Abstract
When an athlete presents with acquired valve disease during pre-participation examination, this often leads to an intensive discussion among the medical staff. Up to now the knowledge of the influence of physical activity on the progression of valvular heart disease (VHD) and ventricular dysfunction is rare. The recommended type of activity (either isometric or dynamic) for a patient with VHD is crucial as it can influence the progression of valvular heart disease as well as ventricular function and the dimensions of heart chambers. Valve defects with a regurgitant component are often better tolerated than stenotic lesions. Dynamic exercise primarily causes increased volume load to the ventricle, whereas static exercise causes mainly a pressure load. Of course, all sports are a combination of these types of effort, but their proportion varies between disciplines. Following adequate clinical evaluation and symptomatic status, echocardiography is the key technique to confirm the diagnosis of VHD as well as to assess its severity and thus prognosis. Indices of left ventricular enlargement and function as well as pulmonary artery pressure are also strong prognostic factors. Transesophageal echocardiography and a stress test to evaluate functional capacity is also of utmost importance to find out if an individual can tolerate the level of exertion expected from the type of sport wished to be engaged in.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Valvular heart disease
- Mitral valve
- Aortic valve
- Pulmonary artery pressure
- Ventricular function
- Ejection fraction
- Echocardiography
-
1.
Learn how to diagnose different valve defects.
-
2.
Learn which diagnostic tool is needed to find the adequate diagnosis.
-
3.
Learn how sports activity influences the progression of VHD.
-
4.
Learn how sports activity influences pulmonary pressure and ventricular function.
-
5.
Learn which type of sports can be recommended in VHD individuals.
1 Introduction
The scope of this chapter is to provide an overview on the different types of VHD and to suggest a strategy how to diagnose them adequately. As the evaluation of the hemodynamic effects of competitive sport in individuals with VHD is challenging we describe the different consequences on cardiac function [1].
2 Aortic Valve Stenosis
The most common cause for aortic valve stenosis (AVS) is a rheumatic or congenital origin. Calcified degenerative stenosis is often associated with congenital abnormality of the aortic valve (e.g. bicuspid valve), especially when aortic stenosis is identified in young patients [2, 3]. Hemodynamic progression often shows marked individual variability and is not reflected by a single objective parameter.
Symptoms such as angina pectoris or dyspnea usually appear in a late stage of the disease. Occurrence of sudden cardiac death (SCD) is by far more probable if one of these symptoms is present. LA size can reflect hemodynamic burden in patients with asymptomatic severe aortic stenosis. Quantitative measurements of LA and diastolic function are helpful to evaluate left ventricular filling pressures with exercise and could be used to identify asymptomatic patients with increased hemodynamic burden [4].
-
Congenital bicuspid aortic valve (BAV), one of the most common congenital heart diseases (0.9–2%), can lead to both AVS and aortic valve regurgitation (AVR; see below). In these individuals LV dimensions of athletes are often near the upper limits of normal.
Evaluation. AVS is frequently detected by auscultation . Determination of the gradient and valve opening area is initially carried out by Doppler-echocardiography (Table 16.1). Exercise testing is recommended in certain cases to assess LV function, development of ST segment depression, blood pressure behavior and possible arrhythmias [5, 6]. The role of exercise testing to clarify symptom status and the use of stress imaging (e.g. stress echocardiography) to evaluate the dynamic component of valvular abnormalities and to unmask subclinical myocardial dysfunction that could be missed at rest is of utmost importance. In patients with “low-flow, low-gradient AVS” (reduced systolic function, a valve opening area <1.0 cm2 and a mean aortic valve gradient <40 mmHg) the use of stress echocardiography is often helpful when attempting to differentiate true severe aortic stenosis from pseudo-severe aortic stenosis, and it provides guidance for adequate therapy through evaluating the contractile reserve of the left ventricle.
The application of strain analysis during transthoracic echocardiography (TTE) allows a deeper physiological understanding of left ventricular (LV) contraction and its relationship with LV structure. Given that the severity of AVS is often progressive, periodical evaluation is necessary. Athletes with a BAV complicated by AVS are managed in the same fashion as athletes with a trileaflet valve.
Classification. Classification is based on the mean aortic valve gradient and aortic valve opening area (AVA):
-
1.
Mild = mean gradient <20 mmHg (AVA > 1.5 cm2).
-
2.
Moderate = mean gradient between 21 and 49 mmHg (AVA 1.0–1.5 cm2).
-
3.
Severe = mean gradient ≥50 mmHg (AVA < 1.0 cm2).
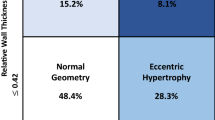
Recommendations for the allowed physical activity should be based on a distinguished strategy. Figure 16.1 shows an example for patients with AVS.
Decision tree on eligibility for different types and intensities of sport according to the clinical severity of aortic valve stenosis (see Chap. 1 for classification of sports). ECG electrocardiogram, LV left ventricular, PAP pulmonary artery pressure
3 Aortic Valve Regurgitation
The commonest causes of AVR include BAV, rheumatic fever, infectious endocarditis, Marfan syndrome, aortic dissection, systemic arterial hypertension and rheumatoid spondylitis. AVR causes dilatation of the LV cavity with increases in LV diastolic and systolic volumes. Bradycardia can worsen the hemodynamic pattern, due to lengthening of the diastolic duration and increase of the regurgitant volume. AVR causes both pressure and volume loading of the left ventricle.
-
Athletes involved in mainly isometric exercise can develop pressure overloads due to high systemic arterial pressure. Hence, the resulting chronically elevated aortic wall tension in strength-trained athletes can be associated with aortic dilatation and regurgitation.
-
Athletes with AVR in the chronic compensated phase are often asymptomatic and can remain so far for many years.
-
In patients with AVR, static exercise causes a reduction of preload resulting in a reduction in LV stroke volume and regurgitant volume.
AVR can be detected by auscultation and, of course, LV dilatation should be evaluated by echocardiography. Facing the fact that LV cavity dimension can also be increased in healthy athletes as a consequence of regular training, this should be considered when assessing LV size in the presence of AVR. As LV dysfunction proceeds, symptoms occur including dyspnea on exertion, arrhythmias and, in advanced cases, angina [7, 8].
People of Afro-Caribbean origin have a lower incidence of BAV. In athletes with BAV, aortic and LV dimensions increase significantly more than in athletes with tricuspid valves, but do not differ from those in the general, non-athlete BAV population. A normally functioning BAV usually does not represent a limit for competitive sport. However, progressive increase in the sizes of both aorta and LV in BAV athletes needs thorough and regular follow-up. Apart from echocardiographic evaluation also Cardiac Magnetic Resonance Imaging (MRI) is of good use. If LV dimensions and Doppler variables fall outside normal values, it may be necessary to interrupt or even stop competitive sport.
Exercise testing (or cardiopulmonary testing) can be helpful in the evaluation of exercise tolerance and blood pressure response. It should be carried out up to the level that is consistent with the particular sport in order to assess ventricular tolerance.
Because of possible progression of AVR over time, periodical evaluation is recommended.
Classification. The hemodynamic severity of AVR can be classified as follows:
-
1.
Mild = absence of peripheral signs of AVR and normal LV and atrial size and function; small dimension of the diastolic flow signal on Doppler-echocardiography.
-
2.
Moderate = peripheral signs of AVR, mild to moderate enlargement of the LV, normal systolic function, moderate dimension of the diastolic flow signal on Doppler-echocardiography.
-
3.
Severe = peripheral signs of AVR, marked dilatation of the LV and/or evidence of LV dysfunction; enlarged atrial size and large dimension of the diastolic flow signal on Doppler-echocardiography.
4 Mitral Valve Stenosis
Mitral valve stenosis (MVS) in young individuals is generally of rheumatic origin. This disease can result in elevated left atrial (LA) pressure, leading to pulmonary hypertension. The increase in heart rate and cardiac output associated with intensive exercise can markedly increase the pulmonary arterial pressure and may eventually lead to acute pulmonary edema. In severe disease, left-sided cardiac output is compromised as a result of poor LV filling. However, exercise intolerance can also be influenced by restrictive lung function and chronotropic intolerance. Embolization by atrial thrombus represents a further complication, which usually occurs in the presence of atrial fibrillation and an enlarged left atrium. Long-term effects of repeated exertion-related increases in pulmonary artery wedge pressure on pulmonary circulation and on the right ventricle are still not well understood.
It still remains elusive to which extend chronic physical activity and especially competitive sports contribute in case of a negative course.
Evaluation. Presence of MVS can be detected by characteristic auscultation, and severity can be determined by non-invasive testing which includes
-
ECG
-
Echocardiography
-
Chest x-ray
-
Exercise testing.
TTE and transesophageal echocardiography (TOE) allow assessment of valve opening area, presence of calcification and papillary muscle function. The contribution of regurgitation should also be considered in the calculation of the valve opening area (Table 16.1). Pulmonary systolic arterial pressure can be assessed by Doppler-echocardiography in the presence of tricuspid regurgitation, even during or after exercise.
-
Exercise testing (or cardiopulmonary testing) can add information regarding the hemodynamic behavior and occurrence of arrhythmias (particularly atrial fibrillation).
-
Invasive testing, e.g. Swan Ganz catheterization, is indicated only in selected cases, when accurate assessment of pressure in the pulmonary circulation is needed for therapeutic or legal purposes.
-
Stress echocardiography may provide additional objective information by assessing changes in mitral gradient and pulmonary artery pressure.
Athletes who develop a significant pulmonary artery systolic pressure during exercise are likely to develop severe adverse effects on RV function over time. Athletes/patients with MVS and atrial fibrillation must receive anticoagulation treatment to avoid systemic embolism. These individuals should avoid contact collision sport. Hemodynamic severity is best characterized by the planimetered mitral valve area and the calculated mitral valve area from the diastolic pressure half-time.
Classification. The severity of MVS can be categorized as follows:
-
1.
Mild = mitral valve opening area 1.5–2.5 cm2, with pulmonary systolic arterial pressure <35 mmHg, and mean gradient <7 mmHg.
-
2.
Moderate = mitral valve opening area 1.0–1.5 cm2, with resting pulmonary systolic arterial pressure between 35 and 50 mmHg, and a mean gradient between 8 and 15 mmHg.
-
3.
Severe = mitral valve opening area <1.0 cm2, with resting pulmonary systolic arterial pressure >50 mmHg , and a mean gradient >15 mmHg.
5 Mitral Valve Regurgitation
The most frequent cause of mitral valve regurgitation (MVR) is the prolapse of leaflets (mitral valve prolapse (MVP)). MVP can appear as a single or bileaflet protrusion and is of relevance in cases of a protrusion of at least 2 mm beyond the long-axis annular plane into the left atrium.
-
It is worth to know that some trials showed that the prevalence of mitral valve prolapse syndrome is lower in black individuals.
Other causes include
-
post-rheumatic fever
-
infectious endocarditis
-
coronary heart disease (ischemic cardiomyopathy)
-
connective tissue disease (e.g. Marfan syndrome)
-
dilated cardiomyopathy.
MVR is responsible for regurgitated blood into the left atrium, which causes increased LV diastolic filling and subsequently raises left atrial pressure. Highly trained athletes presenting with mild mitral (and aortic) valve regurgitation are not disadvantaged regarding their cardiopulmonary capacity, but they have to be evaluated thoroughly.
MVR is clinically detected by dyspnea , exercise intolerance and auscultation. However, the majority of people with mild or moderate MVR remain asymptomatic. The severity of MVR can be assessed by Doppler-echocardiography. TTE is recommended as the first-line imaging modality, two-dimensional TOE is advocated when TTE is of non-diagnostic value or when further diagnostic refinement is required. Three-dimensional echo can provide additional information in patients with complex valve lesions. In assessing the severity of MVR, ECG and chest x-ray are also useful.
Since well-trained athletes often have an increased LV end-diastolic size due to their training history, this should be considered when a decision has to be made whether LV enlargement is caused by MVR or by a physiological adaptation to the years of training. MVR contributes to the unload of LV during systole which can lead to overestimation of true myocardial performance.
-
In athletes, severity of MVR should be based on LV end-systolic volume, and a cut-off of 35 mm/m2 in men (respectively 40 mm/m2 in women) turned out to be useful to distinguish individuals with LV enlargement of clinical relevance.
Physical activity rarely leads to an increased regurgitation fraction due to the reduced systemic vascular resistance, but this effect can be diminished by elevated heart rate. The use of global longitudinal strain could be of potential interest for the detection of subclinical LV dysfunction.
The extent of LA enlargement should also be considered, because of the proclivity for atrial fibrillation. LA volume, systolic pulmonary artery pressure, tricuspid regurgitation, annular size and right ventricular (RV) function are important additional parameters.
-
A significant increase of pulmonary artery pressure with exercise of >60 mmHg has been reported to be of prognostic value.
-
24-h Holter monitoring is recommended when arrhythmias are evident or suspected, and when MVR is due to prolapse of the leaflets.
Athletes with atrial fibrillation must receive anticoagulation treatment, and they should avoid sports with risk of bodily collision. When MVR is due to an isolated MVP the prognosis is good and no sport restriction should be applied.
Classification. There are several methods to classify MVR. The widely accepted PISA-method uses the width of the jet and the velocity to assess the degree of regurgitation, but also CW Doppler characteristics are helpful:
-
1.
Mild = regurgitation width <0.3 cm (PISA), soft density and parabolic CW Doppler MR signal
-
2.
Moderate = regurgitation width 0.3–0.6 cm (PISA).
-
3.
Severe = regurgitation width >0.6 cm (PISA), dense and triangular CW Doppler MR jet, large central MR jet
6 Tricuspid Valve Stenosis
In most cases tricuspid valve stenosis (TVS) is caused by rheumatic fever and is associated with MVS. In the presence of MVS and TVS, patients should be assessed with reference to the MVS. An isolated TVS is very rare (Table 16.1).
-
If the patient is asymptomatic (no dizziness, no dyspnea or peripheral edema), participation in competitive sports may be possible.
Thorough echocardiographic evaluation of the anatomy of the valve and its subvalvular apparatus is important to evaluate the therapeutic strategy. There is no generally accepted grading of TVS but a mean gradient ≥5 mmHg at normal heart rate is considered indicative of clinically significant TVS.
7 Tricuspid Valve Regurgitation
Tricuspid valve regurgitation (TVR) is often the consequence of RV dilatation. Rheumatic fever or infectious endocarditis are less common causes. Primary TVR leads to volume overload of the RV, increased venous pressure and congestive symptoms. The severity of TVR can be determined non-invasively by physical examination, chest x-ray and especially echocardiography. Dense and triangular early peaking regurgitant signal on colour flow, vena contracta flow, PISA radius and early diastolic filling velocity and RV outflow velocity are established echocardiographic parameters to assess the severity of TVR.
8 Multi-valvular Diseases
Multi-valvular diseases frequently occur in connection with rheumatic fever, myxomatous valvular diseases or infectious endocarditis. These conditions can be diagnosed by physical examination and assessed quantitatively by Doppler-echocardiography. If one valvular disease worsens, it might impact the other and result in unfavorable hemodynamic effects. Therefore, close follow-up is warranted in these athletes with regard to participation in competitive sports (see Table 16.1 for recommendations).
9 Postoperative Athletes with a (Bio)prosthetic Heart Valve
Although patients usually improve clinically after heart valve replacement, the long-term mortality can be higher than in a healthy control population. Furthermore, patients with normal hemodynamic patterns at rest may have abnormal values under physical stress.
-
Exercise testing, preferably spiroergometry, should be carried out up to the intensity consistent with that of the sport the athlete wishes to pursue.
Noteworthy, patients with mechanical valves (or bioprosthetic valves in selected cases) need systematic anticoagulation treatment, which further limits their choice of competitive sports. Athletes with artificial valves should undergo periodic reevaluation. Athletes with a prosthetic or bioprosthetic valve who are receiving anticoagulation treatment should not participate in sports with a risk of bodily collision.
10 Athletes Post-valvuloplasty
Valvuloplasty is still performed in some patients with MVS, despite the probability of restenosis and no clear advantage when compared with valve replacement. Aortic valvuloplasty is performed extremely rare in young patients with AVS.
-
In athletes after valvuloplasty, recommendations for sports participation are based on the residual degree of severity of stenosis and/or regurgitation.
-
Exercise testing should be carried out up to the level consistent with the level reached in the sport in which the patient participates.
11 Mitral Valve Prolapse
Mitral valve prolapse (MVP) is mostly associated with myxomatous degeneration of the valve. It preferentially occurs in athletes of tall stature and shows a familial cluster. Ischemic cardiomyopathy and hypertrophic obstructive cardiomyopathy are potential secondary etiologies. Mitral valve prolapse is a disease of all connective tissues, including the tendinous chords; and so, the risk of chordal rupture remains after repair of the regurgitant valve.
-
MVP is often associated with mitral regurgitation.
-
Rhythm disorders (i.e. brady- or tachyarrhythmias), endocarditis, syncope or embolism can also occur.
-
SCD in MVP patients is more common in women, occurs regardless of the degree of regurgitation , and is often associated with myocardial fibrosis in the papillary muscles on contrast-enhanced cardiac magnetic resonance imaging.
The typical auscultatory finding is a late-systolic click and a murmur due to late systolic or holosystolic regurgitation. Elongation and thickening of valve leaflets, degree of mitral regurgitation and LV dimension and function should be assessed by echocardiography. Evaluation should include exercise testing and/or Holter monitoring to assess the presence of arrhythmias. Frequent cardiological evaluation is recommended, because the regurgitation can get worse by progressive degeneration of the leaflets.
12 Transcatheter Interventions for Valvular Heart Disease
The recent development of devices for transcatheter aortic valve implantation (TAVI) , mitral repair (mitral clipping), and closure of prosthetic paravalvular leaks has led to a greatly expanded armamentarium of catheter-based approaches to patients with regurgitant as well as stenotic valvular disease.
-
The use of these new techniques is supposed to be rare in competitive athletes.
-
However, athletes concerned should be judged according to the remaining cardiac defect and with respect to anticoagulation therapy.
In patients after TAVI, combined exercise training (endurance and resistance component) is safe and highly effective and often results in improved quality of life, muscular strength and exercise capacity. However, TAVI procedures are mainly used in elderly patients so far, showing corresponding comorbidities that make competitive sports in these individuals almost impossible. Latest trials on TAVI procedures showed also advantages in younger patients receiving this technique.
13 Prophylaxis for Endocarditis
Infective endocarditis (IE) is an endovascular, microbial infection of intracardiac structures facing the blood, including infections of the large intrathoracic vessels. The early lesion is a vegetation of variable size, although destruction, ulceration or abscess may follow. The increasing accuracy of echocardiography and therapeutic progress have contributed to the prognostic improvement in the last few years.
Patients with
-
previous history of infective endocarditis
-
prosthetic heart valves
-
acquired valve disease
are considered high risk patients and should receive antibiotic prophylaxis when exposed to risk of bacteremia in accordance with the ESC recommendations.
-
As a general rule, all sports activity should be avoided when active infection with fever is present. Resumption of sport activity can be considered when the inflammatory process is completely extinguished, and systematic maintenance of endocarditis prophylaxis must be observed strictly.
14 Aortopathies
The term aortopathies includes several aortic diseases that account for 1.6–5% of SCD in young athletes. Although Marfan syndrome (MFS) is the prototype for the aortopathies, maladaptive remodelling of the vascular extracellular matrix is not unique to MFS. Irrespective of etiology, altered vascular structure may lead to an increase propensity for aortic dilation, dissection, or rupture of aortic wall.
The evaluation of an athlete with suspected MFS includes
-
family and personal medical history
-
physical examination
-
echocardiography
-
genetic testing.
If transthoracic echocardiographic evaluation does not allow precise visualization of the aorta, computed tomography (CT) or MRI should be performed. Particular care should be paid in evaluating tall athletes engaged in certain sports such as basketball and volleyball which may exhibit most of the systemic features of the syndrome. The diagnosis of MFS relies on defined clinical criteria (Ghent nosology; see Chap. 7). Several factors influence aortic root dimensions, including body size, age, height, and gender, and they have to be taken into account [9].
-
The abnormal range is an enlargement at the level of sinuses of Valsalva with a Z-score ≥2.
-
Particular attention with close clinical surveillance should be paid when a rapid change in aortic dilatation is demonstrated (i.e. ≥0.5 cm/year) or when heart or valve function deteriorates.
Also, other rare connective tissue disorders may increase the risk of aortic dilatation/dissection in competitive athletes. These conditions may present a clinical overlap with MFS in the cardiovascular, ocular or skeletal systems.
Whether regular and intensive exercise has an impact on aortic root dimensions is still debated. However, a marked aortic root dilatation does not represent a physiological adaptation to exercise. Life expectancy in patients with aortopathies is largely determined by the risk of aortic dissection and lifestyle risk factors.
Clinical Pearls
-
The majority of athletes with VHD are often asymptomatic for a long time and an abnormal ECG pattern raises a first suspicion on a potential valve defect. Possible symptoms are breathlessness that is disproportionate to the amount of exercise being performed, palpitation or syncope.
-
TTE is the first line investigation to confirm the diagnosis of VHD and provides essential prognostic information in relation to severity of valve dysfunction, ventricular function and pulmonary artery pressure.
-
Valve defects with a predominantly regurgitant component are often better tolerated than stenotic lesions.
-
Recommendations for athletes with VHD need a detailed diagnostic approach and tailored guidance that respect not only the valve disease itself but also potential arrhythmia, pulmonary pressure, size and function of cardiac chambers.
References
Pelliccia A, Fagard R, Bjornstad HH, Anastassakis A, Arbustini E, Assanelli D, et al. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the study group of sports cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European society of cardiology. Eur Heart J. 2005;26(14):1422–45.
Gati S, Malhotra A, Sharma S. Exercise recommendations in patients with valvular heart disease. Heart. 2019;105(2):106–10.
Mellwig KP, van Buuren F, Gohlke-Baerwolf C, Bjornstad HH. Recommendations for the management of individuals with acquired valvular heart diseases who are involved in leisure-time physical activities or competitive sports. Eur J Cardiovasc Prev Rehabil. 2008;15(1):95–103.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739–91.
Levine BD, Baggish AL, Kovacs RJ, Link MS, Maron MS, Mitchell JH, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 1: classification of sports: dynamic, static, and impact: a scientific statement from the American heart association and American college of cardiology. Circulation. 2015;132(22):e262–6.
Pelliccia A, Adami PE, Quattrini F, Squeo MR, Caselli S, Verdile L, et al. Are olympic athletes free from cardiovascular diseases? Systematic investigation in 2352 participants from Athens 2004 to Sochi 2014. Br J Sports Med. 2017;51(4):238–43.
Booher AM, Bach DS. Exercise hemodynamics in valvular heart disease. Curr Cardiol Rep. 2011;13(3):226–33.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129(23):2440–92.
Boraita A, Heras ME, Morales F, Marina-Breysse M, Canda A, Rabadan M, et al. Reference values of aortic root in male and female white elite athletes according to sport. Circ Cardiovasc Imaging. 2016;9(10):e005292.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Review
Review
1.1 Questions
-
1.
What is the most frequent cause of mitral valve regurgitation (MVR) and how can it be diagnosed adequately?
-
2.
Are athletes with bicuspid aortic valve (BAV) allowed to perform sport on a higher level?
-
3.
Which left ventricular size can be accepted in athletes with MVR?
1.2 Answers
-
1.
The prolapse of leaflets (mitral valve prolapse (MVP)) is the most frequent cause of MVR and can appear as a single or bileaflet protrusion. Typical symptoms are dyspnea, exercise intolerance and auscultation. Many individuals are asymptomatic. MVR can be assessed by Doppler-echocardiography. Next to the valve function the extent of left atrial enlargement should also be evaluated, because of the proclivity for atrial fibrillation.
-
2.
Congenital BAV is one of the most common congenital heart diseases appearing in up to every 50th individual and can lead to both AVS and aortic valve regurgitation. A normally functioning BAV usually does not represent a limit for competitive sport but these athletes need regular follow-up evaluation of both aorta and left ventricular size.
-
3.
The relevance of MVR in athletes should also be based on LV end-systolic volume. A cut-off of 35 mm/m2 in men (respectively 40 mm/m2 in women) turned out to be useful to distinguish individuals with LV enlargement of clinical relevance.
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
van Buuren, F., Mellwig, K.P. (2020). Specific Cardiovascular Diseases and Competitive Sports Participation: Valvular Heart Disease. In: Pressler, A., Niebauer, J. (eds) Textbook of Sports and Exercise Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-030-35374-2_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-35374-2_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-35373-5
Online ISBN: 978-3-030-35374-2
eBook Packages: MedicineMedicine (R0)