Abstract
The use of noninvasive brain stimulation techniques (NIBS) has gathered substantial interest in the study of dementia, from the early detection of its pathophysiological course, up to its use in stimulating spared cognitive functions in elderly adults. In the present book chapter, we will provide a brief walkthrough on the most recent relevant findings on the use of transcranial electrical stimulation (tES) along the aging curve, from healthy to pathological states. We will consider how different stimulation approaches have been implemented to provide insight into the complex mechanisms of neurodegeneration and which have been the steps forward in trying to advantage the individual in respect of the pathology. In this regard, we will consider evidence from cognitive and motor stimulation, covering a broad spectrum of modalities used to prompt individual resilience to degeneration. Last, we will suggest future possible directions in the field of brain stimulation, considering the fast technological advancement that is bringing us the possibility to target multiple areas or networks at once, or to control for stimulation using predictive “closed-loop” algorithms tuning the electrical waveforms based on ongoing brain oscillations. Despite adjunctive studies being needed to clarify the underlying mechanisms of action of tES, promising results have been gathered that might directly impact patients and drive future advancement in the field.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Transcranial Electrical Stimulation
- Transcranial Direct Current Stimulation
- Transcranial Alternating Current Stimulation
- Dementia
- Aging
- Gamma Oscillations
- tACS
- tDCS
- Alzheimer’s Disease
- MCI
- Mild Cognitive Impairment
Modern societies are currently facing a rapid growth of their older adults’ population as a function of increased life expectancies and overall greater wellbeing. Consequently, fast therapeutic advances in the treatment of aging-related pathologies are also becoming necessary. Pharmacological interventions and cognitive stimulation approaches remain the leading standards in the field, despite being characterized by potentially serious side-effects and the necessity of longstanding commitment, respectively. In recent years, noninvasive brain stimulation (NIBS) has been proven useful in boosting cognitive and motor performances in healthy young adults, leading to the query of whether similar beneficial effects could be translated to older age individuals as well. Compared to young, older adults are known to undergo substantial structural and functional reorganizations of their brains, exacerbated in the presence of dementia, which are strongly influenced by genetic and environmental factors. Substantial differences in brain functioning are detected since the beginning of the aging curve as a matter of a progressive substantial decrease in gray matter volume and white matter tracts, as well as in a preponderant loss of hemispheric specificity (Hemispheric Asymmetry Reduction in Older Adults, HAROLD [1]) and a progressive more effortful cognitive processing, requiring greater frontal lobe involvement compared to younger individuals (Posterior to Anterior Shift in Aging, PASA [2]). Although cognitive decay accompanies normal aging, its progressive worsening can limit individuals’ independence, first resulting in a diagnosis of Mild Cognitive Impairment (MCI) and subsequently dementia. The most common forms of neurodegenerative diseases include Alzheimer’s Disease (AD) and Frontotemporal Dementia (FTD), followed by other conditions such as Parkinson’s Disease (PD) and Dementia with Lewy Bodies (DLB). Although each differs clinically, certain shared elements exist that make dementia an interesting target for transcranial electrical stimulation (tES). First of all, cortical atrophy generally starts in a limited region of the brain and progressively propagates toward the surrounding tissues. As an example, the entorhinal cortex is where AD is believed to start, followed by the hippocampi and temporal lobes, until when the whole neocortex becomes affected. PD, on the other hand, is characterized by loss of dopaminergic neurons starting in the substantia nigra and progressively involving frontostriatal pathways. This leads to a second important aspect, which is the presence of proteinopathy, meaning an excessive accumulation of—and failure to clear—altered proteins. Examples of such proteins include amyloid-β plaques, tau neurofibrillary tangles, and Lewy Bodies aggregates, whose combination and presence is shared across dementia’s types. As the protein cascade hypothesis is nowadays believed not to be the only mechanism contributing to neurodegeneration, substantial interest is directed toward the role of glial activation and neuroinflammation as new therapeutic targets [3]. A third and last element binding different forms of dementia seems to be the occurrence of cortical atrophy along defined pathways that mirror the topography of networks in the brain. In AD, a gradual disaggregation of the Default Mode Network (DMN) is observed along a posterior-ventral and anterior-dorsal gradient [4], which not only mirrors the pattern of decay reported by other clinical biomarkers (e.g., amyloidosis and hippocampal atrophy) [5], but also shows a significant correlation with the emergent symptomatology [4]. Concomitantly, greater Salience Network (SN) activity is observed [6], whereas the opposite pattern (decreased SN activity and enhanced DMN activity) characterizes FTD [3].
Each of the aforementioned features of dementia represents a critical target and an important starting point for therapeutic and rehabilitative strategies. tES is a useful tool in this direction, as its induced electrical field is less focal compared to that of other techniques, such as Transcranial Magnetic Stimulation (TMS), making it suitable for the targeting of broader cortical regions and brain networks. Moreover, recent results have demonstrated that its repeated application may be efficacious in increasing plasma levels of amyloid-β, which are lower in AD patients compared to healthy controls [7]. Brain stimulation interventions have therefore been developed with the intent to induce more young-like brain functional patterns or to reduce excessive cortical excitability seen in older patients. In doing so, tES has come particularly helpful as it can be used to facilitate depolarization (excitatory effect) or hyperpolarization (inhibitory effect) of the resting membrane potentials of neurons, therefore modulating neuronal firing. Compared to other NIBS techniques, such as TMS, tES is at a lower risk of inducing adverse events, such as epileptic seizures, which can arise in individuals with pathologically higher cortical excitability. Finally, devices are relatively flexible and allow stimulation to be carried out while comfortably at home or during sleep, easing the administration of intervention therapies (see Fig. 22.1). As more evidence is collected on the use of tES as a therapeutic tool in the aging population, the introduction of the concept of perturbation-based biomarkers is also foreseen. Altered response patterns to external perturbations might indeed highlight abnormal brain responses, which could in turn ease the discrimination between normal versus pathological functional decay. In this sense, the use of NIBS techniques may become fundamental to detect brain dysfunctions before cognitive symptoms become overt.
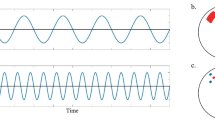
tES application modalities and measurable outcomes. (Left) Different electrode montages can be applied to deliver different current shapes. (Center) The versatility of tES protocols is shown, allowing stimulation to be carried out in various settings, such as before, during, or after cognitive-motor training or in resting-state scenarios, including sleep. (Right) Quantitative outcome measures, for which positive effects have been reported following tES, are listed
1 tES and Cognition
1.1 Healthy Aging
Functional rearrangements occurring along the aging curve progressively result in a reduction in hemispheres’ specialization (HAROLD model [1]), accompanied by a greater need of recruiting frontal regions to carry out a task at hand (PASA model [2]). Both models are at least partly believed to represent compensatory strategies by the brain, which might in turn represent the target of modulatory approaches by means of tES. As such, most stimulation protocols have been ideated either to (1) aid compensatory mechanisms (for example, stimulating frontal regions to boost their role in sustaining task execution) or by (2) contrasting functional shifts, trying to restore young-like cortical recruitment patterns (for example, inhibiting excessive frontal involvement or reducing the cortical hyperexcitability seen in old age). For instance, left and right anterior temporal lobe stimulation has been applied to improve proper names recall in young subjects and elderly adults. Greater improvement was seen when the truthful neural substrate was stimulated in the young group, whereas older adults benefitted more when the opposite (left) lobe was targeted [8], suggesting that stimulation of the nondominant hemisphere could aid compensatory mechanisms that are in action to support task’s request, with higher benefits for the aged group. By means of an opposite approach, semantic word generation was ameliorated in healthy older adults by inhibiting the excessive frontal hyperactivity, which in turn promoted the establishment of more young-like patterns of brain activity, as evidenced by resting-state functional Magnetic Resonance Imaging (rs-fMRI) [9]. Irrespective of the rationale behind the chosen stimulation, one important aspect reported in older adults’ studies concerns the timeframe needed to observe a significant effect. Indeed, especially in memory consolidation protocols, improvement in the recall of previously learnt information has been reported in the hours following, rather than concomitantly, the stimulation. As an example, older adults showed a less steep forgetting curve 1 week after a series of learning sessions where they received sham or anodal transcranial Direct Current Stimulation (a-tDCS), whereas learning rate was not affected [10], suggesting an offline effect on consolidation. Similarly, significant improvement in a free-recall task was observed in the 48 h following a-tDCS, with no substantial effect on immediate recall [11]. In a prior study, the same authors tested the effects of a-tDCS administered during a reminder session of a previously learnt list of words, resulting in a significant reduction in the forgetting rate from 3 to 30 days after [12]. Repeated stimulation sessions over multiple days combined with an active cognitive training (e.g., memory training) also induced beneficial effects up to 4 weeks following the end of stimulation, whereas immediate positive effects were detected only as a function of the cognitive training per se, with no contribution of a-tDCS [13]. Interestingly, transfer effects on cognitive functions outside the targeted one were detected, which equally persisted in the weeks following the stimulation [13]. On the other hand, no difference in the effects of sham tDCS or a-tDCS at 1 or 2 mA was reported on the performance at a visual n-back task assessed during and after 35 min from stimulation [14]. One possible interpretation suggested by the authors is that repeated sessions may be needed to induce significant cognitive effects in older participants. Furthermore, prior work has highlighted how tES effects on elderly adults might occur in the hours following stimulation, opposed to the immediate effects detectable in young individuals. Therefore, the timeline of stimulation and subsequent effects on cognition should always be carefully considered.
Finally, although memory and language impairments represent the most common complaints during aging, many other behaviors become affected that contribute in diminishing individuals’ autonomy in daily life. Few examples include difficulties in dual-task execution, planning, and decision making. As such, the possibility to intervene on those aspects could substantially improve later-life quality, for example for what concerns economic and monetary decisions. As an example, the left Dorsolateral Prefrontal Cortex (DLPFC) has been made a target to facilitate concurrent execution of different tasks, resulting in a significant reduction of the cognitive costs required by each task in the dual assignment condition, but not in a single task condition, also proving the specificity of the stimulation [15]. Further, a-tDCS applied over the right DLPFC significantly improved older adults’ error awareness, which was replicated in a separate experiment [16].
This preliminary yet promising evidence warrants future studies carefully designed to determine the extent to which noninvasive approaches are useful in offsetting, or at least delaying, age-related cognitive decline. These studies should consider customizing stimulation targets based upon individual or population characteristics, which often differ substantially across age groups. Prior studies reporting positive results following the stimulation of a given cortical target, for a given intensity and duration, with a given effect upon a cognitive measure of interest, might not necessarily translate into benefit for a demographically different population. As an example, a-tDCS over the right DLPFC with the cathodal electrode placed over the left DLPFC was successful in substantially decreasing gambling risks among young adults, whereas the identical montage led to a worsening of the same behavior in older adults [17, 18].
Second, even within the same demographic population, substantial differences in the effects of tES can be driven by interindividual differences in baseline cognitive performances. For example, individuals already disadvantaged, who show lower performances on a task, have been reported to benefit less from stimulation compared to their higher-level counterpart. One study proved how older subjects, who showed less lateralized spatial attention at baseline, were negatively affected in their performance following left posterior parietal cortex stimulation in respect to sham [19]. On the other hand, stimulation of the right homologous area had a positive effect in the higher-performing group [19]. Through a similar rationale, left and right DLPFC stimulation yielded better performances on a visual and verbal working memory task in highly educated older adults, whereas an opposite, detrimental effect was reported for the less educated group [20]. Those findings highlight the need to consider interindividual differences, which might explain diverse compensatory capacities in the recruitment of brain regions, in line with the notion of the impact of the Cognitive Reserve on individuals’ functional characterization [21].
1.2 Mild Cognitive Impairment
Mild Cognitive Impairment (MCI) represents an intermediate stage between healthy aging and dementia, characterized by a decrease in cognitive performance compared to a prior level of functioning, which is however not severe enough to affect the independence of the individual in the activities of daily living (ADL) [22]. MCI patients have a high epidemiological impact as they represent 7–24% of all individuals over the age of 65 [23], and 10–15% of older adults with MCI are diagnosed with dementia every year [24, 25]. To date, NIBS approaches have attempted to (1) identify those individuals with MCI who will worsen into dementia, so that early preventative measures can be taken, and (2) intervene against further cognitive decay in this population in order to maximize quality of life and minimize the risk of related disorders, such as depression and anxiety, which often arise from the acknowledgment of one’s own mental decline.
The identification of the ones, among those patients, for which MCI will just represent a transitory phase before a formal diagnosis of dementia, has been proven particularly difficult. Electrophysiological, neuroimaging, and neuropsychological approaches are routinely promoted in clinical practice to characterize structural and functional profiles of the individual [26, 27], but still represent expensive and unsure tools, with high levels of uncertainty especially for borderline patients [28, 29]. However, an important advancement in this direction has been made in recent years thanks to the characterization of brain oscillatory activity and its relationship with cognitive decline [30]. Indeed, altered oscillatory activity and decreased cognitive performances have been linked by prior studies [31], both of them being related to the accumulation of amyloid-β [32, 33], the main protein alteration seen in Alzheimer’s Disease (AD). In particular, the oscillatory activity might appear preserved in a resting condition and altered instead during task execution, with limits of the many biases that can affect task execution (instructions’ comprehension, tiredness, compliance, etc.) [30]. Nevertheless, tACS can be applied to induce brain oscillation passively, mimicking oscillatory patterns associated with cognitive processing [34,35,36]. Based on this rationale, the authors have therefore applied tACS at the gamma frequency band, which plays an important role in ensuring transmission across cortical regions and networks [37], and which prior studies have linked with cognitive processes in aging [38,39,40]. Interestingly, healthy old adults and most MCI patients positively responded to tACS, resulting in an increase in the gamma band as assessed both immediately and 1 hour after the end of stimulation [30]. Furthermore, the gamma after-effects significantly correlated with increased performance at several neuropsychological tasks, such as motor learning, verbal fluency, digit span, and attentive matrices [30]. On the other hand, no significant effect was observed in the AD population; at a 2-year follow-up, MCI patients who also failed to respond to stimulation had converted into AD [30]. One hypothesis is that the reduced capacity of tACS to modulate underlying oscillatory activity could represent an early detector of dysfunctional connectivity between DLPFC and the Dorsomedial Prefrontal Cortex (DMPFC) [30], i.e., sites where tACS was applied in the aforementioned study, thus providing a first evidence of the applicability of perturbation-based biomarkers to detect the presence of—and to monitor—brain diseases.
As for the possibility to actively improve cognitive performances, few other studies have been carried out in recent years showing promising results in this direction. In particular, 20–30 minutes of a-tDCS over the bilateral DLPFC have been successful in ameliorating subjective perceptions of cognitive functioning when compared to sham [41], as well as in improving memory strategies [41] and recall, both immediate and delayed, with beneficial effects persisting up to 1-month follow-up [42]. Interestingly, the combined use of neuroimaging techniques, such as positron emission tomography (PET) and rs-fMRI, has revealed tDCS-induced functional rearrangements, resulting in increased regional metabolism [41] of relevant areas and effective reduction of frontal hyperactivity [43], thus counteracting typical pathological functional shifts.
Apart from overt cognitive decay, other aspects of daily life become affected during the aging course, contributing to the core of dementia-related symptoms. Among those, sleep patterns are readily altered at the MCI stage [44]. In particular, slow-sleep oscillations and thalamocortical spindles play an important role in memory consolidation, such as that disruption of their temporal coupling is suggested to cause the early amnestic symptomatology [45] and to possibly contribute in the MCI to dementia conversion [46, 47]. Based on this rationale, slow-wave oscillations tDCS (so-tDCS) applied during daytime nap in a population of MCI patients was successful in targeting the coupling between slow oscillations and spindle activity, promoting their functional synchronization in the EEG spectra and amplifying both their power [44]. As a consequence, visual declarative memory also improved in the MCI patients [44].
Together, available studies of tES in healthy older adults and in those suffering from MCI have shown promise in targeting neural substrates responsible for age-related changes in cognition. Moreover, tES may be used to directly stimulate and improve the function of cortical regions responsible for a given behavior, or promote compensatory activity of surrounding neural substrates. Hyperactivity and over-recruitment of frontal areas are commonly reported in older adults and might represent compensatory strategies by the brain, which suppression may be desirable to reintroduce young-like patterns and better functional outputs [43].
Worth mentioning is also the feasibility of tailoring tES interventions based on the individual’s habits, enabling the administration of rehabilitative protocols in more ecological environments. Few studies have provided evidences regarding the combined use of tES and cognitive rehabilitation [48], as well as its noninvasiv use during well-established and routinely behaviors, like daytime naps [44] in the older adults. This approach may open the road for future interventions to be carried out directly at home, outside the laboratory environment.
1.3 Dementia
The use of tES is not limited to the quality enrichment of normal aging, or in the prevention of the MCI symptomatology, but rather it has proven useful at the level of dementia too, a disease stage characterized by substantial cortical atrophy and altered functionality that severely limits the independence of the individual in the activities of daily living. Due to the many facets of dementia’s pathological profile, it is not surprising that the mechanisms of action of tES have also been studied over multiple domains [49] (see Fig. 22.2). From its effects on the membrane potential, to the synaptic level, and up to the induced modulation of the brain oscillatory activity and functional connectivity, several studies have reported and commented upon the efficacy of tES [49]. At the level of mere neuronal excitability, alterations in the membrane potential result in abnormal profiles of hypo- versus hyperactivated cortical regions. With respect to AD pathology, the progressive accumulation of amyloid-β has been held responsible for this [50]. In particular, temporoparietal regions [51] have been observed to show slow-wave activity in contrast with the hyperexcitability of the motor cortex [52] and overall greater global cortical excitability [53], which has led to the rationale of applying a-tDCS to increase the activity of the former and cathodal tDCS (c-tDCS) to downregulate the latter. Rebalancing the underlying activity of cortical circuits appears crucial for the restoring of cognitive functioning in AD [54]. Nowadays, it is possible through the established role of tDCS modulating depolarization and hyperpolarization of the neural membranes [55]. Similarly, at synaptic level, the study of the effects of tES on dementia-related alterations has mainly focused on glutamatergic and GABAergic alterations, i.e., the main excitatory and inhibitory neurotransmitters of the brain. tDCS after-effects closely resemble long-term potentiation (LTP) and long-term depression (LTD) at the synaptic level [56], the former being considered responsible for learning and memory processes, which are altered in dementia. In animal models of AD, disruption of LTP was closely related to N-methyl-D-Aspartate (NMDA) receptors disruption in the hippocampus by the accumulation of amyloid-β [57]. Considering that tDCS LTP-like effects are also partly dependent on the NMDA receptors, its use in actively contrasting their disruption and in promoting cortical plasticity is therefore expected. In particular, glutamatergic alteration correlates with cognitive decline in patients [58], who might otherwise benefit from a-tDCS application. Indeed, increased glutamate and glutamine levels were reported in the right parietal cortex following stimulation over the same region [59], proving the specificity of tDCS in targeting molecular patterns that might prompt behavior ural improvements in pathological samples. Apart from the study of amyloid-induced alterations at neurotransmitters’ levels, new approaches are considering tau aggregates and glial activation (an expression of neuroinflammation) as potential targets of interest. Not surprisingly, all those underlying alterations at neuronal and synaptic level sum up in much broader deviations from normality in the brain oscillatory activity and functional connectivity patterns. As already mentioned in the introduction, resting-state networks are progressively altered in various forms of dementia, showing patterns of disaggregation that mirror the spreading of the corresponding proteinopathy and cortical atrophy [4,5,6]. Similarly, altered temporal oscillatory activity has been reported across different brain regions, such as between frontal and parietal regions or between frontal and hippocampal structures in AD [60, 61]. In this sense, the use of tES has mostly been directed toward promoting their functional recoupling, favoring regional synchronization at least momentarily.
tES levels of intervention. tES could be applied to modulate a range of hierarchically organized levels, from synaptic coupling between neurons (moderating membrane’s potential and neurotransmitters release), up to larger-scale functional networks. At the cellular level, excitatory effects can be induced through the stimulation of pyramidal neurons, whereas inhibitory effects are achievable by targeting inhibitory interneurons. Particular interest is nowadays directed toward the potential use of tES in modulating neuroinflammation through microglia targeting. At the whole brain level, pathological targets include physiological mechanisms that might counteract amyloid-β and tau protein levels increase and the associated metabolic decrease as measured via FDG-PET imaging. At the system level, modern devices allow multisite stimulation, enabling the targeting of specific cortical networks. Such technological advances represent a substantial improvement from previous bifocal approaches, whereby large rectangular sponges were applied on the scalp to target broad and unspecific underlying cortical sites
The main aim of any stimulation protocol is improving individual cognitive functioning in order to promote activities of daily living. As such, traditional targets include bilateral or unilateral prefrontal cortices (especially DLPFC) and temporal lobes, as neural substrates of language, executive functional deficits, and memory impairments, respectively. Within AD pathology, a-tDCS applied at home daily for 6 months was successful in boosting global cognitive performances and language abilities, preventing executive functions decay at a marginal level [62]. The authors further reported those changes in cognitive functioning to be accompanied by a preserved glucose regional metabolism in the inferior/middle temporal gyrus for the active group, compared to the metabolic decrease observed in the sham group [62]. Similarly, both a-tDCS and c-tDCS applied over 10 sessions helped improve global cognitive performance at the Mini Mental State Examination (MMSE) in 34 AD patients, with an effect on Performance Intelligent Quotient (p-IQ) at the Wechsler Adult Intelligence Scale (WAIS) for c-tDCS [63]. The induced cognitive changes were further paralleled by a decrease in the P300 latency, an EEG Event-Related Potential (ERP) component known to be pathologically increased in this group of patients [63]. Complex quantitative EEG rearrangements following tES have also been described in other studies. One recent investigation has reported that the tDCS-induced increase in the high-frequency power over temporoparietal regions was positively associated with improvement at the MMSE, partially reversing the abnormal EEG patterns seen in AD [64]. Loss of phase coherence is also commonly reported in AD, as a result of both connection loss between cortical regions and atrophy. In this study, coherence resulted higher after tDCS, positively correlating also with better performances in a word recognition test [64]. Overall, those studies provide evidence of the metabolic and electrophysiological changes that accompany pathological aging and that can be partially addressed by means of noninvasive stimulation. Most importantly, those studies prove how tES induces functional changes that rely on measurable neural changes. Prior researches have also reported increased recognition memory [65], persisting up to 4 weeks [66]. In a single case study, tES combined with traditional cognitive therapy helped to maintain spared cognitive functioning for longer time, promoting patient’s stability up to 3 months [67]. Nevertheless, caution is highly recommended as negative findings have also been reported, possibly due to the greater severity of the population tested and their reduced number [68].
Apart from the pervasive memory impairments, language skills are also impoverished both in AD and FTD, and even more in an FTD variant, known as Primary Progressive Aphasia (PPA). Anomic spells frequently characterize the early stages of those pathologies, contributing to the diminished communication efficiency. Interestingly, tDCS, administered during a picture-naming training, was reported to be efficacious in improving naming capacities in 10 anomic AD and FTD patients, with generalized benefits to also untrained items, as well as in other neuropsychological tasks, such as digit span [69]. Real stimulation, compared to sham, guaranteed the effects to remain for at least 2 weeks after the end of the training [69]. In a sample of PPA patients, a similar stimulation protocol also successfully increased performance over trained items, with a slower rate of decline for those same items in the 6 months following stimulation, but with no effects over untrained ones [70]. On the other hand, generalization over untrained material was reported in a different study where tES was combined with language therapy, once again suggesting the greater synergic effects of combined interventions [71, 72]. Interestingly, a prior study had linked improved performance in naming with greater gray matter volume over the left fusiform gyrus, left middle and right inferior temporal gyri, such as that greater baseline volume over those regions was predictive of greater performance gains following stimulation [73]. Since regional volume loss is among the first characteristics of neurodegeneration, those findings prompt toward the need of addressing cognitive functions as early as possible to maximize patients’ improvement [73]. Although language-related processes and communication skills have been the most targeted aspects of cognition in FTD and PPA patients (see also [74, 75]), very recent applications of tES were capable of addressing other important weakened functions, such as behavioral dyscontrol and the inability to predict others’ responses from the perspective of an impaired Theory of Mind [76, 77]. Both studies are of great importance as personality changes, disinhibition, and misbehavior have a severe effect not only on patient him/herself, but represent a substantial cause of distress for family members and caregivers too.
Finally, one last application for tES interventions has focused on other forms of dementia that since the earliest stages are characterized by the presence of motor-related disorders, as observed in Parkinson’s Disease (PD) and Dementia with Lewy Bodies (DLB). In one of the first studies, a-tDCS over the primary motor cortex (M1) of PD patients had a significant effect on motor functions, as assessed by the Parkinson’s Disease Rating Scale, whereas no effect was reported when c-tDCS was applied or when DLPFC was targeted instead [78]. Similarly to what was reported for AD and FTD patients, a-tDCS applied to prefrontal regions in patients with PD was successful in improving working memory [79], attention [80], and phonemic fluency, which was accompanied by greater connectivity in verbal fluency networks as assessed by rs-fMRI [81]. Subsequent investigation assessing verbal fluency in PD patients also observed an improved response following a-tDCS combined with physical therapy, which persisted at 3-month follow-up [82]. Parkinson’s Disease Cognitive Rating Scale scores also increased following a-tDCS, allowing PD patients with MCI to score within the normal range following stimulation [82].
2 tES and Cognitive-Motor Function
Cognitive decline associated with both biological aging and disease has direct, deleterious effects on motor control with often profound functional implications. In particular, standing, walking, turning, and transferring call upon numerous cognitive-motor brain networks involved in the planning, execution, and adaptation of full-body movements. This high-level control is amplified when our daily activities require us to navigate complex, ever-changing environments, often while completing additional tasks like reading, talking, or making decisions. Cognitive impairment, and in particular executive dysfunction, is in fact a strong independent risk factor for balance decline [83], gait instability [84], ADL disability [85], and falls [86] in older adults. Those with dementia, for example, are five times more likely to suffer from falls and their morbid consequences as compared to older adults living with intact cognitive functions [87, 88]. Thus, in addition to the potential of promoting traditional cognitive outcomes, tES aimed at enhancing the functionality of cognitive-motor brain networks holds promise as a strategy to offset age- and dementia-related declines in cognitive-motor control—especially those that disrupt safe navigation and threaten functional independence.
The potential for NIBS to reduce falls in older adults has not been examined to date. Preliminary yet promising evidence, however, suggest that tES may improve the cortical control of walking (i.e., gait) and standing (i.e., posture) in older adults without overt neurological disease. Limited evidence also suggests that it may be beneficial to mobility in those with MCI or Parkinson’s disease. The majority of this evidence comes from published studies using tDCS with the intent of facilitating the excitability of either the prefrontal or motor cortices. Available work has examined both the acute effects of a single session of stimulation and/or the longer-term effects of multiple sessions over several consecutive weeks.
Zhou and colleagues have published a series of studies suggesting that a-tDCS, designed to target the left DLPFC, acutely improves the control of standing and walking—especially in “dual-task” situations. Participants of each study completed two visits during which dual-task performance was assessed immediately before and after a-tDCS or sham stimulation. The dual-task paradigm involved trials of standing and walking both with and without simultaneous performance of a serial subtraction cognitive task. In healthy young adults [89], in healthy older adults [15], and in very old adults presenting with mild cognitive impairment [90], dual tasking resulted in a significant “cost” (i.e., performance decrement) to both gait and standing postural control. In each cohort, a-tDCS, as compared to sham, significantly reduced the dual-task cost to several metrics of gait and postural control, when tested in the 30 min following stimulation.
Building upon this work, the same group recently published a pilot double-blinded randomized sham-controlled trial of a 2-week, 10-session a-tDCS intervention in very old adults without overt illness or disease, yet who presented with both slow gait and mild-to-moderate executive dysfunction. tDCS, compared to sham, resulted in dual-task gait postural control improvements that persisted throughout a 2-week follow-up period. Moreover, the a-tDCS group exhibited clinically meaningful improvements in global cognitive function as measured by the Montreal Cognitive Assessment (MoCA).
While the foregoing preliminary evidence indicates that tDCS targeting prefrontal regions may improve the dual-task gait and balance performance, the effects of tDCS targeting the motor cortex or other brain regions or networks with known involvement in mobility in aging are still largely unexplored. In one of few other studies, Kaminski et al. [91] examined whether tDCS designed to facilitate the excitability of the primary motor cortex (M1) facilitated learning of a dynamic balance task in 30 healthy older adults. Participants received a single session of tDCS or sham stimulation while completing a balance training task. The researchers reported that both the group receiving tDCS and the group receiving sham stimulation learned from training, yet that tDCS did not influence the level of task learning. Thus, while tES may augment certain aspects of gait and balance in older adults, additional research is needed to determine optimal targets and dosage, if such interventions should be paired with other evidence-based balance and mobility programs, and ultimately, if improvements in gait and balance translate into increased safety and improve ADL performance in older adults with MCI or AD.
Beyond MCI and AD, tES appears to have positive impact on cognitive-motor symptoms in patients with Parkinson’s disease. The available evidence is heterogeneous in both intervention characteristics and outcome measures [92], and potential interactions between tDCS and parkinsonian medications remain poorly understood [93]. Nevertheless, tES, aimed at modulating the excitability of primary motor and/or prefrontal brain regions, appears to improve functional outcomes in this population. Lattari et al. [94], for example, examined the effects of a single session of a-tDCS targeting the left DLPFC in a double-blinded, sham-controlled, within-subject, crossover study in 17 individuals with PD. The intervention and all study assessments were completed with participants in the “on-medication” state. a-tDCS, compared to sham, led to acute improvements in whole-body mobility as measured by the Berg Balance Scale, the Dynamic Gait Index, and the Timed Up-and-Go (TUG). Similarly, Hadoush et al. [95] reported that a 10-session a-tDCS intervention aimed at facilitating bilateral motor and prefrontal excitability, as compared to an inactive sham, led to improved balance and reduced fear of falling in patients with idiopathic Parkinson’s disease. Recently, Dagan et al. [96] reported the immediate after-effects of a single session of “multitarget” tDCS designed to simultaneously facilitate the excitability of the left DLPFC and the leg regions of the bilateral M1. This stimulation significantly reduced the severity of “freezing of gait,” as compared to stimulation targeting M1 alone or an active sham control. These promising immediate after-effects of tDCS on freezing of gait—a complex symptom theorized to arise from abnormalities in both cognitive and motor brain functions—warrant investigation of the longer-term effects of multisession tES interventions on this and other cognitive-motor symptoms in patients who suffer from PD, with and without concomitant cognitive dysfunction.
3 Future Perspectives
Literature studies provide a rationale for the use of tES interventions in the aging process, suggesting a plausible role of stimulation in boosting individual performances, from motor to higher-order cognitive functioning. Nevertheless, substantial improvement is still needed to augment protocol efficiency. First of all, (1) target selection represents a critical aspect, as most approaches rely on stimulating prefrontal cortices (especially left DLPFC) based on their known involvement in higher-order cognitive processes, and relying on the rationale that prior studies had used it too, but substantially failing to consider interindividual topological differences and networks’ structure. Furthermore, this approach limits the application of stimulation to a single region, while it is known that several cortical nodes constitute the frontoparietal network, and therefore the goodness of the task execution is more likely determined by their combined contribution. Therefore, recent technological advances have started promoting the use of multifocal stimulation, whereby a genetic algorithm is used to determine electrode arrangements on the scalp to produce a desired electrical field, maximizing the chances of stimulating the targeted cortical network, while minimizing unspecific cortical effects [97, 98]. So far, motor network stimulation by means of eight separate electrodes was proven more efficient in increasing cortical excitability of the left M1 compared to the traditional bifocal approach, doubling its effects [97].
As stimulation approaches move toward a better spatial tailoring, (2) more time-dynamic tuning of the delivered electrical currents is also foreseen. Indeed, state-dependent effects are known to widely drive stimulation efficacy. Very recently, a-tDCS effects over DLPFC-mediated executive functions were observed to be largely determined by underlying electrophysiological phenomena, such as that the individuals who benefitted more from stimulation were the ones with the lower amplitude at baseline [99]. Continuous monitoring of the underlying brain states could therefore be very informative to determine when to best deliver the electrical pulse, acknowledging that neural populations might be modulated with a different degree depending on their current state [99]. Based on this, closed-loop approaches have started to emerge in the literature, where the simultaneous registration of the individual EEG activity is used to tune the current delivery from the stimulation device. As predictive algorithms are used to determine the forthcoming neural oscillation to be targeted, thus automatizing the process of stimulation, closed-loop approaches have the potential to be applied under various conditions, for example during sleep. (3) Sleep modulation particularly suits neurodegenerative studies, where difficulties in memory consolidation are a hallmark. Based on the rationale that slow-wave oscillations, observed at the scalp level during sleep, reflect large-scale synchronization between cortical and subcortical regions, promoting the consolidation of short-term memory into long-term memory, closed-loop tACS has been successfully applied in healthy subjects to improve memory performances [100]. Furthermore, a strict relationship seems to exist between AD proteinopathy and the quality and duration of sleep, such as that cerebrospinal levels of tau and amyloid-β are associated with poorness in slow-wave sleep in patients [101]. The use of tES during sleep seems therefore a promising tool to address both the mechanisms of protein clearance and those of memory consolidation, with the potential to lead to home-based therapy, posing a new challenge for future studies.
Finally, tACS stimulation has gained renewed interest in recent years for the possibility of (4) targeting gamma oscillations, which are fast EEG oscillations occurring around 40 Hz. Prior animal work has demonstrated that the induction of gamma activity via optogenetics or sensory stimulation reduces amyloid-β plaques [102], and that impaired coupling between (fast) gamma and (slow) theta oscillations over frontal regions was not only associated with impaired working memory performances, but it occurred in AD and MCI patients even before overt behavioral symptoms (for a review, see [103]). Furthermore, failure to respond to tACS applied at the gamma frequency band correctly discriminated between MCI patients designated to convert into AD 2 years later and those who did not [30], proving tACS gamma to be a potential useful perturbation-based biomarker in predicting MCI to AD conversion.
4 Summary
To date, various tES interventions have been proven effective in targeting spared functions in older adults, boosting performance levels at both cognitive and motor tasks and their concomitant execution (dual-task). Evidence on the effectiveness of tES is corroborated by the corresponding changes in neuroimaging, electroencephalographic, and metabolic data recorded before and after stimulation, or compared across active and sham stimulation cohorts. As more evidence will be gathered in future years, the use of tES should be promoted in patients’ care routine, considering its potential use as a therapeutic tool and as a biomarker of disease progression. Future technological advances will further enable us to gain better understanding of the underlying neuropathological mechanisms of dementia, and address innovative therapeutic targets, hoping to further improve everyday medical care.
References
Cabeza R. Hemispheric asymmetry reduction in older adults: the HAROLD model. Psychol Aging. 2002;17(1):85–100.
Davis SW, Dennis NA, Daselaar SM, Fleck MS, Cabeza R. Qué PASA? The posterior–anterior shift in aging. Cereb Cortex. 2008;18(5):1201–9.
Calsolaro V, Edison P. Neuroinflammation in Alzheimer’s disease: current evidence and future directions. Alzheimers Dement. 2016;12(6):719–32.
Jones DT, Knopman DS, Gunter JL, Graff-Radford J, Vemuri P, Boeve BF, et al. Cascading network failure across the Alzheimer’s disease spectrum. Brain. 2016;139(2):547.
Buckner RL. Molecular, structural, and functional characterization of Alzheimer’s disease: evidence for a relationship between default activity, amyloid, and memory. J Neurosci. 2005;25(34):7709–17.
Zhou J, Greicius MD, Gennatas ED, Growdon ME, Jang JY, Rabinovici GD, et al. Divergent network connectivity changes in behavioural variant frontotemporal dementia and Alzheimer’s disease. Brain. 2010;133(5):1352.
Khedr EM, Salama RH, Hameed MA, Elfetoh NA, Seif P. Therapeutic role of transcranial direct current stimulation in Alzheimer disease patients: double-blind, placebo-controlled clinical trial. Neurorehabil Neural Repair. 2019;33(5):384–94.
Ross LA, McCoy D, Wolk DA, Coslett HB, Olson IR. Improved proper name recall in aging after electrical stimulation of the anterior temporal lobes. Front Aging Neurosci. 2011;3:16.
Meinzer M, Lindenberg R, Antonenko D, Flaisch T, Floel A. Anodal transcranial direct current stimulation temporarily reverses age-associated cognitive decline and functional brain activity changes. J Neurosci. 2013;33(30):12470–8.
Floel A, Suttorp W, Kohl O, Kurten J, Lohmann H, Breitenstein C, et al. Non-invasive brain stimulation improves object-location learning in the elderly. Neurobiol Aging. 2012;33(8):1682–9.
Sandrini M, Manenti R, Brambilla M, Cobelli C, Cohen LG, Cotelli M. Older adults get episodic memory boosting from noninvasive stimulation of prefrontal cortex during learning. Neurobiol Aging. 2016;39:210–6.
Sandrini M, Brambilla M, Manenti R, Rosini S, Cohen LG, Cotelli M. Noninvasive stimulation of prefrontal cortex strengthens existing episodic memories and reduces forgetting in the elderly. Front Aging Neurosci. 2014;6:289.
Jones KT, Stephens JA, Alam M, Bikson M, Berryhill ME. Longitudinal neurostimulation in older adults improves working memory. PLoS One. 2015;10(4):e0121904.
Nilsson J, Lebedev AV, Lövdén M. No significant effect of prefrontal tDCS on working memory performance in older adults. Front Aging Neurosci. 2015;7:230.
Manor B, Zhou J, Jor’dan A, Zhang J, Fang J, Pascual-Leone A. Reduction of dual-task costs by noninvasive modulation of prefrontal activity in healthy elders. J Cogn Neurosci. 2015;28(2):275–81.
Harty S, Robertson IH, Miniussi C, Sheehy OC, Devine CA, McCreery S, et al. Transcranial direct current stimulation over right dorsolateral prefrontal cortex enhances error awareness in older age. J Neurosci. 2014;34(10):3646–52.
Fecteau S, Knoch D, Fregni F, Sultani N, Boggio P, Pascual-Leone A. Diminishing risk-taking behavior by modulating activity in the prefrontal cortex: a direct current stimulation study. J Neurosci. 2007;27(46):12500–5.
Boggio PS, Campanhã C, Valasek CA, Fecteau S, Pascual-Leone A, Fregni F. Modulation of decision-making in a gambling task in older adults with transcranial direct current stimulation. Eur J Neurosci. 2010;31:593–7.
Learmonth G, Thut G, Benwell CSY, Harvey M. The implications of state-dependent tDCS effects in aging: behavioural response is determined by baseline performance. Neuropsychologia. 2015;74:108–19.
Berryhill ME, Jones KT. tDCS selectively improves working memory in older adults with more education. Neurosci Lett. 2012;521(2):148–51.
Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8(3):448–60.
Portet F, Ousset PJ, Visser PJ, Frisoni G, Nobili F, Scheltens P, et al. Mild cognitive impairment (MCI) in medical practice: a critical review of the concept and new diagnostic procedure. Report of the MCI Working Group of the European Consortium on Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2006;77(6):714–8.
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551–61.
Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, et al. Current concepts in mild cognitive impairment. Arch Neurol. 2001;58(12):1985–92.
Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. 2014;275(3):214–28.
Drago V, Babiloni C, Bartrés-Faz D, Caroli A, Bosch B, Hensch T, et al. Disease tracking markers for Alzheimer’s disease at the prodromal (MCI) stage. J Alzheimers Dis. 2011;26(s3):159–99.
Bertè F, Lamponi G, Calabrò RS, Bramanti P. Elman neural network for the early identification of cognitive impairment in Alzheimer’s disease. Funct Neurol. 2014;29(1):57–65.
Vega JN, Newhouse PA. Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments. Curr Psychiatry Rep. 2014;16(10):490.
Hugo J, Ganguli M. Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014;30(3):421.
Naro A, Corallo F, De Salvo S, Marra A, Di Lorenzo G, Muscarà N, et al. Promising role of neuromodulation in predicting the progression of mild cognitive impairment to dementia. J Alzheimers Dis. 2016;53(4):1375–88.
Yener GG, Başar E. Sensory evoked and event related oscillations in Alzheimer’s disease: a short review. Cogn Neurodyn. 2010;4(4):263–74.
Sheng M, Sabatini BL, Sudhof TC. Synapses and Alzheimer’s disease. Cold Spring Harb Perspect Biol. 2012;4(5):a005777.
Uhlhaas PJ, Singer W. Neural synchrony in brain disorders: relevance for cognitive dysfunctions and pathophysiology. Neuron. 2006;52(1):155–68.
Santarnecchi E, Muller T, Rossi S, Sarkar A, Polizzotto NR, Rossi A, et al. Individual differences and specificity of prefrontal gamma frequency-tACS on fluid intelligence capabilities. Cortex. 2016;75:33–43.
Hoy KE, Bailey N, Arnold S, Windsor K, John J, Daskalakis ZJ, et al. The effect of γ-tACS on working memory performance in healthy controls. Brain Cogn. 2015;101:51–6.
Cabral-Calderin Y, Anne Weinrich C, Schmidt-Samoa C, Poland E, Dechent P, Bähr M, et al. Transcranial alternating current stimulation affects the BOLD signal in a frequency and task-dependent manner: effect of tACS on the BOLD signal. Hum Brain Mapp. 2016;37(1):94–121.
Abuhassan K, Coyle D. Employing neuronal networks to investigate the pathophysiological basis of abnormal cortical oscillations in Alzheimer’s disease - IEEE Conference Publication. In: Annual international conference of the IEEE Engineering in Medicine and Biology Society (IEEE), 2011. p. 2065–8.
Missonnier P, Herrmann FR, Michon A, Fazio-Costa L, Gold G, Giannakopoulos P. Early disturbances of gamma band dynamics in mild cognitive impairment. J Neural Transm. 2010;117(4):489–98.
Moretti DV, Frisoni G, Fracassi C, Pievani M, Geroldi C, Binetti G, et al. MCI patients’ EEGs show group differences between those who progress and those who do not progress to AD. Neurobiol Aging. 2011;32(4):563–71.
Park JY, Lee KS, An SK, Lee J, Kim J-J, Kim KH, et al. Gamma oscillatory activity in relation to memory ability in older adults. Int J Psychophysiol. 2012;86(1):58–65.
Yun K, Song I-U, Chung Y-A. Changes in cerebral glucose metabolism after 3 weeks of noninvasive electrical stimulation of mild cognitive impairment patients. Alzheimers Res Ther. 2016;8(1):49.
Murugaraja V, Shivakumar V, Sivakumar PT, Sinha P, Venkatasubramanian G. Clinical utility and tolerability of transcranial direct current stimulation in mild cognitive impairment. Asian J Psychiatr. 2017;30:135–40.
Meinzer M, Lindenberg R, Phan MT, Ulm L, Volk C, Floel A. Transcranial direct current stimulation in mild cognitive impairment: behavioral effects and neural mechanisms. Alzheimers Dement. 2015;11(9):1032–40.
Ladenbauer J, Ladenbauer J, Külzow N, de Boor R, Avramova E, Grittner U, et al. Promoting Sleep oscillations and their functional coupling by transcranial stimulation enhances memory consolidation in mild cognitive impairment. J Neurosci. 2017;37(30):7111–24.
Westerberg CE, Mander BA, Florczak SM, Weintraub S, Mesulam M-M, Zee PC, et al. Concurrent impairments in sleep and memory in amnestic mild cognitive impairment. J Int Neuropsychol Soc. 2012;18(3):490.
Wang G, Grone B, Colas D, Appelbaum L, Mourrain P. Synaptic plasticity in sleep: learning, homeostasis and disease. Trends Neurosci. 2011;34(9):452–63.
Ju Y-ES, Lucey BP, Holtzman DM. Sleep and Alzheimer disease pathology—a bidirectional relationship. Nat Rev Neurol. 2014;10(2):115.
Gonzalez PC, Fong KNK, Chung RCK, Ting K-H, Law LLF, Brown T. Can transcranial direct-current stimulation alone or combined with cognitive training be used as a clinical intervention to improve cognitive functioning in persons with mild cognitive impairment and dementia? A systematic review and meta-analysis. Front Hum Neurosci. 2018;12:416.
Hansen N. Action mechanisms of transcranial direct current stimulation in Alzheimer’s disease and memory loss. Front Psychiatry. 2012;3:48.
Blanchard BJ, Thomas VL, Ingram VM. Mechanism of membrane depolarization caused by the Alzheimer Aβ1–42 peptide. Biochem Biophys Res Commun. 2002;293(4):1197–203.
Fernandez A, Maestù F, Amo C, Gil P, Fehr T, Wienbruch C, et al. Focal temporoparietal slow activity in Alzheimer’s disease revealed by magnetoencephalography. Biol Psychiatry. 2002;52(7):764–70.
Di Lazzaro V, Oliviero A, Pilato F, Saturno E, Dileone M, Marra C, et al. Motor cortex hyperexcitability to transcranial magnetic stimulation in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2004;75(4):555–9.
Rossini P, Rossi S, Babiloni C, Polich J. Clinical neurophysiology of aging brain: From normal aging to neurodegeneration. Prog Neurobiol. 2007;83(6):375–400.
Ardolino G, Bossi B, Barbieri S, Priori A. Non-synaptic mechanisms underlie the after-effects of cathodal transcutaneous direct current stimulation of the human brain. J Physiol. 2005;568(2):653–63.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(3):633–9.
Paulus W. Outlasting excitability shifts induced by direct current stimulation of the human brain. Suppl Clin Neurophysiol. 2004;57:708–14.
Yamin G. NMDA receptor–dependent signaling pathways that underlie amyloid β-protein disruption of LTP in the hippocampus. J Neurosci Res. 2009;87(8):1729–36.
Parameshwaran K, Dhanasekaran M, Suppiramaniam V. Amyloid beta peptides and glutamatergic synaptic dysregulation. Exp Neurol. 2008;210(1):7–13.
Clark VP, Coffman BA, Trumbo MC, Gasparovic C. Transcranial direct current stimulation (tDCS) produces localized and specific alterations in neurochemistry: a 1H magnetic resonance spectroscopy study. Neurosci Lett. 2011;500(1):67–71.
Montez T, Poil S-S, Jones BF, Manshanden I, Verbunt JPA, van Dijk BW, et al. Altered temporal correlations in parietal alpha and prefrontal theta oscillations in early-stage Alzheimer disease. Proc Natl Acad Sci U S A. 2009;106(5):1614–9.
Grady CL, Furey ML, Pietrini P, Horwitz B, Rapoport SI. Altered brain functional connectivity and impaired short-term memory in Alzheimer’s disease. Brain. 2001;124(4):739–56.
Im JJ, Jeong H, Bikson M, Woods AJ, Unal G, Oh KJ, et al. Effects of 6-month at-home transcranial direct current stimulation on cognition and cerebral glucose metabolism in Alzheimer’s disease. Brain Stimul. 2019;12(5):1222–8.
Khedr EM, Gamal NFE, El-Fetoh NA, Khalifa H, Ahmed EM, Ali AM, et al. A double-blind randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer’s disease. Front Aging Neurosci. 2014;6:275.
Marceglia S, Mrakic-Sposta S, Rosa M, Ferrucci R, Mameli F, Vergari M, et al. Transcranial direct current stimulation modulates cortical neuronal activity in Alzheimer’s disease. Front Neurosci. 2016;10:134.
Ferrucci R, Mameli F, Guidi I, Mrakic-Sposta S, Vergari M, Marceglia S, et al. Transcranial direct current stimulation improves recognition memory in Alzheimer disease. Neurology. 2008;71(7):493–8.
Boggio PS, Ferrucci R, Mameli F, Martins D, Martins O, Vergari M, et al. Prolonged visual memory enhancement after direct current stimulation in Alzheimer’s disease. Brain Stimul. 2012;5(3):223–30.
Penolazzi B, Bergamaschi S, Pastore M, Villani D, Sartori G, Mondini S. Transcranial direct current stimulation and cognitive training in the rehabilitation of Alzheimer disease: a case study. Neuropsychol Rehabil. 2014;25(6):799–817.
Bystad M, Grønli O, Rasmussen ID, Gundersen N, Nordvang L, Wang-Iversen H, et al. Transcranial direct current stimulation as a memory enhancer in patients with Alzheimer’s disease: a randomized, placebo-controlled trial. Alzheimers Res Ther. 2016;8:13.
Roncero C, Kniefel H, Service E, Thiel A, Probst S, Chertkow H. Inferior parietal transcranial direct current stimulation with training improves cognition in anomic Alzheimer’s disease and frontotemporal dementia. Alzheimers Dement. 2017;3(2):247–53.
Hung J, Bauer A, Grossman M, Hamilton RH, Coslett HB, Reilly J. Semantic feature training in combination with Transcranial Direct Current Stimulation (tDCS) for progressive anomia. Front Hum Neurosci. 2017;11:253.
Tsapkini K, Frangakis C, Gomez Y, Davis C, Hillis AE. Augmentation of spelling therapy with transcranial direct current stimulation in primary progressive aphasia: preliminary results and challenges. Aphasiology. 2014;28(8–9):1112–30.
Tsapkini K, Webster KT, Ficek BN, Desmond JE, Onyike CU, Rapp B, et al. Electrical brain stimulation in different variants of primary progressive aphasia: a randomized clinical trial. Alzheimers Dement. 2018;4:461–72.
Cotelli M, Manenti R, Paternicò D, Cosseddu M, Brambilla M, Petesi M, et al. Grey matter density predicts the improvement of naming abilities after tDCS intervention in agrammatic variant of primary progressive aphasia. Brain Topogr. 2016;29(5):738–51.
Gervits F, Ash S, Coslett HB, Rascovsky K, Grossman M, Hamilton R. Transcranial direct current stimulation for the treatment of primary progressive aphasia: an open-label pilot study. Brain Lang. 2016;162:35–41.
Wang J, Wu D, Chen Y, Yuan Y, Zhang M. Effects of transcranial direct current stimulation on language improvement and cortical activation in nonfluent variant primary progressive aphasia. Neurosci Lett. 2013;549:29–33.
Cotelli M, Adenzato M, Cantoni V, Manenti R, Alberici A, Enrici I, et al. Enhancing theory of mind in behavioural variant frontotemporal dementia with transcranial direct current stimulation. Cogn Affect Behav Neurosci. 2018;18(6):1065–75.
Ferrucci R, Mrakic-Sposta S, Gardini S, Ruggiero F, Vergari M, Mameli F, et al. Behavioral and neurophysiological effects of Transcranial Direct Current Stimulation (tDCS) in fronto-temporal dementia. Front Behav Neurosci. 2018;12:235.
Fregni F, Boggio PS, Santos MC, Lima M, Vieira AL, Rigonatti SP, et al. Noninvasive cortical stimulation with transcranial direct current stimulation in Parkinson’s disease. Mov Disord. 2006;21(10):1693–702.
Boggio PS, Ferrucci R, Rigonatti SP, Covre P, Nitsche MA, Pascual-Leone A, et al. Effects of transcranial direct current stimulation on working memory in patients with Parkinson’s disease. J Neurol Sci. 2006;249(1):31–8.
Elder GJ, Firbank MJ, Kumar H, Chatterjee P, Chakraborty T, Dutt A, et al. Effects of transcranial direct current stimulation upon attention and visuoperceptual function in Lewy body dementia: a preliminary study. Int Psychogeriatr. 2016;28(2):341.
Pereira JB, Junqué C, Bartrés-Faz D, Martì MJ, Sala-Llonch R, Compta Y, et al. Modulation of verbal fluency networks by transcranial direct current stimulation (tDCS) in Parkinson’s disease. Brain Stimul. 2013;6(1):16–24.
Manenti R, Brambilla M, Benussi A, Rosini S, Cobelli C, Ferrari C, et al. Mild cognitive impairment in Parkinson’s disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016;31:715–24.
Muir-Hunter SW, Clark J, McLean S, Pedlow S, Hemmen AV, Odasso MM, et al. Identifying balance and fall risk in community-dwelling older women: the effect of executive function on postural control. Physiother Can. 2014;66(2):179.
Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23(3):329–42.
Johnson JK, Lui L-Y, Yaffe K. Executive function, more than global cognition, predicts functional decline and mortality in elderly women. J Gerontol A Biol Sci Med Sci. 2007;62(10):1134–41.
Mirelman A, Herman T, Brozgol M, Dorfman M, Sprecher E, Schweiger A, et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One. 2012;7(6):e40297.
Shaw FE. Falls in older people with dementia. Geriatr Aging. 2003;6(7):37–40.
Pellfolk T, Gustafsson T, Gustafson Y, Karlsson S. Risk factors for falls among residents with dementia living in group dwellings. Int Psychogeriatr. 2009;21(1):187–94.
Zhou J, Hao Y, Wang Y, Jor’dan A, Pascual-Leone A, Zhang J, et al. Transcranial direct current stimulation reduces the cost of performing a cognitive task on gait and postural control. Eur J Neurosci. 2014;39(8):1343–8.
Manor B, Zhou J, Harrison R, Lo O-Y, Travison TG, Hausdorff JM, et al. Transcranial direct current stimulation may improve cognitive-motor function in functionally limited older adults. Neurorehabil Neural Repair. 2018;32(9):788–98.
Kaminski E, Hoff M, Rjosk V, Steele CJ, Gundlach C, Sehm B, et al. Anodal transcranial direct current stimulation does not facilitate dynamic balance task learning in healthy old adults. Front Hum Neurosci. 2017;11:16.
Lafaucheur J-P, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol. 2017;128(1):56–92.
Rektorova I, Anderkova L. Noninvasive brain stimulation and implications for nonmotor symptoms in Parkinson’s disease. Int Rev Neurobiol. 2017;134:1091–110.
Lattari E, Costa SS, Campos C, de Oliveira AJ, Machado S, Maranhao Neto GA. Can transcranial direct current stimulation on the dorsolateral prefrontal cortex improves balance and functional mobility in Parkinson’s disease? Neurosci Lett. 2017;636:165–9.
Hadoush H, Al-Jarrah M, Khalil H, Al-Sharman A, Al-Ghazawi S. Bilateral anodal transcranial direct current stimulation effect on balance and fearing of fall in patient with Parkinson’s disease. NeuroRehabilitation. 2018;42(1):63–8.
Dagan M, Herman T, Harrison R, Zhou J, Giladi N, Ruffini G, et al. Multitarget transcranial direct current stimulation for freezing of gait in Parkinson’s disease. Mov Disord. 2018;33(4):642–6.
Fischer DB, Fried PJ, Ruffini G, Ripolles O, Salvador R, Banus J, et al. Multifocal tDCS targeting the resting state motor network increases cortical excitability beyond traditional tDCS targeting unilateral motor cortex. Neuroimage. 2017;157:34–44.
Ruffini G, Fox MD, Ripolles O, Cavaleiro Miranda P, Pascual-Leone A. Optimization of multifocal transcranial current stimulation for weighted cortical pattern targeting from realistic modeling of electric fields. Neuroimage. 2014;89:216–25.
Dubreuil-Vall L, Chau P, Ruffini G, Widge AS, Camprodon JA. tDCS to the left DLPFC modulates cognitive and physiological correlates of executive function in a state-dependent manner. Brain Stimul. 2019;12:1456–63.
Jones AP, Choe J, Bryant NB, Robinson CSH, Ketz NA, Skorheim SW, et al. Dose-dependent effects of closed-loop tACS delivered during slow-wave oscillations on memory consolidation. Front Neurosci. 2018;12:867.
Liguori C, Romigi A, Nuccetelli M, Zannino S, Sancesario G, Martorana A, et al. Orexinergic system dysregulation, sleep impairment, and cognitive decline in Alzheimer disease. JAMA Neurol. 2014;71(12):1498–505.
Iaccarino HF, Singer AC, Martorell AJ, Rudenko A, Gao F, Gillingham TZ, et al. Gamma frequency entrainment attenuates amyloid load and modifies microglia. Nature. 2016;540(7632):230–5.
Rajji TK. Impaired brain plasticity as a potential therapeutic target for treatment and prevention of dementia. Expert Opin Ther Targets. 2018;23:21–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Menardi, A., Manor, B., Santarnecchi, E. (2020). tES in Dementia: From Pathophysiology to Treatment. In: Dell'Osso, B., Di Lorenzo, G. (eds) Non Invasive Brain Stimulation in Psychiatry and Clinical Neurosciences. Springer, Cham. https://doi.org/10.1007/978-3-030-43356-7_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-43356-7_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43355-0
Online ISBN: 978-3-030-43356-7
eBook Packages: MedicineMedicine (R0)