Abstract
As per the World Health Organization, cancer is the second leading cause of death globally and is responsible for an estimated 9.6 million deaths in 2018. More than 2 million cases of lung and breast cancer have been reported in 2018. Paclitaxel is a natural product based anti-mitotic agent useful for the treatment of lung cancer, ovarian cancer and breast cancer. Paclitaxel exhibits low oral bioavailability due to poor aqueous solubility and poor permeability. Paclitaxel is the first blockbuster anticancer drug with annual sales of more than US $1 billion in 1997. Taxol®, Abraxane® and Genexol PM® are commercial injectable preparations of paclitaxel with a drug loading of not more than 17% w/w. The toxicity issues of Cremophor® EL used in Taxol® led to the development of different delivery systems sans Cremophor® EL. The maximum tolerated dose of Taxol® is 135 mg/m2. Taxol® exhibited hypersensitivity reactions and required use of special IVEX-2 filter to avoid leaching of plasticizer into the product. Genexol PM® was physically unstable and was ineffective against multidrug-resistant tumor treatment. Abraxane® exhibited limited tumor exposure, tumor uptake, tumor regression and higher half-maximal inhibitory concentration.
In this chapter, we reviewed the literature of paclitaxel delivery systems. Micelles, liposomes, nanoparticles, lipid systems, microparticles, emulsions, solid dispersions, cyclodextrin complexes, implants, prodrugs and hybrid systems have been reported for paclitaxel delivery. The major points of our analysis of the literature are (1) Efficiency of solubility enhancement of paclitaxel was found in the decreasing order for prodrugs, mixed micelles, cyclodextrin complexes and solid dispersions, (2) The oral bioavailability enhancement for nanoparticles, micelles and emulsions of paclitaxel was found to be 7-fold, 5-fold and 4-fold respectively, (3) Decreasing order of reduction in tumor growth was found in emulsion, liposome, prodrug and nanoparticulate delivery system of paclitaxel as compared to that with Taxol®, (4) Genexol PM® and Abraxane® do not require special filters to avoid leaching of plasticizer into the product, (5) Genexol PM® and Abraxane® being free from Cremophor® EL do not exhibit hypersensitivity reaction, (6) Paclitaxel mixed micelles composed of poly (ethylene glycol-co-lactic acid) and D-α-tocopheryl polyethylene glycol 1000 succinate were effective against multidrug-resistant tumor cells in contrast to Genexol PM®, (7) Recombinant chimeric polypeptide conjugated paclitaxel nanoparticles exhibited 2-fold systemic tumor exposure, tumor uptake as compared to Abraxane® and almost complete tumor regression, (8) Paclitaxel loaded polycaprolactone-co-D-α-tocopheryl polyethylene glycol 1000 succinate nanoparticles exhibited 8-fold lower half maximal inhibitory concentration as compared to Abraxane®, (9) Paclitaxel delivery systems such as implants, nanoparticles, solid dispersions, lipid nanoparticles and micelles have been reported with more than 20% drug loading, (10) The maximum tolerated dose of Genexol PM® and Abraxane® could be increased from 135 mg/m2 to 300 mg/m2, and (11) Orally effective paclitaxel formulations such as DHP107 and Oraxol® are under phase II clinical trials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Paclitaxel is a potent broad-spectrum anticancer drug. Paclitaxel is a diterpenoid molecule with a central 8-member taxane ring. Paclitaxel was initially isolated from the bark of Taxus brevifolia, family: Taxaciae (the Western Yew tree). The pure form of paclitaxel was isolated in 1969. Paclitaxel is used in the treatment of breast, ovarian, lung cancer, head and neck cancer. Paclitaxel belongs to class IV of the biopharmaceutical classification system, the most difficult category for drug delivery.
The year-wise publication trend for paclitaxel delivery as per the SciFinder search engine is given (Fig. 6.1). The publication trend reveals that the number of publications have increased 10 times in the last 20 years.
Year-wise publication trend for paclitaxel delivery; this trend has been obtained from SciFinder search on June 24, 2019 using publication year trend; note the increase of publications for paclitaxel delivery over period of 1997–2019; the publication trend signifies demand for newer delivery options for paclitaxel; the existing paclitaxel commercial products lack safety, targeting to specific organs and patient inconvenience due to injections
Paclitaxel was extracted from the bark of the western yew tree Taxus brevifolia. It was identified as one of the active constituents of this plant in 1967. The structure of the compound was elucidated by Wall and Wani 1996. Its cytotoxic activity was reported against human KB carcinoma cell line and mouse leukemia cells. The availability of the compound was limited because of its low yield from the western yew tree. So, Robert A. Holton and his research group came up with a semi-synthetic pathway by which docetaxel was produced from 10-deacetyl baccatin, which was present in abundant quantities in Taxus baccata (Alqahtani et al. 2019). A synthetic method for paclitaxel using C7 protected baccatin III with tricyclic ketone have been reported (Holton et al. 1994).
6.1.1 Chemical Structure of Paclitaxel
Paclitaxel is a diterpenoid compound containing a taxane ring along with other hydrophobic substituents. The empirical formula of paclitaxel is C47H51NO14. The chemical structure of paclitaxel is given (Fig. 6.2).
Chemical structure of paclitaxel and C7 protected position for synthesis of paclitaxel using baccatin III; paclitaxel was extracted from Yew tree initially hence alternative semi-synthetic method using highly abundant baccatin III in the bark of Taxus wallichiana var. mairei has been discovered by protecting baccatin III at C7 position and coupling tricyclic ketone to yield paclitaxel
IUPAC name of the compound is (1S,2S,3R,4S,7R,9S,10S,12R,15S)-4,12-bis(acetyloxy)-1,9-dihydroxy-15-{[(2R,3S)-2-hydroxy-3-phenyl-3-(phenylformamido) propa -noyl]oxy}-10,14,17,1tetramethyl 11-oxo-6-oxatetracyclo[11.3.1.03,10.04,7]heptadec-13-en-2-yl benzoate (Weaver 2014).
Paclitaxel has a unique mechanism of action which differs from other anticancer agents such as vinca alkaloids. Paclitaxel causes polymerization of microtubule and makes these highly stable. Stabilization of microtubules inhibits cell division leading to cell death (Schiff et al. 1979).
6.1.2 Problems Associated with Paclitaxel
Paclitaxel is practically insoluble in water with an aqueous solubility of 0.00556 mg/mL. Paclitaxel is hydrophobic in nature with a Log P value of 3.54 but has poor permeability. The molecular weight of paclitaxel is 853.9. The high molecular weight of the drug might be responsible for the poor permeability. The consequence of poor solubility and permeability of the drug is poor oral bioavailability. Paclitaxel is a substrate for P-glycoprotein which is responsible for drug efflux. High molecular weight of the drug has been attributed to drug efflux. Paclitaxel belongs to class IV of the biopharmaceutical classification system (Varma et al. 2005).
6.1.3 Marketed Paclitaxel Products
The commercial paclitaxel formulations include Taxol®, Abraxane®, Genexol PM® and Lipusu® (Nehate et al. 2014). The first marketed product of paclitaxel is Taxol®, which was marketed by Bristol-Myers-Squibb in 1992. Taxol® is available in three strengths i.e. 30 mg, 100 mg and 300 mg per vial. Taxol® consists of purified Cremophor® EL, anhydrous citric acid and dehydrated alcohol. Taxol® is indicated as first-line and subsequent therapy of ovarian cancer, for the adjuvant treatment of node-positive breast cancer administered subsequently to standard doxorubicin-containing combination therapy, for the first-line treatment of non-small cell lung cancer along with cisplatin in patients who are not potential candidates for curative surgery and/or radiation therapy and for the second-line treatment of AIDS-related Kaposi’s sarcoma. The major side effects of Taxol® observed in patients are hypersensitivity reaction, low blood counts, hair loss, myalgias, peripheral neuropathy, mouth sores, nausea, vomiting, diarrhoea, swelling of feet, low blood pressure and darkening of the skin. Taxol® injection requires premedication with a steroid to avoid hypersensitivity reaction (Rxlist website 2019).
The main problem associated with Taxol® injection is Cremophor® EL related toxicity. Cremophor® EL is not an inert vehicle and it produces undesirable biological effects. Cremophor® EL can cause a severe anaphylactic reaction (Szebeni et al. 1998). Taxol® needs to be administered using proprietary IVEX-2 filters. IVEX-2 filters avoid leaching of di-(2-ethylhexyl) phthalate in the product. Leaching of di-(2-ethylhexyl) phthalate in the product from polyvinyl chloride container and administration set has been reported. The leaching was attributed to presence of Cremophor® EL and dehydrated alcohol in Taxol® formulation (Kim et al. 2005). The literature has cited a number of research publications for the development of delivery systems without using Cremophor® EL in order to have safer formulation.
Abraxane® is the second commercial product of paclitaxel, which was marketed by Abraxis BioScience in 2005. Abraxane® is composed of drug and human serum albumin and has been prepared by high-pressure homogenization method (Ibrahim et al. 2002). Abraxane® is Cremophor EL®-free formulation and hence does not exhibit hypersensitivity and leaching of plasticizer from polyvinyl chloride. The maximum tolerated dose could be increased from 175 mg/m2 to 300 mg/m2 with Abraxane® as compared to that with Taxol® (Gradishar 2006). Lipusu® was the first liposome-based injection of paclitaxel, formulated by Luye Pharmaceutical Co. Ltd. and was marketed in China. Lipusu® contains paclitaxel, lecithin and cholesterol. Lipusu® was effective against breast cancer, ovarian cancer, lung cancer with fewer side effects than Taxol®.
Genexol-PM® is another injectable polymeric micelle based product of paclitaxel, marketed by Samyang Corporation. Genexol-PM® is a poly (ethylene glycol)-b-poly (lactic acid) block co-polymer based micellar formulation. Genexol-PM® does not require steroid premedication and free from the problem of plasticizer leaching from polyvinyl chloride. Genexol-PM® can deliver 300 mg paclitaxel dose without additional toxicity (Kim et al. 2004). Genexol-PM® was stable at 23 °C for 24 h but exhibited precipitation into large needle-like crystals at 40 °C within 2–4 h (Ron et al. 2008). Genexol-PM® was ineffective in cancer patients with multidrug resistance (Fan et al. 2015)
Nanoxel™ is a micellar paclitaxel formulation composed of a copolymer of n-isopropyl acrylamide and n-vinyl pyrrolidone having a mean particle size of 80 nm. The intracellular accumulation of paclitaxel in A549 cell was found to be 2.5-fold and 3.3-fold higher in Nanoxel™ and Abraxane®-treated cells respectively as compared to that of Taxol®. Nanoxel™ at 0.7 mg/mL showed significant aggregation, particle-size growth, and crystallization within 4 h at 40 °C. High-pressure liquid chromatography data revealed slightly lower purity of paclitaxel in Nanoxel™ as compared to both Abraxane® and Genexol PM®. No drug-related mortality was observed following repeated intravenous administration of Abraxane® at dose levels of 5, 15, and 30 mg/kg, while Nanoxel™ exhibited 100% mortality at 15 and 30 mg/kg dose levels in athymic nude mice (Ron et al. 2008; Madaan et al. 2013; Trieu et al. 2008).
6.1.4 Recent Paclitaxel Products Under Clinical Trials
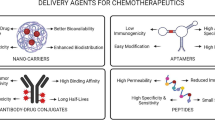
A number of delivery approaches have been reported in the literature to increase the solubility and enhance the antitumor activity of paclitaxel such as micelles, liposomes, nanoparticles, microparticles, solid dispersions, cyclodextrin-drug complex, implants and prodrug. This chapter discusses approaches to paclitaxel delivery. The emphasis is given on choice of material, type of delivery system and performance. Different delivery systems explored for paclitaxel in the literature are discussed in subsequent sections (Fig. 6.3).
Different delivery systems of paclitaxel (a) Micelles: Self-assembled aggregates of polymers or surfactants which have a distinct polar head and non-polar tail region; (b) Liposomes: Spherical vesicular structures, made up of one or more phospholipid bilayers and an aqueous core; (c) PMP/ PNP: Polymeric microparticles/ Polymeric nanoparticles. These are micron sized or nanosized particles made up of a polymeric matrix in which the drug is dispersed or encapsulated or entrapped; (d) Emulsion: Dispersion of two immiscible liquids where the dispersed phase is thoroughly distributed in a dispersion medium with the help of emulsifiers; (e) SLN: Solid lipid nanoparticles, submicron carriers made up of high melting point lipid (solid lipid) core and coated by aqueous surfactant layer; (f) NLC: Nanostructured lipid carriers, also known as second generation SLN, where the solid lipid core is replaced by a mixture of solid lipid and liquid lipid; (g) Inorganic nanoparticle: Inorganic nanoparticles, the core is made up of nanosized inorganic material while the shell is organic, contains drug and/or polymers; (h) Solid dispersion: Dispersion of a drug into a solid, inert matrix of carriers; (i) Hybrid systems: Combination of more than one systems; (j) Implant: Device containing drug, intended to be implanted inside the body; (k) Prodrug: Inactive form of a drug, which is converted to a pharmacologically active form upon metabolism inside the body; (l) CD complex: Cyclodextrin complex, inclusion complex formed by cyclodextrins with drugs; (m) Stent: Metal mesh tube which is implanted in ducts or vessels of the body e.g. coronary artery. Drug-eluting stents are used to deliver drugs to a specific site for a long time
DHP107 is a novel lipid-based mucoadhesive oral paclitaxel formulation composed of an edible lipid and FDA approved emulsifiers. Phase II clinical trial is being conducted for this formulation. The study began on July 25, 2018, and it is expected to be completed by September 2019. The use of the formulation is indicated for metastatic breast cancer (Kang et al. 2018). Another oral formulation of paclitaxel is under phase II clinical trial, named as Oraxol®. Oraxol® consists of paclitaxel and HM30181A, a P-glycoprotein inhibitor. Oraxol® has been found to be well tolerated in patients without any notable hypersensitivity reaction (Lee et al. 2015). The toxicity issues in the existing commercial formulations have led to the development of alternate formulations for paclitaxel.
6.2 Micelle-Based Delivery System
Micelles are nanometre sized structures formed by self-assembly of amphiphilic block copolymers. The hydrophilic part is oriented towards water whereas the hydrophobic portion remains inside the micellar structure (Kwon and Okano 1996). The concentration at which the micelles are formed in water is known as critical micellar concentration. Lower the critical micellar concentration better is the stability of the micelles. The micelles need to be intact for solubilising the hydrophobic drug. Upon ingestion, micelles’ structure may be collapsed due to dilution with aqueous fluids resulting in precipitation of drug. The breakdown of micelles can be avoided by the use of amphiphilic copolymers having a low critical micellar concentration (Owen et al. 2012).
Different amphiphilic polymers have been used in the past for preparation of drug-loaded micelles. These polymers include diblock copolymers such as poly (ethylene glycol)-b-poly (lactide), poly (ethylene glycol)-b- poly (lactide-co-glycolide), etc. Triblock copolymers have also been used for micelle preparation such as poly (ethylene glycol)-poly (ε-caprolactone-co-L lactide) (Wang et al. 2013), monomethoxy poly (ethylene glycol)- poly (caprolactone)-D-α-tocopheryl polyethylene glycol 1000 succinate (Zhang and Zhang 2015). Chitosan has been modified with hydrophobic moieties to form an amphiphilic polymer. These hydrophobic groups include α-tocopherol succinate (Liang et al. 2016), Pluronic F127 (Xu et al. 2015a, b), N-succinyl palmitoyl group (Yuan et al. 2015), N-octyl N-trimethyl group (Zhang et al. 2016), polycaprolactone (Almeida et al. 2018). Serum albumin has been modified with octyl group to make it amphiphilic for micelle preparation (Liu et al. 2011). The schematic of types of paclitaxel micelles are given (Fig. 6.4).
Types of paclitaxel micelles in literature; (a) simple micelle, (b) poly (ethylene glycol)ylated micelle where poly(ethylene glycol) is coated or conjugated to the micelle, (c) targeted micelle; targeting ligands such as folate or hyaluronic acid is conjugated to the micelle, (d) stimuli sensitive micelle; stimuli-responsive i.e. pH/temp/redox-sensitive polymer is conjugated to micelle and (e) functional micelles; functional molecule such as mucoadhesive agent, P-glycoprotein (P-gp) inhibitor or biodegradable polymer is used
6.2.1 Simple Micelle-Based Delivery System
Simple micelles are prepared by using an amphiphilic copolymer. The copolymer may be di or triblock copolymer composed of the hydrophilic and hydrophobic component. Hydrophobically modified serum albumin copolymer was synthesized for preparation of paclitaxel micelles. Serum albumin was chosen as it is endogenously present in the plasma. Serum albumin is biocompatible and nontoxic protein. The reactive primary amino group of albumin was conjugated to octyl chain. The paclitaxel micelles prepared using synthesized octyl conjugated serum albumin exhibited 1.3 times higher drug loading than that of unmodified serum albumin. Octyl group was chosen to enhance interaction between the hydrophobic drug and micelle. In vitro cytotoxicity in Hepg2 cells exhibited a higher percentage of cell viability than Taxol® indicating better safety profile of octyl modified albumin-based paclitaxel micelles (Gong et al. 2009). Lauryl carbamate modified Inulin was used to prepare paclitaxel micelles. Inulin, a hydrophilic carbohydrate offers the advantage of being an alternate for poly(ethylene glycol)ylation, poly(ethylene glycol)ylation and has been found to exhibit production of anti-poly(ethylene glycol) Immunoglobulin M. Paclitaxel micelles of lauryl carbamate modified Inulin exhibited enhanced anticancer activity in mouse melanoma B16F10 cells at half the dose (Muley et al. 2016).
Polyion complex based micelle composed of cationic Pluronic F127 modified chitosan and anionic sodium cholate was reported for paclitaxel delivery. Sodium cholate, a bile salt was chosen to enhance drug loading in the Pluronic based micelles. Pluronic block copolymers are approved by USFDA but have the drawback of low drug loading. The synthesized polymer showed higher drug loading and lower critical micelle concentration. These micelles exhibited inhibition of growth of cancer cells in a drug-resistant MCF7 cell line (Ge et al. 2016). In another report, polyion complex based paclitaxel micelle using Pluronic F127 conjugated chitosan with cysteine was investigated. The polyion complex micelles exhibited four times higher drug loading as compared to Pluronic F127 based micelles. The polyion complex micelles exhibited pH-dependent and sustained release upon oral administration (Xu et al. 2015a, b).
Paclitaxel exhibited poor drug loading in poly (ethylene glycol)-b-poly (ε-caprolactone). Hence, to increase the drug loading, acyl ester bulky prodrugs of paclitaxel were synthesized. The prodrugs were incorporated into poly (ethylene glycol)-b-poly (ε-caprolactone) micelles. The hydrophobic modification of the drug resulted in enhanced solubilization of the prodrug in micelles. These prodrugs exhibited enhancement in drug blood levels as revealed in pharmacokinetics studies in rats. The prodrug micelles not only increased mean residence time and volume of distribution but also sustained the drug release. Chemical modification of the drug resulted in a shift of renal to non-renal clearance of paclitaxel (Forrest et al. 2008).
Paclitaxel micelles prepared using poly (ethylene glycol)-b-poly (lactide) have shown low drug loading. A copolymer of poly (2,4 vinylbenzyloxy)- N, N-diethylnicotinamide) with poly (ethylene glycol) was synthesized and used to prepare paclitaxel micelles. N-N diethylnicotinamide was chosen as a hydrotropic agent. The micelles exhibited 37% by weight drug loading as compared to 27% by weight in poly (ethylene glycol)-b-poly (lactide) micelles. The paclitaxel micelles were stable for 4 weeks at 25 °C whereas there was precipitation of drug in poly (ethylene glycol)-b-poly (lactide) micelles. There was higher antiproliferation of human cancer cells by micelles with synthesized copolymer than poly (ethylene glycol)-b-poly (lactide) micelles (Lee et al. 2007).
6.2.2 Mixed Micelle-Based Delivery System
Mixed micelles utilize two or more polymers to encapsulate the hydrophobic drug in the micelle. The advantages of these over simple micelles include lower critical micelle concentration, higher drug loading and the opportunity to incorporate multiple functionalities in the micellar structure (Attia et al. 2011). Paclitaxel mixed micelles were developed by combining Pluronic P123 with Pluronic F127. The rationale behind such combination relied on co-micellization of these Pluronic grades together during micelle formation. The critical micelle concentration was reduced in mixed micelles as compared to those prepared from Pluronic P123. The mixed micelles reduced half-maximal inhibitory concentration in A549 human lung adenocarcinoma cell lines by 4-fold as compared to Taxol® injection. Mixed micelles exhibited sustained release of paclitaxel. Forty-six percent drug was released after 2 h followed by slow release up to 12 h whereas Taxol® injection released the drug immediately in an aqueous medium containing sodium salicylate by dialysis method at 37 °C and 100 rpm. The mixed micelles exhibited better stability upon 10 times dilution with phosphate buffer solution and storage for 48 h. Ninety percent drug was retained in mixed micelles whereas 35% of the drug was precipitated in Taxol® injection. The precipitation of the drug was attributed to dissociation of the micelles upon dilution in case of Taxol® injection (Wei et al. 2009).
Sterically stabilized mixed micelles of paclitaxel were developed to increase the drug solubilization with lower critical micelle concentration. It was achieved by incorporation of hydrophobic phosphatidylcholine derivative along with poly (ethylene glycol)-g-distearoylphosphatidylethanolamine. The mixed micelles of this graft copolymer exhibited 1000-fold enhancement in paclitaxel solubility. The cytotoxicity study using human breast cancer cell and MCF 7 cell line exhibited comparable cytotoxicity of the mixed micelle with that of 10% paclitaxel solution in dimethyl sulfoxide (Krishnadas et al. 2003). Paclitaxel mixed micelles composed of poly(ethylene glycol-co-lactic acid) and D-α-tocopheryl polyethylene glycol 1000 succinate exhibited higher cellular uptake and effectiveness against multidrug-resistant tumor cells as compared to Genexol PM® (Fan et al. 2015).
Paclitaxel mixed micelles based on Soluplus® and Solutol® HS 15 were prepared for enhancement of drug solubilization. Solutol® HS15 (Murgia et al. 2013) and Soluplus® (Jin et al. 2015) were used in solid dispersions to increase drug solubilization and to prevent drug agglomeration. These mixed micelles exhibited higher plasma concentration in a pharmacokinetic study in Sprague Dawley rats than free paclitaxel. The mixed micelles exhibited higher cytotoxicity than free paclitaxel in MB-231 cell line (Hou et al. 2016). In another study, paclitaxel mixed micelles were prepared by a combination of α- tocopherol polyethylene glycol 1000 succinate and Plasdone® S630. α- tocopherol polyethylene glycol 1000 succinate was chosen for its lower critical micelle concentration of 0.02% w/w and Plasdone® S630® for higher drug solubilization capacity in solid dispersions. The mixed micelles released only 28% drug whereas there was 70% drug release from plain paclitaxel. About 50% drug was released in a sustained manner from mixed micelles upto 50 h. A pharmacokinetic study in Sprague Dawley rats exhibited five times increase in bioavailability of paclitaxel as compared to free paclitaxel. In vitro toxicity study in A459 cells revealed enhanced cytotoxicity of mixed micelles as compared to free paclitaxel (Hou et al. 2017).
6.2.3 Stimuli-Responsive Micelle-Based Delivery System
Micelles which can associate or dissociate with respect to change in stimulus are termed as stimuli-responsive micelles. The stimuli such as variation in pH, oxidation-reduction potential, magnetic field, and ultrasound have been used to fabricate stimuli-responsive micelles. pH-sensitive systems are the most popular among these stimuli since there is a variation in pH of fluids present in the milieu of different sites of the gastrointestinal tract, blood, tumor or body organs. The pH is acidic in the stomach which increases to neutral in the intestine. A pH of 7.4 exists in normal cells whereas it is slightly acidic around tumor cells (Shen et al. 2008). Intracellular and extracellular glutathione concentration varies significantly and hence could be used to trigger an oxidation-reduction reaction (Schafer and Buettner 2001). A pH and oxidation-reduction potential based micelles utilize internal milieu of the human body whereas ultrasound and magnetic field are external stimuli to trigger the release of drug from micelles.
pH-sensitive paclitaxel micelles composed of methoxy poly (ethylene glycol)-b-poly (β-aminoester) were reported. These micelles exhibited 13% and 45% drug release in pH 7.4 and pH 6.0 phosphate buffer solutions respectively after 3 days. The micelles with 16 mg/kg dose exhibited the lowest tumor volume after 10 days of treatment with B16F10 tumor-bearing mice as compared to saline solution (Han et al. 2009).
pH-sensitive paclitaxel micelles using methoxy poly (ethylene glycol)-poly (ε-caprolactone)-D-α-tocopheryl polyethylene glycol 1000 succinate were designed. The purpose of use of biodegradable polycaprolactone core was to dissolve the drug in the core whereas polyethylene glycol could bypass reticuloendothelial system uptake. D-α-tocopheryl polyethylene glycol 1000 succinate was chosen to overcome multidrug resistance. These micelles exhibited complete drug release in pH 5.0 whereas only 60% drug was released in pH 7.4 buffer solution after 140 h. The micelles exhibited higher antitumor activity in A549 cells than the free drug. The pharmacokinetic study in Sprague Dawley rats revealed 4-fold higher bioavailability than the free drug (Zhang and Zhang 2015).
N-octyl-N-(2-carboxyl-cyclohexamethenyl) chitosan-based paclitaxel micelles were investigated. High drug loading of 43.25% w/w was obtained in the micelles with a particle size of 145 nm and low critical micellar concentration of 42 μg/ml. The micelles exhibited pH-sensitive drug release. The pharmacokinetic study in Sprague Dawley mice exhibited longer half-life and a larger volume of distribution than Taxol® (Liu et al. 2011).
Polyethylene glycol-fluorenylmethyoxycarbonyl-disulfide-farnesyl thiosalicylic acid-based paclitaxel micelles were developed for intracellular delivery. Disulfide group was introduced to impart redox-sensitivity to the system. The micelles formed filamentous micelles with 10-fold lower critical micelle concentration values. The drug loading was found to be 34% w/w in the micelles. The micelles exhibited 74% drug release with 10 mM glutathione in release medium but micelles could release only 40% drug in release medium sans glutathione. The intracellular concentration of glutathione is in the millimolar scale whereas it is in the micromolar level outside the cells (Schafer and Buettner 2001). Pharmacokinetics and biodistribution studies revealed more retention of paclitaxel in the bloodstream with accumulation in tumor (Xu et al. 2015a, b).
Thermosensitive multi-arm star-shaped copolymer-based folate decorated paclitaxel micelles were formulated. The micelles were designed using 4-arm block copolymer consisting of poly (N-isopropylacrylamide-co-acrylamide), poly (ε-caprolactone) and folate conjugated methoxy poly (ethylene glycol)/polyethylene glycol. These blocks were chosen for thermosensitive, biodegradable and biocompatible properties respectively. The micelles exhibited temperature-sensitive drug release. The drug release from these micelles was faster at 40 °C than at 37 °C at the end of 100 h. The rationale was based on the fact that temperature in normal cells is ~37.5 °C whereas 40 °C in tumor environment (Rezaei et al. 2012).
Magnetically responsive paclitaxel micelles were designed. The magnetic material used as superparamagnetic iron oxide nanoparticles which were incorporated in poly (N-isopropylacrylamide-r-acrylamide) conjugated to an arginine-glycine-aspartic acid peptide. These micelles were formulated to have dual targeting. The peptide ligand was selected due to its affinity for αvβ3 integrin on cancer cells (Zitzmann et al. 2002) and magnetic force assisted drug release by virtue of iron oxide nanoparticles. The cellular uptake was improved for paclitaxel micelles with peptide in HeLa cells. Incorporation of magnetically responsive material in the micelles exhibited a synergistic effect on cellular uptake in a cell line (Lin et al. 2015).
Paclitaxel micelles based on monomethoxy poly (ethylene glycol)-b-poly (D, L lactide) have increased the maximum tolerated dose to 50 mg/kg from 20 mg/kg for Taxol® in murine B16 melanoma induced female SPF C57 BL/6 mice. This formulation exhibited poor drug internalization (Kim et al. 2001). Howard and coworkers reported local ultrasound-assisted paclitaxel drug internalization from paclitaxel polymeric micelles. Ultrasound enhanced the drug internalization by 20-fold followed by 90% tumor reduction in drug-resistant MCF7/ADmt cell lines (Howard et al. 2006).
6.2.4 Functional Micelle-Based Delivery System
Paclitaxel micelles having specific functionality have been developed in the past. These functionalities include avoidance of multidrug resistance; p-glycoprotein inhibition, biodegradability, mucoadhesive property and the use of carriers with intrinsic anticancer activity. The purpose of functional micelles were to enhance bioavailability, reduce toxicity, and treatment of multidrug-resistant cancer.
P-glycoprotein inhibitors such as brometetradrine (Zhang et al. 2017), N-octyl-N′-phthalyl-O-phosphoryl chitosan derivative (Qu et al. 2019), elacridar (Sarisozen et al. 2012) and Pluronic F127 (Dahmani et al. 2012) were used in compositions of paclitaxel micelles to overcome multidrug resistance. P-glycoprotein causes multidrug resistance by efflux of drug from cells (Gottesman et al. 1996). Various biodegradable polymers such as poly (ethylene oxide)-b-poly (ε-caprolactone) (Cai et al. 2007), block copolymers of poly (ethylene glycol) and poly (lactide) (Yang et al. 2009a, b) and poly (ethylene glycol)-poly (L-lactide)-poly {3(S) methyl-morpholine −2,5 dione} (Zhao et al. 2012) were used to prepare biodegradable paclitaxel micelles. Thioglycolic acid-modified octyl glycol chitosan (Huo et al. 2018) and chitosan grafted polycaprolactone (Almeida et al. 2018) were used to prepare mucoadhesive paclitaxel micelles. Excipients having intrinsic anticancer activity such as Rhein (Wang et al. 2019), methoxy poly(ethylene glycol) conjugated octacosanol (Chu et al. 2016), ethylene glycol-b-dendritic polylysine conjugated phenethyl isothiocyanate (Xiang et al. 2018) and poly (2-ethyl-2 oxazoline) vitamin E succinate and α-tocopherol polyethylene glycol 1000 succinate (Qu et al. 2018) were exploited for preparation of paclitaxel micelles to further substantiate its anticancer activity.
6.2.5 Targeted Micelle-Based Delivery System
Drug delivery to tumor cells can be improved by passive and active targeting of the nanocarriers. Systems that target the systemic circulation can be kept under a passive targeting system. It is a sort of passive process which exploits the natural biodistribution of the carrier and as a result, it eventually accumulates in certain organs, mainly liver and spleen (Yadav et al. 2019). In passive targeting to the tumor, the drug delivery carriers are exploited for their localization in the tumors by enhanced permeation and retention effects, phagocytosis and/or reticuloendothelial system. Nanocarriers having a size between 100 and 800 nm can accumulate in cancer cells due to leaky vasculature of blood vessels and inadequate lymphatic drainage of cancer cells (Iyer et al. 2006).
Active targeting refers to the attachment of certain components to the drug carrier which can direct the system to the target cells. This is based on molecular recognition phenomenon between ligand and receptor. The ligand possesses high affinity for specific receptor or surface determinant that has been overexpressed in the tumor cells. Overexpression of certain receptors like folate, transferrin, lipoprotein can be exploited as a target for cancer targeting. Certain tumor-associated antigens like melanoma-associated antigen, carcinoembryonic antigen, and other antigens e.g. CD44 are also overexpressed in tumor cells (Thanki et al. 2015). Various peptide-based ligands e.g. albumin, Arg-Gly-Asp peptide; carbohydrate-based ligands e.g. β-galactose; vitamin-based ligands e.g. folate; chimeric proteins and antibodies were used for active targeting. Attachments of these ligands or engineered homing devices or antibodies to drug carrier could facilitate the binding of drug carrier to the target cells. The concentration of these surface modifiers should be optimized in order to avoid reticuloendothelial system uptake or interaction with blood components (Kumar Khanna 2012).
Paclitaxel micelles were reported using mixed micelles composed of N-octyl-N′-trimethyl chitosan, poly (ethylene glycol stearate) and heparin sodium (Zhang et al. 2016), peptide ligand for epidermal growth factor receptor conjugated to poly (ethylene glycol)-distearophosphatidylcholine ethanolamine (Ren et al. 2015). Other systems have used dequalinium (Yao et al. 2011) and prostate carcinoma binding peptide 1 (Chen et al. 2016) for mitochondrial and prostate cancer targeting respectively.
Paclitaxel targeted micelles having dual response were designed wherein any two functionalities like pH sensitivity, biodegradability, active targeting and redox sensitivity have been combined. These micelles include folate conjugated poly (ethyleneimine-pluronic) and Pluronic L121 (Xu et al. 2012), Ala-Pro-Arg-Pro-Gly peptide conjugated poly (lactide-co-glycolide)-b-poly (ethylene glycol) copolymer (Guo et al. 2015). Other systems include materials such as hyaluronic acid conjugated deoxycholic acid by a redox-sensitive disulfide bond (Li et al. 2015) and E-selectin binding peptide conjugated hyaluronic acid micelles (Han et al. 2017).
6.2.6 Crosslinked Micelle-Based Delivery System
Micelles structure breaks down causing burst release of drug upon dilution in the body. Crosslinking is used to increase the stability of micelles against such breakdown. Crosslinking enables intactness upon dilution of the micelle (O’Reilly et al. 2006). Core crosslinked paclitaxel micelles for improved stability have been reported using micelles composed of poly (ethylene glycol methyl ether acrylate)-b-poly (carboxyethyl acrylate) by disulfide crosslinking (Du et al. 2016) and crosslinked di/triblock copolymers of methoxy poly (ethylene glycol) and poly (ε-caprolactone) by potassium persulfate (Shuai et al. 2004). The details of various paclitaxel micelles are summarized (Table 6.1).
6.3 Liposomal Delivery System
6.3.1 Simple Liposome-Based Delivery System
Liposomes are spherical vesicular delivery systems composed of phospholipids or other amphiphilic lipids. The advantages of liposomes are bio-compatibility, ease of preparation and applicability for targeted delivery. Liposomes can be used as a drug carrier for both hydrophilic and hydrophobic drugs (Akbarzadeh et al. 2013).
Liposomal paclitaxel formulation composed of soy lecithin and cholesterol were reported. The particle size of liposomes and encapsulation efficiency were found to be 131 ± 30.5 nm and 94.5 ± 3.2% respectively. In-vitro drug release in pH 7.4 phosphate buffer saline was 56% after 96 h. Cytotoxicity study using HeLa cell line exhibited enhanced antitumor efficiency (Nguyen et al. 2017).
6.3.2 Polyethylene Glycolated Liposome-Based Delivery System
Polyethylene glycolation involves coating of poly (ethylene glycol) on liposomes to enhance hydrophilicity and blood circulation time. Liposomes with particle size more than 200 nm are directly taken up by the reticuloendothelial system. The larger particle size of liposomes causes faster elimination of liposomes. The circulation time can be prolonged by poly (ethylene glycol)ylation of liposomes (Sharma and Kumar 2015).
Polyethylene glycolated liposomal formulation of paclitaxel composed of soybean phosphatidylcholine and 1, 2-distearoyl-sn-glycero-3-phosphoethanolamine [methoxy (polyethylene glycol)-2000], Cholesterol, Tween 80 and 3-(4, 5-Dimethyltiazol-2-ly)-2, 5-diphenyl- tetrazolium bromide was reported. This liposomal paclitaxel formulation resulted in enhancement of solubility by 2000 times as compared to conventional liposomes. The pharmacokinetic study on Sprague Dawley rats revealed a 3-fold increase in biological half-life in poly(ethylene glycol)ylated liposomal formulation of paclitaxel (Yang et al. 2007).
6.3.3 Targeted Liposomal Delivery System
The targeted delivery system is a strategy of delivering drugs or medications only to its site of action and not to the other cells, tissues or organs. The concentration of medication is higher in particular cells, tissues or organs as compared to others. Targeting systems have the advantages of improving the therapeutic efficacy and reduction of side effects of drugs (Gupta and Sharma 2011). Passive targeting involves targeting of drugs to the systemic circulation of the body. In this method, drug targeting occurs because of the body’s natural response to physicochemical characteristics of the drug or drug carrier system. Enhanced permeability and retention effect passively target the drug to the tumor cells (Bazak et al. 2014).
Active targeting involves the use of a ligand that has an affinity for specific receptors which are over-expressed in cancerous organs, tissues, and cells. Transferrin, peptides, antibodies, nucleic acids, and their fragments are used as a ligand for active targeting (Atar et al. 2018).
Targeting of paclitaxel liposomal formulation to the lungs composed of phospholipon 90H and Tween-80 were reported. The particle size of liposomes and entrapment efficiency were found to be 8.166 ± 0.459 μm and 92.2 ± 2.56% respectively. These liposomes exhibited 60.26% drug release in 24 h. In vivo pharmacokinetic study in rabbits revealed a 1.6-fold increase in half-life and the significant decrease in plasma clearance than Taxol®. Liposomes of size higher than 8 μm could be the potential carrier for paclitaxel for the treatment of lung cancer (Wei et al. 2014).
Targeting of paclitaxel liposomal formulation to mitochondria composed of triphenyl phosphene, 6-bromohexanoic acid, dicyclohexylcarbodiimide, 4-dimethylamino-pyridine were reported. D- α- tocopheryl poly-ethylene glycol 1000 succinate-triphenylphosphine conjugate was used as the mitochondrial targeting material. The particle size of liposomes and entrapment efficiency were found to be 84.67 ± 0.61 nm and 86.27 ± 3.15% respectively. The liposomes exhibited higher anticancer in-vitro activity in human lung cancer A549 cells. The paclitaxel liposomes could enhance the cellular uptake and were selectively accumulated in mitochondria. The increased uptake of the liposomes enhanced the anticancer efficacy (Zhou et al. 2013).
A targeted paclitaxel liposomal formulation composed of dipalmitoyl phosphatidylcholine, dimyristoyl phosphatidylglycerol/monomethoxy, polyethylene glycol 2000, distearoyl phosphatidylethanolamine and folate-poly(ethylene glycol) 3350-distearyl phosphatidylethanolamine was reported. The particle size of liposomes was found to be 97.1 nm. Cytotoxicity study in the human carcinoma cell line, KB exhibited 4-fold and 2.5-fold lower half maximal inhibitory concentration than non-targeted liposomes and Taxol® respectively. The clearance of Taxol® was 16.5 times higher than folate receptor-targeted liposomes (Wu et al. 2006).
A targeted liposomal paclitaxel formulation composed of dipalmitoyl-sn-glycero-3-phosphocholine and 1, 2-dioleoyl-3-trimethylammonium-propane, and hyaluronic acid was developed. The particle size of liposomes and encapsulation efficiency were found to be 106.4 ± 3.2 nm and 92.1 ± 1.7% respectively. In vitro drug release in pH 7.4 phosphate buffer saline was 95% in 40 h. In vivo antitumor efficacy and biodistribution studies were performed on 4T1 tumour-bearing animal models exhibited higher accumulation of the drug in tumor (Ravar et al. 2016).
6.3.4 Stimuli Sensitive Liposomal Delivery System
Magnetically assisted delivery is a novel approach for delivery of drugs using engineered smart microcarriers which can overcome a number of limitations facing current methods of delivering medicines. The drug is formulated into a pharmaceutically stable formulation which is usually injected through the artery that supplies the target organ or tumor in the presence of an external magnetic field (Koppisetti and Sahiti 2011). Focused ultrasound is a method to increase the permeability of drugs into the blood-brain barrier to promote drug delivery to specific brain regions. It is a potential method of delivery of the drugs into the brain for brain tumors (Burgess et al. 2015).
Focused ultrasound was used to enhance permeation through the blood-brain barrier and blood tumor barrier. 1, 2-dipalmitoyl-sn-glycero-3-phosphocholine, 1, 2-distearoyl-sn-glycero-3-phosphoethanolamine and cholesterol were used to prepare liposomal paclitaxel formulation. Focused ultrasound exposure with a 10 ms pulse length and 1 Hz pulse repetition frequency at 0.64 MPa peak rarefactional pressure was used. In-vivo study in rats showed a 3-fold increase in blood drug level from the ultrasound-assisted liposomal formulation as compared to liposomal paclitaxel formulation (Shen et al. 2017). Paclitaxel loaded magneto liposomes composed of 1, 2-dipalmitoyl-sn-glycero-3-phosphocholine and 1-palmitoyl-2-oleoyl-sn-glycero-3-phospho-rac-glycerol were reported. The encapsulation efficiency of 83 ± 3% was obtained. In-vitro study under magnetic field on HeLa cell line revealed that 89% of cells were killed (Kulshrestha et al. 2012).
6.3.5 Mucoadhesive Liposomal Delivery System
Mucoadhesion is commonly defined as the adhesion between two materials, at least one of which is a mucosal surface. The mucoadhesive property of a delivery system is dependent upon a variety of factors, including the nature of the mucosal tissue and the physicochemical properties of the polymeric formulation (Shaikh et al. 2011).
Mucoadhesive liposomes composed of chitosan, thioglycolic acid and Pluronic F127 were used for paclitaxel oral delivery. The particle size of liposomes was found to be 121.4 nm. In-vivo study on rats revealed a 3-fold higher bioavailability than non-mucoadhesive liposomes. Enhanced mucoadhesion was observed which increased the retention time of the chitosan, thioglycolic acid and Pluronic F127 containing liposomal paclitaxel formulation (Liu et al. 2018).
6.4 Nanoparticle-Based Delivery System
Nanoparticles can be defined as submicron (10–1000 nm) particles or systems derived from polymers, lipids, and/or inorganic materials. Nanoparticle-based systems can overcome some of the limitations associated with conventional cancer therapy (Xin et al. 2017). The limitations include poor solubility of drugs, low specificity to the tumor cells, inability to accumulate in tumor cells, rapid removal of drugs from the systemic circulation and non-specific targeting. Nanoparticles have the potential to increase bioavailability and enhance the delivery of poorly soluble anticancer drugs like paclitaxel (Tran et al. 2017). Due to small size, high surface to volume ratio, ability to modulate drug release and the possibility of surface modification, nanoparticles lead to enhanced accumulation of drugs in tumor cells. Surface modification, use of internal and external stimuli allows selective targeting of drugs to tumor cells. Nanoparticulate systems are also useful to overcome multidrug resistance facilitated by P-glycoprotein efflux pumps in tumor cells (Shi et al. 2017).
6.4.1 Single Nanocarrier Based System
Paclitaxel nanoparticles fabricated using a single polymer have been discussed in this subsection. The carriers can be natural e.g. albumin (Li et al. 2012); semisynthetic e.g. chitosan (Gupta et al. 2017); and synthetic e.g. poly (styrene-co-maleic acid) (Dalela et al. 2015), poly (n-butyl cyanoacrylate) (Huang et al. 2007). Use of biodegradable polymers like poly (lactic-co-glycolic acid) (Le Broc et al. 2013), poly(ε-caprolactone) (Zhu et al. 2010), poly(lactide) (Zhang and Feng 2006) were also reported because of their biocompatibility and non-toxicity. Paclitaxel loaded poly (lactic-co-glycolic acid) nanoparticles were formulated using Poloxamer 188 as a stabilizer. Paclitaxel nanoparticles exhibited sustained release of the drug over a period of 4 days. The formulation was safe for intravenous administration. Pharmacokinetic studies in rats have verified longer retention of drug in the systemic circulation. Mean residence time and plasma half-life were increased by 77 and 45-fold respectively as compared to the pure drug (Mittal et al. 2019).
The chitosan-based biocompatible nanoparticulate system was prepared to achieve better delivery of paclitaxel which has shown burst release followed by sustained release of the drug. The half-maximal inhibitory concentration was reduced by 1.6-fold as compared to the pure drug which was attributed to the higher uptake of nanoparticles. Therapeutic efficacy was induced by apoptosis induction. The drug loading was found to be 11.57% (Gupta et al. 2017). Polygeline has been used as a carrier for paclitaxel delivery. Polygeline based paclitaxel nanoparticles were formulated as a reconstitutable lyophilized powder for intravenous administration. The drug loading was found to be 12.04%. It has shown a relative bioavailability of 89.83% as compared to Abraxane® (Xiong et al. 2019).
6.4.2 Multiple Nanocarriers-Based System
It covers the delivery systems of paclitaxel which contain more than one polymer or carriers. Polymers can remain as separate entities as in the case of layer-by-layer based albumin-bound paclitaxel nanoparticles. The nanoparticle was fabricated by alternate deposition of poly(arginine) and poly (ethylene glycol)-block-poly (L-aspartic acid) onto the drug-albumin conjugate. The drug loading capacity was found to be 48% w/w. The protective layers have improved the colloidal stability as well as biodistribution of albumin-bound paclitaxel nanoparticles. Mean residence time and plasma half-life were increased 5 and 4-fold respectively as compared to albumin-drug conjugate. These multilayer conjugates exhibited enhanced cytotoxicity and apoptosis properties (Ruttala et al. 2017).
Two or more polymers can be copolymerized and loaded with paclitaxel to design paclitaxel loaded nanoparticles. Methoxy poly (ethylene glycol)-poly(ε-caprolactone) nanoparticles loaded with paclitaxel have shown improved anti-glioblastoma activity than Taxol®. The drug loading was found to be 8.2%. High accumulation of the drug in brain cells was observed. The mean survival time was increased to 28 days which was 20 days in Taxol® treated animals. (Xin et al. 2010). Poly (ethylene glycol)ylated poly(ε-caprolactone) based paclitaxel nanoparticles were designed which exhibited similar biodistribution compared to Taxol®. Polyethylene glycol and poly(ε-caprolactone) side chains of the nanoparticles could avoid opsonization (Colombo et al. 2015).
Paclitaxel loaded nanoparticles composed of poly(ε-caprolactone)–co-α-tocopheryl polyethylene glycol 1000 succinate were formulated. The nanoparticles had 6% drug loading. The nanoparticles exhibited sustained drug release over a period of 144 h in pH 7.4 phosphate buffer solution. The half-maximal inhibitory concentration for the nanoparticles was found to be 7.8-fold lower than Abraxane®. In vivo pharmacokinetic study in rats revealed that the half-life was increased by 11 and 1.2-fold as compared to Taxol® and Abraxane® respectively. The formulation could increase the systemic circulation and lower the elimination of drug than its pre-existing marketed formulations (Bernabeu et al. 2014).
6.4.3 Stimuli Sensitive Nanosystem
pH sensitivity can be incorporated into either the corona or core of the nanoparticles. The core-shell type nanoparticles are formulated with pH-dependent solubility and lower critical solution temperature which exhibits drug release at tumor pH (Sutradhar and Amin 2014).
Various polymers have been reported to exhibit pH-responsive release of paclitaxel, such as poly [2-(dimethylamino) ethyl methacrylate-co-methacrylic acid] (Lee et al. 2011), O-carboxymethyl chitosan (Sahu et al. 2011), poly (acrylic acid)-poly(ethylene oxide) (Nguyen et al. 2019), poly(4-vinyl pyridine) (Contreras-Cáceres et al. 2017), poly (lactic acid)-block-poly(ethylenimine) and poly (ethylene glycol)-block-poly (l-aspartic acid sodium salt) (Jin et al. 2018a, b). Chitosan modified poly (lactic-co-glycolic acid) nanoparticles of paclitaxel were designed to overcome the initial burst release of poly (lactic-co-glycolic acid) nanoparticles. The drug loading was found to be 6.42%. Chitosan modified nanoparticles were pH-responsive and have shown faster release in pH 5.5 than at pH 7.4. Enhanced cytotoxicity and cellular uptake in MDA-MB-231 cells were due to chitosan modification (Lu et al. 2019).
Thermoresponsive delivery systems have been explored for paclitaxel where a change in temperature had triggered the release of the drug from the system. A novel thermoresponsive triblock copolymer comprised of methoxy poly (ethylene glycol), poly(octadecanedioicanhydride) and D, L-lactic acid oligomer was developed for paclitaxel delivery. The nanoparticles were formulated as a freeze-dried powder which is suitable for peritumoral or intratumoral injection upon redispersion with water at ambient temperature. The drug loading was found to be 0.90%. Paclitaxel accumulation in tumor cells was enhanced whereas systemic exposure was reduced. Plasma half-life and area under the curve were increased by 4.2 and 1.8-fold respectively as compared to Taxol® in the pharmacokinetic study (Liang et al. 2017).
Paclitaxel conjugated recombinant chimeric polypeptide-based nanoparticles have been reported. The nanoparticles self-assemble into spherical nanoparticles of size below 100 nm. The in vitro dissolution study of the nanoparticles did not release the drug in pH 7.4 phosphate buffer solution but completely released the drug within 6 h in pH 6.5 carbonate buffer solution. The systemic exposure of paclitaxel was increased by 2-fold as compared to that of Abraxane®. The tumor uptake of the nanoparticles was doubled as compared to that with Abraxane®. Abraxane® treated prostate cancer animals could survive less than 60 days, whereas nanoparticle treated animals survived more than 70 days with almost complete tumor reduction (Bhattacharyya et al. 2015).
The reducing environment of tumors serves as a unique internal signal that allows redox-responsive nanoparticles to degrade in tumor cells and release the loaded drug. Rapid drug release can be attributed to the high concentration of glutathione in cancer cells (Guo et al. 2018). Cross-linked polymeric nanocarriers made up of poly (lactic acid) core and glutathione-responsive disulfide cross-linked poly (oligo-ethylene glycol) corona was loaded with paclitaxel. The drug loading capacity was found to be 20%. In vitro release of paclitaxel from the nanoparticles was enhanced in the presence of glutathione in acidic pH. The half-maximal inhibitory concentration showed an 11-fold increase activity in OVCAR-3 cells compared to Taxol® which indicated better antitumor efficacy of the nanoparticles (Samarajeewa et al. 2013).
6.4.4 Functional Polymeric Nanoparticles
Multidrug resistance is the major reason for the failure of conventional anticancer therapy. P-glycoprotein mediated drug efflux from cancer cells is one of the important mechanisms of multidrug resistance (Mansoori et al. 2017). Various nanoparticulate systems of paclitaxel have been formulated to overcome this issue. Paclitaxel was loaded in poly [2-(dimethylamino)-ethyl methacrylate-co-methacrylic acid] to obtain water-soluble nanoparticles. These nanoparticles were able to reverse the multidrug resistance in two p-glycoprotein expressing breast cancer cell lines i.e. MCF/ADR, MT3/ADR cell lines compared to pure paclitaxel. This was due to the uptake of nanoparticles by endocytosis, bypassing the P-glycoprotein efflux pump (Lee et al. 2011).
Poly(lactide)-D-α-tocopheryl polyethylene glycol 1000 succinate copolymer-based nanoparticles of paclitaxel were developed, where D-α-tocopheryl polyethylene glycol 1000 succinate acts as a P-glycoprotein inhibitor. The drug loading was found to be 5.2%. These nanoparticles exhibited much higher in vitro cytotoxicity in HT-29 cells as compared to Taxol® (Zhang and Feng 2006).
P-glycoprotein inhibition potency of tannic acid was used by formulating tannic acid nanoparticles of paclitaxel. Tannic acid has lowered the P-glycoprotein expression; inhibited metastasis, clonogenic formation, proliferation; decreased expression of multidrug-resistant protein; and increased expression of tumor suppressor proteins of MDA-MB-231 breast cancer cells (Chowdhury et al. 2019).
Mucoadhesive polymeric nanoparticles relish localization and prolonged residence at the site of absorption (Boddupalli et al. 2010). Paclitaxel conjugated trimethyl chitosan nanoparticles were developed for oral and intravenous administration of the drug. Intestinal transport of paclitaxel was promoted by the mucoadhesive property of trimethyl chitosan. A pharmacokinetic study in tumor-bearing mice revealed prolong blood retention and improved tumor accumulation of paclitaxel. Further modification of nanoparticles by folic acid has improved the overall antitumor efficacy (He and Yin 2017).
6.4.5 Targeted Polymeric Nanoparticles
Chitosan modified poly (lactic-co-glycolic acid) nanoparticles were loaded with paclitaxel. Chitosan modification produced a positively charged surface which resulted in increased uptake of the nanoparticles into lung cancer cell line A549. Moreover, a lung-specific biodistribution was achieved as compared to Taxol®. The transient formation of aggregates in plasma increased the size of the nanoparticles upon intravenous administration. Electrical interaction between positively charged nanoparticles and negatively charged tumor vasculature enhanced the accumulation of nanoparticles in lung tumor (Yang et al. 2009a, b).
Various active targeting based polymeric nanoparticles have been reported for paclitaxel. Paclitaxel loaded cationized polyacrylamide nanoparticles engineered with recognition peptide VRPMPLQ were designed. The presence of positive charge and the recognition peptide directed the nanoparticles to dysplasia regions in the colon where sialic acid was overexpressed. The uptake of the peptide containing nanoparticles was increased 10-fold as compared to non-peptide nanoparticles (Tiwari et al. 2017). CD44 is a non-kinase transmembrane glycoprotein that is overexpressed in certain cancers like gallbladder cancer, breast cancer and ovarian cancer (Chen et al. 2018). Hyaluronic acid serves as a targeting ligand for overexpressed CD44. Hyaluronic acid decorated serum albumin-based paclitaxel nanoparticles were designed for targeting ovarian cancer cells. The encapsulation efficiency was found to be 90%. The uptake of the nanoparticles was attributed to receptor-mediated endocytosis. A fluorescent dye fluorescein isothiocyanate was labelled to the nanoparticles for in vitro imaging of the tumor. The half-maximal inhibitory concentration was decreased by 4.35-fold in hyaluronic acid conjugated paclitaxel as compared to free paclitaxel (Edelman et al. 2019).
Ganipineni and co-workers have compared passive, active, magnetic and hybrid targeting strategies of paclitaxel for glioblastoma treatment. For passive targeting, paclitaxel and superparamagnetic iron oxide loaded poly (lactic-co-glycolic acid) nanoparticles were formulated. Accumulation of nanoparticles in the U87MG tumor model was due to enhanced permeability and retention effect. Active targeting was based on the fact that αvβ3 integrin is overexpressed in glioblastoma and Arg-Gly-Asp tripeptide was served as a targeting ligand. So, the surface of the nanoparticles was modified with Arg-Gly-Asp to achieve active targeting. The inherent magnetic property of superparamagnetic iron oxide was explored for magnetic targeting. Hybrid targeting was achieved by adding active and magnetic targeting. The best therapeutic effect was obtained in magnetic targeting followed by the hybrid targeting (Ganipineni et al. 2019). The other polymeric nanocarrier based targeted delivery systems of paclitaxel is given (Table 6.2).
6.4.6 Inorganic Nanoparticle-Based System
Inorganic nanoparticles are developed lately in addition to polymeric or organic nanoparticles. Typically, the inorganic nanoparticles are made up of inorganic core and organic shell (Bayda et al. 2018). The core contains metals like iron oxide, gold, aluminium or non-metals like carbon or silica. The shell protects the core from chemical interactions during circulation and/or acts as a substrate for conjugation with biomolecules, such as antibodies, proteins, and oligonucleotides. Inorganic nanoparticles offer good stability and biocompatibility. These can alter the drug release profile and provide the site of attachment for targeting molecules. Additionally, few metallic nanoparticles can also be used for contrast imaging and photodynamic therapy (Núñez et al. 2018).
Paclitaxel was loaded into mesoporous silica nanoparticles of three different pore sizes and was evaluated for in vitro and in vivo antitumor activity. The in vitro release of paclitaxel was dependent on the pore size. Early and late apoptosis was directly proportional to pore size and was boosted as compared to free paclitaxel. Pharmacokinetic parameters were similar to Taxol® (Jia et al. 2013). Paclitaxel was loaded into mesoporous carbon spheres and surface modified by the folate-polyethyleneimine function. The enhanced internalization of nanoparticles by Caco-2 cell lines was due to folate conjugation. The nanoparticles also demonstrated improved oral bioavailability and diminished gastrointestinal toxicity (Wan et al. 2015). Other inorganic nanoparticle-based delivery systems of paclitaxel are given (Table 6.3).
6.4.7 Nanocrystal-Based System
Drug nanocrystals are nanosized, carrier-free, crystalline particles of the drug, usually produced in the form of nanosuspensions and stabilized by surfactants or polymers. Nanocrystals have several advantages over other nanoparticulate systems such as high drug loading capacity, improved solubility, dissolution, stability, and long circulation time. Nanocrystals also enjoy excellent commercialization potentials. So, development of nanocrystals of paclitaxel has gained the interest of researchers in recent years (Lu et al. 2015).
Paclitaxel nanocrystals were prepared using Pluronic F127 as a stabilizer for hyperthermic intraperitoneal chemotherapy of ovarian cancer. The in vitro cytotoxicity against human ovarian carcinoma cell line, SKOV-3, was equivalent to Taxol®. The maximum tolerated dose of the nanocrystals was similar to Taxol® however; the rats treated with the nanocrystals recovered faster after hyperthermic intraperitoneal chemotherapy treatment (De Smet et al. 2012). In another study, Pluronic F127 grafted chitosan copolymer was used as a stabilizer for the development of paclitaxel nanocrystals. Enhanced accumulation of paclitaxel in the Caco-2 cell line as a result of P-glycoprotein inhibitory potential of the stabilizer was observed. The nanocrystals have shown 12.6-fold enhanced absorption as compared to Taxol® (Sharma et al. 2015).
Polyethylene glycol stabilized and Arg-Gly-Asp peptide-functionalized paclitaxel nanocrystals were reported. Nanocrystals were coated with polydopamine which gave a site of attachment to polyethylene glycol and Arg-Gly-Asp peptide. Due to surface modification, the uptake and accumulation of nanocrystals were increased in adenocarcinomic pulmonary cells. In vivo study in pulmonary tumor-bearing mice resulted in enhanced antitumor efficacy in RGD peptide-functionalized paclitaxel nanocrystals as compared to that with Taxol® (Huang et al. 2019).
6.5 Lipid-Based Delivery System
Lipid-based systems possess the advantage of incorporation of the hydrophobic drug in amorphous form. It helps to enhance the solubility of the drugs. It also helps improving permeability by providing lipophilicity to the delivery system. Lipid systems can be prepared using solid lipids or a mixture of solid lipids and liquid lipids. The former is referred to as solid lipid nanoparticles and the later one as nanostructured lipid carriers. Solid lipid nanoparticles, as well as nanostructured lipid carriers of paclitaxel, have been formulated. These include simple lipid-based systems, poly (ethylene glycol)ylated lipid-based systems, oral systems, local systems, pulmonary systems, targeted systems and stimuli-responsive systems.
6.5.1 Simple Lipid-Based Delivery System
Simple lipid-based systems of paclitaxel have been prepared using lipid and surfactants. Paclitaxel nanostructured lipid particles were prepared using fluorescein isothiocynate-octadecylamine using 0.1% Poloxamer 188 aqueous solution by hot melt high-pressure homogenization. The nanoparticles were freeze-dried and were found to have 89 nm size and more than 30 mV zeta potential. The nanoparticles released ~ 80% drug within 48 h but it was about 50% from nanoparticles prepared without octadecyamine. In vitro cellular uptake in A549 cells was found to be higher with octadecylamine nanoparticles (Miao et al. 2015).
In another study, paclitaxel solid lipid nanoparticles composed of trilaurin, phosphotidylcholine were prepared using hot homogenization method. The nanoparticles had a size of ~160 nm. These nanoparticles exhibited sustained release in human plasma over 24 h whereas burst release was observed in Taxol® (Xu et al. 2013).
6.5.2 Lipid-Based Oral Drug Delivery System
Glyceryl monostearate based solid lipid nanoparticles of paclitaxel were prepared by emulsification and evaporation method. Wheat germ agglutinin was conjugated to these solid lipid nanoparticles which exhibited higher cytotoxicity than non-conjugated nanoparticles in A549 cell line. The conjugated nanoparticles exhibited a 2-fold increase of area under the plasma curve and mean residence time during in vivo pharmacokinetic study in rats as compared to the plain drug (Pooja et al. 2016).
6.5.3 Lipid-Based Topical Drug Delivery System
Paclitaxel loaded solid lipid nanoparticles composed of Carbapol 940, stearic acid, egg lecithin and Pluronic PF 68 were reported for topical delivery. Particle size and pH of the formulation were found to be 78 nm and 5.4 respectively. The gel released 70% drug in 24 h in pH 7.4 phosphate buffer solution. The nanoparticle-based gel showed higher permeability through the dialysis membrane than that of plain drug-loaded gel. In vivo study in mice exhibited higher antitumor efficacy (Bharadwaj et al. 2016). Another report for topical delivery of paclitaxel was based on nanostructured lipid carriers composed of glyceryl behenate, capric-caprylic triglycerides mixture with a surfactant cetylpyridinium chloride. The particle size and drug loading were found to be 270–315 nm and 3% respectively. The higher zeta potential of 20 mV was observed. The positive zeta potential helped to increase the permeability of drug through the skin (Tosta et al. 2014).
6.5.4 Lipid-Based Pulmonary Drug Delivery System
Pulmonary lipid nanoparticles are meant for lung cancer treatment. Nanostructure lipid carriers of paclitaxel were designed with a surfactant that can inhibit P-glycoprotein mediated drug efflux. These nanoparticles exhibited sustained release in pH 7.4 phosphate buffer solution. Nanoparticles of Tween 20 exhibited the highest cellular uptake in Caco-2 cell line. In vivo studies of nanoparticles exhibited better therapeutic activity and lung deposition (Kaur et al. 2016).
6.5.5 Lipid-Based Targeted Delivery System
Passive and active targeted lipid-based systems were reported for paclitaxel delivery. Positively charged solid lipid nanoparticles of paclitaxel composed of stearylamine, sodium behenate and polyvinyl alcohol were prepared. These nanoparticles exhibited only 1% drug release after 12 h whereas paclitaxel solution released the drug completely in a phosphate buffer solution with 0.1% v/v Tween 80 solution. Cytotoxicity study in hCMEC/D3 cells exhibited better anticancer activity with improved blood-brain barrier permeation (Chirio et al. 2014). Solid lipid nanoparticles of paclitaxel were prepared using tristearin, hydrogenated soy phosphatidylcholine. The surface of the solid lipid nanoparticles was modified with lactoferrin. The size of nanoparticles and zeta potential were found to be 250 nm and 3.7 mV respectively. Cytotoxicity study in BEAS-2B cell line exhibited a 4-fold reduction in half-maximal inhibitory concentration in lactoferrin conjugate nanoparticles as compared to non-conjugated nanoparticles. In vivo distribution study in albino rats exhibited 1.6-fold higher uptake of the drug as compared to non-targeted nanoparticles (Pandey et al. 2015).
Folate-conjugated poly (ethylene glycol)-cholesteryl hemisuccinate was used to prepare a paclitaxel targeted delivery system. Paclitaxel nanostructured lipid carrier was prepared using oleic acid and stearic acid from the conjugated polymer. Transmission electron microscopy revealed 100 nm size for these carriers. The biodistribution study in albino rats exhibited higher deposition of targeted particles in the kidney (Ucar et al. 2017). Paclitaxel solid lipid nanoparticles prepared using conjugated polymer of Pluronic P85, 1, 2 distearoyl–sn-glycero-3-phosphatidyl-ethanolamine and hyaluronic acid by hot homogenization method were developed. In vitro drug release study revealed complete drug release from the plain drug but the nanoparticles exhibited sustained release up to 48 h in a phosphate buffer solution with 0.5% w/v Tween 80. The targeted nanoparticles exhibited a 4-fold increase in drug concentration in tumor than from free drug in balb/c mice (Wang et al. 2017).
Paclitaxel brain targeted solid lipid nanoparticles were developed. These were composed of transferrin conjugated polyethylene glycol, oleic acid, compritol ATO 888 and cholesterol. These were prepared by the solvent evaporation method. The size of the nanoparticles and drug loading were found to be 160 nm and 8.6% respectively. In vitro release study showed that the drug release was in a sustained manner up to 75 h in pH 7.4 phosphate buffer saline. 6-fold reduction of half maximal inhibitory concentration in HL 60 cells was shown by targeted nanoparticles as compared to non-targeted nanoparticles (Dai et al. 2018).
6.5.6 Lipid-Based Stimuli Sensitive Delivery System
Lipid-based stimuli sensitive delivery systems have been utilized for paclitaxel delivery such as pH-sensitive system, magnetically assisted system, enzyme-dependent system and photosensitive system. Arginine lauryl ester-based cationic nanostructured lipid carriers for paclitaxel were developed. The incorporation of arginine was attributed to the pH-sensitive behaviour of the system. These cationic nanocarriers were further coated with bovine serum albumin to increase their blood circulation time by charge masking. The size of these coated carriers was below 100 nm. These carriers exhibited 60–65% drug release at 5.4 pH buffer but released only ~35% drug at physiological pH of 7.4 buffer saline with 0.1% Tween 80. Biodistribution studies in tumor-bearing mice revealed higher retention time and tumor targeting from these carriers as compared to Taxol® injection (Li et al. 2012).
Magnetically assisted paclitaxel solid lipid nanoparticles containing magnetite and glyceryl monostearate were investigated. The melting point reduction from 56 to 43 °C was observed after the formation of solid lipid nanoparticles. Magnetic hyperthermia assisted drug release occurs as a response to altered temperature upon magnetic field change (Moros et al. 2019). The size of these nanoparticles was found to be 277 nm. The nanoparticles released drug faster at 43 °C but only 20% at room temperature. Magnetic hyperthermia-induced more than 75% drug release from these nanoparticles whereas only 10% drug was released from normal nanoparticles (Oliveira et al. 2018).
Enzyme cleavable paclitaxel solid lipid nanoparticles were prepared using soy phosphatidylcholine and glyceryl monostearate. These were fabricated by conjugation of polyethylene glycol-conjugated peptide that is cleaved by a metalloprotease. These nanoparticles exhibited sustained drug release over a period of 200 h in pH 7.4 phosphate buffer with 0.1% Tween 80 at 37 °C. These nanoparticles exhibited higher cytotoxicity in the HT1080 cell line as compared to Taxol®. In vivo pharmacokinetic study of these nanoparticles in C57BL/6 N mice after incorporation of a fluorophore, dioctadecyl-3, 3, 3′, 3′-tetramethylindodicarbocyanine and 4-chlorobenzesulfonate salt exhibited 50% fluorescence after 10 h post-injection. The unmodified solid lipid nanoparticles were cleared within 4 h of injection in mice (Zheng et al. 2014).
Photosensitive paclitaxel solid lipid nanoparticles composed of a photosensitive material aluminum 1,8,15,22 tetrakis (phenylthio) 29H, 31H-phthalocyanine soy phosphatidylcholine, Pluronic F68 and ascorbic acid were prepared. These nanoparticles exhibited drug release as a consequence of the breakdown of lipids by near-infrared light of 730 nm wavelength. The half-maximal inhibitory concentration of these nanoparticles was 20-fold reduced than Taxol® in A549 cells (Meerovich et al. 2019).
6.6 Microparticulate Delivery System
Microparticles are defined as particulate dispersions or solid particles with a size in the range of 1–1000 μm. The drug is entrapped or encapsulated in a micro-particulate matrix. Microparticles are prepared by spray drying, emulsion polymerization, solvent evaporation, and fluidized bed coating. This microencapsulation strategy gives protection of the drug from the environment, stabilization of sensitive drug substances and masking of unpleasant taste. Hence, microparticles can play an essential role for sustained release, controlled release, enhancing bioavailability and reducing side effects of drugs (Madhav and Kala 2011).
6.6.1 Biodegradable Microparticle-Based Delivery System
Biodegradable polymers comprised of monomers linked to one another through functional groups and have unstable links in the backbone. They are degraded into biologically acceptable molecules in the body. Some common examples of biodegradable polymers are poly (glycolic acid), poly (ε-caprolactone), poly (lactic-co-glycolic acid), chitin, cellulose and alginic acid (Vroman and Tighzert 2009).
Biodegradable paclitaxel microparticles composed of poly (D, L-lactide) were reported. The particle size of microparticles and encapsulation efficiency were found to be 4.6 μm and 90% respectively. Cytotoxicity study using U251 human glioma cells exhibited a 70% reduction in cell viability after 120 h (Song et al. 2010).
Biodegradable paclitaxel composite microparticles composed of poly (lactic-co-glycolic acid) have been reported. The yield and entrapment efficiency were found to be 73.06 ± 1.94% and 29.27 ± 1.09% respectively. Cytotoxicity study revealed that paclitaxel loaded Poly (lactic-co-glycolic acid)-silica microparticles exhibited higher cytotoxicity than those without silica in HeLa cancer cells (Nanaki et al. 2017).
6.6.2 Targeted Microparticles-Based Delivery System
Paclitaxel microparticles composed of Pluronic F-127, Poly (ethylene glycol)-2000 and stearic acid were reported for passive targeting. The particle size of microparticles and encapsulation efficiency were found to be 1.76 ± 0.37 μm and 94.73% respectively. The microparticles exhibited higher cytotoxicity in an in vitro study using SKOC-3 ovarian cancer cells than Taxol® (Han et al. 2019). Paclitaxel loaded microparticles composed of folic acid, chitosan and 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyl tetrazolium bromide were used for active targeting. Folic acid-containing microparticles of paclitaxel showed higher cytotoxicity than unmodified microparticles in L929 cells (Wang et al. 2016).
6.6.3 Stimuli Sensitive Microparticles-Based Delivery System
Stimuli are a state of responsiveness to sensory stimulation or excitability. Stimuli sensitive systems deal with the changes in the physiology of the body with respect to the environment changes. These systems are beneficial for the controlled and sustained delivery of the drug in the body (Bhardwaj et al. 2015). Stimuli responsible drug release can be changed in pH, temperature and magnetic field. Magnetically assisted delivery is a novel approach for delivery of drugs using engineered smart microcarriers which overcome a number of limitations facing current methods of delivering medicines. The drug is formulated into a pharmaceutically stable formulation which is usually injected through the artery that supplies the target organ or tumor in the presence of an external magnetic field (Koppisetti and Sahiti 2011).
Thermosensitive paclitaxel microparticles composed of chitosan, poly (lactide-co-glycolide), polyvinyl alcohol were developed. The particle size of microparticles was 6.38 ± 0.13 μm. These microparticles showed 63.0% reduction in tumor volume in M-234p BALB/c tumor model in comparison with non-thermosensitive microparticles (Pesoa et al. 2018). Magnetic assisted paclitaxel delivery from microparticles composed of magnetite, poly (lactic-co-glycolic acid) and polyvinyl alcohol was investigated. The particle size of microparticles and drug loading were found to be 0.7 to 5 μm and 38% respectively. In-vitro study in MESSA human uterine sarcoma cells showed 5% enhancement in cell killing from magnetic assisted microparticles as compared to Taxol® (Hamoudeh et al. 2008).
6.7 Emulsion-Based Delivery System
Emulsions are liquid biphasic systems in which one phase is dispersed in another immiscible phase. Emulsions are stabilized by the aid of emulsifying agents. This delivery system can be utilized for administration of poorly water-soluble drugs (Goodarzi and Zendehboudi 2019). Microemulsions can be defined as a thermodynamically stable, isotropically clear dispersion of two immiscible liquids. Globule size of microemulsion ranges from 10 to 200 nm. Microemulsions are stabilized by a mixture of surfactants namely, surfactant and co-surfactant (Lawrence and Rees 2000). On the other hand, nanoemulsions are kinetically stable, isotropically clear systems containing two immiscible liquids. The globule size ranges from 50 to 500 nm (Jaiswal et al. 2015). Microemulsions are formed by self-assembly whereas nanoemulsions are formed by mechanical shear. Emulsions can be administrated by oral or parenteral routes.
6.7.1 Simple Emulsion-Based Delivery System
Simple emulsions are made up of a single lipid or a blend of lipid or oil, an emulsifying agent and water. Paclitaxel oleate, a prodrug of paclitaxel, was incorporated in a phospholipid-based oil-in-water emulsion. The oil phase was comprised of egg phosphatidylcholine, triolein, dipalmitoyl phosphatidylethanolamine and stabilized by polysorbate 80 and oleyl chloride. Upon intravenous administration of the emulsion in rabbits, improved biodistribution and cytotoxicity was obtained as compared to Taxol® (Lundberg et al. 2003).
Two microemulsions of paclitaxel were prepared composed of lecithin, butanol, myvacet oil, water and capmul, myvacet oil, water respectively. Both of the systems were less cytotoxic and less hemolytic as compared to commercial Taxol®. A comparatively higher amount of drug i.e. 12 mg paclitaxel per gram of emulsion could be loaded in the microemulsions due to the high solubility of paclitaxel in the oil phase (Nornoo and Chow 2008). The microemulsions have shown the slow and sustained release of the drug as compared to Taxol®. In vivo pharmacokinetic study in rats after intravenous administration revealed that plasma half-life and biodistribution were improved as compared to Taxol® (Nornoo et al. 2008).
Paclitaxel incorporated nanoemulsion of paclitaxel was designed using medium-chain triglyceride as oil phase and Tween 80 as a surfactant. The half-maximal inhibitory concentration of paclitaxel was reduced by 18.82 times in drug-resistant MCF7 cells which indicated that paclitaxel resistance was reversed due to P-glycoprotein inhibition. Tumor volume became 10.06% in microemulsion treated animal models, as compared to paclitaxel solution (Bu et al. 2014).
Tocosol™ is a tocopherol-based formulation of paclitaxel, manufactured by Bayer Schering Pharma. The product failed in phase III clinical trial. Abu-Fayyad and his co-workers have designed an emulsion-based formulation, similar to Tocosol™ but substituting the tocopherol with tocoretinol. The shell of the emulsion was made up of polyethylene glycol and tocoretinol. Cytotoxicity of the nanoemulsion was checked on PANC-1 cells and Bx-PC-3 cells. The new system displayed better results than Tocosol™ along with a reduction in the half-maximal inhibitory concentration value (Abu-Fayyad et al. 2018).
6.7.2 Emulsion-Based System for Targeted Delivery
Emulsion-based systems can be passively or actively targeted to tumor cells. A series of lipid nanoemulsion of paclitaxel was prepared by taking medium and long-chain glycerides, oleic acid as oil phase, Tween 80 and polyethylene glycol as a surfactant. The nanoemulsions have shown stronger cytotoxicity against MCF7 cells. In vivo study in mice revealed that the nanoemulsion had improved biodistribution and intratumor accumulation than Taxol®. The improved activity was correlated to enhanced permeability and retention effect (Chen et al. 2017a, b).
Hyaluronic acid serves as a targeting ligand for CD44 overexpressing cancer cells. Hyaluronic acid-coated nanoemulsion, loaded with paclitaxel was prepared for the treatment of ovarian cancer. D, L-α-tocopheryl acetate, soybean oil was taken as oil phase whereas polysorbate 80 was used as a surfactant. The drug loading was found to be 3.75%. Cell affinity studies in SK-OV-3 and OVCAR-3 cells revealed that hyaluronic acid coated nanoemulsion had 10 times higher targeting ability than uncoated nanoemulsion (Kim and Park 2017).
6.7.3 Self Emulsifying Drug Delivery System
Self emulsifying drug delivery systems are made up of a mixture of oil, surfactant, solvents and can be administrated orally by encapsulating in gelatin capsules. After reaching the gastrointestinal tract, these systems form macro or microemulsions. These systems can protect drugs which are prone to enzymatic hydrolysis in the gastrointestinal tract. It results in the enhanced oral bioavailability of poorly soluble drugs (Gursoy et al. 2003).
A series of self-microemulsifying oily formulations were evaluated for their potential for oral delivery of paclitaxel. The self-emulsifying formulations were made up of different concentrations of paclitaxel, D-alpha tocopheryl polyethylene glycol 1000 succinate, tyloxapol, ethanol, docusate sodium and cyclosporin A. In vivo study in P-glycoprotein knockout mice and wild type mice revealed that bioavailability of paclitaxel was similar to Taxol® after oral administration of the formulations. Efficacy of the formulations was improved due to the presence of cyclosporin A and a P-glycoprotein inhibitor (Oostendorp et al. 2011).
Paclitaxel loaded self-nanoemulsifying drug delivery system was developed using tocopheryl polyethylene glycol succinate as oil; labrasol as a surfactant; lauroglycol 90 as co-surfactant and ethanol as co-solvent. It showed higher cytotoxicity in MDA-MB-231 cells than Taxol®. Drug release from the self-nano emulsifying system has shown sustained release. Survivin, a member of the inhibitor of apoptosis family, was downregulated by the system due to the presence of tocopheryl polyethylene glycol succinate. Its oral bioavailability was 4-fold higher than Taxol® (Meher et al. 2018).
6.8 Solid Dispersion-Based Delivery System
Solid dispersions are a dispersion of drug in the amorphous polymeric matrix. The purpose of solid dispersions is to enhance drug solubility and to stabilize the drug (Huang and Dai 2014). Paclitaxel solid dispersion composed of hydroxypropyl β-cyclodextrin, polyvinyl pyrrolidone, α-tocopherol and polyoxyl 40 hydrogenated castor oil prepared by a supercritical antisolvent process which exhibited a 3-fold increase in solubility as compared to Taxol®. This solid dispersion exhibited higher tumor growth inhibition as compared to Taxol® up to 90 days in female athymic nude mice bearing MDA-MB-231 cancer (Shanmugam et al. 2011). In another study, solid dispersion of paclitaxel referred to as Modrapac001 formulation which was prepared from polyvinyl pyrrolidone K30 and sodium lauryl sulfate. This ternary solid dispersion exhibited a multifold increase in drug dissolution (Moes et al. 2013).
6.9 Cyclodextrin-Based Delivery System
Cyclodextrins are cyclic oligosaccharides of glucose having α-1, 4 glycosidic bonds. It has 6, 7 or 8 units present in α, β and γ derivatives respectively. Cyclodextrins have truncated cone shape wherein the inner cavity is hydrophobic and the outer surface is hydrophilic. Water-insoluble molecules can be incorporated into the hydrophobic cavity of cyclodextrins and they enhance the solubility and/or stability of the molecule. pH-sensitive paclitaxel nanoparticles were prepared using acetylated α-cyclodextrin by oil/water solvent evaporation method. These nanoparticles exhibited faster release i.e. 83% in 8 h in pH 5.0 but slower drug release in pH 7.4 phosphate buffer. The cellular uptake in B16F10 cells exhibited complete cellular uptake within 4 h from pH-sensitive nanoparticles. These nanoparticles exhibited better effectiveness in tumor inhibition in vivo in the melanoma-bearing nude mouse model than the plain drug itself (He et al. 2013).
Poly (anhydride) oral nanoparticles containing a complex of paclitaxel in β-cyclodextrin were developed. The drug loading was negligible with the drug per se but it was increased 2 to 4-fold after complexation of the drug in the nanoparticles. These nanoparticles exhibited 83% relative bioavailability with respect to Taxol® in rats. Hence, these nanoparticles could be useful for parenteral to oral switch of paclitaxel (Agüeros et al. 2010). In another study, when paclitaxel was incorporated into 2, 6 dimethyl β-cyclodextrin complex, the solubility was increased to 2.3 mM (Hamada et al. 2006).
Poly (acrylic acid)-co-β-cyclodextrin was used to prepare paclitaxel nanoparticles. The nanoparticles exhibited 170 nm size and 100-fold solubility enhancement. The nanoparticles showed sustained release at pH 7.4 phosphate buffer over a period of 120 days. In vivo imaging in mice for these nanoparticles revealed their accumulation in the tumor for 144 h due to enhanced permeability and retention effect. In vivo antitumor study in H22 tumor-bearing mice exhibited higher antitumor activity and 50 days of survival time than that of Taxol® (Yuan et al. 2016).
Folate-conjugated cyclodextrin nanoparticles of paclitaxel were used for targeted delivery to tumor cells. Cytotoxicity study in the 4T cell line exhibited higher cytotoxicity than that of Taxol®. The survival rate of these nanoparticles was longer than that of Taxol® in 4T cell-bearing mice (Erdoğar et al. 2018).
6.10 Implant-Based Drug Delivery System
Implants are sterile solid masses consisting of a drug made by compression or moulding. These provide a controlled delivery of drug over a period of time at the site of implantation. Implantation can be done under the skin into the subcutaneous tissue called subcutaneous implant. Two types of implants are available such as biodegradable and non-biodegradable implants. Implants are prepared by compression, moulding or extrusion. The advantages are controlled drug delivery with the minimized side effects (Zaki et al. 2012).
6.10.1 Biodegradable Implant
The advantages of biodegradable systems include polymers used in implants are inert and are converted into nontoxic components such as carbon dioxide and water. There is no need for surgical removal of implants after the therapy. The polymers used in biodegradable implants are polylactic acid, poly (lactide-co-glycolide) and chitosan (Rajgor et al. 2011).
Biodegradable implants of paclitaxel composed of poly (ε-caprolactone), polyethylene glycol 6000 were reported. The drug loading was found to be 93%. In vitro study showed 79% drug release after 30 days in pH 7.4 phosphate buffer saline (Hiremath et al. 2013). Biodegradable chitosan-based film implants of paclitaxel composed of chitosan, lysozyme, Tween 80 and Poloxamer 407 were reported. The drug loading and in vitro release in pH 7.4 phosphate buffer saline after 6 h were 31% and 10% respectively. In vivo study using Swiss mice revealed that the implant was biodegradable as it lost the integrity and identity after 50 days (Dhanikula and Panchagnula 2004). Biodegradable microfiber implants of paclitaxel composed of poly (D, L lactide-co-glycolide) were investigated. The drug loading and encapsulation efficiency were found to be 8.92% and 98% respectively. In vitro release study showed 16% drug release after 9 days in pH 7.4 phosphate buffer saline (Ranganath and Wang 2008).
Biodegradable stent coating to paclitaxel implants composed of poly (lactic-co-glycolic acid) and poly (vinyl alcohol)-graft-poly (lactic-co-glycolic acid) were reported. The drug loading was found to be 10%. In vitro release study showed 64% drug release after 48 days in pH 7.4 phosphate buffer saline (Westedt et al. 2006).
6.10.2 Non-biodegradable Implant
Non-biodegradable implants are used to administer medications. It is useful for patients who need treatment for chronic diseases. These implants need to be removed surgically once the medication has been released. These implants are not designed to be metabolized by the body. These implants start to work immediately upon insertion and can continue releasing drug doses in a controlled manner over the years. The polymers used in non-biodegradable implants are poly (methyl methacrylate), thermoplastic polyurethane and poly (ethylene vinyl acetate (Stewart et al. 2018).
Non-biodegradable stent implants of paclitaxel composed of poly (methyl methacrylate), 316 L stainless steel stents; poly (n-butyl methacrylate) and poly (ethylene-co-vinyl acetate) were reported. In vitro study showed 60% drug release after 14 days in pH 7.4 phosphate buffer solution (Shaulov et al. 2009). In another study, non-biodegradable stent implants of paclitaxel composed of 316 L stainless steel stents, N-(2-carboxyethyl) pyrrole and butyl ester of N-(2-carboxyethyl) pyrrole were reported. In vitro study showed 50% drug release after 30 days in pH 7.4 phosphate buffer solution (Okner et al. 2009).
6.10.3 Site-Specific Implant-Based Delivery System
Targeting to a particular organ or site is a smart approach for delivery of biologically active agents. It enhances the therapeutic efficacy of the drugs and reduces the drug concentration in non-target organs or sites. It can be very useful for the delivery of anticancer drugs to a particular site (Himri and Guaadaoui 2018).
Urinary tract tumor-specific implant of paclitaxel composed of poly(ε-caprolactone) resin PCL 787, alginic acid sodium salt, and gelatin were reported. In vitro release study exhibited complete drug release after 72 h in pH 5.5 artificial urine solution. In-vitro study in T24 cell line revealed the half-maximal inhibitory concentration of 7.3 ng/ml after 72 h. The tumor growth inhibition from paclitaxel implant was 75% in T24 cells (Barros et al. 2016).
Ovarian tumor-specific implant of paclitaxel composed of chitosan, phosphatidylcholine and 3-(4, 5- dimethyl-2-thiazolyl)-2, 5-diphenyl-[2H]-tetrazolium bromide) was reported. In-vitro study in SKOV-3 cells showed half-maximal inhibitory concentration of 0.211 μm/mL of these paclitaxel implant (Ho et al. 2005).
The tracheal tumor-specific implant of paclitaxel composed of Carbopol 974P, ethylene-vinyl acetate was reported. Carbapol 974P was chosen for mucoadhesive effect in the trachea. In vitro release study showed 77% drug release after 85 days in pH 7.8 phosphate buffer solution with 0.5% sodium dodecyl sulfate (Jin et al. 2018a, b).
6.10.4 Stimuli Sensitive Implant
Stimuli sensitive paclitaxel implants composed of poly (D, L lactide-co-glycolide), polyethylene glycol and Tween 80 were reported. The irradiation was performed using Cobalt 60 isotope to enhance the drug release. In vitro study showed 10% drug release after 6 h in pH 7.2 phosphate buffer solution (Wang et al. 2003).
6.10.5 In-Situ Forming Implants
In-situ implants are a potential alternative strategy to preformed implants and they avoid surgery. They are injected as a low viscous solution and transform in the body to a gel or solid depot due to phase separation or lowered solubility (Kempe and Mäder 2012). The in-situ forming implant of paclitaxel composed of polyethylene glycol, trimethylene carbonate and glycolide was reported. In vivo study of this implant in the mouse flank model exhibited higher antitumor efficacy than that of Taxol® (Olbrich et al. 2012). In situ forming injectable paclitaxel implant composed of n-butyl-2-cyanoacrylate and ethyl oleate was reported. It was based on the sol-gel transition. In vitro drug release in pH 7.4 sodium salicylate solution exhibited 25% from the implant versus 91% from Taxol® after 6 days. Fifty percent of the implant was degraded in female ICR mice after 8 weeks and hence it was biodegradable. The tumor inhibition in mice bearing human MDA-MB-231 was 80% whereas it was 44% in Taxol® treated mice (Wu et al. 2017).
6.11 Prodrug-Based Delivery System
The prodrug is defined as an inactive form of a drug, which is converted to a pharmacologically active form upon metabolism inside the body. Various prodrugs of paclitaxel have been designed in order to alter its physicochemical properties to make it suitable for delivery systems.
6.11.1 Small Molecule-Based Prodrug Delivery System
Small molecules such as malic acid, squalene and silicate-based prodrugs of paclitaxel have been developed in the past. The hydrophilic prodrug of paclitaxel was synthesized by incorporation of dihydroxyl derivative using solketal chloroformate. The prodrug exhibited pH-sensitive hydrolysis at the acidic condition. The prodrug exhibited 50 times higher water solubility than the unmodified drug. The prodrug exhibited a 2.5-fold higher maximum tolerable dose as compared to the unmodified drug in Balb/c mice (Niethammer et al. 2001). Silicate ester prodrugs of paclitaxel were synthesized and loaded into poly (ethylene glycol)-b-poly(lactide-co-glycolide) nanoparticles by using flash nanoprecipitation method. The drug loading was found to be 74%. The silicate ester was sensitive to acidic condition leading to hydrolysis followed by drug release. These prodrugs exhibited a 10-fold reduction in half-maximal inhibitory concentration in the cell lines (Han et al. 2015).
The lipidic prodrug of paclitaxel was prepared with lipophilic squalenoyl derivative to increase its lipid affinity. The prodrug was further converted into multilamellar vesicles using 1,2-dimyristoyl-sn-glycero-3-phosphocholine. The prodrug could enhance the loading of the drug into vesicles (Sarpietro et al. 2012).
6.11.2 Peptide-Based Prodrug Delivery System
Peptides such as octreotide and Ac-Cys-Arg-Gly-Asp-Arg-NH2 (Papas et al. 2007) have been used to prepare paclitaxel prodrugs. Octreotide based paclitaxel prodrug was prepared to increase the hydrophilicity of the drug that resulted in 20,000 times solubility enhancement in water than an unmodified drug. The prodrug exhibited sustained drug release over a period of 168 h and faster drug release in acidic pH. In vitro cytotoxicity study in NCI-H446 cells revealed 2.6-fold lower half maximal inhibitory concentration for the octreotide prodrug as compared to the unmodified drug. In vivo antitumor growth inhibition study in NCI-H446 xenograft model exhibited 1.22 times higher antitumor effect of peptide prodrug than that of Taxol® (Huo et al. 2015).
6.11.3 Polymer-Based Prodrug Delivery System
The drug is attached to the polymer chemically either directly or via a spacer. The nature of the polymer and spacer determines the site of release of the drug from the prodrug and its release kinetics (Ringsdorf 1975). The molecular weight of the polymer should be up to 40,000 Da to aid the filtration by kidneys (Hoste et al. 2004). Poly-(γ-L-glutamyl glutamine) conjugate of paclitaxel was developed which showed a 3-fold reduction of tumor growth in NCI-H460 human lung cancer cells than Abraxane® (Feng et al. 2010). Oligo (lactide)8-paclitaxel prodrug composed of poly (ethylene glycol)-b-poly (D, L lactic acid) was reported. Paclitaxel loaded into poly (ethylene glycol)-b-poly (lactic acid) exhibited the issue of stability and faster elimination from the body. In vitro cytotoxicity study in 4T1-Luc breast cancer cells for the drug-loaded synthesized polymer exhibited lower half maximal inhibitory concentration than the plain drug (Tam et al. 2019).
6.11.4 Targeted Prodrug Delivery System
The targeted prodrug of paclitaxel composed of folic acid, distearoyl phosphatidylcholine, triolein cholesteryl oleate and polyethylene glycol was reported. In vitro study showed 10% drug release after 24 h in pH 7.4 phosphate buffer solution. In-vitro study in KB, M109 and CHO cell line revealed higher cytotoxicity compared to Taxol®. In vivo antitumor efficacy in Balb/c mice revealed that folic acid conjugated with paclitaxel containing cholesteryl oleate exhibited higher antitumor efficacy compared to Taxol® (Stevens et al. 2004).
The targeted prodrug of paclitaxel composed of hyaluronic acid, diphenylphosphinic chloride, adipic acid dihydrazide and succinic anhydride was synthesized. In vitro study in H22 cell line revealed higher cytotoxicity compared to paclitaxel alone. In vivo antitumor study in H22 tumor-bearing mice revealed a 4-fold decrease in tumor growth compared to paclitaxel alone (Xu et al. 2015a, b).
Arg-Gly-Asp peptide-based targeting of paclitaxel prodrug composed of poly (lactic-co-glycolic acid), 1-ethyl-3- (3-dimethylaminopropyl) carbodiimide, Soybean lecithin and 3, 3′-dithiodipropionic acid was prepared. In vivo antitumor study in lung tumor-bearing mice revealed peptide modified paclitaxel had higher antitumor efficacy compared to free paclitaxel (Wang et al. 2018).
6.11.5 Stimuli-Sensitive Prodrug Delivery System
Prodrug based pH-sensitive paclitaxel micelles prepared using poly (ethylene glycol), 2-hydroxyethyl vinyl ether and acryloyl chloride was reported. The drug loading capacity was found to be 60.3%. In vitro study in HeLa and MDA-MB-231 cells exhibited higher antitumor activity in poly (ethylene glycol) conjugated paclitaxel compared to paclitaxel alone (Huang et al. 2018).
The photosensitive prodrug of paclitaxel composed of folic acid and polyethylene glycol was reported. The prodrug of paclitaxel was activated by the far-red light. In vitro study in SKOV-3 cells exhibited folic acid conjugated and photosensitive prodrug of paclitaxel with polyethylene glycol exhibited more cytotoxicity than non-conjugated paclitaxel (Thapa et al. 2017).
The redox-sensitive prodrug of paclitaxel composed of methoxy polyethylene glycol amine, N-hydroxysuccinimide, 4-dimethylaminopyridine and 3, 3′-dithiodipropionic acid was reported. These polymeric paclitaxel conjugates were structurally confirmed by 1H NMR and exhibited an approximately 23,000-fold increase in water solubility over parent paclitaxel. In vivo studies on NCI-H466 tumor-bearing nude mice exhibited that redox-sensitive prodrug of paclitaxel conjugates possessed superior tumor targeting ability and antitumor activity compared to Taxol® (Yin et al. 2015).
6.12 Hybrid Delivery System
Liposomes, micelles, polymeric nanoparticles, and lipid-based nanoparticles are some of the most explored delivery systems for paclitaxel. Each of these systems exhibit some inherent problems. Difficulties allied to these systems can be minimized by combining two or more of these systems which can be defined as a hybrid drug delivery system.
Bao and co-workers have developed such a hybrid system by combining gold nanoparticles and liposomes. A thiol-terminated polyethylene glycol-paclitaxel derivative was covalently attached on the surface of gold nanoparticles followed by the incorporation of the conjugate in the phospholipid bilayer region of the liposomes. Due to this, the drug loading was increased to 50.4%. In vitro study exhibited 50% drug release in 7.4 pH phosphate buffer solutions. The hybrid system exhibited prolonged circulation of the drug and increased accumulation in the liver as compared to Taxol®. Improved pharmacokinetic properties of the system were attributed to the protective shell of the liposomes (Bao et al. 2014).
In another study, hybrid liposomes were prepared by incorporating paclitaxel loaded polyionic micelles. The micelles were made up of positively charged Pluronic F127- poly (ethyleneimine) copolymer and negatively charged sodium cholate whereas the liposomes were composed of phospholipid. The drug loading of the final system was found to be 5.45%. It was able to sustain the release of paclitaxel. Cellular uptake of the system by multidrug-resistant breast cancer cells was significantly higher which can be attributed to the P-glycoprotein inhibitory potential of Pluronic F127. Formation of liposome not only allowed intestinal absorption of paclitaxel but also stabilized the drug from gastric degradation. The absolute oral bioavailability of paclitaxel in hybrid liposomes was found to be 37.91% (Li et al. 2017a, b, c).
Silica coated liposomes of paclitaxel were developed by Ingle and co-workers, named as liposils. Stability study of 6 months revealed that the liposils were more stable than corresponding liposomes. In vitro release study showed silica coating was able to retard the drug release from the liposils. The liposils also exhibited in vivo release of paclitaxel over a longer duration than corresponding liposomes and Taxol®. Biodistribution study in B16F10 cells revealed that accumulation of liposils and liposomes was significantly higher in the tumor cells as compared to that of Taxol® (Ingle et al. 2018).
6.13 Miscellaneous Delivery System
Miscellaneous drug delivery systems for paclitaxel based on dendrimer, exosomes, dry powder inhalations, and hydrogels are discussed in this subsection.
6.13.1 Dendrimer-Based Delivery System
Dendrimer-based paclitaxel delivery composed of methoxy polyethylene glycol-succinimidyl carboxymethyl ester, N-ethyl diisopropylamine, poly (amidoamine), α-tocopheryl succinate and polyethylene glycol was reported. The diameter and entrapment efficiency were found to be 31.19 ± 0.07 nm and 78.33 ± 2.81% respectively. In vitro study showed 63.97% drug release after 36 h in pH 7.4 phosphate buffer saline. In vitro cytotoxicity study in B16F10 and MDA MB231 cells demonstrated that the paclitaxel loaded methoxy polyethylene glycol-succinimidyl carboxymethyl ester, N-ethyl diisopropylamine, poly (amidoamine), α-tocopheryl succinate and polyethylene glycol exhibited higher cytotoxicity compared to free paclitaxel (Bhatt et al. 2019).
Dendrimer-based paclitaxel delivery composed of azido-cyanine 5.5, N, N-diisopropylethylamine, and N, N, N′, N′-tetramethyl – (1H-benzotriazol-1-yl) uranium hexafluorophosphate was reported. The diameter and drug content were found to be 74 nm and 20.9% respectively. In vitro cytotoxicity study in 4T1, 3T3 and C2C12 exhibited higher cytotoxicity than paclitaxel injection (Li et al. 2017a, b, c).
6.13.2 Dry Powder Inhalation-Based Drug Delivery
Dry powder inhalation formulation based on paclitaxel micelles composed of folic acid, polyethylene glycol and dextran was reported. The particle size and entrapment efficiency of the micelles were found to be 57 ± 2 nm and 99 ± 2% respectively. In vitro release study from the micelles showed 70% drug release after 24 h in pH 5.0 phosphate buffer. In-vitro study of the micelles in M109-HiFR cell line revealed 2-fold reduction of the half-maximal inhibitory concentration as compared to that of Taxol®. The formulation exhibited a fine particle fraction upto 50% with good redispersibility in physiological buffer (Rosière et al. 2016).
6.13.3 Exosomes
Exosomes of paclitaxel isolated from raw milk of Jersey cows were reported. The particle size and loading efficiency were found to be 108 nm and 8% respectively. In vitro study showed 90% drug release after 48 h in pH 5.0 fed-state simulated-gastric fluid. In vivo antitumor efficacy of exosomes of paclitaxel using athymic nude mice bearing subcutaneous lung cancer A549 xenografts exhibited higher cytotoxicity compared to paclitaxel alone (Agrawal et al. 2017).
6.13.4 Hydrogel-Based Delivery System
Thermosensitive hydrogel formulation of paclitaxel composed of chitosan, β-glycero phosphate and sodium dodecyl sulfate. In vitro release study showed 92% drug release after 30 days in pH 7.4 phosphate buffer saline. In vivo antitumor efficacy of hydrogel formulation of paclitaxel in EMT-6 tumors implanted subcutaneously on Balb/c mice exhibited 4-fold higher efficacy than Taxol® (Ruel-Gariépy et al. 2004).
Self-assembled paclitaxel hydrogel of composed of folic acid, hydroxyl benzotriazole, alkaline phosphatise and 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide was reported. The hydrodynamic diameter and zeta potential were found to be 137.3 ± 15.2 nm and 43.8 ± 3.2 mV respectively. In vitro study in HepG2 cells exhibited higher cytotoxicity compared to free paclitaxel. In vivo antitumor study in nude mouse model exhibited enhanced anticancer efficacy compared to free paclitaxel. In vivo real-time imaging further demonstrated that the hydrogel preferentially accumulated in tumor site (Shu et al. 2017).
6.14 Conclusion
Poor solubility and permeability of Paclitaxel have compelled formulation scientists to commercialize it as injectable products such as Taxol®, Genexol PM®, and Abraxane®. Newer delivery systems like micelles, nanoparticles, liposomes, lipid systems that can overcome the issues associated with the commercial products of paclitaxel have been discussed. Some of these systems have utilized specific materials to impart stimuli sensitivity, targeting or functionality. The highest solubility enhancement has been shown by prodrugs, mixed micelles, cyclodextrin complexes and solid dispersions for paclitaxel. Drug loading could be increased in implants, nanoparticles, emulsions and lipid systems of paclitaxel. Implant and cyclodextrin complexes of paclitaxel exhibited sustained release characteristics for a prolonged period of time. The half-maximal inhibitory concentration of paclitaxel was reduced substantially in the case of micelles, emulsions, nanoparticles. Enhancement in oral bioavailability was found to be best in nanoparticles. More efficient tumor growth inhibition was found in cases of emulsion, liposome, prodrug and nanoparticulate delivery system as compared to that with Taxol®. Non-invasive oral systems of paclitaxel such as DHP107 and Oraxol® are under clinical evaluation.
References
Abu-Fayyad A, Kamal MM, Carroll JL, Dragoi AM, Cody R, Cardelli J, Nazzal S (2018) Development and in-vitro characterization of nanoemulsions loaded with paclitaxel/γ-tocotrienol lipid conjugates. Int J Pharm 536(1):146–157. https://doi.org/10.1016/j.ijpharm.2017.11.062
Agrawal AK, Aqil F, Jeyabalan J, Spencer WA, Beck J, Gachuki BW, Alhakeem SS, Oben K, Munagala R, Bondada S, Gupta RC (2017) Milk-derived exosomes for oral delivery of paclitaxel. Nanomedicine 13(5):1627–1636. https://doi.org/10.1016/j.nano.2017.03.001
Agüeros M, Zabaleta V, Espuelas S, Campanero MA, Irache JM (2010) Increased oral bioavailability of paclitaxel by its encapsulation through complex formation with cyclodextrins in poly (anhydride) nanoparticles. J Control Release 145(1):2–8. https://doi.org/10.1016/j.jconrel.2010.03.012
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, Samiei M, Kouhi M, Nejati-Koshki K (2013) Liposome: classification, preparation, and applications. Nanoscale Res Lett 8(1):102. https://doi.org/10.1186/1556-276X-8-102
Almeida A, Silva D, Gonçalves V, Sarmento B (2018) Synthesis and characterization of chitosan-grafted-polycaprolactone micelles for modulate intestinal paclitaxel delivery. Drug Deliv Transl Res 8(2):387–397. https://doi.org/10.1007/s13346-017-0357-8
Alqahtani FY, Aleanizy FS, El ET, Alkahtani HM, AlQuadeib BT (2019) Paclitaxel. Profiles Drug Subst Excip Relat Methodol 44:205–238. https://doi.org/10.1016/bs.podrm.2018.11.001
Atar K, Eroğlu H, Çalış S (2018) Novel advances in targeted drug delivery. J Drug Target 26(8):633–642. https://doi.org/10.1080/1061186X.2017.1401076
Attia ABE, Ong ZY, Hedrick JL, Lee PP, Ee PLR, Hammond PT, Yang YY (2011) Mixed micelles self-assembled from block copolymers for drug delivery. Curr Opin Colloid Interface Sci 16(3):182–194. https://doi.org/10.1016/j.cocis.2010.10.003
Bao Y, Guo Y, Zhuang X, Li D, Cheng B, Tan S, Zhang Z (2014) D-α-tocopherol polyethylene glycol succinate-based redox-sensitive paclitaxel prodrug for overcoming multidrug resistance in cancer cells. Mol Pharm 11(9):3196–3209. https://doi.org/10.1021/mp500384d
Barros AA, Browne S, Oliveira C, Lima E, Duarte ARC, Healy KE, Reis RL (2016) Drug-eluting biodegradable ureteral stent: new approach for urothelial tumors of upper urinary tract cancer. Int J Pharm 513(1–2):227–237. https://doi.org/10.1016/j.ijpharm.2016.08.061
Bayda S, Hadla M, Palazzolo S, Riello P, Corona G, Toffoli G, Rizzolio F (2018) Inorganic nanoparticles for cancer therapy: a transition from lab to clinic. Curr Med Chem 25(34):4269–4303. https://doi.org/10.2174/0929867325666171229141156
Bazak R, Houri M, El Achy S, Hussein W, Refaat T (2014) Passive targeting of nanoparticles to cancer: a comprehensive review of the literature. Mol Clin Oncol 2(6):904–908. https://doi.org/10.3892/mco.2014.356
Bernabeu E, Helguera G, Legaspi MJ, Gonzalez L, Hocht C, Taira C, Chiappetta DA (2014) Paclitaxel-loaded PCL–TPGS nanoparticles: in vitro and in vivo performance compared with Abraxane®. Colloids Surf B: Biointerfaces 113:43–50. https://doi.org/10.1016/j.colsurfb.2013.07.036
Bharadwaj R, Das PJ, Pal P, Mazumder B (2016) Topical delivery of paclitaxel for treatment of skin cancer. Drug Dev Ind Pharm 42(9):1482–1494. https://doi.org/10.3109/03639045.2016.1151028
Bhardwaj A, Kumar L, Mehta S, Mehta A (2015) Stimuli-sensitive Systems-an emerging delivery system for drugs. Artif Cells Nanomed Biotechnol 43(5):299–310. https://doi.org/10.3109/21691401.2013.856016
Bhatt H, Rompicharla SVK, Ghosh B, Biswas S (2019) α-tocopherol succinate anchored poly(ethylene glycol)ylated poly (Amidoamine) Dendrimer for the delivery of paclitaxel: assessment of in vitro and in-vivo therapeutic efficacy. Mol Pharm. https://doi.org/10.1021/acs.molpharmaceut.8b01232
Bhattacharyya J, Bellucci JJ, Weitzhandler I, McDaniel JR, Spasojevic I, Li X, Lin CC, Chi JTA, Chilkoti A (2015) A paclitaxel-loaded recombinant polypeptide nanoparticle outperforms Abraxane in multiple murine cancer models. Nat Commun 6:7939. https://doi.org/10.1038/ncomms8939
Boddupalli BM, Mohammed ZN, Nath RA, Banji D (2010) Mucoadhesive drug delivery system: an overview. J Adv Pharm Technol Res 1(4):381–387. https://doi.org/10.4103/0110-5558.76436
Bu H, He X, Zhang Z, Yin Q, Yu H, Li Y (2014) A TPGS-incorporating nanoemulsion of paclitaxel circumvents drug resistance in breast cancer. Int J Pharm 471(1–2):206–213. https://doi.org/10.1016/j.ijpharm.2014.05.039
Burgess A, Shah K, Hough O, Hynynen K (2015) Focused ultrasound-mediated drug delivery through the blood–brain barrier. Expert Rev Neurother 15(5):477–491. https://doi.org/10.1586/14737175.2015.1028369
Cai S, Vijayan K, Cheng D, Lima EM, Discher DE (2007) Micelles of different morphologies—advantages of worm-like filomicelles of PEO-PCL in paclitaxel delivery. Pharm Res 24(11):2099–2109. https://doi.org/10.1007/s11095-007-9335-z
Chen H, Wu F, Li J, Jiang X, Cai L, Li X (2016) DUP1 peptide modified micelle efficiently targeted delivery paclitaxel and enhance mitochondrial apoptosis on PSMA-negative prostate cancer cells. Springerplus 5(1):362. https://doi.org/10.1186/s40064-016-1992-0
Chen FY, Zhang Y, Chen XY, Li JQ, Xiao XP, Yu LL, Tang Q (2017a) Development of a hybrid paclitaxel-loaded arsenite nanoparticle (HPAN) delivery system for synergistic combined therapy of paclitaxel-resistant cancer. J Nanopart Res 19(4):155. https://doi.org/10.1007/s11051-017-3848-0
Chen L, Chen B, Deng L, Gao B, Zhang Y, Wu C, Yu N, Zhou Q, Yao J, Chen J (2017b) An optimized two-vial formulation lipid nanoemulsion of paclitaxel for targeted delivery to tumor. Int J Pharm 534(1–2):308–315. https://doi.org/10.1016/j.ijpharm.2017.10.005
Chen C, Zhao S, Karnad A, Freeman JW (2018) The biology and role of CD44 in cancer progression: therapeutic implications. J Hematol Oncol 11(1):64. https://doi.org/10.1186/s13045-018-0605-5
Chirio D, Gallarate M, Peira E, Battaglia L, Muntoni E, Riganti C, Biasibetti E, Capucchio MT, Valazza A, Panciani P, Lanotte M (2014) Positive-charged solid lipid nanoparticles as paclitaxel drug delivery system in glioblastoma treatment. Eur J Pharm Biopharm 88(3):746–758. https://doi.org/10.1016/j.ejpb.2014.10017.
Chowdhury P, Nagesh PK, Hatami E, Wagh S, Dan N, Tripathi MK, Khan S, Hafeez BB, Meibohm B, Chauhan SC, Jaggi M (2019) Tannic acid-inspired paclitaxel nanoparticles for enhanced anticancer effects in breast cancer cells. J Colloid Interface Sci 535:133–148. https://doi.org/10.1016/j.jcis.2018.09.072
Chu B, Qu Y, Huang Y, Zhang L, Chen X, Long C, He Y, Ou C, Qian Z (2016) Poly(ethylene glycol)-derivatized octacosanol as micellar carrier for paclitaxel delivery. Int J Pharm 500(1–2):345–359. https://doi.org/10.1016/j.ijpharm.2016.01.030.
Colombo C, Morosi L, Bello E, Ferrari R, Licandro SA, Lupi M, Ubezio P, Morbidelli M, Zucchetti M, D’Incalci M, Moscatelli D (2015) PEGylated nanoparticles obtained through emulsion polymerization as paclitaxel carriers. Mol Pharm 13(1):40–46. https://doi.org/10.1021/acs.molpharmaceut.5b00383
Contreras-Cáceres R, Leiva MC, Ortiz R, Díaz A, Perazzoli G, Casado-Rodríguez MA, Melguizo C, Baeyens JM, López-Romero JM, Prados J (2017) Paclitaxel-loaded hollow-poly (4-vinylpyridine) nanoparticles enhance drug chemotherapeutic efficacy in lung and breast cancer cell lines. Nano Res 10(3):856–875. https://doi.org/10.1007/s12274-016-1340-2
Dahmani FZ, Yang H, Zhou J, Yao J, Zhang T, Zhang Q (2012) Enhanced oral bioavailability of paclitaxel in pluronic/LHR mixed polymeric micelles: preparation, in vitro and in vivo evaluation. Eur J Pharm Sci 47(1):179–189. https://doi.org/10.1016/j.ejps.2012.05.015
Dai Y, Huang J, Xiang B, Zhu H, He C (2018) Antiproliferative and apoptosis triggering potential of paclitaxel-based targeted-lipid nanoparticles with enhanced cellular internalization by transferrin receptors—a study in leukemia cells. Nanoscale Res Lett 13(1):271. https://doi.org/10.1186/s11671-018-2688-x
Dalela M, Shrivastav TG, Kharbanda S, Singh H (2015) pH-sensitive biocompatible nanoparticles of paclitaxel-conjugated poly (styrene-co-maleic acid) for anticancer drug delivery in solid tumors of syngeneic mice. ACS Appl Mater Interfaces 7(48):26530–26548. https://doi.org/10.1021/acsami.5b07764
De Smet L, Colin P, Ceelen W, Bracke M, Van Bocxlaer J, Remon JP, Vervaet C (2012) Development of a nanocrystalline paclitaxel formulation for HIPEC treatment. Pharm Res 29(9):2398–2406. https://doi.org/10.1007/s11095-012-0765-x
Dhanikula AB, Panchagnula R (2004) Development and characterization of biodegradable chitosan films for local delivery of paclitaxel. AAPS J 6(3):88–99. https://doi.org/10.1208/aapsj060327
Di Mauro PP, Cascante A, Vilà PB, Gómez-Vallejo V, Llop J, Borrós S (2018) Peptide-functionalized and high drug loaded novel nanoparticles as dual-targeting drug delivery system for modulated and controlled release of paclitaxel to brain glioma. Int J Pharm 553(1–2):169–185. https://doi.org/10.1016/j.ijpharm.2018.10.022
Du AW, Lu H, Stenzel M (2016) Stabilization of paclitaxel-conjugated micelles by cross-linking with cystamine compromises the antitumor effects against two-and three-dimensional tumor cellular models. Mol Pharm 13(11):3648–3656. https://doi.org/10.1021/acs.molpharmaceut.6b00410
Edelman R, Assaraf YG, Slavkin A, Dolev T, Shahar T, Livney YD (2019) Developing body-components-based theranostic nanoparticles for targeting ovarian cancer. Pharmaceutics 11(5):216. https://doi.org/10.3390/pharmaceutics11050216
Erdoğar N, Esendağlı G, Nielsen TT, Esendağlı-Yılmaz G, Yöyen-Ermiş D, Erdoğdu B, Sargon MF, Eroğlu H, Bilensoy E (2018) Therapeutic efficacy of folate receptor-targeted amphiphilic cyclodextrin nanoparticles as a novel vehicle for paclitaxel delivery in breast cancer. J Drug Target 26(1):66–74. https://doi.org/10.1080/1061186X.2017.1339194
Fan Z, Chen C, Pang X, Yu Z, Qi Y, Chen X, Liang H, Fang X, Sha X (2015) Adding vitamin E-TPGS to the formulation of Genexol-PM: specially mixed micelles improve drug-loading ability and cytotoxicity against multidrug-resistant tumors significantly. PLoS One 10(4):e0120129
Feng Z, Zhao G, Yu L, Gough D, Howell SB (2010) Preclinical efficacy studies of a novel nanoparticle-based formulation of paclitaxel that out-performs Abraxane. Cancer Chemother Pharmacol 65(5):923–930. https://doi.org/10.1007/s00280-009-1099-1
Forrest ML, Yáñez JA, Remsberg CM, Ohgami Y, Kwon GS, Davies NM (2008) Paclitaxel prodrugs with sustained release and high solubility in poly (ethylene glycol)-b-poly (ε-caprolactone) micelle nanocarriers: pharmacokinetic disposition, tolerability, and cytotoxicity. Pharm Res 25(1):194–206. https://doi.org/10.1007/s11095-007-9451-9
Ganipineni LP, Ucakar B, Joudiou N, Riva R, Jérôme C, Gallez B, Danhier F, Préat V (2019) Paclitaxel-loaded multifunctional nanoparticles for the targeted treatment of glioblastoma. J Drug Target:1–10. https://doi.org/10.1080/1061186X.2019.1567738
Gao Y, Hu L, Liu Y, Xu X, Wu C (2019) Targeted delivery of paclitaxel in liver cancer using hyaluronic acid functionalized mesoporous hollow alumina nanoparticles. Biomed Res Int 2019:10. https://doi.org/10.1155/2019/2928507
Ge Y, Zhao Y, Li L (2016) Preparation of sodium cholate-based micelles through non-covalent bonding interaction and application as oral delivery systems for paclitaxel. Drug Deliv 23(7):2555–2565. https://doi.org/10.3109/10717544.2015.1028604.
Gong J, Huo M, Zhou J, Zhang Y, Peng X, Yu D, Zhang H, Li J (2009) Synthesis, characterization, drug-loading capacity and safety of novel octyl modified serum albumin micelles. Int J Pharm 376(1–2):161–168. https://doi.org/10.1016/j.ijpharm.2009.04.033
Goodarzi F, Zendehboudi S (2019) A comprehensive review on emulsions and emulsion stability in chemical and energy industries. Can J Chem Eng 97(1):281–309. https://doi.org/10.1002/cjce.23336
Gottesman MM, Pastan I, Ambudkar SV (1996) P-glycoprotein and multidrug resistance. Curr Opin Genet Dev 6(5):610–617
Gradishar WJ (2006) Albumin-bound paclitaxel: a next-generation taxane. Expert Opin Pharmacother 7(8):1041–1053. https://doi.org/10.1517/14656566.7.8.1041
Guo P, Song S, Li Z, Tian Y, Zheng J, Yang X, Pan W (2015) In vitro and in vivo evaluation of APRPG-modified angiogenic vessel targeting micelles for anticancer therapy. Int J Pharm 486(1–2):356–366. https://doi.org/10.1016/j.ijpharm.2015.03.067
Guo X, Cheng Y, Zhao X, Luo Y, Chen J, Yuan WE (2018) Advances in redox-responsive drug delivery systems of tumor microenvironment. J Nanobiotechnol 16(1):74. https://doi.org/10.1186/s12951-018-0398-2
Gupta M, Sharma V (2011) Targeted drug delivery system: a review. Res J Chem Sci 1(2):135–138. https://doi.org/10.22159/ijap.2017v9i6.22556.
Gupta U, Sharma S, Khan I, Gothwal A, Sharma AK, Singh Y, Chourasia MK, Kumar V (2017) Enhanced apoptotic and anticancer potential of paclitaxel loaded biodegradable nanoparticles based on chitosan. Int J Biol Macromol 98:810–819. https://doi.org/10.1016/j.ijbiomac.2017.02.030
Gursoy N, Garrigue JS, Razafindratsita A, Lambert G, Benita S, Bloom DR (2003) Excipient effects on in vitro cytotoxicity of a novel paclitaxel self-emulsifying drug delivery system. J Pharm Sci 92(12):2411–2418. https://doi.org/10.1002/jps.10501
Hamada H, Ishihara K, Masuoka N, Mikuni K, Nakajima N (2006) Enhancement of water-solubility and bioactivity of paclitaxel using modified cyclodextrins. J Biosci Bioeng 102(4):369–371. https://doi.org/10.1263/jbb.102.369
Hamoudeh M, Diab R, Fessi H, Dumontet C, Cuchet D (2008) Paclitaxel-loaded microparticles for intratumoral administration via the TMT technique: preparation, characterization, and preliminary antitumoral evaluation. Drug Dev Ind Pharm 34(7):698–707. https://doi.org/10.1080/03639040701842444
Han JK, Kim MS, Lee DS, Kim YS, Park RW, Kim K, Kwon IC (2009) Evaluation of the anti-tumor effects of paclitaxel-encapsulated pH-sensitive micelles. Macromol Res 17(2):99–103. https://doi.org/10.1007/BF03218661
Han J, Michel AR, Lee HS, Kalscheuer S, Wohl A, Hoye TR, McCormick AV, Panyam J, Macosko CW (2015) Nanoparticles containing high loads of paclitaxel-silicate prodrugs: formulation, drug release, and anticancer efficacy. Mol Pharm 12(12):4329–4335. https://doi.org/10.1021/acs.molpharmaceut.5b00530
Han X, Dong X, Li J, Wang M, Luo L, Li Z, Lu X, He R, Xu R, Gong M (2017) Free paclitaxel-loaded E-selectin binding peptide modified micelle self-assembled from hyaluronic acid-paclitaxel conjugate inhibit breast cancer metastasis in a murine model. Int J Pharm 528(1–2):33–46. https://doi.org/10.1016/j.ijpharm.2017.05.063
Han S, Dwivedi P, Mangrio FA, Dwivedi M, Khatik R, Cohn DE, Si T, Xu RX (2019) Sustained release paclitaxel-loaded core-shell-structured solid lipid microparticles for intraperitoneal chemotherapy of ovarian cancer. Artif Cells Nanomed Biotechnol 47(1):957–967. https://doi.org/10.1080/21691401.2019.1576705
He R, Yin C (2017) Trimethyl chitosan based conjugates for oral and intravenous delivery of paclitaxel. Acta Biomater 53:355–366. https://doi.org/10.1016/j.actbio.2017.02.012
He H, Chen S, Zhou J, Dou Y, Song L, Che L, Zhou X, Chen X, Jia Y, Zhang J, Li S (2013) Cyclodextrin-derived pH-responsive nanoparticles for delivery of paclitaxel. Biomaterials 34(21):5344–5358. https://doi.org/10.1016/j.biomaterials.2013.03.068
Himri I, Guaadaoui A (2018) Cell and organ drug targeting: types of drug delivery systems and advanced targeting strategies. In: Nanostructures for the engineering of cells, tissues and organs, pp 1–66. https://doi.org/10.1016/B978-0-12-813665-2.00001-6
Hiremath JG, Khamar NS, Palavalli SG, Rudani CG, Aitha R, Mura P (2013) Paclitaxel loaded carrier based biodegradable polymeric implants: preparation and in vitro characterization. Saudi Pharm J 21(1):85–91. https://doi.org/10.1016/j.jsps.2011.12.002
Ho EA, Vassileva V, Allen C, Piquette-Miller M (2005) In vitro and in vivo characterization of a novel biocompatible polymer–lipid implants system for the sustained delivery of paclitaxel. J Control Release 104(1):181–191. https://doi.org/10.1016/j.jconrel.2005.02.008
Holton RA, Somoza C, Kim HB, Liang F, Biediger RJ, Boatman PD, Shindo M, Smith CC, Kim S (1994) First total synthesis of taxol. 1. Functionalization of the B ring. J Am Chem Soc 116(4):1597–1598. https://doi.org/10.1021/ja00083a066
Hoste K, De Winne K, Schacht E (2004) Polymeric prodrugs. Int J Pharm 277(1–2):119–131. https://doi.org/10.1016/j.ijpharm.2003.07.016
Hou J, Sun E, Sun C, Wang J, Yang L, Jia XB, Zhang ZH (2016) Improved oral bioavailability and anticancer efficacy on breast cancer of paclitaxel via Novel Soluplus®—Solutol® HS15 binary mixed micelles system. Int J Pharm 512(1):186–193. https://doi.org/10.1016/j.ijpharm.2016.08.045
Hou J, Sun E, Zhang ZH, Wang J, Yang L, Cui L, Ke ZC, Tan XB, Jia XB, Lv H (2017) Improved oral absorption and anti-lung cancer activity of paclitaxel-loaded mixed micelles. Drug Deliv 24(1):261–269. https://doi.org/10.1080/10717544.2016.1245370
Howard B, Gao Z, Lee SW, Seo MH, Rapoport N (2006) Ultrasound-enhanced chemotherapy of drug-resistant breast cancer tumors by micellar-encapsulated paclitaxel. Am J Drug Deliv 4(2):97–104
Huang Y, Dai WG (2014) Fundamental aspects of solid dispersion technology for poorly soluble drugs. Acta Pharm Sin B 4(1):18–25. https://doi.org/10.1016/j.apsb.2013.11.001
Huang CY, Chen CM, Lee YD (2007) Synthesis of high loading and encapsulation efficient paclitaxel-loaded poly (n-butyl cyanoacrylate) nanoparticles via miniemulsion. Int J Pharm 338(1–2):267–275. https://doi.org/10.1016/j.ijpharm.2007.01.052
Huang D, Zhuang Y, Shen H, Yang F, Wang X, Wu D (2018) Acetal-linked poly(ethylene glycol)ylated paclitaxel prodrugs forming free-paclitaxel-loaded pH-responsive micelles with high drug loading capacity and improved drug delivery. Mater Sci Eng C 82:60–68. https://doi.org/10.1016/j.msec.2017.08.063
Huang ZG, Lv FM, Wang J, Cao SJ, Liu ZP, Liu Y, Lu WY (2019) RGD-modified poly(ethylene glycol)ylated paclitaxel nanocrystals with enhanced stability and tumor-targeting capability. Int J Pharm 556:217–225. https://doi.org/10.1016/j.ijpharm.2018.12.023
Huo M, Zhu Q, Wu Q, Yin T, Wang L, Yin L, Zhou J (2015) Somatostatin receptor–mediated specific delivery of paclitaxel prodrugs for efficient cancer therapy. J Pharm Sci 104(6):2018–2028. https://doi.org/10.1002/jps.24438
Huo M, Fu Y, Liu Y, Chen Q, Mu Y, Zhou J, Li L, Xu W, Yin T (2018) N-mercapto acetyl-N′-octyl-O, N ″-glycol chitosan as an efficiency oral delivery system of paclitaxel. Carbohydr Polym 181:477–488. https://doi.org/10.1016/j.carbpol.2017.10.066
Hussien NA, Işıklan N, Türk M (2018) Pectin-conjugated magnetic graphene oxide nanohybrid as a novel drug carrier for paclitaxel delivery. Artif Cells Nanomed Biotechnol 46(sup1):264–273. https://doi.org/10.1080/21691401.2017.1421211
Ibrahim NK, Desai N, Legha S, Soon-Shiong P, Theriault RL, Rivera E, Esmaeli B, Ring SE, Bedikian A, Hortobagyi GN, Ellerhorst JA (2002) Phase I and pharmacokinetic study of ABI-007, a Cremophor-free, protein-stabilized, nanoparticle formulation of paclitaxel. Clin Cancer Res 8(5):1038–1044
Ingle SG, Pai RV, Monpara JD, Vavia PR (2018) Liposils: an effective strategy for stabilizing paclitaxel loaded liposomes by surface coating with silica. Eur J Pharm Sci 122:51–63. https://doi.org/10.1016/j.ejps.2018.06.02.
Iyer AK, Khaled G, Fang J, Maeda H (2006) Exploiting the enhanced permeability and retention effect for tumor targeting. Drug Discov Today 11(17–18):812–818. https://doi.org/10.1016/j.drudis.2006.07.005
Jaiswal M, Dudhe R, Sharma PK (2015) Nanoemulsion: an advanced mode of drug delivery system. 3 Biotech 5(2):123–127. https://doi.org/10.1007/s13205-014-0214-0
Jia L, Shen J, Li Z, Zhang D, Zhang Q, Liu G, Zheng D, Tian X (2013) In vitro and in vivo evaluation of paclitaxel-loaded mesoporous silica nanoparticles with three pore sizes. Int J Pharm 445(1–2):12–19. https://doi.org/10.1016/j.ijpharm.2013.01.058
Jiang X, Xin H, Sha X, Gu J, Jiang Y, Law K, Chen Y, Chen L, Wang X, Fang X (2011) Poly(ethylene glycol)ylated poly (trimethylene carbonate) nanoparticles loaded with paclitaxel for the treatment of advanced glioma: in vitro and in vivo evaluation. Int J Pharm 420(2):385–394. https://doi.org/10.1016/j.ijpharm.2011.08.052.
Jin X, Zhou B, Xue L, San W (2015) Soluplus® micelles as a potential drug delivery system for reversal of resistant tumor. Biomed Pharmacother 69:388–395. https://doi.org/10.1016/j.biopha.2014.12.028
Jin M, Jin G, Kang L, Chen L, Gao Z, Huang W (2018a) Smart polymeric nanoparticles with pH-responsive and poly(ethylene glycol)-detachable properties for co-delivering paclitaxel and survivin siRNA to enhance antitumor outcomes. Int J Nanomedicine 13:2405–2426. https://doi.org/10.2147/IJN.S161426
Jin Z, Chen Z, Wu K, Shen Y, Guo S (2018b) Investigation of migration-preventing tracheal stent with high dose of 5-fluorouracil or paclitaxel for local drug delivery. ACS Appl Bio Mater 1(5):1328–1336. https://doi.org/10.1021/acsabm.8b00290
Kang YK, Ryu MH, Park SH, Kim JG, Kim JW, Cho SH, Park YI, Park SR, Rha SY, Kang MJ, Cho JY (2018) Efficacy and safety findings from DREAM: a phase III study of DHP107 (oral paclitaxel) versus iv paclitaxel in patients with advanced gastric cancer after failure of first-line chemotherapy. Ann Oncol 29(5):1220–1226. https://doi.org/10.1093/annonc/mdy055
Kaur P, Garg T, Rath G, Murthy RR, Goyal AK (2016) Development, optimization and evaluation of surfactant-based pulmonary nanolipid carrier system of paclitaxel for the management of drug resistance lung cancer using Box-Behnken design. Drug Deliv 23(6):1912–1925. https://doi.org/10.3109/10717544.2014.993486
Kempe S, Mäder K (2012) In situ forming implants—an attractive formulation principle for parenteral depot formulations. J Control Release 161(2):668–679. https://doi.org/10.1016/j.jconrel.2012.04.016
Kim JE, Park YJ (2017) High paclitaxel-loaded and tumor cell-targeting hyaluronan-coated nanoemulsions. Colloids Surf B: Biointerfaces 150:362–372. https://doi.org/10.1016/j.colsurfb.2016.10.050
Kim SC, Kim DW, Shim YH, Bang JS, Oh HS, Kim SW, Seo MH (2001) In vivo evaluation of polymeric micellar paclitaxel formulation: toxicity and efficacy. J Control Release 72(1–3):191–202. https://doi.org/10.1016/S0168-3659(01)00275-9
Kim TY, Kim DW, Chung JY, Shin SG, Kim SC, Heo DS, Kim NK, Bang YJ (2004) Phase I and pharmacokinetic study of Genexol-PM, a cremophor-free, polymeric micelle-formulated paclitaxel, in patients with advanced malignancies. Clin Cancer Res 10(11):3708–3716
Kim SC, Yoon HJ, Lee JW, Yu J, Park ES, Chi SC (2005) Investigation of the release behavior of DEHP from infusion sets by paclitaxel-loaded polymeric micelles. Int J Pharm 293(1–2):303–310. https://doi.org/10.1016/j.ijpharm.2005.01.011
Koppisetti V, Sahiti B (2011) Magnetically modulated drug delivery systems. Int J Drug Dev Res 3(1):260–266
Krishnadas A, Rubinstein I, Önyüksel H (2003) Sterically stabilized phospholipid mixed micelles: in vitro evaluation as a novel carrier for water-insoluble drugs. Pharm Res 20(2):297–302. https://doi.org/10.1023/A:1022243709003.
Kulshrestha P, Gogoi M, Bahadur D, Banerjee R (2012) In vitro application of paclitaxel loaded magnetoliposomes for combined chemotherapy and hyperthermia. Colloids Surf B: Biointerfaces 96:1–7. https://doi.org/10.1016/j.colsurfb.2012.02.029
Kumar Khanna V (2012) Targeted delivery of nanomedicines. ISRN Pharmacol 2012. https://doi.org/10.5402/2012/571394
Kwon GS, Okano T (1996) Polymeric micelles as new drug carriers. Adv Drug Deliv Rev 21(2):107–116. https://doi.org/10.1016/S0169-409X(96)00401-2
Lawrence MJ, Rees GD (2000) Microemulsion-based media as novel drug delivery systems. Adv Drug Deliv Rev 45(1):89–121. https://doi.org/10.1016/S0169-409X(00)00103-4
Le Broc-Ryckewaert D, Carpentier R, Lipka E, Daher S, Vaccher C, Betbeder D, Furman C (2013) Development of innovative paclitaxel-loaded small poly(lactide-co-glycolide) nanoparticles: study of their antiproliferative activity and their molecular interactions on prostatic cancer cells. Int J Pharm 454(2):712–719. https://doi.org/10.1016/j.ijpharm.2013.05.018
Lee MK, Lim SJ, Kim CK (2007) Preparation, characterization and in vitro cytotoxicity of paclitaxel-loaded sterically stabilized solid lipid nanoparticles. Biomaterials 28(12):2137–2146. https://doi.org/10.1016/j.biomaterials.2007.01.014
Lee Y, Graeser R, Kratz F, Geckeler KE (2011) Paclitaxel-loaded polymer nanoparticles for the reversal of multidrug resistance in breast cancer cells. Adv Funct Mater 21(22):4211–4218. https://doi.org/10.1002/adfm.201100853
Lee KW, Lee KH, Zang DY, Park YI, Shin DB, Kim JW, Im SA, Koh SA, Yu KS, Cho JY, Jung JA (2015) Phase I/II study of weekly oraxol for the second-line treatment of patients with metastatic or recurrent gastric cancer. Oncologist 20(8):896–897. https://doi.org/10.1634/theoncologist.
Li S, Su Z, Sun M, Xiao Y, Cao F, Huang A, Li H, Ping Q, Zhang C (2012) An arginine derivative contained nanostructure lipid carriers with pH-sensitive membranolytic capability for lysosomolytic anti-cancer drug delivery. Int J Pharm 436(1–2):248–257. https://doi.org/10.1016/j.ijpharm.2012.06.040
Li J, Yin T, Wang L, Yin L, Zhou J, Huo M (2015) Biological evaluation of redox-sensitive micelles based on hyaluronic acid-deoxycholic acid conjugates for tumor-specific delivery of paclitaxel. Int J Pharm 483(1–2):38–48. https://doi.org/10.1016/j.ijpharm.2015.02.002
Li X, Yang Y, Jia Y, Pu X, Yang T, Wang Y, Ma X, Chen Q, Sun M, Wei D, Kuang Y (2017a) Enhanced tumor targeting effects of a novel paclitaxel-loaded polymer: poly(ethylene glycol)–PCCL-modified magnetic iron oxide nanoparticles. Drug Deliv 24(1):1284–1294. https://doi.org/10.1080/10717544.2017.1373167
Li Y, Chen Z, Cui Y, Zhai G, Li L (2017b) The construction and characterization of hybrid paclitaxel-in-micelle-in-liposome systems for enhanced oral drug delivery. Colloids Surf B: Biointerfaces 160:572–580. https://doi.org/10.1016/j.colsurfb.2017.10.016
Li N, Cai H, Jiang L, Hu J, Bains A, Hu J, Gong Q, Luo K, Gu Z (2017c) Enzyme-sensitive and amphiphilic PEGylated dendrimer-paclitaxel prodrug-based nanoparticles for enhanced stability and anticancer efficacy. ACS Appl Mater Interfaces 9(8):6865–6877. https://doi.org/10.1021/acsami.6b15505
Liang N, Sun S, Hong J, Tian J, Fang L, Cui F (2016) In vivo pharmacokinetics, biodistribution and antitumor effect of paclitaxel-loaded micelles based on α-tocopherol succinate-modified chitosan. Drug Deliv 23(8):2651–2660. https://doi.org/10.3109/10717544.2015.1045103.
Liang Y, Dong C, Zhang J, Deng L, Dong A (2017) A reconstituted thermosensitive hydrogel system based on paclitaxel-loaded amphiphilic copolymer nanoparticles and antitumor efficacy. Drug Dev Ind Pharm 43(6):972–979. https://doi.org/10.1080/03639045.2017.1287718
Lin MM, Kang YJ, Sohn Y, Kim DK (2015) Dual targeting strategy of magnetic nanoparticle-loaded and RGD peptide-activated stimuli-sensitive polymeric micelles for delivery of paclitaxel. J Nanopart Res 17(6):248. https://doi.org/10.1007/s11051-015-3033-2
Liu J, Li H, Chen D, Jin X, Zhao X, Zhang C, Ping Q (2011) In vivo evaluation of novel chitosan graft polymeric micelles for delivery of paclitaxel. Drug Deliv 18(3):181–189. https://doi.org/10.3109/10717544.2010.520355
Liu Y, Yang T, Wei S, Zhou C, Lan Y, Cao A, Yang J, Wang W (2018) Mucus adhesion-and penetration-enhanced liposomes for paclitaxel oral delivery. Int J Pharm 537(1–2):245–256. https://doi.org/10.1016/j.ijpharm.2017.12.044
Lu J, Chuan X, Zhang H, Dai W, Wang X, Wang X, Zhang Q (2014) Free paclitaxel loaded poly(ethylene glycol)ylated-paclitaxel nanoparticles: preparation and comparison with other paclitaxel systems in vitro and in vivo. Int J Pharm 471(1–2):525–535. https://doi.org/10.1016/j.ijpharm.2014.05.032
Lu Y, Chen Y, Gemeinhart RA, Wu W, Li T (2015) Developing nanocrystals for cancer treatment. Nanomedicine 10(16):2537–2552. https://doi.org/10.2217/NNM.15.73
Lu B, Lv X, Le Y (2019) Chitosan-modified poly(lactide-co-glycolide) nanoparticles for control-released drug delivery. Polymers 11(2):304. https://doi.org/10.3390/polym11020304
Lundberg BB, Risovic V, Ramaswamy M, Wasan KM (2003) A lipophilic paclitaxel derivative incorporated in a lipid emulsion for parenteral administration. J Control Release 86(1):93–100. https://doi.org/10.1016/S0168-3659(02)00323-1
Madaan A, Singh P, Awasthi A, Verma R, Singh AT, Jaggi M, Mishra SK, Kulkarni S, Kulkarni H (2013) Efficiency and mechanism of intracellular paclitaxel delivery by novel nanopolymer-based tumor-targeted delivery system, Nanoxel TM. Clin Transl Oncol 15(1):26–32
Madhav NS, Kala S (2011) Review on microparticulate drug delivery system. Int J PharmTech Res 3(3):1242–1244
Manivasagan P, Bharathiraja S, Bui NQ, Lim IG, Oh J (2016) Paclitaxel-loaded chitosan oligosaccharide-stabilized gold nanoparticles as novel agents for drug delivery and photoacoustic imaging of cancer cells. Int J Pharm 511(1):367–379. https://doi.org/10.1016/j.ijpharm.2016.07.025
Mansoori B, Mohammadi A, Davudian S, Shirjang S, Baradaran B (2017) The different mechanisms of cancer drug resistance: a brief review. Adv Pharm Bull 7(3):339–348. https://doi.org/10.15171/apb.2017.041
Meerovich I, Nichols MG, Dash AK (2019) Low-intensity light-induced paclitaxel release from lipid-based nano-delivery systems. J Drug Target:1–13. https://doi.org/10.1080/1061186X.2019.1571066
Meher JG, Dixit S, Pathan DK, Singh Y, Chandasana H, Pawar VK, Sharma M, Bhatta RS, Konwar R, Kesharwani P, Chourasia MK (2018) Paclitaxel-loaded TPGS enriched self-emulsifying carrier causes apoptosis by modulating survivin expression and inhibits tumour growth in syngeneic mammary tumours. Artif Cells Nanomed Biotechnol:1–15. https://doi.org/10.1080/21691401.2018.1492933.
Miao J, Du Y, Yuan H, Zhang X, Li Q, Rao Y, Zhao M, Hu F (2015) Improved cytotoxicity of paclitaxel loaded in nanosized lipid carriers by intracellular delivery. J Nanopart Res 17(1):10. https://doi.org/10.1007/s11051-014-2852-x
Mittal P, Vardhan H, Ajmal G, Bonde GV, Kapoor R, Mittal A, Mishra B (2019) Formulation, optimization, hemocompatibility and pharmacokinetic evaluation of poly(lactide-co-glycolide) nanoparticles containing paclitaxel. Drug Dev Ind Pharm 45(3):365–378. https://doi.org/10.1080/03639045.2018.1542706
Mo Y, Lim LY (2005) Preparation and in vitro anticancer activity of wheat germ agglutinin (WGA)-conjugated poly(lactide-co-glycolide) nanoparticles loaded with paclitaxel and isopropyl myristate. J Control Release 107(1):30–42. https://doi.org/10.1016/j.jconrel.2004.06.024
Moes J, Koolen S, Huitema A, Schellens J, Beijnen J, Nuijen B (2013) Development of an oral solid dispersion formulation for use in low-dose metronomic chemotherapy of paclitaxel. Eur J Pharm Biopharm 83(1):87–94. https://doi.org/10.1016/j.ejpb.2012.09.016
Moros M, Idiago-López J, Asín L, Moreno-Antolín E, Beola L, Grazú V, Fratila RM, Gutiérrez L, de la Fuente JM (2019) Triggering antitumoural drug release and gene expression by magnetic hyperthermia. Adv Drug Deliv Rev 138:326–343. https://doi.org/10.1016/j.addr.2018.10.004
Muley P, Kumar S, El Kourati F, Kesharwani SS, Tummala H (2016) Hydrophobically modified inulin as an amphiphilic carbohydrate polymer for micellar delivery of paclitaxel for intravenous route. Int J Pharm 500(1–2):32–41. https://doi.org/10.1016/j.ijpharm.2016.01.005
Murgia S, Fadda P, Colafemmina G, Angelico R, Corrado L, Lazzari P, Monduzzi M, Palazzo G (2013) Characterization of the Solutol® HS15/water phase diagram and the impact of the Δ9-tetrahydrocannabinol solubilization. J Colloid Interface Sci 390(1):129–136. https://doi.org/10.1016/j.jcis.2012.08.068
Nanaki S, Siafaka PI, Zachariadou D, Nerantzaki M, Giliopoulos DJ, Triantafyllidis KS, Kostoglou M, Nikolakaki E, Bikiaris DN (2017) Poly(lactide-co-glycolide)/SBA-15 mesoporous silica composite microparticles loaded with paclitaxel for local chemotherapy. Eur J Pharm Sci 99:32–44. https://doi.org/10.1016/j.ejps.2016.12.010.
Nehate C, Jain S, Saneja A, Khare V, Alam N, Dhar Dubey R, Gupta PN (2014) Paclitaxel formulations: challenges and novel delivery options. Current drug delivery 11(6):666–686. https://doi.org/10.2174/156720181166614
Nguyen TL, Nguyen TH, Nguyen DH (2017) Development and in vitro evaluation of liposomes using soy lecithin to encapsulate paclitaxel. Int J Biomater 2017. https://doi.org/10.1155/2017/8234712
Nguyen HT, Soe ZC, Yang KY, Dai Phung C, Nguyen LTT, Jeong JH, Jin SG, Choi HG, Ku SK, Yong CS, Kim JO (2019) Transferrin-conjugated pH-sensitive platform for effective delivery of porous palladium nanoparticles and paclitaxel in cancer treatment. Colloids Surf B: Biointerfaces 176:265–275. https://doi.org/10.1016/j.colsurfb.2019.01.010
Niethammer A, Gaedicke G, Lode HN, Wrasidlo W (2001) Synthesis and preclinical characterization of a paclitaxel prodrug with improved antitumor activity and water solubility. Bioconjug Chem 12(3):414–420. https://doi.org/10.1021/bc000122g
Nornoo AO, Chow DSL (2008) Cremophor®free intravenous microemulsions for paclitaxel: II. Stability, in vitro release and pharmacokinetics. Int J Pharm 349(1–2):117–123. https://doi.org/10.1016/j.ijpharm.2007.07.043
Nornoo AO, Osborne DW, Chow DSL (2008) Cremophor®-free intravenous microemulsions for paclitaxel: I: formulation, cytotoxicity and hemolysis. Int J Pharm 349(1–2):108–116. https://doi.org/10.1016/j.ijpharm.2007.07.042
Núñez C, Estévez SV, del Pilar Chantada M (2018) Inorganic nanoparticles in diagnosis and treatment of breast cancer. JBIC J Biol Inorg Chem 23(3):331–345. https://doi.org/10.1007/s00775-018-1542-z
Okner R, Shaulov Y, Tal N, Favaro G, Domb AJ, Mandler D (2009) Electropolymerized tricopolymer based on N-pyrrole derivatives as a primer coating for improving the performance of a drug-eluting stent. ACS Appl Mater Interfaces 1(4):758–767. https://doi.org/10.1021/am800139s
Olbrich JM, Tate PL, Corbett JT, Lindsey JM III, Nagatomi SD, Shalaby WS, Shalaby SW (2012) Injectable in situ forming controlled release implant composed of a poly-ether-ester-carbonate and applications in the field of chemotherapy. J Biomed Mater Res A 100(9):2365–2372. https://doi.org/10.1002/jbm.a.34179.
Oliveira RR, Carrião MS, Pacheco MT, Branquinho LC, de Souza ALR, Bakuzis AF, Lima EM (2018) Triggered release of paclitaxel from magnetic solid lipid nanoparticles by magnetic hyperthermia. Mater Sci Eng C 92:547–553. https://doi.org/10.1016/j.msec.2018.07.011
Oostendorp RL, Buckle T, Lambert G, Garrigue JS, Beijnen JH, Schellens JH, van Tellingen O (2011) Paclitaxel in self-micro emulsifying formulations: oral bioavailability study in mice. Investig New Drugs 29(5):768–776. https://doi.org/10.1007/s10637-010-9421-7
O’Reilly RK, Hawker CJ, Wooley KL (2006) Cross-linked block copolymer micelles: functional nanostructures of great potential and versatility. Chem Soc Rev 35(11):1068–1083. https://doi.org/10.1039/b514858h
Owen SC, Chan DP, Shoichet MS (2012) Polymeric micelle stability. Nano Today 7(1):53–65. https://doi.org/10.1016/j.nantod.2012.01.002
Pandey V, Gajbhiye KR, Soni V (2015) Lactoferrin-appended solid lipid nanoparticles of paclitaxel for effective management of bronchogenic carcinoma. Drug Deliv 22(2):199–205. https://doi.org/10.3109/10717544.2013.877100
Papas S, Akoumianaki T, Kalogiros C, Hadjiarapoglou L, Theodoropoulos PA, Tsikaris V (2007) Synthesis and antitumor activity of peptide-paclitaxel conjugates. J Pept Sci 13(10):662–671. https://doi.org/10.1002/psc.899.
Pesoa JI, Rico MJ, Rozados VR, Scharovsky OG, Luna JA, Mengatto LN (2018) Paclitaxel delivery system based on poly (lactide-co-glycolide) microparticles and chitosan thermo-sensitive gel for mammary adenocarcinoma treatment. J Pharm Pharmacol 70(11):1494–1502. https://doi.org/10.1111/jphp.13006.
Pooja D, Kulhari H, Kuncha M, Rachamalla SS, Adams DJ, Bansal V, Sistla R (2016) Improving efficacy, oral bioavailability, and delivery of paclitaxel using protein-grafted solid lipid nanoparticles. Mol Pharm 13(11):3903–3912. https://doi.org/10.1021/acs.molpharmaceut.6b00691
Qu X, Zou Y, He C, Zhou Y, Jin Y, Deng Y, Wang Z, Li X, Zhou Y, Liu Y (2018) Improved intestinal absorption of paclitaxel by mixed micelles self-assembled from vitamin E succinate-based amphiphilic polymers and their transcellular transport mechanism and intracellular trafficking routes. Drug Deliv 25(1):210–225. https://doi.org/10.1080/10717544.2017.1419513
Qu G, Hou S, Qu D, Tian C, Zhu J, Xue L, Ju C, Zhang C (2019) Self-assembled micelles based on N-octyl-N’-phthalyl-O-phosphoryl chitosan derivative as an effective oral carrier of paclitaxel. Carbohydr Polym 207:428–439. https://doi.org/10.1016/j.carbpol.2018.11.099
Shaikh R, Singh TRR, Garland MJ, Woolfson AD, Donnelly RF (2011) Mucoadhesive drug delivery systems. J Pharm Bioallied Sci 3(1):89. https://doi.org/10.4103/0975-7406.76478
Rajgor N, Patel M, Bhaskar VH (2011) Implantable drug delivery systems: an overview. Surg Neurol Int 2(2). https://doi.org/10.4103/0975-8453.86297
Ranganath SH, Wang CH (2008) Biodegradable microfiber implants delivering paclitaxel for post-surgical chemotherapy against malignant glioma. Biomaterials 29(20):2996–3003. https://doi.org/10.1016/j.biomaterials.2008.04.002
Ravar F, Saadat E, Gholami M, Dehghankelishadi P, Mahdavi M, Azami S, Dorkoosh FA (2016) Hyaluronic acid-coated liposomes for targeted delivery of paclitaxel, in-vitro characterization and in-vivo evaluation. J Control Release 229:10–22. https://doi.org/10.1016/j.jconrel.2016.03.012
Ren H, Gao C, Zhou L, Liu M, Xie C, Lu W (2015) EGFR-targeted poly (ethylene glycol)-distearoylphosphatidylethanolamine micelle loaded with paclitaxel for laryngeal cancer: preparation, characterization and in vitro evaluation. Drug Deliv 22(6):785–794. https://doi.org/10.3109/10717544.2014.896057
Rezaei SJT, Nabid MR, Niknejad H, Entezami AA (2012) Folate-decorated thermoresponsive micelles based on star-shaped amphiphilic block copolymers for efficient intracellular release of anticancer drugs. Int J Pharm 437(1–2):70–79. https://doi.org/10.1016/j.ijpharm.2012.07.069
Ringsdorf H (1975) Structure and properties of pharmacologically active polymers. In: Journal of Polymer Science, Polymer Symposia, vol 51, no 1. Wiley Subscription Services, Inc., A Wiley Company, New York, pp 135–153. https://doi.org/10.1002/polc.5070510111
Ron N, Cordia J, Yang A, Ci S, Nguyen P, Hughs M, Desai N (2008) Comparison of physicochemical characteristics and stability of three novel formulations of paclitaxel: Abraxane, Nanoxel, and Genexol PM
Rosière R, Van Woensel M, Mathieu V, Langer I, Mathivet T, Vermeersch M, Amighi K, Wauthoz N (2016) Development and evaluation of well-tolerated and tumor-penetrating polymeric micelle-based dry powders for inhaled anti-cancer chemotherapy. Int J Pharm 501(1–2):148–159
Ruel-Gariépy E, Shive M, Bichara A, Berrada M, Le Garrec D, Chenite A, Leroux JC (2004) A thermosensitive chitosan-based hydrogel for the local delivery of paclitaxel. Eur J Pharm Biopharm 57(1):53–63. https://doi.org/10.1016/S0939-6411(03)00095-X
Ruttala HB, Ramasamy T, Shin BS, Choi HG, Yong CS, Kim JO (2017) Layer-by-layer assembly of hierarchical nanoarchitectures to enhance the systemic performance of nanoparticle albumin-bound paclitaxel. Int J Pharm 519(1–2):11–21. https://doi.org/10.1016/j.ijpharm.2017.01.011
Rxlist website (2019) https://www.rxlist.com/taxol-drug.html, July 04, 2019
Sahu SK, Maiti S, Maiti TK, Ghosh SK, Pramanik P (2011) Hydrophobically modified carboxymethyl chitosan nanoparticles targeted delivery of paclitaxel. J Drug Target 19(2):104–113. https://doi.org/10.3109/10611861003733987
Samarajeewa S, Shrestha R, Elsabahy M, Karwa A, Li A, Zentay RP, Kostelc JG, Dorshow RB, Wooley KL (2013) In vitro efficacy of paclitaxel-loaded dual-responsive shell cross-linked polymer nanoparticles having orthogonally degradable disulfide cross-linked corona and polyester core domains. Mol Pharm 10(3):1092–1099. https://doi.org/10.1021/mp3005897
Sarisozen C, Vural I, Levchenko T, Hincal AA, Torchilin VP (2012) Long-circulating poly(ethylene glycol)-PE micelles co-loaded with paclitaxel and elacridar (GG918) overcome multidrug resistance. Drug Deliv 19(8):363–370. https://doi.org/10.3109/10717544.2012.724473
Sarpietro MG, Ottimo S, Paolino D, Ferrero A, Dosio F, Castelli F (2012) Squalenoyl prodrug of paclitaxel: synthesis and evaluation of its incorporation in phospholipid bilayers. Int J Pharm 436(1–2):135–140. https://doi.org/10.1016/j.ijpharm.2012.06.034
Schafer FQ, Buettner GR (2001) Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic Biol Med 30(11):1191–1212
Schiff PB, Fant J, Horwitz SB (1979) Promotion of microtubule assembly in vitro by taxol. Nature 277(5698):665. https://doi.org/10.1038/277665a0
Shanmugam S, Park JH, Chi SC, Yong CS, Choi HG, Woo JS (2011) Antitumor efficacy of solid dispersion of paclitaxel prepared by supercritical antisolvent process in human mammary tumor xenografts. Int J Pharm 403(1–2):130–135. https://doi.org/10.1016/j.ijpharm.2010.10.033
Sharma NK, Kumar V (2015) Liposomal paclitaxel: recent trends and future perspectives. Int J Pharm Sci Rev Res 31(1):205–211
Sharma S, Verma A, Pandey G, Mittapelly N, Mishra PR (2015) Investigating the role of Pluronic-g-Cationic polyelectrolyte as functional stabilizer for nanocrystals: impact on paclitaxel oral bioavailability and tumor growth. Acta Biomater 26:169–183. https://doi.org/10.1016/j.actbio.2015.08.005
Shaulov Y, Okner R, Levi Y, Tal N, Gutkin V, Mandler D, Domb AJ (2009) Poly (methyl methacrylate) grafting onto stainless steel surfaces: application to drug-eluting stents. ACS Appl Mater Interfaces 1(11):2519–2528. https://doi.org/10.1021/am900465t
Shen Y, Tang H, Radosz M, Van Kirk E, Murdoch WJ (2008) pH-responsive nanoparticles for cancer drug delivery. Methods Mol Biol 437:183–216. https://doi.org/10.1007/978-1-59745-210-6_10
Shen Y, Pi Z, Yan F, Yeh CK, Zeng X, Diao X, Hu Y, Chen S, Chen X, Zheng H (2017) Enhanced delivery of paclitaxel liposomes using focused ultrasound with microbubbles for treating nude mice bearing intracranial glioblastoma xenografts. Int J Nanomedicine 12:5613. https://doi.org/10.2147/IJN.S136401
Shi J, Kantoff PW, Wooster R, Farokhzad OC (2017) Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer 17(1):20–37. https://doi.org/10.1038/nrc.2016.108
Shu C, Sabi-mouka EM, Wang X, Ding L (2017) Self-assembly hydrogels as multifunctional drug delivery of paclitaxel for synergistic tumour-targeting and biocompatibility in vitro and in vivo. J Pharm Pharmacol 69(8):967–977. https://doi.org/10.1111/jphp.12732
Shuai X, Merdan T, Schaper AK, Xi F, Kissel T (2004) Core-cross-linked polymeric micelles as paclitaxel carriers. Bioconjug Chem 15(3):441–448. https://doi.org/10.1021/bc034113u
Song TT, Yuan XB, Sun AP, Wang H, Kang CS, Ren Y, He B, Sheng J, Pu PY (2010) Preparation of injectable paclitaxel sustained release microspheres by spray drying for inhibition of glioma in vitro. J Appl Polym Sci 115(3):1534–1539. https://doi.org/10.1002/app.31105
Stevens PJ, Sekido M, Lee RJ (2004) A folate receptor–targeted lipid nanoparticle formulation for a lipophilic paclitaxel prodrug. Pharm Res 21(12):2153–2157. https://doi.org/10.1007/s11095-004-7667-5
Stewart S, Domínguez-Robles J, Donnelly R, Larrañeta E (2018) Implantable polymeric drug delivery devices: classification, manufacture, materials, and clinical applications. Polymers 10(12):1379. https://doi.org/10.3390/polym10121379
Sutradhar KB, Amin ML (2014) Nanotechnology in cancer drug delivery and selective targeting. ISRN Nanotechnol 2014:1–12. https://doi.org/10.1155/2014/939378
Szebeni J, Alving CR, Muggia FM (1998) Complement activation by Cremophor EL as a possible contributor to hypersensitivity to paclitaxel: an in vitro study. JNCI: J Natl Canc Inst 90(4):300–306. https://doi.org/10.1093/jnci/90.4.300
Tam YT, Shin DH, Chen KE, Kwon GS (2019) Poly (ethylene glycol)-block-poly (d, l-lactic acid) micelles containing oligo (lactic acid) 8-paclitaxel prodrug: in vivo conversion and antitumor efficacy. J Control Release 298:186–193. https://doi.org/10.1016/j.jconrel.2019.02.017
Thanki K, Kushwah V, Jain S (2015) Recent advances in tumor targeting approaches. In: Targeted drug delivery: concepts and design. Springer, Cham, pp 41–112. https://doi.org/10.1007/978-3-319-11355-5_2
Thapa P, Li M, Karki R, Bio M, Rajaputra P, Nkepang G, Woo S, You Y (2017) Folate-poly(ethylene glycol) conjugates of a far-red light-activatable paclitaxel prodrug to improve selectivity toward folate receptor-positive cancer cells. ACS Omega 2(10):6349–6360. https://doi.org/10.1021/acsomega.7b01105
Tiwari S, Tirosh B, Rubinstein A (2017) Increasing the affinity of cationized polyacrylamide-paclitaxel nanoparticles towards colon cancer cells by a surface recognition peptide. Int J Pharm 531(1):281–291. https://doi.org/10.1016/j.ijpharm.2017.08.092
Tosta FV, Andrade LM, Mendes LP, Anjos JLV, Alonso A, Marreto RN, Lima EM, Taveira SF (2014) Paclitaxel-loaded lipid nanoparticles for topical application: the influence of oil content on lipid dynamic behavior, stability, and drug skin penetration. J Nanopart Res 16(12):2782. https://doi.org/10.1007/s11051-014-2782-7
Tran S, DeGiovanni PJ, Piel B, Rai P (2017) Cancer nanomedicine: a review of recent success in drug delivery. Clin Transl Med 6(1):44. https://doi.org/10.1186/s40169-017-0175-0
Trieu V, D’Cruz O, Desai, N (2008) Comparison of antitumor activity of three cremophor-free paclitaxel formulations, Abraxane, Nanoxel, and Genexol PM
Ucar E, Teksoz S, Ichedef C, Kilcar AY, Medine EI, Ari K, Parlak Y, Bilgin BES, Unak P (2017) Synthesis, characterization and radiolabeling of folic acid modified nanostructured lipid carriers as a contrast agent and drug delivery system. Appl Radiat Isot 119:72–79. https://doi.org/10.1016/j.apradiso.2016.11.002
Varma MV, Sateesh K, Panchagnula R (2005) Functional role of P-glycoprotein in limiting intestinal absorption of drugs: contribution of passive permeability to P-glycoprotein mediated efflux transport. Mol Pharm 2(1):12–21. https://doi.org/10.1021/mp0499196
Vroman I, Tighzert L (2009) Biodegradable polymers. Materials 2(2):307–344. https://doi.org/10.3390/ma2020307
Wall ME, Wani MC (1996) Camptothecin and taxol: from discovery to clinic. J Ethnopharmacol 51(1–3):239–254. https://doi.org/10.1016/0378-8741(95)01367-9
Wan L, Wang X, Zhu W, Zhang C, Song A, Sun C, Jiang T, Wang S (2015) Folate-polyethyleneimine functionalized mesoporous carbon nanoparticles for enhancing oral bioavailability of paclitaxel. Int J Pharm 484(1–2):207–217. https://doi.org/10.1016/j.ijpharm.2015.02.054
Wang J, Ng CW, Win KY, Shoemakers P, Lee TKY, Feng SS, Wang CH (2003) Release of paclitaxel from polylactide-co-glycolide (poly(lactide-co-glycolide)) microparticles and discs under irradiation. J Microencapsul 20(3):317–327. https://doi.org/10.1080/0265204021000058401.
Wang Y, Jiang G, Qiu T, Ding F (2012) Preparation and evaluation of paclitaxel-loaded nanoparticle incorporated with galactose-carrying polymer for hepatocyte targeted delivery. Drug Dev Ind Pharm 38(9):1039–1046. https://doi.org/10.3109/03639045.2011.637052
Wang F, Shen Y, Xu X, Lv L, Li Y, Liu J, Li M, Guo A, Guo S, Jin F (2013) Selective tissue distribution and long circulation endowed by paclitaxel loaded poly(ethylene glycol)ylated poly (ɛ-caprolactone-co-l-lactide) micelles leading to improved anti-tumor effects and low systematic toxicity. Int J Pharm 456(1):101–112. https://doi.org/10.1016/j.ijpharm.2013.08.008
Wang F, Yang S, Hua D, Yuan J, Huang C, Gao Q (2016) A novel preparation method of paclitaxcel-loaded folate-modified chitosan microparticles and in vitro evaluation. J Biomater Sci Polym Ed 27(3):276–289. https://doi.org/10.1080/09205063.2015.1121366
Wang F, Li L, Liu B, Chen Z, Li C (2017) Hyaluronic acid decorated pluronic P85 solid lipid nanoparticles as a potential carrier to overcome multidrug resistance in cervical and breast cancer. Biomed Pharmacother 86:595–604. https://doi.org/10.1016/j.biopha.2016.12.041
Wang G, Wang Z, Li C, Duan G, Wang K, Li Q, Tao T (2018) RGD peptide-modified, paclitaxel prodrug-based, dual-drugs loaded, and redox-sensitive lipid-polymer nanoparticles for the enhanced lung cancer therapy. Biomed Pharmacother 106:275–284. https://doi.org/10.1016/j.biopha.2018.06.137
Wang X, Guo Y, Qiu L, Wang X, Li T, Han L, Ouyang H, Xu W, Chu K (2019) Preparation and evaluation of carboxymethyl chitosan-rhein polymeric micelles with synergistic antitumor effect for oral delivery of paclitaxel. Carbohydr Polym 206:121–131. https://doi.org/10.1016/j.carbpol.2018.10.096
Weaver BA (2014) How Taxol®/paclitaxel kills cancer cells. Mol Biol Cell 25(18):2677–2681. https://doi.org/10.1091/mbc.e14-04-0916
Wei Z, Hao J, Yuan S, Li Y, Juan W, Sha X, Fang X (2009) Paclitaxel-loaded Pluronic P123/F127 mixed polymeric micelles: formulation, optimization and in vitro characterization. Int J Pharm 376(1–2):176–185. https://doi.org/10.1016/j.ijpharm.2009.04.030
Wei Y, Xue Z, Ye Y, Huang Y, Zhao L (2014) Paclitaxel targeting to lungs by way of liposomes prepared by the effervescent dispersion technique. Arch Pharm Res 37(6):728–737. https://doi.org/10.1007/s12272-013-0181-8
Westedt U, Wittmar M, Hellwig M, Hanefeld P, Greiner A, Schaper AK, Kissel T (2006) Paclitaxel releasing films consisting of poly (vinyl alcohol)-graft-poly (lactide-co-glycolide) and their potential as biodegradable stent coatings. J Control Release 111(1–2):235–246. https://doi.org/10.1016/j.jconrel.2005.12.012
Wu J, Liu Q, Lee RJ (2006) A folate receptor-targeted liposomal formulation for paclitaxel. Int J Pharm 316(1–2):148–153. https://doi.org/10.1016/j.ijpharm.2006.02.027
Wu Y, Wang L, Zhang K, Zhou L, Zhang X, Jiang X, Zhu C (2017) N-Butyl-2-cyanoacrylate-based injectable and in situ-forming implants for efficient intratumoral chemotherapy. Drug Deliv 24(1):729–736. https://doi.org/10.1080/10717544.2017.1309478
Xiang J, Wu B, Zhou Z, Hu S, Piao Y, Zhou Q, Wang G, Tang J, Liu X, Shen Y (2018) Synthesis and evaluation of a paclitaxel-binding polymeric micelle for efficient breast cancer therapy. Sci China Life Sci:1–12. https://doi.org/10.1007/s11427-017-9274-9.
Xin H, Chen L, Gu J, Ren X, Luo J, Chen Y, Jiang X, Sha X, Fang X (2010) Enhanced anti-glioblastoma efficacy by paclitaxel-loaded poly(ethylene glycol)ylated poly (ɛ-caprolactone) nanoparticles: in vitro and in vivo evaluation. Int J Pharm 402(1–2):238–247. https://doi.org/10.1016/j.ijpharm.2010.10.005.
Xin Y, Yin M, Zhao L, Meng F, Luo L (2017) Recent progress on nanoparticle-based drug delivery systems for cancer therapy. Cancer Biol Med 14(3):228–241. https://doi.org/10.20892/j.issn.2095-3941.2017.0052
Xiong K, Wu J, Liu Y, Wu N, Ruan J (2019) Drug carrier-oriented polygeline for preparing novel polygeline-bound paclitaxel nanoparticles. J Pharm Sci 108(6):2012–2021. https://doi.org/10.1016/j.xphs.2019.01.005
Xu W, Cui Y, Ling P, Li LB (2012) Preparation and evaluation of folate-modified cationic pluronic micelles for poorly soluble anticancer drug. Drug Deliv 19(4):208–219. https://doi.org/10.3109/10717544.2012.690005
Xu W, Lim SJ, Lee MK (2013) Cellular uptake and antitumour activity of paclitaxel incorporated into trilaurin-based solid lipid nanoparticles in ovarian cancer. J Microencapsul 30(8):755–761. https://doi.org/10.3109/02652048.2013.788083
Xu W, Fan X, Zhao Y, Li L (2015a) Cysteine modified and bile salt based micelles: preparation and application as an oral delivery system for paclitaxel. Colloids Surf B: Biointerfaces 128:165–171. https://doi.org/10.1016/j.colsurfb.2015.02.031
Xu C, He W, Lv Y, Qin C, Shen L, Yin L (2015b) Self-assembled nanoparticles from hyaluronic acid–paclitaxel prodrugs for direct cytosolic delivery and enhanced antitumor activity. Int J Pharm 493(1–2):172–181. https://doi.org/10.1016/j.ijpharm.2015.07.069
Yadav KS, Mishra DK, Deshpande A, Pethe AM (2019) Levels of drug targeting. In: Basic fundamentals of drug delivery. Academic, pp 269–305. https://doi.org/10.1016/B978-0-12-817909-3.00007-8.
Yang T, Cui FD, Choi MK, Cho JW, Chung SJ, Shim CK, Kim DD (2007) Enhanced solubility and stability of poly(ethylene glycol)ylated liposomal paclitaxel: in vitro and in vivo evaluation. Int J Pharm 338(1–2):317–326. https://doi.org/10.1016/j.ijpharm.2007.02.011
Yang L, Wu X, Liu F, Duan Y, Li S (2009a) Novel biodegradable polylactide/poly (ethylene glycol) micelles prepared by direct dissolution method for controlled delivery of anticancer drugs. Pharm Res 26(10):2332–2342. https://doi.org/10.1007/s11095-009-9949-4
Yang R, Yang SG, Shim WS, Cui F, Cheng G, Kim IW, Kim DD, Chung SJ, Shim CK (2009b) Lung-specific delivery of paclitaxel by chitosan-modified poly(lactide-co-glycolide) nanoparticles via transient formation of microaggregates. J Pharm Sci 98(3):970–984. https://doi.org/10.1002/jps.21487.
Yao HJ, Ju RJ, Wang XX, Zhang Y, Li RJ, Yu Y, Zhang L, Lu WL (2011) The antitumor efficacy of functional paclitaxel nanomicelles in treating resistant breast cancers by oral delivery. Biomaterials 32(12):3285–3302. https://doi.org/10.1016/j.biomaterials.2011.01.038
Yin T, Wu Q, Wang L, Yin L, Zhou J, Huo M (2015) Well-defined redox-sensitive polyethene glycol–paclitaxel prodrug conjugate for tumor-specific delivery of paclitaxel using octreotide for tumor targeting. Mol Pharm 12(8):3020–3031. https://doi.org/10.1021/acs.molpharmaceut.5b00280
Yuan ZQ, Li JZ, Liu Y, Chen WL, Zhang CG, Zhu WJ, Zhou XF, Liu C, Zhang XN (2015) Systemic delivery of micelles loading with paclitaxel using N-succinyl-palmitoyl-chitosan decorated with cRGDyK peptide to inhibit non-small-cell lung cancer. Int J Pharm 492(1–2):141–151. https://doi.org/10.1016/j.ijpharm.2015.07.022
Yuan S, Chen J, Sheng J, Hu Y, Jiang Z (2016) Paclitaxel loaded β-cyclodextrin modified poly(acrylic acid) nanoparticles through multivalent inclusion for anticancer therapy. Macromol Biosci 16:341–349. https://doi.org/10.1002/mabi.201500302
Zaki M, Patil SK, Baviskar DT, Jain DK (2012) Implantable drug delivery system: a review. Int J PharmTech Res 4(1):280–292
Zhang Z, Feng SS (2006) In vitro investigation on poly (lactide)-tween 80 copolymer nanoparticles fabricated by dialysis method for chemotherapy. Biomacromolecules 7(4):1139–1146. https://doi.org/10.1021/bm050953v
Zhang XY, Zhang YD (2015) Enhanced antiproliferative and apoptosis effect of paclitaxel-loaded polymeric micelles against non-small cell lung cancers. Tumor Biol 36(7):4949–4959. https://doi.org/10.1007/s13277-015-3142-7
Zhang X, Chen J, Kang Y, Hong S, Zheng Y, Sun H, Xu C (2013) Targeted paclitaxel nanoparticles modified with follicle-stimulating hormone β peptide show effective antitumor activity against ovarian carcinoma. Int J Pharm 453(2):498–505. https://doi.org/10.1016/j.ijpharm.2013.06.038
Zhang J, Chen R, Fang X, Chen F, Wang Y, Chen M (2015) Nucleolin targeting AS1411 aptamer modified pH-sensitive micelles for enhanced delivery and antitumor efficacy of paclitaxel. Nano Res 8(1):201–218. https://doi.org/10.1007/s12274-014-0619-4
Zhang F, Fei J, Sun M, Ping Q (2016) Heparin modification enhances the delivery and tumor targeting of paclitaxel-loaded N-octyl-N-trimethyl chitosan micelles. Int J Pharm 511(1):390–402. https://doi.org/10.1016/j.ijpharm.2016.07.020
Zhang T, Luo J, Fu Y, Li H, Ding R, Gong T, Zhang Z (2017) Novel oral administrated paclitaxel micelles with enhanced bioavailability and antitumor efficacy for resistant breast cancer. Colloids Surf B: Biointerfaces 150:89–97. https://doi.org/10.1016/j.colsurfb.2016.11.024
Zhao Y, Li J, Yu H, Wang G, Liu W (2012) Synthesis and characterization of a novel polydepsipeptide contained tri-block copolymer (mpoly(ethylene glycol)–PLLA–PMMD) as self-assembly micelle delivery system for paclitaxel. Int J Pharm 430(1–2):282–291. https://doi.org/10.1016/j.ijpharm.2012.03.043
Zhao L, Bi D, Qi X, Guo Y, Yue F, Wang X, Han M (2019) Polydopamine-based surface modification of paclitaxel nanoparticles for osteosarcoma targeted therapy. Nanotechnology 30(25):255101. https://doi.org/10.1088/1361-6528/ab055f
Zheng J, Wan Y, Elhissi A, Zhang Z, Sun X (2014) Targeted paclitaxel delivery to tumors using cleavable poly(ethylene glycol)-conjugated solid lipid nanoparticles. Pharm Res 31(8):2220–2233. https://doi.org/10.1007/s11095-014-1320-8
Zhou J, Zhao WY, Ma X, Ju RJ, Li XY, Li N, Sun MG, Shi JF, Zhang CX, Lu WL (2013) The anticancer efficacy of paclitaxel liposomes modified with mitochondrial targeting conjugate in resistant lung cancer. Biomaterials 34(14):3626–3638. https://doi.org/10.1016/j.biomaterials.2013.01.078
Zhu Z, Li Y, Li X, Li R, Jia Z, Liu B, Guo W, Wu W, Jiang X (2010) Paclitaxel-loaded poly (N-vinylpyrrolidone)-b-poly (ε-caprolactone) nanoparticles: preparation and antitumor activity in vivo. J Control Release 142(3):438–446. https://doi.org/10.1016/j.jconrel.2009.11.002
Zitzmann S, Ehemann V, Schwab M (2002) Arginine-glycine-aspartic acid (RGD)-peptide binds to both tumor and tumor-endothelial cells in vivo. Cancer Res 62(18):5139–5143
Acknowledgements
The authors PA, SK, KV acknowledge scholarship provided by Department of Pharmaceuticals, Government of India.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
A, P., Kar, S., Vignesh, K., Kolhe, U.D. (2020). An Overview of Paclitaxel Delivery Systems. In: Saneja, A., Panda, A., Lichtfouse, E. (eds) Sustainable Agriculture Reviews 43. Sustainable Agriculture Reviews, vol 43. Springer, Cham. https://doi.org/10.1007/978-3-030-41838-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-41838-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41837-3
Online ISBN: 978-3-030-41838-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)