Abstract
Liver elastography offers the possibility of a quick, noninvasive, and painless evaluation of the liver with immediate results at bedside. Liver stiffness measurements (LSM) using transient elastography (TE) appear very easy to perform, however, several conditions must be respected to ensure an optimal evaluation. Thus, patient, operator, and examination characteristics have all been shown to influence the result of LSM. Food intake increases liver stiffness (LS), whereas recent withdrawal in alcoholics is associated with a decrease of LS. Around one hundred exams seem to be required before considering an operator as sufficiently trained for using e.g. a FibroScan device. The measurement site and the FibroScan probe must be correctly chosen to ensure the best quality of LSM. Finally, the intrinsic characteristics of the measurement, especially the IQR/M ratio, must be carefully checked to avoid overestimation of LS. Most of the results come from studies which have evaluated TE, with less data available for the other technologies such as 2D- and point shear wave elastography which require dedicated ultrasound knowledge. For TE, all operators should know and apply the quality criteria for LSM to ensure the reliability of the results and therefore the best management of patients in clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The principle of hepatic elastography is to generate an elastic shear wave and to measure its speed through the liver, from which is calculated the liver stiffness (LS) itself correlated with the severity of chronic liver diseases. For more details, see also book section II “Techniques to measure liver stiffness.” As for all medical exams, some precautions must be taken before and during liver stiffness measurement (LSM) to ensure that the most relevant and clinically meaningful results are obtained. Therefore, conditions related to the patient (fasting, alcohol withdrawal status), to the operator (experience with the device), and to the procedure of examination (measurement site, choice of the FibroScan probe, intrinsic characteristic of the examination) must be carefully controlled to reach the highest quality of liver stiffness measurement.
Fasting
Several studies have evaluated the effect of meal intake on elastography results (Table 41.1). Most of these works evaluated TE whose results significantly increase after eating in half of the patients [1]. The peak increase in LS occurs between 15 and 60 min after meal intake [2,3,4,5], and the increase rises up to 20–40% of the baseline value [2, 3, 6, 7]. LS recovers to initial level within 2–3 h [1, 2, 5, 8]. LS measured with two-dimensional shear wave elastography (2D-SWE) shows also a peak increase before the first hour after meal intake [3, 9], but at lesser extend with a mean 10–20% increase [3, 9, 10]. As for TE, LS recovers to the initial level within 2 h [9]. When measured with magnetic resonance elastography (MRE), LS increases by 5–20% after meal intake [11,12,13].
The portal blood flow increases after eating [3, 6,7,8, 11], and some studies have highlighted a significant correlation between both portal blood flow and LS variations [6, 11]. However, others failed to replicate these findings [3, 7, 8]. The decrease in arterial hepatic blood flow is a physiologic response to increased portal blood flow after a meal (hepatic arterial buffer response; HABR). In a study conducted in 19 cirrhotic patients, the increase in LS was more pronounced in patients lacking this postprandial HABR, suggesting it is an important factor modulating postprandial change in LS [7]. Increasing LS after a meal has a significant impact on the diagnosis of liver fibrosis at the individual level. 11% of healthy volunteers with normal LS shift to >6.0 kPa [1] or to >6.7 kPa [10] after meal intake. In patients with chronic liver disease, performing LSM with TE early after eating leads to overestimation of liver fibrosis in around one-third of the patients [1, 3]. As a consequence, international guidelines recommend to perform LSM after fasting for at least 2 h [14, 15].
The Controlled Attenuation Parameter (CAP) included in the FibroScan device evaluates liver steatosis through quantification of the ultrasound attenuation during TE examination on the FibroScan platform [16, 17]. For more details, see also book section VI “Assessment of hepatic steatosis using CAP.” The data available about CAP evolution after meal intake remains conflicting (Table 41.1): some works have shown a significant decrease [4], whereas others demonstrated a significant increase [3] or no modification [5, 18].
Alcohol Withdrawal
Liver stiffness has been shown to significantly and rapidly decrease after curing the cause of chronic liver diseases, especially in chronic viral hepatitis [19, 20]. In fact, this early decrease is mainly due to inflammation regression rather than immediate fibrosis improvement. This is also the case in alcoholic liver disease, with studies showing around 3 kPa decrease in LS within the month after alcohol withdrawal in half of the patients [21,22,23,24]. LS could continue to decrease 6 months after alcohol withdrawal, up to 6 kPa [24]. Therefore, LS results should be interpreted with caution in this situation to avoid underestimation of liver fibrosis [22, 24]. Inflammation-adapted cutoff values may be used for optimal LS interpretation [25]. A recent study has shown that CAP also significantly decreases in 78% of the patients who stop alcohol consumption [26]. For more details, see also book section IV “Important (patho)physiological confounders of LS.”
Operator Experience
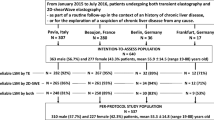
An important point for clinical practice is to assess when an operator is sufficiently trained to perform liver stiffness measurement (Table 41.2). In a large series of 13,369 liver stiffness examinations with FibroScan, operator experience fewer than 500 examinations was independently associated with a higher rate of measurement failure and a higher rate of unreliable examinations [27]. However, two other works performed in 2335 patients with chronic liver disease [28] and 992 NAFLD patients [29] found no independent association between the operator experience and the reliability of FibroScan examination.
Beyond reliability of the examination, training can also be evaluated through interobserver reproducibility between novice and experienced operators. A recent study showed an excellent novice-expert agreement for the FibroScan result as early as the first 100 examinations [30]. Due to its high ease of use, LSM with FibroScan could be delegated to nonmedical staff such as nurse or specialized technicians. To explore this possibility, the training with FibroScan has been evaluated in five novices having different medical status: a physician specializing in hepatology, a medical intern, a third-year medical student, a nurse, and a non-physician clinical research assistant [31]. The novices showed a progressive increase in the success rate of their LSM, especially the two non-physicians who finally required 50 examinations training. Interestingly, novice-expert agreement for LS results was excellent from the ten first patients with no learning curve for any of the five novices. Taken together, these results suggest that increasing experience allow to perform LSM more easily, but that results are relevant from the first examinations. In line with these findings, a study performed in patients with biopsy-proven chronic liver disease showed that operators with moderate experience (50–500 LSM) were as accurate as experienced operators for the diagnosis of cirrhosis using FibroScan (respective AUROC: 0.93 vs. 0.94), and only slightly less accurate for the diagnosis of significant fibrosis (AUROC: 0.89 vs. 0.91) [32].
There are few data available about the training with 2D-SWE or point shear wave elastography (pSWE). The rate of unreliable examinations with 2D-SWE in obese patients is higher for a novice compared to an experimented operator, but the difference is no longer significant in patients with normal weight and in overweight patients [33]. Interobserver agreement for liver stiffness results between novice and expert operators are very good for 2D-SWE [34] as for pSWE [35, 36]. However, one study that used liver biopsy as reference has suggested that around 130 examinations with pSWE are required to optimize diagnostic accuracy [36]. Since both technologies are run on conventional ultrasound machines, normally a dedicated ultrasound knowledge is required.
In summary, it can be considered that around 100 liver stiffness examinations are required before considering an operator as totally trained in the use of an elastography device.
FibroScan Probe
The classic FibroScan M probe is impaired by measurement failure rates reaching 8% in overweight patients and 17% in obese patients [27]. To circumvent this limitation, the manufacturer has developed the XL probe specifically dedicated for obese patients with skin-liver capsule distance >25 mm. Compared with the classic M probe, the XL probe uses a lower central frequency (2.5 vs. 3.5 MHz for the M probe), has a larger tip diameter (12 vs. 9 mm), and measures more deeply below the skin surface (3.5–7.5 cm vs. 2.5–6.5 cm with the M probe). The XL probe provides a lower rate of measurement failure and a similar diagnostic accuracy than the M probe [37,38,39,40]. However, the XL probe result is lower than that of the M probe with consequently a potential risk of underestimation of liver fibrosis. In contrast with the phantoms, the XL probe consistently produced approximately 20% lower liver stiffness values in humans compared with the M probe [40]. In addition to a long skin-liver capsule distance, a high degree of steatosis was also responsible for this discordance. Adjustment of cutoff values for the XL probe (<5.5, 5.5–7, 7–10, and <10 kPa for F0, F1–2, F3, and F4 fibrosis, respectively) significantly improved agreement between the two probes from r = 0.655 to 0.679 [40]. However, a recent work has shown that liver stiffness results obtained with the M probe in patients with BMI <30 kg/m2 are not significantly different from those obtained with the XL probe in obese patients (BMI ≥30 kg/m2) [41]. Therefore, by following the EASL-ALEH Clinical Practice Guidelines (M probe in patients with BMI <30 kg/m2 and XL probe in obese patients) [14], the same diagnostic cutoffs for both probes displayed similar diagnostic accuracy [41]. These results have been confirmed by another study which also evaluated the Automatic Probe Selection tool included in the recent versions of the FibroScan software [42]. The Automatic Probe Selection tool automatically measures the skin-liver capsule distance and indicates the probe to be used as a function of the patient’s morphology. According to their study results, the authors proposed to use the M probe first in patients with BMI <32 kg/m2 and eventually switch to the XL probe according to the recommendation made by the Automatic Probe Selection tool, and to use the XL probe in all patients with BMI ≥32 kg/m2.
Measurement Site
Liver stiffness measurement is performed in patients lying in dorsal decubitus with the right arm behind the head in maximal abduction. The operator has first to choose the correct measurement site, between two ribs at the level of the right lobe of the liver. By evaluating four different measurement sites, it has been suggested that the interobserver reproducibility for FibroScan results is the highest when the measurement is performed at the crossing of the median axillary line and the first intercostal space under the upper limit of the liver dullness [43] (Table 41.3). Another work showed no significant difference in liver stiffness result, AUROC for significant fibrosis or AUROC for cirrhosis among the different measurement sites evaluated [44]. In fact, it is important to correctly place the probe in front of the liver and to ensure a measurement in a liver portion at least 6 cm thick free of large vascular structures. To do this with FibroScan, the operator should control the real-time ultrasound signal on the screen of the device to obtain a typical acoustic signature of the liver characterized by a layered TM mode without heterogeneity and a linear decrease of the A mode. After the shot, the operator must also control that the elastogram displayed on the FibroScan screen is visible throughout the entire window with parallel margins.
Imaging devices including elastography modulus have the advantage to allow the visual selection of the best region of interest within the liver parenchyma. However, liver stiffness results obtained with pSWE are significantly lower when the measurement is performed in the deep portion compared to the superficial portion of the right lobe of the liver, and by intercostal compared to subcostal approach [45]. 2D-SWE seems to perform less for the diagnosis of significant fibrosis when the measurement is performed in the left lobe of the liver [46, 47].
Reliability Criteria
The correct interpretation of elastography results is crucial to ensure appropriate patient management but remains a challenge for physicians because several conditions other than liver fibrosis can increase liver stiffness: liver inflammation [48, 49], cholestasis [50], and central venous pressure [51]. Conflicting data have been observed on steatosis [52,53,54,55] and they are discussed in more detail in chapter “Histological confounders of liver stiffness” in book section IV and in chapter “Liver steatosis (CAP) as modifier of liver stiffness” in book section VI. In addition, intrinsic characteristics of elastography examination should also be carefully considered for the best interpretation of elastography result.
FibroScan
A reliable FibroScan examination has initially been defined as an exam with ≥10 valid shots and ≥60% success rate and an interquartile range/median ratio (IQR/M) ≤30%. However, some works have found that this “classical” definition does not lead to a significant improvement of the noninvasive diagnosis of liver fibrosis [56, 57]. The first study which specifically evaluated the intrinsic characteristics of FibroScan examination demonstrated that IQR/M is a key parameter to consider [58]. Liver stiffness was converted into fibrosis stage according to published cutoffs, discordance was defined as ≥2 stages difference with liver biopsy result, and the multivariate analysis identified IQR/M as independently associated with discordances. There was a 15% discordance rate in FibroScan examinations with IQR/M ≥0.21 vs. 7% in those with IQR/M <0.21. These results were confirmed by another work in which the discordance rate was 22% for FibroScan examinations with IQR/M ≥0.17 vs. 7% for those with IQR/M <0.17 [57]. In this last work, neither the criteria <10 valid shots nor the success rate was associated with discordance between FibroScan and liver biopsy.
The effect of IQR/M on the discordance rate observed in the Lucidarme and Myers studies did not translate in a significant effect on diagnostic accuracy as evaluated with the AUROC [57, 58]. Therefore, another work has used diagnostic accuracy as endpoint rather than discordance between FibroScan and liver biopsy [56]. Multivariate analysis demonstrated that IQR/M independently interacted with the level of liver stiffness to predict liver fibrosis, leading the authors to define three new categories of reliability (Table 41.4): “very reliable” (IQR/M ≤0.10), “reliable” (0.10< IQR/M ≤0.30, or IQR/M >0.30 with liver stiffness <7.1 kPa), and “poorly reliable” (IQR/M >0.30 with liver stiffness ≥7.1 kPa). AUROCs and rate of well classified patients were significantly lower in poorly reliable examinations compared to the two other very reliable and reliable categories. 9.1% of FibroScan examinations were poorly reliable versus 24.3% unreliable examination with the classical definition (≥10 valid shots, ≥60% success rate, and IQR/M ≤30%). The IQR/M ratio reflects the dispersion of the valid acquisitions obtained during the examination and, when increased, it indicates a limitation in correctly assessing the true level of liver stiffness. However, by definition, a high IQR/M implies a smaller interval in low liver stiffness levels. For example, an IQR/M at 0.30 represents a 1.5 kPa interval when liver stiffness is 5.0 kPa, but a 4.5 kPa interval when liver stiffness is 15.0 kPa. Consequently, IQR/M has little impact in low liver stiffness levels, thus explaining why FibroScan examination with IQR/M >0.30 can be considered “reliable” when liver stiffness is <7.1 kPa. Therefore, reliability criteria based only on IQR/M without consideration for the level of LS erroneously exclude reliable examinations and artificially increase the rate of unreliable examinations. An independent validation study has confirmed that the new reliability criteria increase the number of patients with valid FibroScan examinations without compromising the diagnostic accuracy [59]. In this work including 55% cirrhotic patients, the rate of reliable examinations according to the classical definition was 71.6% versus 83.2% of very reliable/reliable examinations according to the new criteria. Compared to classically defined reliable examinations, reliable/very reliable examinations according to the new criteria yielded a similar correlation with fibrosis stages and hepatic venous pressure gradient and showed the same diagnostic accuracy for significant fibrosis or cirrhosis. The new reliability criteria for FibroScan have recently been validated in a cohort of 938 NAFLD patients [60].
Point Shear Wave Elastography (pSWE)
pSWE examinations with IQR/M ≥0.30 have a higher rate of discordance with liver biopsy and a lower diagnostic accuracy for significant fibrosis and for severe fibrosis/cirrhosis [61]. The same methodology used for FibroScan has been applied in 1094 patients with biopsy-proven chronic liver disease to define three categories of reliability for pSWE: “very reliable” (IQR/M <0.15), “reliable” (0.15≤ IQR/M <0.35, or IQR/M ≥0.35 with pSWE result <1.37 m/s), and “poorly reliable” (IQR/M ≥0.35 with pSWE result ≥1.37 m/s) [60]. Unreliable examinations produced a very low diagnostic accuracy for advanced fibrosis (AUROC: 0.657, rate of well classified patients: 57.8%) as well as for cirrhosis (AUROC: 0.659, rate of well classified patients: 50.0%), which made these exams as not suitable for the evaluation of liver fibrosis in clinical practice. Unreliable examinations accounted for 21.4% of all exams and, interestingly, the rate of unreliable examinations significantly increased with the skin-liver capsule distance to reach 52.7% in patients with a distance higher than 30 mm. These reliability criteria for pSWE examination need now to be independently validated.
2D Shear Wave Elastography (2D-SWE)
A recent work performed in a small series of 88 patients with chronic liver disease took clinically significant portal hypertension defined by hepatic venous pressure gradient ≥10 mmHg as endpoint and proposed three categories of reliability for 2D-SWE examination using the standard deviation/mean ratio (SD) and the depth of measurement: “highly reliable” (SD ≤0.10 and depth <5.6 cm), “reliable” (SD >0.10 or depth ≥5.6 cm), “unreliable” (SD >0.10 and depth ≥5.6 cm) [62]. Accuracy of 2D-SWE for the noninvasive diagnosis of clinically significant portal hypertension was significantly different between highly reliable, reliable, and unreliable examinations, with respectively 96%, 76%, and 44% correctly classified patients. Another study performed in 142 patients with alcoholic liver disease or chronic viral hepatitis C did not find any association between reliability and SD below 10% [63]. In this work, 2D-SWE measurements with both SD ≤1.75 kPa and a ROI diameter ≥18 mm had excellent accuracy for the diagnosis of cirrhosis (AUROC = 0.99) whereas AUROC was only 0.75 for the exams with SD >1.75 kPa and diameter <18 mm. Finally, it seems that the SD is an important factor to consider for the interpretation of 2D-SWE results, but further studies performed in large cohorts are required to clearly define and validate the reliability criteria of 2D-SWE.
Controlled Attenuation Parameter (CAP)
It has been recently suggested that CAP examinations with an IQR/M >30 dB/m [64] or >40 dB/m [65] are less accurate for the diagnosis of fatty liver. The interest of using IQR/M >40 dB/m as criteria to identify unreliable CAP examinations has been replicated in a study including patients with alcoholic liver disease [26], but not in another work performed in NAFLD [66]. Further studies are required to determine and validate the reliability criteria for CAP examination.
Abbreviations
- 2D-SWE:
-
Two-dimensional shear wave elastography
- CAP:
-
Controlled Attenuation Parameter
- pSWE:
-
Point shear wave elastography
- IQR/M:
-
Interquartile range/median ratio
- SD/M:
-
Standard deviation/mean ratio
References
Mederacke I, Wursthorn K, Kirschner J, Rifai K, Manns MP, Wedemeyer H, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int. 2009;29(10):1500–6.
Arena U, Lupsor Platon M, Stasi C, Moscarella S, Assarat A, Bedogni G, et al. Liver stiffness is influenced by a standardized meal in patients with chronic hepatitis C virus at different stages of fibrotic evolution. Hepatology. 2013;58(1):65–72.
Kjaergaard M, Thiele M, Jansen C, Staehr Madsen B, Gortzen J, Strassburg C, et al. High risk of misinterpreting liver and spleen stiffness using 2D shear-wave and transient elastography after a moderate or high calorie meal. PLoS One. 2017;12(4):e0173992.
Ratchatasettakul K, Rattanasiri S, Promson K, Sringam P, Sobhonslidsuk A. The inverse effect of meal intake on controlled attenuation parameter and liver stiffness as assessed by transient elastography. BMC Gastroenterol. 2017;17(1):50.
Vuppalanchi R, Weber R, Russell S, Gawrieh S, Samala N, Slaven JE, et al. Is fasting necessary for individuals with nonalcoholic fatty liver disease to undergo vibration-controlled transient elastography? Am J Gastroenterol. 2019;114(6):995–7.
Barone M, Iannone A, Brunetti ND, Sebastiani F, Cecere O, Berardi E, et al. Liver stiffness and portal blood flow modifications induced by a liquid meal consumption: pathogenetic mechanisms and clinical relevance. Scand J Gastroenterol. 2015;50(5):560–6.
Berzigotti A, De Gottardi A, Vukotic R, Siramolpiwat S, Abraldes JG, Garcia-Pagan JC, et al. Effect of meal ingestion on liver stiffness in patients with cirrhosis and portal hypertension. PLoS One. 2013;8(3):e58742.
Alvarez D, Orozco F, Mella JM, Anders M, Antinucci F, Mastai R. Meal ingestion markedly increases liver stiffness suggesting the need for liver stiffness determination in fasting conditions. Gastroenterol Hepatol. 2015;38(7):431–5.
Gersak MM, Badea R, Lenghel LM, Vasilescu D, Botar-Jid C, Dudea SM. Influence of food intake on 2-D shear wave elastography assessment of liver stiffness in healthy subjects. Ultrasound Med Biol. 2016;42(6):1295–302.
Petzold G, Porsche M, Ellenrieder V, Kunsch S, Neesse A. Impact of food intake on liver stiffness determined by 2-D shear wave elastography: prospective interventional study in 100 healthy patients. Ultrasound Med Biol. 2019;45(2):402–10.
Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B. Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One. 2014;9(5):e97355.
Yin M, Talwalkar JA, Glaser KJ, Venkatesh SK, Chen J, Manduca A, et al. Dynamic postprandial hepatic stiffness augmentation assessed with MR elastography in patients with chronic liver disease. Am J Roentgenol. 2011;197(1):64–70.
Zhang J, Arena C, Pednekar A, Lambert B, Dees D, Lee VV, et al. Short-term repeatability of magnetic resonance elastography at 3.0T: effects of motion-encoding gradient direction, slice position, and meal ingestion. J Magn Reson Imaging. 2016;43(3):704–12.
EASL-ALEH Clinical Practice Guidelines. Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63(1):237–64.
Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, et al. EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (Long Version). Ultraschall Med. 2017;38(4):e16–47.
Sasso M, Beaugrand M, de Ledinghen V, Douvin C, Marcellin P, Poupon R, et al. Controlled attenuation parameter (CAP): A novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36(11):1825–35.
Karlas T, Petroff D, Sasso M, Fan JG, Mi YQ, de Ledinghen V, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66(5):1022–30.
Silva M, Costa Moreira P, Peixoto A, Santos AL, Lopes S, Goncalves R, et al. Effect of meal ingestion on liver stiffness and controlled attenuation parameter. GE Port J Gastroenterol. 2019;26(2):99–104.
Singh S, Facciorusso A, Loomba R, Falck-Ytter YT. Magnitude and kinetics of decrease in liver stiffness after antiviral therapy in patients with chronic hepatitis C: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16(1):27–38. e4
Facciorusso A, Garcia Perdomo HA, Muscatiello N, Buccino RV, Wong VW, Singh S. Systematic review with meta-analysis: change in liver stiffness during anti-viral therapy in patients with hepatitis B. Dig Liver Dis. 2018;50(8):787–94.
Mueller S, Millonig G, Sarovska L, Friedrich S, Reimann FM, Pritsch M, et al. Increased liver stiffness in alcoholic liver disease: differentiating fibrosis from steatohepatitis. World J Gastroenterol. 2010;16(8):966–72.
Trabut JB, Thepot V, Nalpas B, Lavielle B, Cosconea S, Corouge M, et al. Rapid decline of liver stiffness following alcohol withdrawal in heavy drinkers. Alcohol Clin Exp Res. 2012;36(8):1407–11.
Gelsi E, Dainese R, Truchi R, Marine-Barjoan E, Anty R, Autuori M, et al. Effect of detoxification on liver stiffness assessed by fibroscan((R)) in alcoholic patients. Alcohol Clin Exp Res. 2011;35(3):566–70.
Gianni E, Forte P, Galli V, Razzolini G, Bardazzi G, Annese V. Prospective evaluation of liver stiffness using transient elastography in alcoholic patients following abstinence. Alcohol Alcohol. 2017;52(1):42–7.
Mueller S, Englert S, Seitz HK, Badea RI, Erhardt A, Bozaari B, et al. Inflammation-adapted liver stiffness values for improved fibrosis staging in patients with hepatitis C virus and alcoholic liver disease. Liver Int. 2015;35(12):2514–21.
Thiele M, Rausch V, Fluhr G, Kjærgaard M, Piecha F, Mueller J, et al. Controlled attenuation parameter and alcoholic hepatic steatosis: diagnostic accuracy and role of alcohol detoxification. J Hepatol. 2018;68(5):1025–32.
Castéra L, Foucher J, Bernard P-H, Carvalho F, Allaix D, Merrouche W, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology. 2010;51(3):828–35.
Pang JX, Pradhan F, Zimmer S, Niu S, Crotty P, Tracey J, et al. The feasibility and reliability of transient elastography using Fibroscan(R): a practice audit of 2335 examinations. Can J Gastroenterol Hepatol. 2014;28(3):143–9.
Vuppalanchi R, Siddiqui MS, Van Natta ML, Hallinan E, Brandman D, Kowdley K, et al. Performance characteristics of vibration-controlled transient elastography for evaluation of nonalcoholic fatty liver disease. Hepatology. 2018;67(1):134–44.
Perazzo H, Fernandes FF, Soares JC, Fittipaldi J, Cardoso SW, Grinsztejn B, et al. Learning curve and intra/interobserver agreement of transient elastography in chronic hepatitis C patients with or without HIV co-infection. Clin Res Hepatol Gastroenterol. 2016;40(1):73–82.
Boursier J, Konate A, Guilluy M, Gorea G, Sawadogo A, Quemener E, et al. Learning curve and interobserver reproducibility evaluation of liver stiffness measurement by transient elastography. Eur J Gastroenterol Hepatol. 2008;20(7):693–701.
Carrion JA, Puigvehi M, Coll S, Garcia-Retortillo M, Canete N, Fernandez R, et al. Applicability and accuracy improvement of transient elastography using the M and XL probes by experienced operators. J Viral Hepat. 2015;22(3):297–306.
Gradinaru-Tascau O, Sporea I, Bota S, Jurchis A, Popescu A, Popescu M, et al. Does experience play a role in the ability to perform liver stiffness measurements by means of supersonic shear imaging (SSI)? Med Ultrason. 2013;15(3):180–3.
Lee ES, Lee JB, Park HR, Yoo J, Choi JI, Lee HW, et al. shear wave liver elastography with a propagation map: diagnostic performance and inter-observer correlation for hepatic fibrosis in chronic hepatitis. Ultrasound Med Biol. 2017;43(7):1355–63.
Boursier J, Isselin G, Fouchard-Hubert I, Oberti F, Dib N, Lebigot J, et al. Acoustic radiation force impulse: a new ultrasonographic technology for the widespread noninvasive diagnosis of liver fibrosis. Eur J Gastroenterol Hepatol. 2009;22(9):1074–84.
Fraquelli M, Baccarin A, Casazza G, Conti CB, Giunta M, Massironi S, et al. Liver stiffness measurement reliability and main determinants of point shear-wave elastography in patients with chronic liver disease. Aliment Pharmacol Ther. 2016;44(4):356–65.
Wong VW, Vergniol J, Wong GL, Foucher J, Chan AW, Chermak F, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol. 2012;107(12):1862–71.
de Ledinghen V, Wong VW, Vergniol J, Wong GL, Foucher J, Chu SH, et al. Diagnosis of liver fibrosis and cirrhosis using liver stiffness measurement: comparison between M and XL probe of FibroScan(R). J Hepatol. 2012;56(4):833–9.
Myers RP, Pomier-Layrargues G, Kirsch R, Pollett A, Duarte-Rojo A, Wong D, et al. Feasibility and diagnostic performance of the FibroScan XL probe for liver stiffness measurement in overweight and obese patients. Hepatology. 2012;55(1):199–208.
Durango E, Dietrich C, Seitz HK, Kunz CU, Pomier-Layrargues GT, Duarte-Rojo A, et al. Direct comparison of the FibroScan XL and M probes for assessment of liver fibrosis in obese and nonobese patients. Hepat Med. 2013;5:43–52.
Wong VW, Irles M, Wong GL, Shili S, Chan AW, Merrouche W, et al. Unified interpretation of liver stiffness measurement by M and XL probes in non-alcoholic fatty liver disease. Gut. 2019;68(11):2057–64.
Berger A, Shili S, Zuberbuhler F, Hiriart JB, Lannes A, Chermak F, et al. Liver stiffness measurement with fibroscan: use the right probe in the right conditions! Clin Transl Gastroenterol. 2019;10(4):e00023.
Boursier J, Konate A, Gorea G, Reaud S, Quemener E, Oberti F, et al. Reproducibility of liver stiffness measurement by ultrasonographic elastometry. Clin Gastroenterol Hepatol. 2008;6(11):1263–9.
Kim SU, Kim JK, Park JY, Ahn SH, Lee JM, Baatarkhuu O, et al. Variability in liver stiffness values from different intercostal spaces. Liver Int. 2009;29(5):760–6.
Kaminuma C, Tsushima Y, Matsumoto N, Kurabayashi T, Taketomi-Takahashi A, Endo K. Reliable measurement procedure of virtual touch tissue quantification with acoustic radiation force impulse imaging. J Ultrasound Med. 2011;30(6):745–51.
Beland MD, Brown SF, Machan JT, Taliano RJ, Promrat K, Cronan JJ. A pilot study estimating liver fibrosis with ultrasound shear-wave elastography: does the cause of liver disease or location of measurement affect performance? AJR Am J Roentgenol. 2014;203(3):W267–73.
Samir AE, Dhyani M, Vij A, Bhan AK, Halpern EF, Mendez-Navarro J, et al. Shear-wave elastography for the estimation of liver fibrosis in chronic liver disease: determining accuracy and ideal site for measurement. Radiology. 2015;274(3):888–96.
Coco B, Oliveri F, Maina AM, Ciccorossi P, Sacco R, Colombatto P, et al. Transient elastography: a new surrogate marker of liver fibrosis influenced by major changes of transaminases. J Viral Hepat. 2007;14(5):360–9.
Arena U, Vizzutti F, Abraldes JG, Corti G, Stasi C, Moscarella S, et al. Reliability of transient elastography for the diagnosis of advanced fibrosis in chronic hepatitis C. Gut. 2008;57(9):1288–93.
Millonig G, Reimann FM, Friedrich S, Fonouni H, Mehrabi A, Büchler MW, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008;48(5):1718–23.
Millonig G, Friedrich S, Adolf S, Fonouni H, Golriz M, Mehrabi A, et al. Liver stiffness is directly influenced by central venous pressure. J Hepatol. 2010;52(2):206–10.
Petta S, Maida M, Macaluso FS, Di Marco V, Camma C, Cabibi D, et al. The severity of steatosis influences liver stiffness measurement in patients with nonalcoholic fatty liver disease. Hepatology. 2015;62(4):1101–10.
Boursier J, de Ledinghen V, Sturm N, Amrani L, Bacq Y, Sandrini J, et al. Precise evaluation of liver histology by computerized morphometry shows that steatosis influences liver stiffness measured by transient elastography in chronic hepatitis C. J Gastroenterol. 2014;49(3):527–37.
Rausch V, Peccerella T, Lackner C, Yagmur E, Seitz HK, Longerich T, et al. Primary liver injury and delayed resolution of liver stiffness after alcohol detoxification in heavy drinkers with the PNPLA3 variant I148M. World J Hepatol. 2016;8(35):1547–56.
Mueller S, Nahon P, Rausch V, Peccerella T, Silva I, Yagmur E, et al. Caspase-cleaved keratin-18 fragments increase during alcohol withdrawal and predict liver-related death in patients with alcoholic liver disease. Hepatology. 2017;66(1):96–107.
Boursier J, Zarski JP, de Ledinghen V, Rousselet MC, Sturm N, Lebail B, et al. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology. 2013;57(3):1182–91.
Myers RP, Crotty P, Pomier-Layrargues G, Ma M, Urbanski SJ, Elkashab M. Prevalence, risk factors and causes of discordance in fibrosis staging by transient elastography and liver biopsy. Liver Int. 2010;30(10):1471–80.
Lucidarme D, Foucher J, Le Bail B, Vergniol J, Castera L, Duburque C, et al. Factors of accuracy of transient elastography (fibroscan) for the diagnosis of liver fibrosis in chronic hepatitis C. Hepatology. 2009;49(4):1083–9.
Schwabl P, Bota S, Salzl P, Mandorfer M, Payer BA, Ferlitsch A, et al. New reliability criteria for transient elastography increase the number of accurate measurements for screening of cirrhosis and portal hypertension. Liver Int. 2015;35(2):381–90.
Boursier J, Cassinotto C, Hunault G, Shili S, Lebigot J, Lapuyade B, et al. Criteria to determine reliability of noninvasive assessment of liver fibrosis with virtual touch quantification. Clin Gastroenterol Hepatol. 2019;17(1):164–71. e5
Fang C, Jaffer OS, Yusuf GT, Konstantatou E, Quinlan DJ, Agarwal K, et al. Reducing the number of measurements in liver point shear-wave elastography: factors that influence the number and reliability of measurements in assessment of liver fibrosis in clinical practice. Radiology. 2018;287(3):844–52.
Procopet B, Berzigotti A, Abraldes JG, Turon F, Hernandez-Gea V, Garcia-Pagan JC, et al. Real-time shear-wave elastography: applicability, reliability and accuracy for clinically significant portal hypertension. J Hepatol. 2015;62(5):1068–75.
Thiele M, Madsen BS, Procopet B, Hansen JF, Moller LMS, Detlefsen S, et al. Reliability criteria for liver stiffness measurements with real-time 2D shear wave elastography in different clinical scenarios of chronic liver disease. Ultraschall Med. 2017;38(6):648–54.
Caussy C, Alquiraish MH, Nguyen P, Hernandez C, Cepin S, Fortney LE, et al. Optimal threshold of controlled attenuation parameter with MRI-PDFF as the gold standard for the detection of hepatic steatosis. Hepatology. 2018;67(4):1348–59.
Wong VW, Petta S, Hiriart JB, Camma C, Wong GL, Marra F, et al. Validity criteria for the diagnosis of fatty liver by M probe-based controlled attenuation parameter. J Hepatol. 2017;67(3):577–84.
Eddowes PJ, Sasso M, Allison M, Tsochatzis E, Anstee QM, Sheridan D, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156(6):1717–30.
Popescu A, Bota S, Sporea I, Sirli R, Danila M, Racean S, et al. The influence of food intake on liver stiffness values assessed by acoustic radiation force impulse elastography-preliminary results. Ultrasound Med Biol. 2013;39(4):579–84.
Simkin P, Rattansingh A, Liu K, Hudson JM, Atri M, Jang HJ, et al. Reproducibility of 2 liver 2-dimensional shear wave elastographic techniques in the fasting and postprandial states. J Ultrasound Med. 2019;38(7):1739–45.
Koizumi Y, Hirooka M, Kisaka Y, Konishi I, Abe M, Murakami H, et al. Liver fibrosis in patients with chronic hepatitis C: noninvasive diagnosis by means of real-time tissue elastography—establishment of the method for measurement. Radiology. 2011;258(2):610–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Boursier, J. (2020). Quality Criteria for Liver Stiffness Measurement by Transient Elastography. In: Mueller, S. (eds) Liver Elastography. Springer, Cham. https://doi.org/10.1007/978-3-030-40542-7_41
Download citation
DOI: https://doi.org/10.1007/978-3-030-40542-7_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40541-0
Online ISBN: 978-3-030-40542-7
eBook Packages: MedicineMedicine (R0)