Abstract
Children exposed to blast events ranging from low-energy fireworks to high-energy explosions can suffer severe, life-threatening injuries. Optimizing survival for these young victims requires a detailed understanding of the common injury patterns, appreciation of the physiologic response of children to blast injuries, and availability of the resources and supplies needed to manage critically injured children. This chapter reviews the epidemiology of blast injuries in children, the physiologic response to blast injury, a recommended approach to injury identification in blast-injured children, and an overview of specific injuries by organ system.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Over the past century, a number of blast events have involved children, starting with the massive explosion in Halifax Harbor in 1917 through the Boston Marathon bombing in 2013 [1,2,3,4]. In fact, because of Dr. Ladd’s involvement in caring for injured children in Halifax, that devastating event has become an important part of the lore surrounding the birth of pediatric surgery. Since then, fireworks injuries, civilian terror incidents, and modern warfare have all led to the further characterization of the unique aspects of pediatric physiology, management, and outcomes following a blast event. Children, especially very young children, consistently have worse outcomes than their adult counterparts after exposure to a blast [5,6,7,8]. Thus, there appears to be an ongoing gap in knowledge and training regarding care for the youngest patients. Optimizing survival for these young victims requires a detailed understanding of the common injury patterns, appreciation of the physiologic response of children to blast injuries, and availability of the resources and supplies needed to manage critically injured children [9]. In this chapter, we advance the discussion from the emergency department section. We will discuss the epidemiology of pediatric blast injuries, review pediatric-specific anatomy and physiology relevant to blast injuries, and describe specific injury patterns and their management.
Epidemiology
Pediatric blast injuries can be divided into those resulting from high- and low-energy ordinance. The most common injuries in the United States are overwhelmingly secondary to low-energy blasts from civilian small ordinance, such as fireworks. High-energy blast mechanisms usually occur in the setting of either civilian terror events or combat.
Fireworks Injuries
Inappropriate use of any type of firework can lead to severe injury – indeed, every type of legally available firework has been implicated in either injury or death [10]. A study by Billrock et al. analyzing data available through the US Consumer Product Safety Commission estimated that greater than 130,000 patients under 20 years of age received treatment in emergency departments for nonfatal firework-related injuries between 1990 and 2014 [11]. Nearly half of all firework-related injuries reported from June to July 2014 in their study occurred in patients under 20 years of age. A single-institution descriptive study from Children’s Mercy in Kansas city revealed that 95% of children injured by fireworks are injured during the 3 weeks surrounding Independence Day [12]. This problem is not unique to celebrations in the United States as reports of blast events during celebrations are present in the international literature as well [13, 14].
No matter the country of origin, injuries are more likely to occur in males and the primary handler of the firework [11, 13, 14]. In the United States, males are three times more likely than females to be injured [11]. Injuries are most likely to the hand (30%), head and neck (22%), and eye (21%) and include most commonly burns, abrasions/contusions, and lacerations. Lower extremity injuries are more prevalent in children aged 0–9 than older children [11]. Unsurprisingly, firecrackers are the most commonly implicated firework; however, injuries due to sparklers are the most common in younger children. Injures are usually secondary to firework explosion; however young children are more likely to be struck by the firework than to be involved in the blast itself [11]. The vast majority of injuries, however, is minor with >90% of patients able to be discharged directly from the emergency department (ED).
Legislation and advocacy have the potential to decrease these entirely preventable events. During the 25 years of the Billrock study, the incidence of pediatric fireworks injuries decreased by 30% [11]. Although the overall incidence of fireworks injuries is decreasing, the rate of inpatient admission is significantly increasing, indicating that when injuries do occur, they are more severe than in times past [15]. Though fireworks laws have become less stringent over time, a strong recommendation is given by the American Academy of Pediatrics to restrict use to demonstration professionals [16] . They recommend families enjoy professional shows rather than participate in private festivities [16].
Civilian Terror Incidents
Children have been increasingly exposed to civilian terror events around the world including the Jerusalem bombings, Oklahoma City bombing, Madrid train bombings, and Boston Marathon bombing, among others [4, 17,18,19]. The majority of persons injured in these events are adults. Yet, the presence of multiple day care centers within proximity to the Alfred P. Murrah Federal Building in Oklahoma City lead to a large number of pediatric injuries. Unfortunately, this incident contributed a robust description of pediatric injury patterns as a result of high-energy blast.
Overall 66 children were victims of the incident in Oklahoma City with 40 treated and released. Among this population, the injury patterns resembled those of the adults injured on that day [20]. Tympanic membrane perforations were extremely common in children, with 25/30 patients from one of the nearby day care centers affected. Seven pediatric patients were hospitalized, and all required admission to the PICU and surgical management. Nineteen children died immediately after the blast. Among the mortalities and the severely injured, head injuries predominated, with severe skull fractures and partial or total cerebral evisceration common [20]. Also common were severe, multiple, orthopedic injures, including traumatic amputations [20]. A retrospective analysis of the Bath School bombing of 1927, an explosive attack with many similarities to the Oklahoma City bombing, reveals a similar injury pattern in children, where injuries to the face, head, and neck predominated [21].
Another detailed assessment of pediatric injuries after terrorist action was recently published from the Israel National Trauma Registry. Ahronson-Daniel et al. compared injury patterns among terror-injured versus non-terror-injured children in the Israel National Trauma Registry from October 2000 to December 2001 [22]. At that time, terror acts against civilian children became the second leading cause of death for children in Israel [23]. Terror-related injuries in children were mostly due to explosion (67%) and resulted in multiple injuries in 65% compared to 65% rate of solitary injury in non-terror trauma victims. The rate of penetrating injury was 54% in terror-related incidents versus 9% in non-terror victims. In the Israeli experience, the majority of explosive devices was packed with projectile foreign bodies that inflicted devastating secondary blast injuries [22]. Burns as a result of terror-related incidents were usually accompanied by penetrating injuries and were more severe . These injury patterns translated into a doubling in OR utilization in terror-injured children versus non-terror injured as well as higher ICU utilization and longer hospital stays [22].
Another series from the Israel National Trauma Registry by Jaffe et al. compared injury patterns among children, adolescents, and adults after terror explosions [24]. Though not statistically significant, there was a suggestion that infants and toddlers were more likely to sustain blunt injuries and less likely to sustain penetrating injury and that infants and toddlers were less likely to sustain injuries to multiple body regions [24]. Injuries among children were more likely to be severe compared to adults (27% vs 12% with ISS 16–24), and children were more likely to have traumatic brain injury (35% vs 20%, p = 0.012) and less likely to have open wounds compared to adults [24].
Combat Blast Injuries
Strategies utilizing explosive devices to cause death/injury from blast have become commonplace in the modern battlespace. The IED has become a weapon of choice of violent extremist organizations, and children are frequently collateral casualties. The experience of treating these casualties is now becoming well documented from US and European military treatment facilities from the conflicts in Iraq and Afghanistan. In an analysis of civilian blast injuries from the JTTR, 1822 patients under age 20 were treated between 2002 and 2010 [6]. IED was the most common blast mechanism across age groups [6]. Most patients were male and greater than 70% had more than one affected body region. Burns and extremity/pelvic injuries were the most common (70% and 50%, respectively) overall, while burns and head and neck injuries were the most common for those less than 15 years old. Chest injuries were the least common, although when present, they tended to be severe (92% with a chest injury had a Chest AIS 3–6) [6]. This is similar to findings in one series of adult victims of civilian terror incidents in Madrid, where the presence of chest injury indicates a high burden of injury [18].
Overall, Edwards et al. found a mortality of 7.8% for children compared to a documented approximately 3% mortality rate for US military casualties [6]. In a subsequent analysis, younger children (less than 3 years) required more neurosurgical interventions, while older children required more interventions for extremity injuries including repeated debridement [25]. A review of neurosurgical cases from the Craig Joint Theater Hospital from 2007 to 2009 reveals that the most common neurosurgical procedure performed on children during that time was craniotomy/craniectomy for penetrating cranial injury secondary to blast in the majority of cases [26]. Pediatric patients presenting with vascular injury to facilities recorded in the JTTR were most likely to be injured by blast (58%), and these patients had a higher incidence of chest trauma (23%) (although chest injuries are not broken down by mechanism) than in other series with a high risk ratio for mortality in those with torso injuries [27].
These patterns of injury are consistent among reports from coalition partners, who describe a similarly high mortality rate for blast-injured children. There seems to be a preponderance of lower extremity injury and more severe head injury in younger children compared to older children and adults [28,29,30]. The civil war in Syria has also produced a large number of pediatric casualties. Though the use of conventional weapons is more common in this conflict as compared to Iraq and Afghanistan, fragmentation injury is the most common mechanism (51%) seen at an Israeli Role 1 facility and extremity and head/cervical spine injuries the most common anatomic sites [31].
These children, injured as collateral casualties, consume a large portion of deployed resources. In a retrospective review of all patients admitted to combat support hospitals and forward surgical teams in Iraq and Afghanistan, Borgman et al. demonstrated that, while pediatric patients only represented 5.8% of admissions, they represent 11% of all bed days. Borgman et al. suggest these numbers may underestimate the actual number of children treated due to a lag in capturing all patients admitted at the beginning of the conflict.
Physiology and Pediatric Vulnerabilities
Children present with unique vulnerabilities to blast injury secondary to multiple aspects of their developing/juvenile anatomy, physiology, and behavior [9]. Many of these qualities make children more vulnerable to injuries of any mechanism. Table 36.1 demonstrates pediatric-specific vulnerabilities by blast mechanism.
In the case of fireworks and unexploded ordinance and/or landmines (all preventable blast injuries), a lack of awareness of potential danger may contribute to some of the observed injuries. This is demonstrated by the pattern of injuries associated with fireworks by age. School-age children and teens are more likely to be injured by firecrackers and illegal fireworks as the handler than younger children/infants. Younger children have limited mobility and are thus more likely to suffer primary blast injuries from fireworks [11]. This low situational awareness and poor mobility may explain some of the wartime observations as well, whereas school-age children are more likely to suffer primary, secondary, and tertiary blast injuries [25]. Furthermore, the high incidence of face/eye injuries in younger patients likely results from curiosity.
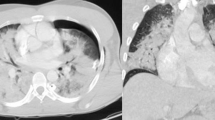
Children are clearly more susceptible to head injury than their adult counterparts secondary to relatively large head size compared to the rest of the body (Fig. 36.1) [17, 20, 32, 33]. A thorough review of anatomic and physiologic differences between adults and children with TBI was recently published by Figaji [33]. As with head-injured children from mechanisms other than blast, preverbal children can present a challenge regarding mental status assessment. It is unknown how primary blast TBI affects the developing brain and the effect that surgical decompression has on outcomes compared to adults, though some posit that children may have a greater capacity for neurologic recovery after TBI than adult counterparts; however, data to support this hypothesis are lacking [33].
Pediatric patient with a secondary blast injury resulting in a penetrating brain injury (a). The fragment was directly adjacent to the sagittal sinus (b), but upon careful exposure and removal of the fragment (c), the sinus was found to be uninjured. The patient’s cranial defect was repaired (d), and she had a full recovery
The pediatric chest presents specific vulnerabilities as well that can be assumed based on anatomy/physiology and epidemiologic observation. From a pulmonary standpoint, there is no indication that children are more susceptible to primary lung blast injury than adults. As above, when a child has injuries to the chest, they are more likely to be severely ill at presentation. Children are likely more susceptible to quaternary injury (toxic inhalation) secondary to increased minute ventilation [17]. Given the decreased musculature and increased compliance of the pediatric chest wall and sternum, children may be at increased risk for cardiac or pulmonary contusion from either primary or tertiary blast effect. The mediastinal structure is less robust in children, and hemodynamically significant shift due to tension from hemo- or pneumothorax may occur at lower pressures [34]. In some cases, death from primary blast results from a robust vagal response leading to bradycardia, hypotension, and apnea. Infants and young children may be more especially vulnerable to this mode of death due to an immature sympathetic drive [17, 35]. Clinicians should be highly suspicious if an infant or young child presents with bradycardia as this represents an inappropriate response to injury. This lack of compensatory drive may precede rapid circulatory collapse.
Gastrointestinal injury can be caused by all blast mechanisms. While the need for laparotomy seems to be less than adult counterparts, blast-injured children, especially preverbal children, may be more difficult to examine and therefore present a unique clinical challenge.
Extremity injuries and burns seem to be especially prevalent in children. This may be secondary to short stature. Children aged 4–9 were more likely to get an amputation in the series published by Edwards et al. [25]. This may be due to increased mobility and lack of situational awareness in this age group.
Rapid Assessment of the Blast-Injured Child
Children who are injured as a result of blast may present across a broad spectrum of acuity. Preparation for assessing a blast-injured child would ideally begin as soon as possible. Information regarding the type of explosive, number of injured people at the scene and their ages, proximity of victims to the blast, blast setting (open or closed space), and prehospital vital signs and possible injuries can be helpful to prepare the trauma team for triaging and resuscitating casualties. This information that can help with assuring the appropriate resources, especially pediatric-specific resources, are immediately available. When appropriate, pediatric specialists, including pediatric-trained nursing staff, and subspecialists may be invaluable in the initial assessment and disposition of pediatric trauma patients [36]. This is especially true of infants and young children.
Given the differences in hemodynamic parameters by age, a simplified method for identifying hemodynamic instability has been developed in children. The shock index (heart rate divided by blood pressure) pediatric age-adjusted (SIPA) has been shown to identify the sickest children presenting to a trauma center after trauma. A SIPA >1.22 in children 4–6 years old, >1 in 6–12 year olds, and > 0.9 in children greater than 13 years of age predicts higher injury severity [37, 38].
A Broselow™ tape can be another invaluable tool in the initial evaluation and resuscitation in children and will estimate, based upon height, needs from endotracheal and chest tube sizing to weight-based (estimated ideal body weight) dosing recommendations for medications commonly utilized during resuscitations [39]. The ability to rapidly obtain recommendations for weight-based dosing and intervention is a necessity. Thus, during the evaluation of a pediatric trauma patient , the Broselow™ tape provides readily available information and can greatly reduce cognitive loading.
In general, clinicians should adhere to ATLS principles. It is important to approach multiple-injured children in a systematic fashion. It is important to remember that a patient may have been injured by any of the five mechanisms related to blast. Specifically, there may be both blunt and penetrating injuries present. Small external wounds may be the only sign of devastating internal injury in a hemodynamically unstable child. The use of plain films and FAST in the resuscitation area can help to focus on specific injuries. In stable children, the use of CT imaging should be based on symptoms, exam, and laboratory evaluation.
For children without life-threatening injuries but who have a tympanic membrane rupture, we extrapolate recommendations posited by DePalma et al. [9]. Because traumatic tympanic membrane rupture may predict risk for late manifestations of primary blast injury to various body systems, an observation period with charted oxygen saturations for 6–8 hours is recommended. It should be noted that, while the majority of patients with severe primary blast injury will also have tympanic membrane rupture, it is possible to have severe primary blast injury without this finding [9].
Characterization, Diagnosis, and Treatment of Specific Injuries
Head Injury
Evaluation of children suspected of having head injury after blast should begin with a history of the blasting mechanism. Calculation of the child’s GCS during ATLS primary survey should be a priority, and patients with a GCS less than 8 should have their airway secured. Gross assessment of motor and sensory functions should be performed if time allows. For children without obvious clinical sign of head injury, recommendations from PECARN regarding subsequent evaluation by CT scan can be extrapolated to this population given the caveat that blast mechanism was not included in this study cohort [40].
As soon as clinically able, hemodynamically stable children with severe TBI or who meet criteria based on recommendations of PECARN should undergo head CT. Patients with severe TBI who are intubated should be kept normocapnic . There are no data to support hyperventilation in children, especially in the setting of possible concomitant blast lung injury.
Early neurosurgical evaluation is recommended, if available, for children with depressed GCS or with intracranial bleeding seen on head CT. Pediatric neurosurgical support may not be available in austere locations, and adult neurosurgeons or general/trauma surgeons with appropriate training may be required to perform stabilization and damage control [26].
The benefits of neuromonitoring and decompressive craniotomy/craniectomy in children with head injury are still unclear due to limited prospective data [33, 41,42,43]. Generally, however, the data supports ICP monitoring and decompression for medically refractory increased ICP in children with severe head injury [44]. This may be especially true in penetrating head injury [26, 45]. There are no data regarding the surgical management of pediatric patients with predominantly primary blast TBI.
Adult wartime experience with predominantly blast-injured soldiers suggests a high rate of neurological improvement over time for those patients who underwent early decompressive surgery [46, 47]. These data do not include early deaths (those that died prior to reaching the hospital). Early resuscitation on the battlefield and the use of body armor, including sophisticated armored helmets, limit the extrapolation of these data to children.
Operative battlefield experience in pediatric traumatic brain injury is mostly due to penetrating (secondary) blast injury [26]. These authors report that the operative principles include wound washout, debridement of devitalized tissue, removal of foreign bodies, removal of hematoma, and hemostasis [26]. Results of operative management of these patients are generally favorable; however, there is an intrinsic selection bias in that patients who made it to rear-echelon care with neurosurgical support may have been more likely to survive regardless of treatment. Quality of life for children after decompressive craniotomy/craniectomy for TBI is generally favorable, but rates of return to normal academic performance are low [44].
Eye Injury
As above, eye injury as a result of blast is fairly common. No pediatric-specific literature exists regarding stabilization and treatment of these injuries. Some injuries may be isolated, while patients with other severe injuries may have eye injuries in conjunction. A careful history, especially from bystanders, should be obtained. In patients with high clinical suspicion of ocular injury, a convex shield (metal or plastic) should be placed to protect the eye from further injury, and precaution should be taken to keep from putting pressure on that eye. Physical exam should focus on evaluation for surgical emergencies such as globe rupture, chemical burns, or orbital compartment syndrome [48]. Visual acuity should be assessed if possible. Practitioners experienced in the visual acuity assessment of preverbal children may be required. CT scan of the head, face, and orbit should be obtained if penetrating eye or orbital injury is suspected to guide surgical therapy. Early ophthalmologic evaluation is imperative.
Chest Injury
Though the chest is the least likely body region to be injured in children based on wartime data, chest injuries in these patients and in adult victims of civilian trauma indicate a high injury burden [18, 49, 50]. Rapid assessment of the chest should begin during the primary survey. In hemodynamically unstable children or those that are obtunded, visual inspection and palpation of the chest wall for injury should be accomplished and treatment of suspected hemo-/pneumothorax accomplished rapidly. Selection of an appropriately sized chest tube for smaller children can be guided by a Broselow™ tape. Plain film of the chest can be obtained as a supplement to physical exam during the primary survey. Cardiac FAST to assess for pericardial fluid should also be accomplished. Further imaging of the pediatric chest with cross-sectional imaging should be based upon hemodynamic stability, history (including suspected blasting mechanism), physical exam, and chest X-ray [51]. Stable patients with suspicion for secondary blast injury should undergo CT to characterize position and trajectory of penetrating fragments to guide subsequent therapy.
Primary lung blast injury as a result of the blast wave traversing the multiple air-fluid interfaces present in the chest/lung may present as respiratory distress, dyspnea, or hemoptysis [17, 35]. CXR may demonstrate “batwing” central opacities [9, 35]. While no characterization specific to pediatric patients exists, its presentation should be similar to that of adults. In patients with suspected primary pulmonary blast injury, crystalloids should be minimized. Treatment for this condition is largely supportive with lung protective ventilation in those patients requiring intubation. Extracorporeal lung support has been utilized with some success in small series of adults after chest trauma, including some civilian blast injuries [52]. This series included some patients with head injuries who underwent ECLS without heparin or after demonstration of stable intracranial bleeding [52]. Given the clinical success of this salvage modality in children, it would be theoretically beneficial.
Thoracotomy is rarely needed in pediatric patients with blast injuries to the chest [25]. The indications for thoracotomy for children with hemorrhage from a chest injury are based loosely on adult indications (15–20 mL/kg blood upon initial placement or 2–3 mL/kg bloody output over 2–3 hours) [34]. Thoracotomy for aerodigestive or mediastinal vascular injury as a result of penetrating injury would have similar indications to non-blast mechanisms.
Abdominal Injury
The requirement for laparotomy as a result of blast is common [25]. It is unclear what proportion of patients undergoing laparotomy after blast is injured by primary blast injury versus secondary or tertiary effects. Regarding primary blast effects, the cecum and terminal ileum seem to be the most likely injured segments of bowel in animal models and in observational study [53]. Primary blast injury to the bowel can create scattered areas of mural hematoma that can progress to necrosis and perforation. Rarely, blast injury to the bowel can perforate primarily. Solid organ injury secondary to primary blasting mechanism is also rare (likely owing to a lack of gas-fluid interface) [53]. It is unknown how the relatively smaller size of the pediatric torso affects these injury patterns.
Indications for abdominal exploration in blast-injured children mirror those of non-blast-injured patients. Hemodynamic instability with evidence of penetrating abdominal injury should warrant emergent exploration. For pediatric patients with hemodynamic instability and no evidence of abdominal penetration, but who have other concerning history or physical findings, FAST exam has been shown to be specific for intra-abdominal fluid and can be used to guide therapy when positive. Low sensitivity for intra-abdominal fluid, however, means a negative FAST examination in children in whom intra-abdominal injury is suspected should not be reassuring and should prompt further workup [54]. Abdominal plain film to assess for free air or pelvic fracture plus diagnostic peritoneal lavage can be helpful in this situation and can help prioritize abdominal exploration versus a continued search for the source of instability.
In hemodynamically stable children without evidence of penetrating abdominal injury, the need for further imaging should be guided by history, physical exam, and laboratory examination. While most pediatric literature calls for a decrease in the use of CT scan for children citing a small but real increase in risk of malignancy over time, we suggest a liberalization of its use in patients with a history of significant blast mechanism and in whom abdominal exam may be unreliable or unavailable (e.g., patients who are ventilated). Otherwise, the use of CT should be restricted to those who have abdominal pain, an increase in liver enzyme levels, a urinalysis positive for microscopic blood, or elevated lipase [34]. Indication for operation based on CT findings would be similar to other mechanisms of injury.
The use of CT scan after urgent surgery for trauma is controversial [55,56,57]. There is emerging evidence, however, supporting the use of CT after damage control surgery to complete diagnostic workup for severely injured patients [56, 57]. Again, there is a lack of data to support the routine use of CT in children who have undergone urgent surgery in order to complete their workup; however, given the complexity of blast injury, we think the use of postoperative CT scan for blast-injured children is a prudent adjunct to surgical exploration.
Extremities and Bony Pelvis
Injuries to the extremity due to blast mechanism again depend on the ordinance. Fireworks injuries to the hands are extremely common and can include burns/abrasions, fractures, and amputations [58]. There is a high association with ophthalmologic injury, so patients with fireworks injuries to the hand should have an ophthalmologic evaluation [58].
High-energy blast mechanisms may lead to large amounts of tissue loss or amputation. Other than burns and superficial wounds, the extremities/pelvis is the most likely body region injured in children who are combat collateral casualties [6]. Prehospital and inhospital use of tourniquets should be utilized to temporize hemorrhage as a result of extremity trauma. Tourniquet use in children injured as combat collateral casualties demonstrated similar efficacy as in adults when used appropriately [59]. Sources of life-threatening junctional or truncal injuries can then be addressed.
To our knowledge, there are no studies looking at the use of pelvic binders in children. It seems reasonable to place a pelvic binder on an older child or teenager who is hypotensive with an unstable pelvis. If a commercially available product is too large, a bedsheet can be utilized similarly for smaller children.
Once life-threatening injury has been addressed, extremities must be evaluated for vascular injury or fracture. In the series by Villamaria et al., the majority of vascular injuries (66%) seen in combat-injured children was to the extremity [27]. The remainder of observed vascular injuries was to the torso and neck. Compared to vascular injuries to the torso, vascular injuries to the extremity carry a lower risk of mortality and are able to be treated with a 95% rate of limb salvage [27].
Splints should be used to stabilize obvious fracture to decrease pain and bleeding. Again, liberal use of plain film should be utilized if underlying fracture is suspected based on history or physical exam. Open fractures should receive appropriate and timely antibiotics upon presentation. Damage control principles for severe open limb fractures should be utilized [60]. Limb salvage in young patients should be sought. Fracture stabilization utilizing wound spanning external fixation should be followed by debridement as necessary. Concomitant vascular injury can then be addressed and soft tissue coverage arranged as necessary. Wounds should be debrided and washed out serially until clean. Definitive reconstruction may require pediatric or trauma orthopedic specialty care.
Unstable pelvic fractures in blast-injured children with associated hemorrhage should be treated with pelvic stabilization, pre-peritoneal packing, and/or angioembolization similar to the treatment for adults with similar injuries. There are some data to support this treatment in older children and teens [61]. Otherwise, in younger children, the use of angioembolization will depend on available resources and expertise in small vessel access [62]. In cases where these resources are unavailable, damage control principles including pelvic packing should be applied and operative therapy/vessel ligation utilized as necessary.
Spine
Pediatric spine injury with low-energy civilian ordinance and fireworks is understandably exceedingly rare. Spine injury as a result of civilian terror events is also rare. Of the hospitalized victims of terror events in Israel from 2000 to 2005, spine injuries were only present in 2% of 0–10 year olds and 4–5% for children and adults greater than 10 years of age [24]. Of those victims of a civilian terror event who present with a deficit consistent with a cervical spine injury (including children), the vast majority of these injuries is due to secondary (penetrating) blast injury [63].
However, spine injury among combatant victims of high-energy blast are very common with injuries usually occurring in the lumbar and thoracic spine secondary to compressive loading from below [64]. The high rate of adult spine injury from predominantly high-energy blast mechanism during recent conflicts is not observed in children [64]. In a small series of pediatric neurosurgical cases from the conflict in Afghanistan, no spine surgeries were performed for pediatric blast victims [26]. The lack of spine injuries is fairly consistent between series though this may be a failure of reporting [20].
Blunt cervical spine injury in civilian mass terror incidents, especially in children, is rare. The majority of the injuries that result in neurologic deficit is due to secondary (penetrating) blast effect and is immediate and nonreversible [63]. One study reports that application of a collar in the field can take several minutes, possibly delaying other life-saving therapy, especially in the setting of penetrating c-spine injury [63, 65]. Therefore, in children, delay of transport for application of a cervical collar is not recommended, especially if the collar is inappropriately sized or delays other field care such as application of tourniquets or pelvic binders. For children who present with a cervical collar after high-energy blast, the neck needs to be inspected early for penetrating injury. Spinal precautions should be utilized until the child can be examined and cleared by neurological exam or is able to undergo skeletal series or CT scan of the spine. Otherwise, guidance provided for imaging and clearance of the pediatric c-spine should be utilized [66].
External/Burns
Burns are the third leading injury related to fireworks in the United States and are more common in some series as a result of fireworks misuse in the developing world [11, 13]. While most burns related to fireworks are not life-threatening, they do have significant potential for morbidity (especially to the face, eyes, and hands).
Pediatric victims of high-energy blast mechanism with resultant burns have increased odds for mortality [6]. For pediatric blast victims in a warzone, 30% TBSA burns correlate with about a 30% chance of mortality [6]. The percent TBSA may correlate with proximity to the blast and may, thus, be a surrogate for other injury. The increased mortality for burned children in austere environments may represent a combination of a lack of resources, specialty training, or poor indigenous nutrition or a combination of factors and has been previously reported [6, 8].
In the case of pediatric victims of blast injury who present with burns, the initial evaluation and resuscitation should, again, take a protocolized approach to ruling out other sources of life-threatening injury. Burn injury can be very distracting and should be de-prioritized. We refer readers to the USAISR burn care clinical practice guideline that has a comprehensive treatment algorithm as well as a section on the care of burned children [67]. Children with signs of airway burns/edema must have their airway assessed and rapidly controlled as the small airway can occlude without much warning with ongoing resuscitation.
Conclusion
Pediatric patients present with a unique pattern of injury following exposure to a blast. Although most pediatric blast injuries are from low-energy devices (e.g., fireworks), civilian terror events and combat operations often result in high-energy pediatric blast injuries. Such high-energy mechanisms present special challenges to care teams that may not routinely care for pediatric patients. Adhering to pediatric-specific ATLS principles and employing guides such as the Broselow™ tape for medication dosing simplify the approach to the severely injured child. Understanding common patterns of injury and their appropriate management will further optimize the outcome of blast-injured children.
Pitfalls
-
Failure to identify severely injured pediatric patients after a blast event
-
Not identifying the patient’s weight with appropriate medication doses and device sizes using a standardized measurement system such as a Broselow™ tape
-
Unfamiliarity with common injury patterns in pediatric patients with blast injury
-
Underutilization of imaging to identify critical injuries
References
Hendrix S. Two ships collided in Halifax Harbor. One of them was a floating, 3,000-ton bomb. 2017 [cited 2018 04/30/2018]. Available from: https://www.washingtonpost.com/news/retropolis/wp/2017/12/06/two-ships-collided-in-halifax-harbor-one-of-them-was-a-3000-ton-floating-bomb/?noredirect=on&utm_term=.ffb07dff2dbc.
Gillis DA, Lewis SD, Little DC. The Halifax explosion and the birth of a surgical specialty-myth or reality. J Pediatr Surg. 2010;45(5):855–8.
Nakayama DK. William Ladd before the Halifax explosion. J Pediatr Surg. 2017;52(12):2093–6.
Gates JD, Arabian S, Biddinger P, Blansfield J, Burke P, Chung S, et al. The initial response to the Boston marathon bombing: lessons learned to prepare for the next disaster. Ann Surg. 2014;260(6):960–6.
Matos RI, Holcomb JB, Callahan C, Spinella PC. Increased mortality rates of young children with traumatic injuries at a US army combat support hospital in Baghdad, Iraq, 2004. Pediatrics. 2008;122(5):e959–66.
Edwards MJ, Lustik M, Eichelberger MR, Elster E, Azarow K, Coppola C. Blast injury in children: an analysis from Afghanistan and Iraq, 2002–2010. J Trauma Acute Care Surg. 2012;73(5):1278–83.
Borgman M, Matos RI, Blackbourne LH, Spinella PC. Ten years of military pediatric care in Afghanistan and Iraq. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S509–13.
Borgman MA, Matos RI, Spinella PC. Isolated pediatric burn injury in Iraq and Afghanistan. Pediatr Crit Care Med. 2015;16(2):e23–7.
DePalma RG, Burris DG, Champion HR, Hodgson MJ. Blast injuries. N Engl J Med. 2005;352(13):1335–42.
Berger LR, Kalishman S, Rivara FP. Injuries from fireworks. Pediatrics. 1985;75(5):877–82.
Billock RM, Chounthirath T, Smith GA. Pediatric firework-related injuries presenting to United States Emergency Departments, 1990–2014. Clin Pediatr (Phila). 2017;56(6):535–44.
Smith GA, et al. The rockets’ red glare, the bombs bursting in air: fireworks-related injuries to children. Pediatrics. 1996;98(1):1–9.
Vaghardoost R, Ghavami Y, Sobouti B, Mobayen MR. Mortality and morbidity of fireworks-related burns on the annual last wednesday of the year festival (charshanbeh soori) in Iran: an 11-year study. Trauma Mon. 2013;18(2):81–5.
Bagri N, Saha A, Chandelia S, Dubey NK, Bhatt A, Rai A, et al. Fireworks injuries in children: a prospective study during the festival of lights. Emerg Med Australas. 2013;25(5):452–6.
Myers J, Lehna C. Effect of fireworks laws on pediatric fireworks-related burn injuries. J Burn Care Res. 2017;38(1):e79–82.
American Academy of Pediatrics: Committee on Injury and Poison Prevention. Fireworks-related injuries to children. Pediatrics. 2001;108(1):190–1.
Hamele M, Poss WB, Sweney J. Disaster preparedness, pediatric considerations in primary blast injury, chemical, and biological terrorism. World J Crit Care Med. 2014;3(1):15–23.
Gutierrez de Ceballos JP, Turégano Fuentes F, Perez Diaz D, Sanz Sanchez M, Martin Llorente C, Guerrero Sanz JE. Casualties treated at the closest hospital in the Madrid, March 11, terrorist bombings. Crit Care Med. 2005;33(1 Suppl):S107–12.
Leibovici D, Gofrit ON, Stein M, Shapira SC, Noga Y, Heruti RJ, et al. Blast injuries: bus versus open-air bombings--a comparative study of injuries in survivors of open-air versus confined-space explosions. J Trauma. 1996;41(6):1030–5.
Quintana DA, Parker JR, Jordan FB, Tuggle DW, Mantor PC, Tunell WP. The spectrum of pediatric injuries after a bomb blast. J Pediatr Surg. 1997;32(2):307–10; discussion 310–1.
Kim D, Mosher BD, Morrison CA, Parker-Lee C, Opreanu RC, Stevens P, et al. A modern analysis of a historical pediatric disaster: the 1927 Bath school bombing. J Surg Res. 2010;163(2):309–16.
Aharonson-Daniel L, Waisman Y, Dannon YL, Peleg K, Members of the Israel Trauma Group. Epidemiology of terror-related versus non-terror-related traumatic injury in children. Pediatrics. 2003;112(4):e280.
Amir LD, Aharonson-Daniel L, Peleg K, Waisman Y, Israel Trauma Group. The severity of injury in children resulting from acts against civilian populations. Ann Surg. 2005;241(4):666–70.
Jaffe DH, Peleg K. Terror explosive injuries: a comparison of children, adolescents, and adults. Ann Surg. 2010;251(1):138–43.
Edwards MJ, Lustik M, Carlson T, Tabak B, Farmer D, Edwards K, et al. Surgical interventions for pediatric blast injury: an analysis from Afghanistan and Iraq 2002 to 2010. J Trauma Acute Care Surg. 2014;76(3):854–8.
Klimo P Jr, Ragel BT, Scott WH Jr, McCafferty R. Pediatric neurosurgery during Operation Enduring Freedom. J Neurosurg Pediatr. 2010;6(2):107–14.
Villamaria CY, Morrison JJ, Fitzpatrick CM, Cannon JW, Rasmussen TE. Wartime vascular injuries in the pediatric population of Iraq and Afghanistan: 2002-2011. J Pediatr Surg. 2014;49(3):428–32.
Thompson, D.C., Crooks RJ, Clasper JC, Lupu A, Stapley SA, Cloke DJ. The pattern of paediatric blast injury in Afghanistan. J R Army Med Corps, 2017 Oct 21 [Epub ahead of print].
Arul GS, Reynolds J, DiRusso S, Scott A, Bree S, Templeton P, et al. Paediatric admissions to the British military hospital at Camp Bastion, Afghanistan. Ann R Coll Surg Engl. 2012;94(1):52–7.
Pannell D, Poynter J, Wales PW, Tien H, Nathens AB, Shellington D. Factors affecting mortality of pediatric trauma patients encountered in Kandahar, Afghanistan. Can J Surg. 2015;58(3 Suppl 3):S141–5.
Bitterman Y, Benov A, Glassberg E, Satanovsky A, Bader T, Sagi R. Role 1 pediatric trauma care on the Israeli-Syrian border-first year of the humanitarian effort. Mil Med. 2016;181(8):849–53.
Kissoon N, Dreyer J, Walia M. Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. CMAJ. 1990;142(1):27–34.
Figaji AA. Anatomical and physiological differences between children and adults relevant to traumatic brain injury and the implications for clinical assessment and care. Front Neurol. 2017;8:685.
Vogel AM, Edwards MJ. Trauma resuscitation and initial evaluation. In: Pediatric surgery - not a textbook: Unbound(R) Medicine. American Pediatric Surgical Association; 2018. https://www.pedsurglibrary.com/apsa.
Ritenour AE, Baskin TW. Primary blast injury: update on diagnosis and treatment. Crit Care Med. 2008;36(7 Suppl):S311–7.
McKechnie PS, Wertin T, Parker P, Eckert M. Pediatric surgery skill sets in Role 3: the Afghanistan experience. Mil Med. 2014;179(7):762–5.
Linnaus ME, Notrica DM, Langlais CS, St Peter SD, Leys CM, Ostlie DJ, et al. Prospective validation of the shock index pediatric-adjusted (SIPA) in blunt liver and spleen trauma: an ATOMAC+ study. J Pediatr Surg. 2017;52(2):340–4.
Acker SN, Ross JT, Partrick DA, Tong S, Bensard DD. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg. 2015;50(2):331–4.
Lubitz DS, Seidel JS, Chameides L, Luten RC, Zaritsky AL, Campbell FW. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann Emerg Med. 1988;17(6):576–81.
Kuppermann N, Holmes JF, Dayan PS, Hoyle JD Jr, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160–70.
Pechmann A, Anastasopoulos C, Korinthenberg R, van Velthoven-Wurster V, Kirschner J. Decompressive craniectomy after severe traumatic brain injury in children: complications and outcome. Neuropediatrics. 2015;46(1):5–12.
Davidson GH, Maier RV, Arbabi S, Goldin AB, Rivara FP. Impact of operative intervention delay on pediatric trauma outcomes. J Trauma Acute Care Surg. 2012;73(1):162–7.
Weintraub D, Williams BJ, Jane J Jr. Decompressive craniectomy in pediatric traumatic brain injury: a review of the literature. NeuroRehabilitation. 2012;30(3):219–23.
Beuriat PA, Javouhey E, Szathmari A, Courtil-Tesseydre S, Desgranges FP, Grassiot B, et al. Decompressive craniectomy in the treatment of post-traumatic intracranial hypertension in children: our philosophy and indications. J Neurosurg Sci. 2015;59(4):405–28.
DeCuypere M, Muhlbauer MS, Boop FA, Klimo P Jr. Pediatric intracranial gunshot wounds: the Memphis experience. J Neurosurg Pediatr. 2016;17(5):595–601.
Bell RS, Mossop CM, Dirks MS, Stephens FL, Mulligan L, Ecker R, et al. Early decompressive craniectomy for severe penetrating and closed head injury during wartime. Neurosurg Focus. 2010;28(5):E1.
DuBose JJ, Barmparas G, Inaba K, Stein DM, Scalea T, Cancio LC, et al. Isolated severe traumatic brain injuries sustained during combat operations: demographics, mortality outcomes, and lessons to be learned from contrasts to civilian counterparts. J Trauma. 2011;70:11–6; discussion 16–8.
Morley MG, Nguyen JK, Heier JS, Shingleton BJ, Pasternak JF, Bower KS. Blast eye injuries: a review for first responders. Disaster Med Public Health Prep. 2010;4(2):154–60.
Edwards MJ, Lustik M, Burnett MW, Eichelberger M. Pediatric inpatient humanitarian care in combat: Iraq and Afghanistan 2002 to 2012. J Am Coll Surg. 2014;218(5):1018–23.
Avidan V, Hersch M, Armon Y, Spira R, Aharoni D, Reissman P, et al. Blast lung injury: clinical manifestations, treatment, and outcome. Am J Surg. 2005;190(6):927–31.
Yanchar NL, Woo K, Brennan M, Palmer CS, Zs Ee M, Sweeney B, et al. Chest x-ray as a screening tool for blunt thoracic trauma in children. J Trauma Acute Care Surg. 2013;75(4):613–9.
Ried M, Bein T, Philipp A, Müller T, Graf B, Schmid C, et al. Extracorporeal lung support in trauma patients with severe chest injury and acute lung failure: a 10-year institutional experience. Crit Care. 2013;17(3):R110.
Owers C, Morgan JL, Garner JP. Abdominal trauma in primary blast injury. Br J Surg. 2011;98(2):168–79.
Scaife ER, Rollins MD, Barnhart DC, Downey EC, Black RE, Meyers RL, et al. The role of focused abdominal sonography for trauma (FAST) in pediatric trauma evaluation. J Pediatr Surg. 2013;48(6):1377–83.
Weis JJ, Cunningham KE, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. The importance of empiric abdominal computed tomography after urgent laparotomy for trauma: do they reveal unexpected injuries? Surgery. 2014;156(4):979–85.
Matsushima K, Inaba K, Dollbaum R, Khor D, Jhaveri V, Jimenez O, et al. The role of computed tomography after emergent trauma operation. J Surg Res. 2016;206(2):286–91.
Mendoza AE, Wybourn CA, Charles AG, Campbell AR, Cairns BA, Knudson MM. Routine computed tomography after recent operative exploration for penetrating trauma: what injuries do we miss? J Trauma Acute Care Surg. 2017;83(4):575–8.
Moore RS Jr, Tan V, Dormans JP, Bozentka DJ. Major pediatric hand trauma associated with fireworks. J Orthop Trauma. 2000;14(6):426–8.
Kragh JF Jr, Cooper A, Aden JK, Dubick MA, Baer DG, Wade CE, et al. Survey of trauma registry data on tourniquet use in pediatric war casualties. Pediatr Emerg Care. 2012;28(12):1361–5.
Zarka S, Lerner A. Complicated war trauma and care of the wounded: the Israeli experience in medical care and humanitarian support of Syrian refugees. New York: Springer; 2017.
Chao NS, Liu CS, Chung KL, Tang PM, Tai DK, Lee KY, et al. Retroperitoneal pelvic packing for haemodynamically unstable pelvic fractures in children and adolescents: a level-one trauma-centre experience. J Pediatr Surg. 2012;47(12):2244–50.
Vo NJ, Althoen M, Hippe DS, Prabhu SJ, Valji K, Padia SA. Pediatric abdominal and pelvic trauma: safety and efficacy of arterial embolization. J Vasc Interv Radiol. 2014;25(2):215–20.
Klein Y, Arieli I, Sagiv S, Peleg K, Ben-Galim P. Cervical spine injuries in civilian victims of explosions: should cervical collars be used? J Trauma Acute Care Surg. 2016;80(6):985–8.
Schoenfeld AJ, Laughlin MD, McCriskin BJ, Bader JO, Waterman BR, Belmont PJ Jr. Spinal injuries in United States military personnel deployed to Iraq and Afghanistan: an epidemiological investigation involving 7877 combat casualties from 2005 to 2009. Spine (Phila Pa 1976). 2013;38(20):1770–8.
Arishita GI, Vayer JS, Bellamy RF. Cervical spine immobilization of penetrating neck wounds in a hostile environment. J Trauma. 1989;29(3):332–7.
Keller MS, Mitchell ICS, Wakeman D, Trappey F, Jeziorczak P, Bass KD, et al. Cervical spine trauma. In: American Pediatric Surgical Association: Not A Textbook. 2017. https://www.pedsurglibrary.com/apsa/view/Pediatric-Surgery-NaT/829476/all/Cervical_Spine_Trauma.
USAISR, Burn care - joint trauma system clinical practice guideline. 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Trappey, A.F., Cannon, J.W. (2020). Pediatric Blast Injuries. In: Callaway, D., Burstein, J. (eds) Operational and Medical Management of Explosive and Blast Incidents. Springer, Cham. https://doi.org/10.1007/978-3-030-40655-4_36
Download citation
DOI: https://doi.org/10.1007/978-3-030-40655-4_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40654-7
Online ISBN: 978-3-030-40655-4
eBook Packages: MedicineMedicine (R0)