Abstract
Several recent national guidelines and reviews conclude that pharmacologic, in addition to mechanical, thromboprophylaxis appears to be safe among TBI patients with stabilized hemorrhagic patterns. Despite this, there are many issues concerning efficiency and safety in severe TBI, especially in patients with coagulopathies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara RecommendationsLevel I
No evidence level I in guiding thromboprophylaxis in TBI exists and stresses the need for adequately powered prospective randomized trials to guide clinical management in different types and severities of TBI.
Level II
There are reliable data supporting mechanical thromboprophylaxis of the lower extremities should start as early as possible and be continued until full mobilization. Several guidelines also recommend this.
Level III
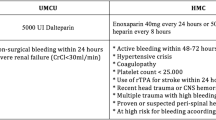
Pharmacological prophylaxis with a low molecular weight heparin (LMWH) should be used in combination with mechanical prophylaxis, when there is no expansion or risk for expansion of hematomas, evaluated by coagulation assays and repetitive CT scans. This area is a typical gray zone area, and there is a high variance when LMWH actually is started due to concerns of hematoma progression. Cava filters should be considered in complex cases.
1 Overview
Patients with severe traumatic brain injury (TBI) are at significant risk of developing venous thromboembolic complications. Patients with intracerebral hemorrhages generally have an altered coagulation profile and often have excessive coagulation after the bleeding has stopped. While in neurointensive care, these patients are often unconscious or sedated and lie still for long periods, potentially causing blood stasis in the deep veins (Kaufman et al. 1983). Intracerebral hemorrhages are an indirect evidence of injured endothelial cells in the brain; some TBI patients have damaged endothelium in other parts of the body as well. The injured areas cause inflammation, increasing the concentration of acute phase reactants, making the blood even more hypercoagulative. All these factors are included in Virchow’s triad, a theory that explains the pathogenesis of venous thrombosis. Venous thromboembolism (VTE) is estimated to occur in 20% of patients with TBI, so guidelines recommend the use of mechanical and pharmacologic thromboprophylaxis (Kaufman et al. 1983; Knudson et al. 2004; Haddad and Arabi 2012). The more severe pulmonary embolism (PE) was estimated to occur in 0.38% of patients with severe TBI (Page et al. 2004). Advanced age, excess weight, and the severity of the TBI all increase the risk of VTE.
There are no specific pediatric concerns, except that children are less prone to thrombotic complications than adults. After start of puberty, children have the same risk as adults.
A number of studies have demonstrated the efficacy and safety of mechanical prophylaxis with either graduated compression stockings or intermittent pneumatic compression. The relative risk of venous thrombosis has been reduced to >50% (Skillman et al. 1978; Turpie et al. 1989) without any changes in mean arterial pressure, intracranial pressure (ICP), or central venous pressure as documented by Davidson et al. (1993). There is a general consensus that thromboprophylaxis of the lower extremities should start as early as possible and be continued until full mobilization, which is also highlighted in guidelines from the Neurocritical Care Society and the Society of Critical Care Medicine (Nyquist et al. 2016).
Among elective neurosurgical patients, there is level I evidence regarding pharmacological prophylaxis (Agnelli et al. 1998), but these data cannot automatically be transferred to TBI patients. Studies among patients with TBI suggest that LMWH is efficacious in reducing the risk of VTE. However, data also show a trend toward an increased risk of intracranial bleeding. LMWH seems to be favorable on survival and VTE frequencies as compared to unfractionated heparin (Benjamin et al. 2017).
There is no clear evidence indicating when it is safe to initiate LMWH treatment. Case studies suggest that LMWH prophylaxis should not be initiated before a 24-h control computed tomography (CT) scan has been performed, demonstrating no progression in existing hematomas or new intracranial bleedings (Black et al. 1986; Gerlach et al. 2003; Kleindienst et al. 2003; Norwood et al. 2002). Later studies suggest starting LMWH between 24 and 72 hours (h) after the trauma while monitoring the patient’s progress with consecutive CTs to avoid initiating LMWH in patients with an expanding intracerebral hemorrhage (ICH) (Haddad and Arabi 2012; Minshall et al. 2011; Dudley et al. 2010).
The risks and benefits of LMWH were evaluated by Dudley et al. in a retrospective study of 287 TBI patients. In this study, patients received LMWH treatment between 48 and 72 h post-trauma after two CTs showing no sign of hemorrhage expansion. There was a low incidence of VTE (7.3%), and only one patient (0.4%) had a symptomatic expansion of a pre-existing ICH (Dudley et al. 2010). No difference in VTE frequencies was seen between two types of LMWH—enoxaparin and dalteparin.
A large observational cohort study of 2468 TBI patients compared early (<72 h) and late (>72 h) initiation of LMWH. The patients who received early prophylaxis had lower incidences of both deep venous thrombosis (DVT) and PE without any increased risk of neurosurgical intervention or death (Byrne et al. 2016). Two other studies have corroborated these results (Koehler et al. 2011; Jamjoom and Jamjoom 2013).
A small randomized, double-blinded pilot study found that patients with minor TBIs who received LMWH after a stable CT within 24 h post trauma (34 patients) had ICH progression rates similar to the placebo group (28 patients) (Phelan et al. 2012). Norwood et al. (2002) found similar results in a prospective, single-cohort observational study including 150 patients. Kurtoglu et al. found no significant differences in mortality or the incidence of DVT or pulmonary embolism (PE) in a small prospective, randomized, controlled trial on brain and spinal trauma patients who were treated with either intermittent graded pneumatic compression devices (60 patients) or LMWH (60 patients). LMWH was administrated after a stable control CT within 24 h post trauma. There was only one exacerbation of an epidural hematoma in each group (Kurtoglu et al. 2004). In a recent systematic review of 21 studies, Margolick et al. concluded that pharmacological prophylaxis started 24–48 h post trauma was safe in “low”-hemorrhagic-risk TBIs with no expansion upon repeated CT scans (Margolick et al. 2018).
The largest prospective study comes from Australia (Skrifvars et al. 2017), but is actually a post hoc analysis of the erythropoietin in traumatic brain injury (EPO-TBI) trial that included twice-weekly lower limb ultrasound screening. VTE was defined as an ultrasound-proven proximal DVT or a clinically detected PE. Of 603 patients, 119 (19.7%) developed VTE, mostly comprising DVT (102 patients, 16.9%) with a smaller number of PE events (24 patients, 4.0%) even if mechanical and pharmacological prophylaxis were adopted in most cases.
However, a national UK survey among 62 neurosurgeons indicated a wide variation when LMWHs were actually started in different types of TBIs, with median LMWH initiation from 1 to 7 days after trauma (Jamjoom et al. 2016). ICP monitoring with or without intraventricular drainage of hemorrhagic cerebrospinal fluid (CSF) may also affect when LMWH treatment is started, sometimes first after catheter withdrawal. A recent retrospective study of 155 patients, however, indicated that both standard heparin and LMWH were safe to administer while using active invasive monitoring devices (Dengler et al. 2016). A concern is at withdrawal, when to optimally stop and when to readminister LMWH.
In complex multitrauma patients who survived to ICU admission, prescreened for high VTE risk, TBI did not further increase the risk for VTE, especially in patients receiving pharmacological and mechanical thromboprophylaxis (Valle et al. 2014). Byrne et al. found LMWH to be superior to heparin in preventing PE in patients after major trauma. Their propensity-matched analysis included 153,474 patients. The matched results were 1.4% PE in patients receiving LMWH and 2.4% PE in the group that received heparin (Byrne et al. 2017).
Minshall et al. compared the safety and efficacy of heparin with the LMWH enoxaparin and found that patients who received LMWH after TBI had fewer complications. However, patients receiving heparin had more severe TBIs, suggesting that heparin was favored by the physicians treating those patients, perhaps due to better monitoring capabilities, a shorter half-life, and the option of better reversal with protamine (Minshall et al. 2011). Dengler et al. retrospectively evaluated heparin and LMWH in TBI patients and found no difference in DVT or hemorrhage expansion using intracranial pressure monitoring devices. In that study, heparin was not reserved for the more severe TBI cases (Dengler et al. 2016).
In addition to the risks discussed above, brain trauma patients can also develop an early acute coagulopathy of trauma shock (aCoTS) (Johansson et al. 2011) or a later disseminated intravascular coagulation (DIC). DIC usually occurs 6–72 hours’ post trauma (Mukhopadhyay et al. 2013). Both aCoTS and DIC are strong predictors of a poor outcome after TBI.
Coagulation monitoring in trauma has evolved to involve tests like thromboelastography (TEG®/ROTEM®) and thrombin generation (TGA) to better reflect hypo- or hypercoagulation than standard laboratory coagulation tests (Johansson et al. 2011; Miao et al. 2017). A recent trauma study reported that although TGA parameters indicated hypercoagulable states, they did not identify patients with DVT or PE (Voils et al. 2016). Hincker et al. identified a preoperative hypercoagulable ROTEM® both with thromboplastin reagent InTEM and tissue factor reagent ExTEM activated profiles (clot formation time (CFT), alpha angle (AA), and maximal clot formation (MCF)) in 10 out of 333 noncardiac surgery patients who developed postoperative DVTs even after LMWH or heparin thromboprophylaxis. There was no indication of this hypercoagulation in the activated partial thromboplastin time (aPTT), protrombin time (PT), or platelet count analyses (Hincker et al. 2014). In TBI patients and other trauma patients, alcohol can induce a hypocoagulable thromboelastographic profile in the initial trauma setting, possibly explaining the DVT-reducing effect of alcohol (Cook et al. 2015).
There are several types of LMWHs. They all inhibit the common coagulation pathway by indirectly inhibiting factor Xa (fXa) and directly inhibiting factor IIa (fIIa) to varying extents as described by each type’s anti-fXa/anti-fIIa ratio. The current gold standard for monitoring LMWH treatment measures the anti-fXa activity in a patient’s plasma. However, this method neglects its anti-fIIa effect. TGA reflects the LMWH inhibition of both fXa and fIIa, potentially providing a better analysis that describes the full effect of the LMWH (Thomas et al. 2015). Usually thromboprophylactic doses of LMWH do not need laboratory monitoring other than platelet count to detect heparin-induced thrombocytopenia.
Also, the LMWH enoxaparin is primarily eliminated through the kidneys, making renal insufficiency an important factor for potential accumulation and thereby increased bleeding risk. Body weight (BW) is also known to affect the enoxaparin dose response (Costantini et al. 2013), with low BW posing a risk of overdose and high BW leading to potentially insufficient thromboprophylaxis under the standard dose regimes. Individual differences in bleeding risk and dose response to LMWH further complicate this issue. LMWHs are generally administered by a subcutaneous injection once a day and exhibit peak and trough effects during treatment. The LMWH anti-fIIa effect can be reversed with protamine more or less depending on the specific type of LMWH’s anti-fXa/anti-fIIa ratio (Thomas et al. 2015).
Finally, recent guidelines from Neurocritical Care Society (NCS) and Society of Critical Care Medicine (SCCM) recommend to start LMWH in patients with stable hematomas and no ongoing coagulopathy within 48 h after hospital admission together with mechanical devices (Nyquist et al. 2016). This strategy is also recommended by the updated TBI guidelines from the UK Brain Trauma Foundation (Carney et al. 2017). They consider that the benefits outweigh the risks—the survey referred to above indicates however that these guidelines are not followed (Jamjoom et al. 2016). A concern is the severity of the TBI and the risk for a progressive hemorrhagic injury (PHI). A risk score to predict PHI has been suggested and might increase the safety of LMWH administration after TBI (Yuan et al. 2012). The systematic review by Shen et al. (2015) concludes that LMWH thromboprophylaxis appears to be safe among TBI patients with stabilized hemorrhagic patterns. Still, there are many issues remaining to optimize its efficiency and safety (Shen et al. 2015; Carney et al. 2017). Vena cava filters are also an option in many trauma centers, especially in multitrauma patients with lower limb, pelvic, and spinal fractures together with TBI (Jeremitsky et al. 2013).
Tips, Tricks, and Pitfalls
-
Today we have no optimal laboratory technique to monitor various anticoagulants or thromboprophylactic drugs.
-
There is a thin balance between aggravating TBI haemorrage with too early pharmacologic thromboprophylaxis and increasing risk for thromboembolism by delaying it.
-
Clinical judgement and evaluation from repetitive CT scans during the first 2–5 (or longer) days is the mainstay.
-
Calf compression and then starting with low dose LMWH thromboprophylaxis after 2–4 days if the TBI induced haemorrhage seems to be stabilised is recommended by most guidelines.
-
High alert to stop LMWH if haemorrhage is expanded – protamin can revert some of its effect depending on the anti-Xa/anti-Iia ratio of the specific LMWH.
-
LMWH should be stopped 12 h before manipulation or withdrawal of intracerebral pressure monitoring/ventricular drainage catheters.
-
Simultaneous DIC, thrombocytopenia should be resolved/treated before considering LMWH.
References
Agnelli G, Piovella F, Buoncristiani P, et al. Enoxaparin plus compression stocking compared with compression stocking alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med. 1998;339:80–5.
Benjamin E, Recinos G, Aiolfi A, et al. Pharmacological thromboembolic prophylaxis in traumatic brain injuries: low molecular weight heparin is superior to unfractionated heparin. Ann Surg. 2017;266:463–9.
Black PM, Baker MF, Snook CP. Experience with external pneumatic calf compression in neurology and neurosurgery. Neurosurgery. 1986;18:440–4.
Byrne J, Mason S, Gomez D, et al. Timing of pharmacologic venous thromboembolism prophylaxis in severe traumatic brain injury: a propensity-matched cohort study. J Am Coll Surg. 2016;223:621–31.
Byrne J, Geerts W, Mason S, et al. Effectiveness of low-molecular-weight heparin versus unfractionated heparin to prevent pulmonary embolism following major trauma. J Trauma Acute Care Surg. 2017;82:252–62.
Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Cook M, Louis S, McCully S, et al. Positive blood alcohol is associated with reduced DVT in trauma. Injury. 2015;46:131–5.
Costantini T, Min E, Box K, et al. Dose adjusting enoxaparin is necessary to achieve adequate venous thromboembolism prophylaxis in trauma patients. J Trauma Acute Care Surg. 2013;74:128–35.
Davidson JE, Williams DC, Hoffman MS. Effect of intermittent pneumatic leg compression on intracranial pressure in brain-injured patients. Crit Care Med. 1993;21:224–7.
Dengler B, Mendez-Gomez P, Chavez A, et al. Safety of chemical DVT prophylaxis in severe traumatic brain injury with invasive monitoring devices. Neurocrit Care. 2016;25:215–23.
Dudley R, Aziz I, Bonnici A, et al. Early venous thromboembolic event prophylaxis in traumatic brain injury with low-molecular-weight heparin: risks and benefits. J Neurotrauma. 2010;27:2165–72.
Gerlach R, Scheuer T, Beck J, et al. Risk of postoperative hemorrhage intracranial surgery after early nadroparin administration: results of a prospective study. Neurosurgery. 2003;53:1028–34.
Haddad S, Arabi Y. Critical care management of severe traumatic brain injury in adults. Scand J Trauma Resusc Emerg Med. 2012;20:12.
Hincker A, Feit J, Sladen R, et al. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18:549.
Jamjoom A, Jamjoom A. Safety and efficacy of early pharmacological thromboprophylaxis in traumatic brain injury: systematic review and meta-analysis. J Neurotrauma. 2013;30:503–11.
Jamjoom AA, Chari A, Salijevska J, et al. A national survey of thromboprophylaxis in traumatic brain injury in the United Kingdom. Br J Neurosurg. 2016;30:240–5.
Jeremitsky E, St Germain N, Kao AH, et al. Risk of pulmonary embolism in trauma patients: not all created equal. Surgery. 2013;154:810–4.
Johansson P, Sørensen A, Perner A, et al. Disseminated intravascular coagulation or acute coagulopathy of trauma shock early after trauma? An observational study. Crit Care. 2011;15:272.
Kaufman H, Satterwhite T, McConnell B, et al. Deep vein thrombosis and pulmonary embolism in head injured patients. Angiology. 1983;34:627–38.
Kleindienst A, Harvey HB, Mater E, et al. Early antithrombotic prophylaxis with low molecular weight heparin in neurosurgery. Acta Neurochir. 2003;145:1085–90.
Knudson MM, Ikossi DG, Khaw L, et al. Thromboembolism after trauma: an analysis of 1602 episodes from the American College of Surgeons National Trauma Data Bank. Ann Surg. 2004;240:490–6.
Koehler D, Shipman J, Davidson M, et al. Is early venous thromboembolism prophylaxis safe in trauma patients with intracranial hemorrhage. J Trauma. 2011;70:324–9.
Kurtoglu M, Yanar H, Bilsel Y, et al. Venous thromboembolism prophylaxis after head and spinal trauma: intermittent pneumatic compression devices versus low molecular weight heparin. World J Surg. 2004;28:807–11.
Margolick J, Dandurand C, Duncan K, et al. A systematic review of the risks and benefits of venous thromboembolism prophylaxis in traumatic brain injury. Can J Neurol Sci. 2018;45:432–44.
Miao W, Zhao K, Deng W, Teng J. Coagulation factor hyperfunction after subarachnoid hemorrhage induces deep venous thrombosis. World Neurosurg. 2017;110:46–50.
Minshall C, Eriksson E, Leon S, et al. Safety and efficacy of heparin or enoxaparin prophylaxis in blunt trauma patients with a head abbreviated injury severity score >2. J Trauma Injury. 2011;71:396–400.
Mukhopadhyay A, Chhabra G, Sharma S, et al. Coagulopathy as prognostic marker in acute traumatic brain injury. J Emerg Trauma Shock. 2013;6:180–5.
Norwood SH, McAuley CE, Berne JD, et al. Prospective evaluation of the safety of enoxaparin prophylaxis for venous thromboembolism in patients with intracranial hemorrhagic injuries. Arch Surg. 2002;137:696–701.
Nyquist P, Bautista C, Jichici D, et al. Prophylaxis of venous thrombosis in neurocritical care patients: an evidence-based guideline: a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care. 2016;24:47–60.
Page RB, Spott MA, Krishnamurthy S, et al. Head injury and pulmonary embolism: a retrospective report based on the Pennsylvania Trauma Outcomes study. Neurosurgery. 2004;54:143–8.
Phelan H, Wolf S, Norwood S, et al. A randomized, double-blinded, placebo-controlled pilot trial of anticoagulation in low-risk traumatic brain injury. J Trauma Acute Care Surg. 2012;73:1434–41.
Shen X, Dutcher SK, Palmer J, et al. A systematic review of the benefits and risks of anticoagulation following traumatic brain injury. J Head Trauma Rehabil. 2015;30:29–37.
Skillman JJ, Collins RE, Coe NP, et al. Prevention of deep vein thrombosis in neurosurgical patients: a controlled, randomized trial of external pneumatic compression boots. Surgery. 1978;83:354–8.
Skrifvars MB, Bailey M, Presneill J, et al. EPO-TBI investigators and the ANZICS Clinical Trials Group. Venous thromboembolic events in critically ill traumatic brain injury patients. Intensive Care Med. 2017;43:419–28.
Thomas O, Lybeck E, Strandberg K, et al. Monitoring low molecular weight heparins at therapeutic levels: dose-responses of, and correlations and differences between aPTT, anti-factor Xa and thrombin generation assays. PLoS One. 2015;10(1):e0116835.
Turpie AG, Hirsh J, Gent M, et al. Prevention of deep vein thrombosis in potential neurosurgical patients. A randomized trial comparing graduated compression stockings alone or graduated compression stockings plus intermittent compression with control. Arch Intern Med. 1989;149:679–81.
Valle EJ, Van Haren RM, Allen CJ, et al. Does traumatic brain injury increase the risk for venous thromboembolism in polytrauma patients? J Trauma Acute Care Surg. 2014;77:243–25.
Voils S, Lemon S, Jordan J, et al. Early thrombin formation capacity in trauma patients and association with venous thromboembolism. Thromb Res. 2016;147:13–5.
Yuan F, Ding J, Chen H, et al. Predicting progressive hemorrhagic injury after traumatic brain injury: derivation and validation of a risk score based on admission characteristics. J Neurotrauma. 2012;29:2137–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Schott, U., Steiness, M.Z. (2020). Prophylaxis Against Venous Thromboembolism (VTE) in Patients with Traumatic Brain Injury (TBI). In: Sundstrøm, T., Grände, PO., Luoto, T., Rosenlund, C., Undén, J., Wester, K. (eds) Management of Severe Traumatic Brain Injury. Springer, Cham. https://doi.org/10.1007/978-3-030-39383-0_71
Download citation
DOI: https://doi.org/10.1007/978-3-030-39383-0_71
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-39382-3
Online ISBN: 978-3-030-39383-0
eBook Packages: MedicineMedicine (R0)