Abstract
Background
Liver stiffness evaluation (LSE) by Fibroscan is now widely used to assess liver fibrosis in chronic hepatitis C. Liver steatosis is a common lesion in chronic hepatitis C as in other chronic liver diseases, but its influence on LSE remains unclear. We aimed to precisely determine the influence of steatosis on LSE by using quantitative and precise morphometric measurements of liver histology.
Methods
650 patients with chronic hepatitis C, liver biopsy, and LSE were included. Liver specimens were evaluated by optical analysis (Metavir F and A, steatosis grading) and by computerized morphometry to determine the area (%, reflecting quantity) and fractal dimension (FD, reflecting architecture) of liver fibrosis and steatosis.
Results
The relationships between LSE and liver histology were better described using morphometry. LSE median was independently linked to fibrosis (area or FD), steatosis (area or FD), activity (serum AST), and IQR/LSE median. Steatosis area ≥4.0 % induced a 50 % increase in LSE result in patients with fibrosis area <9 %. In patients with IQR/LSE median ≤0.30, the rate of F0/1 patients misclassified as F ≥ 2 by Fibroscan was, respectively for steatosis area <4.0 and ≥4.0 %: 12.6 vs 32.4 % (p = 0.003). Steatosis level did not influence LSE median when fibrosis area was ≥9 %, and consequently did not increase the rate of F ≤ 3 patients misclassified as cirrhotic.
Conclusion
A precise evaluation of liver histology by computerized morphometry shows that liver stiffness measured by Fibroscan is linked to liver fibrosis, activity, and also steatosis. High level of steatosis induces misevaluation of liver fibrosis by Fibroscan.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fibroscan (Echosens, Paris, France) is a noninvasive device that measures the velocity of an elastic shear wave, which is induced by a mechanic impulse on the skin, as it moves through the liver [1]. The liver stiffness is then calculated from the speed of the shear wave: the faster the shear wave, the harder the liver. Liver stiffness evaluation by Fibroscan (LSE) is very well correlated with the histological stages of liver fibrosis in patients with chronic hepatitis C [2, 3]. Moreover, two meta-analyses have shown that the accuracy of LSE is very good for the noninvasive diagnosis of significant fibrosis (Metavir F ≥ 2) and excellent for cirrhosis [4, 5]. Consequently, the French Health Authority [6] and more recently the European Association for the Study of the Liver [7] have recognized Fibroscan as a first-line exam for the assessment of liver fibrosis in naïve patients with chronic hepatitis C.
Nevertheless, the interpretation of LSE remains difficult in clinical practice [8]. Indeed, many studies have shown that several conditions other than liver fibrosis influence liver stiffness measured by Fibroscan, such as inflammation, either acute liver injury [9, 10] or flare-up during chronic liver diseases [11], cholestasis [12, 13], central venous pressure [14], or even food intake [15]. Finally, in addition to the prevalence of fibrosis stages in the population studied and statistical limits [16], all these influencing factors may have contributed to the wide heterogeneity of LSE diagnostic cut-offs calculated in previous studies, showing overlap within and between fibrosis stages [17].
The influence of liver steatosis on LSE is still being debated: some studies have shown increasing liver stiffness with higher steatosis levels [18–20] whereas others failed to demonstrate a significant impact [21–24]. In a recent study including 615 patients with chronic hepatitis C, LSE was found to be independently associated with fibrosis stages, activity grades, and also steatosis grades [25]. However, all these studies used rough histological semi-quantitative scores with only fair inter-observer reproducibility [26] to depict the relationship between liver steatosis and liver stiffness. A recent review suggested that computer-assisted digital image liver analysis is more sensitive than optical analysis for the evaluation of liver histology and its relationships with LSE [27]. We have recently developed a fully-automated computerized morphometry software to measure the area (reflecting amount) and the fractal dimension (reflecting architecture) of steatosis or fibrosis on liver specimens [28]. Our method allows for a precise, highly reproducible, and comprehensive measurement of liver histology [28].
The aim of the present study was thus to precisely determine the relationship between LSE and liver steatosis by using computerized morphometry for the evaluation of liver histology; and to evaluate its impact on the accuracy of LSE for the non-invasive diagnosis of liver fibrosis in clinical practice in patients with chronic hepatitis C, i.e., as a cause of discrepant results.
Methods
Patients
The present study pooled 2 cohorts of patients having very similar inclusion and exclusion criteria. Patients were included if they had chronic hepatitis C, defined as both positive anti-hepatitis C virus antibodies and hepatitis C virus RNA in serum. Exclusion criteria were other causes of chronic hepatitis (hepatitis B or HIV co-infection, alcohol consumption >30 g/day in men or >20 g/day in women, hemochromatosis, autoimmune hepatitis) and cirrhosis complications (ascites, variceal bleeding, systemic infection, hepatocellular carcinoma). The first cohort included patients from 4 French centers (Angers, Bordeaux, Grenoble, and Tours) and the second corresponded to the multicenter population of the FIBROSTAR study promoted by the French National Agency for research in AIDS and hepatitis [29]. All patients gave their informed consent. The study protocol conformed to the ethical guidelines of the current Declaration of Helsinki and received approval from the local ethics committees.
Histological examination
Optical analysis
Liver fibrosis was evaluated according to Metavir fibrosis (F) staging, and activity according to Metavir activity (A) grading. Significant fibrosis was defined as Metavir F ≥ 2 and cirrhosis as F4. Steatosis grading was determined according to the percentage of hepatocytes with steatosis vesicles: grade 0, <5 %; 1, 5–33 %; 2, >33–66 %; 3, >66 %. In the first cohort, histological evaluation was performed in each center by blinded senior pathologists specialized in hepatology. In the FIBROSTAR study, histological lesions were centrally evaluated by two senior experts with a consensus reading in cases of discordance.
Morphometric analysis
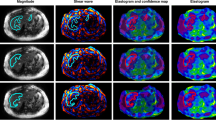
The method used for morphometric analysis has been previously described [28] and is detailed in the Supplemental Material. Briefly, liver biopsies were scanned to obtain high quality images (30,000 × 30,000 pixels; Fig. 1). Artifacts (folds, dust) were then manually removed. A labeled digital image with 3 patterns (steatosis vesicles in white, fibrosis tissue in black and other elements in grey) was obtained via an automatic thresholding technique using a home-made algorithm. Finally, other automatic algorithms developed in our laboratory determined the area of steatosis (area of steatosis vesicles/complete liver surface) and the fractal dimension (FD) of steatosis according to the Kolmogorov method of box counting [30]. The area of fibrosis and the FD of fibrosis were determined at the same time as steatosis morphometry, with a similar method [28]. All morphometric measurements were performed on the entire specimen area.
Morphometric measurement of area of steatosis. a Capture of optical image of liver specimen with picrosirius staining (×20). b Labeled digital image with 3 classes (steatosis vesicles in white, fibrosis tissue in black, and other elements in grey). c Binary digital image with steatosis vesicles in white used to calculate the area of steatosis
Fibroscan
Liver stiffness evaluation was performed using the standard probe (M probe) by an experienced observer (>50 examinations before the study) blinded for patient data, in the week preceding liver biopsy. Examination conditions were those recommended by the manufacturer [31]. LSE was stopped when 10 valid measurements were recorded. LSE results (kilopascals, kPa) were expressed as the median and the interquartile range of all valid measurements. Diagnostic cut-offs used for LSE median were those specifically determined for chronic hepatitis C in the meta-analysis of Stebbing et al. [5]: 8.44 kPa for significant fibrosis and 16.14 kPa for cirrhosis. Interquartile range/median (IQR/M) corresponded to the ratio LSE IQR/LSE median. LSE with result ≥7.1 kPa and IQR/M >0.30 were considered unreliable, as recently published [32].
Statistical analysis
Quantitative variables were expressed as mean ± standard deviation unless otherwise specified. Correlations between quantitative variables were evaluated using the Spearman (R s) or the Pearson (R p) correlation coefficients. The Lowess curve by weighted least squares was used to determine the average trend of relationships between variables [33].
To determine the histological lesions linked to LSE median, we performed multiple linear regressions including LSE median (expressed as Ln kPa) as the dependent variable and the liver lesions (fibrosis, activity, steatosis) as predictors. Since liver fibrosis and steatosis can be expressed semi-quantitatively by optical analysis or quantitatively by computerized morphometry (area or FD), we performed three multivariate models: the first included as predictors the liver lesions determined by optical analysis (“optical model”), the second included areas determined by computerized morphometry (“area model”), and the third included FD (“fractal model”). The “area model” and the “fractal model” included quantitative descriptors of liver fibrosis and steatosis. We thus used serum aspartate (AST) and alanine (ALT) aminotransferases as a quantitative surrogate marker of liver inflammation/activity, as they were very well correlated with the pathological activity grades. Finally, the “optical model” included Metavir F stage, Metavir A grade, and steatosis grade; the “area model” included area of fibrosis, area of steatosis, and serum aminotransferases; and the “fractal model”: FD of fibrosis, FD of steatosis, and serum aminotransferases. All multivariate analyses were adjusted for age, sex, liver biopsy length, and IQR/M. Statistical software was SPSS version 18.0 (IBM, Armonk, NY, USA).
Results
Patients
224 patients were included in the Angers, Bordeaux, Grenoble, and Tours centers. The FIBROSTAR study included 512 patients, 86 of whom were secondarily excluded because they were already included in the first cohort. Thus, 650 patients were included in the present study; their characteristics are detailed in Table 1. Mean biopsy length was 25.4 ± 8.4 mm, 96.2 % of biopsies were ≥15 mm length and 72.9 % were ≥20 mm. 8.7 % of LSE were considered unreliable.
Relations between optical and morphometric histology (Table 2)
Steatosis
The area and FD of steatosis were exponentially related and highly correlated (R s = 0.908, p < 10−3; Figure S1 in Supplemental Material). The area (R p = 0.894, p < 10−3) and the FD (R p = 0.867, p < 10−3) of steatosis were very well correlated with steatosis grades and significantly different between adjacent grades (Fig. 2a, b).
Fibrosis
Similarly to steatosis morphometry, the area and the FD of fibrosis were exponentially related and highly correlated (R s = 0.946, p < 10−3; Figure S2a). The FD of fibrosis had a more linear relationship with fibrosis stages (R p = 0.654, p < 10−3) than did the area of fibrosis (R p = 0.534, p < 10−3; Figures S2b and S2c).
Activity
Serum AST (R p = 0.406, p < 10−3) and ALT (R p = 0.347, p < 10−3) were significantly correlated with Metavir A grades (Figure S3a).
Liver lesions linked to liver stiffness
Univariate analysis
Optical liver histology LSE median was significantly correlated with Metavir F stages (R s = 0.613, p < 10−3), Metavir A grades (R s = 0.331, p < 10−3), and steatosis grades (R s = 0.285, p < 10−3; Table 2). LSE median was significantly different between most adjacent F stages and A grades, but for steatosis the difference was significant only between grades 0 and 1 (Fig. 3). Within each fibrosis stage, there was no difference for LSE median among Metavir A or steatosis grades (Figure S4).
Morphometric liver histology LSE median was significantly correlated with the area (R s = 0.449, p < 10−3) or the FD (0.528, p < 10−3) of fibrosis, and with the area (R s = 0.233, p < 10−3) or the FD (R s = 0.265, p < 10−3) of steatosis (Table 2). Serum AST (R s = 0.425, p < 10−3) and ALT (R s = 0.365, p < 10−3) were significantly correlated with LSE median.
Multivariate analysis
In the “optical model”, using classical semi-quantitative predictors by optical analysis, LSE median was independently linked to fibrosis stage and steatosis grade (Table 3). However, in the subgroup of patients with a reliable liver biopsy (≥20 mm) and a reliable LSE, the steatosis grade did not remain independently associated to LSE median and was replaced by the activity grade. When using quantitative predictors by computerized morphometry in the “area model” and the “fractal model”, fibrosis, activity (serum AST), and steatosis were always independently associated with LSE median, in both the whole population and the subgroup of patients with reliable biopsy and LSE.
Figure 4 depicts LSE median as a function of area of fibrosis and AST level or area of steatosis, in the whole population (see detailed results in Table S1). LSE median significantly increased with the AST, whatever the fibrosis level (Fig. 4a). Similarly, LSE median significantly increased with the level of liver steatosis but only in patients with an area of fibrosis <9.0 % (Fig. 4b). In this subgroup, compared to patients with an area of steatosis <1.0 % (LSE median 7.3 ± 3.5 kPa), patients with an area of steatosis between 1.0 and 4.0 % had a 15 % increase in LSE median (8.4 ± 5.0 kPa, p = 0.035), and those with an area of steatosis ≥4.0 % had a 50 % increase in LSE (10.9 ± 7.3 kPa, p < 0.001). In patients with an area of fibrosis ≥9.0 %, liver steatosis had no significant influence on LSE median. The average trend between LSE median and area of fibrosis as a function of AST or area of steatosis is depicted in Figure S5.
Impact on fibrosis stage diagnosis in clinical practice
As AST and area of steatosis were associated with an increase in LSE median, we conducted further evaluations to see if they caused the misclassification of F0/1 patients into a diagnosis of significant fibrosis (Metavir F ≥ 2) by Fibroscan, or F ≤ 3 patients into cirrhosis.
F0/1 patients
19.9 % of F0/1 patients had a LSE median ≥8.5 kPa and were thus misclassified as F ≥ 2 when the LSE cut-off of Stebbing et al. [5] was used. By stepwise forward binary logistic regression including area of steatosis, AST, ALT, biopsy length, and IQR/M, the rate of misclassified patients was independently associated with IQR/M [1st step, p = 0.031, expβ = 5.241 (95 %CI 1.168–23.512)] and area of steatosis [2nd step, p = 0.033, expβ = 1.118 (95 %CI 1.009–1.238)]. The rates of F0/1 patients misclassified as F ≥ 2 by Fibroscan as a function of IQR/M and area of steatosis are depicted in Fig. 5a. Misclassification significantly increased with the level of steatosis in LSE with IQR/M ≤0.30, whereas steatosis had no influence when IQR/M was >0.30. In F0/1 patients with IQR/M ≤0.30, the rate of misclassification was 12.6 % for area of steatosis <4.0 vs 32.4 % for area of steatosis ≥4.0 % (p = 0.003).
Influence of AST or liver steatosis on LSE accuracy. a Rate of patients with LSE median ≥8.5 kPa among F0/1 patients, as a function of IQR/M and area of steatosis. b Rate of patients with LSE median ≥16.2 kPa among F ≤ 3 patients, as a function of IQR/M and AST expressed as upper limit of normal (ULN: 45 UI/L)
F ≤ 3 patients
5.2 % of F ≤ 3 patients had a LSE median ≥16.2 kPa and were thus misclassified as cirrhotic by LSE [5]. By stepwise forward binary logistic regression, the rate of misclassified patients was independently associated with AST [1st step, p < 10−3, expβ = 1.011 (95 %CI 1.005–1.017)] and IQR/M [2nd step, p = 0.004, expβ = 6.068 (95 %CI 1.782–20.667)]. The rates of F ≤ 3 patients misclassified as cirrhotic by Fibroscan as a function of AST and IQR/M are depicted in Fig. 5b. Misclassification significantly increased with the level of AST, excepted when IQR/M was ≤0.10.
Discussion
Steatosis is a highly common lesion in chronic liver diseases and its influence on liver stiffness as measured by Fibroscan remains still controversial [18–25]. Through sensitive and precise measurements of liver histology by computerized morphometry, the present study clearly demonstrates the significant influence of liver steatosis on Fibroscan results in a large cohort of 650 patients with chronic hepatitis C. Our results show that area of steatosis is an independent predictor of liver stiffness measured by Fibroscan, and that steatosis induces an increase in liver stiffness in patients with mild/moderate fibrosis (area of fibrosis <9 %) with consequently an increase in the rate of F0/1 patients misclassified as F ≥ 2 by Fibroscan. Steatosis level has no influence on LSE median when fibrosis area is ≥9 %, and consequently does not increase the rate of F ≤ 3 patients misclassified as cirrhotic.
Previous studies that evaluated the influence of steatosis on liver stiffness measurement by Fibroscan had several limitations [18–25]. First, they were impaired by the use of rough histological semi-quantitative scores. For example, when steatosis grading is used, the result remains “grade 2” despite a wide range of fat-containing hepatocytes, ranging from 33 to 66 %. Second, the pathological classifications used for steatosis grading in these studies were heterogeneous. Third, some authors have found that the evaluation of liver histology by semi-quantitative scoring may be poorly reproducible [26]. Finally, it seems inappropriate to explain the quantitative and “physical” measurement of Fibroscan, i.e., the speed of a shear wave in the liver parenchyma, via “artificial” and semi-quantitative histological score classifications. In this setting, we demonstrated that the evaluation of liver histology by pathological semi-quantitative scores fails to demonstrate a significant and independent impact for steatosis on liver stiffness measured by Fibroscan: LSE median was not significantly different among steatosis grades within each fibrosis stage (Figure S4), and steatosis grading was not an independent predictor of LSE median in patients with reliable biopsy and LSE (Table 3).
Our evaluation of liver histology by computerized morphometry circumvents all these limitations: it allows for a quantitative, precise, and highly reproducible evaluation of quantity (area, expressed as %) or architecture (fractal dimension) of liver fibrosis and steatosis [28]. In a recent review on the assessment of fibrosis on liver biopsies, it was suggested that quantitative computerized morphometry is likely a better histological index than stage scores for the validation of LSE and other non-invasive markers of fibrosis [27].
To our knowledge, three studies have already evaluated the correlation between LSE median and liver fibrosis measured by computerized morphometry [19, 34, 35]. However, the number of patients included in these studies did not exceed 165, and those published by Ziol et al. [19] and Wong et al. [35] included patients with various causes of liver disease. Although these three studies showed significant correlations between area of fibrosis and LSE median, the results of multivariate analyses aiming to identify the parameters associated with LSE median were heterogeneous. The study by Nitta et al. [34] did not evaluated liver steatosis and showed LSE median as independently associated with area of fibrosis, ALT, GGT, prothrombin time, and hyaluronic acid. In the Ziol et al. [19] study, independent predictors of LSE median were area of fibrosis and steatosis (expressed as % fat-containing hepatocytes), with no effect for liver activity (expressed as high versus otherwise). Finally, Wong et al. [35] found that ALT ≥ upper limit of normal and Metavir A ≥ 2 were independent predictors of LSE median. However, in this last work, the area of fibrosis was not introduced in the multivariate analysis and liver steatosis was considered only as a binary variable (absent versus present).
Thus, a major strength of our work is that we took all liver lesions (fibrosis, steatosis, and activity) into account in the same analysis. Even more, those lesions were evaluated in a quantitative (not semi-quantitative) manner using computerized morphometry (area, fractal dimension) for fibrosis or steatosis, and serum aminotransferases as quantitative surrogate markers of activity. We confirmed that liver stiffness measured by Fibroscan is independently linked to the amount (area) or architecture (FD) of liver fibrosis and to liver activity. Morphometric measurements of liver histology allowed us to demonstrate the independent influence of steatosis on LSE median. Indeed, the area and FD of steatosis were independent predictors of liver stiffness (Table 3). Moreover, an area of steatosis higher than 4.0 %, considered as significant steatosis [28], induced a 50 % increase in LSE median in patients with an area of fibrosis <9 %. The influence of liver steatosis disappeared when the area of fibrosis was higher than 9 %. In addition, multivariate analysis identified liver fibrosis as the main predictor of LSE median (Table 3). Taken together, these results show that fibrosis has a greater impact than steatosis on LSE median. Finally, steatosis increases liver stiffness as measured by Fibroscan only in patients without severe fibrosis, whereas its influence is discarded by severe fibrosis.
Our results show that liver steatosis and serum aminotransferases level have a significant impact on the diagnostic accuracy of Fibroscan in clinical practice. As those lesions increased LSE median, we evaluated whether they induced the misclassification of F0/1 patients (as assessed by histology) into F ≥ 2 and F ≤ 3 patients into cirrhosis in Fibroscan assessments. Because its influence on LSE median was significant only in patients with an area of fibrosis <9 %, area of steatosis was an independent predictor of the misclassification of F0/1 patients to significant fibrosis, but not of F ≤ 3 patients to cirrhosis. Interestingly, steatosis increased the rate of misclassified F0/1 patients when IQR/M was ≤0.30 whereas it has no effect when IQR/M was >0.30 (Fig. 5a). We have previously shown that IQR/M >0.30 was associated with unreliable LSE examination [32]. The result of the present study confirms this findings with a high rate of F0/1 patients misclassified as F ≥ 2 when IQR/M >0.30. Consequently, the poor quality of LSE (IQR/M >0.30) with subsequent unreliable results has probably masked the influence of steatosis on LSE median. This result confirms previous studies that established the IQR/M ratio as a major parameter for LSE interpretation [32, 36, 37]. Surprisingly, AST was not an independent predictor for the misclassification of F0/1 patients to significant fibrosis. This was probably due to the low AST level in this subgroup (Figure S3b). Indeed, 61 % of F0/1 patients had AST <upper limit of normal and only 8 % had AST ≥2 times the upper limit of normal. In contrast, AST level was a strong predictor for the misclassification of F ≤ 3 patients to cirrhosis (Fig. 5b).
Finally, our results indicate that physicians have to consider examination reliability (i.e., IQR/M) and other liver lesions (i.e., activity and steatosis) when they interpret LSE median. However, although IQR/M and AST are easy to obtain in daily practice, no routine measurement of liver steatosis is currently available. Ultrasonography can accurately detect fatty liver [38], but this device does not provide a precise quantification of liver steatosis and thus cannot contribute to correct the steatosis impact on Fibroscan results. Recently, Fibroscan manufacturers have developed a new technology that measures the attenuation of the ultrasonic wave (in addition to its speed) in the liver using signals acquired by the FibroScan M probe. This “controlled attenuation parameter” (CAP) was developed on the postulate that fat affects ultrasound propagation [39]. CAP is measured at the same time, on the same volume, and on the same signal as a valid liver stiffness measurement by Fibroscan. Consequently, in practice, CAP and liver stiffness measurements are provided simultaneously by the Fibroscan device. In a recent study including 615 patients with chronic hepatitis C, CAP results were significantly correlated with the histological grades of steatosis [25]. Moreover, the accuracy of CAP for the diagnosis of mild, moderate, or severe steatosis was very good with AUROCs ranging from 0.80 to 0.88. Finally, liver fibrosis had no influence on CAP values. Thus, by using computerized morphometry as a reference for liver lesion evaluation, it may be possible to develop an algorithm that corrects LSE median according to CAP value, AST, and IQR/M for a better noninvasive determination of liver fibrosis amounts.
In addition to the amount (area), our software for morphometry determines the fractal dimension reflecting the architecture of liver fibrosis or steatosis [28, 30]. Contrary to the area expressed as percentage, fractal dimension is not meaningful for physicians. However, our results showed that fractal dimension better correlated with LSE median than did the area of liver lesions (Table 2). Moreover, in the whole population, the multivariate model including fractal dimensions better explained LSE median (a R 2 = 0.408) than did the model including area of liver lesions (a R 2 = 0.369, Table 3). However, this was not the case in the subgroup of patients with reliable biopsies and LSE, where models reached similar a R 2. Thus, further studies are required to determine whether fractal dimension is a better descriptor for LSE than area of liver lesions.
Despite the evaluation of liver fibrosis, steatosis and activity, our multivariate models failed to explain more than 50 % of LSE median (see cumulative a R 2 in Table 3). Indeed, LSE median is influenced by vascular congestion [14], cholestasis [12], and probably several other liver lesions such as edema. Currently, it is not possible to quantitatively evaluate these lesions and consequently precisely determine their influence on LSE. Finally, Fibroscan allows for a global evaluation of liver lesions linked to patient outcome [40–43]. Thus, rather than continuing to evaluate the diagnostic accuracy of LSE in cross-sectional studies, it now seems necessary to move towards longitudinal studies with the aim of determining its prognostic value against clinical events [8].
In conclusion, by using sensitive software for morphometry that quantitatively measures liver fibrosis and steatosis, we showed that liver stiffness measured by Fibroscan is mainly influenced by liver fibrosis, but also by liver steatosis. Other influencing factors are activity and IQR/M (reflecting LSE reliability). Liver steatosis and activity induced an increase in LSE median, and consequently an overestimation of Metavir F stages. Multivariate models did not explain more than 50 % of liver stiffness, suggesting an influence of several other nonevaluated liver lesions. Finally, Fibroscan allows for a global evaluation of liver injury and not only liver fibrosis.
Abbreviations
- LSE:
-
Liver stiffness evaluation
- FD:
-
Fractal dimension
- IQR/M:
-
Interquartile range/median
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
References
Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–13.
Castera L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, Haaser M, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128:343–50.
Ziol M, Handra-Luca A, Kettaneh A, Christidis C, Mal F, Kazemi F, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology. 2005;41:48–54.
Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, et al. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960–74.
Stebbing J, Farouk L, Panos G, Anderson M, Jiao LR, Mandalia S, et al. A meta-analysis of transient elastography for the detection of hepatic fibrosis. J Clin Gastroenterol. 2010;44:214–9.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol. 2011;55:245–64.
Boursier J, Cales P. Clinical interpretation of Fibroscan(R) results: a real challenge. Liver Int. 2010;30:1400–2.
Arena U, Vizzutti F, Corti G, Ambu S, Stasi C, Bresci S, et al. Acute viral hepatitis increases liver stiffness values measured by transient elastography. Hepatology. 2008;47:380–4.
Sagir A, Erhardt A, Schmitt M, Haussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology. 2008;47:592–5.
Coco B, Oliveri F, Maina AM, Ciccorossi P, Sacco R, Colombatto P, et al. Transient elastography: a new surrogate marker of liver fibrosis influenced by major changes of transaminases. J Viral Hepat. 2007;14:360–9.
Millonig G, Reimann FM, Friedrich S, Fonouni H, Mehrabi A, Buchler MW, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008;48:1718–23.
Yashima Y, Tsujino T, Masuzaki R, Nakai Y, Hirano K, Tateishi R, et al. Increased liver elasticity in patients with biliary obstruction. J Gastroenterol. 2011;46:86–91.
Millonig G, Friedrich S, Adolf S, Fonouni H, Golriz M, Mehrabi A, et al. Liver stiffness is directly influenced by central venous pressure. J Hepatol. 2010;52:206–10.
Mederacke I, Wursthorn K, Kirschner J, Rifai K, Manns MP, Wedemeyer H, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int. 2009;29:1500–6.
Poynard T, Halfon P, Castera L, Munteanu M, Imbert-Bismut F, Ratziu V, et al. Standardization of ROC curve areas for diagnostic evaluation of liver fibrosis markers based on prevalences of fibrosis stages. Clin Chem. 2007;53:1615–22.
Tsochatzis EA, Gurusamy KS, Ntaoula S, Cholongitas E, Davidson BR, Burroughs AK. Elastography for the diagnosis of severity of fibrosis in chronic liver disease: a meta-analysis of diagnostic accuracy. J Hepatol. 2011;54:650–9.
Lupsor M, Badea R, Stefanescu H, Grigorescu M, Sparchez Z, Serban A, et al. Analysis of histopathological changes that influence liver stiffness in chronic hepatitis C. Results from a cohort of 324 patients. J Gastrointestin Liver Dis. 2008;17:155–63.
Ziol M, Kettaneh A, Ganne-Carrie N, Barget N, Tengher-Barna I, Beaugrand M. Relationships between fibrosis amounts assessed by morphometry and liver stiffness measurements in chronic hepatitis or steatohepatitis. Eur J Gastroenterol Hepatol. 2009;21:1261–8.
Sanchez-Conde M, Montes Ramirez ML, Bellon Cano JM, Caminoa A, Rodriguez FA, Garcia JG, et al. Impact of liver steatosis on the correlation between liver stiffness and fibrosis measured by transient elastography in patients coinfected with human immunodeficiency virus and hepatitis C virus. J Viral Hepat. 2011;18:e278–283.
Arena U, Vizzutti F, Abraldes JG, Corti G, Stasi C, Moscarella S, et al. Reliability of transient elastography for the diagnosis of advanced fibrosis in chronic hepatitis C. Gut. 2008;57:1288–93.
Kim SU, Kim do Y, Ahn SH, Kim HM, Lee JM, Chon CY, et al. The impact of steatosis on liver stiffness measurement in patients with chronic hepatitis B. Hepatogastroenterology. 2010;57:832–38.
Wong VW, Vergniol J, Wong GL, Foucher J, Chan HL, Le Bail B, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51:454–62.
Yoneda M, Yoneda M, Mawatari H, Fujita K, Endo H, Iida H, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with nonalcoholic fatty liver disease (NAFLD). Dig Liver Dis. 2008;40:371–8.
Sasso M, Tengher-Barna I, Ziol M, Miette V, Fournier C, Sandrin L, et al. Novel controlled attenuation parameter for noninvasive assessment of steatosis using Fibroscan: validation in chronic hepatitis C. J Viral Hepat. 2012;19:244–53.
Rousselet MC, Michalak S, Dupre F, Croue A, Bedossa P, Saint-Andre JP, et al. Sources of variability in histological scoring of chronic viral hepatitis. Hepatology. 2005;41:257–64.
Germani G, Hytiroglou P, Fotiadu A, Burroughs AK, Dhillon AP. Assessment of fibrosis and cirrhosis in liver biopsies: an update. Semin Liver Dis. 2011;31:82–90.
Boursier J, Chaigneau J, Roullier V, Laine F, Sandrini J, Michalak S, et al. Steatosis degree, measured by morphometry, is linked to other liver lesions and metabolic syndrome in patients with NAFLD. Eur J Gastroenterol Hepatol. 2011;23:974–81.
Zarski JP, Sturm N, Guechot J, Paris A, Zafrani ES, Asselah T, et al. Comparison of 9 blood tests and transient elastography for liver fibrosis in chronic hepatitis C: the ANRS HCEP-23 study. J Hepatol. 2012;56:55–62.
Moal F, Chappard D, Wang J, Vuillemin E, Michalak-Provost S, Rousselet MC, et al. Fractal dimension can distinguish models and pharmacologic changes in liver fibrosis in rats. Hepatology. 2002;36:840–9.
Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48:835–47.
Boursier J, Zarski JP, de Ledinghen V, Rousselet MC, Sturm N, Le Bail B, et al. Determination of reliability criteria of liver stiffness evaluation by transient elastography. Hepatology. 2013;57:1182–91.
Borkowf CB, Albert PS, Abnet CC. Using lowess to remove systematic trends over time in predictor variables prior to logistic regression with quantile categories. Stat Med. 2003;22:1477–93.
Nitta Y, Kawabe N, Hashimoto S, Harata M, Komura N, Kobayashi K, et al. Liver stiffness measured by transient elastography correlates with fibrosis area in liver biopsy in patients with chronic hepatitis C. Hepatol Res. 2009;39:675–84.
Wong GL, Wong VW, Choi PC, Chan AW, Chum RH, Chan HK, et al. Assessment of fibrosis by transient elastography compared with liver biopsy and morphometry in chronic liver diseases. Clin Gastroenterol Hepatol. 2008;6:1027–35.
Lucidarme D, Foucher J, Le Bail B, Vergniol J, Castera L, Duburque C, et al. Factors of accuracy of transient elastography (Fibroscan) for the diagnosis of liver fibrosis in chronic hepatitis C. Hepatology. 2009;49:1083–9.
Myers RP, Crotty P, Pomier-Layrargues G, Ma M, Urbanski SJ, Elkashab M. Prevalence, risk factors and causes of discordance in fibrosis staging by transient elastography and liver biopsy. Liver Int. 2010;30:1471–80.
Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54:1082–90.
Sasso M, Beaugrand M, de Ledinghen V, Douvin C, Marcellin P, Poupon R, et al. Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Forestier J, Dumortier J, Guillaud O, Ecochard M, Roman S, Boillot O, et al. Noninvasive diagnosis and prognosis of liver cirrhosis: a comparison of biological scores, elastometry, and metabolic liver function tests. Eur J Gastroenterol Hepatol. 2010;22:532–40.
Masuzaki R, Tateishi R, Yoshida H, Goto E, Sato T, Ohki T, et al. Prospective risk assessment for hepatocellular carcinoma development in patients with chronic hepatitis C by transient elastography. Hepatology. 2009;49:1954–61.
Robic MA, Procopet B, Metivier S, Peron JM, Selves J, Vinel JP, et al. Liver stiffness accurately predicts portal hypertension related complications in patients with chronic liver disease: a prospective study. J Hepatol. 2011;55:1017–24.
Vergniol J, Foucher J, Terrebonne E, Bernard PH, le Bail B, Merrouche W, et al. Noninvasive tests for fibrosis and liver stiffness predict 5-year outcomes of patients with chronic hepatitis C. Gastroenterology. 2011;140:1970–9.
Acknowledgments
We thank the following contributors: Gilles Hunault, Pascal Veillon, Gwenaëlle Soulard; and Kevin L. Erwin (for English proofreading). This work was financially supported by PAI Volubilis, ANRS (French National Agency for AIDS and Viral Hepatitis) for HC/EP23 FIBROSTAR, University Hospital of Angers.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the Multicentre group ANRS HC EP23 FIBROSTAR are given in the Appendix.
Electronic supplementary material
Below is the link to the electronic supplementary material.
FIBROSTAR study
FIBROSTAR study
Hepatologists: R. Poupon, A. Poujol, Saint-Antoine, Paris; A. Abergel, Clermont-Ferrand; J.P. Bronowicki, Nancy; J.P. Vinel, S. Metivier, Toulouse; V. de Ledinghen, J. Foucher, J. Vergniol, Bordeaux; O. Goria, Rouen; M. Maynard-Muet, C. Trepo, Lyon; Ph. Mathurin, Lille; D. Guyader, H. Danielou, Rennes; O. Rogeaux, Chambéry; S. Pol, Ph. Sogni, Cochin, Paris; A. Tran, Nice; P. Calès, Angers; P. Marcellin, T. Asselah, Clichy; M. Bourliere, V. Oulès, Saint Joseph, Marseille; D. Larrey, Montpellier; F. Habersetzer, Strasbourg; M. Beaugrand, Bondy; V Leroy, MN Hilleret, Grenoble.
Biologists: R-C. Boisson, Lyon Sud; M-C. Gelineau, B. Poggi, Hôtel Dieu, Lyon; J-C. Renversez, Candice Trocmé, Grenoble; J. Guéchot, R. Lasnier, M. Vaubourdolle, Paris; H. Voitot, Beaujon, Paris; A. Vassault, Necker, Paris; A. Rosenthal-Allieri, Nice; A. Lavoinne, F. Ziegler, Rouen; M. Bartoli, C. Lebrun, Chambéry; A. Myara, Paris Saint-Joseph; F. Guerber, A. Pottier, Elibio, Vizille. MC Beauvieux, Bordeaux.
Pathologists: E-S. Zafrani, Créteil; N. Sturm, Grenoble.
Methodologists: A. Bechet, J-L Bosson, A. Paris, S. Royannais, CIC, Grenoble; A. Plages, Grenoble.
Rights and permissions
About this article
Cite this article
Boursier, J., de Ledinghen, V., Sturm, N. et al. Precise evaluation of liver histology by computerized morphometry shows that steatosis influences liver stiffness measured by transient elastography in chronic hepatitis C. J Gastroenterol 49, 527–537 (2014). https://doi.org/10.1007/s00535-013-0819-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0819-9