerongen G et al (2017) Delineating morbillivirus entry, dissemination and airborne transmission by studying in vivo competition of multicolor canine distemper viruses in ferrets. PLoS Pathog 13(5):e1006371. https://doi.org/10.1371/journal.ppat.1006371
DeLay PD, Stone SS, Karzon DT, Katz S, Enders J (1965) Clinical and immune response of alien hosts to inoculation with measles, rinderpest, and canine distemper viruses. Am J Vet Res 26(115):1359–1373
Delpeut S, Sawatsky B, Wong XX, Frenzke M, Cattaneo R, von Messling V (2017) Nectin-4 interactions govern measles virus virulence in a new model of pathogenesis, the squirrel monkey (Saimiri sciureus). J Virol 91(11):e02490–e02416. https://doi.org/10.1128/JVI.02490-16
Dilraj A, Cutts FT, de Castro JF, Wheeler JG, Brown D, Roth C et al (2000) Response to different measles vaccine strains given by aerosol and subcutaneous routes to schoolchildren: a randomised trial. Lancet 355(9206):798–803. https://doi.org/10.1016/S0140-6736(99)95140-1
Dilraj A, Sukhoo R, Cutts FT, Bennett JV (2007) Aerosol and subcutaneous measles vaccine: measles antibody responses 6 years after re-vaccination. Vaccine 25(21):4170–4174. https://doi.org/10.1016/j.vaccine.2007.03.003
Dorig RE, Marcil A, Chopra A, Richardson CD (1993) The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 75(2):295–305
Drewe JA, O’Riain MJ, Beamish E, Currie H, Parsons S (2012) Survey of infections transmissible between baboons and humans, Cape Town, South Africa. Emerg Infect Dis 18(2):298–301. https://doi.org/10.3201/eid1802.111309
Durrheim DN, Crowcroft NS (2017) The price of delaying measles eradication. Lancet Public Health 2(3):e130–e131. https://doi.org/10.1016/S2468-2667(17)30026-9
Durrheim DN, Crowcroft NS, Strebel PM (2014) Measles—the epidemiology of elimination. Vaccine 32(51):6880–6883. https://doi.org/10.1016/j.vaccine.2014.10.061
Edens C, Collins ML, Ayers J, Rota PA, Prausnitz MR (2013) Measles vaccination using a microneedle patch. Vaccine 31(34):3403–3409. https://doi.org/10.1016/j.vaccine.2012.09.062
Edens C, Collins ML, Goodson JL, Rota PA, Prausnitz MR (2015) A microneedle patch containing measles vaccine is immunogenic in non-human primates. Vaccine 33(37):4712–4718. https://doi.org/10.1016/j.vaccine.2015.02.074
El Mubarak HS, Yuksel S, van Amerongen G, Mulder PGH, Mukhtar MM, Osterhaus ADME et al (2007) Infection of cynomolgus macaques (Macaca fascicularis) and rhesus macaques (Macaca mulatta) with different wild-type measles viruses. J Gen Virol 88(7):2028–2034. https://doi.org/10.1099/vir.0.82804-0
Enders JF, Peebles TC (1954) Propagation in tissue cultures of cytopathogenic agents from patients with measles. Proc Soc Exp Biol Med 86(2):277–286
Epstein JH, Price JT (2009) The significant but understudied impact of pathogen transmission from humans to animals. Mt Sinai J Med 76(5):448–455. https://doi.org/10.1002/msj.20140
Essbauer S, Pfeffer M, Meyer H (2010) Zoonotic poxviruses. Vet Microbiol 140(3–4):229–236. https://doi.org/10.1016/j.vetmic.2009.08.026
Finkeldey W (1931) Über Riesenzellbefunde in den Gaumenmandeln, zugleich ein Beitrag zur Histopathologie der Mandelveränderungen im Maserninkubationsstadium. Virchows Arch 281:323–329
Fraser CE, Chalifoux L, Sehgal P, Hunt RD, King NW (1978) A paramyxovirus causing fatal gastroenterocolitis in marmoset monkeys. Primates Med 10:261–270
Frenzke M, Sawatsky B, Wong XX, Delpeut S, Mateo M, Cattaneo R et al (2013) Nectin-4-dependent measles virus spread to the cynomolgus monkey tracheal epithelium: role of infected immune cells infiltrating the lamina propria. J Virol 87(5):2526–2534. https://doi.org/10.1128/JVI.03037-12
Goldberger J, Anderson JF (1911) An experimental demonstration of the presence of the virus of measles in the mixed buccal and nasal secretions. J Am Med Assoc 57:476–478
Good RA, Zak SJ (1956) Disturbances in gamma globulin synthesis as experiments of nature. Pediatrics 18(1):109–149
Gortazar C, Reperant LA, Kuiken T, de la Fuente J, Boadella M, Martinez-Lopez B et al (2014) Crossing the interspecies barrier: opening the door to zoonotic pathogens. PLoS Pathog 10(6):e1004129. https://doi.org/10.1371/journal.ppat.1004129
Griffin DE (2013) Measles virus. In: Knipe DM, Howley PM (eds) Fields Virology. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, pp 1042–1069
Griffin DE (2014) Current progress in pulmonary delivery of measles vaccine. Expert Rev Vaccines 13(6):751–759. https://doi.org/10.1586/14760584.2014.915753
Hall WC, Kovatch RM, Herman PH, Fox JG (1971) Pathology of measles in rhesus monkeys. Vet Pathol 8(4):307–319
Hastings BE, Kenny D, Lowenstine LJ, Foster JW (1991) Mountain gorillas and measles: ontogeny of a wildlife vaccination program. Proc Am Assoc Zoo Vet 1991:198–205
Henderson DA (1982) Global measles eradication. Lancet 2(8291):208
Herfst S, Bohringer M, Karo B, Lawrence P, Lewis NS, Mina MJ et al (2017) Drivers of airborne human-to-human pathogen transmission. Curr Opin Virol 22:22–29. https://doi.org/10.1016/j.coviro.2016.11.006
Hime JM, Keymer IF, Baxter CJ (1975) Measles in recently imported colobus monkeys (Colobus guereza). Vet Rec 97(20):392
Jones-Engel L, Engel GA, Schillaci MA, Lee B, Heidrich J, Chalise M et al (2006) Considering human-primate transmission of measles virus through the prism of risk analysis. Am J Primatol 68(9):868–879. https://doi.org/10.1002/ajp.20294
Kaur T, Singh J, Tong S, Humphrey C, Clevenger D, Tan W et al (2008) Descriptive epidemiology of fatal respiratory outbreaks and detection of a human-related metapneumovirus in wild chimpanzees (Pan troglodytes) at Mahale Mountains National Park, Western Tanzania. Am J Primatol 70(8):755–765. https://doi.org/10.1002/ajp.20565
Kessler MJ, London WT, Madden DL, Dambrosia JM, Hilliard JK, Soike KF et al (1989) Serological survey for viral diseases in the Cayo Santiago rhesus macaque population. P R Health Sci J 8(1):95–97
Kondgen S, Kuhl H, N’Goran PK, Walsh PD, Schenk S, Ernst N et al (2008) Pandemic human viruses cause decline of endangered great apes. Curr Biol 18(4):260–264. https://doi.org/10.1016/j.cub.2008.01.012
Laksono BM, de Vries RD, Verburgh RJ, Visser EG, de Jong A, Fraaij PLA et al (2018) Studies into the mechanism of measles-associated immune suppression during a measles outbreak in the Netherlands. Nat Commun 9(1):4944
Lemon K, de Vries RD, Mesman AW, McQuaid S, van Amerongen G, Yuksel S et al (2011) Early target cells of measles virus after aerosol infection of non-human primates. PLoS Pathog 7(1):e1001263. https://doi.org/10.1371/journal.ppat.1001263
Leonard VH, Hodge G, Reyes-Del Valle J, McChesney MB, Cattaneo R (2010) Measles virus selectively blind to signaling lymphocytic activation molecule (SLAM; CD150) is attenuated and induces strong adaptive immune responses in rhesus monkeys. J Virol 84(7):3413–3420. https://doi.org/10.1128/JVI.02304-09
Levy BM, Mirkovic RR (1971) An epizootic of measles in a marmoset colony. Lab Anim Sci 21(1):33–39
Lin WH, Griffin DE, Rota PA, Papania M, Cape SP, Bennett D et al (2011) Successful respiratory immunization with dry powder live-attenuated measles virus vaccine in rhesus macaques. Proc Natl Acad Sci U S A 108(7):2987–2992. https://doi.org/10.1073/pnas.1017334108
Lin WH, Vilalta A, Adams RJ, Rolland A, Sullivan SM, Griffin DE (2013) Vaxfectin adjuvant improves antibody responses of juvenile rhesus macaques to a DNA vaccine encoding the measles virus hemagglutinin and fusion proteins. J Virol 87(12):6560–6568. https://doi.org/10.1128/JVI.00635-13
Liszewski MK, Atkinson JP (1992) Membrane cofactor protein. Curr Top Microbiol Immunol 178:45–60
Lorenz D, Albrecht P (1980) Susceptibility of tamarins (Saguinus) to measles virus. Lab Anim Sci 30(4 Pt 1):661–665
Low N, Kraemer S, Schneider M, Restrepo AM (2008) Immunogenicity and safety of aerosolized measles vaccine: systematic review and meta-analysis. Vaccine 26(3):383–398. https://doi.org/10.1016/j.vaccine.2007.11.010
Low N, Bavdekar A, Jeyaseelan L, Hirve S, Ramanathan K, Andrews NJ et al (2015) A randomized, controlled trial of an aerosolized vaccine against measles. N Engl J Med 372(16):1519–1529. https://doi.org/10.1056/NEJMoa1407417
Ludlow M, Nguyen DT, Silin D, Lyubomska O, de Vries RD, von Messling V et al (2012) Recombinant canine distemper virus strain Snyder Hill expressing green or red fluorescent proteins causes meningoencephalitis in the ferret. J Virol 86(14):7508–7519. https://doi.org/10.1128/JVI.06725-11
Ludlow M, de Vries RD, Lemon K, McQuaid S, Millar E, van Amerongen G et al (2013a) Infection of lymphoid tissues in the macaque upper respiratory tract contributes to the emergence of transmissible measles virus. J Gen Virol 94(Pt 9):1933–1944. https://doi.org/10.1099/vir.0.054650-0
Ludlow M, Lemon K, de Vries RD, McQuaid S, Millar EL, van Amerongen G et al (2013b) Measles virus infection of epithelial cells in the macaque upper respiratory tract is mediated by subepithelial immune cells. J Virol 87(7):4033–4042. https://doi.org/10.1128/JVI.03258-12
Ludlow M, Rennick LJ, Nambulli S, de Swart RL, Duprex WP (2014) Using the ferret model to study morbillivirus entry, spread, transmission and cross-species infection. Curr Opin Virol 4:15–23. https://doi.org/10.1016/j.coviro.2013.11.001
MacArthur JA, Mann PG, Oreffo V, Scott GB (1979) Measles in monkeys: an epidemiological study. J Hyg 83(2):207–212
MacLoughlin RJ, van Amerongen G, Fink JB, Janssens HM, Duprex WP, de Swart RL (2016) Optimization and dose estimation of aerosol delivery to non-human primates. J Aerosol Med Pulm Drug Deliv 29(3):281–287. https://doi.org/10.1089/jamp.2015.1250
Matsubara Y, Morikawa Y, Yoshikawa Y, Nagashima K, Yamanouchi K (1985) Encephalitis induced in non-human primates by canine distemper virus adapted to human neural cells. Jpn J Exp Med 55(3):99–108
Meyer HM Jr, Brooks BE, Douglas RD, Rogers NG (1962) Ecology of measles in monkeys. Am J Dis Child 103:307–313
Mina MJ, Metcalf CJ, de Swart RL, Osterhaus AD, Grenfell BT (2015) Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science 348(6235):694–699. https://doi.org/10.1126/science.aaa3662
Morens DM, Holmes EC, Davis AS, Taubenberger JK (2011) Global rinderpest eradication: lessons learned and why humans should celebrate too. J Infect Dis 204(4):502–505. https://doi.org/10.1093/infdis/jir327
Moss WJ, Strebel P (2011) Biological feasibility of measles eradication. J Infect Dis 204(Suppl 1):S47–S53. https://doi.org/10.1093/infdis/jir065
Muehlenbein MP, Martinez LA, Lemke AA, Ambu L, Nathan S, Alsisto S et al (2008) Perceived vaccination status in ecotourists and risks of anthropozoonoses. EcoHealth 5(3):371–378. https://doi.org/10.1007/s10393-008-0192-y
Muhlebach MD, Mateo M, Sinn PL, Prufer S, Uhlig KM, Leonard VH et al (2011) Adherens junction protein nectin-4 is the epithelial receptor for measles virus. Nature 480(7378):530–533. https://doi.org/10.1038/nature10639
Nagata T, Ochikubo F, Yoshikawa Y, Yamanouchi K (1990) Encephalitis induced by a canine distemper virus in squirrel monkeys. J Med Primatol 19(2):137–149
Nahmias AJ, Griffith D, Salsbury C, Yoshida K (1967) Thymic aplasia with lymphopenia, plasma cells, and normal immunoglobulins. Relation to measles virus infection. J Am Med Assoc 201(10):729–734
Naniche D, Varior-Krishnan G, Cervoni F, Wild TF, Rossi B, Rabourdin-Combe C et al (1993) Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J Virol 67(10):6025–6032
Nicolle C (1931) La maladie du jeune age des chiens est transmissible experimentalement a l’homme sous forme inapparente. Arch Inst Pasteur Tunis 20:321–323
Noyce RS, Bondre DG, Ha MN, Lin LT, Sisson G, Tsao MS et al (2011) Tumor cell marker PVRL4 (nectin 4) is an epithelial cell receptor for measles virus. PLoS Pathog 7(8):e1002240. https://doi.org/10.1371/journal.ppat.1002240
Origgi FC, Sattler U, Pilo P, Waldvogel AS (2013) Fatal combined infection with canine distemper virus and orthopoxvirus in a group of Asian marmots (Marmota caudata). Vet Pathol 50(5):914–920. https://doi.org/10.1177/0300985813476060
Peebles TC, McCarthy K, Enders JF, Holloway A (1957) Behavior of monkeys after inoculation of virus derived from patients with measles and propagated in tissue culture together with observations on spontaneous infections of these animals by an agent exhibiting similar antigenic properties. J Immunol 78(1):63–74
Permar SR, Moss WJ, Ryon JJ, Monze M, Cutts F, Quinn TC et al (2001) Prolonged measles virus shedding in human immunodeficiency virus-infected children, detected by reverse transcriptase-polymerase chain reaction. J Infect Dis 183(4):532–538. https://doi.org/10.1086/318533
Permar SR, Klumpp SA, Mansfield KG, Kim WK, Gorgone DA, Lifton MA et al (2003) Role of CD8+ lymphocytes in control and clearance of measles virus infection of rhesus monkeys. J Virol 77(7):4396–4400. https://doi.org/10.1128/Jvi.77.7.4396-4400.2003
Permar SR, Klumpp SA, Mansfield KG, Carville AA, Gorgone DA, Lifton MA et al (2004) Limited contribution of humoral immunity to the clearance of measles viremia in rhesus monkeys. J Infect Dis 190(5):998–1005. https://doi.org/10.1086/422846
Polack FP, Lee SH, Permar S, Manyara E, Nousari HG, Jeng Y et al (2000) Successful DNA immunization against measles: neutralizing antibody against either the hemagglutinin or fusion glycoprotein protects rhesus macaques without evidence of atypical measles. Nat Med 6(7):776–781. https://doi.org/10.1038/77506
Potkay S, Ganaway JR, Rogers NG, Kinard R (1966) An epizootic of measles in a colony of rhesus monkeys (Macaca mulatta). Am J Vet Res 27(116):331–334
Premenko-Lanier M, Rota PA, Rhodes G, Verhoeven D, Barouch DH, Lerche NW et al (2003) DNA vaccination of infants in the presence of maternal antibody: a measles model in the primate. Virology 307(1):67–75. https://doi.org/10.1016/S0042-6822(02)00036-3
Qiu W, Zheng Y, Zhang S, Fan Q, Liu H, Zhang F et al (2011) Canine distemper outbreak in rhesus monkeys, China. Emerg Infect Dis 17(8):1541–1543. https://doi.org/10.3201/eid1708.101153
Racaniello V (2011) Virology. An exit strategy for measles virus. Science 334(6063):1650–1651. https://doi.org/10.1126/science.1217378
Remfry J (1976) A measles epizootic with 5 deaths in newly-imported rhesus monkeys (Macaca mulatta). Lab Anim 10(1):49–57
Rennick LJ, de Vries RD, Carsillo TJ, Lemon K, van Amerongen G, Ludlow M et al (2015) Live-attenuated measles virus vaccine targets dendritic cells and macrophages in muscle of nonhuman primates. J Virol 89(4):2192–2200. https://doi.org/10.1128/JVI.02924-14
Reynolds MG, Damon IK (2012) Outbreaks of human monkeypox after cessation of smallpox vaccination. Trends Microbiol 20(2):80–87. https://doi.org/10.1016/j.tim.2011.12.001
Reynolds MG, Carroll DS, Karem KL (2012) Factors affecting the likelihood of monkeypox’s emergence and spread in the post-smallpox era. Curr Opin Virol 2(3):335–343. https://doi.org/10.1016/j.coviro.2012.02.004
Roeder PL (2011) Rinderpest: the end of cattle plague. Prev Vet Med 102(2):98–106. https://doi.org/10.1016/j.prevetmed.2011.04.004
Rota PA, Moss WJ, Takeda M, de Swart RL, Thompson KM, Goodson JL (2016) Measles. Nat Rev Dis Primers 2(1):16049. https://doi.org/10.1038/nrdp.2016.49
Sabin AB, Flores Arechiga A, Fernandez de Castro J, Albrecht P, Sever JL, Shekarchi I (1984) Successful immunization of infants with and without maternal antibody by aerosolized measles vaccine. II. Vaccine comparisons and evidence for multiple antibody response. J Am Med Assoc 251(18):2363–2371
Sakai K, Nagata N, Ami Y, Seki F, Suzaki Y, Iwata-Yoshikawa N et al (2013a) Lethal canine distemper virus outbreak in cynomolgus monkeys in Japan in 2008. J Virol 87(2):1105–1114. https://doi.org/10.1128/JVI.02419-12
Sakai K, Yoshikawa T, Seki F, Fukushi S, Tahara M, Nagata N et al (2013b) Canine distemper virus associated with a lethal outbreak in monkeys can readily adapt to use human receptors. J Virol 87(12):7170–7175. https://doi.org/10.1128/JVI.03479-12
Schillaci MA, Jones-Engel L, Engel GA, Kyes RC (2006) Exposure to human respiratory viruses among urban performing monkeys in Indonesia. Am J Trop Med Hyg 75(4):716–719
Scott GB, Keymer IF (1975) The pathology of measles in Abyssinian Colobus monkeys (Colobus guereza): a description of an outbreak. J Pathol 117(4):229–233. https://doi.org/10.1002/path.1711170405
Sheldon JD, Cushing AC, Wilkes RP, Anis E, Dubovi EJ (2017) Serologic response to canine distemper vaccination in captive Linnaeus’s two-toed sloths (Choloepus didactylus) after a fatal canine distemper virus outbreak. J Zoo Wildl Med 48(4):1250–1253. https://doi.org/10.1638/1042-7260-48.4.1250
Shishido A (1966) Natural infection of measles virus in laboratory monkeys. J Med Sci Biol 19(4):221–222
Spelman LH, Gilardi KV, Lukasik-Braum M, Kinani JF, Nyirakaragire E, Lowenstine LJ et al (2013) Respiratory disease in mountain gorillas (Gorilla beringei beringei) in Rwanda, 1990–2010: outbreaks, clinical course, and medical management. J Zoo Wildl Med 44(4):1027–1035. https://doi.org/10.1638/2013-0014R.1
Stittelaar KJ, Wyatt LS, de Swart RL, Vos HW, Groen J, van Amerongen G et al (2000) Protective immunity in macaques vaccinated with a modified vaccinia virus Ankara-based measles virus vaccine in the presence of passively acquired antibodies. J Virol 74(9):4236–4243. https://doi.org/10.1128/Jvi.74.9.4236-4243.2000
Stittelaar KJ, Kuiken T, de Swart RL, van Amerongen G, Vos HW, Niesters HG et al (2001) Safety of modified vaccinia virus Ankara (MVA) in immune-suppressed macaques. Vaccine 19(27):3700–3709. https://doi.org/10.1016/S0264-410x(01)00075-5
Stittelaar KJ, de Swart RL, Vos HW, van Amerongen G, Sixt N, Wild TF et al (2002) Priming of measles virus-specific humoral- and cellular-immune responses in macaques by DNA vaccination. Vaccine 20(16):2022–2026
Strating A (1975) Measles vaccine in dogs: efficacy against aerosol challenge with virulent canine distemper virus. J Am Vet Med Assoc 167(1):59–62
Strebel PM, Cochi SL, Hoekstra E, Rota PA, Featherstone D, Bellini WJ et al (2011) A world without measles. J Infect Dis 204(Suppl 1):S1–S3. https://doi.org/10.1093/infdis/jir111
Sun Z, Li A, Ye H, Shi Y, Hu Z, Zeng L (2010) Natural infection with canine distemper virus in hand-feeding Rhesus monkeys in China. Vet Microbiol 141(3–4):374–378. https://doi.org/10.1016/j.vetmic.2009.09.024
Tatsuo H, Ono N, Tanaka K, Yanagi Y (2000) SLAM (CDw150) is a cellular receptor for measles virus. Nature 406(6798):893–897. https://doi.org/10.1038/35022579
van Binnendijk RS, van der Heijden RW, Osterhaus ADME (1995) Monkeys in measles research. Curr Top Microbiol Immunol 191:135–148
van Binnendijk RS, Poelen MC, van Amerongen G, de Vries P, Osterhaus AD (1997) Protective immunity in macaques vaccinated with live attenuated, recombinant, and subunit measles vaccines in the presence of passively acquired antibodies. J Infect Dis 175(3):524–532
Visser IKG, van Bressem MF, Barrett T, Osterhaus ADME (1993) Morbillivirus infections in aquatic mammals. Vet Res 24(2):169–178
von Messling V, Springfeld C, Devaux P, Cattaneo R (2003) A ferret model of canine distemper virus virulence and immunosuppression. J Virol 77(23):12579–12591
Warthin AS (1931) Occurrence of numerous large giant cells in the tonsils and pharyngeal mucosa in the prodromal stage of measles. Arch Pathol 11:864–874
Welshman MD (1989) Measles in the cynomolgus monkey (Macaca fascicularis). Vet Rec 124(8):184–186
WHO (2017) Progress towards regional measles elimination - worldwide, 2000–2016. Wkly Epidemiol Rec 92(43):649–659
Willy ME, Woodward RA, Thornton VB, Wolff AV, Flynn BM, Heath JL et al (1999) Management of a measles outbreak among Old World nonhuman primates. Lab Anim Sci 49(1):42–48
Yamanouchi K, Yoshikawa Y, Sato TA, Katow S, Kobune F, Kobune K et al (1977) Encephalomyelitis induced by canine distemper virus in non-human primates. J Med Sci Biol 30(5):241–257
Yoshikawa Y, Ochikubo F, Matsubara Y, Tsuruoka H, Ishii M, Shirota K et al (1989) Natural infection with canine distemper virus in a Japanese monkey (Macaca fuscata). Vet Microbiol 20(3):193–205. https://doi.org/10.1016/0378-1135(89)90043-6
Zhu YD, Fennelly G, Miller C, Tarara R, Saxe I, Bloom B et al (1997) Recombinant bacille Calmette-Guerin expressing the measles virus nucleoprotein protects infant rhesus macaques from measles virus pneumonia. J Infect Dis 176(6):1445–1453
Zhu Y, Rota P, Wyatt L, Tamin A, Rozenblatt S, Lerche N et al (2000) Evaluation of recombinant vaccinia virus—measles vaccines in infant rhesus macaques with preexisting measles antibody. Virology 276(1):202–213. https://doi.org/10.1006/viro.2000.0564
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
de Vries, R.D., Kuiken, T., de Swart, R.L. (2020). Morbillivirus Infections in Non-human Primates: From Humans to Monkeys and Back Again. In: Knauf, S., Jones-Engel, L. (eds) Neglected Diseases in Monkeys. Springer, Cham. https://doi.org/10.1007/978-3-030-52283-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-52283-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-52282-7
Online ISBN: 978-3-030-52283-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)