Abstract
Historically, nipple-sparing mastectomy (NSM) has been limited by both oncologic and anatomic considerations. From an oncologic standpoint, NSM was offered to women with smaller peripheral tumors with clinically negative nodes. Anatomically, NSM was contraindicated in women with breasts that were excessively large or ptotic (Baker Grade II or III ptosis). To overcome these anatomic limitations in larger, ptotic breasts, a staged nipple-sparing mastectomy following mastopexy or reduction mammoplasty was first described in 2011 to expand the indications for NSM. Early results were encumbered by wound healing complications due to a short interval between stages. Since that time, treatment algorithms and techniques have been improved to enhance oncologic safety and improve wound healing complications. Women are offered a nipple-repositioning procedure (i.e., mastopexy or reduction mammoplasty) combined with a lumpectomy during the initial stage. They are then allowed to achieve full tissue healing for 10–12 weeks before undergoing definitive NSM. This allows women only with large, ptotic breasts to pursue NSM without sacrificing the tissue viability of the nipple-areola complex.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Breast reconstruction
- Nipple-sparing mastectomy
- Oncoplastic reconstruction
- Reduction mammoplasty
- Mastopexy
Introduction
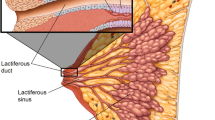
Nipple-sparing mastectomy involves the preservation of the skin of the breast including the nipple-areola complex (NAC) with the removal of all underlying breast parenchyma. This technique was first described in one form or another as early as the 1960s; however, concerns for its oncologic safety and technical feasibility impeded its widespread adoption [1,2,3]. Steadfast research into NSM, however, has demonstrated both safety and efficacy over the years.
Early work focused on safety in the prophylactic population. In 1999, a Mayo Clinic report on prophylactic mastectomy for risk reduction showed a 90–95% reduction in breast cancer risk following mastectomy in patients who underwent either total mastectomy or nipple-sparing mastectomy [4]. More recent advances in systemic therapies and surgical technique have extended the indications for NSM to patients with a diagnosis of cancer [5,6,7,8]. At the same time, genetic testing identifies increasing numbers of women who carry a higher risk for breast cancer for whom bilateral mastectomy is indicated. Increasingly these women demand the superior aesthetics afforded by preservation of the nipple-areola complex (NAC) [9].
Although NSM has grown increasingly popular as surgeons and patients have become more comfortable with the technique for both oncologic resection and prophylaxis in breast cancer, it is most widely offered to patients with small or nonptotic breast [9,10,11,12]. Several modifying techniques have been described with an aim toward allowing nipple preservation in the large or ptotic breast. In 1987, Woods first reported on a technique for “subcutaneous” mastectomy with concurrent mastopexy in a single stage; however, the technique as described required thick flaps to be raised and residual breast tissue to remain to allow adequate perfusion to the NAC and skin flaps [13]. Broer et al. described a similar single-stage technique of preserving the NAC on an inferiorly based pedicle at the time of NSM, which is performed through a Wise pattern incision [14]. In that report of eight patients, the fourth intercostal perforating artery is identified with the assistance of Doppler ultrasonography and incorporated into a large (10 cm) inferior pedicle which is de-epithelialized prior to mastectomy.
Others have described a two-stage approach to employ the use of the delay phenomenon to preserve perfusion to the NAC [15]. In a study of 20 patients by Jensen et al., NAC perfusion was successfully maintained in all patients undergoing an initial delay procedure involving undermining of the NAC and surrounding tissue with lymph node sampling and subareolar biopsy followed by NSM 7–21 days later. At the time of NSM, the NAC was raised using a hybrid peri-areola and lateral incision, or “hemi-batwing,” design. This technique was similarly reported by several other groups [16,17,18]. Our institution and others have adopted yet another approach performed in two stages involving a first-stage nipple repositioning procedure (oncoplasty, reduction mammoplasty, or mastopexy) at the time of tumor extirpation and lymph node sampling followed by a second-stage definitive NSM and reconstruction at 10–12 weeks (Fig. 21.1).
The Ideal NSM Candidate
Following mastectomy, the NAC and mastectomy skin flaps must survive only on perfusion supplied by the subdermal plexus, effectively restricting the quantity of tissue that can be adequately perfused. Conventional NSM, thus, is limited by the size of the breast envelope. In 2009, Spear et al. reported guidelines for the ideal candidate for NSM by introducing the Georgetown Criteria based not only on oncologic but also on anatomic parameters (Table 21.1) [19]. From an oncologic standpoint, NSM was offered to women with smaller peripheral tumors with clinically negative nodes. Anatomically, NSM was contraindicated in women with breasts that were excessively large or ptotic (Baker Grade II or III ptosis). These criteria were similar to other institutions such as the Mayo Clinic where NSM was offered to women with cancers 2 cm or smaller which were also 2 cm from the nipple based on clinical examination or preoperative imaging [12]. Similar to the Georgetown Criteria, anatomic contraindications at that institution included women with large or ptotic breasts, but also a high body mass index (BMI) or prior breast surgery (including reduction mammoplasty). Though the oncologic parameters for NSM have since been broadened by various centers, the anatomic realities of the larger, more ptotic breast still limit traditional NSM [20].
Challenging the Ideal: Nipple-Sparing Mastectomy After Mastopexy or Reduction Mammoplasty for the Large or Ptotic Breasts
Despite early apprehension to offering NSM for patients that had previously undergone reduction mammoplasty or mastopexy, it is now possible to extend the anatomical criteria to NSM through a two-stage approach. Breasts that were previously thought to be too large or ptotic for NSM may first be reduced and the nipple repositioned to a more anatomically appropriate location prior to mastectomy (Fig. 21.2a). In 2011, Spear et al. demonstrated that non-ideal patients with macromastia or Grade II/III ptosis may safely undergo a staged nipple-sparing mastectomy (NSM) [21]. In that series, patients underwent a nipple-repositioning procedure (either reduction mammoplasty or mastopexy) 3–4 weeks prior to definitive NSM with minimal complications. Of 24 breasts that underwent reduction mammoplasty or mastopexy prior to NSM, 17% required return to the operating room for the debridement of the NAC or skin flap necrosis, with only one implant explantation. This relatively high rate of reoperation ultimately resulted in delays in oncologic treatment as initiation of chemotherapy and/or radiation required complete soft tissue healing.
(a) Preoperative clinical image of a patient with Grade II ptosis prior to right breast lumpectomy with oncoplastic reconstruction and left breast reduction mammoplasty. (b) Clinical image 12 weeks following right lumpectomy and oncoplastic reconstruction with contralateral nipple-repositioning operation. (c) Postoperative clinical image of the same patient 3 months following definitive bilateral nipple-sparing mastectomy and direct to implant reconstruction
Further work has continued to build on that early experience, and our institution now incorporates a lumpectomy and lymph node biopsy at the time of the first-stage nipple-repositioning operation (Fig. 21.1). By including the extirpative surgery at the time of nipple repositioning, we are afforded an extended recovery of 10–12 weeks prior to the second stage and definitive NSM. This lengthier interval between stages allows for adequate tissue healing and reperfusion to minimize NAC loss. Since this change in procedure, our ongoing analysis of our new approach has shown a reduction in reoperation for mastectomy skin or NAC necrosis to 4%.
We have also noticed an increase in patients with larger breasts who otherwise would have pursued breast conservation therapy (BCT) now considering completion mastectomy to avoid radiation therapy. This has been particularly apparent in those patients whose lumpectomy surgical margins return positive. Incorporating the oncologic operation at the same time as nipple repositioning also creates an avenue toward NSM for a subset of patients who previously intended on pursuing BCT (Fig. 21.1). If surgical margins taken during lumpectomy and oncoplasty are found to be positive for residual cancer, patients who had intended to pursue BCT may now elect to proceed toward completion NSM with reduced risk of NAC loss. They may undergo adjuvant chemotherapy following lumpectomy and oncoplasty prior to NSM. This alternative pathway allows the patient to avoid the potential for further disfigurement caused by re-resection as well as radiation therapy required of BCT.
The safety and efficacy of the two-stage approach has since been duplicated. Alperovich et al. reported on a series of eight patients (13 breasts) with a history of previous reduction mammoplasty or mastopexy who underwent subsequent unplanned NSM [22]. No patients in that cohort experienced NAC or mastectomy flap loss at mean follow-up of 10.5 months. This study, however, was notable for the increased length of time between the nipple-repositioning operation and mastectomy at a mean interval of 51.8 months (r, 33 days – 11 years) demonstrating that a longer interval between stages could improve outcomes. This group was able to achieve successful outcomes despite the previous reduction pattern being unknown to the surgeon at the time of breast reconstruction.
Operative Technique
Stage One: Oncologic Resection and Nipple-Repositioning with Oncoplastic Reconstruction
The first-stage operation begins with surgical markings in the preoperative holding area made in conjunction with the breast oncology team and the aid of mammography to isolate the location of the tumor for resection (Fig. 21.3). A Wise-pattern skin reduction is marked, and a suitable NAC pedicle is chosen to allow for perfusion from a location away from that of the planned lumpectomy. Critically, pedicles are chosen which maintain as much periareolar dermis and superiorly based vasculature to the NAC as possible. Generally this will require maintaining the integrity of the dermis at the base of the chosen pedicle. This ensures that the blood supply to the NAC is not compromised during the second stage when an inframammary approach is used for NSM.
Intraoperatively, the NAC is marked with a cookie cutter and the chosen pedicle is de-epithelialized. After the completion of the oncologic resection by the breast oncology team, the plastic surgery team proceeds with oncoplastic reconstruction of the affected breast with the primary objectives of repositioning the NAC to an anatomically congruent location and reducing the skin envelope for a successful reconstruction after second-stage completion mastectomy. Parenchymal resection at this stage is not the primary goal, as definitive reconstruction will occur after the second stage. Thus, no attempt is made at parenchymal repositioning or shaping. A contralateral reduction mammoplasty or mastopexy procedure is performed for symmetry at this time (Fig. 21.2b).
Stage Two: Completion NSM and Definitive Reconstruction
The second-stage completion NSM occurs at a minimum of 10–12 weeks following the index operation (Fig. 21.2c). This time period is within the range of standard practice for patients who would otherwise go on to receive radiotherapy following BCT. This lengthy interval between first and second stages is intended to reduce wound healing complications noted with more accelerated protocols. If required, adjuvant chemotherapy is performed following the ablative surgery and prior to definitive mastectomy once successful wound healing has been achieved. Chemotherapy commences within 8 weeks of the ablative surgery, in line with current recommendations [23].
The NSM is performed through an inframmmary incision by the breast oncology team and includes separate pathologic evaluation of retroareolar tissues [19, 24]. Past experience with periareolar and lateral incisions have proven to lead to untoward complications involving nipple necrosis and lateralization of the NAC [25]. By favoring superiorly based pedicles to the NAC during the first stage, this blood supply is not violated during an inframammary approach at the second stage.
It is essential that the mastectomy skin flaps are of adequate thickness to ensure tissue perfusion. Our institution routinely employs the use of fluorescence angiography to assess the vascularity of mastectomy flaps, and this technology has allowed us to offer direct-to-implant (DTI) reconstruction when adequate tissue perfusion is confirmed. The determination to proceed with direct-to-implant reconstruction or tissue expander-based reconstruction is made after both clinical assessment and fluorescence angiography. Particular attention is made to the inferolateral mastectomy flap immediately inferior to the NAC, which represents a watershed area of tissue most likely to have decreased perfusion with Wise-pattern scars. In vivo use of fluorescence angiography has the added benefit of assessing tissue perfusion in real time and in conjunction with the breast oncology team prior to reconstruction. As our experience grows with this technology, we have seen a trend toward more robust mastectomy flaps and thus our ability to perform direct-to-implant reconstructions. Prior to our routine use of this technology, 100% of patients underwent reconstruction with tissue expanders. Since our implementation of fluorescence angiography, however, 76.9% of patients undergoing prosthetic-based reconstruction have benefited from DTI reconstructions and are thus spared an additional operation required for exchange to a permanent prosthesis. Of this subset of patients, none have experienced NAC or mastectomy flap ischemia or necrosis, compared to up to 7.5% and 14.4%, respectively, in previously published reports of DTI following NSM [26].
Staged Reconstruction with Autologous Free Tissue Transfer
Despite the assistance of fluorescence angiography in improving rates of mastectomy flap and NAC necrosis, our continued experience with staged NSM following reduction mammoplasty and/or mastopexy has shown a trend toward higher rates of NAC and mastectomy flap ischemia following immediate autologous reconstruction. These ischemic changes were seen despite adequate intraoperative perfusion as seen on fluorescence angiography. We attribute these changes to postoperative flap edema seen in autologous reconstruction as well as the ischemic insult caused by prolonged retraction of the mastectomy flaps required for vessel exposure during microsurgery and now prefer to perform immediate tissue expander placement at the time of mastectomy, followed by delayed free tissue reconstruction.
Conclusion
Historically, anatomic considerations aimed at maintaining perfusion to the mastectomy skin flaps and NAC limited NSM to women with smaller, nonptotic breasts. Incorporating a two-stage approach to those with macromastia or Baker Grade II or III ptosis may allow more women to benefit from the superior aesthetics of NSM. In the initial stage, the tumor is removed and lymph nodes sampled similar to BCT. The affected breast is reconstructed with oncoplasty at that time and the contralateral breast undergoes a mastopexy or reduction mammoplasty for symmetry. After 10–12 weeks, the second stage proceeds with definitive NSM and reconstruction.
References
Freeman BS. Technique of subcutaneous mastectomy with replacement; immediate and delayed. Br J Plast Surg. 1969;22:161–6.
Hinton CP, Doyle PJ, Blamey RW, Davies CJ, Holliday HW, Elston CW. Subcutaneous mastectomy for primary operable breast cancer. Br J Surg. 1984;71:469–72.
Kissin MW, Kark AE. Nipple preservation during mastectomy. Br J Surg. 1987;74:58–61.
Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340:77–84.
Agarwal JP, Mendenhall SD, Anderson LA, Ying J, Boucher KM, Liu T, Neumayer LA. The breast reconstruction evaluation of acellular dermal matrix as a sling trial (BREASTrial): design and methods of a prospective randomized trial. Plast Reconstr Surg. 2015;135:20–8e.
Petit JY, Veronesi U, Orecchia R, et al. Risk factors associated with recurrence after nipple-sparing mastectomy for invasive and intraepithelial neoplasia. Ann Oncol. 2012;23:2053–8.
Gabos Z, Thoms J, Ghosh S, Hanson J, Deschenes J, Sabri S, Abdulkarim B. The association between biological subtype and locoregional recurrence in newly diagnosed breast cancer. Breast Cancer Res Treat. 2010;124:187–94.
Lin NU, Vanderplas A, Hughes ME, et al. Clinicopathologic features, patterns of recurrence, and survival among women with triple negative breast cancer in the national comprehensive Cancer network. Cancer. 2012;118:5463–72.
de Alcantara Filho P, Capko D, Barry JM, Morrow M, Pusic A, Sacchini VS. Nipple-sparing mastectomy for breast cancer and risk reducing surgery: the Memorial Sloan-Kettering Cancer Center experience. Ann Surg Oncol. 2011;18:3117–22.
Coopey SB, Tang R, Lei L, et al. Increasing eligibility for nipple sparing mastectomy. Ann Surg Oncol. 2013;20:3218–22.
Wang F, Peled AW, Garwood E, et al. Total skin-sparing mastectomy and immediate breast reconstruction: an evolution of technique and assessment of outcomes. Ann Surg Oncol. 2014;21:3223–30.
Krajewski AC, Boughey JC, Degnim AC, Jakub JW, Jacobson SR, Hoskin TL, Hieken TJ. Expanded indications and improved outcomes for nipple-sparing mastectomy over time. Ann Surg Oncol. 2015;22:3317–23.
Woods JE. Detailed technique of subcutaneous mastectomy with and without mastopexy. Ann Plast Surg. 1987;18(1):51–61.
Broer N, Narayan D, Lannin D, Grube B. A novel technique for nipple-sparing mastectomy and immediate reconstruction in patients with macromastia. Plast Reconstr Surg. 2010;126(2):89e–92e.
Jensen JA, Lin JH, Kapoor N, Giuliano AE. Surgical delay of the nipple-areolar complex: a powerful technique to maximize nipple viability following nipple-sparing mastectomy. Ann Surg Oncol. 2012;19(10):3171–6.
Bertoni DM, Nguyen D, Rochlin D, et al. Protecting nipple perfusion by devascularization and surgical delay in patients at risk for ischemic complications during nipple-sparing mastectomies. Ann Surg Oncol. 2016;23:2665–e72.
Palmieri B, Baitchev G, Grappolini S, et al. Delayed nipple sparing modified subcutaneous mastectomy: rationale and technique. Breast J. 2005;11:173–e8.
Martinez CA, Reis SM, Sato EA, Boutros SG. The nipple-areola preserving mastectomy: a multistage procedure aiming to improve reconstructive outcomes following mastectomy. Plast Reconstr Surg Glob Open. 2015;3:e538.
Spear SL, Hannan CM, Willey SC, Cocilovo C. Nipple-sparing mastectomy. Plast Reconstr Surg. 2009;123:1665–73.
Hieken TJ, Boolbol SK, Dietz JR. Nipple-sparing mastectomy: indications, contraindications, risks, benefits, and techniques. Ann Surg Oncol. 2016;23(10):3138–44.
Spear SL, Rottman SJ, Seiboth LA, Hannan CM. Breast reconstruction using a staged nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg. 2012;129(3):572–81.
Alperovich M, Tanna N, Samra F, Blechman K, Shapiro RL, Guth AA, Axelrod DM, Choi M, Karp NS. Nipple-sparing mastectomy in patients with a history of reduction mammaplasty or mastopexy: how safe is it? Plast Reconstr Surg. 2013;131(5):962–7.
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016;2(3):322–9.
Spear SL, Hannan C, Seiboth L, Al-Attar A. Nipple-sparing mastectomy: a review of indications, techniques and safety. Plast Reconstr Surg. 2010;126:25.
Rawlani V, Fiuk J, Johnson SA, Buck DW 2nd, Hirsch E, Hansen N, Khan S, Fine NA, Kim JY. The effect of incision choice on outcomes of nipple-sparing mastectomy reconstruction. Can J Plast Surg. 2011 Winter;19(4):129–33.
Choi M, Frey JD, Alperovich M, Levine JP. Karp NS. “breast in a day”: examining single-stage immediate, permanent implant reconstruction in nipple-sparing mastectomy. Plast Reconstr Surg. 2016;138(2):184e–91e.
Spear SL, Willey SC, Feldman ED, et al. Nipple-sparing mastectomy for prophylactic and therapeutic indications. Plas Reconstr Surg. 2011;128:1005–14.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Willey, S.C., Pittman, T.A., Economides, J.M. (2020). Staged Nipple-Sparing Mastectomy for Patients with Large or Ptotic Breasts. In: Klimberg, V., Kovacs, T., Rubio, I. (eds) Oncoplastic Breast Surgery Techniques for the General Surgeon. Springer, Cham. https://doi.org/10.1007/978-3-030-40196-2_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-40196-2_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40195-5
Online ISBN: 978-3-030-40196-2
eBook Packages: MedicineMedicine (R0)