Abstract
Mesial temporal lobe epilepsy (MTLE) is one of the most common focal epilepsy syndromes. Roughly one third of patients with MTLE continue to have disabling seizures despite multiple trials of antiepileptic medications. Surgical resection of the mesial temporal lobe in patients with drug-resistant mesial temporal epilepsy can lead to freedom from disabling seizures in 60–90% of patients. However proper patient selection is essential in order to achieve high rates of seizure freedom. In this chapter, we first discuss the pathophysiology and semiology of mesial temporal lobe epilepsy. After reviewing the diagnosis, we detail the preoperative workup necessary to determining if a patient is appropriate for surgery. Surgical intervention for mesial temporal epilepsy has evolved significantly over the past two decades. We discuss in detail the classical surgical approaches including anterior temporal lobectomy and selective amygdalohippocampectomy in addition to outcomes and complications of surgery. We then discuss newer surgical approaches to MTLE, including stereotactic laser amygdalohippocampotomy, stereotactic radiosurgery, and neuromodulation, emphasizing how these new techniques supplement traditional approaches in order to provide surgical options to a greater population of patients with MTLE.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Seizure
- Mesial temporal epilepsy
- Mesial temporal lobe epilepsy
- Mesial temporal sclerosis
- Anterior temporal lobectomy
- Selective amygdalohippocampectomy
- Stereotactic laser amygdalohippocampotomy
- Hippocampal transections
- Responsive neurostimulation
- Deep brain stimulation of the anterior nucleus of the thalamus
- Gamma Knife
- Epilepsy surgery
- Surgical techniques
Introduction
Mesial temporal lobe epilepsy (MTLE) is a common, well-defined focal epilepsy syndrome. The surgical evaluation and treatment of patients with MTLE is also the most extensively studied among focal epilepsy syndromes. Epilepsy affects roughly 1% of the population, and more than 30% of patients with epilepsy have drug-resistant (used interchangeably with medically refractory) epilepsy [1,2,3]. The International League Against Epilepsy (ILAE) defines drug-resistant epilepsy as failure of adequate trials of two tolerated and appropriately chosen and used antiepileptic drug schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom [4]. Of patients with drug-resistant epilepsy, roughly 25% are candidates for surgical intervention.
Epilepsy surgery has a long history, with the earliest report from Dudley in the early nineteenth century [5, 6]. However the superiority of surgical resection over continued medical management in properly selected patients with drug-resistant MTLE was only rigorously confirmed in 2001 when Wiebe and colleagues showed 64% freedom from disabling seizures after anterior temporal lobectomy (ATL) compared to only 8% rate with continued medical management [7]. Since that time, epilepsy surgery has become significantly more accepted, leading to advances in patient selection, surgical technique, and technological innovation. Despite these advances, the surgical treatment of epilepsy remains underutilized [8]. Surgical treatment of epilepsy is also more cost-effective compared to continued medial management. While surgery requires a large upfront cost, recurring costs from seizures poorly controlled with medical management build up over time and outrun the cost of surgery within 5–10 years [9,10,11]. Not only is the cost of epilepsy surgery less than the combined costs of a lifetime of disability from seizures, but many patients continue to suffer from disabling seizures that could be cured or greatly reduced with surgery. Epilepsy surgery requires an interdisciplinary team of neurologists, neurosurgeons, radiologists, and neuropsychologists. This chapter outlines perspectives from many of these parties, reviewing the pathophysiology of MTLE, patient presentation, presurgical evaluation, and evolution of the modern surgical options used to treat MTLE. We also present strategies for preventing harm and achieving maximal efficacy with surgery for patients undergoing MTLE surgery.
The Mesial Temporal Lobe and Mesial Temporal Lobe Epilepsy (MTLE)
Mesial temporal sclerosis (MTS), classically referred to as Ammon’s horn sclerosis, is the most common pathology underlying mesial temporal lobe epilepsy, accounting for 50–60% of MTLE cases. Low-grade tumors contribute an additional 20–30% of MTLE cases, and other etiologies including vascular malformations, neuronal loss, or other patterns of gliosis account for the remaining 10–20% [12, 13]. The most common tumors leading to mesial temporal lobe epilepsy include ganglioglioma (40%), dysembryoplastic neuroepithelial tumor (DNET) (20%), and diffuse low-grade glioma (20%). Less common tumors include pilocytic astrocytoma and pleomorphic xanthoastrocytoma [14].
Radiographically, hippocampal sclerosis is exhibited by increased T2 fluid-attenuated inversion recovery (FLAIR) signal in the hippocampus, loss of hippocampal architecture, and sclerosis of the hippocampus (Fig. 24.1). Atrophy of the ipsilateral fornix can also be frequently seen. Histology shows neuronal cell loss with chronic astrogliosis. Gliosis is accompanied by a loss of pyramidal neurons and granule cell dispersion.
Right mesial temporal sclerosis. T2-weighted coronal image through the bilateral hippocampi illustrates classic findings of mesial temporal sclerosis. Note the sclerotic right hippocampus with loss of internal architecture (white arrow). The right hippocampus also appears slightly hyperintense compared to the left, better visualized on T2-FLAIR (not shown). The ipsilateral fornix (black arrow) is also small compared to the contralateral fornix
The mechanism by which hippocampal sclerosis leads to epilepsy is poorly understood. Hippocampal sclerosis is an acquired lesion, often associated with prolonged febrile seizures in childhood. After significant sclerosis, the hippocampus and surrounding mesial temporal structures can become independent seizure foci capable of generating epileptiform discharges that can spread, manifesting as mesial temporal epilepsy.
The anatomy of the mesial temporal lobe is complex, and complete understanding of the three-dimensional relationship of mesial temporal structures requires close anatomical study. Mesial temporal structures include the hippocampus, amygdala, subiculum, and entorhinal cortex. The mesial temporal lobe is highly connected to the frontal, temporal, and parietal lobes through Papez’s circuit. Working knowledge of the relationships between these structures and their surroundings (Fig. 24.2) is essential to performing mesial temporal surgeries safely. Excellent reviews of mesial temporal anatomy are available [15,16,17].
Temporal lobe gross anatomy. Important lateral neocortical landmarks include the superior temporal gyrus, middle temporal gyrus, and inferior temporal gyrus. The Sylvian fissure divides the frontal lobe from the temporal lobe, and the lateral temporal gyri are separated by the superior temporal sulcus and inferior temporal sulcus (a). Inferiorly, the fusiform gyrus is medial to the inferior temporal gyrus, separated by the lateral occipital temporal sulcus. The collateral sulcus divides the medial aspect of the fusiform gyrus from the parahippocampal gyrus (b). The optic tract, along with other important structures not shown (anterior choroidal artery, posterior cerebral artery, cranial nerve III), runs in the ambient and crural cisterns just medial to the parahippocampus and the uncus (c). With the parahippocampal gyrus removed, the proximity of the mesial hippocampal structures (fimbria, hippocampus, amygdala, uncus) to thalamic structures (lateral geniculate nucleus and pulvinar) as well as the cerebral peduncle can be appreciated (d). Ant., anterior; Calc., calcarine; Cent., central; Chor., choroidal; Coll., collateral; Fiss., fissure; Gen., geniculate; Inf., inferior; Lat., lateral; Ling., lingual; Occ., occipital; Occip., occipital; Parahippo., parahippocampal; Par., parietal; Ped., peduncle; Post., posterior; Seg., segment; Sulc., sulcus; Sup., superior; Termp., temporal; Tr., tract. (From Kucukyuruk B, et al. [17]. https://creativecommons.org/licenses/by/3.0/)
Semiology of Mesial Temporal Lobe Epilepsy
The semiology of mesial temporal lobe epilepsy is both classic and variable. Isolated seizures of the hippocampus can be clinically silent, often manifesting only as behavioral arrest. Additional symptoms occur with propagation of epileptiform discharges to closely connected structures. Careful attention to the semiology, particularly the temporal progression of the semiology, can help to determine the precise location of the seizure onset zone (SOZ) as well as the path by which the epileptiform activity spreads.
Mesial temporal seizures can be divided into several subtypes based on the SOZ and network of structures involved. These subtypes include mesial (amygdala, hippocampus, parahippocampal gyrus, entorhinal cortex), temporopolar, mesiolateral, lateral, and temporal “plus” subtypes [18]. Isolated mesial temporal seizures often first manifest only as behavioral arrest. Additional signs of amygdala or hippocampal seizures include epigastric discomfort, caused by spread from the amygdala to the posterior insula. Other symptoms include auras of fear, déjà vu or déjà rêvé, and oral or gestural automatisms from early spread to the frontal operculum. Oral automatisms are characterized by lip smacking or chewing. Gestural automatisms include picking, fumbling, and fidgeting with the hands. Contralateral head version often occurs prior to seizure generalization and is also highly suggestive of mesial temporal onset. Patients with seizure onsets within any of the mesial structures often fall into this semiology subtype.
Seizures with temporopolar SOZ have very similar semiology to those of mesial temporal onset but tend to have faster onset of both clinical symptoms and loss of awareness (i.e., impaired consciousness) [19]. The faster loss of awareness likely stems from earlier involvement of the superior temporal gyrus (STG), as the temporal pole is a continuation of the superior temporal gyrus bending inferiorly approaching the lesser wing of the sphenoid. Temporopolar seizures quickly involve the STG, an area of association cortex with robust white matter tract connectivity to a broad array of brain networks, leading to loss of awareness. In contrast, mesial temporal seizures spread first to the temporal pole prior to interacting with the superior temporal gyrus en route to other structures, leading to slower appearance of seizure semiology compared to temporopolar onset seizures.
Mesiolateral temporal onset seizures, like temporopolar onset seizures, also manifest in early loss of awareness. Early vocalizations as well as oral and verbal automatisms are also characteristic. The semiology of these seizures overlaps with the mesial subtype: mesiolateral seizures can start from near simultaneous epileptiform activity from independent mesial and lateral neocortical structures [20, 21].
Lateral temporal onset seizures typically manifest with an auditory aura followed by frequent secondary generalized tonic clonic activity. They are typically of short duration. A lateral temporal SOZ can be secondary to a lesion in the lateral temporal neocortex but can also occur in MRI-negative temporal lobe epilepsy [20, 21]. However there are also rare cases of pure lateral temporal neocortex onset epilepsy with radiographic mesial temporal sclerosis where the only suggestion of neocortical onset is seizure semiology [22]. This highlights the importance of semiology in determination of the SOZ, as performing a selective mesial temporal resection would fail to achieve seizure freedom in such a patient.
Temporal “plus” epilepsy manifests with gustatory, auditory, or vestibular auras, ipsilateral tonic motor signs, contraversion, and postictal dysphoria. This semiology arises from combinations of involvement between the insula, frontal and temporal operculum, orbitofrontal cortex, and temporo-parieto-occipital junction. This complex semiology can arise from fast spread of temporal lobe seizures or from seizure onset zones in the involved epileptic networks [23]. It is imperative that whenever a non-mesial temporal semiology is encountered, the anatomic region responsible for that behavior be investigated in addition to the mesial and neocortical temporal structures prior to consideration for surgery.
Diagnosis and Preoperative Workup
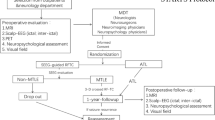
The goals of the presurgical workup are to confirm the diagnosis of epilepsy, identify an epileptogenic lesion if present, determine the size and location of the SOZ, and finally determine the feasibility and safety of resection. Many tools are used to perform this evaluation, and the results from one study can often inform multiple of the above goals. The results from each test must be critically examined for congruous and incongruous findings prior to planning resective surgery.
Confirmation of Epilepsy Diagnosis
Video EEG in an epilepsy monitoring unit remains the gold standard for the diagnosis of epilepsy. Subjective reports from epilepsy monitoring units at busy surgical epilepsy centers suggest that 20–30% of patients referred for surgical epilepsy evaluation have psychogenic non-epileptic seizures (previously referred to as pseudoseizures) and do not in fact have epilepsy [24]. Confirmation of the epilepsy diagnosis by means of video EEG monitoring in an experienced EMU is essential prior to further surgical evaluation. Ictal onset of MTLE is characterized by a diverse set of patterns on scalp EEG, most commonly with cessation of interictal discharges, followed by ipsilateral temporal rhythmic delta-theta activity [25].
Identification of Epileptogenic Lesion
A high-resolution MRI is essential for determining the presence or absence of an intracranial lesion as a source of seizures. This MRI should be reviewed by neurologists, neuroradiologists, and neurosurgeons experienced at diagnosing epileptogenic foci. Diagnoses such as small temporal encephaloceles, cortical dysplasias, or periventricular nodular heterotopias are easy to miss if not explicitly considered. Surgical outcomes are better when an epileptogenic focus is identified, and surgery will fail to achieve seizure freedom if an epileptogenic focus is missed and left in place after surgical resection. Studies using 7T MRI scanners have shown that even in cases of MRI-negative epilepsy (by 3T MRI), there can be epileptogenic lesions visible on 7T MRI thought to be primary epileptogenic foci [26]. The importance of careful scrutiny of MRI scans is emphasized by the fact that after identifying such 3T MRI-negative lesions on 7T MRI, a significant percentage of these lesions can be seen on 3T MRI in retrospect. Preoperative MRI should include T1-weighted, T2-weigted, and susceptibility-weighted images. Some centers routinely obtain CT scans to screen for small bony defects suggestive of encephalocele. The most common etiology of MTLE is mesial temporal sclerosis (Fig. 24.3a).
Identification of the seizure onset zone. Coronal (left) and axial (right) cuts through a T2-FLAIR MRI scan show classic left mesial temporal sclerosis (white arrow) (a). Interictal 18F-FDG PET scan shows hypometabolism in the left temporal pole and mesial temporal region (white arrowheads), corresponding to the region of mesial temporal sclerosis (b). Axial, coronal, and sagittal images showing MEG findings suggestive of a left mesial temporal spike cluster. Note the convention for MEG is to display the patient’s left on the left side of the screen, the opposite of standard radiographic convention (c). (Images courtesy of Dr. Audrey Nath)
Determination of Seizure Onset Zone (SOZ)
Determination of the SOZ is essential to achieving seizure freedom; surgical cessation of seizures requires complete removal or disconnection of the entire SOZ. Several tests can help determinate the location and size of the SOZ. An initial hypothesis should be generated based on scalp EEG recordings; however confirmation is necessary due to the poor spatial resolution of scalp EEG.
Fluorodeoxyglucose F 18 (18F-FDG) PET is commonly used for localization. 18F-FDG is a radioactive glucose analog. Like glucose, 18F-FDG is taken up readily by metabolically active cells at a rate proportional to cellular metabolic activity. Also like glucose, after cellular uptake 18F-FDG is phosphorylated and trapped in the cell. 18F-FDG lacks the 2-hydroxyl group present in normal glucose and cannot be further metabolized until after radioactive decay, leading to accumulation of 18F-FDG in proportion to metabolic activity in cells. The PET scan displays the distribution of 18F-FDG throughout the brain. Eventually 18F decays to 18O converting 18F-FDG to glucose-6-phosphate which can then be metabolized just as ordinary glucose. PET scans are typically performed during interictal periods to facilitate easy scheduling. During ictal periods seizing brain has increased metabolism and increased local cerebral perfusion. In contrast, during interictal periods the seizure onset zone exhibits abnormal hypometabolism. These areas of hypometabolism are readily identifiable by 18F-FDG PET. 18F-FDG PET findings in MTLE often include hypometabolism of the hippocampus and surrounding anterior temporal structures (Fig. 24.3b). Importantly, while an area of hypometabolism often includes the SOZ, this is not always the case. The SOZ may only be a small part of a hypometabolic region seen on 18F-FDG PET.
Ictal SPECT is another nuclear medicine study measuring changes in local cerebral blood flow related to seizures. Ictal SPECT must be performed in a monitored setting with video EEG for confirmation of seizure onset. A tracer, often technetium-99m (Tc-99m) labelled hexamethylpropyleneamine oxime (HMPAO), is injected at the time of seizure onset. In contrast to 18F-FDG PET, the tracer in SPECT distributes according to blood flow, not metabolism. Since blood flow is closely coupled to brain metabolism (flow-metabolism coupling), the tracer distribution closely approximates metabolic activity. Since actively seizing areas of the brain have increased metabolic demand, generally leading to increased local cerebral blood flow, the tracer rapidly distributes in higher quantities to actively seizing locations in the brain where it remains for several hours after the seizure. The ictal SPECT reading is compared to an interictal SPECT in the same patient to determine what areas of the brain have increased local cerebral perfusion during seizures [27], suggestive of the SOZ. Ictal SPECT is most useful in partial epilepsy, and the efficacy decreases with secondarily generalized tonic-clonic activity. Ictal SPECT findings in MTLE generally show increased cerebral blood flow on the side of MTLE in mesial and often lateral anterior temporal structures.
Magnetoencephalography (MEG) localizes the SOZ by measuring changes in the local magnetic field of the brain. In normal brain tissue, populations of axons are roughly aligned in the cerebral mantle. Synchronized firing of populations of neurons changes the current flow leading to the alterations in the magnetic field detected by MEG. Both EEG and MEG are measuring the same neurophysiologic process. Importantly, since magnetic fields are produced tangentially to the direction of current, MEG is best at measuring electrical activity in sulci which produce alterations in the magnetic fields outside the scalp. Magnetic field alterations from electrical activity in gyri often escape detection from the magnetometers arranged around the head since these field alterations occur within the head. EEG, by contrast, detects electrical signal from populations of neurons in both gyri and sulci. The electric fields measured by EEG are heavily distorted by bone and scalp making exact localization of electrical activity difficult. Magnetic fields are not as distorted by these structures, allowing MEG to localize electrical activity with much greater precision than EEG. For this reason, MEG is used for anatomic localization of epileptic populations of neurons, providing additional evidence for the location of the SOZ (Fig. 24.3c). MEG machines are costly and are not widely available. Many busy and successful epilepsy centers do not use MEG in their presurgical epilepsy evaluation.
Neuropsychological Evaluation
A comprehensive neuropsychological evaluation is an essential part of the presurgical evaluation. Specific neuropsychological deficits can suggest involvement of anatomic structures in the epilepsy network. Furthermore, results from neuropsychological testing can also be used to predict the morbidity of different surgical approaches. Neuropsychological deficits from MTLE fall into three predominant categories: memory impairments, executive function impairments, and language impairments [28].
Working memory, including short-term memory, is commonly impaired in patients with MTLE. Severity of working memory impairment is higher with dominant (usually left) temporal lobe epilepsy, earlier age of onset, increased seizure burden, and hippocampal sclerosis [29]. Working memory deficits can further be divided into verbal memory impairment (strongly associated with dominant side MTLE [30, 31]) and spatial memory impairment (more associated with nondominant side MTLE [32]). Deficits in long-term autobiographical memory are also possible, even in cases with intact working memory [33,34,35]. Such deficits arise from an inability to consolidate episodic memory (context-dependent) despite normal abilities to store semantic knowledge and single items (context-free memory) [36]. Verbal memory function is classically localized to the dominant hippocampus, with spatial memory more associated with the nondominant hippocampus.
Deficits specific to executive function are less well defined. Difficulty forming new associations and registering information [37,38,39,40], decreased feedback-based decision-making [41], and poor mental flexibility under high cognitive loads [42] have all been demonstrated in the MTLE population. The mechanism for executive function impairment remains poorly understood but may stem from the high connectivity between mesial temporal and prefrontal structures, frequently involving prefrontal regions in MTLE seizure networks.
Word finding and naming deficits are the most common language impairments in MTLE, present in up to 40% of cases. These deficits are most often present when seizures arise from the language-dominant (usually left) lobe [43, 44]. These language impairments have a significant detrimental impact on daily life [45]. Importantly, auditory naming (by oral definition) is more affected than visual (by picture card) naming [43, 46]; deficits in auditory naming are predictive of seizure focus laterality in 85% of patients [47]. Verbal and auditory naming is classically localized to the dominant lateral temporal neocortex [48, 49]. However, the exact locations are variable and include networks across the anterior temporal, middle temporal, inferior temporal, and posterior superior temporal neocortex [50, 51].
Given the memory and language function of the dominant temporal lobe, determination of language and memory dominance can have a large impact on operative planning and predicting postoperative neuropsychological outcomes. Removing dominant mesial temporal structures often leads to worsening neuropsychological deficits. The intracarotid amobarbital (Wada) test has classically been used to determine language dominance. Over the last decade, language dominance testing with the Wada has slowly been replaced with fMRI, sparing patients periprocedural risk and discomfort associated with catheterization. fMRI has been shown to be a reliable alternative to Wada with similar prediction accuracy for postoperative naming and verbal memory decline after ATL [52].
The most reliable predictors of verbal memory decline after resective surgery for MTLE are dominant lobe temporal epilepsy (dominant side resection), excellent preoperative verbal memory IQ (>120), MRI-negative epilepsy, and late age onset of epilepsy. These risk factors are important in both patient counseling and determination of what surgery to perform.
After confirming the diagnosis of MTLE with video EEG, an interdisciplinary team of neurosurgeons, neurologists, neuroradiologists, and neuropsychologists carefully review and discuss the temporal progression of the seizure semiology; the anatomic findings on MRI, the location of the SOZ as determined by interictal PET, ictal SPECT, and/or MEG; and the neuropsychological testing. The team generates a hypothesis of the seizure focus and seizure network, probing all tests for concordant and discordant data. The multidisciplinary team then makes a decision about invasive monitoring and/or surgical treatment.
Invasive Electroencephalography Monitoring
Invasive monitoring techniques are covered in detail in Chap. 23. A few points specific to MTLE are discussed here. If there is strong concordance between seizure semiology, preoperative MRI with MTS, seizure onset zone studies, and neuropsychological testing, some centers advocate advancing directly to surgical resection without invasive monitoring [53]. If a lesion other than MTS is present on MRI and thought to be the seizure focus, invasive monitoring is also not required but may be helpful in aiding resection of the entire seizure onset zone to achieve the best seizure freedom outcome. If any of the previously discussed preoperative evaluation is discordant or suggestive of more than one seizure focus, we recommend proceeding with invasive electroencephalography monitoring. Epilepsy monitoring with video and invasive electroencephalography is commonly referred to as phase 2 monitoring.
Effective invasive recordings can be performed with either subdural grids and strips or stereoelectroencephalography (sEEG). The precise location of the implants should be guided by a hypothesis of the seizure onset zone and epileptic networks based on careful consideration of semiology and other aforementioned preoperative test results. For subdural grids and strips, the lateral temporal neocortex is often covered by a grid, while subdural strips can be wrapped around the anterior temporal pole and slid inferiorly to record from fusiform and parahippocampal gyri. Care must be taken when inserting subtemporal strips, as large draining veins from the temporal lobe may traverse this space on their way to the transverse sinus. sEEG electrode trajectories should be planned to sample all suspected anatomic structures under consideration as epileptogenic foci, as well as from the suspected epilepsy network. Particular care must be taken to avoid superficial subdural vascular structures when planning sEEG trajectories to prevent intracranial hemorrhage during electrode placement.
Resective Surgeries for Mesial Temporal Epilepsy
Surgery for the treatment of medically refractory MTLE has evolved significantly over the last two decades. Resective surgery with anterior temporal lobectomy (ATL) remains the gold standard for medically refractory MTLE. Selective amygdalohippocampectomy (SAHC) is an approach that leaves the lateral temporal neocortex in place while removing all mesial temporal structures. Lateral temporal neocortex is preserved with the goal of decreasing postoperative cognitive deficits, particularly naming and language problems.
Anterior Temporal Lobectomy (ATL) Procedure
Anterior temporal lobectomy (ATL) has been the mainstay of treatment for MTLE for half a century. Over time, the amount of lateral neocortex commonly resected has decreased, which has not correlated to loss of efficacy in seizure control when radiographic and electrocorticographic testing colocalizes to the mesial temporal structures. When lateral temporal neocortex is implicated in seizure onset, resection of the mesial temporal structures is also indicated for effective seizure control [54, 55]. There is a wide degree of variation from surgeon to surgeon in how an anterior temporal lobectomy is performed, leading some to conclude that there is no “standard” anterior temporal lobectomy. Here we describe our practice.
Prior to surgery, patients are continued on their current antiepileptic medication regimen. Some surgeons prefer to discontinue valproic acid and its derivatives (e.g., divalproex) 5–7 days prior to surgery due to decreased platelet function, though influence on intraoperative blood loss is debated [56]. Preoperative antibiotics and 10 mg IV dexamethasone are administered just prior to incision. Dexamethasone is tapered over 1 to 2 weeks after surgery. The surgery is usually performed under general anesthesia, as the amount of lateral temporal neocortical resection is small leading to low risk of postoperative language dysfunction. If significant lateral temporal neocortical resection is required for a dominant temporal lobe lesion, surgery can be performed awake to allow for intraoperative language mapping. Speech mapping can also be performed in the epilepsy monitoring unit (EMU) via stimulation with a subcortical grid during phase 2 monitoring allowing for safe dominant lateral temporal neocortical resection under general anesthesia.
In general, our mesial temporal resection which we describe below includes the anterior 3 cm of both the parahippocampal gyrus and hippocampus, the inferior amygdala, and the uncus. The surgery can be divided into four steps: (1) craniotomy, (2) anterolateral neocortical resection, (3) microsurgical resection of mesial temporal structures (amygdala, hippocampus, and parahippocampal gyrus), and (4) closure.
The patient is positioned on the operating room table supine with a shoulder roll. The head of bed is elevated to bring the head above the level of the heart. The head is placed in a three-point skull pin fixation device, extended slightly, and turned away from the side of surgery. The bed is also rotated to bring the frontotemporal area horizontal to the floor. Cranial navigation can be used but is not necessary, as anatomic landmarks are routinely used to guide the surgery.
A reverse question mark incision is used beginning immediately behind the hairline and extending posteriorly to just superior to the superior temporal line. The incision is taken down just anterior to the ear to the root of the zygoma (Fig. 24.4a), and a myocutaneous flap is elevated and maintained by fish-hook retractors. A modified pterional craniotomy is performed with inferior border at the floor of the middle fossa defined by the root of the zygoma, anterior border at the frontal process of the zygomatic bone, posterior border at approximately the posterior border of the pinna, and superior border at the superior temporal line (Fig. 24.4b). The sphenoid wing should be cut flush with the edge of the craniotomy but does not need to be drilled down further as would be done for exposure of the circle of Willis. The dura is opened in a horseshoe flap and reflected against the temporalis muscle. This exposure should reveal the inferior frontal gyrus, the Sylvian fissure, and the anterior 5–6 cm of superior (STG ), middle (MTG), and inferior temporal gyri (ITG) (Fig. 24.5a).
Skin incision and craniotomy for anterior temporal lobectomy. A small reverse question mark incision beginning behind the hairline is used to elevate a myocutaneous flap (a). A modified pterional craniotomy is then performed, with special attention to the anterior and inferior cuts to ensure access to the temporal pole, the inferior temporal gyrus, and the floor of the middle fossa (b). (Artist: Winifred Hamilton, PhD, Baylor College of Medicine, Houston, TX. From Yoshor D, et al. [57] with permission from Elsevier)
Neocortical incisions for anterior temporal lobectomy and selective amygdalohippocampectomy. Conservative neocortical resection can be achieved by beginning the incision in the middle temporal gyrus parallel to the superior temporal sulcus (incision 1a). The cortical incision is directed slightly posteriorly and inferiorly until the temporal horn of the lateral ventricle is encountered. Alternatively, an incision can be made in the superior temporal gyrus (incision 1b) if language functional cortex is not present. The incision is carried back posteriorly for up to 5 or 6 cm, though the exact amount of neocortical removal is determined on a case-by-case basis. The vein of Labbe represents a firm posterior resection boundary and should always be preserved. Selective amygdalohippocampectomy preserves lateral neocortical structures and is most often performed through a middle or inferior temporal gyrus transcortical corridor (not shown) or via a trans-sulcal approach through the inferior temporal sulcus (incision 1c) (a). After entrance into the temporal horn of the lateral ventricle, the collateral eminence is identified just inferior and lateral to the hippocampus, and an incision is carried down from this landmark to the collateral sulcus (incision 2). This step completes the lateral neocortical resection (b). FG, fusiform gyrus; ITG, inferior temporal gyrus; MTG, middle temporal gyrus; PHG, parahippocampal gyrus; Ped., peduncle; STG, superior temporal gyrus; v., vein. (Artist: Winifred Hamilton, PhD, Baylor College of Medicine, Houston, TX. From Yoshor D, et al. [57] with permission from Elsevier)
After initial exposure, then next step is lateral temporal neocortical resection. This portion of surgery is typically performed under loupe magnification. Preservation of veins, namely, the large Sylvian veins and the vein of Labbe, is of utmost importance to prevent the development of venous infarct. The vein of Labbe runs 4–6 cm posterior to the temporal tip and demarks a posterior limit to resection. Resection is also limited posteriorly by the petrous ridge, but ideally should be only as large as needed to remove epileptogenic temporal neocortex and provide access to the hippocampus in the floor of the temporal horn of the lateral ventricle. To prevent postoperative language deficit, damage to the anterior superior temporal gyrus in the dominant hemisphere must be avoided. Additionally, branches of the middle cerebral artery that perfuse posterior temporal cortex can arise in the anterior Sylvian fissure and pass over the anterior 4 cm of STG and MTG. Damage to these vessels can also lead to language deficits and should be avoided.
The initial entry incision is made parallel to the superior temporal sulcus either in the MTG (Fig. 24.5a, incision 1a) or STG (Fig. 24.5b, incision 1b). The posterior border of the lateral neocortical resection is commonly 3–4 cm for dominant hemisphere and 4–5 cm for nondominant hemisphere resections, though this can be tailored based on the involvement of lateral neocortical structures in the SOZ as determined by the presurgical workup. If an MTG incision is used, dissection is directed orthogonally directly to the temporal horn of the lateral ventricle (Fig. 24.5b, incision 1a). For a STG incision, dissection must be directed slightly inferiorly toward the middle fossa floor to hit the temporal horn and avoid dissecting through the Sylvian fissure into the insula (Fig. 24.5b, incision 1b). Gray matter of the temporal operculum and cerebrospinal fluid (CSF) may be encountered at a depth of 1–2 cm as dissection is carried past the medial aspect of the Sylvian fissure en route to the temporal horn of the lateral ventricle. 2 to 5 cm posterior from the temporal tip, the superficial MTG or STG incision is redirected at a right angle, cutting across the MTG and ITG down to the middle fossa floor creating the posterior border of the lateral neocortical resection. This incision is dissected down, directed in a slightly posterior angle, until entrance into the temporal horn of the lateral ventricle at an average depth of 3–3.5 cm. Measuring this depth on preoperative MRI and using it as a reference during surgery is often helpful.
If difficulty is encountered in locating the temporal horn, frameless stereotaxy can be of use. Alternatively, a careful dissection guided by anatomy is at least as effective as computer-assisted navigation and is not limited by brain shift; the collateral fissure/sulcus can be located medial to the fusiform gyrus and then followed superiorly through the collateral eminence and into the temporal horn just lateral to the hippocampus.
After entering into the temporal horn, the initial STG or MTG incision parallel to the superior temporal sulcus can be carried anteriorly to the temporal tip, taking care to preserve any Sylvian veins draining into the sphenoparietal sinus. The collateral eminence, often seen as a bulge on the floor of the temporal horn running parallel and just lateral to the hippocampus, can then be incised and dissected down to the collateral fissure (Fig. 24.5b, incision 2). Subpial dissection down the collateral fissure on the side of the fusiform gyrus, carried from posterior to anterior, will end at the floor of the middle fossa completing the disconnection and allowing removal of the lateral temporal neocortex.
The microscope is then brought into position for resection of the mesial temporal structures. Traditionally retractors have been used to hold open the anterior portion of the temporal horn. However dynamic retraction with suction and bipolar can be utilized to prevent unnecessary tissue trauma. If retractors are used, it is imperative that the retractor placed on the remaining STG or Sylvian fissure (Fig. 24.6b, retractor R1) does not push too hard or too deep to cause injury to the underlying internal capsule, optic tract, or globus pallidus.
Removal of mesial temporal structures. After removal of lateral neocortical structures, the anterior choroidal point is identified, and the choroid plexus is elevated superiorly and medially. An incision is carried from the anterior choroidal point anteriorly through the amygdala in the direction of M1 (incision 3, panel b). Removal of amygdala superior to this plane endangers the basal ganglia. The inferolateral portion of the amygdala can then be removed (b). The fimbria and alveus are then disconnected and removed from the hippocampus (incision 4, panels a and c). Care is taken to preserve mesial pia in order to prevent entry into the ambient and crural cisterns in which travel delicate arterial and venous structures supplying the brainstem. The pia of the hippocampal fissure is identified, and hippocampal feeding arteries are divided freeing the hippocampus from its medial attachments (incision 5, panel a). Beginning at the floor of the middle fossa, subpial dissection of the parahippocampal gyrus is performed until the parahippocampal gyrus is freed from its inferior attachments at the inferior side of the hippocampal fissure (incision 6, panel a). AChA, anterior choroidal artery; C, tail of the caudate; GP, globus pallidus; IC, internal capsule; OT, optic tract; PCA, posterior cerebral artery; PHG, parahippocampal gyrus; P, putamen; THLV, temporal horn of the lateral ventricle; v., vein. (Artist: Winifred Hamilton, PhD, Baylor College of Medicine, Houston, TX. From Yoshor D, et al. [57] with permission from Elsevier)
First, we make an incision from the tip of the choroid fissure through the amygdala aiming toward the medial aspect of the greater wing of the sphenoid (Fig. 24.6b, incision 3). This incision is based on an imaginary line connecting the anterior choroidal point to the first segment of the middle cerebral artery (M1), defining the superior border of the amygdala resection. The anterior choroidal point (also referred to as inferior choroidal point or simply choroidal point) is defined as the anterior border of the choroid plexus, where the anterior choroidal artery enters the temporal horn of the lateral ventricle. An alternative landmark to M1 is the limen insulae, defined by the anterior border of the insula, at the lateral limit of the anterior perforating substance where the anterior and posterior stems of the lateral sulcus join. Venturing superior to this line endangers the basal ganglia and can lead to traveling up the temporal stem (see Fig. 24.5b, location of the basal ganglia up the temporal stem).
The amygdala can then be removed with subpial suction aspiration, taking care to preserve the pia overlaying the sphenoid and tentorium. It is imperative that this pial plane is preserved, as it serves as a protective border covering the tentorial incisura, beyond which lies the posterior cerebral artery (PCA), basal vein of Rosenthal, anterior choroidal artery (AChA), third and fourth cranial nerves, cerebral peduncle, optic tract, and brainstem. Removal of the amygdala reveals the pia medial to the parahippocampal cortex (Fig. 24.6a, c). The parahippocampal gyrus is then dissected medially in subpial fashion until the subiculum is reached (Fig. 24.6a, incision 6).
More posteriorly, the choroid is gently lifted medially to reveal the underlying choroidal fissure. Just lateral to the choroidal fissure, the fimbria and alveus are removed from the body of the hippocampus with gentle suction aspiration (Fig. 24.6a, c, incision 4) to reveal the edge of the hippocampal fissure (Figs. 24.6a and 24.7a). The hippocampal fissure is comprised of the union of a pia-arachnoid plane, on one side extending down from the choroidal fissure and on the other side extending up from the medial parahippocampal gyrus. The pia-arachnoid plane extending from the choroidal fissure into the hippocampal fissure often contains a 2–3 mm vein traveling to the hippocampus which must be coagulated and cut (Figs. 24.6a and 24.7a, incision 5), revealing the subiculum underneath. Importantly, posterior to this vein, arterial branches of the AChA anteriorly and PCA posteriorly run through the pia-arachnoid plane of the hippocampal fissure to supply the hippocampus. En passage vessels can also pass through the hippocampal fissure before returning to supply the posterior internal capsule. Arteries must be carefully inspected and en passage vessels preserved to prevent infarction of the posterior capsule and postoperative hemiplegia. Additionally, the course of the PCA may be variable. Occasionally the PCA can be found strongly attached to the subiculum. The PCA must therefore be identified anteriorly as it runs past the tentorial incisura. Its course can be tracked posteriorly prior to incising the subiculum (Fig. 24.7a, b).
Removal of the hippocampus. Arteries and veins traveling to the hippocampus within the hippocampal fissure are cut to detach the hippocampus (incision 5, panel a). Care is taken to preserve en passage vessels within the hippocampal fissure, as branches of the anterior choroidal artery and posterior cerebral artery may traverse the fissure en route to eloquent structures. After devascularization of the hippocampus, careful subpial dissection is used to free the subiculum and parahippocampal cortex from its mesial pia (incision 6, panel b). Finally, an incision is made roughly 3 cm posterior from the pes hippocampus through the tail of the hippocampus and the parahippocampal gyrus (incision 7, panel b). This allows for en bloc removal of the hippocampus and hippocampal gyrus (c). PCA, posterior cerebral artery; PHG, parahippocampal gyrus. (Artist: Winifred Hamilton, PhD, Baylor College of Medicine, Houston, TX. From Yoshor D, et al. [57] with permission from Elsevier)
The subpial dissection connecting the parahippocampal gyrus to the subiculum can then be continued medially to join the hippocampal fissure (Fig. 24.6a, incision 6). Proceeding in this manner allows for approaching the vessels in the hippocampal fissure from both superomedial and inferolateral angles in order to identify en passage vessels. Alternatively, the pia of the subiculum can be incised from superomedially (Fig. 24.7b, incision 6), which can then be carried subpially to connect with the subpial dissection of the medial parahippocampal cortex. An incision through the posterior hippocampus and parahippocampal gyrus is then made roughly 3 cm posterior to the head (pes) of the hippocampus (Fig. 24.7b, incision 7), usually corresponding to 1 cm posterior to the location of the vein traveling into the hippocampal fissure that was previously coagulated and cut. This maneuver frees the hippocampus and parahippocampal gyrus for en bloc removal (Fig. 24.7c). The remainder of the uncus can then be removed with subpial dissection and gentle suction, taking care to preserve small perforating arteries entering the brainstem from the underlying PCA, posterior communicating artery, and AChA. The pial plane covering the crural and ambient cisterns should not be bipolared. Remaining hippocampus can also be removed at this time with gentle suction, following the tail until it curves up and away from the operative field. The hippocampus should be removed posteriorly until at least the coronal plane in line with the lateral mesencephalic sulcus. The lateral geniculate nucleus can sometimes be viewed through the medial pia protecting the ambient cistern and can also serve as a posterior hippocampal resection marker.
Intraoperative recording of the hippocampus can be performed to guide resection. Aggressive resection of spike-generating areas in mesial temporal structures may lead to improved seizure freedom [57]; however this is not well proven and has generally fallen out of practice. If desired, hippocampal recordings are performed after lateral neocortical resection, prior to mesial temporal resection. A strip of four to six electrodes is to be placed through the temporal horn of the lateral ventricle directed posteriorly toward the occipital horn on the ventricular surface of the hippocampus. The use of intraoperative electrocorticography requires strict limitation of inhalational anesthetic use.
Bipolar electrocautery and oxidized regenerated cellulose are used to obtain hemostasis, and the cavity is filled with sterile saline prior to watertight closure of the dura. The bone flap is then replaced, antibiotic irrigation used, and the incision closed in layers.
Selective Amygdalohippocampectomy (SAHC) Procedure
The impetus for developing the selective amygdalohippocampectomy (SAHC) is twofold. First, a convergence of evidence from electrophysiologic, functional imaging, and animal models suggests that resection of mesial temporal structures alone can result in similar seizure outcomes. Second, sparing lateral neocortical structures might spare some of the postoperative neuropsychological deficits associated with ATL. ATL on the other hand allows for better visualization and en bloc resection of mesial temporal structures, as described above.
SAHC can be performed through a variety of approaches. It was first described more than half a century ago via a transcortical approach through the MTG [58]. Other approaches include transsylvian [59, 60] and infratemporal [61] approaches. There are advantages and disadvantages to each approach, but acceptable outcomes can be achieved with all [62]. Here we will briefly describe the transcortical approach, which remains the most popular today.
The patient is positioned similarly as for the ATL, supine and with a large bump allowing the head to be rotated 90 degrees away from the side of surgery, parallel to the floor. The head is placed in a three-point skull pin fixation device, and cranial navigation is used since the limited exposure of the surgery can easily lead to confusion between anatomic landmarks. A linear incision is used just anterior to the ear, running from the level of just superior to tragus, superiorly about 7 cm. The temporalis is incised linearly and retracted laterally, and then a craniotomy is performed roughly 4 cm in diameter. The dura is then opened and flapped inferiorly.
The initial incision for the transcortical approach can be made through the middle or inferior temporal gyrus, or through the inferior temporal sulcus (Fig. 24.5a, b, incision 1c). Bipolar electrocautery is used to create a 1.5–2 cm opening not more than 3.5 cm posterior to the temporal pole. This cortical or sulcal incision is carried down to the temporal horn of the lateral ventricle using cranial navigation as needed to direct the dissection. A self-retaining retractor is then used to maintain the cortical opening. Resection of the medial temporal structures follows a similar approach to those detailed above for ATL, with some distinctions aimed at maintaining “safe zones” to avoid disorientation. Part of the amygdala is first removed using a combination of electrocautery and suction. This removal is directed to exposing the pia overlying the medial floor of the middle fossa, picking up the pial plane as it travels off the middle fossa floor to protect the surgeon from more medial lying structures in the carotid, crural, and ambient cisterns. Subpial dissection is then continued posteriorly to remove the uncus, taking care to identify the tentorial incisura. Again, the medial pial plane must be carefully preserved to protect cranial nerves III and IV, the PCA and AChA, and the cerebral peduncle.
After removal of the uncus, the choroidal fissure is identified posteriorly within the temporal horn of the lateral ventricle. Again, this fissure marks the superior border of the resection to prevent damage to the optic tract and cerebral peduncle. The choroid can be swept superiorly, protected with a cottonoid and held in place with the tip of a retractor. Retraction posteriorly will reveal the pes hippocampus, and the hippocampus and fimbria are then mobilized off the choroidal fissure in the posterior direction. The posterior border of resection is defined by the plane of the tectal plate seen on neuronavigation, allowing for removal of approximately 2.5 cm of hippocampus. After reaching the posterior border and transecting the hippocampus in this plane, dissection is continued inferiorly from posterior to anterior, freeing the pes hippocampus from the parahippocampal gyrus. The hippocampus is now free except for its attachment on the pia-arachnoid plane of the hippocampal fissure. The hippocampus is freed from the hippocampal fissure in anterior to posterior direction, taking care to only divide arteries feeding the hippocampus and preserving the en passage vessels from AChA anteriorly and PCA posteriorly.
Outcomes for Resective Surgeries
The goal of resective surgery is seizure freedom. While outcomes for clinical trials of antiepileptic medications are often measured by the percent of patients achieving a meaningful reduction in seizure frequency (50% or greater reduction), outcomes for surgical treatment of epilepsy are held to a higher standard and graded using the Engel Classification of Postoperative Outcome (Table 24.1) [63] and/or the ILAE Postoperative Outcome Classification (Table 24.2) [64].
The first randomized controlled trial of ATL vs. continued medical management in MTLE showed 64% freedom from disabling seizures (58% when including all randomized for consideration for surgery) at 1 year after ATL compared to 8% after continued medical management [7]. The surgical group achieved 38% complete seizure freedom compared to only 3% in the medical group at 1 year. The surgery group also had significantly improved quality of life compared to the medically managed treatment arm. This trial confirmed the role of surgery in medically refractory epilepsy secondary to MTS and helped to popularize the surgery. At the time of publication in 2001, it was estimated that only about 2% of people eligible to undergo surgery for epilepsy actually underwent epilepsy surgery [65].
Additional studies and meta-analyses suggest that 60–90% of patients achieve Engel I outcome after ATL [7, 66,67,68,69,70,71,72,73] and that these outcomes are largely preserved after 5 years. Modern series achieving the highest rates of Engel I outcome after ATL place strong emphasis on the preoperative workup, reporting very high rates of concordance between semiology, MRI findings, and neuropsychological evaluations [73]. Engel I outcome rates of 70–80% can be considered a modern benchmark for seizure reduction after ATL.
Seizure reduction after SAHC is generally compared to outcomes for ATL. No randomized controlled trial comparing SAHC to ATL has been performed, and most single studies have small sample sizes suggesting equivalence or slight superiority of seizure reduction with ATL. A meta-analysis of papers comparing seizure freedom outcomes after ATL and SAHC showed an 8% increased occurrence of freedom from disabling seizures after ATL compared to SAHC [74]. This analysis of 11 studies comparing 1203 participants (620 ATL vs. 583 SAHC) stratified outcomes into freedom from disabling seizures (Engel I) vs. continued seizures (Engel II–IV). The 8% risk difference translates to a number needed to treat of 13 patients for 1 additional patient to achieve seizure freedom following ATL. The superiority of ATL compared to SAHC was maintained when the analysis was limited to only patients with MTS (n = 1092). The superiority of ATL to SAHC for seizure freedom has also been shown in other large meta-analyses [75].
Neuropsychological impairment can increase after ATL. Verbal memory impairment occurs in 25–50% of patients who undergo dominant right side ATL and 30% who undergo left side ATL [76]. Studies examining outcomes of both ATL and SAHC report no difference in verbal memory deficits between the two surgeries, reporting deficits in 40–50% of left-sided surgeries and 30% of right-sided surgeries [77, 78]. Patients at the highest risk for postoperative verbal memory impairment include those with a normal-appearing hippocampus and intact verbal memory on the dominant side, as well as patients with hippocampal sclerosis on the resection side but impaired memory function on the contralateral side. Other risk factors include very high preoperative verbal IQ and late age of epilepsy onset. Spatial memory tends to be more resilient compared to verbal memory after ATL, even when the nondominant hippocampus is resected.
Language deficits, particularly naming difficulty, can appear in up to 25% of patients following dominant side ATL [79]. These deficits can be permanent or transient. Other reports have shown improvement in naming and language corresponding to decrease in seizure frequency [80, 81]. Overall, postoperative language and naming deficits tend to be less severe and rarer compared to memory deficits.
The rationale behind performing SAHC stems from the idea that preservation of non-epileptic lateral temporal neocortex will prevent postoperative neuropsychological decline, specifically in regard to language and naming. Whether patients who undergo SAHC instead of ATL actually have better neuropsychological function remains a subject of debate; some studies show better functional outcomes after SAHC [82,83,84], while some show equivalence [77, 85]. Variability in neuropsychological batteries among studies has made large meta-analyses difficult.
Postoperative executive function outcomes are not as well defined as memory and language effects. Most studies suggest that executive function improves after surgery and that this improvement correlates closely with seizure reduction [86,87,88,89]. Overall, despite worsening in verbal memory, quality of life measures improve after ATL and SAHC, correlating closely with seizure freedom and reduction in disabling seizure frequency.
Both ATL and SAHC are safe surgeries. Major complications including death, hemiparesis, hemianopsia, and cranial nerve injury resulting in permanent deficit are rare (<1%). New postoperative contralateral superior quadrantanopsia is common and results from interruption of the optic radiations in Meyer’s loop as they travel over the temporal horn of the lateral ventricle. Quadrantanopsia occurs in up to 100% of some series but is generally clinically silent.
Psychiatric symptoms after ATL include worsening of depressive symptoms, new-onset depression [90, 91], and occasionally postoperative psychosis [92, 93]. Depression often occurs alongside MTLE [94]. Along with poor postoperative seizure control, depression is a risk factor for postoperative psychiatric symptoms [95].
Stereotactic Laser Amygdalohippocampotomy (SLAH)
Stereotactic laser amygdalohippocampotomy (SLAH) has recently been developed as a “minimally invasive” approach for destroying mesial temporal structures, gaining popularity over the past 5 years. Laser interstitial thermotherapy (LITT) is a thermoablative technique with growing applications, thanks to advances in magnetic resonance thermography allowing real-time monitoring of changes in temperature. Stereotactic laser amygdalohippocampotomy (stereotactic laser amygdalohippocampectomy is also used interchangeably in literature) is a technique for the treatment of mesial temporal lobe epilepsy in which a laser probe heats the surrounding tissue causing a permanent lesion. Technical details and general principles of LITT are reviewed in Chap. 16.
Stereotactic Laser Amygdalohippocampotomy Procedure
For mesial temporal epilepsy, the procedure is performed after a standard workup as done for ATL or SAHC. The laser fiber assembly is placed using whichever stereotactic platform the surgeon prefers, including standard skull-mounted frame, robotic system, or frameless system. There are currently two commercially available LITT systems: Visualase Thermal Therapy System (Medtronic, Minneapolis, MN, USA) and NeuroBlate Laser Ablation System (Monteris, Plymouth, MN, USA). The details below describe use of the former system.
The trajectory of the laser fiber is along the long axis of the amygdalohippocampal complex beginning from an occipital entry point (Fig. 24.8a). The entry point is chosen to enable safe entry to the pial surface of an occipital gyrus, avoiding vasculature as visualized using a contrast-enhanced MRI. The occipital horn should also be avoided when possible to prevent deflection of the laser cannula off the ependymal surface. Besides standard stereotactic concerns such as vessel avoidance, an additional consideration for these procedures is planning for thermal spread. Heat sinks, including the temporal horn and basal cisterns, prevent heat spread into those structures and limit thermal damage in those directions.
Stereotactic laser amygdalohippocampotomy procedure. The laser cannula trajectory is planned with the laser entering in the occipital lobe and traveling down the long axis of the amygdalohippocampal complex (a). The laser fiber assembly is then placed under stereotactic guidance (b). The patient is transported to MRI to obtain multiplanar cuts of the laser fiber assembly. This confirms proper placement and defines planes for temperature monitoring (c). Ablation is performed under real-time MR thermography monitoring. Composite irreversible damage zones (orange) represent the location of the final lesion. The laser is pulled back 2 times in order to extend the length of the ablation down the long axis of the hippocampus (d). A T1-weighted post-contrast MRI is obtained to document the ablation volume and check for intracranial hemorrhage (e). (From Youngerman BE, et al. [96]. Reprinted with permission from John Wiley and Sons)
The patient is positioned according to the stereotactic system used. Some use a supine positioned with a head turn, others supine beach-chair with neck flexed (semi-slouched), and yet others a prone position. We use a semi-slouched position with a stereotactic robotic system. After prep and drape of a small region around the planned entry point, a 4 mm stab incision is made, and a 3.2 mm burr hole is drilled along the planned trajectory. We use a titanium anchor bolt affixed with a T-handle wrench to maintain the trajectory. If needed, we pass monopolar cautery through a coated probe to open the dura. We measure and calculate the distance to the planned target from the bolt and pass a guide rod down the trajectory to create a path to target. The 1.6 mm laser cannula is then placed through the anchor bolt along the trajectory to the distal (closest to temporal pole) part of the planned ablation volume. A laser with 10 mm diffuser tip is then placed into the laser cannula (Fig. 24.8b).
After locking the laser catheter in place with the skull anchor bolt, the patient is transferred to the MRI scanner, and the catheter is visualized with a volumetric scan (Fig. 24.8c). The scanner is configured to visualize the catheter trajectory in one, two, or three orthogonal planes. The addition of more planes adds time to each thermal image acquisition. We usually use two planes, axial and sagittal. Low-temperature (usually 45–50 C) and high-temperature (usually 90 C) safety points are selected. The low limit is placed near structures at risk such that the laser automatically shuts off before heating those structures beyond the point of irreversible cell death. The high-temperature limit prevents tissue from reaching evaporation temperatures and releasing gas.
Temperature is monitored using fast spoiled gradient-recalled echo at several second intervals (usually 3–8 seconds depending on how many planes are acquired, as mentioned above) to map irreversible and cumulative damage zones (Fig. 24.8d). The most distal ablation volume is performed first, so that subsequent ablations can be achieved by incrementally withdrawing the laser catheter along the trajectory. After ablation of the first volume, the laser cannula is withdrawn in approximately 1 cm increments to perform subsequent ablations. Three to five serial ablations are usually required along the trajectory of the laser to complete the lesion [96]. The posterior extent of the ablation is typically the coronal plane of the lateral mesencephalic sulcus or quadrigeminal plate. Post-ablation T1 post-contrast and diffusion-weighted MRI sequences are obtained to document ablation volume (Fig. 24.8e). The presence of hemorrhage can be assessed with a fast field echo (FFE) or gradient echo sequence. After completion of the ablation, the laser cannula and anchor bolt are removed, and the stab incision is closed with a suture or staple. Most patients can be discharged from the hospital on postoperative day 1.
Both seizure freedom outcomes and operative morbidity are influenced by ablation geometry and extent [97,98,99]. A recent multicenter study suggests that extent of ablation of the anterior, inferior, and medial structures of the temporal lobe play the largest role in determining seizure freedom [100]. Increasing amygdala ablation volume correlated with improved seizure freedom, as did the inclusion of the hippocampal head, parahippocampal gyrus, and entorhinal and perirhinal cortices. In contrast, ablation of the hippocampal body and tail posteriorly, beyond a coronal plane at the level of the lateral mesencephalic sulcus, was associated with poorer epilepsy control outcomes. Posterior hippocampal ablation likely led to worse outcomes because of the curvature of the amygdalohippocampal complex. A straight laser cannula generally does not allow for both the ablation of the anterior inferior medial structures and the posterior hippocampal body and tail in one trajectory. Failure to ablate enough amygdala is a common pitfall leading to poor postoperative seizure control. Most centers perform the ablation with one laser; however some centers elect to use two laser trajectories in cases of severe mesial temporal sclerosis where a sharp curvature of the amygdala medially from the trajectory of the hippocampus does not allow for ablation of the necessary volumes of both the hippocampus and amygdala.
Importantly, the ablation trajectory must avoid straying too anteriorly putting the trigeminal nerve at risk as it enters Meckel’s cave. A superior ablation trajectory, above the level of the choroidal fissure, can cause visual deficit after damage to the optic tract. A more posterior ablation can cause a contralateral superior quadrantanopsia via damage to the optic radiations [101] or contralateral homonymous hemianopsia due to damage to the lateral geniculate body.
Outcomes After Stereotactic Laser Amygdalohippocampotomy
Multiple single-institution series of SLAH suggest that seizure freedom rates are approximately 55–60% (reports range from 38% to 78%) at 1 year after ablation [96, 98,99,100, 102,103,104,105,106,107]. These rates improve to 60–89% in patients with radiographic evidence of hippocampal sclerosis. The largest series to date, a multicenter retrospective cohort study of 234 patients who underwent SLAH for MTLE, reported Engel I outcomes in 58% at 1 year and 57.5% at 2 years [100]. This study showed Engel I or II outcomes in 77.1% and 80.2% at 1 and 2 years, respectively. The presence or absence of radiographic hippocampal sclerosis did not impact outcome, but patients with focal to bilateral tonic-clonic seizures were less likely to achieve Engel I outcomes [96].
Overall complication rates occur in approximately 15–20% of cases [100, 104, 108]. Radiographic rates of hemorrhage are approximately 1–2%, with less than 1% resulting in permanent neurologic injury. Visual complications including quadrantanopsias or cranial nerve III or IV deficits occur in approximately 5% of procedures.
Neurocognitive outcomes have also been reported in many of these series; however definitive outcomes are difficult to generalize due to the small number of patients in each study and the range of different neurocognitive measures used. As with SAHC, SLAH spares lateral neocortical structures. Preliminary direct comparisons of SLAH and ATL suggest that postoperative decline in object recognition and naming are less for SLAH compared to ATL [109]. Surprisingly, selective outcomes suggest that some aspects of verbal memory are spared even with ablation of language-dominant mesial temporal structures. However, the exact nature of the neurocognitive effect (e.g., naming, fluency, verbal memory, learning) varies from series to series. Some, for example, report preservation of verbal memory with decline of learning [108], while others report relative preservation of learning but decline in memory [103]. Larger studies with consistent neurocognitive testing are needed to clarify the neurocognitive effects of SLAH.
To better characterize the efficacy and side effect profile of SLAH, the Stereotactic Laser Ablation for Temporal Lobe Epilepsy (SLATE) study is an industry-sponsored prospective open-label trial of MRI-guided laser ablation using the Visualase system that is currently enrolling. The trial is scheduled to complete in 2022 after enrolling 150 patients. Endpoints including seizure freedom, adverse events, quality of life, and neuropsychological outcomes will be assessed at 12 months [110].
Considering the body of available early data, SLAH appears to be a safe and less invasive approach to the treatment of MTLE in patients with or without mesial temporal sclerosis. SLAH seems to have lower rates of seizure control compared to open surgery (ATL and SAHC). However, the morbidity of SLAH appears to be lower than open surgery. Additionally, the neurocognitive deficits after SLAH may be milder compared to open surgery. The results of the SLATE study will allow for a more definitive comparison of surgical approaches in the future.
Other Procedures
While resection of mesial temporal structures remains the gold standard surgical treatment of MTLE, and ablation continues to gain traction, a number of alternatives are available. Stereotactic radiosurgery has been under investigation and may provide an alternative for patients unable to undergo surgical treatment. Additionally, multiple neuromodulation alternatives are now FDA approved in the United States for treatment of medically refractory epilepsy. These neuromodulation approaches are increasingly used in patients who continue to have disabling seizures despite mesial temporal resection, patients with bilateral mesial temporal epilepsy, and patients who may not be candidates for resective surgery. Finally, hippocampal transection, a surgical technique that attempts to disconnect mesial structures to stop spread of seizures while largely maintaining those mesial structures, was developed as an approach to avoid postoperative cognitive deficit, but has largely been supplanted by ablative and/or neuromodulatory approaches and will not be discussed further.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) can be used as a nonsurgical alternative for the treatment of MTLE caused by mesial temporal sclerosis. Several pilot studies showed remission rates ranging from 47% to 85% after marginal radiation doses ranging from 20 to 29 Gy [111,112,113,114], with safety profiles comparable to anterior temporal lobectomy. Specifically, promising verbal memory outcomes were initially demonstrated and were one initial driver for adoption of SRS [115]. However, seizure remission after SRS is delayed as radiation effects take time, and outcomes were seen gradually over 12–24 months after SRS. Moreover, seizures sometimes get worse before they get better secondary to irritative effects of radiation.
The Radiosurgery versus Open Surgery for Mesial Temporal Lobe Epilepsy (ROSE) trial [116], a multicenter randomized controlled trial comparing 24 Gy SRS versus ATL for medically refractory unilateral mesial temporal lobe epilepsy, failed to show non-inferiority of SRS compared to ATL at 3-year follow-up. The primary outcome of seizure remission rate, defined as freedom from seizures causing impairment of consciousness between months 25 and 36 after treatment, was 52% for SRS (n = 31) compared to 78% for ATL (n = 27). The trial demonstrated immediate efficacy and durability for ATL, with 81% seizure freedom by 3 months maintained at 85% seizure freedom during the final 3-month block (33–36 months after surgery). For SRS, seizure freedom during the first 3 months was only 6%, rising gradually over time to 74% during the last 3-month study period (33–36 months after SRS), re-demonstrating the delayed efficacy of SRS. Neurocognitive outcomes were roughly comparable between the SRS and ATL arms. Importantly, verbal memory outcomes were not statistically different between treatment arms, and overall quality of life outcomes correlated with seizure remission, and therefore quality of life improvement was delayed in the SRS arm compared to the ATL arm. The ROSE trial suggests that ATL should remain the gold standard for treatment of medially refractory MTLE, with SRS a possible alternative in patients unable to tolerate surgery.
Neuromodulation
Neuromodulation for epilepsy is discussed in detail in Chap. 27. Here we present a short summary of neuromodulation specifically for MTLE. Presently, there are three categories of neuromodulation for epilepsy: vagus nerve stimulation (VNS), deep brain stimulation (DBS) of the anterior nucleus of the thalamus, and responsive neurostimulation (RNS). All three of these modalities can be applied to refractory MTLE.
VNS has been approved since 1997 for the treatment of drug-resistant focal epilepsy. VNS is not a first-line treatment for drug-resistant MTLE. However, it can be used in populations of patients with unilateral MTLE unable to undergo mesial temporal resection or ablation, patients with unilateral MTLE who continue to have seizures after ATL or SAHC, or patients with MTLE of bilateral onset. Exact rates of response in this specific population are difficult to determine from the literature, but roughly 50% of patients with focal epilepsy will achieve a decrease of 50% or more in seizure frequency at 1 and 2 years after VNS implantation [117]. When compared to resection, however, these rates are notably inferior, as they are equivalent to an Engel III outcome. This comparison highlights the preference of resection over neuromodulation for those who are candidates.
DBS of the anterior nucleus of the thalamus (ANT) was approved in the United States in 2018 after the Stimulation of the Anterior Nucleus of the Thalamus for Epilepsy (SANTE) trial [118], a multicenter, double-blind randomized trial for focal epilepsy, and 5-year follow-up [119] showed promising results. The ANT is intimately associated with the mesial temporal structures through the medial limbic (Papez) circuit. Efferent projections to the ANT arise from the subiculum and CA1, reaching the ANT through the postcommissural fornix or via the mammillary bodies and mammillothalamic tract. The ANT also sends afferent projections directly and indirectly to the parahippocampal gyrus and hippocampus, leading to a complex network of direct and indirect thalamic-to-mesial cortical loops [120].
The SANTE trial and long-term follow-up reported a median reduction in seizures of 44% at 1 year and 76% at 5 years for the subgroup of patients with seizures of temporal lobe origin. These results appear better than those for VNS, but again, notably worse than those for resective surgery, as the rate of seizure freedom (Engel I) was very low. While median reduction in seizure frequency was greater compared to placebo, response rate (>50% decrease in seizure frequency) was not significantly different compared to placebo (34% active vs. 25% sham, p > 0.05) during the 3-month blinded phase. Patients with a history of prior resective surgery had median seizure reductions of 53% at 1 year and 67% at 5 years. Importantly, both the populations of participants with temporal epilepsy and the population of participants who underwent prior resective surgery contained participants with non-MTLE epilepsies; however these results serve as guidance for subjects with MTLE for future study. Morbidity of ANT DBS include infection (10%), lead misplacement (8%), depression (37%), and memory impairment (27%) [119]. Importantly, the efficacy of DBS appears to increase with time and will hopefully get better as refinements are made in lead placement and stimulation parameters.
The RNS system (NeuroPace Inc., Mountain View, CA) is another neuromodulation alternative for patients with MTLE unable to undergo resective or ablative procedures. In contrast to ANT DBS, which is an open-loop stimulation paradigm applying a constant prescribed dose of stimulation, the RNS system employs a closed-loop paradigm in which brain activity is recorded, and stimulation only occurs if the device detects activity suggestive of an oncoming seizure.
RNS leads for MTLE are most often placed down the long axis of the amygdalohippocampal complex unilaterally or bilaterally. Additional subtemporal strips can be placed, also unilaterally or bilaterally. Only two leads can be connected to the stimulation device in the current version of the system. To date, the strongest data for the use of RNS for MTLE comes from a prospective trial of 111 subjects with MTLE [121]. Seventy-two percent of the subjects had bilateral MTLE, with the remaining 28% with unilateral onset. Twelve percent of these subjects had failed temporal lobectomy. At 6 years, disabling seizures were reduced by median 67%, and 65% of subjects had at least a 50% decrease in seizure frequency (Engel III). During the open-label period, 45% of subjects had seizure-free periods of over 3 months, and 15% had seizure-free periods of at least 1 year (Engel I). No differences were seen between subjects with bilateral vs. unilateral onset, or subjects who had previously undergone resective surgery vs. surgerically naïve subjects. There was also not a statistically significant difference between subjects with depth electrodes in the hippocampus and those with depth electrodes outside placed more laterally outside the hippocampus, although there was a trend toward better seizure control with hippocampal stimulation electrodes. Side effects included implant-site infection (12%) involving superficial soft tissue and necessitating device explant, device lead damage (6%), intracranial hemorrhage (3%), photopsia (14%), transient memory impairment (6%), and depression (5%). As with DBS, seizure control with RNS improves over time after implantation [122] and will likely continue to improve as lead placement and stimulation parameters continue to be refined.
While neuromodulation approaches are becoming increasingly common, they should not be considered replacements for ATL or SAHC. The rates of seizure freedom are significantly higher for ATL and SAHC compared to RNS or ANT DBS. As such, neuromodulation should be reserved for patients who are not candidates for ATL/SAHC, or for patients who have already undergone resective surgery but continue to have uncontrolled seizures.
Conclusions
Mesial temporal lobe epilepsy is a common focal epilepsy syndrome that can be amenable to surgery in properly selected patients. Patient selection is of utmost importance and requires extensive presurgical evaluation by a multidisciplinary team. Anterior temporal resection remains the gold standard operation, achieving freedom from disabling seizures in 70–80% of patients. Selective amygdalohippocampectomy remains a reasonable alternative, though rates of seizure freedom are slightly lower with an unclear neurocognitive advantage over anterior temporal lobectomy. Stereotactic laser ablation is a new less invasive technique that has the potential to achieve similar outcomes to selective amygdalohippocampectomy. Results of the ongoing trials should help clarify the efficacy and neurocognitive effect of laser ablation. Responsive neurostimulation and anterior nucleus of the thalamus deep brain stimulation are new tools for patients unable to undergo resective surgery and offer an option for patients with bilateral onset mesial temporal epilepsy. Surgical treatments of mesial temporal epilepsy have evolved rapidly over the past two decades, and active research continues to push the boundary forward.
Abbreviations
- AChA:
-
Anterior choroidal artery
- AED:
-
Antiepileptic drug
- ANT:
-
Anterior nucleus of the thalamus
- ATL:
-
Anterior temporal lobectomy
- C:
-
Caudate
- CSF:
-
Cerebrospinal fluid
- DBS:
-
Deep brain stimulation
- EEG:
-
Electroencephalogram
- EMU:
-
Epilepsy monitoring unit
- FDG:
-
Fludeoxyglucose
- HMPAO:
-
Hexamethylpropyleneamine oxime
- IC:
-
Internal capsule
- ITG:
-
Inferior temporal gyrus
- LITT:
-
Laser interstitial thermal therapy
- MEG:
-
Magnetoencephalography
- MTLE:
-
Mesial temporal lobe epilepsy
- MTG:
-
Middle temporal gyrus
- OT:
-
Optic tract
- P:
-
Putamen
- PCA:
-
Posterior cerebral artery
- PET:
-
Positron emission tomography
- PHG:
-
Parahippocampal gyrus
- RNS:
-
Responsive neurostimulation
- SAHC:
-
Selective amygdalohippocampectomy
- sEEG:
-
Stereoelectroencephalography
- SLAH:
-
Stereotactic laser amygdalohippocampotomy
- SOZ:
-
Seizure onset zone
- SPECT:
-
Single-photon emission computerized tomography
- SRS:
-
Stereotactic radiosurgery
- STG:
-
Superior temporal gyrus
- SUB:
-
Subiculum
- Tc-99m:
-
Technetium-99m
- THLV:
-
Temporal horn of the lateral ventricle
- VNS:
-
Vagus nerve stimulation
References
Cockerell OC, Johnson AL, Sander JW, Hart YM, Shorvon SD. Remission of epilepsy: results from the National General Practice Study of Epilepsy. Lancet. 1995;346(8968):140–4.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Mohanraj R, Brodie MJ. Diagnosing refractory epilepsy: response to sequential treatment schedules. Eur J Neurol. 2006;13(3):277–82.
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 2009;51(6):1069–77.
Stone JL, Jensen RL. Benjamin Winslow Dudley and Early American trephination for posttraumatic epilepsy. Neurosurgery. 1997;41(1):263–8.
Patchell RA, Young AB, Tibbs PA. Classics in neurology. Benjamin Winslow Dudley and the surgical treatment of epilepsy. Neurology. 1987;37(2):290–1.
Wiebe S, Blume WT, Girvin JP, Eliasziw M, Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001;345(5):311–8.
Englot DJ, Ouyang D, Garcia PA, Barbaro NM, Chang EF. Epilepsy surgery trends in the United States, 1990–2008. Neurology. 2012;78(16):1200–6.
Wiebe S, Gafni A, Blume WT, Girvin JP. An economic evaluation of surgery for temporal lobe epilepsy. J Epilepsy. 1995;8(3):227–35.
Picot M-C, Neveu D, Kahane P, Crespel A, Gélisse P, Hirsch E, et al. Cost-effectiveness of epilepsy surgery in a cohort of patients with medically intractable partial epilepsy – preliminary results. Rev Neurol (Paris). 2004;160 Spec N:5S354–67.
Widjaja E, Li B, Schinkel CD, Ritchie LP, Weaver J, Snead OC, et al. Cost-effectiveness of pediatric epilepsy surgery compared to medical treatment in children with intractable epilepsy. Epilepsy Res. 2011;94(1–2):61–8.
York MK, Rettig GM, Grossman RG, Hamilton WJ, Armstrong DD, Levin HS, et al. Seizure control and cognitive outcome after temporal lobectomy: a comparison of classic Ammon’s horn sclerosis, atypical mesial temporal sclerosis, and tumoral pathologies. Epilepsia. 2003;44(3):387–98.
Armstrong DD. The neuropathology of temporal lobe epilepsy. J Neuropathol Exp Neurol. 1993;52(5):433–43.
Osborn AG, Hedlund GL, Salzman KL. Osborn’s brain. 2nd ed. Philadelphia: Elsevier; 2017.
Wen HT, Rhoton AL, de Oliveira E, Cardoso ACC, Tedeschi H, Baccanelli M, et al. Microsurgical anatomy of the temporal lobe: part 1: mesial temporal lobe anatomy and its vascular relationships as applied to amygdalohippocampectomy. Neurosurgery. 1999;45(3):549–92.
Wen HT, Rhoton AL, de Oliveira E, Castro LHM, Figueiredo EG, Teixeira MJ. Microsurgical anatomy of the temporal lobe: part 2: Sylvian fissure region and its clinical application. Neurosurgery 2009;65(6 Suppl):1–35.
Kucukyuruk B, Richardson RM, Wen HT, Fernandez-Miranda JC, Rhoton AL. Microsurgical anatomy of the temporal lobe and its implications on temporal lobe epilepsy surgery. Epilepsy Res Treat. 2012;2012:1–17.
Kahane P, Bartolomei F. Temporal lobe epilepsy and hippocampal sclerosis: lessons from depth EEG recordings. Epilepsia. 2010;51:59–62.
Chabardès S, Kahane P, Minotti L, Tassi L, Grand S, Hoffmann D, et al. The temporopolar cortex plays a pivotal role in temporal lobe seizures. Brain. 2005;128(8):1818–31.
Bartolomei F, Wendling F, Vignal JP, Kochen S, Bellanger JJ, Badier JM, et al. Seizures of temporal lobe epilepsy: identification of subtypes by coherence analysis using stereo-electro-encephalography. Clin Neurophysiol. 1999;110(10):1741–54.
Maillard L, Vignal J-P, Gavaret M, Guye M, Biraben A, McGonigal A, et al. Semiologic and electrophysiologic correlations in temporal lobe seizure subtypes. Epilepsia. 2004;45(12):1590–9.
Arzimanoglou A, Kahane P. The ictal onset zone: general principles, pitfalls and caveats. In: Lüders HO, editor. Textbook of epilepsy surgery. London: Informa Healthcare; 2008. p. 597–602.
Barba C, Barbati G, Minotti L, Hoffmann D, Kahane P. Ictal clinical and scalp-EEG findings differentiating temporal lobe epilepsies from temporal “plus” epilepsies. Brain. 2007;130(7):1957–67.
Benbadis SR, O’Neill E, Tatum WO, Heriaud L. Outcome of prolonged video-EEG monitoring at a typical referral epilepsy center. Epilepsia. 2004;45(9):1150–3.
Dericioglu N, Saygi S. Ictal scalp EEG findings in patients with mesial temporal lobe epilepsy. Clin EEG Neurosci. 2008;39(1):20–7.
Feldman RE, Delman BN, Pawha PS, Dyvorne H, Rutland JW, Yoo J, et al. 7T MRI in epilepsy patients with previously normal clinical MRI exams compared against healthy controls. Bernhardt BC, editor. PLoS One. 2019;14(3):e0213642.
Varghese GI, Purcaro MJ, Motelow JE, Enev M, McNally KA, Levin AR, et al. Clinical use of ictal SPECT in secondarily generalized tonic-clonic seizures. Brain. 2009;132(Pt 8):2102–13.
Zhao F, Kang H, You L, Rastogi P, Venkatesh D, Chandra M. Neuropsychological deficits in temporal lobe epilepsy: a comprehensive review. Ann Indian Acad Neurol. 2014;17(4):374–82.
Black LC, Schefft BK, Howe SR, Szaflarski JP, Yeh H, Privitera MD. The effect of seizures on working memory and executive functioning performance. Epilepsy Behav. 2010;17(3):412–9.
Wagner DD, Sziklas V, Garver KE, Jones-Gotman M. Material-specific lateralization of working memory in the medial temporal lobe. Neuropsychologia. 2009;47(1):112–22.
Düzel E, Hufnagel A, Helmstaedter C, Elger C. Verbal working memory components can be selectively influenced by transcranial magnetic stimulation in patients with left temporal lobe epilepsy. Neuropsychologia. 1996;34(8):775–83.
Abrahams S, Morris RG, Polkey CE, Jarosz JM, Cox TCS, Graves M, et al. Hippocampal involvement in spatial and working memory: a structural MRI analysis of patients with unilateral mesial temporal lobe sclerosis. Brain Cogn. 1999;41(1):39–65.
Kapur N, Millar J, Colbourn C, Abbott P, Kennedy P, Docherty T. Very long-term amnesia in association with temporal lobe epilepsy: evidence for multiple-stage consolidation processes. Brain Cogn. 1997;35(1):58–70.
Blake RV, Wroe SJ, Breen EK, McCarthy RA. Accelerated forgetting in patients with epilepsy: evidence for an impairment in memory consolidation. Brain. 2000;123(3):472–83.
Butler CR, Zeman AZ. Recent insights into the impairment of memory in epilepsy: transient epileptic amnesia, accelerated long-term forgetting and remote memory impairment. Brain. 2008;131(9):2243–63.
Tramoni E, Felician O, Barbeau EJ, Guedj E, Guye M, Bartolomei F, et al. Long-term consolidation of declarative memory: insight from temporal lobe epilepsy. Brain. 2011;134(3):816–31.
Kim C-H, Lee S-A, Yoo H-J, Kang J-K, Lee J-K. Executive performance on the Wisconsin card sorting test in mesial temporal lobe epilepsy. Eur Neurol. 2007;57(1):39–46.
Horner MD, Flashman LA, Freides D, Epstein CM, Bakay RAE. Temporal lobe epilepsy and performance on the Wisconsin card sorting test. J Clin Exp Neuropsychol. 1996;18(2):310–3.
Oyegbile TO, Dow C, Jones J, Bell B, Rutecki P, Sheth R, et al. The nature and course of neuropsychological morbidity in chronic temporal lobe epilepsy. Neurology. 2004;62(10):1736–42.
Hermann B, Seidenberg M, Lee E-J, Chan F, Rutecki P. Cognitive phenotypes in temporal lobe epilepsy. J Int Neuropsychol Soc. 2007;13(01):12–20.
Labudda K, Frigge K, Horstmann S, Aengenendt J, Woermann FG, Ebner A, et al. Decision making in patients with temporal lobe epilepsy. Neuropsychologia. 2009;47(1):50–8.
McDonald CR, Delis DC, Norman MA, Tecoma ES, Iragui VJ. Discriminating patients with frontal-lobe epilepsy and temporal-lobe epilepsy: utility of a multilevel design fluency test. Neuropsychology. 2005;19(6):806–13.
Bell BD, Seidenberg M, Hermann BP, Douville K. Visual and auditory naming in patients with left or bilateral temporal lobe epilepsy. Epilepsy Res. 2003;55(1–2):29–37.
Loring DW, Meador KJ, Lee GP. Effects of temporal lobectomy on generative fluency and other language functions. Arch Clin Neuropsychol. 1994;9(3):229–38.
Mayeux R, Brandt J, Rosen J, Benson DF. Interictal memory and language impairment in temporal lobe epilepsy. Neurology. 1980;30(2):120–5.
Hamberger MJ, Seidel WT. Auditory and visual naming tests: normative and patient data for accuracy, response time, and tip-of-the-tongue. J Int Neuropsychol Soc. 2003;9(3):479–89.
Hamberger MJ, Tamny TR. Auditory naming and temporal lobe epilepsy. Epilepsy Res. 1999;35(3):229–43.
Price CJ, Devlin JT, Moore CJ, Morton C, Laird AR. Meta-analyses of object naming: effect of baseline. Hum Brain Mapp. 2005;25(1):70–82.
Damasio H, Tranel D, Grabowski T, Adolphs R, Damasio A. Neural systems behind word and concept retrieval. Cognition. 2004;92(1–2):179–229.
Hamberger MJ, McClelland S, McKhann GM, Williams AC, Goodman RR. Distribution of auditory and visual naming sites in nonlesional temporal lobe epilepsy patients and patients with space-occupying temporal lobe lesions. Epilepsia. 2007;48(3):531–8.
Hamberger MJ, Seidel WT, Goodman RR, Perrine K, McKhann GM. Temporal lobe stimulation reveals anatomic distinction between auditory naming processes. Neurology. 2003;60(9):1478–83.
Binder JR. Functional MRI is a valid noninvasive alternative to Wada testing. Epilepsy Behav. 2011;20(2):214–22.
Diehl B, Lüders HO. Temporal lobe epilepsy: when are invasive recordings needed? Epilepsia. 2000;41(Suppl 3):S61–74.
Jooma R, Yeh HS, Privitera MD, Gartner M. Lesionectomy versus electrophysiologically guided resection for temporal lobe tumors manifesting with complex partial seizures. J Neurosurg. 1995;83(2):231–6.
Cascino GD, Kelly PJ, Sharbrough FW, Hulihan JF, Hirschorn KA, Trenerry MR. Long-term follow-up of stereotactic lesionectomy in partial epilepsy: predictive factors and electroencephalographic results. Epilepsia. 1992;33(4):639–44.
Ward MM, Barbaro NM, Laxer KD, Rampil IJ. Preoperative valproate administration does not increase blood loss during temporal lobectomy. Epilepsia. 1996;37(1):98–101.
Yoshor D, Hamilton WJ, Grossman RG. Temporal lobe operations for drug-resistant epilepsy. In: Schmidek HH, Roberts DW, editors. Schmidek and Sweet’s operative neurosurgical techniques: indications, methods, and results. 5th ed. Philadelphia: Saunders Elsevier Inc; 2006. p. 1383–93.
Niemeyer P. The transventricular amygdalohippocampectomy in temporal lobe epilepsy. In: Baldwin M, Bailey P, editors. Temporal lobe epilepsy. Springfield: Charles C. Thomas; 1958. p. 461–82.
Wieser HG, Yaşargil MG. Selective amygdalohippocampectomy as a surgical treatment of mesiobasal limbic epilepsy. Surg Neurol. 1982;17(6):445–57.
Yaşargil MG, Wieser HG, Valavanis A, von Ammon K, Roth P. Surgery and results of selective amygdala-hippocampectomy in one hundred patients with nonlesional limbic epilepsy. Neurosurg Clin N Am. 1993;4(2):243–61.
Park TS, Bourgeois BFD, Silbergeld DL, Dodson WE. Subtemporal transparahippocampal amygdalohippocampectomy for surgical treatment of mesial temporal lobe epilepsy. J Neurosurg. 1996;85(6):1172–6.
Hoyt AT, Smith KA. Selective Amygdalohippocampectomy. Neurosurg Clin N Am. 2016;27(1):1–17.
Engel J, Van Ness PC, Rasmussen T, Ojemann L. Outcome with respect to epileptic seizures. In: Engel J, editor. Surgical treatment of the epilepsies. New York: Raven Press; 1993. p. 609–21.
Wieser HG, Blume WT, Fish D, Goldensohn E, Hufnagel A, King D, et al. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia. 2008;42(2):282–6.
Engel J Jr. A greater role for surgical treatment of epilepsy: why and when? Epilepsy Curr. 2003;3(2):37–40.
Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Shinnar S, et al. Initial outcomes in the Multicenter Study of Epilepsy Surgery. Neurology. 2003;61(12):1680–5.
Sperling MR, O’Connor MJ, Saykin AJ, Plummer C. Temporal lobectomy for refractory epilepsy. JAMA. 1996;276(6):470–5.
Wyler AR, Hermann BP, Somes G. Extent of medial temporal resection on outcome from anterior temporal lobectomy: a randomized prospective study. Neurosurgery. 1995;37(5):982–90; discussion 990–1.
Engel J, Wiebe S, French J, Sperling M, Williamson P, Spencer D, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in Association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology. 2003;60(4):538–47.
Cohen-Gadol AA, Wilhelmi BG, Collignon F, White JB, Britton JW, Cambier DM, et al. Long-term outcome of epilepsy surgery among 399 patients with nonlesional seizure foci including mesial temporal lobe sclerosis. J Neurosurg. 2006;104(4):513–24.
Elsharkawy AE, Alabbasi AH, Pannek H, Oppel F, Schulz R, Hoppe M, et al. Long-term outcome after temporal lobe epilepsy surgery in 434 consecutive adult patients. J Neurosurg. 2009;110(6):1135–46.
Schramm J, Lehmann TN, Zentner J, Mueller CA, Scorzin J, Fimmers R, et al. Randomized controlled trial of 2.5-cm versus 3.5-cm mesial temporal resection in temporal lobe epilepsy—part 1: intent-to-treat analysis. Acta Neurochir. 2011;153(2):209–19.
Elliott RE, Bollo RJ, Berliner JL, Silverberg A, Carlson C, Geller EB, et al. Anterior temporal lobectomy with amygdalohippocampectomy for mesial temporal sclerosis: predictors of long-term seizure control. J Neurosurg. 2013;119(2):261–72.
Josephson CB, Dykeman J, Fiest KM, Liu X, Sadler RM, Jette N, et al. Systematic review and meta-analysis of standard vs selective temporal lobe epilepsy surgery. Neurology. 2013;80(18):1669–76.
Hu W-H, Zhang C, Zhang K, Meng F-G, Chen N, Zhang J-G. Selective amygdalohippocampectomy versus anterior temporal lobectomy in the management of mesial temporal lobe epilepsy: a meta-analysis of comparative studies. J Neurosurg. 2013;119(5):1089–97.
Martin RC, Sawrie SM, Roth DL, Gilliam FG, Faught E, Morawetz RB, et al. Individual memory change after anterior temporal lobectomy: a base rate analysis using regression-based outcome methodology. Epilepsia. 1998;39(10):1075–82.
Gleissner U, Helmstaedter C, Schramm J, Elger C. Memory outcome after selective amygdalohippocampectomy: a study in 140 patients with temporal lobe epilepsy. Epilepsia. 2002;43(1):87–95.
Clusmann H, Schramm J, Kral T, Helmstaedter C, Ostertun B, Fimmers R, et al. Prognostic factors and outcome after different types of resection for temporal lobe epilepsy. J Neurosurg. 2002;97(5):1131–41.
Langfitt JT, Rausch R. Word-finding deficits persist after left anterotemporal lobectomy. Arch Neurol. 1996;53(1):72–6.
Davies KG, Maxwell RE, Beniak TE, Destafney E, Fiol ME. Language function after temporal lobectomy without stimulation mapping of cortical function. Epilepsia. 1995;36(2):130–6.
Hermann BP, Wyler AR, Somes G. Language function following anterior temporal lobectomy. J Neurosurg. 1991;74(4):560–6.
Pauli E, Pickel S, Schulemann H, Buchfelder M, Stefan H. Neuropsychologic findings depending on the type of the resection in temporal lobe epilepsy. Adv Neurol. 1999;81:371–7.
Paglioli E, Palmini A, Portuguez M, Paglioli E, Azambuja N, da Costa JC, et al. Seizure and memory outcome following temporal lobe surgery: selective compared with nonselective approaches for hippocampal sclerosis. J Neurosurg. 2006;104(1):70–8.
Clusmann H, Kral T, Gleissner U, Sassen R, Urbach H, Blümcke I, et al. Analysis of different types of resection for pediatric patients with temporal lobe epilepsy. Neurosurgery. 2004;54(4):847–60.
Jones-Gotman M, Zatorre RJ, Olivier A, Andermann F, Cendes F, Staunton H, et al. Learning and retention of words and designs following excision from medial or lateral temporal-lobe structures. Neuropsychologia. 1997;35(7):963–73.
Wachi M, Tomikawa M, Fukuda M, Kameyama S, Kasahara K, Sasagawa M, et al. Neuropsychological changes after surgical treatment for temporal lobe epilepsy. Epilepsia. 2001;42(Suppl 6):4–8.
Novelly RA, Augustine EA, Mattson RH, Glaser GH, Williamson PD, Spencer DD, et al. Selective memory improvement and impairment in temporal lobectomy for epilepsy. Ann Neurol. 1984;15(1):64–7.
Hermann BP, Wyler AR, Richey ET. Wisconsin card sorting test performance in patients with complex partial seizures of temporal-lobe origin. J Clin Exp Neuropsychol. 1988;10(4):467–76.
Rausch R, Crandall PH. Psychological status related to surgical control of temporal lobe seizures. Epilepsia. 1982;23(2):191–202.
Naylor AS, Rogvi-Hansen Bá R-H, Kessing L, Kruse-Larsen C. Psychiatric morbidity after surgery for epilepsy: short-term follow up of patients undergoing amygdalohippocampectomy. J Neurol Neurosurg Psychiatry. 1994;57(11):1375–81.
Quigg M, Broshek DK, Heidal-Schiltz S, Maedgen JW, Bertram EH. Depression in intractable partial epilepsy varies by laterality of focus and surgery. Epilepsia. 2003;44(3):419–24.
Christodoulou C, Koutroumanidis M, Hennessy MJ, Elwes RDC, Polkey CE, Toone BK. Postictal psychosis after temporal lobectomy. Neurology. 2002;59(9):1432–5.
Mace CJ, Trimble MR. Psychosis following temporal lobe surgery: a report of six cases. J Neurol Neurosurg Psychiatry. 1991;54(7):639–44.
Altshuler L, Rausch R, Delrahim S, Kay J, Crandall P. Temporal lobe epilepsy, temporal lobectomy, and major depression. J Neuropsychiatry Clin Neurosci. 1999;11(4):436–43.
Hermann BP, Wyler AR, Ackerman B, Rosenthal T. Short-term psychological outcome of anterior temporal lobectomy. J Neurosurg. 1989;71(3):327–34.
Youngerman BE, Oh JY, Anbarasan D, Billakota S, Casadei CH, Corrigan EK, et al. Laser ablation is effective for temporal lobe epilepsy with and without mesial temporal sclerosis if hippocampal seizure onsets are localized by stereoelectroencephalography. Epilepsia. 2018;59(3):595–606.
Wu C, Boorman DW, Gorniak RJ, Farrell CJ, Evans JJ, Sharan AD. The effects of anatomic variations on stereotactic laser amygdalohippocampectomy and a proposed protocol for trajectory planning. Neurosurgery. 2015;11:345–57.
Jermakowicz WJ, Kanner AM, Sur S, Bermudez C, D’Haese P-F, Kolcun JPG, et al. Laser thermal ablation for mesiotemporal epilepsy: analysis of ablation volumes and trajectories. Epilepsia. 2017;58(5):801–10.
Vakharia VN, Sparks R, Li K, O’Keeffe AG, Miserocchi A, McEvoy AW, et al. Automated trajectory planning for laser interstitial thermal therapy in mesial temporal lobe epilepsy. Epilepsia. 2018;59(4):814–24.
Wu C, Jermakowicz WJ, Chakravorti S, Cajigas I, Sharan AD, Jagid JR, et al. Effects of surgical targeting in laser interstitial thermal therapy for mesial temporal lobe epilepsy: a multicenter study of 234 patients. Epilepsia. 2019;00:1–13.
Yin D, Thompson JA, Drees C, Ojemann SG, Nagae L, Pelak VS, et al. Optic radiation tractography and visual field deficits in laser interstitial thermal therapy for amygdalohippocampectomy in patients with mesial temporal lobe epilepsy. Stereotact Funct Neurosurg. 2017;95(2):107–13.
Willie JT, Laxpati NG, Drane DL, Gowda A, Appin C, Hao C, et al. Real-time magnetic resonance-guided stereotactic laser amygdalohippocampotomy for mesial temporal lobe epilepsy. Neurosurgery. 2014;74(6):569–84; discussion 584–5.
Donos C, Breier J, Friedman E, Rollo P, Johnson J, Moss L, et al. Laser ablation for mesial temporal lobe epilepsy: surgical and cognitive outcomes with and without mesial temporal sclerosis. Epilepsia. 2018;59(7):1421–32.
Le S, Ho AL, Fisher RS, Miller KJ, Henderson JM, Grant GA, et al. Laser interstitial thermal therapy (LITT): seizure outcomes for refractory mesial temporal lobe epilepsy. Epilepsy Behav. 2018;89:37–41.
Grewal SS, Zimmerman RS, Worrell G, Brinkmann BH, Tatum WO, Crepeau AZ, et al. Laser ablation for mesial temporal epilepsy: a multi-site, single institutional series. J Neurosurg. 2018:1–8.
Tao JX, Wu S, Lacy M, Rose S, Issa NP, Yang CW, et al. Stereotactic EEG-guided laser interstitial thermal therapy for mesial temporal lobe epilepsy. J Neurol Neurosurg Psychiatry. 2018;89(5):542–8.
Gross RE, Stern MA, Willie JT, Fasano RE, Saindane AM, Soares BP, et al. Stereotactic laser amygdalohippocampotomy for mesial temporal lobe epilepsy. Ann Neurol. 2018;83(3):575–87.
Kang JY, Wu C, Tracy J, Lorenzo M, Evans J, Nei M, et al. Laser interstitial thermal therapy for medically intractable mesial temporal lobe epilepsy. Epilepsia. 2016;57(2):325–34.
Drane DL, Loring DW, Voets NL, Price M, Ojemann JG, Willie JT, et al. Better object recognition and naming outcome with MRI-guided stereotactic laser amygdalohippocampotomy for temporal lobe epilepsy. Epilepsia. 2015;56(1):101–13.
Stereotactic Laser Ablation for Temporal Lobe Epilepsy (SLATE). Clinical Investigational Plan Study Sponsor: Medtronic Navigation, Inc. [Internet]. 2016 [cited 2019 May 13]. Available from: https://clinicaltrials.gov/ct2/show/NCT02844465.
Barbaro NM, Quigg M, Broshek DK, Ward MM, Lamborn KR, Laxer KD, et al. A multicenter, prospective pilot study of gamma knife radiosurgery for mesial temporal lobe epilepsy: seizure response, adverse events, and verbal memory. Ann Neurol. 2009;65(2):167–75.
Regis J, Rey M, Bartolomei F, Vladyka V, Liscak R, Schrottner O, et al. Gamma knife surgery in mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 2004;45(5):504–15.
Bartolomei F, Hayashi M, Tamura M, Rey M, Fischer C, Chauvel P, et al. Long-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsy. Neurology. 2008;70(19):1658–63.
Rheims S, Fischer C, Ryvlin P, Isnard J, Guenot M, Tamura M, et al. Long-term outcome of gamma-knife surgery in temporal lobe epilepsy. Epilepsy Res. 2008;80(1):23–9.
Quigg M, Broshek DK, Barbaro NM, Ward MM, Laxer KD, Yan G, et al. Neuropsychological outcomes after Gamma Knife radiosurgery for mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 2011;52(5):909–16.
Barbaro NM, Quigg M, Ward MM, Chang EF, Broshek DK, Langfitt JT, et al. Radiosurgery versus open surgery for mesial temporal lobe epilepsy: the randomized, controlled ROSE trial. Epilepsia. 2018;59(6):1198–207.
Englot DJ, Chang EF, Auguste KI. Efficacy of vagus nerve stimulation for epilepsy by patient age, epilepsy duration, and seizure type. Neurosurg Clin N Am. 2011;22(4):443–8.
Fisher R, Salanova V, Witt T, Worth R, Henry T, Gross R, et al. Electrical stimulation of the anterior nucleus of thalamus for treatment of refractory epilepsy. Epilepsia. 2010;51(5):899–908.
Salanova V, Witt T, Worth R, Henry TR, Gross RE, Nazzaro JM, et al. Long-term efficacy and safety of thalamic stimulation for drug-resistant partial epilepsy. Neurology. 2015;84(10):1017–25.
Child ND, Benarroch EE. Anterior nucleus of the thalamus: functional organization and clinical implications. Neurology. 2013;81(21):1869–76.
Geller EB, Skarpaas TL, Gross RE, Goodman RR, Barkley GL, Bazil CW, et al. Brain-responsive neurostimulation in patients with medically intractable mesial temporal lobe epilepsy. Epilepsia. 2017;58(6):994–1004.
Nair DR, Morrell MJ. Nine-year prospective safety and effectiveness outcomes from the long-term treatment trial of the RNS® system. In: American Epilepsy Society 2018 Annual Meeting. New Orleans, Louisiana; 2018. p. Abstract 2.075.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Karas, P.J., Sheth, S.A., Yoshor, D. (2020). Epilepsy: Mesial Temporal. In: Pouratian, N., Sheth, S. (eds) Stereotactic and Functional Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-030-34906-6_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-34906-6_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34905-9
Online ISBN: 978-3-030-34906-6
eBook Packages: MedicineMedicine (R0)