Abstract
The unique characteristics of terror-related explosion events necessitate a thorough reevaluation process to prepare all levels of medical treatment for casualties of such incidents, from the prehospital setting, through the hospitals, and all the way to rehabilitation and mental health. This chapter discusses the main operational considerations stemming from the modern trends of terror explosion injuries noted in recent evidence-based research. In particular, the chapter describes how explosive device characteristics interact with physical location of the explosion to define the patterns of injury and required clinical resources, as well as the influence of the general setting of the event (military/civilian, urban/rural) on scene and medical management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Operational considerations
- Terror-related blast events
- Explosive device characteristics
- Detonation location
- Incident setting
- Multidimensional injury pattern (MIP)
- Improvised explosive device (IED)
- Vehicle-based explosive device (VBIED)
Introduction
In previous decades, most blast events occurred in the military and industrial arenas, but the current threat shifts more toward terrorism. Indeed, injuries caused by terror-related explosions are of major concern in recent years, with increasing threats of terrorism worldwide. Prime examples are the Oklahoma bombing (1995), September 11th attacks (2001), Madrid train bombings (2004), London underground bombing (2005), Mumbai attacks (2008), Paris attacks (2015), Brussels bombings (2016), the Manchester suicide attacks (2016), and more. What once was presumed to be a concern mainly for countries close to conflict zones, such as Israel, Iraq, Afghanistan, and some regions of India and Pakistan, is now a global threat.
A common misconception is to confuse blast injuries with blast events. The former describes a type of injury mechanism found in the latter. In reality, blast events usually result in combined injuries, of which “blast effect” is only a single kind. Blast events take different shapes and forms, which occur in varying contexts. These events can occur in combat-related scenarios (e.g., war or civil conflicts), criminal acts (e.g., assassinations and mafia-driven incidents), and terrorism.
Terror-related blast events frequently cause multiple casualties, with a risk of overwhelming healthcare services in the case of Mass Casualty Events (MCE), and are associated with immediate and delayed psychological effects, both to the victims present at the scene and on the wider community level. They also produce patterns of injury that are different from prior experience with industrial explosions and military casualties: multiple penetrating injuries from improvised fragment elements combined with other types of blast-related trauma result in injuries of much higher severity in survivors of the immediate blast.
In general, injuries caused by blast are typically divided into five types. Primary blast injuries are direct effects caused by initial overpressure or underpressure associated with the explosive detonation. These include rupture of tympanic membranes, pulmonary damage, and rupture of the hollow viscera. Secondary blast injuries are caused by debris carried by the blast (e.g., small shrapnel), leading to penetrating trauma or fragmentation injuries. Tertiary blast injuries are caused by the physical displacement of the victim, for instance, being thrown by the blast wind or being affected by structural collapse. These include crush injuries, blunt trauma, fractures and traumatic amputations, open or closed brain injuries, and penetrating trauma. Quaternary blast injuries include all other injuries, such as burns, asphyxia, crush injuries, and inhalation of toxic compounds. Quinary blast injury is a relatively new concept. It includes delayed effects such as chronic pain, malnutrition, and immunosuppression [1,2,3,4].
The unique characteristics of terror-related explosion events require a thorough review to prepare all levels of medical treatment for casualties of such incidents, from the prehospital setting, through the hospitals, and all the way to rehabilitation and mental health. This chapter will therefore discuss the main operational considerations stemming from the modern trends of terror explosion injuries noted in recent evidence-based research. In particular, the chapter will describe how explosive device characteristics interact with physical location of the explosion to define the patterns of injury and required clinical resources, as well as the influence of the general setting of the event (military/civilian, urban/rural) on scene and medical management.
Epidemiology of Explosion Injuries
Blast casualties are different from explosion casualties (e.g., industrial explosion), and both are different from terror-related explosion casualties. While the first two might demonstrate mostly the classical blast injuries, such as traumatic amputations , blast lung and intestine perforation, accompanied by less severe injuries, such as ruptured tympanic membrane [1, 5], the casualties of terror-related explosions will likely present a more diverse and complex pattern of injury.
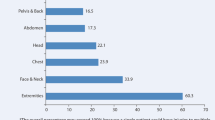
For instance, studies from the Second Intifada in Israel (2000–2005) show that about two-thirds of the blast victims presented with penetrating injuries, 48% suffered from blunt injuries, and high-severity burns were presented with 20% of terror explosion victims (Fig. 4.1) [6, 7]. A large proportion of secondary blast injuries will be to the extremities, followed by torso injuries [6]. Tertiary trauma will lead to contusions, bone and skull fractures. Blast trauma per se is also encountered but on a lower scale than expected: a recent study has found that only 14% of primary blast injuries were present among explosion survivors [7]. A relatively high proportion of casualties (~19%) presented with combined injuries (e.g., blast and penetrating). Similar patterns of injury from explosive incidents were reported from fighting in Iraq and Afghanistan, especially after the conflicts have entered the counter-insurgency phase [8, 9].
Perhaps one of the most important characteristic of terror-related explosion injuries, however, is multidimensional injury pattern (MIP), that is, the manifestation of injuries of different mechanisms in the same patient. MIP contributes to an overall higher injury severity and lower odds of survival [8]. Injuries to multiple body regions are also to be expected.
On the other hand, when reviewing the full spectrum of past explosion events, the first thing to notice is how different all these events are both in their contextual profile and the patterns of casualties they produce. Some of the events, such as criminal assassinations and home accidents, may produce only a single casualty; others, such as most terror attacks, produce significantly more treatable injuries than deaths, whereas explosions resulting in building collapse may cause an appalling death rate on par with the volume of treatable injuries. The patterns of treatable injuries from different explosion events also seem to differ greatly, even when the events themselves belong to a similar category, such as terror attacks or industrial accidents.
The extent to which individuals become affected by explosion events, as well as the severity of injuries, number of casualties, types of injuries, and medical resources needed, varies in accordance with several factors, including type of explosive device, physical location of the detonation, and the setting of the event.
Type of Explosive Devices
The results of a terror-related explosion incident will greatly depend on the type of explosive device and the way it is used to inflict damage. A suicide bomber vest will disperse shrapnel at the torso level in a circular pattern causing upper body injuries to people in the vicinity of the explosion, while an improvised explosive device (IED) left on the ground will mostly injure the lower body parts [6, 10]. A vehicle-based explosive device (VBIED) will contain much more explosives and will therefore cause much more damage than a suicide bomber; however, an explosion at a munitions factory or storage facility is likely to be of incomparably bigger proportions. A small charge implanted in a car for criminal assassination will rarely physically injure someone outside the car. On the other hand, terrorists may use more than one explosive device or even more than one kind of device in the same attack in order to maximize the number of casualties. Finally, a high-explosive aircraft bomb will mostly cause blast and penetrating injuries, whereas a fuel/air bomb dropped by the same aircraft will cause mostly burns.
Another important aspect to consider in type of explosive device is the use of metal fragments in order to maximize injury in terroristic explosions. Often, these elements will cause penetrating injuries that pose a medical challenge on their own merits. Yet, as suggested already above, when it comes to terrorism we can expect everything. For example, when executing the terror attack at Mike’s Place Pub in Tel-Aviv on April 30, 2003, in order to get past security guards, the terrorist avoided using any metal components in the explosive device, including shrapnel. While the results of this attack were horrific, the casualties presented with almost no penetrating injuries, rather only blast, blunt, and burns injuries. The only penetrating wounds were caused by glass broken on site as a result of the explosion.
The type of explosive device will also likely influence the way it is used. Perhaps one of the most prominent examples illustrating this is the Boston Marathon bombings on April 15, 2013. The perpetrators of this terror attack used a pressure cooker bomb as an IED. This low-yield IED, given its shape and weight, was left by the terrorists near a building and on the ground. The explosion resulted in predominantly secondary blast injuries (i.e., penetrating wounds caused by ball bearings, nails, screws, and pieces of the pressure cooker housing acting as shrapnel) mostly to the lower limbs. Almost three-quarters (32 out of 43) of patients undergoing radiography in this event retained shrapnel fragments, mostly embedded in the lower extremities [3].
In striking contrast to the Boston marathon bombing, we describe one of the suicide attacks that occurred on a bus to Jerusalem in 1979. As the bus was making its way to Jerusalem, near Ma’ale Edumim, on the outskirts of the city, a bomb exploded inside the bus. The terrorists placed it in the overhead compartments usually used to place small carry-on bags. The resulting casualties suffered mostly from head and chest injuries. In other suicide terror incidents, in which terrorists carried their explosive vest on their torso, the resulting casualties demonstrated scattered injuries to all body parts.
Indeed, no two explosions are the same. This is when dealing with terror-related explosions. The characteristics of these events change greatly depending on a multitude of factors contributing to the outcomes of the event. The examples provided above from Boston and Israel are helpful in demonstrating the difficulty in establishing a unified profile of explosion events. In essence, this means that emergency planners, as well as medical practitioners, should work on principles rather than protocols when preparing for and responding to an explosion event.
Physical Location of the Detonation
To a great extent, the results of an explosion incident depend not only on the explosive, penetrating agents, and resulting fireball but also their interaction with the surrounding space. Depending on the level of confinement of the location and its structural composition, the severity of injuries may differ. For example, confined spaces may enhance the impact on the potential victims through the refraction of the blast wave from the walls and the containment of the fireball, resulting in extremely high temperatures [4, 5, 11]. On the other hand, more open spaces will quickly dissipate the shockwave and fireball, but will provide a noninhibited pathway for the flying debris and shrapnel. While these differences seem highly intuitive, it is worth noting that researchers are still debating whether or not these basic differences are enough to properly explain the resulting variation in the patterns of injuries (Table 4.1).
Thus, it was found that that the injury patterns are different between a simple explosion inside a building and an explosion strong enough to cause the building to collapse, as in the latter case the addition of crush injuries heightens the overall injury severity, with the situation further aggravated by the need to extract the victims from under the rubble [11]. Explosions inside buildings are characterized by a larger proportion of critical (ISS 25+) injuries, among all due to severe TBI and abdomen injuries and a combination of multiple injuries [7].
The classification of open versus closed spaces, in the context of explosions, was further developed in light of terror-related explosion incidents. In Israel, for example, vast differences in patterns of injuries were observed between casualties of explosions happening inside a building versus inside a bus, both considered as “closed spaces.” It was also found that buses, and by association train cars , could be considered as a kind of “hyper-confined” spaces. This is true because of them being narrow and with lower ceilings, having metal rather than concrete walls, and usually containing a dense crowd of potential victims before the explosion. Buses/train cars are different from inside buildings, as the higher confinement cause greater immediate mortality due to blast and higher proportion of primary blast injuries among survivors [7, 12]. Among survivors of the initial explosion inside a bus, a relatively high proportion (19%) of severe chest injuries could be encountered; almost half of the survivors will sustain injuries to multiple body regions [7]. Despite the differences, in all confined settings an explosion results in increased frequency of burns because even though the effects of a blast wave inside a confined space may vary depending on the context, the containment by four walls will consistently increase the effect of the fireball produced by the explosion [7, 11].
An additional variation regarding explosions involving buses is between explosions inside buses and near them. In cases when the suicide bomber was not allowed to enter or an intentional attack was performed by closing to a bus with a VBIED, it was found that the injuries are much less severe, with most injuries being superficial due to glass fragments. Data also shows an increased volume of lower extremity fractures due to bus walls bending inwards [13].
Lastly, some significant variations in injury profiles were registered regarding so called semi-confined or semi-open spaces, such as open markets and restaurants, as well as explosions next to a building wall [7, 14]. A somber example of this scenario was the Dolphinarium nightclub explosion in Israel that happened on June 1, 2001. This suicide bombing killed 21 teenagers waiting in line outside next to the concrete wall and injured an additional 100 civilians. After inquiring into the exceptionally high mortality of this incident, it was found that in this scenario the refraction of the blast wave from a single wall may have magnified the blast wave effect and increased both the volume and the severity of casualties [7]. The presence of a large crowd of people next to a building wall in semi-open environments also explains the higher incidence of primary blast injuries in explosions near buildings as compared to those that happened inside buildings, because people already inside a building are not necessarily clustered near the walls and could be more freely distributed through the inner space.
Regarding completely open settings, it is important to remember that physical factors at play here are less universal and homogenous. Therefore, the resulting impact is being strongly dependent on the profile of the event (e.g., the number and the composition of explosive devices and the density of the crowd [15]). In an open setting, the blast overpressure and thermal energy dissipate rapidly and penetrate trauma by shrapnel elements predominates [4, 11]. The most frequent injuries expected would be to the abdomen and extremities [7, 11].
In terms of injury severity, the proportion of severe injuries tends to increase almost linearly in relation to the level of enclosure, it being the highest inside buildings (especially if the building collapses), followed by explosions inside buses and train cars, explosions near buildings, and open spaces [7] (Fig. 4.2). The lowest proportion of severe injuries is usually found in explosions near buses, as in this case the metal walls of the bus and sometimes its motor serve to protect people sitting inside. This hierarchy of injury severity is important to comprehend as it affects the requirements for hospital resources following the explosion event. Victims arriving from more enclosed environments require proportionally more surgeries and ICU beds and have higher in-hospital mortality.
Setting of the Event
Whether an explosion will result in fewer or many casualties and/or higher or lower levels of injury severity also depends on circumstantial factors associated with the event’s setting. For example, the density of services provided in the vicinity of the event, namely, whether the event takes place in urban or rural setting. Geography is expected to lead to dramatic differences in event management and patient outcomes for given injury patterns.
With the exception of industrial explosions, the majority of explosions, especially terror-related ones, occur in urban settings. This is true in light of the larger pool of high-profile targets and greater chances to find large crowds [16]. On the other hand, security may be perceived as lower in the countryside, inviting a potential attack, perhaps with additional assault measures other than explosives. For example, during a double terror attack at the Utoya Island resort in Norway (2011), the terrorist detonated explosive devices in Oslo, prior to executing a firearms-based murder spree [17]. Israel has abundant experience in multimodal terror attacks, yet accounts of such incidents were also recorded in Madrid train bombings, Boston Marathon bombing, London underground bombings, etc. [10, 18, 19].
Urban and rural settings also differ on the kind of explosion we expect to occur in them [16]. For instance, most criminal acts utilizing explosives, such as throwing grenades or planting bombs into cars for assassinations or Mafia-style threatening, tend to happen more frequently in urban environments. In rural places, on the contrary, we can expect more industrial explosions, as industrial zones in developed countries rarely remain within city limits. Domestic explosive incidents (i.e., those happening inside a house) may happen both in urban and rural environments, though their origins are likely to be different, with natural gas explosions more characteristic to cities and agricultural assets, such as fertilizers or grain storage facilities, more of a blast risk in the countryside.
Perhaps the most important aspect highlighting the differences between urban and rural settings is the accessibility to medical resources and services (i.e., “services density”). The number and the quality of hospitals and EMS in the urban area exceed that which exists in a rural setting. With longer transport times to medical treatment, as is the case in most rural settings, there are significantly higher odds of aid arriving too late and patients deteriorating while waiting for definitive treatment. A large number of severe patients may also overwhelm areas with lower health services density and quality of trauma-related healthcare services. In many cases, explosion events in rural areas require utilization of helicopters as a main mean of transportation to and from the scene. In case of MCE, this may lead to evacuation performed by medical priorities , with patients most likely to benefit from immediate evacuation receiving priority over others. However, lack of proper facilities for utilizing ambulance or military/police helicopters may still cause significant delays in patient evacuation, as happened in the Utoya attack [17].
While the potential abundance of healthcare services in urban and especially metropolitan areas is clearly an advantage, the inability to utilize them properly can quickly become a challenge. All attempts to get to the scene or evacuate casualties from it could be thwarted by intensive city traffic, the disturbance of the transport grid due to a serious explosion event, and the need to employ security and safety. While on the scene in urban environment, systematic triage has to be employed in order to guide evacuation efforts to different hospitals based on proximity and level of care, the number and severity of remaining casualties, and available transportation means. Some evacuations may be performed by the police or by the bystanders; however, this uncoordinated effort may lead to crowding of the closest hospitals, while other facilities in the same city used suboptimally [10]. Due to these challenges, in a rural environment, it could be more advisable to “bring the hospital to the event” (“Stay and Play”) than to “bring the event to the hospital” (“Scoop and Run”), as practiced in urban scenarios.
Military Versus Civilian Contexts: Explosive Devices, Injuries, and Operational Considerations
Injuries caused by explosions are well documented in the context of combat zones [20]. Explosions represent the most common mechanism of injury (78%) and death (63%) on the modern battlefield [21]. According to [22], nearly three-quarters of all combat injuries over the period from 2005 to 2009 (31 per 10,000 deployed) were due to explosions. In the recent conflicts in Iraq and Afghanistan, the incidence of primary blast injury in US military personnel was 12.2%; however, blast overpressure was the cause of death in only 1.5% [5]. Much of our understanding of blast injuries stems from military-based contexts. Yet, there is a growing threat of blast injury in civilian contexts. This threat spans from terrorism [8], through criminal acts, all the way to industrial accidents [23].
Due to the extensive experience with blast trauma obtained in the recent military conflicts, it is very tempting to rely on knowledge from military medicine in regards to this type of injury event. However, injuries from terror and war are not necessarily comparable [24]. There are vast differences between the military and the civilian contexts of explosion injuries, as well as between the different types of civilian contexts, such as terror-related, industrial/domestic accidents, and criminal activities. These differences concern both the explosive devices and circumstances causing the explosion, the epidemiology of produced injuries, the location of event site, and the balance between vulnerabilities and protective factors important for preparedness and response (Table 4.2). Therefore, extrapolation from military texts, such as the Combat Casualty Care textbook, should be undertaken with caution [2]. According to Reade [2]: “Mistaken preconceptions of the medical consequences of explosion can lead planners and managers to allocate resources incorrectly and clinicians to focus attention away from the most likely pathology.”
The differences between military- and civilian-based explosion scenario are ample. It is worthwhile to consider several of the prominent ones in order to highlight the importance in additional research and study into civilian contexts to solidify our understanding of blast injuries in modern times. Perhaps the most obvious difference between the two contexts is demographics. The demographic composition of military and civilian casualty population is very different, with military explosion victims being much younger and mostly male while terror victims have a wider age and gender distribution [24]. This is especially important due to higher incidence of pediatric and geriatric cases among terror victims, with both groups presenting unique challenges for the responders. Blast injuries of children younger than 11 years old present a specifically major challenge, due to their higher rates of traumatic brain injury (TBI), lower rates of injuries to extremities, and overall higher injury severity [25].
In addition, considering the differences in target populations across the two contexts (i.e., soldiers versus civilians), it is readily understandable why military explosion incidents cause less-severe injuries; soldiers wildly use protective gear, such as helmets and body armor [25, 26]. With the most important body areas protected, injury patterns in military casualties will be very different from civilians. Civilian victims of terror explosions are also worse off in terms of sustained injuries, as a result of a combination of penetrating injuries, with blast, blunt, and burn injuries occurring to the same patient. Aiming to cause more casualties, terrorists equip their bombs with penetrating agents, such as bearing balls, nails, nuts, and bolts, resulting in a large volume of penetrating injuries. This improvised shrapnel may result in multiple injuries of the same patient, while increasing the demand for surgeries for the patients arriving from the event [8].
Reade [2] provides a detailed account of the epidemiology of civilian explosion injuries. According to the author, most survivors of explosion injury do not have clinically significant primary blast trauma. Mainly, civilian victims of terrorism, for example, present with penetrating low-energy transfer blast fragmentation wounds or crush injury in the case of structural collapse. The number of patients and the number of affected body parts is the main difference between blast and nonblast civilian victims. Table 4.2 summarizes the characteristics of civilian explosion incidents [2].
The literature provides additional insights into the unique characteristics and epidemiology of civilian explosion injuries. For instance, Regens, Schultheiss, and Mould [27] surveyed the data of 77,258 successful terrorist MCIs that occurred between 1970 and 2013 that involved the use of explosives, firearms, and/or incendiaries. They reported that explosions cause more complex damage than other conventional weapon types, including traumatic amputation of extremities, ruptured eardrums, mild-to-severe traumatic brain injury, and/or penetrating injuries from shrapnel. Supporting evidence from [28] notes that conventional blunt, penetrating, and thermal trauma are the most common forms of injury following high-explosive detonations. Soft tissue, orthopedic, and head injuries dominate, and severe head injury is a leading cause of death in explosion victims.
In a study published in 2010, Peleg et al. demonstrated the abovementioned differences between civilian and military casualties when comparing injury data of both cohorts in the context of war (Second Lebanon War in 2006) and terrorism (Second Intifada during 2000–2003). According to the study, critical injuries and multiple body regions injuries were more likely in terror scenarios rather than war. Soldiers tended to present with less severe injuries from war than terror incidents. In-hospital mortality was higher in terror scenarios (7%) compared to war (2%), particularly among civilians [24].
Moreover, the mechanism of injury varied for civilians and soldiers according to conflict type. Specifically, the study reported that civilians in terror compared with war presented with less-blunt injuries (36% vs 45%, p = 0.042), approximately the same rate of penetrating injuries (~70%) and more burn injuries (10% vs 2%, p = 0.002). Civilians and soldiers also differed in injuries caused by multiple mechanisms with a prevalence of ~20% among civilians compared to only 10% among soldiers. Differences were also observed in terms of injury severity. Mild wounds (ISS: 1–8) were reported for 53% of civilians and 67% of soldiers, whereas critical wounds (ISS: 25+) reported for 17% of civilians and 6% of soldiers. Civilians compared with soldiers were twice as likely to present with internal wounds (30% vs 15%, respectively). See also Table 4.3 [24]. Broadly, terror victims were more severely wounded than war casualties.
Other Civilian Considerations of Explosion Events
In the overall context of explosion events, it is imperative to discuss also nonintentional events involving explosives, such as domestic or industrial accidents. These incidents may involve a larger volume of casualties. A domestic explosion scenario may result from gas, gasoline, or boiler explosions and fuel-air mixture explosions, such as sawdust, grain dust, or even pain [29,30,31]. Electric hardware and fireworks accidents are also common [2]. Industrial explosions mainly result from overpressured gases and liquids, misuse of industrial explosives and faulty machinery. Accidents at ammunition storage facilities and fertilizer plants may be especially destructive, causing vast devastation and significant mortality and morbidity, sometimes measured in the hundreds [29, 30].
In these scenarios, casualties suffering from severe blast trauma would likely be declared as fatalities on-scene, while patients presenting for treatment would suffer mostly from a combination of blunt and penetrating trauma, with burns and tympanic blast injuries also present in some patients [29, 30]. Entrapment of victims due to building collapse and continuing fires endangering both victims and the first responders are also likely. Additionally, as most industrial facilities are located in a nonurban environment, the evacuation times may be longer, with coordination challenges related to destination protocols and mode of transportation.
Industrial accidents resulting in explosions are widely documented [23, 30]. We can learn about the injury characteristics of such events from the example of the incident in the West Fertilizer Company plant in West, Texas. On April 17, 2013, a fire and subsequent explosion occurred at the factory, causing severe damage to the nearby neighborhood. A total of 252 nonfatal casualties directly related to the explosion were treated. Of those, about half had documented abrasions/contusions and lacerations/penetrating trauma. Other injuries included TBI (21%), tinnitus/hearing problems (14%), eye injuries (12%), inhalational injuries (12%), sprain/strain (11%), fractures/dislocations (8%), tympanic membrane ruptures (5%), and burns (2%). Primary blast injuries, including pneumothorax, blast lung, and blast abdomen injuries, were seen in 5% of patients [29].
Implications for Preparedness and Treatment
The most important aspect of explosion events is how they are different in terms of their geographic location and the parameters of their physical environment, their social context, and the technical characteristics of the explosive mechanism or device behind the explosion. These differences cause significant variation in the volume and profile of casualties, the speed and the complexity of the response, as well as the consequent demand for medical resources. With so many factors influencing the response effort, it is nigh impossible to develop a universal system of preparedness for explosion events, even if we narrow our scope exclusively to MCEs. Because of a multitude of potential scenarios, it is hard to produce a point-by-point response plan that will be robust enough to guide the responders in each specific scenario.
A more optimal approach would be to rely not on protocols but on several universal, yet flexible principles, which will have the potential to be applicable to every scenario. Such an approach will enable quick adaptation to most needs raised by any given situation without unnecessary encumbrance by strict protocols. These principles should concern the basics of scene management, the knowledge on potential challenges and contradictions characteristic to explosion casualties, the priorities and procedures for triage at different stages and for evacuation, the capabilities of available response teams and coordination between them, and the limitations and advantages incurred by different contexts and locations.
Conclusion
No two explosions are the same. This is especially true when dealing with terror-related explosion incidents, which often result in diverse and complex patterns of injuries. The epidemiology of explosion injuries, as learned from decades of experience with terror-related and other explosion incidents, is highly complex and requires careful attention to details if one wishes to tailor the response adequately. In this chapter, we demonstrated the effects of different factors on injury pattern as a result of explosions. We highlighted the importance of the explosive device, the location of the detonation, and the general setting of the incident over the outcomes. Lessons learned from years of experience, as well as carefully crafted research spanning over decades, provide the evidence-based conclusions needed to improve and perfect the medical response to terror-related and other explosion incident.
References
DePalma RG, Burris DG, Champion HR, Hodgson MJ. Blast injuries. N Engl J Med. 2005;352(13):1335–42.
Reade MC. Blast injury - what to expect in civilian vs military contexts. ICU Manag Pract. 2015;15(4):164–6.
Singh AK, Ditkofsky NG, York JD, Abujudeh HH, Avery LA, Brunner JF, et al. Blast injuries: from improvised explosive device blasts to the Boston Marathon bombing. Radiographics. 2016;36(1):295–307.
Beaven A, Parker P. Blast injuries: a guide for the civilian surgeon. Surgery. 2018;36(8):394–401.
Champion HR, Holcomb JB, Young LA. Injuries from explosions: physics, biophysics, pathology, and required research focus. J Trauma Acute Care Surg. 2009;66(5):1468–77.
Aharonson-Daniel L, Klein Y, Peleg K. Israel Trauma Group. Suicide bombers form a new injury profile. Ann Surg. 2006;244(6):1018–23.
Rozenfeld M, Givon A, Shenhar G, Renert L, Peleg K. A new paradigm of injuries from terrorist explosions as a function of explosion setting type. Ann Surg. 2016;263(6):1228–34.
Kluger Y, Kashuk J, Mayo A. Terror bombing-mechanisms, consequences and implications. Scand J Surg. 2004;93(1):11–4.
Kelly JF, Ritenour AE, McLaughlin DF, Bagg KA, Apodaca AN, Mallak CT, et al. Injury severity and causes of death from operation Iraqi freedom and operation enduring freedom: 2003–2004 versus 2006. J Trauma. 2008;64:S21–7.
Kellermann AL, Peleg K. Lessons from Boston. N Engl J Med. 2013;368:1956–7.
Arnold JL, Halpern P, Tsai M-C, Smithline H. Mass casualty terrorist bombings: a comparison of outcomes by bombing type. Ann Emerg Med. 2004;43:263–73.
Kosashvili Y, Loebenberg MI, Lin G, Peleg K, Feigenberg Z, Kluger Y, et al. Medical consequences of suicide bombing mass casualty incidents: the impact of explosion setting on injury patterns. Injury. 2009;40:698–702.
Golan R, Soffer D, Givon A, Israel Trauma Group, Peleg K. The ins and outs of terrorist bus explosions: injury profiles of on-board explosions versus explosions occurring adjacent to a bus. Injury. 2014;45:39–43.
Almogy G, Rivkind AI. Terror in the 21st century: milestones and prospects--part I. Curr Probl Surg. 2007;44(8):496–554.
Kress M. The effect of crowd density on the expected number of causalities in a suicide attack. Nav Res Logisit. 2005;52:22–9.
Stamm BH. Terrorism risks in rural and frontier America. IEEE Eng Med Biol. 2002;21(5):100–11.
Sollid SJ, Rimstad R, Rehn M, Nakstad AR, Tomlinson A-E, Strand T, et al. Oslo government district bombing and Utøya island shooting July 22, 2011: the immediate prehospital emergency medical service response. Scand J Trauma Resusc Emerg Med. 2012;20(1):3.
Aylwin CJ, König TC, Brennan NW, Shirley PG, Davies G, Walsh MS, et al. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2007;368(9554):2219–25.
De Ceballos JPG, Turégano-Fuentes F, Perez-Diaz D, Sanz-Sanchez M, Martin-Llorente C, Guerrero-Sanz JE. 11 March 2004: the terrorist bomb explosions in Madrid, Spain--an analysis of the logistics, injuries sustained and clinical management of casualties treated at the closest hospital. Crit Care. 2005;9(1):104–11.
McGuire R, Hepper A, Harrison K. From Northern Ireland to Afghanistan: half a century of blast injuries. J R Army Med Corps. 2019;165(1):27–32.
Cannon JW, Hofmann LJ, Glasgow SC, Potter BK, Rodriguez CJ, Cancio LC, et al. Dismounted complex blast injuries: a comprehensive review of the modern combat experience. J Am Coll Surg. 2016;223(4):652–64.
Greer N, Sayer N, Kramer M, Koeller E, Velasquez T, Wilt TJ. Prevalence and epidemiology of combat blast injuries from the Military Cohort 2001–2014. VA ESP Project #09–009; 2016.
Pittman W, Han Z, Harding B, Rosas C, Jiang J, Pineda A, et al. Lessons to be learned from an analysis of ammonium nitrate disasters in the last 100 years. J Hazard Mater. 2014;280:472–7.
Peleg K, Jaffe DH. Israel Trauma Group. Are injuries from terror and war similar?: a comparison study of civilians and soldiers. Ann Surg. 2010;252(2):363–9.
Jaffe DH, Peleg P, Israel Trauma Group. Explosive injuries: a comparison of children, adolescents, and adults. Ann Surg. 2010;251:138–43.
Peleg K, Rivkind A, Aharonson-Daniel L, Israel Trauma Group. Does body armor protect from firearm injuries? J Am Coll Surg. 2006;202:643–8.
Regens JL, Schultheiss A, Mould N. Regional variation in causes of injuries among terrorism victims for mass casualty events. Front Public Health. 2015;3:198.
Wightman JM, Gladish SL. Explosions and blast injuries. Ann Emerg Med. 2001;37(6):664–78.
Metzger K, Akram H, Feldt B, Stone K, Alvey S, Henley S, et al. Epidemiologic investigation of injuries associated with the 2013 fertilizer plant explosion in West, Texas. Disaster Med Public Health Prep. 2016;10(4):583–90.
Laboureur DM, Han Z, Harding BZ, Pineda A, Pittman WC, Rosas C, et al. Case study and lessons learned from the ammonium nitrate explosion at the West Fertilizer facility. J Hazard Mater. 2016;308:164–72.
Kao H-K, Yung Loh CY, Kou H-W, Kao K-C, Hu H-C, Chang C-M, et al. Optimizing mass casualty burns intensive care organization and treatment using evidence-based outcome predictors. Burns. 2018;44(5:1077–82.
Weil YA, Mosheiff R, Liebergall M. Blast and penetrating fragment injuries to the extremities. J Am Acad Orthop Surg. 2006;14:S136–S139.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Peleg, K., Bodas, M., Rozenfeld, M. (2020). Operational Considerations: Review of Contemporary Data. In: Callaway, D., Burstein, J. (eds) Operational and Medical Management of Explosive and Blast Incidents. Springer, Cham. https://doi.org/10.1007/978-3-030-40655-4_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-40655-4_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40654-7
Online ISBN: 978-3-030-40655-4
eBook Packages: MedicineMedicine (R0)