Abstract
Insomnia is the most frequently reported sleep disorder and may manifest as early morning awakening, or difficulty falling asleep or staying asleep. While preliminary data exist regarding the use of meditation-based interventions for individuals suffering from chronic sleep disturbances, data on standardized treatment models using yoga and meditation interventions together in an integrated and evidence-based manner are rather lacking. The Yoga and Mindfulness Based Cognitive Therapy for Insomnia (Y-MBCTi) model integrates the cognitive-behavioral treatments for insomnia with the principles and practices of standardized yoga and mindfulness meditation in a customized manner. Healthcare professionals can use this model in their routine clinical practice to address the sleep-related problems of their patients in a targeted, time-limited, and standardized way. With a case series consisting of data from four chronic insomnia sufferers, we discuss the utility of the Y-MBCTi, which can be used alone or in combination with other evidence-based approaches like hypnotic medications and agents used to treat sleep conditions such as excessive sleepiness.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Insomnia is characterized by subjective dissatisfaction with one’s quantity or quality of sleep. It is the most frequently reported sleep disorder and may manifest as early morning awakening, or difficulty falling asleep or staying asleep. Approximately 10–15% of the adult population suffers from insomnia, which can have significant negative consequences if left untreated [1]. Prevalence of insomnia increases with age and may be primary or secondary to other conditions. Insomnia costs the US economy 63 billion dollars per year [2]. A study involving more than 10,000 working adults revealed that more than 20% of them had experienced periods of insomnia that lasted over a year [3]. Furthermore, inadequate or nonrestorative sleep is associated with a variety of medical, psychiatric, or cognitive complications in both adolescents and adults [4, 5]. Patients with sleep-related problems often do not verbalize their struggles with insomnia or seek professional help for these problems. For example, the incidence of insomnia in the primary care setting can be as high as 69%, but only one-third of patients discuss their sleep problem with their physician [6]. Hypnotic medications are frequently used to treat insomnia, but some patients prefer nondrug approaches to avoid tolerance and dependence [7].
Mindfulness-based approaches have emerged as novel strategies for stress reduction and emotion regulation, among other health benefits. Although preliminary work has been conducted on using meditation-based interventions for individuals suffering from chronic sleep disturbances, data on standardized treatment models using yoga and meditation interventions together in an integrated and evidence-based manner are rather lacking. In this chapter, we provide an overview of the science behind sleep and insomnia and describe how a standardized approach using yoga and mindfulness-based cognitive therapy (Y-MBCT) can address these issues. This model can be used by healthcare professionals in their routine clinical practice to address their patients’ sleep-related problems in a targeted, time-limited, and customized way. We discuss the utility of the Yoga and Mindfulness Based Cognitive Therapy for Insomnia (Y-MBCTi), a proof of concept model backed by preliminary data that can be used alone or in combination with other evidence-based approaches, including medications for insomnia and related conditions such as excessive sleepiness or parasomnias (strange phenomena happening during sleep).
Approach to Assess Insomnia
The diathesis-stress model [8], more commonly known as the “3-P” model (predisposing, precipitating, and perpetuating factors), is quite relevant to assess the factors that contribute to the development and maintenance of insomnia. Of note, the 3-P model applies equally well to a wide variety of psychological-behavioral conditions besides insomnia.
In evaluating insomnia, there are several factors one must take into consideration. A central task is to determine whether the insomnia is a process-C (circadian) condition or process-S (related to homeostasis) condition. These are independent mechanisms and need to be assessed separately in each patient suffering from sleep problems because treating a Process-C-based insomnia as a Process-S -based insomnia can result in treatment failure. In the Process-S, the likelihood of falling into nonrapid eye movement (NREM) sleep is increased by the amount of time previously spent awake and thus promotes sleep. The Process-C tends to offset the Process-S so that we do not go to sleep until we are ready (i.e., it follows a circadian arousal process that promotes alertness). The Horne Ostberg questionnaire can be used to determine whether the sleep complaints are circadian rhythm-based (morningness-eveningness) [9].
Another task is to determine whether it is a rapid eye movement (REM) stage or non-REM (NREM) problem. REM sleep is essentially independent of Process S and Process C. It is important to have a basic understanding of these two types of sleep to help determine the correct diagnosis and, subsequently, implement effective treatment interventions. These have been already explained in Chap. 1 of this book.
The differential diagnosis of insomnia can be systematically assessed by examining six domains as described later:
-
(a)
Is any medical condition(s) causing the insomnia?
-
(b)
Is any psychiatric condition(s) causing the insomnia?
-
(c)
Is any substance abuse causing the insomnia?
-
(d)
Is the insomnia circadian rhythm Process-C based?
-
(e)
Are there associated parasomnias or movement disorders such as restless leg syndrome (RLS) or periodic limb movement disorder (PLMD)?
-
(f)
Finally, if (a) to (e) are negative, then the possibility of primary insomnia should be entertained and referral to a sleep disorder center should be made.
Role of Yoga and Mindfulness Interventions in Insomnia
Insomnia is one of many areas in which a mindfulness-based approach appears to be particularly suitable. Emerging evidence predominantly from the adult population suggests that mindfulness-based interventions (MBIs) can be effective in the treatment of insomnia. In practice, MBIs are often combined with other therapeutic approaches. For example, mindfulness-based stress reduction (MBSR; [10]) is a widely used structured group program to reduce stress and improve self-regulation. Similarly, mindfulness-based cognitive therapy (MBCT) merges mindfulness with cognitive-behavioral therapy (CBT) and thus typically includes mindfulness meditation in addition to sleep restriction, stimulus control, sleep education, and sleep hygiene. A few studies have examined the effects of mindfulness-based stress reduction (MBSR) , mindfulness-based therapy for insomnia (MBT-I), and the addition of mindfulness as a component in a multimodal approach [1, 11]. Our group conducted a meta-analysis of the relevant studies [12] with the purpose of assessing the effects of mindfulness interventions (MBIs) on sleep disturbance in the general population. This meta-analysis examined 16 pertinent studies that enrolled a total of 575 individuals from 8 to 87 years of age. In all, 82.1% of participants were female (472 out of 575 participants). The outcome measures of sleep were total sleep time (TST; the number of minutes that the individual actually slept during one night); sleep onset latency (SOL; minutes taken by the individual from the bed time until falling asleep); sleep efficiency (SE; time slept divided by the total time spent in bed); and wake after sleep onset (WASO; the number of minutes spent awake after initially falling asleep). Sleep measurements were evaluated before and after MBIs, using both subjective and objective methods. In the majority of studies, these sleep parameters were calculated on the basis of self-reported sleep logs (i.e., subjective measurements). We found MBIs to be associated with a large increase in sleep efficiency (SE; effect size = 0.88; p < 0.0001) and a medium increase in total sleep time (TST; ES = 0.47; p = 0.003) as assessed by sleep logs. In addition, wake after sleep onset and sleep onset latency also showed medium to large decreases (WASO: ES = −0.84, p < 0.0001; SOL: ES = −0.55, p < 0.00001). Changes in sleep when measured by polysomnography and actigraphy, however, were not statistically significant. In this meta-analysis, the sleep improvements as assessed by sleep logs continued 2–6 months following the treatment initiation. Although interpretation is limited by the subjective nature of the assessment tool and the small number of studies on MBIs for insomnia, especially in adolescent populations, these results suggest that mindfulness-based interventions can improve sleep.
It is important to note that yoga and meditation interventions are heterogeneous, involve many different components, and often are not used in a standardized manner [13]. There are many distorted views surrounding yoga and meditation, with a lack of clarity as to what these terms mean in actual day-to-day practice. In addition, their use is often carried out in nontargeted ways. For example, yoga is largely understood as a physical or postural technique, while meditation is seen as a breathing technique. This kind of dichotomous view and fragmented use of yoga and meditation restrict their scope and their utility. It not only prevents the integration of body and mind, but also poses significant challenges in research when evaluating the comparative efficacy of yoga or meditation interventions across different studies. Yoga and meditation interventions are more effective when used in combined, synergistic, and targeted ways [14]. Such a holistic and integrated approach is in accordance with the ancient Indian scheme of the Eight-limbed Yoga of Patanjali (Sanskrit: Astanga yoga) [15], or the Noble Eightfold Path of the Buddha (Pali: Atthangika Magga [16]) as they were proposed originally. In fact, literature [17, 18] suggests that the integrated use of the varying aspects of yoga is more effective than the use of specific components in isolation. As discussed earlier, MBIs have shown promising effects for the treatment of insomnia across a limited number of predominantly uncontrolled studies. However, data on standardized treatment models using both yoga and meditation interventions together in an integrated and evidenced manner are rather lacking. The Y-MBCTi model integrates the cognitive-behavioral treatments for insomnia with the principles and practices of standardized yoga and mindfulness meditation interventions in a customized manner. The translational format of the Y-MBCTi model is based on the psychobiology of sleep physiology and pathologies. It combines this information with not only standardized and evidence-based meditation protocols, but also yoga interventions and behavioral therapy modules so that the multiple components can be used in an integrated and customized manner.
The Components of the Y-MBCTi Model
Y-MBCT i model is targeted, time-limited (8–10 sessions) and translational in nature (3 T’s). It is targeted because it targets insomnia from biopsychosocial perspectives using subjective and objective approaches. It is time-limited because over 8–10 sessions it involves administration of a standardized protocol to treat insomnia. It is translational in nature because it integrates the basic science behind sleep physiology and pathology with the five cognitive-behavioral therapy modules as well as with the principles and practices of standardized yoga and meditation interventions in a way tailored to the individual patient.
Goal of Y-MBCTi
The translational format of the Y-MBCTi model is backed by basic research on the psychobiology of sleep and related pathologies. It combines these insights with evidence-based meditation protocols, both yoga interventions and behavioral therapy modules, so that these heterogenous approaches can be used in an integrated and personalized manner. The goal of the Y-MBCTi model is to help the afflicted individuals increase their awareness of the mental and physical states that develop with chronic insomnia and to develop adaptive ways of working with these undesirable states. In this model, meditation exercises are used to help the patient monitor the mental and physical states associated with their chronic insomnia without reacting to them in an overwhelmed way. Discussion takes place between the patient and the treatment provider about how to create this mindful state in a customized way and how to apply it to problematic situations that may arise in one’s daily life as a result of insomnia.
The mindful state (described later) is systematically developed in the individual and characterized by alertness, calmness, and a nonreactive stance. In particular, attention is brought to the mental and physical states of sleepiness and fatigue as participants are taught to discern these two states. The cognitive–behavioral therapies (CBT) embedded in the Y-MBCTi model include a focus on reducing unwanted wakefulness at night, decreasing the ruminations and anticipatory anxiety (catastrophization) related to the impact of insomnia on the individual’s life, and effectively managing the emotional reactions to the sleep disturbances and daytime fatigue.
Components of Y-MBCTi
The Y-MBCTi model involves a broad array of many psychotherapeutic components that can be categorized under two main therapeutic approaches:
-
(a)
Standardized yoga and meditation protocols (discussed later)
-
(b)
Cognitive-behavioral therapies (CBT)
The CBT portions are divided into five main components (detailed later):
-
(i)
Sleep restriction
-
(ii)
Stimulus control
-
(iii)
Behavioral activation
-
(iv)
Behavioral experiments
-
(v)
Mindfulness-based graded exposure therapy (MB-GET, [18, 19])
The yoga and meditation modules consist of an initial sleep assessment followed by the implementation of the standardized Y-MBCTi protocol. The sleep assessment includes:
-
(i)
Obtaining a thorough history using the 3-P model
-
(ii)
Administration of the assessment scales: the Insomnia Severity Index scale (ISI, [4]) and the Assessment Scale for Mindfulness Interventions (ASMI, [13, 19, 20])
-
(iii)
Assessment using biological measures (EEG, etc.) at different time intervals as outlined later in Fig. 4.1
The standardized Y-MBCTi protocol includes the following:
-
(a)
Training on the standardized yoga and meditation protocols: This is the first step in the Y-MBCTi protocol. This step helps the patient regain a state of mind (the mindful state) necessary to observe life stressors more neutrally or in a less reactive manner rather than being flooded by or habitually repeating them without control. The mindful state (which is simultaneously alert, calm, and detached/nonreactive), once attained, brings more focus and attentional reorientation. This shift enables the patient to engage in nonjudgmental self-observation of their thoughts, feelings, (unpleasant) memories, sensations, and impulses/behaviors (Buddha’s five factors model of human experience [13, 20]) instead of habitually indulging in them in a repetitive and emotionally charged manner.
-
(b)
The second step in the Y-MBCTi protocol involves conducting a behavior analysis (identifying antecedents, behaviors that are problematic, and consequences: the ABC paradigm) and training the patient on five components of CBT. This step is done only after generating the five-factor inventory of the insomnia experience which is similar to the thought records often used in CBT sessions (e.g., for the treatment of anxiety or depression). However, it is more all-encompassing (detailed in Pradhan et al. [19]). This step enables the provider to formulate a collaborative treatment plan targeted toward handling the sleep problem(s).
The five main components of the CBT intervention in Y-MBCTi are briefly described later:
-
1.
Sleep restriction [21] is an empirically supported treatment for insomnia that complements the mindfulness principles. It involves regulating sleep by setting a limited time in bed (e.g., 12:00 a.m. to 6:00 a.m.). By restricting the amount of time in bed, the individual avoids compensatory behaviors for sleep loss such as taking naps or staying in bed to catch more sleep. These compensatory behaviors can lead to a reduced homeostatic drive for sleep and thus perpetuate the sleep problem.
-
2.
Stimulus control [22] is another empirically supported treatment for insomnia that can work well in conjunction with the mindfulness techniques. Stimulus control involves associating the bed and bedroom with feeling sleepy. Activities like eating, doing work, or watching TV in bed are discouraged as it weakens this association. Patients should not go to bed until they feel sleepy and they should get out of bed if unable to sleep for a period of time. This concept is designed to help maximize the opportunity of falling asleep more easily.
-
3.
Behavioral activation : This is specifically targeted towards reducing daytime sleepiness, which may be a result of insomnia itself or it may be a by-product of the sleep restriction technique, especially during the early stages of its use.
-
4.
Behavioral experiments: The behavioral experiments are driven by basic data about the patient generated by the five-factor inventory of insomnia and the weekly activity schedule (illustrated below in Fig. 4.2). These experiments are aimed at challenging the dysfunctional thoughts (cognitive distortions) and behaviors related to insomnia and thus serve a crucial role in the Y-MBCTi protocol.
-
5.
Mindfulness-Based Graded Exposure Therapy (MB-GET [19, 20]). MB-GET is another CBT method used to reduce the significant amount of dread, catastrophizing, and anticipatory anxiety seen in patients with sleep problems, especially insomnia. MB-GET involves increasing awareness but decreasing reactivity to both sleep and insomnia-related symptoms and their precursors (antecedents). The act of consciously, purposefully, and calmly focusing on sleep problems, their antecedents, and consequences as done in MB-GET is truly a contemplative and responsive approach, rather than reactive. This set of techniques makes or tries to make symptoms more objective targets of reflection and neutral (detached) observation rather than an intolerable source of subjective anxiety, frustration, and dysphoria. The behavioral experiments and the MB-GET interventions often complement each other. As compared to the traditional exposure-based treatments that have been criticized for relative lack of patient engagement, the mindfulness component inherent in the MB-GET model promotes patient engagement with the exposure tasks, in addition to enhancing the efficacy and empowerment [23].
By combining these sleep-related behavioral change interventions with mindfulness meditation, participants are taught to make significant changes in the way they approach both sleeping and waking stress, and they master the ability to bring yoga and mindfulness into their daily lives.
The schematic presentation of the methodology of the Y-MBCTi model is depicted in Fig. 4.1.
Customizations in the Y-MBCTi
Assessment, treatment planning, and delivery of the interventions in the Y-MBCTi model are customized on the basis of the client’s scores on the following measures:
-
1.
Level of mindfulness : This is measured by the Assessment Scale for Mindfulness Interventions (ASMI; Pradhan [13]). This is a clinician-rated 18-item scale and measures the level of mindfulness in seven dimensions, including its practice. Scores range from 0 to 90 with higher scores indicating a higher level of mindfulness.
-
2.
Level of stress : This is measured by the Perceived Stress Scale (PSS) [24]. The PSS is a widely used 10-item self-administered scale that measures the degree to which the various situations in one’s life are appraised as stressful. Items were designed to explore how unpredictable, uncontrollable, and overloaded the clients find their lives. The scale also includes a number of direct queries about current levels of experienced stress. Scores range from 0 to 40 with higher scores indicating a higher level of stress. The items are easy to understand, and the response alternatives are simple to grasp.
-
3.
Insomnia Severity Index (ISI, [25]): This clinician-administered scale assesses the severity of both nighttime and daytime components of insomnia. It has seven questions and the total scores range from 0 to 28.
Interpretation of the total score categories ranges from no clinically significant insomnia (scores from 0 to 7), subthreshold insomnia (8–14), moderately severe clinical insomnia (15–21) to severe clinical insomnia (22–28). A positive “Treatment Response” on this scale is defined as a decrease in the ISI scores by at least 8 points; “Remission” is defined as ISI scores less than 8. In contrast, “Deterioration” is defined as an increase of ≥3 points in ISI scores [26, 27]. The aforementioned measures serve as guides for the implementation of the various components of this multimodal treatment model.
-
4.
The weekly activity schedule (see Fig. 4.2): This is a rather simple and easy-to-do behavioral module that serves as a primer of the behavioral structure that is to be used in an incremental manner by combining the desirable behaviors/activities with positive reinforcement strategies. This helps in establishing sleep-promoting behaviors and healthy coping mechanisms.
Achieving the Meditation Skills Before Implementing the CBT Interventions is the Key to Success in this Therapy
After the patient is systematically trained in the standardized yoga and meditation modules as demonstrated in Fig. 4.1, she or he is encouraged to focus more on the practice of meditation to achieve a mindful state, which in turn can be used to carry out the CBT interventions in a less emotionally charged and more organized manner. In the Y-MBCTi model, emphasis is placed on meditation skills as well as meditation practice because both are complementary to each other and necessary for applying this multicomponent model effectively. In the Y-MBCTi model, as the program progresses, participants are taught to use mindfulness principles and behavioral strategies when working through undesirable states. Using mindful awareness as a platform, participants are taught to respond to sleep disturbance with mindfulness skills and contemplation rather than react automatically by increasing their (often unsuccessful) efforts to rest. For example, awareness of internal cues (sleepiness rather than fatigue) along with a recognition of ineffective reactive tendencies (avoid fatigue by going to bed) is used to make changes in both the relationship to sleep and sleep-promoting behaviors.
General Instructions on Meditation for Clients Using the Y-MBCTi Model
If you are suffering from insomnia, research shows that you will likely benefit greatly from a regular mindfulness practice (at least 15–20 minutes daily) like this one [20]. A little bit each day (even 10 minutes) is better than one longer session once a week [13, 20]. A good habit is to practice meditation in bed upon rising in the morning and again in bed just before falling asleep. This routine helps you begin and end your days with mindfulness and constitutes an important step in cultivating the meditative lifestyle (i.e., the Buddha’s Middle Way) [24].
Instructions for Meditation
-
(i)
Find a place where you can sit still or stand or lie down undisturbed for 10–20 minutes: it is better to keep the spine erect during this practice. Please reduce any unwanted bodily movements by locking yourself into an easy posture (Sanskrit: asana). Allow yourself to settle, both mentally and physically.
-
(ii)
This is an attention practice rather than a physical practice: the primary task is to feel comfortable, breathe slowly from the belly with your mouth closed, and OBSERVE your breath. You should bring focus to the physical sensations associated with breathing (such as touch, hot/cold sensations) and the movements in your body while breathing. Take your time to make yourself as comfortable as possible so that your mind is not drawn too much toward bodily discomfort, if any. You can use any cushions, stools, or other props to ensure comfort. You may choose to close your eyes.
-
(iii)
If you’re feeling agitated, tense, or stressed, take a moment to tune into your body and notice any parts that may be tense (e.g., shoulders, face, jaw, chest). Use the STOPP module [19] to reduce any agitation. The STOPP module of mindfulness is Pradhan’s behavioral adaptation of the Middle Way philosophy of mindfulness traditions, which has been successfully applied in clinical situations within the age range of 6–80 years [19, 20]. STOPP is an acronym for Stress, Three (or Ten or Twenty or Thirty) meditative breaths, Observe, Practice and Progress. The STOPP module specifically helps to quickly de-escalate anger or hyperarousal symptoms as they arise spontaneously in daily life in response to triggers.
-
(iv)
Next, you will practice the “Three Point Sensate Focus” meditation [20], which is one of the cornerstones of the Y-MBCT i model. As the name suggests, you will use three physical aspects of meditation to keep your attention grounded on the breath and bodily sensations (“grounding the mind onto the body”). Examples include touch, sound, hot/cold sensations, beginning-middle and end of each in-breath and out-breath, or breath-associated movements. You can begin by taking the whole focus of your attention to the tip of the nostrils. Note the sensations of breath entering and leaving the body. You may note a slightly cool sensation as you inhale and a warmer sensation upon exhalation. Allow the sensation to completely absorb your attention. Stay with this practice for 3–5 minutes (about 15–20 standardized meditative breaths) during each practice session.
-
(v)
Next, follow the flow of the breath as it moves through the nostrils, down the throat and into the lungs (inhalation). Then back out the lungs through the throat and out the nostrils (exhalation). Allow the mind to follow the passage of the breath as it enters and leaves your body.
-
(vi)
Know that thoughts, feelings, or memories may drift through your mind. That’s perfectly normal. There is no need to resist them or try to push them away. No need to be concerned with the nature of any particular thought. Be a gentle, impartial (neutral) observer to any thoughts that may arise and label them as “just distractions.” Refocus on your breath and associated sensations or movements.
-
(vii)
Continue your meditation until you achieve the mindful state (concurrent alertness, relaxation, and detachment/nonreactivity to the ongoing stimuli). This may take 5-25 minutes.
-
(viii)
When you are ready to complete the practice, over three slow and deep belly breaths, bring your awareness back to your body by feeling the weight of your body against the chair, by registering any sound from your surroundings, and by recalling the room you’re sitting in. Begin to move and stretch your body and open the eyes. Feel free to sit peacefully and readjust to your surroundings before going about your day.
The Five-Step SPASM Method for Honing Meditation Skills
In addition to the instructions given previously, the SPASM method is used in the Y-MBCTi model to hone the meditation skills further in the practitioner. Details of the five steps in the SPASM method are as follows:
-
S: Sit Straight and Still, Slow down the breath rate
-
P: Pause momentarily after breathing out
-
A: Be Aware of the distractions but do nothing, just Accept/observe them and Acknowledge their presence
-
S: Refocus on the physical Sensations (such as breath sensations, sounds, etc.) rather than on the thoughts or other distractions
-
M: Middle Way: To decrease a striving and self-critical/perfectionist attitude during meditation practice, it is important to follow the Buddha’s Middle Way. This creates mindful awareness (e.g., a state of calmness, alertness, and detached/open monitoring of the objects in one’s awareness) that helps cultivate a “being” state of mind rather than a “doing” or “striving” state of mind [13]. Of note, unlike the striving/perfectionist attitude (which is an extreme style), the Middle Way is the path of moderation.
General Instructions on Sleep Hygiene for Clients Using the Y-MBCTi Model
Instructions on sleep hygiene include but are not limited to the following:
-
Keep the bedroom dark, noiseless and with a comfortable bed.
-
Keep the time that you go to bed and wake up fixed, in order to create a daily sleep routine. Use an alarm to do so. Contrary to popular belief, maintaining the same daily wake-up time is more important than maintaining the same bed time because circadian rhythm is more sensitive to the former.
-
Start your day with mindfulness practice and end your day with mindfulness practice, all in the bed. This is quite easily done by practicing 40–60 standardized meditative breaths using the “Three Point Sensate Focus” meditation protocol [20].
-
Avoid alcoholic drinks and stimulants (i.e., caffeinated beverages) for up to 4–6 hours before going to bed. Avoid heavy physical exercise within a 3-hour window of going to bed.
-
Remain in bed and meditate even if you’re not able to sleep. This prevents arousal states and also allows for conditioning the meditation to induce a sleepy state.
-
Try your best to avoid sleeping when you are not in bed. If you can’t help it, restrict the daytime nap to less than 30–45 minutes.
Results of the Y-MBCTi Model in Four Patients (Tables 4.1 and 4.2)
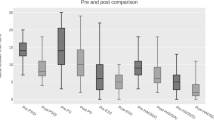
The methodology of this open label case series was adopted from our meta-analysis published earlier [12]. The outcome measures of sleep were total sleep time (TST; the number of minutes that the individual actually slept during one night); sleep onset latency (SOL; minutes taken by the individual from the bed time until falling asleep); sleep efficiency (SE; time slept divided by total time spent in bed); and wake after sleep onset (WASO; the number of minutes spent awake after initially falling asleep). These sleep outcome measures were calculated on the basis of self-reported sleep logs (subjective measurements).
As shown in Table 4.1, the mean age of participants was 44 years (SD = 17.26 years) and mean duration of insomnia was 8.25 years (SD = 2.06 years). The mean number of Y-MBCTi sessions was 9.5 (SD = 1.91).
The pre- and posttreatment data on efficacy of Y-MBCTi in these four patients are shown in Table 4.2. Posttreatment, all four patients improved not only on all sleep parameters (ISI, SE, SOL, TST, and WASO scores) but also in their level of mindfulness (as reflected in their ASMI scale scores).
Conclusion and Future Directions
When examining the neurophysiology and psychobiology of sleep and integrating it with the quintessential pragmatism of cognitive-behavioral therapy and self-empowering methods of yoga and mindfulness, the rationale for and utility of the Y-MBCTi model becomes more evident. This model can be used as a stand-alone therapy or in combination with sleep-promoting medications. Although the evidence presented here is preliminary, it does suggest that the Y-MBCTi model is feasible and has the potential to bridge some of the existing treatment gaps within the realm of therapy for sleep-related problems such as insomnia [28]. Moving forward, in our ongoing clinical research, we intend to study the efficacy of the Y-MBCTi model using a randomized control trial design in a large sample. We will also examine the potential utility of the multisystem real-time biofeedback parameters (consisting of real-time EEG, heart rate variability, and breath pattern analysis) to see if they can serve as biomarkers of treatment response.
References
Ong J, Sholtes D. A mindfulness-based approach to the treatment of insomnia. J Clin Psychol. 2010;66:1175–84.
Kessler R, Berglund PA, Coulouvrant C, Hajak G, Roth T, Shahly V, Shillington AC, Stephenson JJ, Walsh JK. Insomnia and the performance of US Workers: results from the America Insomnia Survey. Sleep. 2011;34:1161–71.
Siegfried J. The high cost of insomnia. 2018. Retrieved on 24 May 2019. Available from: https://www.healthguidance.org/entry/16599/1/the-high-cost-of-insomnia.html.
Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9.
Committee on Sleep Medicine and Research, Institute of Medicine. Sleep disorders and sleep deprivation: an unmet public health problem. Washington, DC: National Academies Press; 2006.
Yamashiro Y, Kryger MH. Nocturnal oximetry: is it a tool for sleep disorders? Sleep. 1995;18:167–71.
Morin C, Gaulier B, Barry T, Kowatch R. Patient’s acceptance of psychological and pharmacological therapies for insomnia. Sleep. 1992;15:302–5.
Spielman AJ, et al. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10:541–53.
Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110.
Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4:33–47.
Ong JC, Shapiro SL, Manber R. Mindfulness meditation and cognitive behavioral therapy for insomnia: a naturalistic 12-month follow-up. Explore. 2009;5:30–6.
Kanen J, Nazir R, Sedky K, Pradhan BK. The effects of mindfulness-based interventions for sleep disturbances: a meta-analysis. Adolesc Psychiatry. 2015;5(2):105–15.
Pradhan BK. Yoga and Mindfulness Based Cognitive Therapy (Y-MBCT): a clinical guide. Gewerbestrasse: Springer International Publishers; 2014.
Brown RP, Gerbarg PL. Sudarshan Kriya Yogic (SKY) breathing in the treatment of stress, anxiety, and depression: clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7.
Satchidananda S. The yoga sutras of Patanjali: translations and commentary. Yogaville: Integral Yoga Publications; 1978.
Nyanamoli B. The path of purification (Visuddhimagga). Kandy: Buddhist Publication Society; 1975.
Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front Psych. 2013;3:117.
Pradhan BK, Sharma A. The time has come for integrating complementary medicine into psychiatry. Adolesc Psychiatry. 2015;5:71–2.
Pradhan BK, Pinninti NR, Rathod S. Brief interventions for psychosis: a clinical compendium. Gewerbestrasse: Springer International Publishers; 2016.
Pradhan BK, Pinninti NR, Rathod SR. Chapter-3: Trauma Interventions using Mindfulness Based Extinction and Reconsolidation of memories (TIMBER). In: TIMBER psychotherapy: for PTSD, depression and traumatic psychosis. Gewerbestrasse: Springer International Publishers; 2019.
Spielman AJ, Sasky P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10:45–56.
Bootzin RR, Epstein D, Wood JM. Case studies in insomnia. In: Hauri PJ, editor. Stimulus control instructions. New York: Plenum; 1991. p. 19–28.
Strauss C, Rosten C, Hayward M, Lea L, Forrester E, Jones AM. Mindfulness-based exposure and response prevention for obsessive compulsive disorder: study protocol for a pilot randomized controlled trial. Trials. 2015;16:1–7.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–96.
Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8.
Wise EA. Methods for analyzing psychotherapy outcomes: a review of clinical significance, reliable change, and recommendations for future directions. J Pres Assess. 2004;82:50–9.
Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307.
Pradhan BK. Updates on sleep disorders. Lecture presented at: the American Psychiatric Association Annual Conference; 5–9 May 2018; New York City.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pradhan, B., Malik, S. (2020). Yoga and Mindfulness-Based Cognitive-Behavioral Therapy for Insomnia (Y-MBCTi). In: Sedky, K., Nazir, R., Bennett, D. (eds) Sleep Medicine and Mental Health. Springer, Cham. https://doi.org/10.1007/978-3-030-44447-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-44447-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44446-4
Online ISBN: 978-3-030-44447-1
eBook Packages: MedicineMedicine (R0)