Abstract
The context of this work concerns the development of a connected smartwatch for the continuous daily monitoring of physiological parameters to prevent cardiovascular diseases, and for the follow-up of the efficiency of treatments, against hypertension for example. This paper focuses on a particular parameter, the blood pressure (BP), to be automatically measured from the Photoplethysmogram (PPG) signal, to be acquired using a smartwatch. The proposed method is based on the automatic pulse wave detection from the PPG signal. Then, using the Lasso algorithm, a relation has been established between the blood pressure and the spectral representation of the normalized pulse wave, combined with other physiological information (age, body mass index and hear rate). The proposed method has been evaluated on a recent large public database of 219 subjects, covering a large range of ages (20–89), body mass indices and of blood pressures. Experimental results show acceptable performances in terms of accuracy. Compared to a recent related work depicting a slightly lower estimation error, a strength of our approach regards its robustness with respect to the signal quality, this being crucial for a use in daily routine in real IoT conditions, as it is the case in this context of smartwatch.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
During the last 15 years, a lot of research has been made on photoplethysmography signal (PPG). In 1996, [1] evaluated morphological changes of the pulse wave due to ventilation, anaesthesia, etc\(\ldots \) Moreover, this study also underlined the relevance of analyzing peripheral pulse wave in cardiac function, for diagnosis purpose. Since then, some research has been focused on predicting arterial blood pressure thanks to PPG signal as it would allow non-invasive and continuous monitoring. Coupling PPG monitoring with Internet of Things (IoT) application could provide to the doctor real-time measurement and trends over weeks of patient’s blood pressure. This would allow the early detection of hypertension, as well as the follow-up of the efficiency of the anti-hypertension treatment, therefore facilitating its adaptation [2, 3]. In many ways, this kind of technology would help to improve healthcare system.
This work takes place within the context of the development of a smartwatch iHeartWatch with Axelife which is able to record several physiological parameters, including PPG signal, from wirst. This smartwatch is connected to a smartphone itself connected to the web. The longterm goal is to provide predictive data analysis to improve patient’s cardiovascular diagnosis and thus help in decision making. In this context, the first challenge for the early detection of cardiovascular diseases is to monitor blood pressure over time thanks to PPG sensor, as illustrated by Fig. 1.
In this paper, the proposed approach is based on spectral signal analysis rather than on temporal features, that are assumed to be more tedious to acquire, and more sensitive to signal quality, as illustrated by recent works [4], ignoring some abnormal PPG signals. Similarly to [4], our approach exploits physiological features, this being often ignored by most other related methods. Note that this work has to be integrated in a more complex acquisition and signal processing system which should be able to contextualize and select admissible pulse waves.
Rest of the paper is organized as follows. Section 2 focuses on the description of the method used with the different processing steps. Section 3 describes the data and experimental results. Sections 4 and 5 respectively contains a discussion and a conclusion.
2 Method
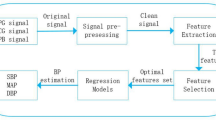
The block-diagram in Fig. 2 provide an overview of the proposed approach, including several steps of signal processing that are described herebelow.
2.1 Pre-processing
Preprocessing is require to further exploit PPG signal. This first preliminary step is crucial, as underlined by related works dedicated to the study of filtering techniques on public databases [5, 6]. In our work, preprocessing consists in several steps.
Step 1 - Filtering
We use a low pass linear-phase FIR filter to suppress high frequencies in the signal (Fig. 3B) with cuff-off frequency of 10 Hz which allows to suppress any power-line interference (50 Hz, 60 Hz, etc.). A smoothing is then applied by means of a digital filter with a polynomial order of three.
Step 2 - Extraction of pulse wave
Pulse wave extraction is achieved by searching for the minimal values between systolic peaks (Fig. 3C).
Step 3 - Normalisation of the signal in amplitude and time
Each extracted pulse wave has been normalized between 0 and 1, to focus on the shape of the wave, regardless to its amplitude. Then, time normalisation has been applied (length of pulse wave set to 1), to remove the dependency to the heart rate (and in particular to its variations over the set of pulse waves). Note that the heart rate is measured using another sensor (averaged measure over several cardiac cycle) (Fig. 4D).
Step 4 - Mean of pulse wave for each subject
Each signal embeds several pulse waves. To get a more robust blood pressure estimation, an averaged normalized pulse waves have been considered over all subject’s signals (average over the set of detected pulse waves). Leading to a single mean pulse wave per subject (Fig. 4E).
Step 5 - Rotation and zero threshold
Last pre-processing step consisted in rotating the pulse wave horizontally and thus being able to perform zero padding in order to increase the spectral resolution (Fig. 4F).
2.2 Feature Extraction
Feature extraction is performed in the frequency domain (FFT). This choice enables to avoid the detection of specific keypoints in the time domain, as considered in [4], on which are extracted time-domain-based features. Note that we only consider spectrum coefficients ranging from 0 to 10 Hz (Fig. 5).
2.3 Lasso Algorithm
Lasso is a regression analysis method [7]. It is used in large problems resolution, when there is an important set of features potentially linked to a target value. This algorithm can perform a restricted selection of variables significantly connected the target value to make an accurate prediction. Lasso algorithm has been applied on following variables, including physiological ones (age, body mass index (BMI), heart rate) and those related to the PPG signal (spectral coefficients).
3 Experiments
For experiments, a public database [6] has been considered, with the underlying advantage of facilitating the comparison with third party works.
Data were collected at the People’s Hospital of Guilin (PHG) in China [6] during a clinical laboratory measurement. It is composed of 657 PPG signals of 2.1 s each from 219 subjects (3 signals per subject). We end-up with a total of 212 pulse waves (one by subject) after the pre-processing steps. The 7 subjects missing is due to bad signal quality (mostly outliers for PHG database, see example Fig. 6B) that failed the automatic extraction of the pulse waves. It covers a large range of ages [20–89] and a large range of blood pressure too as its incorporates 3 types of hypertensive states. Furthermore, the database includes physiological information like height, weight, heart rate but also it contains an illness record about diabetes, cerebral infraction and cerebrovascular disease.
To establish a relationship between PPG waveforms and BP, the data acquisition procedure has been conducted in accordance with standard experimental conditions. It is important to mention that each subject was sitting in a comfortable position for 10 min to reach a rest state which allows reliable non-invasive cuff-less and continuous PPG signal measurement. However, this database comprise one drawback, the duration of the signals is very short, 2.1 s. Note that there is no possibility to evaluate dynamic changes.
During the experimentation, Lasso algorithm gave us some specific frequencies to use as features in order to predict BP. Table 1 shows the spectral frequencies and physiological characteristics selected to predict Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP).
Results of BP prediction performance are reported in Table 3. They are presented as Mean Absolute Error (MAE) and standard deviation (SD) of the MAE in terms of millimeter of mercury (mmHg), this being the standard unit for blood pressure in medicine. Formula are presented in Table 2. We computed K-fold cross-validated mean squared prediction error to evaluate total efficiency of our model.
According to [9], the criteria to fulfil AAMI protocol is that the mean difference and standard deviation between the given value of the mercury standard device and the one of the test devices must be in within 5 mmHg ± 8 mmHg. From this point of view, even if we do not use exactly the same performance values, [4] seems closer to be accepted than us as long as their is a control on signal quality otherwise our algorithms will probably perform the same or better on PHG database.
We tried to compute pulse waves without normalisation in amplitude too but results were a bit worse, therefore justifying our choice. In our sense, normalization is relevant due to environmental condition that can influence the signal amplitude measured. Especially due to temperature, lighting, skin contact quality, degree of pressure applied on the sensor against skin. All of those combined could influence estimation results if the pulse waves are not normalised.
Discarded subjects regards the proportion of the database that has been ignored. In our case, few subjects has been automatically discarded, while in [4], this has been done by visual control the signal quality. They do not give any explanation about the reason of ignoring these signals, nor any quantitative measure about the impact of the signals on the value of the MAE.
4 Discussion
The proposed method leads to acceptable performances in terms of MAE but appears more robust than [4]. Note that our results remain acceptable from a medical point of view, at least to provide an information about the evolution of the blood pressure in such a context of continuous daily monitoring using a smartwatch. The robustness regards to ability of our proposal to process all PPG signals, except the 7 cases which have been automatically discarded. In [4], about 13% of signals (i.e. 4 times more) have been ignored. Moreover, it must be underlined that these irrelevant signals have been manually discarded, based on a visual control of their quality. In our sense, it is crucial not to be too sensitive to signal quality or, at least, to be able to automatically detect irrelevant signals (this being done manually in [4]). This is particularly critical for a use in real conditions (smartwatch), which is not the case for the considered database where signals have been acquired in a controlled environment. This lack of robustness of [4] is probably due to the large number of temporal features to be extracted (12 features), each one with a dedicated algorithm focusing on the detection of some keypoints on the pulse wave. To illustrate this aspect, we have also implemented these features using the method described in [4]: Fig. 6 provides some examples of uncorrectly detected key points on some pulse waves. It has been observed that in many cases, keypoints were uncorrectly recovered, due to the variability of the signal. In our case, the observed robustness is probably due to the fact that, except for the step focusing on the pulse wave detection, our proposal is based on spectral representation of the signal (Fourier transform), and a straightforward measurement of the relation between this representation and the blood pressure (using the Lasso algorithm). Our work is only compared with [4] because of the considered database. Indeed, this recently published database is the only one providing, together with PPG signals, physiological information regarding subjects (this being not the case of other databases such as MIMIC [8]). Such an information has been proved to be required [4] to ensure a better estimation of the blood pressure.
5 Conclusion
IoT-based devices such as smartwatch are really promising systems for the non-invasive daily monitoring of the cardiovascular system in order to prevent diseases such as hypertension. A difficulty is the automatic and robust measurement of physiological parameters for a use in daily routine in real condition, with, for instance, lightening and temperature variations. The proposed method aims at providing such a robust estimation of the blood pressure from the PPG signal. Although providing a slightly larger error than a recent work on this topic, measurements remain useful to provide a trend of the evolution of the blood pressure in a non invasive manner. A strength of this method is its robustness with respect to the quality of the signal, and its ability to automatic ignore irrelevant waves, this being manually done in recent related works. Future steps will focus on the error reduction by integrating other signal features and additional external physiological information.
References
Murray, W.B., Foster, P.A.: The peripheral pulse wave: information overlooked. J. Clin. Monit. 12(5), 365–377 (1996)
Perloff, D., Sokolow, M., Cowan, R.: The prognostic value of ambulatory blood pressures. JAMA 249(20), 2792–2798 (1983)
Perloff, D., Sokolow, M., Cowan, R.: The prognostic value of ambulatory blood pressure monitoring in treated hypertensive patients. J. Hypertens. Suppl.: Official J. Int. Soc. Hypertens. 9(1), S33-9 (1991)
Yang, S., Zhang, Y., Cho, S.Y., Morgan, S.P., Correia, R., Wen, L.: Cuff-less blood pressure measurement using fingertip photoplethysmogram signals and physiological characteristics. In: Optics in Health Care and Biomedical Optics VIII, vol. 10820, p. 1082036. International Society for Optics and Photonics, October 2018
Liang, Y., Elgendi, M., Chen, Z., Ward, R.: An optimal filter for short photoplethysmogram signals. Sci. Data 5, 180076 (2018)
Liang, Y., Chen, Z., Liu, G., Elgendi, M.: A new, short-recorded photoplethysmogram dataset for blood pressure monitoring in China. Sci. Data 5, 180020 (2018)
Efron, B., Hastie, T., Johnstone, I., Tibshirani, R.: Least angle regression. Ann. Stat. 32(2), 407–499 (2004)
Goldberger, A.L., et al.: PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation 101(23), e215–e220 (2000)
O’Brien, E., Waeber, B., Parati, G., Staessen, J., Myers, M.G.: Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ 322(7285), 531–536 (2001)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 ICST Institute for Computer Sciences, Social Informatics and Telecommunications Engineering
About this paper
Cite this paper
Mouney, F., Tiplica, T., Hallab, M., Dinomais, M., Fasquel, JB. (2020). Towards a Smartwatch for Cuff-Less Blood Pressure Measurement Using PPG Signal and Physiological Features. In: Garcia, N., Pires, I., Goleva, R. (eds) IoT Technologies for HealthCare. HealthyIoT 2019. Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering, vol 314. Springer, Cham. https://doi.org/10.1007/978-3-030-42029-1_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-42029-1_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42028-4
Online ISBN: 978-3-030-42029-1
eBook Packages: Computer ScienceComputer Science (R0)