Abstract
Nipple-sparing mastectomy (NSM) is now an option for most patients undergoing mastectomy for cancer treatment or risk reduction. Successful NSM requires careful patient selection, proper technique to minimize complications, and meticulous removal of glandular tissue to ensure oncologic safety. NSM is now considered a safe approach for risk reduction and is endorsed by the most recent NCCN guidelines. There are few absolute contraindications to NSM in breast cancer patients; these include direct involvement of the nipple areola complex by tumor on preoperative clinical exam or imaging and the presence of pathological nipple discharge. Locoregional recurrence rates after therapeutic NSM are similar to rates after skin-sparing mastectomies and range from 0 to 4.6% with 10–60 months of follow-up. When NSM patients have been matched to skin-sparing mastectomy patients, no significant difference has been found in 5-year disease-free survival or overall survival rates. The vast majority of studies report no local recurrences within the nipple areola complex. Complication rates for NSM are now acceptably low, with complete nipple necrosis rates of approximately 2%. Proper patient selection can help minimize complications. Patient reported outcomes with NSM for risk reduction and cancer are consistently favorable.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Nipple-sparing mastectomy
- Total skin-sparing mastectomy
- Subcutaneous mastectomy
- Breast cancer
- Breast cancer risk reduction
Introduction
Although the term “mastectomy” implies removal of all breast tissue, a variety of mastectomy techniques have been used, which vary based on indication and extent of skin and glandular tissue excised. There has been continuing reduction in the extent of surgery required for successful treatment of breast cancer over the last 50 years. This has included the transition from the radical mastectomy to the modified radical mastectomy then to the simple (or total) mastectomy [1]. Breast reconstruction techniques were developed over time, initially applied only as delayed reconstructions performed 1–2 years after mastectomy due to concerns that reconstruction would delay detection of recurrent cancer or have other negative effects on oncologic outcomes. As the safety of delayed reconstruction was recognized, options for immediate reconstruction at the time of mastectomy were explored. It became clear the preservation of more breast skin could improve cosmetic outcomes.
The subcutaneous mastectomy technique was first described by Rice and Strickler in 1951 for risk reduction or treatment of benign disease. A subcutaneous mastectomy intentionally leaves glandular tissue beneath the nipple areola complex to preserve its blood supply [2]. The actual term “subcutaneous mastectomy” was coined by Freeman in 1962 and was endorsed strictly for benign disease or risk reduction [3]. Retention of this amount of subareolar and subcutaneous breast tissue is less effective for risk reduction, and there are numerous reports of breast cancer occurrences after subcutaneous mastectomy, especially in BRCA mutation carriers [4, 5]. This approach has largely been abandoned in favor of more modern nipple-sparing techniques.
In 1991, the skin-sparing mastectomy was formally introduced by Toth and Lappert [6]. With this technique, the nipple areola complex and all visible glandular tissue are removed, but the rest of the skin envelope and inframammary fold are preserved. This facilitates immediate breast reconstruction and improves cosmetic outcomes. Studies comparing skin-sparing mastectomy plus immediate or delayed reconstruction to mastectomy without reconstruction have shown equivalent local recurrence rates, confirming the safety of skin-sparing mastectomy for breast cancer treatment [7].
Although nipple reconstruction with skin grafts, local flaps, and tattooing improves cosmetic outcomes, only a limited approximation of the native nipple appearance is possible. This led to renewed interest in developing oncologically safe nipple-sparing mastectomy techniques. In contrast to the old subcutaneous mastectomy, today’s nipple sparing, or total skin-sparing mastectomy, strives to leave no glandular tissue behind the nipple areola complex or under the skin flaps. Successful NSM requires careful patient selection, proper technique to maintain nipple perfusion and minimize complications, and meticulous removal of glandular tissue.
Oncologic Safety
Occult Nipple Involvement
Historical rates of occult nipple involvement identified in nipple-sacrificing mastectomies are as high as 50%, leading to concerns about the safety of saving the nipple [3]. However, many older studies predated the use of screening mammography and included nipples with worrisome clinical findings, such as nipple retraction. In addition, the definition of nipple involvement varied in different studies; in some studies, nipples were considered positive if they contained lobular carcinoma in situ, now considered benign atypia, or if cancer was found as far as 2 cm from the nipple [3, 8,9,10,11]. Brachtel and colleagues at our institution examined 316 mastectomies with clinically uninvolved nipples in a more modern series and found occult cancer in 21% of nipples [12].
Despite high rates of nipple involvement in nipple-sacrificing mastectomy specimens, rates of positive nipple margins in modern nipple-sparing mastectomy series are much lower. In more recent series of NSM performed for cancer treatment, rates of positive nipple margins range from 2.5 to10%, likely reflecting careful patient selection [13,14,15,16,17,18,19].
Patient Selection for Nipple-Sparing Mastectomy
Initially patients with tumors greater than 2 cm or with tumor-to-nipple distances less than 2 cm were excluded from NSM, because these features were found to increase the likelihood of occult nipple involvement [20]. With experience and observation of low rates of nipple involvement, eligibility for NSM has expanded to include the majority of patients undergoing mastectomy [21, 22]. Few absolute contraindications to nipple sparing remain; these include direct involvement of the nipple areola complex on preoperative clinical exam or imaging or the presence of pathologic nipple discharge (Fig. 2.1).
In some centers, even patients with locally advanced breast cancer are considered eligible for nipple sparing. In a recent study of 139 patients with stage 2B or stage 3 breast cancer treated with NSM, only 5% of patients developed an isolated local recurrence at a mean follow-up of 41 months and no recurrence involved the retained nipple areola complex [23]. The authors concluded that with appropriate multimodality therapy, nipple sparing does not increase risk of local recurrence, even in patients with locally advanced disease.
Patients who have had prior radiation or who need post-mastectomy radiation are also candidates for NSM. Although prior radiation and post-mastectomy radiation increase risk for complications with any reconstruction, most patients who undergo NSM with radiation do well [24]. Tang and colleagues at our institution compared 816 NSM with no radiation to 69 NSM in previously irradiated breasts [24]. Prior radiation increased the rate of skin necrosis from 4.5 to 11.6% and increased risk of total nipple necrosis from 0.9 to 4.3% [24]. Among 97 NSM that received post-mastectomy radiation, 10.3% had skin necrosis and 4.1% had total nipple necrosis. Rates of implant loss were 2.2% without radiation, 2.9% with prior radiation, and 8.2% with post-mastectomy radiation [24]. Risk factors for complications with radiation included smoking, age >55, breast volume >800 cm3, and periareolar incision placement [24]. It was concluded that prior radiation or the need for post-mastectomy radiation are not absolute contraindications to NSM and that complications could be minimized with appropriate patient selection [24].
Cosmetic factors are also considered when assessing eligibility for NSM. Nipple sparing is contraindicated in patients for whom the retained nipple would be in an unacceptable position on the reconstructed breast. Marked breast ptosis or very large breast size may result in poor nipple position if the nipple is preserved. Salgarello and colleagues advise against NSM in patients with bra size larger than a D cup and for D cup breasts with grade 3 ptosis, that is, ptosis with the nipple well below the inframammary fold [25]. In addition, an excised breast weight of more than 750 g and a sternal notch-to-nipple distance of greater than 26 cm have been found to increase skin flap complications in patients undergoing skin-sparing mastectomies, so caution with use of NSM is also advised in these patients [26].
Nipple Mastectomy for Risk Reduction
NSM for risk reduction is endorsed by the most recent NCCN guidelines [27] (Fig. 2.2). Risk reduction surgery should be considered in women with a known BRCA 1 or BRCA 2 mutation, or another gene mutation with a significantly increased risk of breast cancer, or a compelling family history of breast cancer [27]. In a retrospective analysis of 639 women treated with bilateral prophylactic subcutaneous mastectomy from 1960 to 1993 for a family history of breast cancer, Hartmann and colleagues noted a 90% reduction in breast cancer at 14-year median follow up [4]. Twenty-six of these patients were later found to have BRCA 1 or BRCA2 mutations; 23 had been treated with subcutaneous mastectomy and three with simple mastectomy [28]. No cancers had developed at 13.4-year median follow-up among these BRCA mutation carriers. Using published data for the likelihood of breast cancer in BRCA1 and BRCA2 mutation carriers, they would have expected six to nine breast cancers to develop during the follow-up period with no intervention. Their results suggest that the risk of breast cancer is reduced by 89.5–100.0% in BRCA1 and BRCA2 mutation carriers after prophylactic subcutaneous mastectomy [28]. With current NSM techniques that excise all subareolar tissue, even greater risk reduction may be possible.
Yao et al. reported on NSM in 397 breasts of 201 BRCA1 and BRCA2 carriers, 125 had a BRCA1 mutation, and 76 had a BRCA2 mutation; 150 (74.6%) patients underwent NSM solely for risk reduction and 51 (25.4%) underwent NSM for unilateral cancer and contralateral risk reduction [29]. Incidental cancers were found in four (2.7%) of the 150 risk reduction patients and two (3.9%) of the 51 cancer patients. The nipple areola complex was involved with cancer in three (5.8%) of the cancer patients. No prophylactic mastectomy had a positive nipple margin. With a mean follow-up of 32.6 months, no patient developed a recurrence at the NAC, although four patients (three cancer patients and one prophylactic) experienced cancers elsewhere – two locally and two in the axilla [29]. When Peled and colleagues reviewed outcomes of 26 BRCA mutation carriers who underwent NSM for risk reduction and 27 BRCA mutation carriers who underwent NSM for unilateral breast cancer and contralateral risk reduction, they found no evidence of new or recurrent cancers, respectively, at 51-month mean follow-up [30]. In a recent multi-institutional study of risk-reducing NSM in 348 patients with BRCA mutations, Jakub et al. reported no evidence of cancer at 56-month mean follow-up [31]. Although follow-up in NSM series is limited, to date NSM appears to be a safe approach for risk reduction and for cancer treatment in high-risk patients.
Oncologic Outcome of Therapeutic Nipple-Sparing Mastectomy
Despite increasing use of NSM in the last 5–10 years, concerns remain about oncologic safety given the lack of long-term follow-up. Sites potentially at risk for new or recurrent breast cancer after NSM include the retained nipple areola complex and skin flaps, particularly at the periphery of the breast where visualization may be difficult with incisions used for NSM. Review of 297 NSM for cancer at Massachusetts General Hospital found a 3.0% risk of locoregional recurrence at 42-month median follow-up, with no recurrence involving the retained nipple areola complex [32]. These results are consistent with oncologic outcomes in other NSM series reported over the last 5 years, summarized in Table 2.1. Locoregional recurrence rates after NSM range from 0 to 4.6% at 10–60 months of follow-up [14, 15, 21, 22, 30, 33,34,35,36].
Only two modern studies report any tumor recurrences in the retained nipple after NSM. Lohsiriwat and colleagues from Italy performed 861 NSM for cancer and seven patients (0.8%) developed recurrences in the nipple areola complex with 50 months median follow-up [35]. The mean time to nipple recurrence was 32 months, and in all cases the nipple areola complex was removed. At a mean of 47 months after nipple removal, no patient developed any further local or distant recurrence. Lohsiriwat et al. describe leaving at least 5 mm of glandular tissue beneath the nipple areola complex to prevent necrosis and giving a single dose of radiation to the nipple areola complex and 1 cm beyond, a technique which is different than those used in North American studies [35]. Recently, Orzalesi et al. reviewed a national multi-institutional registry of NSM performed in Italy which included 1,006 patients [36]. Of 755 cases included in the locoregional recurrence analysis, 5 (0.7%) developed a recurrence of the nipple areola complex at a mean 36-month follow-up. In this series, no particular technique was described for dissection under the nipple areola complex [36].
In a review of 20 NSM series, De La Cruz and colleagues found disease-free survival in series with <3-year follow-up, 3–5-year follow-up, and >5-year follow-up was 93.1%, 92.3%, and 76.1%, respectively [37]. Many of the studies with >5 years of follow-up included patients treated in the mid-1980s and 1990s [38, 39]. More recent retrospective cohort studies comparing NSM plus immediate reconstruction to mastectomy without reconstruction have shown no significant difference in local or distant recurrence rates with NSM [40, 41]. When Adam et al. matched 67 NSM plus reconstruction patients to 203 mastectomy without reconstruction patients, they found no significant difference in estimated 5-year disease-free survival (94.1 and 82.5%, p = 0.068) or in overall survival (OS) (96.2 and 91.3%, p = 0.166) between them [40]. In fact, they noted a nonsignificant trend toward worse outcomes in the mastectomy without reconstruction group and concluded that NSM with reconstruction was a safe alternative. Similarly, when Park and colleagues compared 114 patients who underwent skin-sparing or nipple-sparing mastectomy plus immediate reconstruction to a matched control group of patients who underwent mastectomy with no reconstruction, they found no significant difference in 5-year locoregional recurrence-free survival between the two groups, 96.4% and 96.1%, respectively (p = 0.552) [41].
Surgical Technique
Incision Placement
The ideal incision for NSM would allow thorough resection of all of the breast tissue by the breast surgeon and ease of reconstruction for the plastic surgeon, through an aesthetically favorable scar [42]. In addition, preservation of nipple and areola blood supply is critical to successful nipple sparing. Following mastectomy, blood is supplied to the NAC from the periphery of the breast through the subdermal plexus in the skin flaps. Incisions used for NSM must preserve inflow to the nipple.
There are six basic types of incisions for NSM: inferolateral, inframammary, lateral radial, inferior radial, periareolar, and through extension of a prior scar. With the inferolateral incision, the incision begins on the lateral border of the breast at the same horizontal level as the nipple (3 o’clock position on the left breast and 9 o’clock position on the right breast). The incision is curved inferomedially along the outer border of the breast. The incision continues medially until it intersects with an imaginary vertical line through the nipple at the 6 o’clock position [42] (Fig. 2.3). The incision length is typically 10–12 cm and must be long enough to accommodate the surgeon’s hand. This incision preserves the internal mammary perforators that supply the medial skin flaps and provides easy access to the axilla. The inferolateral incision provides a favorable cosmetic result, but its inferior location can make dissection of the superomedial breast more challenging [43]. Access to the superior and medial aspects of the breast is facilitated by separating the breast from the pectoralis muscle.
The inframammary fold incision remains in the inferior portion of the breast along the inframammary fold, centered beneath the nipple, and spans 12–14 cm [44]. It is useful for DIEP flap reconstructions as it provides good medial exposure for the anastomosis of the deep inferior epigastric vessels to the internal mammary vessels. This incision also has the cosmetic advantage of being completely hidden by the breast in the upright position. It has the disadvantage of giving a more challenging exposure and usually requires a longer scar, which could interfere with blood supply to the nipple or inferior skin flap [42]. Another disadvantage of this incision is that a separate axillary incision is usually required for axillary staging [44].
The lateral radial and inferior radial incisions are more similar to incisions used for standard skin-sparing mastectomies and may be technically easier than the inferolateral and inframammary incisions. However, both leave visible scars prominent on the breast, and the lateral radial incision has been known to cause deviation of the nipple toward the scar [45]. On the other hand, an inferior radial incision is sometimes favored if a patient has larger breasts and would benefit from skin excision to raise the nipple to a more superior position on the reconstructed breast. A periareolar incision placed either along the superior or inferior half of the areola and usually with a lateral radial extension can also be utilized [43]. This approach may be technically easier for the surgeon as it is similar to the traditional skin-sparing mastectomy approach. Not surprisingly, however, placing an incision along the edge of the areola has been associated with a higher risk of nipple necrosis and nipple loss. Some authors believe that incisions in this location should be avoided, although others have found it an acceptable approach [33, 46].
Overview of Technique
Decisions about incision placement should be made in collaboration with the plastic surgeon and, to the extent possible, take patient preference into account. At our institution the majority of NSM are performed via an inferolateral approach; this allows the mastectomy and sentinel lymph node biopsy or axillary dissection to be performed through a single incision. Inferolateral and inferior incisions require modifications in technique compared to standard skin-sparing mastectomy incisions which are more centrally located on the breast. In our inferolateral approach, after the incision is made, a short flap is raised to the chest wall inferiorly and laterally, preserving the inframammary fold. If a sentinel lymph node biopsy with frozen section is planned, dissection can then be continued along the lateral border of the breast and serratus anterior muscle until the axillary fat pad is encountered. The sentinel lymph node can then be obtained, and frozen section performed while the mastectomy is completed.
Next, we have found it helpful to define the inferior edge of the pectoralis major muscle and to separate the breast from the underlying pectoralis muscle medially to the sternum and superiorly to the clavicle early in the procedure. This allows for easier retraction and manipulation of the breast tissue to aid in visualization of the Cooper’s ligament dissection plane, particularly in the medial and superior skin flaps. The anterior dissection occurs at the junction of the hypodermis and the anterior mammary fascia, dividing Cooper’s ligaments, identical to that of a skin-sparing mastectomy. Facelift or “bear claw” retractors may be used to elevate the skin edge and provide countertraction on the breast tissue to aid in the dissection. Once the dissection continues farther medially and superiorly, lighted retractors or a technique of eversion of the skin flap with the surgeon’s hand while the assistant puts traction on the breast tissue is also helpful. During all retraction maneuvers, care is taken to avoid trauma to the skin flaps and nipple.
It is important to avoid making excessively thin flaps that compromise blood supply to the skin and nipple. If the dissection is maintained in the Cooper’s ligament plane and not in the subcutaneous fat itself, perfusion to the skin flaps is usually preserved. Studies of skin-sparing mastectomies have shown that skin flaps of 4–5 mm in thickness lead to rates of skin necrosis up to 17% whereas skin flaps >10 mm have skin necrosis rates of less than 5% [47]. For superficial tumors, it is better to take a separate anterior margin from the skin flap directly over the tumor rather than make the entire skin flap too thin.
At the level of the nipple, we use a technique where areolar skin flaps are raised, leaving the nipple duct bundle intact. This can be done with blunt dissection using a curved clamp as there are no Cooper’s ligaments under the areola and minimizes trauma to the areola skin. A curved clamp is then passed around the duct bundle just beneath the areola, as is done when isolating a vessel bundle for ligation. A second clamp is used to grasp the nipple duct bundle immediately below the nipple and areola dermis, and the external skin is examined to be sure that no skin is included in the clamp. The clamp is rotated 90° away from the skin toward the surgeon to pull additional ductal tissue down from the nipple papilla, and the bundle is then sharply divided, first on the superficial surface of the clamp and then on the deep side of the clamp (Fig. 2.4). The contents of the clamp constitute the nipple margin specimen for pathology assessment. This technique removes most of the ductal tissue within the nipple papilla and leaves an anterior margin that is the underside of the nipple and areola dermis, leaving no ductal tissue or breast tissue beneath the nipple areola complex (Fig. 2.4b).
Nipple Margin Assessment
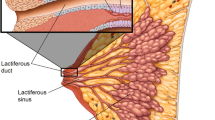
Based on pathology evaluation of cancer-containing nipples, we know that invasive cancer and ductal carcinoma in situ generally spread by direct extension sequentially into the retroareolar tissues and subareolar ducts and then into the nipple papilla itself [12]. Therefore, safe nipple preservation requires adequate sampling and pathology analysis of excised tissue from within the nipple and immediately beneath the areola, to be sure that no tumor remains in the retained nipple.
Histological assessment of the nipple margin specimen may be performed on frozen section, which allows for immediate management of a positive margin, or on permanent section. Accurate nipple margin assessment on frozen section is difficult, and distinguishing benign atypia from intraductal carcinoma is challenging, potentially resulting in unnecessary nipple excision. Therefore, permanent section analysis of nipple margins appears to be the best strategy for maximizing nipple preservation [19, 48]. With permanent section assessment, the management of a positive nipple margin can be determined in the context of complete pathologic staging and with knowledge of the full treatment plan.
If the nipple margin contains invasive cancer or ductal carcinoma in situ, it is considered positive, and the nipple should be removed. Nipple removal is not required for atypia or lobular carcinoma in situ. Rates of positive nipple margins in therapeutic NSM range from 2.5 to 10% [13,14,15,16,17,18,19]. In our series of 37 nipples excised for positive nipple margins, the excised nipple contained cancer only 30% of the time [17]. Recently, our group has transitioned from complete nipple areola complex excision for positive nipple margins to excision of just the nipple papilla with retention of most of the areola skin. In general, we have found that if the areola can be saved, reconstruction of the nipple is easier and the cosmetic result is better. With 36-month follow-up using this technique, we have had no recurrences at the site of nipple removal or in any retained areola [17].
Complications
Nipple Necrosis
In a recent systematic review of NSM, Piper and colleagues identified 23 studies which reported nipple necrosis rates [49]. Of 2980 cases, 263 (8.8%) reported some degree of nipple necrosis, either partial or total. Complete nipple loss due to necrosis occurred in 2% of cases overall, with a range of 0–10% across series [49].
Mastectomy Skin Flap Necrosis
Mastectomy skin flaps can undergo a spectrum of ischemic changes postoperatively. Changes can range from mild color change, either erythema or cyanosis, suggesting decreased perfusion, to partial thickness necrosis with epidermolysis, and to full-thickness necrosis with eschar formation [50]. In a systemic review of 16 studies, the rate of partial or full-thickness skin flap necrosis was 9.5% [49]. Colwell and colleagues found that increasing body mass index, smoking, periareolar incisions, and preoperative radiation were significant predictors of NSM complications [46].
Implant Loss
In a systemic review of 16 studies, the rate of expander-implant loss was 3.9% [49]. Rates of skin ischemia and implant loss decrease with experience. In a recent review of nearly 500 NSM plus implant or tissue expander reconstructions at Massachusetts General Hospital, the rate of implant loss was only 1.9%, despite nearly 60% of reconstructions being single-stage direct to implant [46].
Patient Satisfaction
Cosmetic Outcome
Patient reported satisfaction measures after NSM for both risk reduction and cancer treatment are consistently favorable [51] (Fig. 2.5). Using BREAST-Q scores, Howard and colleagues found that patient satisfaction with breast appearance and overall psychosocial well-being were higher after NSM with reconstruction than at the preoperative, baseline assessment [51]. When Metcalfe looked at outcomes among NSM and skin-sparing mastectomy patients 4 years after surgery, they found that patients undergoing NSM had higher satisfaction with their reconstructed breasts and higher sexual well-being scores compared to skin-sparing mastectomy patients [52]. It is important to remember to inform patients preoperatively that their nipples and central breast skin will be numb after nipple-sparing mastectomy.
Conclusion
Eligibility for nipple-sparing mastectomy for risk reduction and for breast cancer treatment continues to increase. Meticulous surgical technique is essential to preserve blood supply to the nipple and skin flaps, while also ensuring adequate excision of the breast tissue. In appropriately selected patients, nipple-sparing mastectomy is oncologically safe and the risk of complications is acceptably low.
Abbreviations
- NSM:
-
Nipple-sparing mastectomy
- NCCN:
-
National Comprehensive Cancer Network
- cm:
-
Centimeter
- BRCA:
-
Breast cancer susceptibility gene
- NAC:
-
Nipple areola complex
- DIEP:
-
Deep inferior epigastric perforator
References
Sakorafas GH, Safioleas M. Breast cancer surgery: an historical narrative. Part III. From the sunset of the 19th to the dawn of the 21st century. Eur J Cancer Care. 2010;19:145–66.
Rice CO, Strickler JH. Adeno-mammectomy for benign breast lesions. Surg Gynecol Obstet. 1951;93(6):759–62.
Rusby JE, Smith BL, Gui GPH. Nipple sparing mastectomy. Br J Surg. 2010;97:305–16.
Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340:77–84.
Kasprzak L, Mesurolle B, Tremblay F, Galvez M, Halwani F, Foulkes WD. Invasive breast cancer following bilateral subcutaneous mastectomy in a BRCA2 mutation carrier: a case report and review of the literature. World J Surg Oncol. 2005;3:52.
Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg. 1991;87(6):1048–53.
Yi M, Kronowitz SJ, Meric-Bernstam F, et al. Local, regional, and systemic recurrence rates in patients undergoing skin-sparing mastectomy compared with conventional mastectomy. Cancer. 2011;117:916–24.
Smith J, Payne WS, Carney JA. Involvement of the nipple and areola in carcinoma of the breast. Surg Gynecol Obstet. 1976;143:546–8.
Lagios MD, Gates EA, Westdahl PR, Richards V, Alpert BS. A guide to the frequency of nipple involvement in breast cancer. A study of 149 consecutive mastectomies using a serial subgross and correlated radiographic technique. Am J Surg. 1979;138:135–42.
Wertheim U, Ozzello L. Neoplastic involvement of nipple and skin flap in carcinoma of the breast. Am J Surg Pathol. 1980;4:543–9.
Andersen JA, Gram JB, Pallesen RM. Involvement of the nipple and areola in breast cancer. Value of clinical findings. Scand J Plast Reconstr Surg. 1981;15:39–42.
Brachtel EF, Rusby JE, Michaelson JS, Chen LL, Muzikansky A, Smith BL, et al. Occult nipple involvement in breast cancer: clinicopathologic findings in 316 consecutive mastectomy specimens. J Clin Oncol. 2009;27:4948–54.
Crowe JP, Patrick RJ, Yetman RJ, Djohan R. Nipple-sparing mastectomy update: one hundred forty-nine procedures and clinical outcomes. Arch Surg. 2008;143(11):1106–10.
Boneti C, Yuen J, Santiago C, et al. Oncologic safety of nipple skin-sparing or total skin-sparing mastectomies with immediate reconstruction. J Am Coll Surg. 2011;212:686–95.
Filho PA, Capko D, Barry JM, et al. Nipple-sparing mastectomy for breast cancer and risk-reducing surgery: the memorial Sloan-Kettering Cancer Center experience. Ann Surg Oncol. 2011;18:3117–22.
Petit JY, Veronisi U, Orecchia R, et al. Nipple sparing mastectomy with nipple areola intraoperative radiotherapy: one thousand and one cases of a five years experience at the European institute of oncology of Milan (EIO). Breast Cancer Res Treat. 2009;117:333–8.
Tang R, Coopey SB, Merrill AL, et al. Positive nipple margins in nipple-sparing mastectomies: rates, management, and oncologic safety. J Am Coll Surg. 2016;222:1149–55.
Camp MS, Coopey SB, Tang R, et al. Management of positive sub-areolar/nipple duct margins in nipple-sparing mastectomies. Breast J. 2014;20:402–7.
Amara D, Peled AW, Wang F, et al. Tumor involvement of the nipple in total skin-sparing mastectomy: strategies for management. Ann Surg Oncol. 2015;22:3803–8.
Rusby JE, Brachtel EF, Othus M, et al. Development and validation of a model predictive of occult nipple involvement in women undergoing mastectomy. Br J Surg. 2008;95:1356–61.
Coopey SB, Tang R, Lei L, et al. Increasing eligibility for nipple-sparing mastectomy. Ann Surg Oncol. 2013;20:3218–22.
Krajewski AC, Boughey JC, Degnim AC, et al. Expanded indications and improved outcomes for nipple-sparing mastectomy over time. Ann Surg Oncol. 2015;22:3317–23.
Peled AW, Wang F, Foster FD, et al. Expanding the indications for total skin-sparing mastectomy: is it safe for patients with locally advanced disease? Ann Surg Oncol. 2016;23:87–91.
Tang R, Coopey SB, Colwell AS, et al. Nipple-sparing mastectomy in irradiated breasts: selecting patients to minimize complications. Ann Surg Oncol. 2015;22:3331–7.
Salgarello M, Visconti G, Barone-Adesi L. Nipple-sparing mastectomy with immediate implant reconstruction: cosmetic outcomes and technical refinements. Plast Reconstr Surg. 2010;126:1460–71.
Davies K, Allan L, Roblin P, Ross D, Farhadi J. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast. 2011;20:21–5.
NCCN Clinical Practice Guidelines: Breast cancer risk reduction v1.2016 [Internet]. Available from: https://wwwnccnorg/professionals/physician_gls/pdf/breast_riskpdf. 2016.
Hartmann LC, Sellers TA, Schaid DJ, et al. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst. 2001;93:1633–7.
Yao K, Liederbach E, Tang R, et al. Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol. 2015;22:370–6.
Peled AW, Irwin CS, Hwang ES, Ewing CA, Alvarado M, Esserman LJ. Total skin-sparing mastectomy in BRCA mutation carriers. Ann Surg Oncol. 2014;21:37–41.
Jakub J, Peled A, Gray R, et al. Multi-institutional study of the oncologic safety of prophylactic nipple-sparing mastectomy in a BRCA population [Abstract]. In: Proceedings from the 17th annual meeting of the American Society of Breast Surgeons. 2016 April 13–17, Dallas.
Coopey SB, Tang R, Rai U, et al. Oncologic safety of nipple sparing mastectomy in women with breast cancer [Abstract]. In: Proceedings from the 17th annual meeting of the American Society of Breast Surgeons. 2016 April 13–17, Dallas.
Peled AW, Foster RD, Stover AC, et al. Outcomes after Total skin-sparing mastectomy and immediate reconstruction in 657 breasts. Ann Surg Oncol. 2012;19:3402–9.
Jensen JA, Orringer JS, Giuliano AE. Nipple-sparing mastectomy in 99 patients with a mean follow-up of 5 years. Ann Surg Oncol. 2011;18:1665–70.
Lohsiriwat V, Martella S, Rietjens M. Paget’s disease as a local recurrence after nipple-sparing mastectomy: clinical presentation, treatment, outcome, and risk factor analysis. Ann Surg Oncol. 2012;19:1850–5.
Orzalesi L, Casella D, Santi C, et al. Nipple sparing mastectomy: surgical and oncological outcomes from a national multicentric registry with 913 patients (1006 cases) over a six year period. Breast. 2016;25:75–81.
De La Cruz L, Moody AM, Tappy EE, Blankenship SA, Hecht EM. Overall survival, disease-free survival, local recurrence, and nipple–areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015;22:3241–9.
Gerber B, Krause A, Dieterich M, Kundt G, Reimer T. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg. 2009;249:461–8.
Benediktsson KP, Perbeck L. Survival in breast cancer after nipple sparing subcutaneous mastectomy and immediate reconstruction with implants: a prospective trial with 13 years median follow-up in 216 patients. Eur J Surg Oncol. 2008;34:143–8.
Adam H, Bygdeson M, De Boniface J. The oncological safety of nipple-sparing mastectomy: a Swedish matched cohort study. Eur J Surg Oncol. 2014;40:1209–15.
Park SH, Han W, Yoo TK, et al. Oncologic safety of immediate breast reconstruction for invasive breast cancer patients: a matched case control study. J Breast Cancer. 2016;19:68–75.
Colwell AS, Gadd M, Smith BL, Austen WG. An inferolateral approach to nipple-sparing mastectomy. Ann Plast Surg. 2010;65:140–3.
Sacchini V, Pinotti JA, Barros ACSD, et al. Nipple-sparing mastectomy for breast cancer and risk reduction: oncologic or technical problem? J Am Coll Surg. 2006;203:704–14.
Harness JK, Vetter TS, Salibian AH. Areola and nipple–areola sparing mastectomy for breast cancer treatment and risk reduction: report of an initial experience in a community hospital setting. Ann Surg Oncol. 2011;18:917–22.
Djohan R, Gage E, Gatherwright J, et al. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg. 2010;125:818–29.
Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg. 2014;133:496–506.
Robertson SA, Rusby JE, Cutress RI. Determinants of optimal mastectomy skin flap thickness. Br J Surg. 2014;101:899–911.
Rusby JE, Kirstein LJ, Brachtel EF, et al. Nipple-sparing mastectomy: lessons from ex vivo procedures. Breast J. 2008;14:464–70.
Piper M, Peled AW, Foster RD, Moore DH, Esserman LJ. Total skin-sparing mastectomy: a systematic review of oncologic outcomes and postoperative complications. Ann Plast Surg. 2013;70:435–7.
Lemaine V, Hoskin TL, Farley DR, et al. Introducing the SKIN score: a validated scoring system to assess severity of mastectomy skin flap necrosis. Ann Surg Oncol. 2015;22:2925–32.
Howard MA, Sisco M, Yao K, et al. Patient satisfaction with nipple-sparing mastectomy: a prospective study of patient reported outcomes using the BREAST-Q. J Surg Oncol. 2016;114:416–22.
Metcalfe KA, Cil TD, Semple JL, et al. Long-term psychosocial functioning in women with bilateral prophylactic mastectomy: does preservation of the nipple-areolar complex make a difference? Ann Surg Oncol. 2015;22:3324–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Coopey, S.B., Smith, B.L. (2018). Nipple-Sparing Mastectomy. In: Howard-McNatt, M. (eds) Changing Paradigms in the Management of Breast Cancer . Springer, Cham. https://doi.org/10.1007/978-3-319-60336-0_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-60336-0_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60335-3
Online ISBN: 978-3-319-60336-0
eBook Packages: MedicineMedicine (R0)