Abstract
Mechanical ventilation is a life-support system used in many environments, including the emergency department, operating room, and intensive care unit (ICU). The monitoring of respiratory mechanics has received much attention recently. In this context, tidal volume, respiratory rate and respiratory system plateau (P plat) and driving (ΔP) pressures are the ventilator variables classically assessed and reported in clinical trials. However, when analyzed separately, they are not associated with inhospital mortality in patients without the acute respiratory distress syndrome (ARDS). On the other hand, mechanical power, which represents the amount of energy transferred from the mechanical ventilator to the respiratory system over time, is demonstrably associated with inhospital mortality. Mechanical power is calculated by the combination of tidal volume, respiratory rate, P plat, and ΔP. Recent advances have been made in the calculation of mechanical power, not only in volume-controlled but also in pressure-controlled ventilation, in critically ill patients. These advances rely on the computation of the elastic and resistive components of mechanical power, as well as on the computation of mechanical power during assisted breaths. In this chapter, we list ten reasons why mechanical power should be monitored as a tool to guide ventilator strategies in patients without ARDS. We believe that the development of algorithms for embedding in mechanical ventilators and the provision of real-time information on mechanical power could help physicians better guide their ventilator strategies in patients without ARDS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Critical ill patients
- Respiratory system mechanics
- Ventilator-induced lung injury
- Mechanical power
- Inhospital mortality
1 Introduction
Mechanical ventilation is frequently used in patients without acute respiratory distress syndrome (ARDS): during surgery, in the intensive care unit (ICU; e.g., to support breathing in respiratory and neurological failure), and for artificial respiration in cardiac arrest. Even though mechanical ventilation is a life-saving strategy, it may cause ventilator-induced lung injury (VILI) . Analyses of the main factors involved in VILI have focused on separate evaluation of static parameters—such as tidal volume; peak (P peak), plateau (P plat), and driving (ΔP) pressures; and positive end-expiratory pressure (PEEP)—and of dynamic ones—airflow, inspiratory time, and respiratory rate. However, in the real-world setting, these factors interact with each other. Thus, combining these factors into a single parameter—the “mechanical power ” imparted to the lung by the ventilator—may be a more suitable strategy for both research and clinical purposes.
Although early implementation of protective ventilation in patients without ARDS has been associated with better prognosis [1], optimization of mechanical ventilation settings is considered less important in daily clinical practice. In this chapter, we will discuss ten questions regarding the importance of the sole single ventilator parameter that has been associated with mortality in patients without ARDS: mechanical power . This parameter will then be discussed, focusing on the use of different formulas for its calculation and on the evidence of its impact on lung damage from preclinical and clinical studies.
2 Is Tidal Volume Associated with Mortality in Patients Without ARDS? No
The tidal volumes that are used in mechanically ventilated patients without ARDS have progressively been decreasing; however, the evidence for benefits of low tidal volumes remains scarce. A systematic review evaluated the change in tidal volume during a 39-year period (from 1975 to 2014) [2] and showed that tidal volumes have decreased significantly in the ICU (annual decrease of 0.16 ml/kg) and in the operating room (annual decrease of 0.09 ml/kg). In the PReVENT study [1], tidal volume was around 8 ml/kg predicted body weight (PBW) and did not differ between surviving patients and those who died. In a secondary analysis of the PRoVENT, tidal volume was not identified as a potential parameter associated with survival in patients without ARDS [3], which could be attributed to the fact that most patients were protectively ventilated. In the PReVENT trial, low tidal volume and intermediate tidal volume strategies were compared in patients without ARDS, focusing on the number of ventilator-free days and mortality rate at 28 days [1]. The low-tidal-volume group started at 6 ml/kg PBW, with decrements of 1 ml/kg PBW every hour to a minimum of 4 ml/kg PBW, whereas the intermediate-tidal-volume group started at 10 ml/kg PBW. P plat was maintained at less than 25 cmH2O; if it exceeded this threshold, tidal volume was progressively reduced by 1 ml/kg PBW. Ventilator-free days and mortality rate at 28 days did not differ between the low-tidal-volume (mean = 7.3 ml/kg PBW) and intermediate-tidal-volume (mean = 9.1 ml/kg PBW) groups. The intermediate-tidal-volume group showed higher P plat and ΔP in the first 3 days of the study, but still within a protective range for patients without ARDS. Additionally, use of the low-tidal-volume strategy was associated with CO2 retention and respiratory acidosis, perhaps related to less efficient alveolar ventilation. Furthermore, the use of oversedation to maintain low tidal volume may be associated with increased delirium, ventilator asynchrony, and the possibility of effort-induced lung injury. To date, there are no clinical trial data showing benefit or harm of low-tidal-volume ventilation in patients without ARDS. Since ARDS is only very rarely recognized at its onset, the safest approach is to use protective ventilation with tidal volume <8 ml/kg PBW.
3 Is Driving Pressure Associated with Mortality in Patients Without ARDS? No
The driving pressure of the respiratory system (ΔP,RS) can be easily calculated at the bedside as P plat minus pressure at end-expiratory occlusion (PEEP + intrinsic PEEP). The ΔP,RS represents the tidal volume normalized by the respiratory system compliance. Since the compliance of the respiratory system is proportional to the volume of aerated lung, ΔP,RS is the tidal volume corrected for the end-expiratory lung volume, thus estimating the strain during tidal breath. In other words, if tidal volume remains constant, if the compliance of the respiratory system is low, the ΔP,RS will proportionally increase; conversely, if the compliance of the respiratory system is high, the ΔP,RS will proportionally decrease. Furthermore, under constant respiratory system compliance, ΔP,RS will increase at higher tidal volumes. Finally, ΔP,RS might be affected by the effects of PEEP on non-aerated lung areas. At a constant tidal volume, if PEEP increases lung volume by recruitment of previously collapsed alveoli, ΔP,RS will decrease; if PEEP increases lung volume by overdistension of previously aerated alveoli, ΔP,RS will increase. In patients without ARDS, the lung volume at end-expiration and the compliance of the respiratory system are either within normal ranges or moderately reduced, and low PEEP levels are usually applied, thus avoiding alveolar overdistension. In a retrospective study, ΔP,RS on day 1 was not associated with hospital mortality in patients without ARDS [4]. A secondary analysis of the PRoVENT trial [3] showed no association between ΔP,RS (≤12 vs. >12 cmH2O) and hospital mortality. However, caution is warranted, given the relatively small sample size of the study. Therefore, to date there is no indication to guide ventilatory strategy on the basis of ΔP,RS alone in patients without ARDS.
4 Is P peak Associated with Mortality in Patients Without ARDS? Yes
P peak is determined by the inspiratory flow and the position where pressure is measured along the respiratory circuit. In fact, it represents the total pressure gradient, at a fixed flow, to overcome the elastic, resistive, and viscoelastic properties of the respiratory system, the artificial airways, and the ventilator circuit. P peak is one of the easiest respiratory variables to monitor at the bedside during mechanical ventilation. In patients with increased airway resistance, under volume-controlled ventilation, after occluding the airways at end-inspiration, the difference between P peak and P plat represents the resistive properties (patient and ventilator circuit), whereas during pressure-controlled ventilation, P peak is close to P plat, since flow at expiration is almost zero. In patients without increased airway resistance and/or ventilator circuit obstruction, P peak is approximately equal to P plat. A secondary analysis of PRoVENT reported a significant association between P peak > 18 cmH2O and inhospital mortality in patients without ARDS [3]. In conclusion, we suggest using a P peak pressure < 30 cmH2O and a P plat < 25 cmH2O in mechanically ventilated patients without ARDS in volume- and pressure-controlled ventilation.
5 Is PEEP Associated with Mortality in Patients Without ARDS? Yes
PEEP has been proposed to prevent or at least minimize atelectrauma during controlled mechanical ventilation. However, PEEP can also lead to lung injury due to overdistension (so-called volutrauma) and impair right ventricular function and hemodynamics. In a systematic review [5] of preclinical studies in small and large mammals, “high PEEP” (versus lower PEEP) or “PEEP” (versus no PEEP) was associated with improved respiratory system compliance and better oxygenation. However, “high PEEP” and “PEEP” were also associated with occurrence of hypotension, a reduction in cardiac output or development of hyperlactatemia, with no differences in mortality. Based on the findings of this systematic review in experimental settings, it is uncertain whether PEEP at any level truly prevents lung injury, and most trials suggested potential harmful effects on the systemic circulation. Patients without ARDS who have less atelectasis and better compliance of the respiratory system seem to have a better balance between benefit and harm in favor of lower PEEP levels. Nevertheless, whether higher PEEP levels can be associated with clinical improvement over time is unknown. A meta-analysis of clinical trials [6] compared lower (2.0 ± 2.8 cmH2O) vs. higher (9.7 ± 4.0 cmH2O) levels of PEEP and found no benefits in terms of mortality and duration of invasive ventilation in surgical or medical ICU patients. In addition, pooling all data in a recent cohort [3] of patients without ARDS, high PEEP levels (>5 cmH2O) were associated with higher hospital mortality. A prospective randomized controlled trial in patients without ARDS to test the effects of low PEEP (lowest possible PEEP between 0 and 5 cmH2O) and high PEEP (PEEP of 8 cmH2O) on the number of ventilator-free days and survival at day 28 is ongoing [7]. To date, the evidence suggests that PEEP should not exceed 5 cmH2O in patients without ARDS.
6 Is Respiratory Rate Associated with Mortality in Patients Without ARDS? No
Respiratory rate is one of the easiest variables to measure at the bedside. It may be controlled by the ventilator, by the patient, or both. Usually, respiratory rate is set to keep an adequate level of arterial partial pressure of carbon dioxide (PaCO2) and arterial pH. Experimental studies have shown that increased respiratory rate may be associated with VILI [8, 9]. From a physiological standpoint, the respiratory rate can reflect the number of cycles of injured stress and strain in the lung parenchyma. In the PReVENT trial [1], respiratory rate was higher in volume-controlled compared to pressure-support ventilation groups, regardless of tidal volume. Conversely, PaCO2 was higher in the low-tidal-volume compared to intermediate-tidal-volume group during volume-controlled ventilation, but not in pressure-support ventilation, suggesting that the increased spontaneous breathing decreased the dead space, thus improving gas exchange. In conclusion, we suggest using assisted mechanical ventilation modes in patients without ARDS, thus allowing selection of an appropriate respiratory rate for the patient.
7 Mechanical Energy and Power Calculations: Should We Abandon More Complex Formulas in Favor of Simplified Ones? Yes
The contribution of the energy and power applied to the lung parenchyma during mechanical ventilation, resulting in VILI, is known as ergotrauma . Work is force × distance and, in the case of the lungs, since pressure is force/area and volume is length × area, the product of pressure and volume is force × length, which is the work done during lung inflation. Work of breathing and energy are expressed in the same unit (J). Energy has been calculated as tidal volume (ml) × ΔP (cmH2O), which gives a unit of ml/cmH2O. (To convert from ml/cmH2O to joules, all variables should be transformed to SI units.) Power is the rate of energy expenditure (Energy × Respiratory rate) [10, 11].
Different equations are available to calculate mechanical power . Since resistive properties are included, it should be mentioned that mechanical power calculation depends on the site of airway pressure measurement, i.e., whether at the end of the tracheal tube or at a transducer within the mechanical ventilator. In the first condition, only the resistance of the endotracheal tube is added to the airway resistance of the patient, while in the second condition, the total resistance encompasses the whole of the mechanical ventilator circuit, including the endotracheal tube. To correctly calculate mechanical power, the resistances of both the tracheal tube and mechanical ventilator should be subtracted or otherwise accounted for.
The complex equation initially described by Gattinoni et al. [12] is:
where 0.098 is the conversion factor for units, E rs is the respiratory system elastance, I:E is the ratio between inspiratory and expiratory time, and R aw is the airway resistance.
One important benefit of using this more complex formula is that it enables quantification of the relative contribution of each component (tidal volume, respiratory rate, ΔP,RS, PEEP, I:E, and airflow). This has been done previously by changing one parameter at a time and observing the overall effect on mechanical power [12]. Therefore, this formula takes into account the resistive properties and PEEP (and, consequently, lung volume changes caused by PEEP). The main disadvantages of this formula are that it is laborious to calculate and may be conditioned to perfect calibration of the mechanical ventilator, since more variables are used to calculate the mechanical power.
Furthermore, there are controversies regarding the computation of mechanical energy in a static condition, since there is no cyclic movement of the respiratory system after sole application of PEEP [10]. Therefore, when PEEP is included and lung volume is changed by PEEP application, both the static and dynamic components of mechanical energy should be calculated.
The static component of mechanical energy , which takes into account elastic mechanical power (MPELAST) , can be calculated using the following formula:
The dynamic component of mechanical energy , which takes into account resistive mechanical power (MPRES) , can be calculated using the following formula:
The simplest formula, which includes both elastic and resistive properties and is intended for use in critically ill patients [13], is composed of tidal volume, P peak, respiratory rate, and ΔP [12]:
Serpa Neto et al. [13] tested the hypothesis that mechanical power would be independently associated with patient-centered outcomes in mechanically ventilated critically ill patients for 48 h. This study was performed in two large cohorts of ICU patients whose data were prospectively collected in two databases. Mechanical power was independently associated with higher inhospital mortality, higher ICU mortality, fewer ventilator-free days, and longer ICU and hospital stays. One of the most important findings of this post hoc analysis was that, even at low tidal volume and low ΔP,RS, high mechanical power was associated with worse outcomes in critically ill patients. The combination of potential respiratory variables related to lung injury into a single parameter, instead of using only one respiratory variable, may have high predictive value for worse outcomes in the critically ill.
The concept of intensity, which is the distribution of mechanical power per unit of lung surface area [11, 14] or static compliance of the respiratory system (C,RS = Tidal volume/ΔP,RS), has also been proposed.
For the aforementioned formula, intensity (J/min) is given as = 0.098 × Tidal volume × Respiratory rate × (P peak − ½ × ΔP,RS)/Tidal volume/ΔP,RS.
If PEEP and resistive properties are added to the mechanical power formula, the intensity would be stated as:
A recent study investigated whether mechanical power normalized for predicted body weight (norMP) could be a better marker of mortality compared to other ventilator variables [15]. NorMP (AUC = 0.751) showed good predictive value for mortality compared to non-normalized mechanical power (AUC = 0.747). Mechanical power normalized by respiratory system compliance (a surrogate of intensity) was an even better predictor of mortality (AUC = 0.753).
8 Does Use of a Simple Formula Enable Calculation of Mechanical Power in Volume-Controlled Ventilation? Yes: Simply Change the Variables and Observe the Consequences
Usually, changing a single respiratory variable may not promote lung protection if this change is not followed by significant changes in lung mechanics [16]. This phenomenon can be observed in different clinical scenarios. However, calculation of mechanical power using the simplest formula, which takes into account tidal volume, respiratory rate, P peak, and ΔP,RS, can help understand why lung protection may not occur after changing only one respiratory variable.
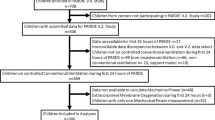
The effects of different tidal volumes on mechanical power during volume-controlled ventilation have been simulated in a hypothetical patient with a PBW equal to 64 kg (the average body weight reported in patients without ARDS) [3]. The inspiratory:expiratory ratio was kept constant at 1:2. Three different respiratory system compliance values—0.02 l/cmH2O (low), 0.04 l/cmH2O (intermediate), and 0.06 l/cmH2O (high)—were tested, with tidal volume reduced from 10 to 6 ml/kg PBW, total minute ventilation kept constant (9.6 l/min), and PEEP = 5 cmH2O. To maintain minute ventilation constant, respiratory rate was increased from 15 to 25 bpm. As shown in Fig. 3.1, together with the increment in respiratory rate from 15 to 25 bpm, a decrease in inspiratory time (from 1.3 to 0.8 s) is expected, as well as a concomitant increase in airflow (from 0.36 to 0.59 l/s), which would increase the resistive pressure. Considering a patient with constant airway resistance (4 cmH2O/l/s), the increase in airflow would increase the resistive pressure to approximately 1.5 cmH2O, which would have an impact on P peak. Reduction in tidal volume was associated with lower mechanical power in all conditions. Furthermore, the percentage of decrease in mechanical power after the reduction in tidal volume was greater at low compared to intermediate or higher compliances of the respiratory system (19% vs. 11% vs. 9%, respectively). This suggests that the effects of tidal volume reduction on mechanical power are greater at low respiratory system compliance.
Simulation of the effects of mechanical power (MP) during volume-controlled mechanical ventilation in a patient with a predicted body weight of 64 kg (the average body weight of patients without ARDS). Inspiratory:expiratory ratio kept constant at 1:2. Three different respiratory system compliance (C RS) values—0.02 l/cmH2O (low), 0.04 l/cmH2O (intermediate), and 0.06 l/cmH2O (high)—were tested, with tidal volume (V T) reductions from 10 ml/kg predicted body weight (PBW) to 6 ml/kg PBW, while keeping total minute ventilation (V E) constant (9.6 l/min) at positive end-expiratory pressure (PEEP) = 5 cmH2O. To maintain constant minute ventilation, respiratory rate (RR) was increased from 15 to 25 bpm. A decrease in inspiratory time (from 1.3 to 0.8 s) and concomitant increase in airflow (from 0.36 to 0.59 l/s) are expected to follow, increasing the resistive pressure. Assuming a patient with constant airway resistance (4 cmH2O/l/s), the increase in airflow would increase the resistive pressure by about 1.5 cmH2O, with an impact in P peak (one of the components of the mechanical power calculation). Reductions in V T were associated with lower mechanical power in all conditions. Furthermore, the percent decrease in mechanical power after the reduction in V T was greater at low compared to intermediate or higher respiratory system compliances (19% vs. 11% vs. 9%, respectively)
Becher et al. [17], in a retrospective analysis of two previous studies, proposed two power equations for pressure-controlled ventilation (MPPCV): a simplified formula,
and a comprehensive equation,
where R is resistance and C is compliance. Both formulas were compared to reference values obtained through integration of pressure-volume loops from the mechanical ventilator. The authors found that the simplified equation estimated mechanical power for pressure-controlled ventilation with a small bias, which resulted from not taking T slope into account. On the other hand, the comprehensive equation was able to correct this bias, but requires knowledge of T slope, resistance, and compliance. The formula proposed by Becher et al. was tested in a recent small validation study by van der Meijden et al. [18], in which the authors proposed a different equation:
These authors found that, for higher mechanical power values, the method proposed by Becher et al. [17] was somewhat inaccurate, although testing in larger samples was still warranted. Meanwhile, Becher et al. tested the equation proposed by van der Meijden et al. using a dataset of 301 pressure-volume loops obtained from 42 patients [19]. The authors found that on average, the equation proposed by van der Meijden et al. led to underestimation of mechanical power, with a bias of −0.56 J/min and a correlation coefficient of r 2 = 0.937, which is inferior to both the “simplified” and “comprehensive” equations originally proposed by Becher et al. (r 2 = 0.981 and r 2 = 0.985, respectively). In addition, the difference could be related to the assumption that, during pressure-controlled ventilation, end-inspiratory flow and pressure rise time are zero. In those respiratory cycles with end-inspiratory flow above zero, the formula will thus lead to underestimation of mechanical power, while pressure rise times above zero will lead to overestimation of mechanical power. The exchange of letters between these two groups of authors, with equation proposals and reanalysis of a larger dataset, is a step towards better understanding of mechanical power calculation during pressure-controlled ventilation [20].
9 Can Mechanical Power Be Computed During Assisted Ventilation? Yes
Mechanical energy and power, by definition, represent the total energy transferred from the mechanical ventilator in association with the respiratory muscles. To date, clinical studies have focused on relaxed respiratory muscles; therefore, only the mechanical power provided by the ventilator is computed [12, 21]. Nevertheless, the mechanical power generated by the respiratory muscles was calculated using an esophageal catheter in two pediatric studies [22, 23]. In an experimental study, mechanical power was calculated during pressure-support ventilation in rats. However, the authors chose to calculate only the portion attributable to the mechanical ventilator, which was reduced in pressure-support ventilation compared to pressure-controlled ventilation [24]. The calculation of lung mechanical power was done using the trapezoidal rule, as the integral of the inspiratory transpulmonary pressure versus the inspired tidal volume curve by numeric integration. A similar calculation was done in controlled mechanical ventilation [12].
There are further challenges to be overcome regarding calculation of respiratory system mechanical power during spontaneous breathing : (1) adjustment for chest wall movement; (2) distribution of mechanical power across the lung surface, which may not follow the same distribution determined by lung inhomogeneity [10]; and (3) the proper contribution of respiratory muscle activity to overall mechanical power under assisted mechanical ventilation.
10 Is Mechanical Power Associated with Lung Injury in Experimental Models? Yes
Recent studies have described the impact of mechanical power on VILI [25, 26, 29, 30]. In one such investigation, lung edema was observed when transpulmonary mechanical power was higher than 12.1 J/min [25]. Several analyses have been done to evaluate the relative contribution of tidal volume and respiratory rate to mechanical power [12]. An experimental study [26] investigated the impact of high and low mechanical power, obtained as combinations of low and high tidal volume and respiratory rate, on VILI. Mechanical power was calculated using different formulas [12, 27, 28]. Even when combined with high tidal volume, low mechanical power resulted in greater lung damage, thus suggesting the importance of using protective low tidal volume in ARDS [26]. PEEP is also an important parameter to calculate mechanical power. In this line, Collino et al. investigated the effects of increasing PEEP values on mechanical power in healthy lungs [30]. For this purpose, piglets were ventilated by a tidal volume (14.9 ml/kg) similar to functional residual capacity (FRC), which gives an overall strain close to 1, and increasing levels of PEEP were tested (0, 4, 7, 11, 14, and 18 cmH2O) for 50 h. Mechanical power was calculated by the formula proposed by Gattinoni et al. [12], which takes into account the PEEP × ΔV related to PEEP.
The authors showed that mechanical power was constant from 0 up to 7 cmH2O, which could be reflected by improvement of lung elastance within this range. On the other hand, increasing PEEP from 7 up to 18 cmH2O was associated with greater damage and relevant hemodynamic instability. This experimental study emphasizes that PEEP may be a major determining factor of damage in certain settings, while in others, the driving pressure, respiratory rate, and tidal volume may be more important. More recently, Felix et al. [31] tested the hypothesis that the impact of an abrupt increase in tidal volume would be attenuated if tidal volume were increased slowly enough to reduce alveolar mechanical heterogeneity and VILI. Although the primary focus was not related to mechanical power itself, the authors showed that extending the adaptation period increased cumulative power and induced VILI, since animals were exposed to injurious strain earlier and for a longer time [32]. Therefore, the rapid recognition of high mechanical power mitigates lung damage.
11 Is Mechanical Power Associated with Mortality in Patients Without ARDS? Yes
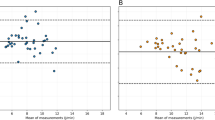
In their dual-dataset study , Serpa Neto et al. [13] observed an association between increased risk of death and mechanical power higher than 17.0 J/min (Fig. 3.2). The most important result of this post hoc analysis was that even at low tidal volume and low ΔP, high mechanical power was associated with fewer ventilator-free days, longer ICU stays, and higher inhospital mortality. Similar findings were found in a secondary analysis of 1705 mechanically ventilated patients without ARDS [33]. By using the same formula described by Serpa Neto et al. [13], the authors found that ΔP, P plat, and mechanical power were associated with inhospital mortality.
Mechanical power tolerance. For anesthesia in a patient with normal lungs, the reported values are within very low limits, around 12 J/min. In critically ill patients without acute respiratory distress syndrome (non-ARDS), the threshold value of mechanical power to prevent ARDS is <17 J/min. In ARDS, regardless of severity, values are higher than in non-ARDS. For mild, moderate, and severe ARDS, the tolerated values are 22, 24, and 27 J/min. If mechanical power exceeds 27 J/min, extracorporeal membrane oxygenation (ECMO) should be considered
12 Conclusion
In patients without ARDS, ventilatory management has been associated with mortality. Commonly targeted ventilator parameters, such as tidal volume and ΔP, are not associated with mortality in patients without ARDS, while respiratory rate—which has been comparatively neglected in clinical trials—is gaining attention. Mechanical power, which pools these variables to reflect the amount of energy transferred from the mechanical ventilator to the lung parenchyma over time, can be easily calculated at the bedside. Experimental and clinical data show it is associated with VILI and outcomes. In short, mechanical power might be considered as a potential tool to optimize ventilation settings in patients without ARDS and should be validated for this purpose in prospective observational and interventional studies.
References
Simonis FD, Serpa Neto A, Binnekade JM, et al. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial. JAMA. 2018;320:1872–80.
Schaefer MS, Serpa Neto A, Pelosi P, et al. Temporal changes in ventilator settings in patients with uninjured lungs: a systematic review. Anesth Analg. 2019;129:129–40.
Simonis FD, Barbas CSV, Artigas-Raventos A, et al. Potentially modifiable respiratory variables contributing to outcome in ICU patients without ARDS: a secondary analysis of PRoVENT. Ann Intensive Care. 2018;8:39.
Schmidt MFS, Amaral A, Fan E, et al. Driving pressure and hospital mortality in patients without ARDS: a cohort study. Chest. 2018;153:46–54.
Algera AG, Pisani L, Chaves RCF, et al. Effects of PEEP on lung injury, pulmonary function, systemic circulation and mortality in animals with uninjured lungs-a systematic review. Ann Transl Med. 2018;6:25.
Serpa Neto A, Filho RR, Cherpanath T, et al. Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: a systematic review and meta-analysis of randomized controlled trials. Ann Intensive Care. 2016;6:109.
Algera AG, Pisani L, Bergmans DCJ, et al. RELAx—REstricted versus Liberal positive end-expiratory pressure in patients without ARDS: protocol for a randomized controlled trial. Trials. 2018;19:272.
Vaporidi K, Voloudakis G, Priniannakis G, et al. Effects of respiratory rate on ventilator-induced lung injury at a constant PaCO2 in a mouse model of normal lung. Crit Care Med. 2008;36:1277–83.
Grasso S, Stripoli T, Mazzone P, et al. Low respiratory rate plus minimally invasive extracorporeal CO2 removal decreases systemic and pulmonary inflammatory mediators in experimental acute respiratory distress syndrome. Crit Care Med. 2014;42:e451–60.
Huhle R, Serpa Neto A, Schultz MJ, et al. Is mechanical power the final word on ventilator-induced lung injury?—no. Ann Transl Med. 2018;6:394.
Silva PL, Ball L, Rocco PRM, Pelosi P. Power to mechanical power to minimize ventilator-induced lung injury? Intensive Care Med Exp. 2019;7(Suppl 1):38.
Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42:1567–75.
Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44:1914–22.
Guldner A, Braune A, Ball L, et al. The authors reply. Crit Care Med. 2017;45:e328–e9.
Zhang Z, Zheng B, Liu N, et al. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45:856–64.
Gattinoni L, Tonetti T, Quintel M. Intensive care medicine in 2050: ventilator-induced lung injury. Intensive Care Med. 2018;44:76–8.
Becher T, van der Staay M, Schadler D, Frerichs I, Weiler N. Calculation of mechanical power for pressure-controlled ventilation. Intensive Care Med. 2019;45:1321–3.
van der Meijden S, Molenaar M, Somhorst P, Schoe A. Calculating mechanical power for pressure-controlled ventilation. Intensive Care Med. 2019;45:1495–7.
Becher T, van der Staay M. Calculation of mechanical power for pressure-controlled ventilation: author’s reply. Intensive Care Med. 2019;45:1498–9.
Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188:220–30.
van der Staay M, Chatburn RL. Advanced modes of mechanical ventilation and optimal targeting schemes. Intensive Care Med Exp. 2018;6:30.
Wolfson MR, Bhutani VK, Shaffer TH, Bowen FW Jr. Mechanics and energetics of breathing helium in infants with bronchopulmonary dysplasia. J Pediatr. 1984;104:752–7.
Kao LC, Durand DJ, Nickerson BG. Improving pulmonary function does not decrease oxygen consumption in infants with bronchopulmonary dysplasia. J Pediatr. 1988;112:616–21.
Magalhaes PAF, Padilha GA, Moraes L, et al. Effects of pressure support ventilation on ventilator-induced lung injury in mild acute respiratory distress syndrome depend on level of positive end-expiratory pressure: a randomised animal study. Eur J Anaesthesiol. 2018;35:298–306.
Cressoni M, Gotti M, Chiurazzi C, et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology. 2016;124:1100–8.
Santos RS, Maia LA, Oliveira MV, et al. Biologic impact of mechanical power at high and low tidal volumes in experimental mild acute respiratory distress syndrome. Anesthesiology. 2018;128:1193–206.
Guerin C, Papazian L, Reignier J, et al. Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials. Crit Care. 2016;20:384.
Marini JJ, Jaber S. Dynamic predictors of VILI risk: beyond the driving pressure. Intensive Care Med. 2016;42:1597–600.
Moraes L, Silva PL, Thompson A, et al. Impact of different tidal volume levels at low mechanical power on ventilator-induced lung injury in rats. Front Physiol. 2018;9:318.
Collino F, Rapetti F, Vasques F, et al. Positive end-expiratory pressure and mechanical power. Anesthesiology. 2019;130:119–30.
Felix NS, Samary CS, Cruz FF, et al. Gradually increasing tidal volume may mitigate experimental lung injury in rats. Anesthesiology. 2019;130:767–77.
Marini JJ. Evolving concepts for safer ventilation. Crit Care. 2019;23(Suppl 1):114.
Fuller BM, Page D, Stephens RJ, et al. Pulmonary mechanics and mortality in mechanically ventilated patients without acute respiratory distress syndrome: a cohort study. Shock. 2018;49:311–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Silva, P.L., Rocco, P.R.M., Pelosi, P. (2020). Ten Reasons to Use Mechanical Power to Guide Ventilator Settings in Patients Without ARDS. In: Vincent, JL. (eds) Annual Update in Intensive Care and Emergency Medicine 2020. Annual Update in Intensive Care and Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-37323-8_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-37323-8_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37322-1
Online ISBN: 978-3-030-37323-8
eBook Packages: MedicineMedicine (R0)