Abstract
Mitochondria are the energy houses of cells. Cell functioning and stability are critical responsibilities of mitochondria. The other functioning of cells includes ATP production, intracellular calcium ion regulation, production of reactive oxygen species, radical scavenging property, regulation of the cell survival and death, and caspase family of protease stimulation. Mitochondrial dysfunction can be described as abnormality in functioning in addition to the production of reactive species. Mitochondrial dysfunction leads to the development of metabolic syndromes such as obesity, diabetes, and neurodegenerative disorders. Since the past, many studies have been done on morphology, physiology, and pharmacology of mitochondria involved in metabolic diseases. By adopting interventions that include lifestyle intervention, pharmacologic approaches, and the targeted-mitochondrial methodologies, the progression of metabolic disease decelerates. These approaches are involved in maintaining mitochondrial number and morphology, eliminate dysfunctional mitochondria, and reduce oxidative stress in metabolic disorders. The aim of the study is to illuminate the role of mitochondria in the metabolic disorder and sum up the process of the targeted mitochondrial molecule to treat metabolic syndrome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Mitochondria are rod-shaped organelles found intracellularly. Mitochondria are also known as the driving force of cell because it produces most of the energy supply of cells in the form of adenosine triphosphate (ATP) and also plays a dynamic part in metabolizing nutrients. There are many other cell functions performed by mitochondria like energy metabolism along with the production of ion radicals, homeostasis, and cell integrity [1, 2]. Mainly, glucose is oxidized to produce ATP via OXPHOS and also the metabolites of Kreb’s cycle and fatty acid are also oxidized to produce ATP. Presently, it is now a well-known fact that pathophysiological changes produced in mitochondria in metabolic disease are directly linked with decreased mitochondrial working with the time as age increases, the biogenesis of mitochondria is decreased which may be due to changes in pattern of segregation and merging of mitochondrial cells and inhibiting the process of mitophagy. In this process, the dysfunctional mitochondria are removed [3]. The reactive oxygen species belong to a free radical family, it includes O2−, OH−, and peroxyl [4]. Mitochondrial cells have many defense processes to pledge the production of ROS, as it is a predictable process and can be held whenever generated. This overproduction of reactive oxygen species causes the DNA, lipids, and proteins to degrade to some extent [2]. Oxidative stress is a risk factor for several diseases, including cancer, diabetes, stroke, aging, and neurodegenerative diseases [5]. There are various pathophysiological conditions that emerge due to oxidative stress which is related to metabolic disorders [5].
Metabolic syndrome is a cluster of health issues that include obesity, diabetes, and dyslipidemia. These conditions increased the risk of elevated blood glucose level, heart and blood vessel diseases. In this modern era, it may be the major health issue of this society. Metabolic syndrome has several causes that act together like overweight and obesity. Also, other factors involved in metabolic diseases are social, personal, and economic burden [6]. From previous studies, it was evident that environmental factors and genetic variability participate in increasing the situation of metabolic syndrome [7]. There are numerous data available that proves the role of mitochondrial dysfunction and aging in the pathophysiology of aging, neurodegenerative disorder, and metabolic disease [5]. However, the basic mechanism of metabolic syndrome still remains unknown. This review article basically focused on the mode of action involved in mitochondrial abnormality and the link between this abnormality and the metabolic syndrome. So that the pharmacologic actions were taken to target dysfunctional mitochondria to prevent the health hazards associated with a metabolic disorder.
Functional and Dysfunctional Mitochondria
Mitochondria are cytoplasmic membranous organelle; it has its own self-replicating genome. Mitochondria play a vital role in maintaining metabolic homeostasis and are mediators of cell integrity. The energy produced by mitochondria in eukaryotes is by oxidation of NADHA/FADH2 via glycolysis. In addition to glycolysis, other mechanisms are also involved in generating NADH2/FADH2; these are the TCA cycle, oxidative phosphorylation, and β-oxidation of fatty acids. These processes are controlled by transcription factors present in mitochondria and there are about 800–1000 copies of mtDNA present in the single mitochondrion that is inherited and packaged in nucleoids [8]. However, nucleoids are widely spread in the matrix of mitochondria but mostly reside in the vicinity of cristae. Cristae is an organelle that carries the OXPHOS system. Between inner and outer membrane there is a small space present which is called intermembrane space. The outer and intramembranous space of mitochondria has more penetration power than the inner membrane. The permeability of the inner membrane is low because the inner membrane has enzymes that perform the ETC process to generate ATP. The mitochondrial matrix is surrounded by a mitochondrial membrane where the TCA cycle produces electrons that are taken up by ETC to produce ATP. The OXPHOS process is derived through the production of electrochemical gradient across the inner membrane [9].
The electron transport chain contains five subunits of enzyme complexes. These are complex I (NADH ubiquinone reductase), complex II (succinate dehydrogenase), complex III (Ubiquinol-cytochrome c reductase), complex IV (cytochrome c oxidase), and complex V (F0F1 ATP synthase). They are located in the inner mitochondrial membrane [10]. Electrons are donated by the TCA cycle which then travel to the electron transport chain. These electrons travel from enzyme complex I to V. Transport of protons is also coupled with the transfer of electrons along the ETC that generate electrochemical gradient which produces ATP [11]. Mitochondria continuously produce reactive species by metabolizing oxygen. The electron flow through the electron transport chain is an imperfect process. Mitochondria consume incompletely reduced oxygen and produce reactive species such as (•O−2) which is also called “Primary” ROS [12]. The secondary ROS is also generated due to the excessive generation of primary ROS [13]. It has been proved that the deoxyribose, backbone of DNA, i.e., a nitrogenous base, purine and pyrimidine, damages due to the interlinking of hydroxyl radical with DNA [2]. The increased production of reactive species causes damage in mitochondrial proteins/enzymes, DNA, and other cell structures as a result of an abnormality in mitochondrial functioning and failure to produce ATP in mitochondria [12]. The electron transport chain also generates other reactive species of nitrogen. Nitration induced by reactive nitrogen species is affected by cellular proteins and glutathione. Similarly, free radicals which are produced freely can also inhibit the oxidative damage both by enzymatic and non-enzymatic mechanism. The mechanisms involved can scavenge free radicals by antioxidants or lead to generation of free radicals.
The oxidative stress which is produced by increased release of free radicals can be overcome by several defense mechanisms. The following are involved in enzymatic defense mechanism such as SOD, CAT, GR, and GPx. Similarly, the non-enzymatic defense system possesses antioxidant compounds such as Vitamin C and E, glutathione, etc. The ionic imbalance produces damage in the cells which causes other abnormalities to appear in the cell including impairment of enzymatic functions which further degrade the mitochondrial function [5]. In diabetes, the number and functioning of mitochondria are reduced by reducing oxidative phosphorylation [14]. In mammalian cells, as a key regulator of body functions, neurodegenerative disorders occur even due to minute change in mitochondria [15]. Figure 3.1 represents the mechanisms involved in functional and dysfunctional mitochondria.
Mechanisms Controlling Mitochondrial Replication
Mitochondria in combination with nuclear and mitochondrial genome maintain its physiology and morphology with the help of various transcription factors. These transcriptional factors include nuclear respiratory factor, mitochondrial transcriptional factor A, PPARs, uncoupling proteins, estrogen and its related factors α and γ [16], Tfam, NRF, and NRF-2. To maintain the integrity of mitochondria, various stimuli are involved, which may be pathological and physiological. In combination with the above compounds, co-transcriptional regulatory factors are also involved in regulating a number of mitochondria. Physical exercise, dietary changes, and muscle movements are also the stimuli that contribute to maintaining the number of mitochondria. These transcriptional factors interact with co-transcriptional factor Peroxisome proliferator-activated receptor (PPAR)-γ coactivator-1α (PGC-1α) to control the transcription of the main enzyme in mitochondria and also synthesize mtDNA [17]. In the case of low energy, along with transcription factors, there are two more enzymes to compensate for the low energy state, these include AMP-activated protein kinase and mammalian counterpart of silent information regulator 2. These are also called as metabolic sensors. In the case of low energy state, the AMP activates protein kinase phosphorylate and mammalian counterpart of silent information regulator 2. In a low energy state, AMPK phosphorylates and SIRT1 acetylates to regulate PGC-1α [18]. The role of PGC-α and other transcriptional factors is well-portrayed in literature. It has been proved in many studies that due to pathologic conditions changes occur in morphology and number of mitochondria in different body organs such as heart and skeletal muscles [1].
Fission and Fusion Balance of Mitochondria
Mitochondria host the process of fission and fusion and its balance, the balance between these two processes is called mitochondrial dynamics (Fig. 3.2). Mitochondrial dynamics are involved in maintenance during cell growth and cell death and its pathway and also eradicate the worn-out mitochondria [19]. This process was explained for the first time when the yeast was budded [20].
The shape and size of mitochondria fluctuate frequently due to external stimuli which may include the number of nutrients and others. Mitophagy is a process in which mitochondria fuse with lysosomes via fusion and remove the dysfunctional mitochondria; in other words, it is an autophagy-lysosomal system [21]. When the amount of nutrients increases from its demand and cellular dysfunction worsens, it causes mitochondrial fragmentation and increases the risk of metabolic diseases [22]. The impairment of mitochondria causes the failure of oxidative capacity which results in overproduction of reactive oxygen species. Since the past, many kinds of literature have been documented giving us the data of regulators involved in fusion and fission. The mitochondrial fusion process is controlled by three GTPase, these are mitofusin 1 and 2 and optic atrophy1 [23]. The outer membrane of mitochondria holds Mitofusin 1 and Mitofusin 2, while the inner one holds OPA 1. While on the other hand fission is regulated by two GTPase genes, FIS 1 (on the outer membrane of mitochondria), and Drp 1(on outer membrane and cytosol). The fusion process works by intermixing of mitochondrial content and maintaining the electrical conductivity [24]. When normal functioning of mitochondria is disturbed by diminishing fusion or fission process which results in increased generation of reactive species, the enzyme activities alter in mitochondria, decreased in calcium balance (homeostasis), inhibition of production of ATP and low energy metabolism. The studies earlier have proved that changes occur in mitochondria due to increasing metabolic and neurodegenerative disorders [25].
Oxidative Damage to Mitochondria Triggering Its Dysfunction
The imbalance between two antagonistic forces is referred to as oxidative stress which causes the production of ROS and minimizes antioxidants. It is also a well-known fact that the damaging effect of reactive oxygen species is more as compare to compensatory. Mitochondrial dysfunction is a series of events that occur in mitochondria which involve dysfunction in mitochondrial biogenesis, changes produced in the membrane potential, and the decrease in size, number, and oxidative proteins of mitochondria [26]. In the body, it is a routine process of generating reactive oxygen species by oxygen metabolism in which mitochondria have the lead role in generating these reactive species [12]. These reactive species when interacting with other cellular components like DNA, protein, lipids, etc. in the OXPHOS process result in mitochondrial dysfunction [27]. Metabolic syndrome involves many diseases such as hypertension, obesity, hyper-dyslipidemia, and others. Changes in mitochondrial functions increase the risk of diseases like diabetes, obesity, dyslipidemia, and cardiovascular diseases. The abnormal cell metabolism causes the irregular generation of energy and its consumption, which are the main cause of metabolic syndromes [28]. Morphological changes occur due to enhanced glucose levels and increased reactive species [29]. When the signaling pathway of insulin is inhibited it causes the accumulation of fatty acids and lipids which can also be the reason for metabolic syndrome [30]. The following data, mentioned in Fig. 3.3, give us a detailed discussion about the connection between metabolic disorders and mitochondrial dysfunction.
Mitochondrial Involvement in Obesity
Presently, obesity has a strong impact on our society and is a major health issue worldwide. It is the main health issue created due to metabolic syndrome and also linked with other risk factors associated with other diseases. There are many factors that involve in generating obesity such as environmental and genetic factors. Mitochondrial dysfunction is also the cause of obesity. As explained from studies the NADPH oxidase and anti-oxidative enzymes in obese mice have declined due to increased release of reactive oxygen species in adipose tissues [31]. Interestingly, it has also been documented that abdominal obesity is generated by mitochondrial dysfunction such as in rodents and humans [32]. The gene expression is also reduced in an obese person. So, the obesity can be linked with gene expression of mitofusin 2 lost in skeletal muscle, the mitochondrial dysfunction starts in the tissue [33].
Mitochondrial Involvement in Insulin Resistance
When the level of insulin attains lesser response by cells, the condition is termed as insulin resistance. There are many factors that contribute to insulin resistance which include increased age, decreased physical exercise, obesity, and tension. So, it can say that oxidative stress in mitochondria may be the reason for insulin resistance [1]. Though it is still not confirmed that metabolic diseases such as insulin are caused by mitochondrial alterations or disorder, many studies have documented this fact that alteration in mitochondrial number and morphology cause to generate insulin resistance in skeletal muscle [34]. When glucose level increases from its demand the reactive species of oxygen also increases which causes mitochondrial alterations [29]. Similarly, when insulin signaling pathways inhibited, it causes accumulation of fatty acids and lipids which results in the generation of metabolic syndrome [30]. In various studies, mitochondrial metabolism markers have altered in the person who is insulin resistant. From the data, it is found that mitochondrial changes in skeletal muscle cause the increase in deposition of lipids and develop insulin resistance. It is also a well-known fact that lesser fatty acid oxidation results in stopping insulin signaling which leads to free fatty acid and insulin resistance and also decreases oxidation and ATP production in these individuals [29]. However, advance researches are needed to describe the mitochondrial function and insulin sensitivity via the antioxidant pathway.
Mitochondrial Involvement in Diabetes
Since the past, there is an increased incidence of type 2 diabetes and this number has become a major problem worldwide. Now diabetes increases up to 382 million individuals and this number is increasing rapidly. Many factors are involved in diabetes but still, the main reason is not clear. Myocytes, adipocytes, and hepatocytes are the insulin-sensitive cells when get resistant they are called insulin resistant along with that abnormal functioning of pancreatic cells is also the main factor that contributes to insulin resistance. Now, recent studies have proved that the involvement of mitochondrial abnormal functioning causes an excess of reactive species which induce diabetes [29]. T2DM is the outcome of lesser tissue sensitivity and secretion of insulin [35, 36]. recent study was done on diabetic and obese patients showed decreased glucose production and impaired lipid homeostasis in skeletal muscle [35]. In obese persons, the fat mass causes low glucose transport, stops insulin to perform its action, and increases FFA and others [37]. The hyperglycemic condition develops when the glucose level rises from its range and insulin sensitivity decreases [38]. In a diabetic person, at cellular level mitochondrial respiration and its density decrease which also decreases the energy production in the form of ATP and mRNA. Insulin resistance and type 2 diabetic patients at the cellular level have reduced mitochondrial respiration, ATP production and mitochondrial density and mRNA [39]. Oxidative stress always increases with the intake of the high-calorie diet which causes OXPHOS to increase its enzyme protein expression. In the brain, the increase in reactive oxygen species in the OXPHOS process is the major cause of oxidative damage of mtDNA [40]. When the insulin signaling pathway is inhibited by an excess of reactive species and also interferes with acetyl CoA to being oxidized in obese and diabetic persons results in increased lipid and diacylglycerol [1]. In diabetic and obese conditions, mitochondrial synthesis has impaired [35]. PGC-1α also involved in the generation of mitochondria [41]. In addition, mitochondrial dysfunction may be the target of therapeutic measures to treat diseases such as obesity and diabetes.
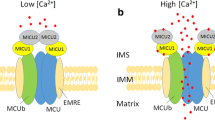
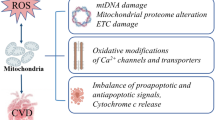
Mitochondrial Involvement in Cardiovascular Complications
Heart diseases are also a major issue around the globe. There are many factors which are involved in cardiovascular diseases, these are an environmental and genetic factor. From studies, it is confirmed that oxidative stress is directly proportional to an increased number of mtDNA. The heart can generate many reactive species in the heart cells including cardiac myocytes, endothelial cells, and neutrophils. There are many in vivo and in vitro researches available that documented that oxidative stress has a high impact on reducing reactive species in the cells [6]. The reactive species in the heart are generated when ETC complexes I and III get disrupted [42]. In accordance with this, other mechanisms are also involved in damaging heart tissues by producing reactive oxygen species, these are NADPH oxidase, xanthine oxidoreductase, or NOS. The increased reactive oxygen species decreases the antioxidant capacity of cell and causes cell injury which results in an alteration in gene expression, damaging mtDNA and abnormality in the functioning of endothelial cells [6], this results in failing heart muscle called myocardium [43]. Additionally, reactive oxygen species activate contractile functions, activate enzymes and transcription factors. Thus, the reactive oxygen species could be involved in cardiovascular diseases.
Mitochondrial Involvement in Stroke
Stroke is the main cause of death in developing countries. There are many factors that induce a stroke. They may be economical, physiological, or others. Among these, oxidative stress is also the contributing factor which causes a stroke by tissue injury [44], this oxidative stress then evolves abnormality in mitochondria, so mitochondrial dysfunction is also indirectly the cause of brain stroke. As the mitochondrial disorder causes decreased supply of oxygen and glucose to the tissues, it decreases the production of ATP and also the pathway of cell death change [45]. There are a series of experimentation done on the stroke model, to generate a stroke model the oxygen supply of the stroke model is stopped and also the glucose source is terminated which results in decreased oxidative metabolism. There are series of events generated in a nutrient-deprived stroke model which causes high storage of reduced material and accumulation of reactive oxygen species [44]. The tissue damage starts in the form of necrosis and apoptosis when the heart muscle gets focal ischemia due to oxidative stress [46, 47]. Thus, peroxynitrite radical is the causative agent of brain stroke. Thus it is proved that in the ischemic brain, oxidative metabolism is the result of the overproduction of reactive species brain [45].
Concluding Remarks
Mitochondria, the membranous organelle is involved in cell death and survival [47]. The main functions of mitochondria include the production of energy. Also, it hosts many cellular functions including metabolism of energy, generation of reactive species, and Ca2+ homeostasis along with cell integrity. Alteration in the morphology and function of mitochondria produces metabolic disorders in humans. Mitochondrial dysfunctions in metabolic syndrome that were reported in recent studies were impaired dynamics of mitochondria, deformity of synthesis of mitochondria, abnormal functioning of mitochondria, and production of reactive oxygen species. Furthermore, the researchers showed that maintaining mitochondrial dynamics and functions is mandatory to treat metabolic diseases. If we want to slow down the progression of metabolic disease, many interventions and approaches are helpful to make life better. These include lifestyle intervention, pharmaceutical plans to treat the patient in better ways, and mitochondrial-targeted molecules for the treatment of patients. However, the link between metabolic syndrome and mitochondrial function has not been fully elucidated. Similarly, genetics and its susceptibility with metabolic syndromes and the role of epigenetics are unclear. Additionally, the treatments related to metabolic syndromes are not so beneficial as the body physiology varies from population to population.
Conflict of Interest
Nothing to declare.
References
Kim JA, Wei Y, Sowers JR. Role of mitochondrial dysfunction in insulin resistance. Circ Res. 2008;102:401–14.
Halliwell B, Gutteridge JMC. Free radicals in biology and medicine. 4th ed. Oxford: Oxford University Press; 2007.
Chistiakov DA, Sobenin IA, Revin VV, Orekhov AN, Bobryshev YV. Mitochondrial aging and age-related dysfunction of mitochondria. Biomed Res Int. 2014;2014:238463.
Halliwell B. Reactive species and antioxidants. Redox biology is a fundamental theme of aerobic life. Plant Physiol. 2006;141:312–22.
Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens. 2000;18:655–73.
Schwarz PE, Reimann M, Li J, Bergmann A, Licinio J, Wong ML, Bornstein SR. The metabolic syndrome - a global challenge for prevention. Horm Metab Res. 2007;39:777–80.
Pollex RL, Hegele RA. Genetic determinants of the metabolic syndrome. Nat Clin Pract Cardiovasc Med. 2006;3:482–9.
Reddy PH, Reddy TP, Manczak M, Calkins MJ, Shirendeb U, Mao P. Dynaminrelated protein 1 and mitochondrial fragmentation in neurodegenerative diseases. Brain Res Rev. 2011;67:103–18.
Chen XJ, Butow RA. The organization and inheritance of the mitochondrial genome. Nat Rev Genet. 2005;6:815–25.
Sherratt HS. Mitochondria: structure and function. Rev Neurol. 1991;147(6–7):417–30.
Andreyev AY, Kushnareva YE, Starkov AA. Mitochondrial metabolism of reactive oxygen species. Biochem Biokhimiia. 2005;70:200–14.
Murphy MP. How mitochondria produce reactive oxygen species. Biochem J. 2009;417:1–13.
Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006;160:1–40.
Canto C, Auwerx J. PGC-1alpha, SIRT1 and AMPK, an energy sensing network that controls energy expenditure. Curr Opin Lipidol. 2009;20:98–105.
Reddy PH. Mitochondrial oxidative damage in aging and Alzheimer’s disease: implications for mitochondrially targeted antioxidant therapeutics. J Biomed Biotechnol. 2006;2006:31372.
Ventura-Clapier R, Garnier A, Veksler V. Transcriptional control of mitochondrial biogenesis: the central role of PGC-1alpha. Cardiovasc Res. 2008;79:208–17.
Virbasius JV, Scarpulla RC. Activation of the human mitochondrial transcription factor A gene by nuclear respiratory factors: a potential regulatory link between nuclear and mitochondrial gene expression in organelle biogenesis. Proc Natl Acad Sci U S A. 1994;91:1309–13.
Reznick RM, Shulman GI. The role of AMP-activated protein kinase in mitochondrial biogenesis. J Physiol. 2006;574:33–9.
Hales KG. The machinery of mitochondrial fusion, division, and distribution, and emerging connections to apoptosis. Mitochondrion. 2004;4:285–308.
Shaw JM, Nunnari J. Mitochondrial dynamics and division in budding yeast. Trends Cell Biol. 2002;12:178–84.
Ding WX, Yin XM. Mitophagy: mechanisms, pathophysiological roles, and analysis. Biol Chem. 2012;393:547–64.
Wai T, Langer T. Mitochondrial dynamics and metabolic regulation. Trends Endocrinol. Metab. 2016;27:105–17.
Cipolat S, Martins de Brito O, Dal Zilio B, Scorrano L. OPA1 requires mitofusin 1 to promote mitochondrial fusion. Proc Natl Acad Sci U S A. 2004;101:15927–32.
Twig G, Hyde B, Shirihai OS. Mitochondrial fusion, fission and autophagy as a quality control axis: the bioenergetic view. Biochim Biophys Acta. 2008;1777:1092–7.
Reddy PH, Tripathi R, Troung Q, Tirumala K, Reddy TP, Anekonda V, Shirendeb UP, Calkins MJ, Reddy AP, Mao P, Manczak M. Abnormal mitochondrial dynamics and synaptic degeneration as early events in Alzheimer’s disease: implications to mitochondria-targeted antioxidant therapeutics. Biochim Biophys Acta. 2012;1822:639–49.
Pieczenik SR, Neustadt J. Mitochondrial dysfunction and molecular pathways of disease. Exp Mol Pathol. 2007;83:84–92.
Harper ME, Bevilacqua L, Hagopian K, Weindruch R, Ramsey JJ. Ageing, oxidative stress, and mitochondrial uncoupling. Acta Physiol Scand. 2004;182:321–31.
Gastaldi G, Giacobino JP, Ruiz J. Metabolic syndrome, a mitochondrial disease? Rev Med. 2008;4:1387–8.
Kowaltowski AJ, de Souza-Pinto NC, Castilho RF, Vercesi AE. Mitochondria and reactive oxygen species. Free Radic Biol Med. 2009;47:333–43.
Choksi KB, Boylston WH, Rabek JP, Widger WR, Papaconstantinou J. Oxidatively damaged proteins of heart mitochondrial electron transport complexes. Biochim Biophys Acta. 2004;1688:95–101.
Woo C-Y, Jang JE, Lee SE, Koh EH, Lee K-U. Mitochondrial dysfunction in adipocytes as a primary cause of adipose tissue inflammation. Diabetes Metab J. 2019;43(3):247–56.
Zhang E, Al-Amily IM, Mohammed S, Luan C, Asplund O, Ahmed M, Ye Y, Ben-Hail D, Soni A, Vishnu N, Bompada P, De Marinis Y, Groop L, Shoshan-Barmatz V, Renström E, Wollheim CB, Salehi A. Preserving insulin secretion in diabetes by inhibiting VDAC1 overexpression and surface translocation in β cells. Cell Metab. 2019;29:64–77. https://doi.org/10.1016/j.cmet.2018.09.008.
Sparks LM, Xie H, Koza RA, Mynatt R, Hulver MW, Bray GA, Smith SR. A highfat diet coordinately downregulates genes required for mitochondrial oxidative phosphorylation in skeletal muscle. Diabetes. 2005;54:1926–33.
Ashrafian H, Frenneaux MP, Opie LH. Metabolic mechanisms in heart failure. Circulation. 2007;116:434–48.
Ajayi EIO, Molehin OR, Oloyede OI, Kumar V, Amara VR, Kaur J, Karpe P, Tikoo K. Liver mitochondrial membrane permeability modulation in insulin-resistant, uninephrectomised male rats by Clerodendrum volubile P. Beauv and Manihot esculenta Crantz. Clin Phytosci. 2019;5:31. https://doi.org/10.1186/s40816-019-0124-0.
Sergi D, Naumovski N, Heilbronn LK, Abeywardena M, O’Callaghan N, Lionetti L, Luscombe-Marsh N. Mitochondrial (Dys)function and insulin resistance: from pathophysiological molecular mechanisms to the impact of diet. Front Physiol. 2019;10:532. https://doi.org/10.3389/fphys.2019.00532.
Sung HK, Song E, Jahng JWS, Pantopoulos K, Sweeney G. Iron induces insulin resistance in cardiomyocytes via regulation of oxidative stress. Sci Rep. 2019;9:4668. https://doi.org/10.1038/s41598-019-41111-6.
Irving BA, Nair KS. Aging and diabetes: mitochondrial dysfunction. Curr Diab Rep. 2007;7:249–51.
Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A. 2003;100:8466–71.
Corral-Debrinski M, Horton T, Lott MT, Shoffner JM, Beal MF, Wallace DC. Mitochondrial DNA deletions in human brain: regional variability and increase with advanced age. Nat Genet. 1992;2:324–9.
Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999;98:115–24.
Brown GC, Borutaite V. There is no evidence that mitochondria are the main source of reactive oxygen species in mammalian cells. Mitochondrion. 2012;12:1–4.
Rigotto G, Basso E. Mitochondrial dysfunctions: a thread sewing together alzheimer’s disease, diabetes, and obesity. Oxid. Med. Cell. Longev. 2019;2019:7210892. https://doi.org/10.1155/2019/7210892.
Wardelmann K, Blümel S, Rath M, Alfine E, Chudoba C, Schell M, Cai W, Hauffe R, Warnke K, Flore T, Ritter K, Weiß J, Kahn CR, Kleinridders A. Insulin action in the brain regulates mitochondrial stress responses and reduces diet-induced weight gain. Molecular Metabolism. 2019;21:68–81.
Zhang J, Bao Y, Zheng L, Zhou X. Polycystic ovary syndrome and mitochondrial dysfunction. Reprod Biol Endocrinol. 2019;17:67. https://doi.org/10.1186/s12958-019-0509-4.
Mehta SL, Manhas N, Raghubir R. Molecular targets in cerebral ischemia for developing novel therapeutics. Brain Res Rev. 2007;54:34–66.
Dallner G, Sindelar PJ. Regulation of ubiquinone metabolism. Free Radic Biol Med. 2000;29(3–4):285–94.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Murtaza, G., Tariq, M., Shawahna, R. (2021). Mitochondrial Dysfunction in Metabolic Disorders. In: Akash, M.S.H., Rehman, K., Hashmi, M.Z. (eds) Endocrine Disrupting Chemicals-induced Metabolic Disorders and Treatment Strategies. Emerging Contaminants and Associated Treatment Technologies. Springer, Cham. https://doi.org/10.1007/978-3-030-45923-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-45923-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45922-2
Online ISBN: 978-3-030-45923-9
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)