Abstract
Pulsatility of the blood circulation has evolved in the animal kingdom over hundreds of millions of years. The result, an exquisitely balanced self-sustaining system, supports our lives. Man-made efforts to assist or replace this system have led to saving millions of lives with cardiopulmonary bypass, intra-aortic balloon pumping, extracorporeal membrane oxygenation, and a variety of extracorporeal and implantable pumps for cardiac assist or replacement. In most of these, continuous-flow pumps have dominated. Experience has unveiled limitations of continuous flow and rekindled interest in man-made pulsatile blood pumps. This chapter reviews pulsatile physiology and pulsatile blood pumps.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pulse
- Microcirculation
- Capillary flow
- Blood cells
- Perfusion pressure
- Shearing force
- Thrombosis
- Hemorrhage
- Stroke
- Survival
Introduction
For 500 million years, there have been hearts. The phylum Chordata (having a spine or notochord) is characterized as having a heart. The heart and lungs evolved into separate pulmonary and circulatory systems in amphibians about 350 million years ago. In the timeline of mammalian evolution, precursors to man appeared over 50 million years ago, and Homo sapiens (humans) the final descendant of the great apes appeared 250,000–500,000 years ago [1]. Evolution has created our incredibly complex biology. Yet, there is a consistency and simplicity. All higher animals have pulsatile, heart beating circulations that bear a striking resemblance. The embryonic development of the human heart in the early stages recapitulates the longitudinal two-chambered heart of fish. Our hearts and circulatory systems of vessels have evolved over a time. The physics, biology, anatomy, and physiology of this complex system provide 4–8 l of oxygenated blood flow every minute in adults. The resting beat rate of the heart is 70–100 per minute, and the volume of the pulse delivered is between 60 and 100 ml/beat. Arterial blood pressure is 120/70 mmHg, and the peak rate of pressure change as the blood is ejected from the left ventricle is over 1200 mmHg/s. About 80% of the resistance to flow is due to the microvasculature. Approximately 23% of the flow goes to the kidneys and 14% to the brain [2]. The remainder is distributed to other organs and tissues. Homeostasis of the blood in a normo-coagulable state has also evolved. The major factors in this complex and incompletely understood system are the platelets and the coagulation system. A fine balance prevents hypocoagulability that leads to bleeding and hypercoagulability that leads to clotting. The introduction of foreign materials such as those found in blood pumps to these systems causes activation as well as degradation of platelets and procoagulants. Antiplatelet and anticoagulant therapies are therefore necessary but may lead to bleeding. Bleeding also results from destruction of von Willebrand factor multimers by continuous-flow pumps [3].
The first circulatory assist for the open-heart surgery in 1954 [4] was biological. A small child could be supported by cross-circulation with his parent while the child’s heart was emptied during surgical repair. This work of Dr. C.W. Lillehei triggered interest in open-heart surgery. The concept of using a “pump oxygenator” was pursued by many after the initial success of Gibbon using as an oxygenator a screen over which a thin layer of the blood passed allowing for gas exchange [5]. Continuous flow was then used with a series of different models of oxygenators including disc, bubble over “iron wool,” and finally tiny hollow tubes. Cardiopulmonary bypass (CPB) was initially performed with roller pumps and later with centrifugal pumps that delivered a continuous flow. To compensate for the inadequacy of continuous flow, surgeons learned to operate quickly and to use hypothermia to slow total body metabolism. After an initial surge of interest in pulsatile cardiopulmonary bypass, it has nearly disappeared, but not because it was proven to be inferior. It was just more difficult to deliver a physiologic pulse compared to the simplicity of delivering continuous flow.
Mechanical circulatory support blood pumps in current clinical use and those that preceded them have provided life-saving blood flow at a price. The continuous-flow pumps, ventricular assist devices (VADs), came into use because they are smaller and thus easier to implant (Cheng et al.) and more durable than the pulsatile electric HeartMate XVE, a pump that had on average a 15- to 20-month durability (covered later in the chapter). The evaluation of these continuous-flow assist pumps is complicated by the function of the native heart. In some patients native heart pulsations are present and can be palpated and used for standard blood pressure measurement with a cuff. These patients’ hearts open the aortic valve in native heart systole as often as every beat. Lumping together all continuous-flow patients, those that have retained more native heart pulsatility with those that have less call into question outcome reports particularly as they relate to adverse events. Some now call the flow with LVADs “low pulsatile flow” based upon the observation that a good proportion of the patients have some measurable pulse pressure [6]. In some reports [7] clinical complications with continuous-flow, non-pulsatile pumps have included pump thrombosis [8], ascending aortic thrombosis, hemolysis, aortic insufficiency, hemorrhagic and ischemic stroke, gastrointestinal bleeding, infection, right heart failure, aortic leaflet fusion, thinning of the peripheral blood vessel walls, endothelial damage, and sympathetic nervous system hyperactivity associated with hypertension [9, 10]. Other unanticipated, subtler acute, and chronic complications may be possible [11]. The intermediate-term changes created by continuous flow on the circulatory system and end organs are a pathophysiology that is poorly understood. However, improved short-term survival of heart failure patients with these devices compared to medical therapy has led to implantation of over 20,000 devices worldwide with the largest numbers in the USA and Germany [12]. Most patients do well for a limited time. Most seem to be neurologically intact and have normal end-organ function. However, looking at a composite end point of death, stroke, bleeding (primarily GI), device malfunction, and device-related infection [13], in over 12,000 patients from 2008 to 2014 with continuous-flow VADs, there was 50% occurrence at 3 months, 80% at 2 years, and 90% at 30 months. This end point omitted other complications that may have been concomitant including aortic insufficiency, right heart failure, leaflet fusion of the aortic valve, vascular wall pathology, endothelial damage, and hypertension. Also, those on continuous flow for bridge to transplantation (BTT) have only a 31% chance of transplantation after 1 year of continuous flow and just over 40% chance at 21 months. Those defined preimplantation as bridge to decision has only a 25% chance of transplantation at 2 years. Survival after a continuous-flow LVAD is 80%, 70%, 59%, and 48% at 1, 2, 3, and 4 years after implantation, respectively. Thus, the continued clinical experience with non-pulsatile devices has unveiled problems. Clinicians are now seeing and following patients, who have limited pulsation or no pulse at all. This is superimposed upon our complex and incompletely understood circulatory system. The question remains whether continuous flow is truly a good long-term intervention [14]. The experience with continuous-flow devices thus far has resulted in some [15,16,17] taking a renewed interest in pulsatile flow. Moazami and colleagues [15] concluded that “The true effects of chronic reduced pulsatility on hemostasis, the peripheral vasculature, and end organ function are largely unknown.” They also reviewed continuous-flow device problems of hemostasis, hemolysis, ventricular recovery, vascular thinning, end-organ function, and characteristics of pulsatility and proposed methods of flow modulation. They concluded that adding pulsation to LVADs may improve problems in these areas.
The device complication profile was significantly different with pulsatile-flow devices. Most notable was the very low incidence of GI bleeding, hemorrhagic stroke, aortic insufficiency, aortic valve fusion, vascular pathology, and pump thrombosis. Cheng and colleagues [16] reviewed studies comparing continuous-flow devices and pulsatile-flow devices regarding left ventricular (LV) unloading, LV remodeling, bridge to transplantation, aortic fusion and regurgitation, gastrointestinal bleeding, and right heart failure. They concluded that the major advances of continuous-flow devices are smaller size and increased durability and that these were responsible for improvements in survival. Further, they propose modifying continuous-flow devices to make them pulsatile devices. To have a better grasp of pulsatile versus non-pulsatile, we may need to look beyond short- and intermediate-term clinical results. We may need to more critically evaluate the impact on the microcirculation. This chapter will focus on the effects of pulsatile devices on the circulatory system with consideration given to both macro- and microcirculation.
Basic Information
Microvascular Circulation
As blood flows through the vascular tree, arterial branches become progressively smaller until reaching the capillary bed (Table 17.1) [18]. Pulsation becomes blunted. Transmural capillary pressure varies from 4 mmHg in the liver to 40 mmHg in the kidney glomerulus. Capillaries are tiny vessels of endothelial cells one cell layer thick. At any moment, only 5% of the blood volume is in the capillaries, but the approximate cross-sectional area of the capillary bed is 4500 cm2 [19], and the total surface area of the capillary walls in an adult is >70 m2 [20]. This huge area facilitates exchange including gases, molecules, fluid, nutrients, wastes, and hormones. Capillary diameter is about 5 μm at the proximal end and 9 μm at the distal end [19]. The microvascular walls are lined with a 1–2 μm layer of glycocalyx or “endothelial surface layer” (Fig. 17.1) [21]. Red blood cells (RBCs) tend to migrate away from larger vessel walls and to aggregate. Red blood cells passing through capillaries move single file (Fig. 17.1). Red blood cells 8–10 μm in diameter deform and squeeze through capillaries (Fig. 17.2). Separation of RBC from plasma often occurs at branch points resulting in shunting and nonhomogeneous flow to the capillary bed. As blood passes through progressively smaller vessels, the viscosity drops until it reaches vessels that approximate and then become smaller than the size of the RBC. Then it rises. At this point, RBC deformation occurs into parachute shaped or asymmetric crepe-shaped cells and the viscosity increases. White blood cells including lymphocytes, monocytes, and neutrophils are slightly larger, have less flexible cell membranes, and have more viscous cytoplasm than RBCs [22]. In low flow or inflammatory conditions, they may develop pseudopods and attach to the precapillary endothelium obstructing proximal capillaries [22]. Under normal conditions, leukocytes deform denuding the endothelial surface layer and move more slowly through capillaries than red blood cells. When RBCs are following a leukocyte, they form a slow-moving “train.” Mechanisms for capillary obstruction exist. Low energy, low flow, or low pressure could create microinfarctions and explain some observed clinical problems noted with continuous-flow device support. Venules may increase resistance in the system by RBC aggregation and slow rolling along walls by WBC.
Red blood cells changing shape and selectively flowing in one capillary branch. (Republished with permission of Annual Reviews, Inc., from Secomb [21]; permission conveyed through Copyright Clearance Center, Inc.)
RBC deformation varies with the capillary diameter. (Republished with permission of Annual Reviews, Inc., from Secomb [21]; permission conveyed through Copyright Clearance Center, Inc.)
Pulsatility may be necessary for optimal capillary bed perfusion. Inadequate microvascular perfusion in non-pulsatile support may be the cause of hemorrhagic stroke, AV malformation gastrointestinal bleeding, and other organ damage or dysfunction. The chronic effects of continuous-flow pumps in the microcirculation are not known. One wonders if simple non-pulsatile pressure is enough to make this system work optimally and chronically. And in the absence of pulsation, what increase in mean pressure must be necessary to drive blood cells through the capillary bed?
Besides the constraints of size of cellular elements and capillary diameter, arterioles, metarterioles, and precapillary sphincters may constrict in response to neural or humoral stimuli and thereby limit flow. Most of the resistance of the circulation is in the small arteries and arterioles. They constrict when pressure increases and dilate when pressure decreases, thus regulating vascular tone [21]. Other pulsatility-sensitive mechanisms for regulating resistance include calcium regulation by integrin mechanical receptors and NO release of endothelial cells in response to shear stress. This autoregulation of flow maintains adequate brain and kidney blood flows. In the case of very low pressure at the capillary inflow, these tiny vessels are subject to a critical closing pressure. They spontaneously close due to surrounding interstitial pressure being greater than the pressure at the capillary entrance. Lymphatic flow is facilitated by pulsatility. Interstitial volume and pressure may increase in the absence of pulsatility [22].
Pulsatile Perfusion
The pathophysiology of chronic continuous-flow pumping is just becoming apparent. Paradoxically, patients who do better with continuous flow have stronger pulsatility from their native hearts. The microvascular circulation is a likely site of pathology. My (JC) impression is that pathologic lesions in this extensively redundant system may at first be difficult to detect and may need to reach a critical number over time before becoming clinically manifest. In contrast to continuous flow, pulsatile pumps produce pulses in humans and animals that are very similar to those from the heart when the stroke volume is delivered to the proximal aorta. Wave propagation and flows are in the normal range.
The native pulse starts with the heart, and the pulse wave is propagated along the aorta and other elastic arteries (Fig. 17.3). The speed of the wave increases with increasing rigidity of the vessel; thus, it is faster in stiffer and in older calcified systems [23]. Waves caused by pulsation become more prominent as they pass distally. This results from antegrade waves and reflected waves [23]. This complex wave interaction produces pressure-flow relationships that depend upon branching sites and reflected waves. This wave is associated with the blood that flows in a laminar fashion in the larger vessels and creates shear axial and radial stress and strain (Fig. 17.4). These forces, shear stress, and cyclic strain and stretch on the endothelium activate genes controlling production of signaling molecules including growth factors that relate to endothelial apoptosis and integrins. Systemic vasorelaxation is NO production mediated and is related to vessel stretch [24]. Pulsatility is athero-protective. Pulsation also influences protein production and collagen synthesis in smooth muscle.
Progression of a composite pressure wave along seven levels of an arterial tree. The wave changes shape and becomes amplified by wave reflections as it travels from the proximal aorta (1) to distal aorta (7). (Reprinted by permission from Springer Nature: “Wave reflections” in Zamir [23])
The pulse wave propagation forces in an elastic vessel. (Reprinted by permission from Springer Nature: “Pulsatile flow in an elastic tube” in Zamir [23])
As the volume of the blood ejected from the heart or a pulsatile device reaches the larger vessels, the elastic lamina is stretched and causes local movements of the blood that leads to wave propagation. The aorta is “loaded” in systole and unloads in diastole, the Windkessel effect (Fig. 17.5).
As flow velocity increases within a vessel, the tendency to go from laminar to turbulent flow was described by Reynolds [25]. This is a phenomenon of parallel vectors of flow turning into flow with energy vibrating in random directions. The Reynolds number which relates fluid density and velocity with the diameter of the vessel and the fluid viscosity is used to assess this tendency. A number of >2000 poise is a conservative upper boundary of laminar flow. The aorta with an inner diameter of 2.5 cm under normal physiologic conditions with a flow of 5 l/min has a Reynolds number of 1063. Given the same conditions and flow, an inner diameter of 1.2 cm such as the HeartMate II outflow conduit would have a Reynolds number of 2211 poise.
Defining pulsatility clinically with current measurements available is most often done with pulse pressure (systolic/diastolic). Organ perfusion pressure is defined as mean arterial minus mean venous pressure. Recovery of end-organ function in critically ill patients depends on adequate organ perfusion. If the arterial pressure is adequate, but the central venous pressure is high (i.e., low organ perfusion pressure), perfusion may not be good enough to promote recovery. This concept seems to be most important for renal recovery. An example of this can be seen with the total artificial heart (TAH). With the TAH, the mean arterial pressure (MAP) is normal say 70 mmHg, and the CVP is usually around 10 or less giving a kidney perfusion pressure of 60 mmHg. If the MAP is 70 mmHg, but the CVP is 25 mmHg (from right heart failure after LVAD implantation), the kidney perfusion pressure is 45 mmHg. In patients with acute kidney injury (AKI), we nearly always see complete renal recovery with the TAH. In the multi-institutional TAH study (Ref. [26]), renal function returned to normal within 2 weeks. In a recent study from Virginia Commonwealth University [27] of patients with preimplantation renal insufficiency, 75% had renal function on TAH support improved from estimated glomerular filtration rate of 48 ml/min to 56–66 ml/min with a 6-month follow-up.
Pulsatility index (PI) has been used in HeartMate II continuous-flow LVAD patients to quantitate pulsatility (max. pump flow – minimum pump flow/average flow over 15 s × 10). Native heart pulsation can be strong enough to open the aortic valve or so weak that it just augments pump flow during systole, ejecting through the LVAD. For the adverse event of gastrointestinal bleeding, a lower pulsatility index (less pulsation in the circulation) correlates with more bleeding [28]. This is also true of aortic insufficiency. A lower pulse index is related to a greater incidence of aortic insufficiency.
Pulse Energy
Comparison of the Driving Force of Continuous and Pulsatile Pumps
In 1966, Shepard et al. described “energy equivalent pressure” (EEP) as the hemodynamic work per cc of blood pumped [29]. This measurement was based upon instantaneous measurements of pressure and flow. EEP is measured in mmHg. For continuous flow, the EEP equals the mean arterial pressure, a straight line over time. In a normal patient, one cardiac cycle, for pulsatile-flow EEP, is in the range of 40 mmHg greater than the mean. The magnitude of this difference over one systolic cycle is the area between the straight-line continuous flow curve and the pulsatile curve. No doubt, the energy of the pulse is much greater.
Another way of looking at this difference is surplus hemodynamic energy (SHE) which is equal to the EEP minus mean arterial pressure times 1332 (This converts the pressure to energy units (erg/cc)). Figure 17.6 shows a comparison of pulsatility of normal hearts, failing hearts, pulsatile VADs (PVAD), and continuous-flow VADs. There is almost no SHE for continuous flow. This subject is summarized nicely by Soucy, Slaughter et al. in a review of defining pulsatility in continuous-flow VADs [30].
SHE for the continuous-flow pumps is zero in the absence of native heart pulsation. PVAD is pulsatile ventricular assist device; CVAD is continuous-flow ventricular assist device. (Reprinted from Soucy et al. [30], with permission from Elsevier. This article supports the concept of modifying current continuous-flow pumps to give them some pulsatility)
The extra energy available with a pulse would appear to be an advantage. The microcirculation may need this extra energy to maintain adequate capillary flows as physiologic conditions change. Something simple like orthostatic change might be an example. Rising from a sitting to a standing position with continuous flow might limit cerebral perfusion.
Pulsatile Cardiopulmonary Bypass and ECMO
Pulsatility has been applied to cardiopulmonary bypass machines for support during routine operations as well as to extracorporeal membrane oxygenation (ECMO) when used for cardiac support. Damping of pulsations has been observed. This is most likely due to relatively small plastic cannulas placed in the aorta [31]. The better access options would seem to be either very large cannulas (24–28 Fr) or placement of a small graft (8–12 mm inner diameter). Peripheral grafting might simplify the procedure.
Speed changes in roller pumps create a pulse as does simultaneous use of intra-aortic balloon pumps . These are not physiologic pulses, and neither of these has become widely used; nevertheless many reports of improved results exist. A review of the literature by Sunagawa and colleagues covers the controversy [32].
Pulsatile flow on cardiopulmonary bypass has been found to optimize endothelial release of vasoactive substances, prevent activation of the renin-angiotensin system, decrease microcirculatory heterogeneity, reduce vasopressin and catecholamine levels, increase bronchial flow to the lungs, and improve subendocardial perfusion of the fibrillating heart. In clinical use, pulsatility has been found in some studies to decrease mortality [33], decrease the incidence of myocardial infarction, improve whole body flow, decrease pro-inflammatory cytokine release, improve postoperative renal function, reduce the length of hospital stay, and reduce the need for postoperative mechanical circulatory support. A meta-analysis reviewed over 200 papers comparing pulsatile bypass with continuous flow and concluded that there was “great variability among the techniques for creating pulsatility,” but that with pulsatile flow, postoperative creatinine clearances were higher, and serum lactates were lower [34]. Improved results have also been reported in the pediatric population [35]. Pulsatility has also been used in ECMO cases with some good preliminary results [36].
Problems with adding pulsatility by speed control of the currently used centrifugal pumps include the requirement for a “minimal pump speed” to prevent backflow and to maintain pressure, the possibility of generating air microemboli with abrupt alternation from low to high speed, and the sensitivity to afterload. As afterload increases, centrifugal and axial pump output decreases. Current roller pumps can pump against high resistance and create high pressure. But, on the inflow side, they can create a vacuum. Both types of pumps do not seem to be well suited for duplicating a normal physiologic pulse. A cardiopulmonary bypass pump (VentriFlo True Pulse Pump [Design Mentor, Pelham, NH]) that works like the heart, displacing volume with each beat and producing pulses that appear physiologic, is currently undergoing animal testing [37]. It promises for the first time in routine cardiopulmonary bypass to deliver true pulsatile flow (Fig. 17.7). Animal studies compared capillary flow with the VentriFlo pulsatile pump and the Rotoflow centrifugal continuous flow pump at the same mean flow and pressure. At 6 h of normothermic bypass, a normal capillary flow pattern was maintained with the VentriFlo compared to an abnormal heterogeneous pattern with the Rotoflow that included high-flow shunting, slow flow, sluggish flow, and no-flow areas [38].
Intra-Aortic Balloon Pumping
The intra-aortic balloon pump (IABP) has been widely used for over 50 years. This pneumatic technology has been very important in the treatment of severe ischemic heart disease before and after surgical intervention. An IABP catheter with balloon (usually 30–40 ml) is inserted via the femoral artery in the descending aorta. Pneumatic pulsation is timed (gated) with respect to the cardiac cycle as sensed using a pressure or an EKG tracing. It is used for counterpulsation meaning delivery of the pulse is timed to start just at the end of systole (aortic valve closure). Air is rapidly pumped into the balloon. Diastolic pressure and hence coronary artery flow is augmented. The second major effect is creating a presystolic pressure dip by deflating the balloon just before systole, thus reducing the afterload that the left ventricle must pump against. This is standard in patients with coronary artery disease, patients with heart failure and coronary artery disease, and some patients with heart failure alone. As a blood pump alone, it may augment the cardiac output by about 500–800 ml/min. This is not enough to make a significant difference in most heart failure patients. A laboratory comparison of ECMO, IABP, continuous-flow (CF) VAD, and pulsatile-flow (PF) VAD was done in a piglet model [39]. It demonstrated better left ventricular blood supply demand ratio during CFVAD, PFVAD, and ECMO but not IABP as well as improved global myocardial blood supply during PFVAD and CFVAD, but not ECMO or IABP.
As a treatment for severe heart failure that is not related to myocardial ischemia, the benefit of 500–800 ml/min additional flow with IABP is in most cases outweighed by the morbidity and mortality of the procedure. But, in patients with marginal coronary blood flow and heart failure, it can lead to significant improvement in cardiac function. The most common IABP morbidity is due to vascular injury or occlusion [40] from the intra-arterial catheter. Less commonly, we have seen bleeding problems when patients are heparinized for more than a few days, thrombocytopenia, aortic injury, distal embolism, and rarely perforation of the aorta (usually fatal).
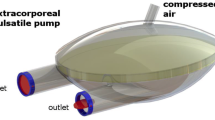
Extracorporeal Pulsatile Ventricular Assist Devices
There have been two types of pulsatile VADs, extracorporeal and intracorporeal. Both have saved thousands of lives. The Pierce-Donachy (Thoratec) pumps developed by Donachy and associates were the most popular extracorporeal [41], first implanted by Hill and Farrar and associates [42] and then by many others [43] as well as our own center. The extracorporeal pumps sit outside the body. Inflow and outflow cannulas are connected to the native heart and the prosthetic ventricle. They are versatile in that they do not need to fit inside the body, and they may be connected to the native heart in a variety of ways. The blood is drained from the native heart by a transcutaneous tube. It enters the pumping chamber via an inflow one-way valve and is pumped out by air pressure on the outside of the sac. This creates a pulse as blood flows out the outflow valve and outflow cannula into the aorta or pulmonary artery. The pulse is not timed with the native heart pulsation (Fig. 17.8) [44]. Because implantation involves the simple placement of cannulas in the heart, it is technically easy for the surgeon and not too risky for the patient. Connection options include inflow from atrium or from the ventricle. Outflow is to the appropriate artery (aorta or pulmonary artery). It is also easy to use a biventricular configuration. In biventricular support, options for drainage from either the atrium or the ventricle exist. The RVAD may have a right atrial or right ventricular (body) inflow cannula filling the prosthetic ventricle. Likewise, the LVAD may have an inflow cannula in either the left atrium or the left ventricle (apex) filling the left VAD. The outflow cannulas are attached through a graft sewn directly to the pulmonary artery (RVAD) or aorta (LVAD). With direct ventricular drainage, ventricular decompression is superior, cardiac outputs from the device tend to be higher, and results with biventricular configuration are superior to atrial cannulation. They deliver adequate pulsatile flow to maintain life and give the adult-sized patient the option of a considerable amount of mobility with a portable driver that has worked best in the LVAD, not BIVAD, configuration.
Markers on asynchronous VAD. Arterial pressure tracing showing native heart pressure with peaks marked by green dots and LVAD pressure with peaks marked by red dots. The native heart rate is about 90 beats/min. The LVAD rate is about 60 beats/min. There is no coordination of the LVAD rate with the native heart rate (asynchronous). Simultaneous beats result in higher systolic pressure
In this era, choosing between biventricular support and left ventricular was not a problem. Identification of right heart failure was not difficult. Our program and many others used a biventricular configuration more often than univentricular (LVAD) [45, 46]. There was no hesitation to support the right ventricle when it was failing on maximal medical therapy as judged by high CVP (>15 mmHg) and low RV ejection fraction (<20% by Multigated Acquisition Scan (MUGA)).
These VADs delivered pulses that were asynchronous with respect to the native heartbeat. In adults, it was rare to see pump outputs of greater than 5 l/min in either the univentricular or biventricular configuration. Long and narrow cannulas may have been the limiting factor. One of the problems we encountered in large patients with body surface areas of >2.5 m2 was continued heart failure with device therapy regardless of whether there was univentricular or biventricular support. We also found that once on mechanical support, a cardiac index of ≤2.0 l/min/m2 was unfavorable for survival and that >2.5 l/min/m2 cardiac index with device support in critically ill patients predicted survival [47, 48]. In our experience with the Thoratec VADs, this was achievable in most smaller patients (body surface area of <2 m2) [49].
Extracorporeal Pulsatile LVADs in Children
We used the Thoratec PVAD in a small (17 kg) boy [50]. He was the smallest to have a Thoratec LVAD. The device has a 70 ml stroke volume. Pumping at full stroke volume caused severe systolic hypertension with peak pressures of 170 mmHg. To solve this problem, we converted from a full fill mode (blood pumped only when the prosthetic ventricle was full) to a partial fill mode (filled only to about 40 ml then ejected by controlling the beat rate and the % systole). This cured his hypertension by reducing the stroke volume. He went on to successful transplantation and long-term survival with the donor heart of a 35-year-old woman.
The basic function of the Thoratec pump was passive fullfilling of the prosthetic ventricle as detected by a Hall effect sensor followed by full ejection. The rate of the pumping was therefore dependent on the rate of device filling. In adults, this worked well, but not in small children because they require much smaller stroke volumes than 70 ml.
We were fortunate to be the first in the USA to use the Berlin Heart in the 7-year-old child in October 2000 [51]. He was transplanted after 1 month and is alive 18 years later. This device was made primarily for children in a variety of ventricular sizes with stroke volumes from 10 to 60 ml. It may be implanted in the same configurations as noted for the Thoratec device. It consists of a rigid case, polyurethane tricuspid inflow and outflow valves, and blood and air chambers separated by a polyurethane diaphragm. It has been used in hundreds of children with better results in patients with cardiomyopathy and dilated hearts than in children with complex congenital cardiac disease [52]. We used the Berlin Heart and the Medos Heart, both pulsatile, as well as the continuous Rotoflow pump in children and neonates to treat acutely decompensating congestive heart failure. In children <2 years old and infants with decompensating cardiomyopathies, LVAD decompression with a cannula in the left ventricular apex [53, 54] provided excellent LV decompression and nearly uniformly led to rapid (hours to days) myocardial recovery. Seventy percent had native heart recovery and device removal with no episodes of recurrent heart failure. The key to success appeared to be LV decompression regardless of the pumping mechanism. Once the LV size reduced, LV wall thickness increased, and the hearts began ejecting almost immediately. Continued LVAD support allowed time for nearly complete reverse remodeling. Weaning from support averaged 2 weeks. Heart failure did not recur.
Problems with small pulsatile devices in small children with cardiomyopathy have included bleeding (44%), hypertension (34.5%), major infection (25%), stroke (11–24%), end-organ failure (30–50%), and pump change-out in 30–100% of patients [55]. Survival to 1-year post-implant has been just over 80% for cardiomyopathy patients and 30% for congenital heart disease patients [47]. The large number of pump change-outs resulted from thrombosis. Causes include low flows, small cannula sizes, and polyurethane inflow and outflow valves. Our method of anticoagulation was consistent for over 15 years and has been reviewed in full for children [56] and for adults [57]. This protocol resulted in acceptable thromboembolic and bleeding rates, but children were more challenging than adults presumably from smaller tubes, lower flows, polyurethane valves, small devices, and less washing of the device by blood flow.
Implanted Pulsatile-Flow LVADs
Two implantable pulsatile LVADs were widely used, HeartMate (two models: HeartMate I and HeartMate XVE) and Novacor. Each was abandoned in favor of smaller, easier to implant, continuous-flow pumps: HeartMate II, HeartWare, and now HeartMate 3. The pulsatile HeartMate devices (HeartMate I and XVE) also had durability issues and the Novacor embolism issues. A clinical comparison of the two devices from the Bad Oeynhausen group showed a slight survival advantage with the Novacor and documented the adverse events that were specific to each device [58].
There was a third device, unique because it was the only totally implantable LVAD with no wires or tubes passing through the skin. It featured transcutaneous energy transmission by induction coils. It also required that a volume compensator be placed in the chest, a necessity for preventing vacuum as the pump diaphragm moved from full to empty. The compensator was a balloon that allowed air to flow in and out from pump to compensator and vice versa as the pump diaphragm moved back and forth. A complete implant included the pump, a controller (electronic brains of the device) with battery, a volume compensator placed in the left chest, and the energy receiver subcutaneously above the right breast. A brief history of this device named “Lion Heart” is well summarized by the principle investigator Dr. Walter Pae [59]. There was a significant reduction in infections with this totally implanted device as compared to all other devices that had transcutaneous “drive lines” [59].
Novacor Ventricular Assist System
The Novacor left ventricular assist system, the invention of Peer Portner, PhD, was first used successfully as a bridge to transplantation (BTT) by Dr. Philip Oyer in 1984 at nearly the same time as the first Thoratec BTT by Donald Hill [60, 61]. In a novel spring-loaded, passively filling device with a smooth surface polyurethane lining on dual pusher plates, bovine pericardial inflow and outflow valves, and Dacron tube inflow and outflow conduits (later the inflow conduit was PTFE), the Novacor was driven by a solenoid-based motor. The inflow conduit was placed in the apex of the left ventricle and the outflow conduit in the ascending aorta. It filled during native heart systole and pumped the blood forward in diastole (counterpulsation pumping mechanism). Outputs from the pump were in the 6 l/min range. The initially recommended implantation technique for the Novacor as well as for the HeartMate pulsatile pump was more difficult than extracorporeal VADs. It required creating a pocket in the left abdominal wall between the muscular and fascial layers that extended caudally to near the iliac crest. An alternative technique described by Icenogle (T. Icenogle, personal communication) was adopted in our program. It involved marsupial-like partitioning of the anterior abdominal cavity with a large thick perforated PTFE sheet that was stapled to the inside of the abdominal wall. The device was placed anterior to the sheet, between the sheet and the anterior abdominal wall muscles, leaving the abdominal contents posterior to the sheet. The cephalic end of the sheet was stapled or sewn to the diaphragm such that the device space was in direct communication with the pericardial space. This completely separated the pump from the abdominal contents and eliminated extensive abdominal wall surgery at implant and explant as well as resulting in much less bleeding. No infections were seen with this technique.
With the Novacor device, there were no issues of GI bleeding, aortic insufficiency, or pump thrombosis. The major issue in some programs was embolic stroke variously reported to occur in 20–47% of cases [62]. The source of the emboli was most likely the inflow conduit from the left ventricular apex to the pump. It was Dacron and later switched to PTFE and contained a tissue valve. It was 6–9 cm in length. Pseudomembrane formation was reported in this conduit and was implicated in the strokes. Of interest was a high inter-institutional variability in the reported incidence of stroke suggesting varied operative and management techniques may have had a major impact. Another component of this device that was successfully tried in sheep, but never in humans, was a transcutaneous belt energy transformer that would have made the device totally implantable. A review of the clinical experience was written by the Stanford group [63].
HeartMate Left Ventricular Assist Devices
The HeartMate LVAD (HeartMate I and HeartMate XVE models) was implantable and about the same size as the Novacor (a discus shape of 11 cm in diameter and 4 cm in thickness). The implantation technique and positioning were like that of the Novacor heart. It appeared in two forms. The first was pneumatic, a single pusher plate displaced by pulses of air pressure [64]. The other side of the pumping chamber was part of the rigid titanium case. Both the diaphragm and rigid wall inside the pumping chamber were microscopically “textured,” sintered titanium on the rigid side, and flocked polyurethane on the pusher plate. Porcine xenograft valves on the inflow side and outflow side were part of their respective conduits. As time passed, the design was improved. Renamed the HeartMate XVE, it now had an electric motor [65]. The textured lining was envisioned to lead to an endothelial lining that would be non-thrombogenic. Rather it led to a coagulum of randomly distributed proteins and blood elements that resulted in a localized coagulopathy characterized by fibrinolysis and thrombin formation [66]. As a result of this, patients did not need any anticoagulant and were often just given aspirin alone or in combination with dipyridamole. The other issue created by this textured surface lining of the pump was immunological compromise. Opportunistic organisms infected the patients. Twenty-eight percent were infected with Candida within 3 months of implant [67]. It was found that CD4 T cells in patients with this device had increased susceptibility to cell death. This was a new finding not seen with smooth surface pump linings. Even so, the REMATCH trial [68] of 129 patients randomized between LVAD and medical treatment for very sick end-stage heart failure patients found significantly better survival at 1 year in the LVAD group (medical group survival 25%, LVAD group 52%). Complications with the LVAD included infection, bleeding, device malfunction, and neurologic dysfunction, and comparing the number for all complications, there were 2.35 times as many complications in the LVAD group as in the medical group. Right heart failure was noted in 17% of the implanted patients. By 2005, despite the wave of enthusiasm from the REMATCH trial, it was clear that a high percentage of HeartMate pumps were failing at 12–18 months following implantation primarily from inflow valve failure (regurgitation) and motor failure. This ended enthusiasm about this device as a long-term therapy. Of interest with this pump, GI bleeding and aortic insufficiency were rare, and there was no pump thrombosis .
The Total Artificial Heart
As of August 1, 2019, 1920 total artificial hearts had been implanted in humans since the Akutsu Heart by Cooley in 1969. The SynCardia (formerly called CardioWest and Jarvik-7) has accounted for 97% of implants and over 666 patient implant years with the longest being over 5 years [69]. This is an orthotopic biventricular (Fig. 17.9) pneumatic pulsatile pump lined with smooth segmented polyurethane, with tilting disk carbon pyrolite inflow and outflow valves (SynHall valves). A four-layered diaphragm separates the blood side from the air side (Fig. 17.10). Drive lines from the semirigid ventricles exit from the skin about 12 cm below the left costal margin and are connected to a driver that has adjustments for each ventricle for air pressure, beat rate, vacuum, and % systole (this determines the length of systole for one heart beat and is usually set at 50%). The flow rate of air exiting each ventricle is measured by pneumo-tachometers. Instantaneous measurement of the area under the air flow curve provides beat-to-beat stroke volume since the air volume exiting is equal to the blood volume entering the pump (fill volume). From this, instantaneous cardiac output is automatically calculated. Also, from this, the user sets the device so that the ventricle is only 70–80% filled (partial fill). Partial filling is a major advantage of pneumatic technology in total artificial hearts. It assures that the left and right ventricles are always in balance. It allows the patient to have an automatic “Starling” mechanism and allows the user to control for the effects of wide blood volume swings as might occur with volume transfusion. The ventricle maximal volume capacity is 70 ml. If we partially fill to “fill volume” of 50 ml (70% fill), at the end of the filling period, 20 ml of air remains on the other side of the four-layered diaphragm. If the right ventricle pumps more blood on the next beat, the increased volume simply displaces the left ventricle diaphragm a bit more, say 5 ml. And if less volume, say 10 ml, is pumped from the right on the next beat, the diaphragm is displaced by 10 ml less that the preceding beat. Similarly, if the patient goes for a walk and has increased venous return from his muscle pumps, more than 2 l/min increase in pump output can be automatically accommodated (20 ml reserve/beat times 120 beats/min provides 2400 ml/min increased flow). No sensor or feedback is required, and no adjustments need to be made. As it turns out, the fill volume is a surrogate for the CVP. An example of this is a patient on dialysis. Every 2- to 3-day dialysis, resulting in large volume shifts are not seen in patients with normal renal function. The clinician can watch the TAH fill volume each day. When it exceeds 60–65 ml, he sends the patient for hemodialysis and takes off enough fluid volume with the dialysis to drop the TAH fill volume to 50 ml. Thus, the mantra for the SynCardia TAH is “partial fill, full eject.” In patients with normal renal function, it is rare to need any adjustment in the driver controls after the first few days following implantation.
SynCardia total artificial heart. The native ventricles are removed and replaced by prosthetic left and right ventricles that each have inflow and outflow valves (pyrolite carbon SynHall valves). The drive lines pass from the device in the mediastinum through layers of muscle, subcutaneous fat, and skin. They are attached in this drawing to the Companion Driver for inhospital use. Transition to a wearable driver (Freedom driver) is made prior to discharge. (Reprinted from “Total artificial heart” in Selke et al. [70], 2010 with permission from Elsevier)
Cutawaydrawing of SynCardia total artificial left ventricle showing partial filling (fill volume to 50–60 ml) and full ejection (full excursion of diaphragms ejects fully with each beat). (Reprinted from “Total artificial heart” in Selke et al. [70], 2010 with permission from Elsevier)
There are three drivers available. The original console was very large containing an active console, a backup console, numerous alarms, and compressed air tanks. This has been an excellent driver but was phased out. The current drivers are the Companion which weighs about 50 pounds and is used in the hospital and the Freedom driver a 13.5-pound portable console that can be carried by the patient when he is discharged from the hospital.
Our first use of this device was in August of 1985 in a young man with biventricular failure [71]. The device replaced both ventricles and all four valves. It functioned well maintaining end-organ function in a critically ill person for whom there was no donor heart available. He was transplanted about 10 days later and lived for 5 years, the first successful bridge to transplant with a TAH. Since that time, we completed a multi-institutional trial from 1993 to 2002 [26]. In that trial 81 TAH-implanted patients were compared to matched controls. In the TAH group, 79% survived to transplantation, and 86% of those transplanted survived for over 1 year compared with the control group where 46% were transplanted and 69% of those survived for over 1 year after transplantation. More clinical data has been accumulated [72,73,74,75]. In these studies as in the multi-institutional study, patients were nearly all INTERMACs status 1 (“Crash and burn”: expected survival hours to days). Only 15% of LVAD continuous-flow patients since 2008 have been INTERMACS profile 1 [76, 77]. For continuous-flow pumps, most recipients are less sick with 38% of recipients being INTERMACS profile 3 (inotrope dependent, may be at home). Another indication for using the TAH is the central venous pressure (CVP). This may be the most important determinant of right heart failure in patients that are failing medical therapy indicating need for biventricular support. In our multi-institutional study, in patients on maximal medical therapy prior to implant, the mean CVP was 20 ± 7 mmHg. This stands in contrast to nearly every report on LVADs where the CVP before LVAD implantation has been around 12 mmHg and a CVP of >16 is a known risk factor for death after LVAD implantation [78]. One other factor that we considered pre-TAH implant was the RV ejection fraction on first-pass MUGA scan, where <20% ejection fraction was taken as right heart failure.
TAH Function
Function of the TAH is unique in current clinical usage in that it replaces orthotopically both ventricles giving the clinician complete control of the left- and right-sided circulations. There is no right heart failure with the TAH until the maximal pump flow of 9.8 l/min is exceeded (beat rate of 140 times full fill volume of 70 ml). Flow and output are not dependent on the shape and function of the native left and right ventricles. There are no native ventricles with the TAH. They have been removed to make room for the prosthetic ventricles. The criteria most often used to insure that the device will fit and not compress the inferior vena cava (IVC) or left pulmonary veins once the patient’s chest is closed are BSA > 2 m2, native heart LVEDD of ≥70 mm on echocardiogram, a “large heart” on chest X-ray with a CT ratio of >0.5, and on chest CT scan a distance of ≥10 cm from posterior sternum to anterior vertebral body at a level of T10 (tenth thoracic vertebra). There is also a recently introduced TAH with each ventricle 20 ml smaller, the “50 cc TAH.” Seventy-five patients have been implanted [79] with 53% in women and 18% in children. Finally, when there is still doubt about size, “virtual implantation” has been done many times [80, 81] and provides the radiologist and surgeon with superimposed views of the prosthetic ventricles placed three dimensionally on the chest CT scan of the potential recipient of the TAH. As a frequent consultant on these studies, I believe that in almost all cases, this has been very helpful in making the “fit” determination.
The implantation technique is not difficult; it is just “new” to most transplant surgeons. It involves doing a cardiectomy on the ventricular side of the AV groove, trimming the ventricular muscle to within 1 cm of the AV groove, closing the orifice of the coronary sinus, ligating the left atrial appendage, sewing in atrial connectors and great vessel grafts, passing the transcutaneous drive lines, and attaching the two ventricles. A detailed description of the implantation technique was reported by Arabia [82]. Additional implant and management information have been reported by an author (JC) [83, 84].
Once implanted and functioning, the SynCardia TAH pulsatile flow to the lungs and the body is physiologic. In the multi-institutional study [26] involving mean values for 95 patients just after TAH implantation, the cardiac index rose from 1.9 to 3.2 l/min/m2, the systolic pressure rose from 93 to 122 mmHg, the CVP fell from 20 to 14 mmHg, and the organ perfusion pressure (mean arterial pressure minus mean CVP) rose from 49 to 68 mmHg. Renal and hepatic function returned to normal from elevated pre-implant levels within 2 weeks. Most patients (75%) were out of bed within 1 week, and 60% were walking >100 ft within 2 weeks. A summary of 15 years of experience using the TAH with a consistent anticoagulation protocol [85] revealed that there were 8 strokes in 99 consecutive patients, most within 2–6 days after implantation and attributed to the operation. There were 2 strokes in chronically anticoagulated patients over a period of 24 patient years or 0.08 strokes per patient year. And there were two strokes in the two patients that developed prosthetic valvular infections. There were four GI bleeds, two known to be traumatic (esophagus and stomach) and two of unknown cause. There was no pump thrombosis. The anticoagulation protocol employed antiplatelet and anticoagulant therapy and monitored both. There was documented subclinical hemolysis attributed to the four mechanical valves. Hematocrit postimplantation was in the 20–25% range. Chronic anemia observed in these patients was felt to be due to low-grade hemolysis (free hemoglobin levels of <15–20 mg/dl, no obvious hemoglobinuria) and to inflammation caused by chronic contact of the blood with the TAH [86]. A moderate anemia may have some advantages. It decreases blood viscosity and by decreasing resistance and increasing pump output increases the “washing effect” of the blood passing through the ventricles. The high flows through the TAH, generally 6–8 l/min, are standard. Shear stress within the ventricles can be measured [87]. Thrombogenecity of various devices based upon platelet activation was found to be greater in continuous-flow devices [88] and much greater than that found in the pulsatile devices (M.J. Slepian, personal communication). Some antiplatelet drugs can control platelet activation in the TAH, but not in continuous-flow devices [89]. No cases of pump thrombosis have been reported with the SynCardia TAH.
While 70–80% of patients with the SynCardia device in experienced centers have been transplanted within 6 months [75] and the FDA device approval is limited to bridge to transplantation, the experience with long-term survival has been substantial. Over 395 patients have been implanted for more than 6 months, over 175 for 1 year, over 43 for 2 years, and over 6 for 4 years. An international experience with 47 SynCardia recipients that have had the device for at least 1 year has been published by Torregrossa and multiple institutions [90]. They addressed durability. There were 2 membrane perforations, 1 at 971 and the other at 801 days postimplantation in their group of 47 patients. Their search of the world literature is found including the two they reported a total of six reported incidents, three deaths. The earliest perforation was at 2 days and said to be related to an unauthorized resterilization at high temperature before implantation and perforation of one layer of the RV diaphragm. This patient survived with a reimplant of the RV. There were two events within 4–6 months of implantation with one death and three at over 693 days with two deaths. Thus, 0.4% of patients (approximately 1400 implants had been done at the time of their report) have had diaphragm failure, and 0.2% have subsequently died. An update from the company as of October 1, 2018, reports 8 perforations in 666 patient years or 0.01 events per patient year (S. Venkataramani, SynCardia Systems, Tucson, personal communication). The diaphragm has four layers, and there have not been any catastrophic leaks. This provides time to take remedial action.
Comparison of Pulsatile Devices: Extracorporeal VADs, LVAD, and TAH
From 1985 to 2000, at the University of Arizona, we had implanted 48 extracorporeal VADs (18 Symbion and 30 Thoratec), 37 implantable LVADs (Novacor), and 55 total artificial hearts (SynCardia, CardioWest). Patient selection was based upon failure of medical therapy, clinical condition, patient size, the presence or absence of right heart failure, and the presence or absence of renal failure. The study compared Thoratec extracorporeal (n = 26 [18 BIVAD and 8 LVAD]), Novacor LVAD (n = 23), and the TAH (n = 43) [91]. The TAH recipients were larger and had lower cardiac output and higher central venous pressures (CVPs) (20 ± 7 mmHg) than the other two groups. The percent surviving to transplantation were 75% TAH, 56% LVAD, and 38% BIVAD. Strokes were seen in 8% of TAH, 25% of LVAD, and 12% with the BIVADs. This unique single-center study comparing three devices had consistent selection and management protocols. Our conclusion was that biventricular support should be used in unstable patients with right heart failure. Patients too small for a TAH received a Thoratec. Novacor LVADs were reserved for more stable patients without right heart or renal failure.
Risk Factor Analysis
In the absence of studies directly comparing devices within the same institution, risk factor studies have been used to try to understand the impact of device types on the physiology of the patient. In 2008, we summarized ten pulsatile VAD and TAH risk factor studies [92]: two TAH, four Thoratec, two HeartMate, and two Novacor. For the TAH, significant multivariate risk factors for death included history of smoking and prothrombin time ≥16 s and had odds ratios of 10 and 4, respectively. For the Novacor, HeartMate, and Thoratec, CVP ≥ 16 mmHg, a diagnosis of right heart failure, renal failure markers (BUN > 40 mg/dl, creatinine elevation), reoperation, and mechanical ventilation were found to be significant predictors of mortality. These study results support our selection algorithm based upon our finding that biventricular failure in potential transplant candidates was best treated with the total artificial heart. If fitting the TAH appeared questionable, we used Thoratec BIVAD support.
Conclusions
It is difficult to think about modes of perfusion without comparing continuous and pulsatile flow. There is a huge experience with continuous-flow devices. Even the biggest enthusiasts admit there are many problems. Issues not seen with pulsatile devices have become apparent with continuous flow. Smaller size, ease of implantation, and greater durability favor continuous-flow devices. Disadvantages that lead to complications appear to be high shearing forces within the devices and, in many cases, decreased pulsatility or no pulsatility. Also, the LVAD does not treat right heart failure that in the previous era was routinely treated with preemptive pulsatile BIVAD or TAH placement. According to the INTERMACS registry, use of LVADs in the sickest patients and in patients with right heart failure has declined [13, 77]. Use in profile 1 patients has been stable at 15% for 10 years, for profile 2 patients use decreased from 40% to 36%, and in profile 3 use increased from 25% to 38%. At the same time in 17,000 implants, RV failure at the time of LVAD implantation was associated with a 3.76-fold increase in mortality [77]. We have learned that pulsation in LVAD patients is a good thing. There are less complications in patients with native heart pulsatility, and strategies for increasing native heart pulsatility in LVADs such as decreasing the rpm and allowing the aortic valve to be opened on every third beat are under consideration [12].
The physiology of pulsatile devices approaches and in the case of the TAH nearly duplicates the native heart. Shearing forces within the devices are much lower leading to less platelet activation that is controllable with available antiplatelet therapy. Size was not and is not a problem with the extracorporeal VADs that are still easily implanted. The implantable pulsatile LVADs required a bigger operation than current LVADs, but “not that big.” Durability was a problem with the HeartMate pneumatic and electric models that became significant by post-implant months 12–18. But, on the positive side, device “auto-anticoagulation” was caused by a low-grade fibrinolytic state. Only minimal if any antiplatelet therapy was used. The Novacor electric LVAD was durable. It had a long inflow conduit that in some hands caused an unacceptable amount of thromboembolism. The TAH is not difficult to implant providing the fitting guidelines are met nor is it difficult to explant if the recommended technique is followed [77]. Orthotopic implantation provides the shortest device blood flow pathway and allows the highest pump outputs. It is useful for bridge to transplantation in sicker patients and those with right heart failure. The INTERMACS profile 1 patients, the sicker potential transplant recipients with higher CVPs, can be salvaged (Table 17.2 Indications for TAH). Destination therapy with the TAH is being actively studied.
By 12 months of implantation time, approximately twice the percentage of TAH recipients are transplanted compared with LVADs. TAH advantages include removal of diseased myocardium and complete circulatory control of right and left sides.
The pathologic consequences of continuous flow were mentioned in the introduction of this chapter. Concern for these and the high frequency of death and multiple end points found in the INTERMACS registry [9] leads to the question of developing new or reexamining older pulsatile systems. Addressing the issue of biventricular failure is simple – use a biventricular device.
Compromising to find workable solutions has been the standard in mechanical perfusion since the days of Lillehei and Gibbon. Continuous flow has been the easier and more practical path to follow. Roller pumps and then centrifugal pumps led the way. Cardiopulmonary bypass with continuous-flow technology has been stagnant for decades. Some notable progress toward achieving true pulsatility for cardiopulmonary bypass has been mentioned [37, 38]. Axial flow pumps historically followed much later with the HeartMate II. Experience with continuous flow has led to great success but also to enough numbers of unanticipated and bad consequences that the question has been raised about the fundamental physiology. Does continuous flow provide enough energy to propel the blood through the circulatory system compared to pulsatile flow? Are we seeing inadequate capillary bed perfusion as a cause of GI bleeding in continuous-flow devices? If so, could this be present in other organs and causing problems such as hemorrhagic cerebral infarcts? Are we able to detect microcirculatory disease at an early stage? Beneficial effects of pulsatility on sympathetic nervous system function, neurohumoral signaling, and vascular and valvular function are also lost with continuous flow.
The other major difference between continuous-flow devices and pulsatile is trauma to the blood. Forces on platelets and red blood cells as well as proteins such as von Willebrand multimers are generated by rotary devices spinning at 2500–10,000 rpm. These are much greater than shear stress of pulsatile pumps that produce a true physiologic pulse. Consequently, with continuous flow pumps, platelet activation and hemolysis are seen and are procoagulant.
Durability is another consideration. If 6–10% of continuous-flow pumps thrombose within 1 year and need replacement and there is a significant mortality in the following year (30%) [93], durability is an issue. Granted some continuous-flow device, patients have survived for over 5 years. Most have not. Survival is 48% at 5 years. The only pulsatile device to have durability issues was the HeartMate XVE.
Summarizing the pulsatile era, the results were good, and bridge to transplantation became successful. Pulsatility did not stand out as a problem. It simply mimicked the normal human circulation. Durability, size, and thromboembolism as we have outlined were problems with some of the devices. Durability in the broadest sense of the word means absence of device failure over some specified number of years. We have nothing mechanical that approaches the durability of the transplanted heart. Size reduction as seen with current continuous-flow pumps comes at the price of damage to the blood by obligatory continuous rotary flow, not to mention the problems inherent in lack of pulsatility and retention of diseased ventricles. A return to pulsatility in LVADs may now be in order.
The gold standard for pulsatile perfusion is volume displacement. Technologies may not necessarily need to be electrical and miniaturized. An example is left-right balance and an automatic Starling mechanism in the pneumatic TAH. Thus far, other implantable technologies have struggled with this balance that is vital for biventricular support and is simply accomplished with pneumatic technology and partial fill full eject pump management.
References
Bishopric NH. Evolution of the human heart from bacteria to man. Ann N Y Acad Sci. 2005;1047:13–29.
Barrett KE, Barman SM, Boitano S, Brooks HL. Ganong’s review of medical physiology. 24th ed. New York: The McGraw Hill Companies, Inc.; 2012. p. 602.
Saeed O, Rangasamy S, Reyes M. Speed reduction does not restore high molecular weight von Willebrand multimers during HeartMate II support: an in vivo study. ASAIO J. 2018;64(5):e123–5.
Cooley DA. C. Walton Lillehei, the “Father of open heart surgery”. Circulation. 1999;100(13):1364–5.
Hill JD. John H. Gibbon, Jr. Development of the first successful heart lung machine. Ann Thorac Surg. 1982;34:337–4.
Rangasamy S, Madan S, et al. Non-invasive measures of pulsatility and blood pressure during continuous flow left ventricular assist device. ASAIO J. 2019;65(3):241–6.
Cornwell WK, Urey M, et al. Continuous flow circulatory support: the Achilles heel of current left ventricular assist devices? Circ Heart Fail. 2015;8:850–2.
Starling R, Moazami N, Silvestry S, et al. Unexpected abrupt increase in left ventricular assist device thrombosis. NEJM. 2014;370:33–40.
Markham DW, Fu Q, Palmer MD, et al. Sympathetic neural and hemodynamic responses to upright tilt in patients with pulsatile and nonpulsatile left ventricular assist devices. Circ Heart Fail. 2013;6:293–9.
Cornwell WK, Tarumi T, et al. Restoration of pulsatile flow reduces sympathetic nerve activity among individuals with continuous flow left ventricular assist devices. Circulation. 2015;132:2316–22.
Purohit SN, Cornwell WK, et al. Living without a pulse. Circ Heart Fail. 2018;11:1–11. e004670. https://doi.org/10.1161/Circheartfailure.117.004670.
Aissaoui N, Morshuis M, Maoulida H, et al. Management of end-stage heart failure patients with or without ventricular assist device: an observational comparison of clinical and economic outcomes. Eur J Cardiothorac Surg. 2018;53(1):170–7. https://doi.org/ 10.1093/ejcts/ezx258. PMID:28950304ClinicalTrial
Kirklin JK, Naftel DC, et al. The seventh InterMacs annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34:1495–504.
Miller L. We always need a pulse or do we? J Cardiovasc Trans Res. 2012;5:296–301.
Moazami N, Dembitsky WP, Adamson R, Steffen RJ, Soltesz EG, Starling RC, Fukamachi K. Does pulsatility matter in the era of continuous-flow blood pumps? J Heart Lung Transplant. 2015;34:999–1004.
Cheng A, Williamitis CA, Slaughter M. Comparison of continuous flow and pulsatile flow left ventricular assist devices: is there any advantage of pulsatility? Ann Cardiothorac Surg. 2014;3(6):573–81.
Guan Y, Karkhanis T, Wang S, et al. Physiologic benefits of pulsatile perfusion during mechanical circulatory support for the treatment of acute and chronic heart failure in adults. Artif Organs. 2010;34(7):529–36.
Barrett KE, Barman SM, Boitano S, Brooks HL. Ganong’s review of medical physiology. 24th ed. New York: The McGraw Hill Companies, Inc.; 2012. p. 571.
Barrett KE, Barman SM, Biotano S, Brooks HL. Ganong’s review of medical physiology. 24th ed. New Delhi: Tata McGraw-Hill; 2012. p. 571.
Popel AS, Johnson PC. Microcirculation and hemorheology. Annu Rev Fluid Mech. 2005;37:43–69.
Secomb TW. Blood flow in the microcirculation. Annu Rev Fluid Mech. 2017;49:443–61.
Schmid-Shoenbein GW. The damaging potential of leukocyte activation in microcirculation. Angiology. 1993;44(1):45–56.
Zamir M. The physics of pulsatile flow. New York: Springer-Verlag; 2000. p. 114–5.
Domanski MJ, Giddens DP. Optimization of pulsatile flow for mechanical circulatory support. J Heart Lung Transplant. 2013;32:577–8.
Zamir M. The physics of pulsatile flow. New York: Springer-Verlag; 2000. p. 18.
Copeland JG, Smith RG, Arabia FA, et al. Cardiac replacement with a total artificial heart as a bridge to transplantation. NEJM. 2004;351:859–67.
Quader MA, Goodreau AM, et al. Renal function recovery with total artificial heart support. ASAIO J. 2016;62:87–91.
Wever-Pinzon O, et al. Pulsatility and the risk of non-surgical bleeding in patients supported with continuous flow ventricular assist device HeartMate II. Circ Heart Fail. 2013;6:517–26.
Shepard RB, Simpson BD, Sharp JF. Energy equivalent pressure. Arch Surg. 1966;93(5):30–40.
Soucy KG, Koenig SC, Giridharan GA, Sobieski MA, Slaughter MS. Defining pulsatility during continuous-flow ventricular assist device support. J Heart Lung Transplant. 2013;32:581–7.
Dinardo J. Anesthesia for cardiac surgery. Stamford: Appleton & Lange; 1998. p. 385.
Sunagawa G, Koprivanac M, Karimov JH, Mozami N, Fukamachi K. Is a pulse absolutely necessary during cardiopulmonary bypass? Expert Rev Med Devices. 2017;14(1):27–35. https://doi.org/10.1080/17434440.2017.1265445.
Ji B, Undar A. An evaluation of the benefits of pulsatile versus non-pulsatile perfusion during cardiopulmonary procedures in pediatric and adult patients. ASAIO J. 2006;52:357–61.
Sievert A, Sistino J. Meta-analysis of renal benefits of pulsatile perfusion in cardiac surgery. J Extra Corpor Technol. 2012;44:10–4.
Alkan-Bozkaya T, Akçevin A, Türkoğlu H, Ündar A. Impact of pulsatile perfusion on clinical outcomes of neonates and infants with complex pathologies undergoing cardiopulmonary bypass procedures. Artif Organs. 2013;37:82–6.
Agati S, Mignosa C, Ciccarello G, et al. Pulsatile ECMO in neonates and infants: first European clinical experience with a new device. ASAIO J. 2005;51:508–12.
Sunagawa G, Karimov JH. New technology to achieve true physiologic pulsatile flow during cardiopulmonary bypass. ASAIO annual conference, San Francisco, CA; June 15–18, 2016.
Sunagawa G, Karimov JH, et al. Impact of physiologic pulsatile flow on microcirculation during cardiopulmonary bypass. ASAIO poster presentation; 2016.
Bartoli CR, Koenig SC, et al. Extracorporeal membrane oxygenation vs counterpulsatile, pulsatile, and continuous flow left ventricular unloading for pediatric mechanical circulatory support. Pediatr Crit Care Med. 2013;14(9):e424–37.
Meco M, et al. Morbidity and mortality from intra-aortic balloon pumps. J Cardiovasc Surg. 2002;13:17–23.
Donachy JH, Landis DL, Rosenberg G, Prophet GA, Ferrar IO, Pierce WS. Design and evaluation of a left ventricular assist device: the angle port pump. In: Unger F, editor. Assisted circulation. Berlin: Springer-Verlag; 1979.
Farrar DJ, Hill JD, Gray LA, Pennington DG, McBride LR, Pierce WS, Pae WE, Glenville B, et al. Heterotopic prosthetic ventricles as a bridge to cardiac transplantation. N Engl J Med. 1988;318:333–40.
Pennington G, Kanter KR, et al. Seven years’ experience with the Pierce-Donachy ventricular assist device. J Thorac Cardiovasc Surg. 1988;96:901–11.
Icenogle TB, Williams RJ, Smith RG, et al. Extracorporeal pulsatile biventricular support after cardiac transplantation. Ann Thorac Surg. 1989;47:614–6.
Farrar DJ, Hill JD, Pennington DG, et al. Preoperative and postoperative comparison of patients with univentricular and biventricular support with Thoratec ventricular assist device as a bridge to cardiac transplantation. J Thorac Cardiovasc Surg. 1997;113:202–9.
McBride LR, Naunheim KS, et al. Clinical experience with 111 Thoratec ventricular assist devices. Ann Thorac Surg. 1999;67:1233–9.
Mehta VK, Copeland JG, Arabia FA, Smith RG, Banchy ME. Analysis of premorbid comorbid factors associated with biventricular assist device and total artificial heart: a single center experience. J Heart Lung Transplant. 2000;19:65.
Mehta VK, Copeland JG, Arabia FA, Banchy ME, Smith RG. Mechanical ventricular support as a bridge to transplant: risk factors and selection. ASAIO J. 2000;46:192.
Copeland JG, Smith RG, Nolan P, et al. Comparison of the CardioWest total artificial heart, the Novacor left ventricular assist system, and the Thoratec ventricular assist system in bridge to transplantation. Ann Thorac Surg. 2001;71(3):S92–7.
Copeland JG, Arabia FA, Smith RG. Bridge to transplantation with a Thoratec LVAD in a 17 kg child. Ann Thorac Surg. 2001;71(3):1003–4.
Arabia FA, Tsau PH, Smith RG, Nolan P, Paramesh V, Bose R, Woolley DS, Sethi GK, Rhenman BE, Copeland JG. Pediatric bridge to heart transplantation: application of the Berlin Heart, Medos Heart, and Thoratec ventricular assist devices. J Heart Lung Transplant. 2006;25:16–21.
Morales D, Zafar F, Almond CS, et al. Berlin Heart EXCOR use in patients with congenital heart disease. J Heart Lung Transplant. 2017;36:1209–16.
Zimmerman H, Covington D, Smith RG, Inhat C, Barber B, Copeland JG. Recovery of dilated cardiomyopathies in infants and children using left ventricular assist devices. ASAIO J. 2010;56:364–8.
Ihnat C, Zimmerman H, Copeland JG, Meany FJ, Soboyna RE, Larsen BT, Blair D, Barber BJ. Left ventricular assist device support: a longitudinal echocardiographic follow-up and search for predictors of successful weaning in young children with heart failure as a bridge to recovery. Congenit Heart Dis. 2011;6:234–40. https://doi.org/10.1111/j.1747-0803.2011.00494.x.
Maeda K, Almond C, et al. Refining of the pump exchange procedure in children supported with the Berlin Heart EXCOR ventricular assist device: 10 years experience at a single institution. J Heart Lung Transplant. 2015;34(4S):588.
Copeland H, Nolan P, Covington D, Gustafson M, Smith RG, Copeland JG. A method of anticoagulation for children on mechanical circulatory support. Artif Organs. 2011;35:1018–23.
Copeland J, Copeland H, Nolan P, Gustafson M, Slepian M, Smith R. Results with an anticoagulation protocol in 99 SynCardia total artificial heart patients. ASAIO J. 2013;59:216–20.
El-Banayosy A, Arusoglu L, et al. Novacor left ventricular assist system versus HeartMate vented electric left ventricular assist system as a long-term mechanical circulatory support device in bridging patients: a prospective study. J Thorac Cardiovasc Surg. 2000;119:581–7.
Pae W, Collell JM, et al. Does total implantability reduce infection with the use of a left ventricular assist device? The LionHeart experience in Europe. J Heart Lung Transplant. 2007;26:219–29.
Starnes V, Oyer P, Portner PM, et al. Isolated left ventricular assist as bridge to cardiac transplantation. J Thorac Cardiovasc Surg. 1988;96:62–71.
Portner PM, Oyer PE, Pennington G, et al. Implantable electrical left ventricular assist system: bridge to transplantation and the future. Ann Thorac Surg. 1989;47:142–50.
Schmid C, et al. Cerebral and systemic embolization during left ventricular support with the Novacor LVAS. Ann Thorac Surg. 1998;65(6):1703–10.
Robbins R, Kwon M, Portner P, Oyer PE. The totally implantable Novacor left ventricular assist system. Ann Thorac Surg. 2000;71(3):S162–5.
Frazier OH, Rose EA, et al. Multicenter clinical evaluation of the HeartMate 1000 IP left ventricular assist device. Ann Thorac Surg. 1992;53:1080–90.
Dowling RD, Park SJ, Pagani AJ, et al. HeartMate VE LVAS design enhancements and its impact on device reliability. Eur J Cardiothorac Surg. 2004;25(6):958–63.
Spanier T, Oz M, Levin H, et al. Activation of coagulation and fibrinolytic pathways in patients with left ventricular assist devices. J Thorac Cardiovasc Surg. 1996;112:1090–7.
Ankersmit HJ, Tugudea S, Spainier T, et al. Activation induced T-cell death and immune dysfunction after implantation of left ventricular assist device. Lancet. 1998;354(9178):550–5.
Rose E, Gelijns A, et al. Long term use of a left ventricular assist device for end stage heart failure. NEJM. 2001;345:1435–43.
Syncardia Systems Inc, 1992 E Silverlake Rd, Tucson Az, 85713.
Zimmerman H, Copeland JG, Aquila LA, Smith RG. Total Artificial Heart. In: Selke FW, DelNido PJ, Swanson SJ, editors. Sabiston and spencer surgery of the chest. Vol 2, Philadelphia: Saunders; 2010; pp 1525–32.
Copeland JG, Levinson MM, Smith RG, et al. The total artificial heart as a bridge to transplantation: a report of 2 cases. JAMA. 1986;256(21):2191–5.
Copeland JG, Copeland H, Gustafson M, et al. Experience with over 100 total artificial heart implants. J Thorac Cardiovasc Surg. 2012;143:227–34.
Leprince P, Bonnet N, Rama A, et al. Bridge tot transplantation with the Jarvik-7 (CardioWest) total artificial heart: a single center 15 year experience. J Heart Lung Transplant. 2003;22:1296–303.
Torregrossa G, Anyanwu A, et al. SynCardia: the total artificial heart. Ann Cardiothorac Surg. 2014;3(6):612–20.
Arabia FA, Gregoric I, Kasarajan JD, Moriguchi JD, et al. Total artificial heart (TAH): survival, outcomes, risk factors, adverse events in InterMacs. J Heart Lung Transplant. 2016; abstract A 3190.
Stevenson LW, et al. INTERMACS profiles of advanced heart failure: the current picture. J Heart Lung Transplant. 2009;28:535–41.
Kirklin JK, et al. Eight annual INTERMACS report: special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36:1080–6.
Leitz K, Long J, et al. Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era. Circulation. 2007;116:497–505.
Courtesy of SynCardia Systems Statistics as of August 1, 2018, 1992, Tucson, AZ.
Virtual sizing done by ASU/Phoenix Children’s Hospital through SynCardia Systems, 1992, Tucson, AZ.
Moore R, Lorts A, et al. Virtual implantation of the 50 cc SynCardia total artificial heart. J Heart Lung Transplant. 2016;35:824.
Arabia FA, Copeland JG, Pavie A, Smith RG. Implantation technique for the CardioWest total artificial heart. Ann Thorac Surg. 1999;68:698–704.
Copeland JG, Arabia FA, Tsau P, et al. Total artificial hearts: bridge to transplantation. Cardiol Clin. 2003;21:101–13.
Copeland JG, Arabia FA, Smith RG, et al. Synthetic membrane neo-pericardium facilitates total heart explantation. J Heart Lung Transplant. 2001;20:654–6.
Copeland J, Copeland H, Nolan P, Gustafson M, Slepian M, Smith R. Results with an anticoagulation protocol in 99 SynCardia total artificial heart recipients. ASAIO J. 2013;59:216–20.
Pierce CN, Larson DL, Arabia FA, Copeland JG. Inflammatory mediated chronic anemia in patients supported with a mechanical circulatory assistance device. J Extra Corpor Technol. 2004;36:10–5.
Slepian MJ, Alemu Y, et al. The SynCardia total artificial heart: in vivo, in vitro, and computational modeling studies. J Biomech. 2013;46:266–75.
Girdhar G, Xenos M, et al. Device thrombogenicity emulation: a novel method for optimizing mechanical circulatory support device thromboresistance. PLoS One. 2012;7(e32463):1–8.
Valerio L, Tran PL, et al. Aspirin has limited ability to modulate shear-mediated platelet activation associated with elevated shear stress of ventricular assist devices. Thromb Res. 2016;140:110–7.
Torregrossa G, Morshuis M, et al. Results with the SynCardia TAH beyond one year. ASAIO J. 2014;60(6):626–34.
Copeland JG, Smith RG, Arabia FA, et al. Comparison of the CardioWest total artificial heart, the Novacor left ventricular assist system, and the Thoratec ventricular assist system in bridge to transplantation. Ann Thorac Surg. 2001;71:S92–7.
Copeland JG, Smith RG, Bose RK, et al. Risk factor analysis for bridge to transplantation with the CardioWest TAH. Ann Thorac Surg. 2008;85:1639–44.
Moazami N, Milano C, et al. Pump replacement for left ventricular assist device failure can be done safely and is associated with a low mortality. Ann Thorac Surg. 2013;95:500–5.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Copeland, J., Copeland, H. (2020). Pulsatile Mechanical Circulation, Physiology, and Pump Technology. In: Karimov, J., Fukamachi, K., Starling, R. (eds) Mechanical Support for Heart Failure . Springer, Cham. https://doi.org/10.1007/978-3-030-47809-4_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-47809-4_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47808-7
Online ISBN: 978-3-030-47809-4
eBook Packages: MedicineMedicine (R0)