Abstract
The battle in general, particularly in surgery, never is won by splendid weapons but owing to a brilliant mind and skills of the fighter. Prior to CT scanning, what we were able to see by radiological techniques was usually Waters’ projection also named as “occipitomental view” (a radiographic view, where an X-ray beam is angled at 37° to the orbitomeatal line), mostly as to depict the maxillary and sinus, not ethmoid sinuses and particularly not sphenoid sinus. In particular cases, but not routinely, tomography of the sinuses was used. Both Waters’ projection and tomography of the sinuses were just approximate, without any precise demonstration of the bony structures of the sinuses. The navigation system is a relatively new tool which appeared during the last decade of the twentieth century. Later on, more authors started to report their results and experiences with navigation systems in FESS [Hemmerdinger SA, Jacobs JB, Lebowitz RA. Otolaryngol Clin N Am 38:453–460, 2005; Olson G, Citardi MJ. Otolaryngol Head Neck Surg 123:188–194, 2000; Chu ST. Use of navigation system with FESS in 38 cases. In: The 75th Symposium of the Taiwan Otolaryngological Society, November 9, 2004; Reardon EJ. Otolaryng Clin N Am 2005;38:515–525]. Nowadays, navigation systems are widely used. As to possible advantages of such systems, I can say that most of the standard procedures of the endonasal endoscopic sinus surgery can be performed without the help of navigation. Still, sporadic pitfalls with this technique can result in serious complications, particularly when dealing with anterior skull base, pituitary gland surgery, CSF leak connected to the skull base tumors, etc. Under the assistance of a navigation system, these can be avoided.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
17.1 Introduction
Yes, undoubtedly, some of these tools have made endoscopic sinus surgery more effective. One should not rely exclusively on the technical privileges that new instruments, equipment, and utensils offer simply because the most important thing to perform successful surgery is not the “weapon,” regardless of how splendid it is. The battle in general, particularly in surgery, never is won by splendid weapons but owing to a brilliant mind and skills of the fighter.
17.2 Computed Tomography (CT)
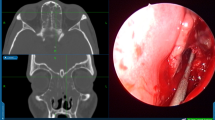
Prior to CT scanning, what we were able to see by radiological techniques was usually Waters’ projection (Fig. 17.1), also named as “occipitomental view” (a radiographic view, where an X-ray beam is angled at 37° to the orbitomeatal line), mostly as to depict the maxillary and sinus, not ethmoid sinuses and particularly not sphenoid sinus. In particular cases, but not routinely, tomography of the sinuses was used. Both Waters’ projection and tomography of the sinuses (Fig. 17.2) were just approximate, without any precise demonstration of the bony structures of the sinuses.
A coronal CT scan showing the following signs: suspected submucosal cleft palate (red arrow—the palatal processes of the right and left maxilla are not in contact), and intermaxillary bone is distorted (blue arrow): it usually has the shape of the capital letter “Y” and usually is “inserted” between the palatal processes of both maxillas. This intermaxillary bone is asymmetric; the right “ala” of the letter “Y” is positioned very low, whereas the left ala is sticking in an upright position. Because of that, the inferior border of the anterior nasal septum had the opportunity to slide out of the naturally presumed “holder” (made by two symmetric alas of the letter “Y”). It skipped out to the right nasal cavity from the bolster and thus formed so-called septal anterior crest, while on the opposite left side, a very typical groove (green arrow) appeared as a consequence of septal sliding out. The groove is the “trademark” of the famous type 6 septal deformity, very frequently connected to the cleft palate. One can see also that something is going on in both maxillary sinuses; they even seem to be partially unusually septated, i.e., divided in the superior and inferior “floor,” mostly in their posterior part (black arrows). The right maxillary sinus seems to have some content of discharge or even polypous tissue, particularly in the “lower floor.” The ostiomeatal complex looks unhealthy bilaterally as does the ethmoid sinus, while the crista galli looks unusual. Such features would not have been seen and recognized in previous radiological images like Waters’ and tomography images. This is the real advantage of a correctly performed CT scanning of the paranasal sinuses. CT scanning has changed the complete concept of diagnosis, treatment, and surgical approaches to the paranasal sinuses
The information given by computed tomography (CT) of the paranasal sinuses needs to be interpreted according to the patient’s history and examination. Incidental mucosal changes are found in a third of asymptomatic adults and 45% of children [1].
Anatomical variations found in the paranasal sinuses are no more common in symptomatic patients, making it unlikely that these either initiate or sustain paranasal sinus disease.
CT provides a roadmap for the surgeon and is vital in the diagnosis of atypical sinus infections, malignancy, and CRS (chronic rhinosinusitis) complications. ENT surgeons need to communicate with radiological colleagues, giving the details of the presentation to obtain maximum benefit from the scan. So the development of minimally invasive sinus surgery, particularly in terms of the functional endonasal endoscopic sinus surgery (FESS) techniques, was enabled owing to the advances in radiological imaging like axial, coronal, and sagittal projections in computed tomography (CT) scanning, as well as the nuclear magnetic resonance (NMR) scanning. We are now able to see many anatomical details without entering into the skull and sinuses; everything is perfectly visible! Rhinologists should not rely exclusively on the radiological findings; they should be able to “read” the CT or NMR scans by themselves. During over 30 years of working with CT scans of the paranasal sinuses, radiologists have failed to mention sinus septi nasi nor the defect of the lateral nasal wall next to the natural ostium of the maxillary sinus. Pneumatized crista galli with obvious content inside has never been described.
17.3 Navigation Systems
The navigation system is a relatively new tool which appeared during the last decade of the twentieth century [2]. Later on, more authors started to report their results and experiences with navigation systems in FESS [3,4,5, 11]. Nowadays, navigation systems (Fig. 17.3) are widely used.
As to possible advantages of such systems, I can say that most of the standard procedures of the endonasal endoscopic sinus surgery can be performed without the help of navigation. Still, sporadic pitfalls with this technique can result in serious complications, particularly when dealing with anterior skull base, pituitary gland surgery, CSF leak connected to the skull base tumors, etc. Under the assistance of a navigation system, these can be avoided.
On the other hand, to use navigation system routinely, i.e., even in simple surgical cases, is unnecessary and leads directly to the development of less skilled endoscopic surgeons: without the navigation system, they could literally be lost in space. The surgeon must be able to understand at what exactly he or she is looking, what is the uncinate process, what is the ethmoidal bulla, how does the anterior wall of the sphenoid sinus look like, and how to approach to the bottom of the frontal sinus without help from navigation. Navigation should be used in particular clinical cases, mostly when it goes for transnasal endoscopic skull base surgery, optic nerve decompression, duraplasty endoscopic procedures, etc., i.e., for the surgical procedures which anyway require an experienced surgeon. Navigation system is not at all suitable for the beginners in FESS. There is no need to use navigation for the simple FESS; I would say routine surgical procedures.
17.4 Balloon Sinuplasty
Regarding balloon sinuplasty, I would say that it is just one more utensil within the armamentarium that an endoscopic sinus surgeon has on the table. In most of the cases, balloon sinuplasty is used as to “correct” the natural ostium of the maxillary sinus. But, most of the articles obviously present the cases of Two Holes Syndrome, i.e., the defect of the fontanel, which otherwise can be easily endoscopically identified, and the balloon is inflated within the natural ostium (which in most of the cases is closed because of chronically swollen mucosa). What really happens is the same story as what some other endoscopic surgeon does using the backbiting forceps as to remove the tissue bridge that divides the defect of the fontanel and dysfunctional natural ostium of the maxillary sinus [6, 7]. In terms of that, balloon sinuplasty does not represent any advantage in the treatment of chronic maxillary sinusitis. The problem of improving the drainage of the frontal sinus is different in the sense that to do this properly and to have later on the permanent good result, the anterior at least partial endoscopic ethmoidectomy is required as to enable balloon catheter to be directed and placed to the ostium of the frontal sinus. In this very case, one should not forget that the lateral and particularly superior part of the infundibulum, like the lower section of the opening of the frontal sinus, could in some cases be in a close contact to the orbit; even more, it can be a part of the upper medial bony wall of the orbit when the frontal sinus is well or even very well pneumatized. So, to apply the pressure by inflaming the balloon blindly in these circumstances could be inappropriate.
In this moment, we have to ask ourselves: what exactly is the balloon doing to the surrounding tissues while inflamed? Just pushing them to make some more room for the sinus drainage and ventilation? If yes, how exactly does it happen? Are there any uncontrolled fractures of the surrounding bony elements? To my mind, the best option is to operate endoscopically, step by step, until the bottom of the frontal sinus becomes clearly visible. Balloon sinuplasty sounds great and, up to date, is an attractive utensil, but one should think twice before using this tool. To my mind, it goes for a step backward, not at all an advantage.
NHS UK states that:
In a study of 115 patients, the balloon was successfully inserted in 347 out of 358 sinuses (97%). After 1 week, 232 out of 341 sinuses were clear (68%) and after 24 weeks, this had increased to 246 out of 304 sinuses being clear (81%). Two studies looked at symptom relief. A study of 1036 patients reported that 95% of patients had improved symptoms and 73% of patients were completely free of symptoms after an average of 40 weeks following the procedure. The study of 115 patients measured symptoms using a scale which ranged from 0 (least severe) to 5 (most severe). Before the procedure, the average score was 2.14. After the procedure, the average score had improved to 1.27. Another study of 70 patients, in which 35 patients had this procedure and 35 patients had a different procedure (called functional endoscopic sinus surgery), showed that the patients in the balloon group had greater improvements. Two studies looked at whether any further procedures were needed. Out of a total of 1145 patients, 28 needed a further procedure. [8]
17.5 Conclusion
There is no doubt that the invention of the CT scan and the Hopkins rod have increased our knowledge and understanding of sinus disease. Outcome measures in sinus surgery are complex [9] and have shifted in emphasis from those of the operator such as endoscopic appearances, ostial patency, or CT scan changes to those of the patient. Eighty percent of respondents in a recent study of patients’ and physicians’ views on outcome measurement in CRS considered symptomatic improvement the most important [10].
Currently there is a randomized trial ongoing in the UK to evaluate the benefit of surgery over continued medical therapy in CRS patients who have failed an initial course of medical treatment.
References
Jones NS. CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci. 2002;27(1):11–7. Review
Anon JB, Rontal M, Zinreich SJ. Computer-assisted endoscopic sinus surgery: current experience and future developments. Oper Tech Otolaryngol Head Neck Surg. 1995;6:163–70.
Hemmerdinger SA, Jacobs JB, Lebowitz RA. Accuracy and cost analysis of image-guided sinus surgery. Otolaryngol Clin North Am. 2005;38:453–60.
Chu ST. Use of navigation system with FESS in 38 cases. In: The 75th symposium of the Taiwan Otolaryngological Society, November 9; 2004.
Reardon EJ. The impact of image-guidance systems on sinus surgery. Otolaryngol Clin North Am. 2005;38:515–25.
Karanfilov B, et al. Office-based balloon sinus dilation: a prospective, multicenter study of 203 patients. International Forum of Allergy & Rhinology. 2012;3(5):404–11.
Weiss RL, et al. Long-term outcome analysis of balloon catheter sinusotomy: two-year follow-up. Otolaryngol-Head and Neck Surg. 2008;139(3 Suppl 1):38–46.
Noon E, Hopkins C. Review article: outcomes in endoscopic sinus surgery. BMC Ear Nose Throat Disord. 2016;16:9. https://doi.org/10.1186/s12901-016-0030-8.
Hopkins C, Philpott C, Crowe S, Regan S, Degun A, Papachristou I, Schilder AG. Identifying the most important outcomes for systematic reviews of interventions for rhinosinusitis in adults: working with patients, public and practitioners. Rhinology. 2016;54(1):20–6.
Olson G, Citardi MJ. Image-guided functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2000;123:188–94.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mladina, R. (2021). Have Technical Advances Improved CRS Outcomes?. In: Cingi, C., Bayar Muluk, N., Scadding, G.K., Mladina, R. (eds) Challenges in Rhinology. Springer, Cham. https://doi.org/10.1007/978-3-030-50899-9_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-50899-9_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50898-2
Online ISBN: 978-3-030-50899-9
eBook Packages: MedicineMedicine (R0)