Abstract
Although rare, uveal melanoma is the most common primary intraocular cancer. These tumors threaten eyesight and shorten life expectancy via treatment-refractory liver metastases. Radiation treatments represent the most used means of achieving local control. Among the varied means of delivering ionizing radiation, image-guided photon radiosurgery represents an accessible, effective and noninvasive alternative. It remains to be defined which patients are best suited to radiosurgery as compared to the more commonly prescribed plaque brachytherapy or proton beam therapy.
Despite the lack of prospective confirmation, it is assumed that local treatment can impact overall survival as radiotherapy arrests tumor growth, and the risk of metastasis is known to increase with tumor size. Although organ preservation is common, long-term visual acuity is disappointing as radiation retinopathy is common.
As image-guided radiosurgery systems assume a fixed relationship between targets and the skull, the main technical challenge in radiosurgery is to ensure a reproducible relationship between the eyeball and the cranium. In proton beam therapy, targeting is accomplished though the suturing of tantalum fiducials to the sclera, whereas in image-guided radiosurgery, the preference is for less invasive methods—retrobulbar anesthesia, closed-eye treatment, or patient-assisted gaze fixation systems.
Using a fractionation scheme of 50 Gy in 5 fractions for medium-sized tumors, the aim should be to exceed 90% in 5-year local control and 80% in 5-year enucleation-free survival.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Ocular melanoma is a rare disease. The incidence in Canada is approximately 0.7 per 100,000 population per year. This represents approximately 385 cases per year in Canada, and 80 cases in the province of Quebec—many of which are referred to our institution [1]. The reported incidence in the United States and Europe is similar, but it is significantly lower in non-Caucasian populations, notably in Africa and Asia [2].
The treatment of choroidal melanoma is controversial because of the paucity of high-level evidence and the visual toxicity of available treatments [3]. Small tumors can be clinically indistinguishable from large nevi. Thus, for smaller tumors the question arises as to whether the patient’s eyesight should be risked in the management of a lesion that might not have the potential for progression. Conversely, should a suspicious lesion be observed, potentially exposing the patient to a higher risk of metastatic disease? For medium-sized tumors, the main controversy is the choice of a treatment modality in the absence of convincing prospective comparisons. For large tumors in which visual outcomes are poor and distant metastases frequent, one can debate which patients should have eye preservation therapy and which should proceed with primary enucleation. For patients presenting with metastatic tumors and paucisymptomatic eyes, it remains undefined which patients benefit from immediate local therapy in the face of generally ineffective systemic therapy and limited life expectancy.
The Collaborative Ocular Melanoma Study (COMS) confirmed in a randomized trial that, for medium-sized tumors, organ preservation can be attempted without significantly impacting overall survival. Nonetheless, enucleation remains an option for patients with limited visual potential for whom follow-up would be burdensome. Although the COMS trial was limited to I-125 brachytherapy, its conclusions are assumed to apply to other local therapies known to produce similar levels of local tumor control. The main modalities are transpupillary thermotherapy, endoresection, plaque brachytherapy [4], proton beam therapy [5], and stereotactic radiation [6]. Treatment selection is based on tumor size, tumor location, patient preference, treatment availability, and, in large part, the treating physician’s opinion. In our practice, we choose to offer plaque brachytherapy (iodine or ruthenium, depending on tumor thickness) to most patients with small- or medium-sized tumors but prefer stereotactic radiation for juxtapapillary tumors. In this context, the CyberKnife robotic radiosurgery platform allows delivery of a high dose of radiation to the small target volume within the eye with a steep dose gradient [7]. Similarly to other radiosurgery platforms, the CyberKnife can accurately target structures having a rigid relationship to the skull. However it does not intrinsically provide a means to track eye movement. Our practice is to achieve eye immobilization using an in-house system of which we have characterized the reproducibility [8]. Our experience with this system over the past years informs sections of this manuscript.
2 Staging
Local spread of uveal melanoma to other organs is rare, as is lymph node involvement. Most staging efforts center on the size of the primary tumor and its involvement of substructures of the eye. Until benefit is shown to adjuvant systemic therapy, the main purpose of local staging is to offer prognostic information and select a local management strategy. The tumor is principally characterized by ultrasound but MRI can contribute to the finding of extrascleral extension [9]. The eighth Edition of the American Joint Committee on Cancer proposes a detailed tumor staging system for ciliary body and choroid uveal melanoma. This system is based on the thickness of the tumor, the maximal basal diameter, involvement of the ciliary body, and extraocular extension. For example, a tumor of 12 mm or less in diameter and 3 mm or less in height as well as those of 9 mm or less in diameter and 6 mm or less in height are T1 tumors—T1a if there is no ciliary involvement or extraocular extension. At the other end of the spectrum, a T4 tumor is any tumor with more than 5 mm of extraocular extension, any tumor of more than 18 mm of basal diameter, more than 15 mm of height, or a tumor combining a diameter of more than 15 mm with a height of more than 12 mm. The complexity and relative clinical uselessness of this staging system might explain why the simpler COMS staging system remains in use. In this revised 3-tiered system, tumors are divided into small, medium, and large tumors [10].
-
COMS Small: Diameter 5–16 mm and height 1–2.5 mm
-
COMS Medium: Diameter >16 mm and height ≤2 mm or diameter <16 mm and height 2.6–10 mm
-
COMS Large: Diameter >16 mm and height >2 mm or height >10 mm
When uveal melanoma spreads beyond the orbit, the disease will have a strong predilection for the liver. Median survival for patients with metastatic disease is less than 1 year and the evidence that any liver-directed therapy or systemic cancer therapy prolongs survival or improves quality of life is weak [11, 12]. Although approximately 10%, 25%, and 50% of patients with small, medium and large tumors will eventually develop metastatic disease, the yield of liver imaging at the time of diagnosis is low. Ultrasound, CT scan, and MRI imaging are reasonable means of screening for liver metastases (there is no good evidence of incremental benefit of total body FDG/PET imaging), but will all be more likely to yield incidental findings than true positive findings of metastatic disease [13].
3 Rationale for Radiation Therapy
Over a 12-year period from 1986 to 1998, 1317 patients with medium-sized uveal melanoma were randomized to enucleation or iodine-125 brachytherapy. These trial participants represented nearly half of eligible patients in the participating institutions. Mortality in both treatment arms was similar at 12 years with better visual outcomes in patients spared enucleation. In the brachytherapy arm, the 5-year actuarial risk of treatment failure was 10.3%, and the enucleation rate was 12.5% [14]. This high-level evidence has cemented radiotherapy as a standard treatment for medium-sized uveal melanoma. The body of evidence to support the treatment of smaller or larger tumors is mainly retrospective. Based on reported outcomes of thousands of patients, the eye preservation rate is high and the local control favorable. Long-term preservation of visual acuity is disappointing—especially for larger tumors.
The evidence for non-radiation eye preservation therapies is limited. Transpupillary thermotherapy (TTT) may be a reasonable option for the smallest tumors [15]. However, when patients are poorly selected, the local control will be poor and the visual outcomes disappointing [16]. Endoresection is a more complex procedure which also aims to avoid late radiation toxicity (at the cost of more acute toxicity) for which the jury is still out [17].
4 Single-Fraction Radiosurgery
Radiosurgery devices had started to be used to treat small brain tumors with apparent satisfactory local control and limited toxicity when the first report of single-fraction radiosurgery for uveal melanoma was published in the late 1980s. At the time, radiosurgery programs used semi-invasive head immobilization, and fractionated treatments were rare and cumbersome [18]. The initial doses used were high by today’s standard—60–90 Gy in a single fraction. As an illustration, in 1992–1993, the Sheffield group recruited 14 patients with uveal melanoma to be treated using the Leksell Gamma Knife. The typical treatment was 70 Gy in a single fraction using a spherical “shot.” The entire procedure was accomplished in a single morning under retrobulbar anesthesia (“Akinesia of the globe was achieved by a standard retrobulbar injection of local anesthetic. Approximately 4 mL of a mixture lignocaine 2% and bupivacaine 0.5% was used followed by gentle massage of the globe for 5 min.”). Although early tumor responses were seen, 13 of the 14 patients had serious adverse reactions leading the authors to the sober conclusion that “Several issues must be resolved before stereotactic radiosurgery can be accepted as a viable alternative method of treating intraocular tumors. An optimal dose which adequately treats the tumor with a minimum of side effects has yet to be established. Similarly, the value of fractionating the dose remains unknown.” [19].
Over the ensuing decades, the single-fraction experience has grown, and the dose prescription refined to be closer to 20 Gy. Although outcomes are quite favorable in selected small series [20], the 5-year actuarial eye retention rate (73%) and local control (70.8%) in the largest series of 271 patients (treated with 18–22 Gy) may be lower than expected. As the experience remains limited and heterogeneous compared to the published series using 5 fractions, it is difficult to ascertain if the local control and enucleation rates are comparable. There is certainly a trend across radiation oncology away from ablative single-fraction treatments, whether it be in prostate cancer, lung cancer, or brain metastases. Irrespective of biological concerns, the margin required to ensure target coverage is inversely proportional to the number of fractions and make single-fraction treatments especially sensitive to various uncertainties. It remains that a single day procedure is convenient and while the jury remains out, single-fraction radiosurgery will continue to be appropriately used for selected patients in a small number of clinical programs.
5 Image-Guided Radiosurgery and Hypofractionated Radiotherapy
Although there is no prospective comparative data, the outcomes in a review of more than 10,000 patients treated with proton therapy at various institutions in North America and Europe compare favorably with I-125 plaque brachytherapy in terms of local control, eye preservation, and toxicity [21]. This is in keeping with a randomized study of 184 patients meeting broad eligibility criteria who were randomized to 70 CGE of helium ion therapy (5 fractions over 7–11 days) or 70 Gy to the tumor apex (changed mid-trial to 1 mm beyond the tumor apex) using I-125 plaque brachytherapy. In this trial, local control and enucleation-free survival were significantly improved in the particle therapy group. Although the difference was less marked when tumors <2 mm from the optic disc were excluded, it remained statistically significant [22]. These results must of course be interpolated with caution as helium ions are biologically different from photons/protons, and the brachytherapy treatments delivered in the trial were not in keeping with the standards of the COMS trial (85 Gy to a minimum of 6 mm from the plaque) or the recommendations of the American Brachytherapy Society (85 Gy to the tumor apex with a radial margin of 2–3 mm) [23].
As the dosimetry of stereotactic photon radiation does not appear meaningfully different from that of proton therapy, it is logical to transpose the proton experience to the more widely available and less costly stereotactic photon treatments [24, 25]. In this context, the best described treatment schedule is 50 Gy over 5 fractions. This dose is supported by a trial randomizing 188 patients with small- or medium-sized choroidal melanomas (<15 mm in diameter and <5 mm in height) to 50 CGE or 70 CGE of proton irradiation over the same 5 fractions. In this trial, the lower dose resulted in less visual field toxicity and similar oncological outcomes [26]. As photon plans tend to be less homogeneous than proton plans, the minimum dose to the tumor will anyways be closer to 60 Gy when the prescription to the PTV is 50 Gy.
Selected series of hypofractionated photon stereotactic radiation are presented in Table 35.1. No firm conclusions should be drawn as the series are relatively small and heterogeneous, but the outcomes are compatible with those reported for the same fractionation schemes delivered with proton beam irradiation.
6 Toxicity
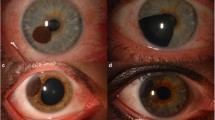
Radiation treatment of uveal melanoma is highly focused and thus, the principal toxicity of radiosurgery will be from irradiation of the eye and globe. Other than enucleation as a consequence of painful glaucoma, the most common and most concerning toxicity will be the loss of visual acuity. This risk will depend on the location of the tumor within the eye and its size, but it is appropriate to expect less than half of patients with good pre-treatment visual acuity to maintain good visual acuity in the years following treatment. A greater risk will be seen in patients with large tumors and those with tumors encroaching on the macula or optic disc. Radiation retinopathy will be the most common related injury although patients may also suffer from cataract, secondary glaucoma, radiation maculopathy, optic neuropathy, retinal and vitreous hemorrhages, and retinal detachment. When enucleated eyes are examined, radiation injury is marked at the level of blood vessels which develop outpouchings, fusiform dilatation, and microaneurysms. Collateral circulation can be seen and vascular incompetence results in vascular leakage, edema, and retinal detachment. The capillary lumens also narrow leading to ischemia and infarction [30]. Elevated levels of vascular-endothelial growth factor participate in mediating toxicity and anti-VEGF therapy may reduce vascular permeability and improve neovascular glaucoma, subretinal fluid, and retinal detachment. The benefit of prophylactic intravitreal anti-VEGF antibodies is controversial [31], but our institutional bias is in favor of early use of these drugs following radiotherapy of uveal melanoma.
Though retinal toxicity can be unavoidable, with optimization of the dose to the lachrymal gland and anterior chamber, the risk of xerophthalmia, keratitis, cataract, or loss of eyelashes can be minimized.
Beyond the orbit, there will be a low total body dose which likely incurs a small excess risk of malignancy. Although we have modeled the risk of extracranial second malignancies to exceed that of intracranial radiation-induced malignancies, it would not be possible to distinguish these tumors from the background risk of cancer. An aggressively behaving meningioma or an orbital sarcoma would be more readily attributed to radiotherapy [32]. The main factors to consider in the risk of radiation-induced malignancy would be patient age at the time of treatment, number of monitor units delivered and generation of the CyberKnife unit. As the absolute risk is modeled to be less than 1% at 20 years, it will typically not factor into the decision to treat.
Low total body doses will be more relevant in the case of pregnancy. The dose to the fetus can be in the order of magnitude of 0.5% of the prescription dose which is enough to be clinically relevant [33]. Pregnancy status should thus be ascertained in women of childbearing potential, and treatment of a pregnant woman should only proceed after considering the alternatives (ruthenium plaque brachytherapy, for example) and after implicating the radiation safety officer.
There are several reports of quality of life in patients irradiated for ocular melanoma. Few compare different radiation modalities, and the only high-level data is from the comparison of enucleation to iodine-125 brachytherapy [34, 35]. It is clear that, as with other patients diagnosed with cancer, the diagnosis of ocular melanoma is associated with a reduced quality of life. The main areas of impact relate to decreased vision, ocular discomfort, and mood disturbance. In the first years following treatment, patients benefit from a vision-preserving treatment but the benefit decreases after the second year as the incidence of radiation toxicity increases. Unsurprisingly, quality of life is better in those patients not suffering from secondary glaucoma. Depression is seen irrespective of treatment modality (although it may correlate with eyesight) and anxiety might be more likely to resolve with time in patients undergoing enucleation [36, 37].
7 Conclusion
Robotic stereotactic irradiation is one tool in the varied radiotherapy armamentarium for choroidal melanoma. It is a convenient and noninvasive treatment for which the results are in keeping with those of the more commonly described iodine plaque brachytherapy and proton beam therapy. Although prospective comparisons are not expected in the near future, continued accumulation and publication of retrospective evidence may further increase clinical adoption.
8 Practical Guide
Our treatment technique has previously been published [38]. The patient undergoes a 1.5 T planning MRI. Focused sequences are obtained with the patient fixing a dot within the coil (placed in the approximate position of the light used in our immobilization device). Three sequences are obtained, a thin slice T2 2D Turbo Spin Echo, a 3D 1 mm isotropic T2 series, and a gadolinium-enhanced 3D T1 isotropic series (Fig. 35.1). The patient is then immobilized supine in a thick (3.2 mm) thermoplastic mask with Kevlar reinforcement, a cutout for the eyes (in patients unable to see with the involved eye, immobilization is based on the seeing eye), and a wide base to support the camera system. The camera system is part of a custom immobilization device which provides a light for the patient to fix the position which can be recorded and reproduced (Fig. 35.2). The camera system allows for monitoring of patient compliance. The position of the iris is marked on a transparency overlaid on the screen linked to the monitoring camera. Simulation CT is acquired with 2 mm thick slices every 1 mm. The field of view is sufficient to visualize the entire immobilization device.
In the planning system, CT and MRI sequences are manually co-registered using the insertion and the optic nerve and lens as principal landmarks. The gross tumor volume (GTV) is segmented using both MRI sequences and fundus schema. The dimensions of the contoured volume are checked in relation to those measured on ocular ultrasound. A 2 mm planning target margin (PTV) is added, which is trimmed where it obviously extends beyond the sclera. Organs at risk contoured include ipsilateral lens, ipsilateral optic nerve, ipsilateral lachrymal gland, contralateral eye, immobilization device, and oral cavity. A shell structure is created 1.5 mm beyond the PTV. Collimator selection is a compromise between dose conformity and the treatment duration. The immobilization device is blocked with a 2–3 cm margin. In each case, the contralateral eye and oral cavity are either blocked or spared via strict optimization criteria. The plan is optimized so that the entire PTV is covered by at least 95% of the prescription dose and 99% is covered by 100% of the prescription isodose volume (typically this is 65–75% of the maximum dose). The conformity index (CI) is kept below 1.5, and the 25 Gy isodose volume is inspected for conformity. The lachrymal gland is optimized to a mean dose of less than 23.4 Gy. The entire contralateral eye (with a 1 cm margin) is kept below 2 Gy. When possible, the ipsilateral lens is kept under 2 Gy. Target coverage is prioritized over organs at risk, but a very steep gradient is created at the optic nerve in order to reduce the dose as much as possible without underdosing the PTV.
The dose is calculated considering tissue heterogeneity using a ray tracing algorithm. An independent monitor unit calculation is used to verify the plan. A dry run is performed with the mask, a head phantom and the immobilization device to identify potential collisions prior to the first fraction. The fractions are typically delivered every other day but can be delivered daily for patients in whom a 2-week treatment would be burdensome. During treatment, the position of the iris is monitored to be within the markings taken at simulation. Typically, the treatment is delivered in 1-min increments between which the patient can rest their eyes (Table 35.2).
References
New cases and age-standardized rate for primary cancer (based on the May 2015 CCR tabulation file), by cancer type and sex, Canada, provinces and territories. 2016 March 11. http://www5.statcan.gc.ca/cansim/a05.
Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye (Lond). 2017;31(2):241–57.
Damato B. Does ocular treatment of uveal melanoma influence survival? Br J Cancer. 2010;103(3):285–90.
Lommatzsch PK, Lommatzsch R. Treatment of juxtapapillary melanomas. Br J Ophthalmol. 1991;75(12):715–7.
Seddon JM, et al. Uveal melanomas near the optic disc or fovea. Visual results after proton beam irradiation. Ophthalmology. 1987;94(4):354–61.
Emara K, et al. Stereotactic radiotherapy in the treatment of juxtapapillary choroidal melanoma: preliminary results. Int J Radiat Oncol Biol Phys. 2004;59(1):94–100.
Roberge D, et al. Treatment of medium-sized juxtapapillary melanoma with external Co-60 photon therapy. Radiother Oncol. 2005;74(1):71–3.
Iskanderani O, et al. Reproducibility of a noninvasive system for eye positioning and monitoring in stereotactic radiotherapy of ocular melanoma. Technol Cancer Res Treat. 2017;16(3):352–6.
Recsan Z, et al. MRI for the evaluation of scleral invasion and extrascleral extension of uveal melanomas. Clin Radiol. 2002;57(5):371–6.
Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study. COMS report no. 1. Arch Ophthalmol. 1990;108(9):1268–73.
Khoja L, et al. Meta-analysis in metastatic uveal melanoma to determine progression-free and overall survival benchmarks: an international rare cancers initiative (IRCI) ocular melanoma study. Ann Oncol. 2019;30:1370.
Rantala ES, Hernberg M, Kivela TT. Overall survival after treatment for metastatic uveal melanoma: a systematic review and meta-analysis. Melanoma Res. 2019;29(6):561–8.
Strobel K, et al. Limited value of 18F-FDG PET/CT and S-100B tumour marker in the detection of liver metastases from uveal melanoma compared to liver metastases from cutaneous melanoma. Eur J Nucl Med Mol Imaging. 2009;36(11):1774–82.
Jampol LM, et al. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: IV. Local treatment failure and enucleation in the first 5 years after brachytherapy. COMS report no. 19. Ophthalmology. 2002;109(12):2197–206.
Shields CL, et al. Primary transpupillary thermotherapy for small choroidal melanoma in 256 consecutive cases: outcomes and limitations. Ophthalmology. 2002;109(2):225–34.
Harbour JW, et al. Transpupillary thermotherapy versus plaque radiotherapy for suspected choroidal melanomas. Ophthalmology. 2003;110(11):2207–14; discussion 2215.
Reichstein D, Karan K. Endoresection utilizing pars plana vitrectomy for benign and malignant intraocular tumors. Curr Opin Ophthalmol. 2019;30(3):151–8.
Roberge D, et al. Hypofractionated stereotactic radiotherapy for low grade glioma at McGill University: long-term follow-up. Technol Cancer Res Treat. 2006;5(1):1–8.
Rennie I, et al. The use of single fraction Leksell stereotactic radiosurgery in the treatment of uveal melanoma. Acta Ophthalmol Scand. 1996;74(6):558–62.
Sikuade MJ, et al. Outcomes of treatment with stereotactic radiosurgery or proton beam therapy for choroidal melanoma. Eye (Lond). 2015;29(9):1194–8.
Verma V, Mehta MP. Clinical outcomes of proton radiotherapy for uveal melanoma. Clin Oncol (R Coll Radiol). 2016;28(8):e17–27.
Mishra KK, et al. Long-term results of the UCSF-LBNL randomized trial: charged particle with helium ion versus Iodine-125 plaque therapy for choroidal and ciliary body melanoma. Int J Radiat Oncol Biol Phys. 2015;92(2):376–83.
Nag S, et al. The American Brachytherapy Society recommendations for brachytherapy of uveal melanomas. Int J Radiat Oncol Biol Phys. 2003;56(2):544–55.
Weber DC, et al. Proton beam radiotherapy versus fractionated stereotactic radiotherapy for uveal melanomas: a comparative study. Int J Radiat Oncol Biol Phys. 2005;63(2):373–84.
Daftari IK, et al. Newer radiation modalities for choroidal tumors. Int Ophthalmol Clin. 2006;46(1):69–79.
Gragoudas ES, et al. A randomized controlled trial of varying radiation doses in the treatment of choroidal melanoma. Arch Ophthalmol. 2000;118(6):773–8.
Dunavoelgyi R, et al. Local tumor control, visual acuity, and survival after hypofractionated stereotactic photon radiotherapy of choroidal melanoma in 212 patients treated between 1997 and 2007. Int J Radiat Oncol Biol Phys. 2011;81(1):199–205.
Fernandes BF, et al. Neovascular glaucoma after stereotactic radiotherapy for juxtapapillary choroidal melanoma: histopathologic and dosimetric findings. Int J Radiat Oncol Biol Phys. 2011;80(2):377–84.
van den Bosch T, et al. Risk factors associated with secondary enucleation after fractionated stereotactic radiotherapy in uveal melanoma. Acta Ophthalmol. 2015;93(6):555–60.
Groenewald C, Konstantinidis L, Damato B. Effects of radiotherapy on uveal melanomas and adjacent tissues. Eye (Lond). 2013;27(2):163–71.
Haji Mohd Yasin NA, et al. Choroidal melanoma treated with stereotactic fractionated radiotherapy and prophylactic intravitreal bevacizumab: the Dunedin Hospital experience. J Med Imaging Radiat Oncol. 2016;60(6):756–63.
Scaringi C, et al. Radiation-induced malignant meningioma following proton beam therapy for a choroidal melanoma. J Clin Neurosci. 2015;22(6):1036–7.
Pantelis E, et al. Radiation dose to the fetus during CyberKnife radiosurgery for a brain tumor in pregnancy. Phys Med. 2016;32(1):237–41.
Chabert S, Velikay-Parel M, Zehetmayer M. Influence of uveal melanoma therapy on patients’ quality of life: a psychological study. Acta Ophthalmol Scand. 2004;82(1):25–31.
Miniati M, et al. Quality of life, depression, and anxiety in patients with uveal melanoma: a review. J Oncol. 2018;2018:5253109.
Moschos MM, et al. Depression in choroidal melanoma patients treated with proton beam radiotherapy. Anticancer Res. 2018;38(5):3055–61.
Melia M, et al. Quality of life after iodine 125 brachytherapy vs enucleation for choroidal melanoma: 5-year results from the collaborative ocular melanoma study: COMS QOLS report no. 3. Arch Ophthalmol. 2006;124(2):226–38.
Beliveau-Nadeau D, Callejo S, Roberge D. Technique for robotic stereotactic irradiation of choroidal melanoma. Cureus. 2016;8(4):e582.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Roberge, D. (2020). Uveal Melanoma. In: Conti, A., Romanelli, P., Pantelis, E., Soltys, S., Cho, Y., Lim, M. (eds) CyberKnife NeuroRadiosurgery . Springer, Cham. https://doi.org/10.1007/978-3-030-50668-1_35
Download citation
DOI: https://doi.org/10.1007/978-3-030-50668-1_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50667-4
Online ISBN: 978-3-030-50668-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)