Abstract
Infertility has become a major social concern, with high demand for treatment. Due to the high prevalence of genetic abnormalities among men suffering from infertility with severe oligozoospermia and azoospermia, cytogenetic testing is highly warranted. These tests can diagnose some, but not all, of the causes of poor reproductive potential in men. Unfortunately, these genetic tests are considered a monetary burden to some patients. As a result, these patients are deprived of the proper diagnosis and treatment for their infertility problems. In addition, these genetic tests are not readily available in centres, especially in developing countries, and are not covered by insurance. Genetic diagnoses are valuable for the determination of the prognosis, decisions regarding treatment options and management for both the male partner and the couple as a whole. Inadequate evaluation of the genetic causes of male infertility may affect management due to a lack of proper counselling and the suboptimal prevention of vertical transmission of genetic defects during assisted reproductive technologies. Despite recent advances in technology and diagnostic examinations, many men do not have identifiable causes of their infertility. The epidemiology of male infertility is difficult to study for several reasons. There are considerable variations in the frequency of male infertility and its aetiologies worldwide, and its nature has been poorly studied in heterogeneous data. Knowing the global epidemiology of different causes of infertility is fundamental for the effective delivery of care to these affected individuals. Only a handful of large-scale studies have addressed the epidemiology of genetic aetiologies of male infertility, and the published data are littered with significant shortcomings. Further high-quality methodological studies are needed to establish the true epidemiology of each genetic cause of male infertility. A deep understanding of all the aspects of the genetic conditions causing male infertility is needed in order to offer infertile couples the most appropriate treatment for their disorders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Epidemiology
- Male infertility
- Genetic abnormalities
- Chromosomal abnormalities
- Azoospermia
- Severe oligozoospermia
- Klinefelter syndrome
- Y chromosome microdeletions
- 47,XYY
- 46,XX
- Congenital bilateral absence of vas deferens
- Kallmann syndrome
- Robertsonian translocation
- Reciprocal translocation
- Inversion
-
Despite exhaustive efforts to determine the exact nature of the causes of male infertility, many are still diagnosed with idiopathic male infertility.
-
The true incidence and aetiologies of male infertility remain poorly studied and characterized.
-
Geographical variation is believed to be the cause of different incidences of male infertility.
-
The main genetic variants leading to male infertility are chromosomal alterations, inversions, translocation, Y chromosome microdeletions and gene mutations.
-
A comprehensive male evaluation for all partners of infertile couples should be performed in order to uncover possible significant and treatable medical conditions before pursuing therapies with ART.
-
Large-scale, prospective, epidemiological studies may enhance our understanding of the genetic disorders of male infertility.
Introduction
Infertility, as defined by the recent consensus-based and evidence-driven set of terminologies set by the International Committee for Monitoring Assisted Reproductive Technologies (ICMART), is a “disease characterized by the failure to establish a clinical pregnancy after 12 months of regular, unprotected sexual intercourse or due to an impairment of a person’s capacity to reproduce either as an individual or with his/her partner” [1]. Infertility affects 15% of couples desiring to have a child [2]. Male factor as a sole cause of infertility accounts for 20% of cases, while both male and female factors contribute in another 20–30% of cases [3]. Another study of male infertility data from five European countries showed that 6.4–42.4% of cases were due to male factors [4].
Aetiologies of male factor infertility are multifactorial. In 30–40% of cases, the cause of male infertility remains undiscovered, termed idiopathic [5]. Half of the cases of idiopathic infertility could be due to known or unknown genetic abnormalities [6]. The frequency of known genetic abnormalities increases with the severity of the spermatogenic defect. Numerical and structural defects comprise the main chromosomal abnormalities affecting paternity of men wanting to father a child [7]. This accounts for 6% of infertile men. Azoospermic men experience higher prevalence rates up to 15%.
With the advancement of assisted reproductive technologies (ART), such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), clinicians must know the role played by genetics in complex male factor infertility cases [8]. The frequency of the inheritance of mutations through these assisted reproduction procedures and their impact on future generations are not yet fully discerned.
Male factor infertility is a complicated disorder, wherein underlying aetiologies often remain undetected [5]. Future research on the genetics and molecular defects in sperm production and function is warranted to improve detection. This will lead to more focused treatment of men with genetic abnormalities. The prevalence of genetic anomalies warns clinicians of the importance of genetic testing in male factor infertility. This chapter will focus on the epidemiology of the common genetic disorders causing poor male reproductive potential, with clinical applications.
Epidemiology of Infertility
The true incidence and aetiologies of male infertility remain poorly studied and characterized [9]. In 2007, Boivin et al. performed an international estimate of infertility prevalence from 25 population surveys [10]. It was estimated that 72.4 million people were infertile. From this group, approximately 40.5 million people were seeking infertility medical care. Mascarenhas et al. estimated the prevalence of infertility between 1990 and 2010 in 190 countries [11]. The authors identified 277 demographic and reproductive health surveys and obtained the individual-level questionnaire responses. In this systematic analysis of surveys, there was an increase in the absolute number of couples experiencing infertility, from 42.0 million in 1990 to 48.5 million in 2010. In America, an estimated seven million couples seek infertility care annually [12]. Data of 11,067 men from the National Survey of Family Growth performed by the Centers for Disease Control and Prevention to determine the frequency of male infertility evaluations showed that only 18% of couples did not complete a male infertility evaluation when the male partners were asked. This increased to 27% when 25,846 female partners were asked. This corresponds to 370,000–860,000 men who were not seen and examined during an infertility evaluation. In the latest result on the study by Agarwal et al., at least 30 million men were considered infertile [13]. The highest rates were observed in Africa and Eastern Europe. Across the world, Australia and Central and Eastern Europe had the most number of infertile men, consisting of 8–9% and 8–12%, respectively. Other regions, such as North America (4.5–6%), sub-Saharan Africa (2.5–4.8%) and Europe (7.5%), showed lower calculated percentages of infertile men.
A literature search of systematic reviews and meta-analyses of population-based studies was performed on the factors that affect male infertility [13]. Out of 86 relevant articles, 16 were included in the study. The percentage of male infertility cases globally varied from 2.5 to 12% (Table 5.1). The calculated global data revealed that 20–70% had a cause of infertility that was attributable to male factor [13]. This is a wide-range percentage compared to the commonly cited percentage of 20%, which was derived from a multicentre survey of 1686 couples in 3 French regions [3]. In this recent study by Agarwal, the calculated percentages of male infertility worldwide were based on a review of the current literature. This current study demonstrates the infertility cases in regions that were due to male factor (Table 5.2), which included Asia (37%), sub-Saharan Africa (20–40%), Oceania (40%), Africa (43%), Europe (50%), North America (50%), Latin America (52%), Central/Eastern Europe (55.73%) and the Middle East (60–70%).
Geographical variation is believed to be the cause of different incidences of male infertility. Ikechebelu et al. evaluated 314 infertile couples from Southeastern Nigeria for the aetiologies of their poor reproductive potential [14]. Thirty-five percent (n = 110) of the cases had secondary infertility, while 65% (n = 204) had primary infertility. Male factor infertility was responsible for 42.4% of the infertile couples. The most common causes for male infertility were oligozoospermia and asthenozoospermia, amounting to 35.9% and 32.3%, respectively. In Western Siberia, 333 (16.7%) couples were considered infertile from 2000 randomly selected married couples in an epidemiological study conducted by Philippov et al. [15]. From the semen analysis of the men tested, 45.7% had identifiable abnormalities, while 54.3% remained idiopathic. Inflammatory disease of the male accessory gland was the most common cause of male infertility, amounting to 12.9% of cases, and 8.6% of these inflammatory cases resulted in obstructive azoospermia. Aflatoonian et al. studied the demographic characteristics of infertile couples in the province of Yazd, Iran [16]. Among 5200 couples, 5.52% (n = 277) experienced infertility. Of these infertile couples, 3.48% and 2.04% had primary and secondary infertility, respectively. The prevalence of infertility was higher in couples living in urban areas compared to those living in rural areas, but this difference was not statistically significant (p = 0.001). In a Polish multicentre study of 1517 individuals, 18.9% of couples were both contributory to poor reproductive potential. Idiopathic aetiologies were seen in 15.99% of cases [17]. Male factor infertility accounted for 55.73% of cases. A cross-sectional population survey on fertility status conducted by Datta et al. in Britain was applied to 8869 women and 6293 men aged 16–74 years [18]. Approximately 10% of men reported infertility in this group. The prevalence of infertility was noted to be higher among individuals who postponed their parenthood. In addition, 57.3% of the men seeking help for their infertility problems had better education and higher status in their occupations. In 2004, Bayasgalan et al. determined the clinical patterns and major causes of 430 infertile couples attending an infertility clinic in Mongolia [19]. Male factor infertility was present in 25.6% of cases. Obstructive azoospermia (8.4%) and acquired testicular damage (5.4%) showed higher prevalence compared to other causes. In India, an estimated 15–20 million couples suffered from infertility in 2009 [20].
More accurate infertility rates can be observed in developed countries, such as Australia, Europe and North America, compared to developing countries. These countries have organizations, such as the National Survey of Family Growth [21], Australian Institute for Health and Welfare [22] and European Association of Urology (EAU) [23], that provide the most detailed reporting of data available in infertility problems. Despite the figures, it is very difficult to determine an unbiased prevalence of male infertility within the global, regional or national populations due to the low methodological quality of evidence [24].
General Epidemiology of Genetic Infertility
Complex and multifactorial conditions can cause male infertility, and aetiologies of male infertility can be either acquired or congenital. Despite all exhaustive efforts to determine the exact nature of the causes of male infertility, many are still diagnosed with idiopathic male infertility. A number of these causes can be explained by genetic abnormalities [25]. The search for “hidden” genetic factors was widely inefficacious in detecting recurrent genetic factors with potential clinical applications [26].
Genetic anomalies, including numerical and structural chromosomal abnormalities, have been linked with unexplained oligozoospermia and azoospermia [27]. The prevalence of chromosomal abnormalities is indirectly proportional to sperm concentration [28]. These are seen less in men with normal sperm concentrations (<1%) compared to men with oligozoospermia (5%) or azoospermia (10–15%).
Azoospermia can be identified in 15% of men with poor reproductive potential [29]. This can be classified as obstructive azoospermia (OA) and non-obstructive azoospermia (NOA). Forty percent of azoospermic men present as OA, while the remaining 60% are NOA, and the latter is frequently associated with testicular failure. Some of the causes of NOA remain unknown. This might be secondary to genetic abnormalities. Genetic anomalies causing azoospermia can be grouped into two large categories comprised of chromosomal and non-chromosomal [30]. Chromosomal anomalies can be further subdivided into structural abnormalities, including chromosomal inversions and translocations and Y chromosome microdeletions (YCMD) , and numerical abnormalities (aneuploidy). Non-chromosomal anomalies include sperm mitochondrial genome defects and epigenetic alterations of the genome. A higher incidence of aneuploidy can be observed in men with NOA. In a chromosome analysis of azoospermic men undergoing ICSI, the overall aneuploidy rate of 11.4% (p = 0.0001) in men with NOA was significantly higher than the 1.8% rate demonstrated in epididymal sperm from men with OA and the 1.5% rate detected in ejaculated sperm [31]. Cytogenetic analysis is significant in male infertility, as suggested by the frequency of chromosomal abnormalities in these infertile men, especially if the couple will undergo ART [32].
Some epidemiological studies are available on the genetic basis leading to the poor reproductive potential of male infertility. In an earlier review of pooled data from 11 surveys of 9766 men with severe oligozoospermia and azoospermia, the incidence of chromosomal abnormalities was 5.8% [33]. Autosomal abnormalities were detected in 1.5% of this combined population of men. On the other hand, sex chromosome anomalies were higher in azoospermic and infertile men, with an incidence of 4.2%. In another series of studies of 94,465 newborn male infants, chromosomal abnormalities were detected in 0.38% (n = 366) compared to phenotypically normal newborns. Of those with anomalies , 0.25% (n = 232) were diagnosed with autosomal defects, while 0.14% had sex chromosomal abnormalities (n = 131). In another study, a cytogenetic investigation in France was performed in infertile men with low sperm concentration over a period of 25 years [34]. In total, 13,154 men were clinically examined and biologically investigated to determine the genetic abnormalities of their poor reproductive outcomes. Somatic cytogenetic abnormalities were detected in 7.7% of these infertile men. The highest abnormalities were observed in men with NOA (16.7%, n = 108), followed by men with sperm counts <5 × 106/ml (9.7%, n = 63), 5–10 × 106/ml (4.3%, n = 27) and > 10–20 × 106/ml (0.5%, n = 3). Sex chromosomal abnormalities were demonstrated more often in patients with NOA (77.1%, p < 0.001) compared to men with oligozoospermia and obstructive azoospermia. Nagvenkar et al. determined the chromosomal constitution of 88 infertile Indian men, comprising 42 azoospermic men and 46 severe oligozoospermic men undergoing ICSI [35]. Overall, 10.2% had chromosomal abnormalities ; higher rates were observed in men with azoospermia (14.3%) compared to men with severe oligozoospermia (6.5%). Robertsonian translocation was detected in one patient. In a study by Samli et al., 819 men with azoospermia (n = 383) and oligozoospermia (n = 436) were evaluated for genetic factor as their cause of their infertility [28]. Chromosomal abnormalities were diagnosed in 12% (n = 47) of azoospermic men and 4% (n = 20) of oligozoospermic men. In the azoospermia group, 19% (n = 9) of the chromosomal anomalies were due to autosomal abnormalities, while 80% (n = 38) were secondary to gonosomal abnormalities. Among 2710 infertile couples who were candidates for ART in Italy, 74 aberrant karyotypes were found [36]. This corresponded to 1.5% (n = 40) in men. Most of the observed chromosomal abnormalities (2.2%) were from men whose partners underwent ICSI; this was higher compared to men whose partners underwent intrauterine insemination (IUI) (0.3%) and IVF (1.1%). In another study in Brazil, Mafra et al. made a retrospective genetic assessment of 143 infertile men composed of 100 men with severe oligozoospermia and 43 men with NOA [37]. Genetic abnormalities were detected in 18.8% of all infertile men. Nine men had chromosomal abnormalities, of which four were from the azoospermia group and five from the oligozoospermia group. YCMD was found in 4.2% of men, all of which were detected in the azoospermia and oligozoospermia groups. A study in the Middle East showed a 9.59% incidence of chromosomal abnormalities in 511 patients [38]. Nineteen (10.6%) of 179 Qatari men had chromosomal abnormalities, while 30 (9.04%) of 332 non-Qatari men were similarly diagnosed. Chromosomal abnormalities were diagnosed in 10.78% of azoospermic men, while they were detected in 7.5% of oligozoospermic men. Overall, the most common chromosomal abnormality was Klinefelter syndrome , which was present in 19 men. This was followed by 13 men with YCMD [azoospermia factor (AZF)a = 1; AZFb and c = 5; AZFc = 7]. Both Robertsonian translocation and reciprocal translocation were demonstrated in six men in each abnormality. Five men had other chromosomal aberrations. Punab et al. conducted a 9-year monocentre, prospective, clinical-epidemiological study of 8518 infertile men from Estonia with reduced total sperm count (<39 million per ejaculate) in at least 2 consecutive semen analyses [39]. Among these male partners of infertile couples, 20.4% (n = 1737) had severe male factor infertility. In 40 per cent (n = 695) of cases, the primary cause of infertility was determined, but 60% (n = 1042) remained idiopathic. In patients with known genetic aetiologies (n = 135), 87.4% had extreme infertility comprised of azoospermia, cryptozoospermia and aspermia. The prevalence of congenital abnormalities was not clearly associated with the severity of deranged spermatogenesis. In Eastern China, Xie et al. reviewed the cytogenetic results from 912 men with NOA (n = 534) and severe oligozoospermia (n = 378), while 215 normozoospermic men served as the control group [40]. Genetic anomalies were detected in 22.6% (n = 206) of cases. Among these, 27.35% (n = 146) of azoospermic men and 15.9% (n = 60) of oligozoospermic men had genetic abnormalities. Four (1.9%) men from the control group and 138 (25.8%) men from the NOA group had chromosomal abnormalities. The NOA group had a higher frequency of the 47,XXY karyotype compared to the oligozoospermic group (8% vs 1.1%, respectively). Likewise, a higher incidence of YCMD was observed in the NOA group (17.8% vs 13.2%, respectively).
The main genetic variants leading to male infertility are chromosomal alterations, inversions, translocation, Y chromosome microdeletions and gene mutations [41].
Epidemiology of Specific Genetic Abnormalities
Klinefelter Syndrome
Klinefelter syndrome (KS) is considered the most common chromosomal aneuploidy in infertile men with testicular failure [42]. This is more frequently seen in men with azoospermia, with a prevalence of 10%, and severe oligozoospermia, with a prevalence of 0.7%. Only 12% of patients with KS are detected prenatally, while diagnosis during their childhood and adolescence is approximately 25%; more than half of them will be left undiagnosed during their lifetime [43]. The classic form 47,XXY constitutes 80–90% of all cases of KS [44]. Of the other variants of KS, 48,XXYY occurs more frequently in 1:18,000–1:40,000 male births [45] compared to other forms , such as 48,XXXY and 49,XXXXY [46], which appear in 1:50,000 and 1:85,000–1:100,000 male births, respectively.
In Denmark, all cytogenetic examinations have been registered in the central registry since 1961 [47]. Of 76,526 prenatal examinations , 163 foetuses were detected with the KS karyotype. This resulted in a prevalence of 213 per 100,000 males. Among 2,480,858 males born between 1931 and 2000, postnatal diagnosis of KS was described in 696 boys and men. Among boys aged 10–14 years, the prevalence of diagnosed KS was 14.2 per 100,000 males, while a prevalence of 35–40 per 100,000 was observed in males aged 25–54 years. In America, a newborn screening for methylated FMR1 DNA to test for KS was performed in 36,124 newborn males [48]. In total, 57 were diagnosed with KS, showing an incidence of 1 in 633 newborn males. Of 16,252 samples from white males, 27 had KS. Of 10,979 samples from African Americans, 20 had KS. Three newborn males out of 5396 samples from Hispanic males and 847 Asian males were diagnosed with KS. In the Middle East, KS was diagnosed in 19 of 511 men [38]. The frequency of these genetic abnormalities increases with the severity of the spermatogenic defect.
A meta-analysis on sperm recovery and ICSI outcomes on men with KS was performed by Corona et al. in 37 trials comprising 1248 patients. An overall 44% sperm retrieval rate was detected per TESE cycle [49]. Similar results were observed for the biochemical pregnancy rate (43%) and live birth rate (43%).
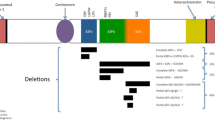
Y Chromosome Microdeletions
YCMD is the second most common genetic cause of male factor infertility after KS [50]. The Y chromosome contains different genes that are important for the development of testis and spermatogenesis in humans [51]. The long arm of the Y chromosome (Yq) is susceptible to intrachromosomal deletions, and AZF microdeletions occur in infertile men. YCMD can occur in distinct variations, including AZFa, AZFb and AZFc. In the general population, Yq microdeletions are estimated to occur in 1:4000 men. However, in infertile men, their frequency is 1:12. The worldwide prevalence of AZF microdeletions in infertile men is 7% based on an analysis of more than 30,000 chromosomes.
YCMD is usually seen in men with severe oligozoospermia and azoospermia. In a meta-analysis by Yousefi-Razin et al. among Iranian infertile men, the frequency of Yq microdeletions was 12.1%, particularly among those with severe oligozoospermia and azoospermia [52]. Johnson et al. determined the threshold sperm concentration for genetic analysis of YCMD in 1473 infertile men in a multi-ethnic urban population in the United Kingdom [53]. In this study, the prevalence of microdeletions was 4%. Among men with AZF microdeletions, none of them had a sperm concentration more than 0.5 × 106/ml. Using this lowered sperm concentration threshold, a high sensitivity of 100% and increased specificity of 31% were observed.
Various AZF loci microdeletions differ among various populations according to global estimates. Chellat et al. determined the frequency of YCMD among 80 Algerian infertile men with azoospermia (n = 49) and oligoasthenoteratozoospermia (n = 31) and compared them to 20 fertile control men [54]. Only one man from the azoospermia group had AZFc microdeletions, suggesting an overall AZF deletion rate of 1.3% among this group of men. Among 1306 infertile Korean men who underwent molecular screening for YCMD, microdeletions were detected in 7.7% (n = 101) of cases [55]. AZFc microdeletions (54.4%) were the most commonly detected deletions, followed by AZFb (7.9%) and AZFa (5.0%). Among men with AZFc microdeletions, 38.4% had azoospermia, and 96.4% had oligozoospermia (<1 × 106 sperm/ml, 85.2%; 1–5 × 106 sperm/ml, 11.1%; 5–20 × 106 sperm/ml, 3.7%). Out of 146 Tunisian infertile men with sperm counts <5 × 106/ml (azoospermic =76; oligospermic = 70), 6.85% (n = 10) had AZF deletions [56]. Among azoospermic men, 11.84% (n = 9) had microdeletions. AZFc microdeletions were detected in eight azoospermic men and one oligozoospermic man. Three azoospermic men demonstrated AZFa, AZFB and AZFc microdeletions. In a study by Sen et al. in Indian populations, 3.4% (n = 56) of 1636 infertile men had Yq microdeletions [57]. This increased to 5.8% (n = 215) when additional data from published studies in the Indian population were included, constituting a total of 3647 cases. AZFc microdeletions (46.6%) were the most commonly observed, particularly in azoospermic men. Compared to Western populations, the Indian population had a lower frequency of Yq microdeletions.
AZFc is the most commonly deleted locus in male infertility, accounting for 60–70% of cases. This is followed by microdeletions of AZFa (0.5–4%), AZFb (1–5%) and AZFb+c (1–3%) [58]. Bansal et al. studied the AZFc region of the Y chromosome for complete (b2/b4) and partial microdeletions (gr/gr, b1/b3, b2/b3) [59]. This involved 822 infertile men and 255 proven fertile men. Higher cases of partial AZFc microdeletions were observed compared to complete deletions (6.20% vs 0.97%). gr/gr (5.84%) was most commonly seen in partial deletions. Although no significant difference was observed, men with gr/gr deletions had lower sperm counts compared to those without the deletions (54.20 ± 57.45 million/ml vs 72.49 ± 60.06 million/ml, p = 0.071). In addition, men with gr/gr deletions were at significantly higher risk of poor reproductive potential (OR = 1.821, 95% CI = 1.39–2.37, p = 0.000).
In men with severe testicular histopathology, including hypospermatogenesis, maturation arrest and Sertoli cell-only syndrome , 22–55% may harbour these microdeletions [59].
Congenital Bilateral Absence of Vas Deferens
Cystic fibrosis (CF) is the most commonly occurring autosomal recessive disorder in 1:1600 individuals from Northern European descent/non-Hispanic white populations [60]. Anomalies in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which controls the elevation of sweat sodium chloride concentrations through the adenosine monophosphate (AMP) pathway and regulation of the exocrine epithelial cell tubal secretion consistency, can result in CF. The Cystic Fibrosis Mutation Database has identified more than 2000 CFTR mutations [61].
Congenital bilateral absence of the vas deferens (CBAVD) is strongly related to cystic fibrosis (CF) [62]. The CFTR gene, which is located on chromosome 7, is mutated in 60–90% of men with CBAVD [8, 63]. Men with this type of abnormality can either have two mild mutations in the CFTR gene or a combination of mild and severe mutations [8]. F50del is considered the most severe CFTR gene mutation, occurring in 60–70% of men with CBAVD [8]. Mutations of the CFTR gene may still be undetectable in 25% of men with CBAVD despite the completeness of CFTR gene screening. However, using comprehensive and rapid genotyping of mutations and haplotypes combined with searches for rare large realignments, 87.9% of CFTR defects can be detected in men with CBAVD [64]. CBAVD can be observed in 4–7% of azoospermic men and 25% of men with obstructive azoospermia [65].
Among the 27,177 cystic fibrosis chromosomal analyses from 29 European countries and 3 countries from North Africa, Estivill et al. studied the geographic distribution of 272 cystic fibrosis mutations [66]. The most common severe mutation encountered was delta F508, comprising 66.8% of the cases. Individuals from Denmark had the highest frequency of delta F508 mutations, while individuals from Algeria had the lowest (26.3%). Overall, 217 mutations were uncommon, with less than 1% frequency, while 55 mutations were common in 1 or more areas of Europe. On the other hand, the 5 T variant in intron 8 is the most common mild mutation in CBAVD [67].
In earlier studies by Kuligowska et al., transrectal ultrasound was performed in 276 infertile men with low semen volume and azoospermia [68]. There was an absence of anatomic abnormalities in 25.4% (n = 70) of cases. CBAVD was detected in 34.1% (n = 94) of men, while 11.2% (n = 31) were diagnosed with unilateral absence of the vas deferens.
Congenital unilateral absence of the vas deferens (CUAVD) is a different disease entity compared to CBAVD that results from embryologic Wolffian duct aberrancy [69]. Renal agenesis is usually seen in men with CUAVD. There is a 20% rate of CUAVD among men with unilateral renal genesis. On the other hand, men with CUAVD show a 79% rate of unilateral renal agenesis [62, 70]. If unilateral renal agenesis appears in CBAVD, this might be secondary to abnormal development of the entire mesonephric duct at a very early stage in the development of the embryo rather than a CF mutation [71].
47,XYY
Another chromosomal aneuploidy is XYY, which occurs in approximately 1:1000 live male newborns [72]. This happens due to nondisjunction at meiosis II, producing an extra Y chromosome. Men with 47,XYY syndrome have a wide variety of clinical presentations. These men are noted to have decreased fertility potential. Kim et al. presented three men with 47,XYY syndrome with varying degrees of oligozoospermia [73]. Most of these men had a normal phenotype; however, they were at greater risk for behavioural difficulties, learning disability, delayed development in speech and language and tall physical makeup [74].
In the Danish Cytogenetic Central Registry, 208 men were identified with 47,XYY from 1968 to 2008 [75]. The average prevalence was 14.2 per 100,000, and their median age at the time of diagnosis was 17.1 years. Shorter lifespans were also observed compared to men with normal karyotypes. The median age of survival was statistically less by approximately 10.4 years compared to the control group (67.5 years vs 77.9 years, respectively, p < 0.0001). In Iran, 37 cases of infertile men with 47, XYY were identified in a retrospective study [76]. Mosaicism was observed in 13 men, while 24 men had non-mosaicism. Among men with non-mosaic patterns, 9 had azoospermia, and 15 had oligozoospermia. Secondary infertility was demonstrated in two of the non-mosaic and three of the mosaic men.
Since this can be missed easily due to its wide spectrum of clinical presentations, accurate detection of this constitutional karyotype will help clinicians to correctly manage these men who undergo fertility evaluations [77].
46, XX
46,XX is a sex development disorder affecting 1:20,000 male newborns [78]. These individuals are phenotypically male and also display psychosexual identification as male. Their gonads are of a testicular pattern without evidence of ovarian tissues either grossly or microscopically. In addition, they have no female genital organs. The sex-determining region Y (SRY) is translocated to either end of the X chromosome or to an autosome [79].
In a review of records of patients evaluated for male fertility at two different institutions, six were identified to have 46,XX karyotypes. The mean age at diagnosis was 34.3 ± 4.5 years, and primary infertility was observed in all men. Semen analysis showed normal-volume azoospermia. Hormonal profiles of these men were consistent with hypergonadotropic hypogonadism. A literature search was done by Majzoub et al. that included 29 papers comprising 49 men with 46,XX [80]. Men with this disorder presented with sexual dysfunction (21%), reduced hair distribution (26.6%) and gynaecomastia (40%). In 83.7% of patients, the SRY gene was detected. The majority of these were translocated to a sex chromosome (95%) rather than an autosome (5%). In Turkey, ten men with 46,XX were identified upon evaluation in an infertility clinic between 2004 and 2015 [81]. The majority of cases (n = 8) had deletions of AZFa, AZFb and AZFc regions. Since most of them presented with hypergonadotropic hypogonadism, a negative effect of replacement therapies should be carefully observed. Lashkari et al. reported the genetic components of 8144 azoospermic and severe oligozoospermic Iranian men [82]. Among these men, 57 men were identified with 46,XX male sex reversal syndrome. Sixteen men presented with testosterone deficiencies, while 15 men were SRY-positive. In a recent publication from China of 144 males with 46,XX, hypergonadotropic hypogonadism was the main presentation of these men regardless of the availability of SRY [83]. Treatment options offered were limited to ART using donor sperm.
Kallmann Syndrome
Kallmann syndrome is one of the most common causes of hypogonadotropic hypogonadism. Mutations of the KAL1 gene are responsible for 30–70% of Kallmann syndrome cases. More than 25–50 genes were reported to cause idiopathic hypogonadotropic hypogonadism. Fifty per cent of all hereditary cases were mutations from these genes [84,85,86]. Hallmarks of this genetic disorder are anosmia and hypogonadotropic hypogonadism [87]. Fifty per cent of patients with this disorder result from incomplete embryonic migration of gonadotropin-releasing hormone (GnRH) synthesizing neutrons. Approximately 10–20% of men will demonstrate spontaneous reproductive function recovery despite lifelong treatment [86].
Over a period of 5 years, 32 individuals (male = 26; female = 6) from 12 Jordanian and Palestinian families were evaluated for Kallmann syndrome [88]. Nineteen patients had olfactory tract agenesis discovered on magnetic resonance imaging (MRI). Anosmia was found in 27 patients, while 5 patients were hyposmic. Among the men affected with Kallmann syndrome, 73% had cryptorchidism, while 65% had microphallus. All other male patients demonstrated delayed puberty, hypogonadism and infertility.
Even though the genetic understanding of this syndrome is mostly unknown, mutations were identified in 5–10% of men with this condition [89]. Mutations in the KAL gene and AHC gene may lead to X-linked recessive hypogonadotropic hypogonadism.
Translocations
In men with severe male factor infertility, chromosomal translocations are the most commonly observed autosomal structural aberration [39]. Reciprocal translocation and Robertsonian translocation comprise this type of chromosomal anomaly. The carriers of Robertsonian translocation have a fusion of the long arms of two acrocentric chromosomes [90]. This rearrangement occurs when there is fusion of the complete long arms of two homologous or non-homologous acrocentric chromosomes [13,14,15, 21, 22, and] and a loss of the short arms of the translocated chromosomes [91]. The most commonly observed aberrations are t(13q;14q) and t(14q;21q). In earlier studies on populations of infertile men, approximately 0.8% were noted to be carriers of Robertsonian translocations, which was nine times higher than the general population. This rearrangement is found in 1:1000 newborns [42, 92]. Reciprocal translocation is a mutual exchange of chromosomal materials and segments between non-homologous chromosomes. This occurs in 0.7% of severely oligozoospermic and azoospermic men [93, 94].
There are stronger alterations of semen quality in men with Robertsonian translocations compared to reciprocal translocations. Both reciprocal and Robertsonian translocations are associated with a high rate of sperm aneuploidy.
Mayeur et al. performed a retrospective observational study over a period of 10 years on the association of these chromosomal translocations with sperm defects [91]. One hundred and five fertile men were compared to 81 men carrying reciprocal translocations and 63 men carrying Robertsonian translocations. Men with Robertsonian translocations (14.3%) were less frequently observed with normozoospermia compared to men with reciprocal translocations (39.5%). Men with Robertsonian translocations (10.8 ± 14.0 × 106/ml; 14.6 ± 12.7) had statistically lower sperm concentrations and motility compared to the fertile group (90.8 ± 58.7 × 106/ml; 33.2 ± 6.6%) and reciprocal translocations (49.0 ± 50.1 × 106/ml; 22.1 ± 12.5%). Kim et al. reported a cytogenetic analysis of Korean patients suspected for chromosomal anomalies [95]. Among 4117 cases, 17.5% (n = 721) had chromosomal abnormalities. Aberrations in the structural chromosome of autosomes were found in 73% (n = 527) of cases. Translocations (43.6%) were the most frequent among this set of aberrations.
Inversions
Chromosomal inversions occur following two breaks in a chromosome and a subsequent 180° rotation of the segment before reinsertion [96]. In the general population, approximately 1–3% of individuals can demonstrate inversion, although the exact number remains unknown [95, 97, 98]. Carriers of this abnormality are at risk of infertility due to abnormal gamete production if there are an odd number of crossovers between the normal homologous chromosome and the inverted segment [96]; this will result in duplication or deletion. Chromosomal inversion can lead to infertility due to spermatogenic disturbances. These arise by the loops or eccentric fragments formed during meiosis. Suboptimal semen parameters can be observed in men with inversion carriers due to disrupted meiotic behaviour [99]. The risk of having a live birth with an unbalanced chromosomal karyotype is 1–10% [100]. A high degree of structural variability has been observed in human chromosome 9 [101].
The most common type of inversion is the pericentric inversion of chromosome 9, with an overall incidence of 1.98%, which is more frequently observed among those of African-American descent [102]. Male factor infertility is observed in 12% of patients with pericentric inversion [103].
Dana et al. performed a cytogenetic investigation of 900 infertile couples from Romania, of which 430 men had azoospermia and 76 oligozoospermia [104]. Among the individuals studied, 24 men (2.73%) had an inversion of chromosome 9. Mozdarani et al. studied 600 Iranian couples attending an infertility clinic. Fourteen men (4.69%) carrying a chromosome 9 inversion were detected [105]. During a 10-year period, Ait-Allah et al. reviewed the results of 652 cytogenetic studies on mid-trimester amniocentesis [102]. Pericentric inversion of chromosome 9 was detected in 27 cases. In this study, the incidence of inversion was 4.1%. In a Syrian population, 1 patient had an inversion out of 162 infertile men who underwent cytogenetic testing [106]. Pericentric inversion can present a variety of abnormal sperm parameters. In a study by Sasagawa et al. in six infertile men with pericentric inversion of chromosome 9 [107], semen analysis showed normozoospermia (n = 1), asthenozoospermia (n = 3), oligozoospermia (n = 1) and azoospermia (n = 1).
More reports and studies of chromosomal inversions are needed to assess their frequency and outcomes [98].
Significance and Difficulties in Epidemiological Studies in Genetic Male Infertility
Male infertility is a complex disease with a fundamental genetic basis. Due to the advent of ART, research on genetic aetiologies of male infertility has promptly expanded [108]. Genetic testing is now offered to infertile men to achieve appropriate diagnosis and treatment, including prognostic assessment. The detection of genetic factors in infertile men has become good practice for the applicable management of infertile partners.
A comprehensive male evaluation for all partners of infertile couples should be performed in order to uncover possible significant and treatable medical conditions before pursuing therapies with ART [109]. The difference of outcome of children born by ART and natural conception may be hampered by the genetic risks of infertile couples. Compared to the general neonatal population, ICSI foetal genetic testing showed an increase in de novo sex chromosomal aneuploidy (from 0.2% to 0.6%) and structural autosomal abnormalities (from 0.07% to 0.4%) and an increase in the number of inherited structural anomalies, mostly from the infertile male partner [110].
With the advancement of molecular genetic techniques, improvements in the diagnosis and treatment of male infertility have been observed. Clinical studies, karyotype investigation and biomarker research will equip clinicians to better and more deeply understand the aetiologies of male infertility. In an earlier retrospective study in 2 university-based male infertility clinics, 13 (1.1%) of 1236 patients had significant pathology [111]. One patient presented with azoospermia and bilateral small testis. Karyotyping revealed evidence of KS. The authors recommended that a comprehensive evaluation of the male partner by a male infertility specialist be provided for all couples presenting with fertility problems, including appropriate laboratory testing, such as genetic testing. Significant medical conditions are not frequently discovered during routine fertility assessments of the male partner. Since semen analysis can be easily performed in any laboratory, and no effective treatment exists for male factor infertility, comprehensive male factor infertility evaluations are usually bypassed, and most couples proceed directly to ART. This practice results in significant delays and even non-diagnosis of serious underlying medical conditions of men labelled as “infertile” and their potential children. In another study, Kolettis et al. determined the incidence of significant medical pathologies determined during a male infertility evaluation of 536 patients at 2 academic infertility practices [112]. Six per cent (n = 33) of men were identified as having significant anomalies. Genetic abnormalities were detected in 27 patients. Of these, 24 men had CF mutations, while the remaining 3 men had karyotypic abnormalities. Other pathologies discovered were testicular cancer (n = 1), prostate cancer (n = 10), diabetes mellitus (n = 3) and hypothyroidism (n = 1). Some doubt the usefulness of male infertility evaluations because good reproductive outcomes can be achieved even without this evaluation and testing. This practice may lead to significant underlying medical problems or genetic abnormalities being overlooked. Unfortunately, bypassing male factor infertility evaluations and going straight to ART will not provide the exact aetiology of infertility. As a result, appropriate management is not offered to these infertile men.
Genetic testing is fundamental for clinical decision-making in the treatment of infertile men. It can spare one from unnecessary medical or surgical treatment [61]. However, there is a lack of national and international rules for the genetic approach to evaluate infertile couples [36]. According to the available guidelines on male infertility, karyotyping and Y chromosome microdeletion are requested if there is azoospermia or severe oligozoospermia [sperm count <5 million/ ml [113] or <10 million/ml [23]]. Despite the availability and proper clinical use of the proven genetic assays for male factor infertility, these can diagnose only 20% of cases [114].
The widespread utilization of sperm chromosome aneuploidy testing has been impeded by the technical nature of the procedure and the cost associated with fluorescence in situ hybridization (FISH) probes [114]. In addition, these analysis techniques are available at a limited number of reference laboratories. Genetic testing remains an underutilized assay that might be beneficial for infertile men and their partners [115]. Because of the financial burden of genetic testing, Khurana et al. developed a nomogramme using sperm concentration and motility, serum testosterone level and testicular volume to predict the probability of advising genetic testing [116]. They also performed a cost analysis using this model. Utilization of this nomogramme missed 15.4% of genetic anomalies. Using the optimal cut-off value of 13.8%, a direct cost savings of 45% were observed.
In 2006, the Human Genetics section of World Health Organization (WHO) released the implications of genetic testing services in developing countries [117]. Some of the reasons they cited as preventing its full implementation and development were poverty, few trained health professionals, less priority from policy makers given to genetic services and cultural and religious factors. There is also a lack of epidemiological data from genetic diseases. Thong et al. reported on the challenges of medical genetics in developing low- and middle-income countries in the Asia Pacific regions [118]. Due to limited birth defects or rare disease registries in this region from a lack of accurate data on genetic conditions , the development of necessary genetic services is hampered [119].
Overall, the epidemiology of male infertility is a challenging study for well-described reasons. Winter et al. narrated the problems encountered in this type of study [120]. Male infertility is not a reportable disease, and the majority of individuals who undergo treatment are predominantly on an outpatient basis. Paying out of pocket and a lack of insurance coverage impede these infertile couples from seeking medical help for their problems. There is an underestimation of the outcomes based on the nature of men’s fecundity. The true statistical numbers have been weakly estimated in the available heterogeneous studies. A wide variety of influencing factors are hindering these studies to better characterize the true nature of male infertility and its global and regional incidence. These include race, country, geography and unique at-risk groups that are needed to arrive at the true value for this epidemiologic research.
Many infertile men are not being evaluated for infertility. This reflects a potential implication to reproductive goals and men’s health. Comprehensive male factor infertility evaluation is crucial because correct male evaluation and genetic testing can discover conditions that impose a threat to the health of these infertile men and their potential children.
Conclusion
The inability to father a child is a global health concern. Genetic disorders are more frequently seen in idiopathic infertile men with severe oligozoospermia and azoospermia. Careful screening of these patients and referrals to infertility specialists for long-term follow-up and surveillance are warranted. The percentage of each type of male infertility varies in different geographic populations and in different available bodies of literature. The prevalence and patterns of aetiologies of infertility are diverse in all societies worldwide. Genetic testing can identify specific genetic conditions that could be transferred to the offspring through ART and can impact the ability to acquire sperm by different sperm retrieval techniques. Further genetic studies will continue to advance our knowledge in the clinical and biological domains. However, some uncommon genetic causes have heterogeneous phenotypes, and a potential lack of symptoms specific for a particular disorder may hinder diagnosis and treatment. As we continue to discover more about the genetics of male infertility, we will arrive at a better evaluation and subsequent appropriate management of these men with poor reproductive potential. Large-scale, prospective, epidemiological studies may enhance our understanding of the genetic disorders of male infertility.
Review Criteria
An extensive search of studies examining the epidemiology of genetic disorders in male infertility was performed using search engines, such as ScienceDirect, OVID, Google Scholar, PubMed and MEDLINE. The overall strategy for study identification and data extraction was based on the following keywords: “epidemiology”, “male infertility”, “genetic abnormalities”, “chromosomal abnormalities”, “azoospermia”, “severe oligozoospermia”, “Klinefelter syndrome”, “Y chromosome microdeletions”, “47,XYY”, “46,XX”, “congenital bilateral absence of vas deferens”, “Kallmann syndrome”, “Robertsonian translocation”, “reciprocal translocation” and “inversion”. Articles published in languages other than English were not considered.
References
Zegers-Hochschild F, Adamson D, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on infertility and fertility care. Fertil Steril. 2017;108(3):393–406.
Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. Fertil Steril. 2002;77:873–82.
Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, al e. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod. 1991;6(6):811–6.
Olsen J, Küppers-Chinnow M, Spinelli A. Seeking medical help for subfecundity: a study based upon surveys in five European countries. Fertil Steril. 1996;66(1):95–100.
Bracke A, Peeters K, Punjabi U, Hoogewijs D, Dewilde S. A search for molecular mechanisms underlying male idiopathic infertility. Reprod Biomed Online. 2018;36(3):327–39. https://doi.org/10.1016/j.rbmo.2017.12.005. Epub 2017 Dec 27.
Krausz C. Male infertility: pathogenesis and clinical diagnosis. Best Pract Res Clin Endocrinol Metab. 2011;25(2):271–85. https://doi.org/10.1016/j.beem.2010.08.006.
Dohle GR, Halley DJ, Van Hemel JO, van den Ouwel AM, Pieters MH, et al. Genetic risk factors in infertile men with severe oligozoospermia and azoospermia. Hum Reprod. 2002;17(1):13–6.
Georgiou I, Syrrou M, Pardalidis N, Karakitsios K, Mantzavinos T, et al. Genetic and epigenetic risks of intracytoplasmic sperm injection method. Asian J Androl. 2006;8(6):643–73.
Povey AC, Stocks SJ. Epidemiology and trends in male subfertility. Hum Fertil (Camb). 2010;13(4):182–8. https://doi.org/10.3109/14647273.2010.515700.
Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22(6):1506–12. Epub 2007 Mar 21.
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356. https://doi.org/10.1371/journal.pmed.1001356. Epub 2012 Dec 18.
Eisenberg ML, Lathi RB, Baker VL, Westphal LM, Milki AA, Nangia AK. Frequency of the male infertility evaluation: data from the national survey of family growth. J Urol. 2013;189(3):1030–4. https://doi.org/10.1016/j.juro.2012.08.239. Epub 2012 Sep 23.
Agarwal A, Mulgund A, Hamada A, Chyatte MR. Unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:37. https://doi.org/10.1186/s12958-015-0032-1.
Ikechebelu JI, Adinma JI, Orie EF, Ikegwuonu SO. High prevalence of male infertility in southeastern Nigeria. J Obstet Gynaecol. 2003;23(6):657–9.
Philippov OS, Radionchenko AA, Bolotova VP, Voronovskaya NI, Potemkina TV. Estimation of the prevalence and causes of infertility in western Siberia. Bull World Health Organ. 1998;76(2):183–7.
Aflatoonian A, Seyedhassani SM, Tabibneijad N. The epidemiological and etiological aspects of infertility in Yazd province of Iran. Iran J Reprod Med. 2009;7(3):117–22.
Bablok L, Dziadecki W, Szymusik I, Wolczynski S, Kurzawa R, et al. Patterns of infertility in Poland - multicenter study. Neuro Endocrinol Lett. 2011;32(6):799–804.
Datta J, Palmer MJ, Tanton C, Gibson LJ, Jones KG, et al. Prevalence of infertility and help seeking among 15 000 women and men. Hum Reprod. 2016;31(9):2108–18. https://doi.org/10.1093/humrep/dew123. Epub 2016 Jun 30.
Bayasgalan G, Naranbat D, Tsedmaa B, Tsogmaa B, Sukhee D, et al. Clinical patterns and major causes of infertility in Mongolia. J Obstet Gynaecol Res. 2004;30(5):386–93.
Poongothai J, Gopenath TS, Manonayaki S. Genetics of human male infertility. Singap Med J. 2009;50(4):336–47.
Martinez G, Daniels K, Chandra A. Fertility of men and women aged 15-44 years in the United States: National Survey of Family Growth, 2006-2010. Natl Health Stat Rep. 2012;51:1–28.
Collins HP, Kalisch D. The health of Australia’s males. Health. Australian Institute of Health and Welfare: Canberra; 2011.
Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European association of urology guidelines on male infertility: the 2012 update. Eur Urol. 2012;62:324–32.
Barratt C, Bjorndahl L, De Jong C, Lamb D, Martini FO, et al. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance—challenges and future research opportunities. Hum Reprod Update. 2017;23(6):660–80.
Stouffs K, Seneca S, Lissens W. Genetic causes of male infertility. Ann Endocrinol (Paris). 2014;75(2):109–11. https://doi.org/10.1016/j.ando.2014.03.004. Epub 2014 Apr 24.
Krausz C, Escamilla AR, Chianese C. Genetics of male infertility: from research to clinic. Reproduction. 2015;150(5):R159–74. https://doi.org/10.1530/REP-15-0261.
Chandley AC. Chromosome anomalies and Y chromosome microdeletions as causal factors in male infertility. Hum Reprod. 1998;13(Suppl 1):45–50.
Samli H, Samli MM, Solak M, Imirzalioglu N. Genetic anomalies detected in patients with non-obstructive azoospermia and oligozoospermia. Arch Androl. 2006;52(4):263–7.
Wosnitzer M, Goldstein M, Hardy MP. Review of Azoospermia. Spermatogenesis. 2014;4:e28218. eCollection 2014.
Lee JY, Dada R, Sabanegh E, Carpi A, Agarwal A. Role of genetics in azoospermia. Urology. 2011;77(3):598–601. https://doi.org/10.1016/j.urology.2010.10.001. Epub 2010 Dec 31.
Palermo GD, Colombero LT, Hariprashad JJ, Schlegel PN, Rosenwaks Z. Chromosome analysis of epididymal and testicular sperm in azoospermic patients undergoing ICSI. Hum Reprod. 2002;17(3):570–5.
Mackic-Djurovic M, Hasic S, Kiseljakovic E, Rukavina D, Ibrulj S. Cytogenetic abnormalities found in patients with reproductive problems. Med Arch. 2017;71(6):396–9. https://doi.org/10.5455/medarh.2017.71.396-399.
Johnson MD. Genetic risks of intracytoplasmic sperm injection in the treatment of male infertility: recommendations for genetic counseling and screening. Fertil Steril. 1998;70(3):397–411.
Vincent MC, Daudin M, De MP, Massat G, Mieusset R, et al. Cytogenetic investigations of infertile men with low sperm counts: a 25-year experience. J Androl. 2002;23(1):18–22; discussion 44-5.
Nagvenkar P, Desai K, Hinduja I, Zaveri K. Chromosomal studies in infertile men with oligozoospermia & non-obstructive azoospermia. Indian J Med Res. 2005;122(1):34–42.
Riccaboni A, Lalatta F, Caliari I, Bonetti S, Somigliana E, Ragni G. Genetic screening in 2,710 infertile candidate couples for assisted reproductive techniques: results of application of Italian guidelines for the appropriate use of genetic tests. Fertil Steril. 2008;89(4):800–8. Epub 2007 Aug 6.
Mafra FA, Christofolini DM, Bianco B, Gava MM, Glina S, et al. Chromosomal and molecular abnormalities in a group of Brazilian infertile men with severe oligozoospermia or non-obstructive azoospermia attending an infertility service. Int Braz J Urol. 2011;37(2):244–50; discussion 250-1.
Arafa M, Majzoub A, AlSaid S, Ansari W, Al Ansari A, Elbardisi Y, Elbardisi H. Chromosomal abnormalities in infertile men with azoospermia and severe oligozoospermia in Qatar and their association with sperm retrieval intracytoplasmic sperm injection outcomes. Arab J Urol. 2018;16(1):132–9.
Punab M, Poolamets O, Paju P, Vihljajev V, Pomm K. et. al. Causes of male infertility: a 9-year prospective monocentre study on 1737 patients with reduced total sperm counts. Hum Reprod. 2017;32(1):18–31. Epub 2016 Nov 17.
Xie C, Chen X, Liu Y, Wu Z, Ping P. Multicenter study of genetic abnormalities associated with severe oligospermia and non-obstructive azoospermia. J Int Med Res. 2018;46(1):107–14. https://doi.org/10.1177/0300060517718771. Epub 2017 Jul 21.
Patel B, Parets S, Akana M, Kellogg G, Jansen M, et al. Comprehensive genetic testing for female and male infertility using next-generation sequencing. J Assist Reprod Genet. 2018;35(8):1489–96. https://doi.org/10.1007/s10815-018-1204-7. Epub 2018 May 19.
De Braekeleer M, Dao TN. Cytogenetic studies in male infertility: a review. Hum Reprod. 1991;6(2):245–50.
Pieters J, Kooper A, Feuth T, Smits A. Considering factors affecting the parental decision to abort after a prenatal diagnosis of a sex chromosome abnormality. Genet Med. 2012;14:558–9.
Forti G, Corona G, Vignozzi L, Krausz C, Maggi M. Klinefelter’s syndrome: a clinical and therapeutical update. Sex Dev. 2010;4(4–5):249–58. https://doi.org/10.1159/000316604. Epub 2010 Jul 21.
Sørensen K, Nielsen J, Jacobsen P, Rolle T. The 48,XXYY syndrome. J Ment Defic Res. 1978;22(3):197–205.
Kleczkowska A, Fryns JP, Van den Berghe H. X-chromosome polysomy in the male. The Leuven experience 1966-1987. Hum Genet. 1988;80(1):16–22.
Bojesen A, Juul S, Gravholt CH. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab. 2003;88(2):622–6.
Coffee B, Keith K, Albizua I, Malone T, Mowrey J, et al. Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. Am J Hum Genet. 2009;85(4):503–14. https://doi.org/10.1016/j.ajhg.2009.09.007.
Corona G, Pizzocaro A, Lanfranco F, Garolla A, Pelliccione F, et al. Sperm recovery and ICSI outcomes in Klinefelter syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2017;23(3):265–75. https://doi.org/10.1093/humupd/dmx008.
Krausz C, Hoefsloot L, Simoni M, Tüttelmann F, European Academy of Andrology; European Molecular Genetics Quality Network. EAA/EMQN best practice guidelines for molecular diagnosis of Y-chromosomal microdeletions: state-of-the-art 2013. Andrology. 2014;2(1):5–19. https://doi.org/10.1111/j.2047-2927.2013.00173.x.
Colaco S, Modi D. Genetics of the human Y chromosome and its association with male infertility. Reprod Biol Endocrinol. 2018;16(1):14. https://doi.org/10.1186/s12958-018-0330-5.
Yousefi-Razin E, Nasiri MJ, Omrani MD. Frequency of Y chromosome microdeletions among Iranian infertile men with Azoospermia and severe Oligozoospermia: a meta-analysis. J Reprod Infertil. 2016;17(4):208–12.
Johnson M, Raheem A, De Luca F, Hallerstrom M, Zainal Y, et al. An analysis of the frequency of Y-chromosome microdeletions and the determination of a threshold sperm concentration for genetic testing in infertile men. BJU Int. 2019;123(2):367–72. https://doi.org/10.1111/bju.14521. Epub 2018 Sep 9.
Chellat D, Rezgoune ML, McElreavey K, Kherouatou N, Benbouhadja S, et al. First study of microdeletions in the Y chromosome of Algerian infertile men with idiopathic oligo- or azoospermia. Urol Int. 2013;90(4):455–9. https://doi.org/10.1159/000347046. Epub 2013 Mar 16.
Kim MJ, Choi HW, Park SY, Song IO, Seo JT, Lee HS. Molecular and cytogenetic studies of 101 infertile men with microdeletions of Y chromosome in 1,306 infertile Korean men. J Assist Reprod Genet. 2012;29(6):539–46. https://doi.org/10.1007/s10815-012-9748-4. Epub 2012 Mar 29.
Rejeb I, M’rad R, Maazoul F, Trabelsi M, Ben Jemaa L, et al. Y chromosome microdeletions in Tunisian infertile males. Pathol Biol (Paris). 2008;56(3):111–5. Epub 2007 Nov 26.
Sen S, Pasi AR, Dada R, Shamsi MB, Modi D. Y chromosome microdeletions in infertile men: prevalence, phenotypes and screening markers for the Indian population. J Assist Reprod Genet. 2013;30(3):413–22. https://doi.org/10.1007/s10815-013-9933-0. Epub 2013 Jan 24.
Hinch AG, Altemose N, Noor N, Donnelly P, Myers SR. Recombination in the human Pseudoautosomal region PAR1. PLoS Genet. 2014;10(7):e1004503. https://doi.org/10.1371/journal.pgen.1004503. eCollection 2014 Jul.
Bansal SK, Jaiswal D, Gupta N, Singh K, Dada R, et al. Gr/gr deletions on Y-chromosome correlate with male infertility: an original study, meta-analyses, and trial sequential analyses. Sci Rep. 2016;6:19798. https://doi.org/10.1038/srep19798.
Liou TG, Rubenstein RC. Carrier screening, incidence of cystic fibrosis, and difficult decisions. JAMA. 2009;302(23):2595–6. https://doi.org/10.1001/jama.2009.1865.
Krausz C, Cioppi F, Riera-Escamilla A. Testing for genetic contributions to infertility: potential clinical impact. Expert Rev Mol Diagn. 2018;18(4):331–46. https://doi.org/10.1080/14737159.2018.1453358. Epub 2018 Mar 22.
Lissens W, Mercier B, Tournaye H, Bonduelle M, Férec C, et al. Cystic fibrosis and infertility caused by congenital bilateral absence of the vas deferens and related clinical entities. Hum Reprod. 1996;11(Suppl 4):55–78; discussion 79-80.
Ferlin A, Raicu F, Gatta V, Zuccarello D, Palka G, Foresta C. Male infertility: role of genetic background. Reprod Biomed Online. 2007;14(6):734–45.
Bareil C, Guittard C, Altieri JP, Templin C, Claustres M, des Georges M. Comprehensive and rapid genotyping of mutations and haplotypes in congenital bilateral absence of the vas deferens and other cystic fibrosis transmembrane conductance regulator-related disorders. J Mol Diagn. 2007;9(5):582–8.
Singh R, Hamada AJ, Bukavina L, Agarwal A. Physical deformities relevant to male infertility. Nat Rev Urol. 2012;9(3):156–74. https://doi.org/10.1038/nrurol.2012.11.
Estivill X, Bancells C, Ramos C. Geographic distribution and regional origin of 272 cystic fibrosis mutations in European populations. The Biomed CF Mutation Analysis Consortium. Hum Mutat. 1997;10(2):135–54.
Patrizio P, Leonard DG. Mutations of the cystic fibrosis gene and congenital absence of the vas deferens. Results Probl Cell Differ. 2000;28:175–86.
Kuligowska E, Fenlon HM. Transrectal US in male infertility: spectrum of findings and role in patient care. Radiology. 1998;207(1):173–81.
Shapiro E, Goldfarb DA, Ritchey ML. The congenital and acquired solitary kidney. Rev Urol. 2003;5:2–8.
Donohue RE, Fauver HE. Unilateral absence of the vas deferens. A useful clinical sign. JAMA. 1989;261(8):1180–2.
McCallum T, Milunsky J, Munarriz R, Carson R, Sadeghi-Nejad H, Oates R. Unilateral renal agenesis associated with congenital bilateral absence of the vas deferens: phenotypic findings and genetic considerations. Hum Reprod. 2001;16(2):282–8.
Jacobs PA, Melville M, Ratcliffe S, Keay AJ, Syme J. A cytogenetic survey of 11,680 newborn infants. Ann Hum Genet. 1974;37(4):359–76.
Kim IW, Khadilkar AC, Ko EY, Sabanegh ES Jr. 47,XYY Syndrome and Male Infertility. Rev Urol. 2013;15(4):188–96.
Children and young adults with sex chromosome aneuploidy-- follow-up, clinical and molecular studies. Minaki, Ontario, Canada, June 7-10, 1989. Birth Defects Orig Artic Ser. 1990;26(4):1–304.
Stochholm K, Juul S, Gravholt CH. Diagnosis and mortality in 47,XYY persons: a registry study. Orphanet J Rare Dis. 2010;5:15. https://doi.org/10.1186/1750-1172-5-15.
Borjian Boroujeni P, Sabbaghian M, Vosough Dizaji A, Zarei Moradi S, Almadani N, et al. Clinical aspects of infertile 47,XYY patients: a retrospective study. Hum Fertil (Camb). 2017:1–6. https://doi.org/10.1080/14647273.2017.1353143.
El-Dahtory F, Elsheikha HM. Male infertility related to an aberrant karyotype, 47,XYY: four case reports. Cases J. 2009;2(1):28. https://doi.org/10.1186/1757-1626-2-28.
de la Chapelle A. Nature and origin of males with XX sex chromosomes. Am J Hum Genet. 1972;24:71–105.
Rajender S, Rajani V, Gupta NJ, Chakravarty B, Singh L, Thangaraj K. SRY-negative 46,XX male with normal genitals, complete masculinization and infertility. Mol Hum Reprod. 2006;12:341–6. https://doi.org/10.1093/molehr/gal030.
Majzoub A, Arafa M, Starks C, Elbardisi H, Al Said S, Sabanegh E. 46 XX karyotype during male fertility evaluation; case series and literature review. Asian J Androl. 2017;19(2):168–72. https://doi.org/10.4103/1008-682X.181224.
Akinsal EC, Baydilli N, Demirtas A, Saatci C, Ekmekcioglu O. Ten cases with 46,XX testicular disorder of sex development: single center experience. Int Braz J Urol. 2017;43(4):770–5. https://doi.org/10.1590/S1677-5538.IBJU.2016.0505.
Mohammadpour Lashkari F, Totonchi M, Zamanian MR, Mansouri Z, Sadighi Gilani MA, et al. 46,XX males: a case series based on clinical and genetics evaluation. Andrologia. 2017;49(7) https://doi.org/10.1111/and.12710. Epub 2016 Nov 24.
Chen T, Tian L, Wu F, Xuan X, Ma G, et al. Clinical and genetic analysis in males with 46,XX disorders of sex development: a reproductive centre experience of 144 cases. Andrologia. 2019:e13232. https://doi.org/10.1111/and.13232.
Topaloglu AK, Kotan LD. Genetics of hypogonadotropic hypogonadism. Endocr Dev. 2016;29:36–49. https://doi.org/10.1159/000438841. Epub 2015 Dec 17.
Topaloğlu AK. Update on the genetics of idiopathic hypogonadotropic hypogonadism. J Clin Res Pediatr Endocrinol. 2017;9(Suppl 2):113–22. https://doi.org/10.4274/jcrpe.2017.S010. Epub 2017 Dec 27.
Boehm U, Bouloux PM, Dattani MT, de Roux N, Dodé C, et al. Expert consensus document: European consensus statement on congenital hypogonadotropic hypogonadism--pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2015;11(9):547–64. https://doi.org/10.1038/nrendo.2015.112. Epub 2015 Jul 21.
Fechner A, Fong S, McGovern P. A review of Kallmann syndrome: genetics, pathophysiology, and clinical management. Obstet Gynecol Surv. 2008;63(3):189–94. https://doi.org/10.1097/OGX.0b013e3181641278.
Abujbara MA, Hamamy HA, Jarrah NS, Shegem NS, Ajlouni KM. Clinical and inheritance profiles of Kallmann syndrome in Jordan. Reprod Health. 2004 Oct 24;1(1):5.
Layman LC. Genetics of human hypogonadotropic hypogonadism. Am J Med Genet. 1999;89(4):240–8.
Martin RH. Cytogenetic determinants of male fertility. Hum Reprod Update. 2008;14(4):379–90. https://doi.org/10.1093/humupd/dmn017. Epub 2008 Jun 4.
Mayeur A, Ahdad N, Hesters L, Brisset S, Romana S, et al. Chromosomal translocations and semen quality: a study on 144 male translocation carriers. Reprod Biomed Online. 2019;38(1):46–55. https://doi.org/10.1016/j.rbmo.2018.10.003. Epub 2018 Nov 13.
Antonelli A, Gandini L, Petrinelli P, Marcucci L, et al. Chromosomal alterations and male infertility. J Endocrinol Investig. 2000;23(10):677–83.
Mau-Holzmann UA. Somatic chromosomal abnormalities in infertile men and women. Cytogenet Genome Res. 2005;111(3–4):317–36.
García-Rodríguez A, Gosálvez J, Agarwal A, Roy R, Johnston S. DNA damage and repair in human reproductive cells. Int J Mol Sci. 2018;20(1). pii: E31) https://doi.org/10.3390/ijms20010031.
Kim SS, Jung SC, Kim HJ, Moon HR, Lee JS. Chromosome abnormalities in a referred population for suspected chromosomal aberrations: a report of 4117 cases. J Korean Med Sci. 1999;14(4):373–6.
Balasar Ö, Zamani AG, Balasar M, Acar H. Male infertility associated with de novo pericentric inversion of chromosome 1. Turk J Urol. 2017;43(4):560–2. https://doi.org/10.5152/tud.2017.79346. Epub 2017 Dec 1.
Teo SH, Tan M, Knight L, Yeo SH, Ng I. Pericentric inversion 9--incidence and clinical significance. Ann Acad Med Singap. 1995;24(2):302–4.
Cotter PD, Babu A, McCurdy LD, Caggana M, Willner JP, Desnick RJ. Homozygosity for pericentric inversions of chromosome 9. Prenatal diagnosis of two cases. Ann Genet. 1997;40(4):222–6.
Kirkpatrick G, Chow V, Ma S. Meiotic recombination, synapsis, meiotic inactivation and sperm aneuploidy in a chromosome 1 inversion carrier. Reprod Biomed Online. 2012;24(1):91–100. https://doi.org/10.1016/j.rbmo.2011.09.013. Epub 2011 Oct 7.
Gardner RJM, Sutherland GR. Chromosome abnormalities and genetic counseling. Am J Hum Genet. 1997;60(6):1567–8.
Cheong KF, Knight LA, Tan M, Ng IS. Variants of chromosome 9 in phenotypically normal individuals. Ann Acad Med Singap. 1997;26(3):312–4.
Ait-Allah A, Ming PM, Salem H, Reece A. The clinical importance of pericentric inversion of chromosome 9 in prenatal diagnosis. J Mat Fetal Invest. 1997;7:126–8.
Guttenbach M, Engel W, Schmid M. Analysis of structural and numerical chromosome abnormalities in sperm of normal men and carriers of constitutional chromosome aberrations. A review. Hum Genet. 1997;100(1):1–21.
Dana M, Stoian V. Association of pericentric inversion of chromosome 9 and infertility in romanian population. Maedica (Buchar). 2012;7(1):25–9.
Mozdarani H, Meybodi AM, Karimi H. Impact of pericentric inversion of Chromosome 9 [inv (9) (p11q12)] on infertility. Indian J Hum Genet. 2007;13(1):26–9. https://doi.org/10.4103/0971-6866.32031.
Al-Achkar W, Wafa A, Moassass F. Cytogenetic abnormalities and Y-chromosome microdeletions in infertile Syrian males. Biomed Rep. 2013;1(2):275–9. Epub 2012 Nov 21.
Sasagawa I, Ishigooka M, Kubota Y, Tomaru M, Hashimoto T, Nakada T. Pericentric inversion of chromosome 9 in infertile men. Int Urol Nephrol. 1998;30(2):203–7.
Foresta C, Ferlin A, Gianaroli L, Dallapiccola B. Guidelines for the appropriate use of genetic tests in infertile couples. Eur J Hum Genet. 2002;10(5):303–12.
Okutman O, Rhouma MB, Benkhalifa M, Muller J, Viville S. Genetic evaluation of patients with non-syndromic male infertility. J Assist Reprod Genet. 2018;35(11):1939–51. https://doi.org/10.1007/s10815-018-1301-7. Epub 2018 Sep 26.
Van Steirteghem A, Bonduelle M, Devroey P, Liebaers I. Follow-up of children born after ICSI. Hum Reprod Update. 2002;8(2):111–6.
Honig SC, Lipshultz LI, Jarow J. Significant medical pathology uncovered by a comprehensive male infertility evaluation. Fertil Steril. 1994;62(5):1028–34.
Kolettis PN, Sabanegh ES. Significant medical pathology discovered during a male infertility evaluation. J Urol. 2001;166(1):178–80.
Jarow J, Sigman M, Kolettis PN, et al. The optimal evaluation of the infertile male: best practice statement reviewed and validity confirmed 2011. Available online: https://www.auanet.org/education/guidelines/male-infertility-d.cfm
Hotaling J, Carrell DT. Clinical genetic testing for male factor infertility: current applications and future directions. Andrology. 2014;2(3):339–50. https://doi.org/10.1111/j.2047-2927.2014.00200.x. Epub 2014 Apr 7.
Carrell DT, Emery BR. Use of automated imaging and analysis technology for the detection of aneuploidy in human sperm. Fertil Steril. 2008;90(2):434–7. Epub 2007 Oct 23.
Khurana KK, Baker K, Gao T, Sabanegh ES Jr. The economic burden of genetic tests for the infertile male: a pilot algorithm to improve test predictive value. J Urol. 2014;191(4):1066–71. https://doi.org/10.1016/j.juro.2013.10.069. Epub 2013 Oct 23.
Ballantyne A, Goold I, Pearn A, WHO Human Genetics Programme. Medical genetic services in developing countries : the ethical, legal and social implications of genetic testing and screening. Geneva: World Health Organization; 2006. http://www.who.int/iris/handle/10665/43288
Thong MK, See-Toh Y, Hassan J, Ali J. Medical genetics in developing countries in the Asia-Pacific region: challenges and opportunities. Genet Med. 2018;20(10):1114–21. https://doi.org/10.1038/s41436-018-0135-0. Epub 2018 Aug 10.
Thong MK. Birth defects registries in the genomics era: challenges and opportunities for developing countries. Front Pediatr. 2014;2(60) https://doi.org/10.3389/fped.2014.00060.eCollection2014.
Winters BR, Walsh TJ. The epidemiology of male infertility. Urol Clin North Am. 2014;41(1):195–204. https://doi.org/10.1016/j.ucl.2013.08.006. Epub 2013 Sep 13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Martinez, M.P., Elbardisi, H., Majzoub, A., Arafa, M. (2020). Epidemiology of Genetic Disorders in Male Infertility. In: Arafa, M., Elbardisi, H., Majzoub, A., Agarwal, A. (eds) Genetics of Male Infertility. Springer, Cham. https://doi.org/10.1007/978-3-030-37972-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-37972-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37971-1
Online ISBN: 978-3-030-37972-8
eBook Packages: MedicineMedicine (R0)