Abstract
Targeted therapeutic surgical lesioning for Parkinson disease has a history extending over 100 years, involving almost every level of the central nervous system often with serendipitous discovery of therapeutic approaches. Despite a near abandonment of lesioning for Parkinson disease after the introduction of levodopa, a resurgence of interest in lesioning was appreciated after recognizing limitations of medications over time in some patients. While the introduction of deep brain stimulation has made lesioning second-line treatment in some parts of the world, unilateral stereotactic lesioning remains an effective and viable option for therapeutic intervention, particularly in an era with incisionless approaches for targeted lesioning.
Stereotactic lesioning has been established as an efficacious and safe surgical option for patients with Parkinson disease with suboptimal symptom control or levodopa-induced dyskinesias who had previously responded to levodopa therapy, providing substantial therapeutic relief of tremor, bradykinesia, rigidity, and dyskinesias with some risk of weakness, speech alterations, and visual field deficits. Thalamotomy provides near-complete arrest of tremor with some risk of paresthesias, weakness, and dysarthria. Results vary based on modality used. In this chapter, the functional anatomy and physiologic basis of lesioning for each potential target (thalamus, pallidum, and subthalamic nucleus) are reviewed in detail. Given therapeutic alternatives of deep brain stimulation, comparisons between stimulation and lesioning are likewise detailed, including a thorough discussion of indications and contraindications for therapeutic stereotactic lesioning for Parkinson disease. Surgical preparation, technique, and outcomes are detailed for radiofrequency ablations, focused ultrasound, and radiosurgical approaches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Parkinson disease
- Pallidotomy
- Thalamotomy
- Subthalamotomy
- Radiofrequency ablation
- MR-guided focused ultrasound
Historical Background
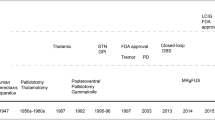
Rest tremor, bradykinesia, postural instability, and rigidity have remained the principle diagnostic criteria for Parkinson disease (PD) since James Parkinson’s early description in 1817 [1]. Leriche performed the earliest known PD surgery in 1912—a bilateral posterior cervical rhizotomy for rigidity [2]. For the next several decades, surgeons began experimenting with lesioning the pyramidal tracts: motor cortectomy [3], midbrain pedunculotomy [4], cerebellar dentatectomy [5], anterolateral cordotomy [6], lateral pyramidal tractotomy [7], posterolateral chordotomy [8], sympathetic ramicotomy, and ganglionectomy [9]. After an inadvertent anterior choroidal artery occlusion during a midbrain pedunculotomy arrested a patient’s tremor without hemiplegia, Cooper went on to perform planned surgical ligations of the anterior choroidal artery to alleviate tremor and rigidity. As expected due to the variable distribution of the anterior choroidal artery, surgical results were less than predictable [10, 11]. In 1939, Meyers performed the first surgery targeting the basal ganglia by ablating 2/3 of the caudate nucleus head to induce tremor cessation [12]. With the goal of identifying the optimal target, he subsequently designed a series of experimental surgeries in the extrapyramidal structures, the internal capsule, and pallidofugal fibers using local anesthesia to be able to correlate incremental lesions with clinical response in real time. His systematic approach led him to conclude that pallidofugal targets were superior in reducing tremor and rigidity [13].
Spiegel and Wycis revolutionized functional neurosurgery in 1947 by introducing stereotactic equipment to enable accurate and reproducible lesions in deep brain structures. Numerous stereotactic atlases were subsequently published using the intercommissural line to define the coordinate system [14]. Surgeons favored pallidotomy in parkinsonian patients and experimented not only with novel stereotaxic methods but also with lesioning modalities during both open and closed surgeries—coagulation, chemicals, ultrasound, and electrolysis [15,16,17,18]. Patients achieved greatest therapeutic benefit from lesions in the ventral and posterior regions of the globus pallidus interna [19]. After an accidental thalamotomy serendipitously arrested tremor and supported by the meticulous neuroanatomical work by Hassler, pallidotomy fell out of favor even though it produced superior reductions in rigidity and bradykinesia scores [20]. The next technical advance, microelectrode recordings, allowed electrophysiologists to rigorously analyze the anatomic components integral to movement disorders and enabled surgeons to more precisely define thalamic borders in the operating room. With these methods, surgeons were able to identify the optimal thalamic target for tremor control: the ventral intermediate nucleus. However, these lesions provided little relief of akinesia and rigidity [21]. The subthalamic region was also explored during this period as a method to interrupt pallidofugal and rubrothalamic fibers [22].
Although over 37,000 stereotactic neurosurgical operations had been performed for movement disorders predominately for PD, the introduction of levodopa led to a near-complete abandonment of neurosurgical interventions for PD [23]. Several factors accounted for the eventual resurgence of surgical management of the disease: levodopa’s diminished effectiveness over time, the development of medically refractory symptoms (flexed posture, freezing, loss of reflexes), and disabling side effects that significantly impaired quality of life (dyskinesias, motor fluctuations, psychiatric conditions) [24]. Laitinen’s 1992 landmark paper reintroduced posteroventral pallidotomy as an effective tool for managing advanced PD; his lesions produced excellent and durable reductions in tremor, rigidity, bradykinesia, and medication-induced dyskinesias with few side effects [25, 26]. Bilateral pallidotomies were trialed, and though patients experienced greater benefit than after unilateral operations, many reported greater risk of severe complications including dysarthria, gait disturbance, and swallowing difficulties [27]. Both unilateral and bilateral subthalamotomies were also revisited as lesioning targets in PD with improvements in all cardinal symptoms and reductions in levodopa-induced dyskinesias; however, improvements in tremor and dyskinesias seemed to be temporary and side effects more apparent [28, 29].
The introduction of deep brain stimulation (DBS) in the 1990s relegated lesioning to second-line therapy once again. The observation that high-frequency macrostimulation abolished tremor and predicted successful surgical outcome during thalamotomy served as the foundation for DBS technology. In DBS, the stimulation from a permanently implanted electrode was found to produce similar functional improvements as ablation and with an improved safety profile [30]. Lesioning became reserved for patients with contraindications to DBS, who did not achieve sufficient improvement from DBS, or for whom the cost of DBS and associated medical follow-up would prove too burdensome [31].
Advances in neuroimaging have improved visualization of target nuclei and enabled the introduction of two noninvasive lesioning methods—Gamma Knife (GK) and MRI-guided focused ultrasound (MRgFUS). Although radiosurgery’s delayed response and lack of real-time patient assessment for lesional effects make it less predictable than radiofrequency ablation, MRgFUS has shown promise in relieving parkinsonian symptoms with minimal side effects and the ability to monitor the patient during the procedure [32,33,34].
Functional Anatomy
A generalized model of basal ganglia (BG) circuitry provides sufficient context to understand both the hypoactive parkinsonian symptoms and the clinical response from ablating specific nuclei. In PD, alterations to these circuits change a patient’s ability to start and continue motion. Motor symptoms are generally divided into two categories: positive and negative. Positive symptoms are tremor, rigidity, and dystonia, while negative symptoms are bradykinesia (slowed movement), akinesia (absent movement), and loss of postural reflexes. Another major source of disability in PD patients arises after years of levodopa use: involuntary and often painful muscle contractions known as dyskinesias develop in 40% of patients after 4–6 years of medical therapy and in 90% after 9–15 years [35].
As the main BG input source, the striatum incorporates projections from the substantia nigra pars compacta (SNc), the intralaminar nuclei of the thalamus, and widespread cortical areas including the motor cortex, premotor cortex, and supplementary motor area [36, 37]. With the exception of projections from the subthalamus (STN), most BG connections are inhibitory. Two distinct pathways connect the input (striatum) to the two output nuclei (globus pallidus interna, GPi, and SN pars reticulata, SNr). The “direct” pathway facilitates motion through a monosynaptic connection from the striatum to GPi/SNr, while the “indirect” pathway diminishes unwanted or excessive motion through a polysynaptic relay from the striatum through GP external (GPe) and STN before reaching GPi/SNr. Pallidal projections terminate in the ventral oral posterior thalamic nucleus. The other important thalamic nuclei with regard to parkinsonian pathology—the ventral intermediate thalamic nucleus (VIM)—receives projections from the contralateral cerebellum and projects to the ipsilateral primary motor cortex, premotor cortex, and supplementary motor area [38, 39].
This circuit model serves as a simplified framework to explain the development of parkinsonism from the primary neuropathology—connecting the degeneration of SNc neurons to excessive inhibition of the thalamocortical and brainstem motor systems to the symptoms of hypoactive movement. A dopaminergic deficiency results from nigrostriatal neuronal loss. Via the direct pathway, the nigrostriatal dopaminergic deficiency reduces GPi inhibition. Via the indirect pathway, reduced nigrostriatal dopamine overly inhibits GPe, disinhibits STN, and activates GPi/SNr. The additive inhibitory effects from the direct pathway’s reduction in GPi inhibition and the indirect pathway’s increase in GPi/STN activity collectively reduce activity in thalamocortical and brainstem motor centers to produce the characteristic impoverished movement of bradykinesia and akinesia [40, 41].
Parkinsonian tremor is likely due to abnormal oscillating neuronal networks within the BG circuit appearing where groups of neurons exhibit a discharge pattern whose frequency is synchronized with limb tremor frequency. These so-called tremor cells exist in the ventralis intermedius (VIM) thalamus, STN, and GPi in tremor conditions as diverse as multiple sclerosis, essential tremor, and PD with the exception of cerebellar tremor syndromes [42, 43].
Physiologic Basis for Lesioning
Pallidotomy
In PD, nigrostriatal neuron degeneration and dopamine deficiency induces GPi hyperactivity through the combined effects of the direct and indirect pathways; this leads to excessive thalamic inhibition and reduced cortical activation, which produces hypokinetic parkinsonian symptoms. Metabolic studies have demonstrated that lesioning of the sensorimotor regions of the GPi in pallidotomy modulates this abnormal circuitry. Ablating GPi reduces lentiform metabolism and pathologic thalamic hyperinhibition, which increases frontal and prefrontal cortex metabolism; these metabolic changes have been correlated with symptom reduction [44, 45].
Thalamotomy
In non-cerebellar tremor syndromes, abnormally oscillating neuronal networks comprised of tremor cells in STN, GPi, and VIM thalamus are associated with a rest tremor. Postthalamotomy metabolic and perfusion studies demonstrated network remodulation differences between the resting and active state. The VIM thalamus appeared functionally disconnected from the laterofrontal and parietal association cortices at rest, while the primary motor cortex exhibited decreased perfusion during motion concomitant with tremor relief [45, 46]. Though thalamotomy arrests tremor, its minor impact on other parkinsonian symptoms has reduced the VIM thalamotomy to a more selective one in patients with tremor-predominant PD only.
Subthalamotomy
Subthalamic hyperactivity is one of several physiological manifestations of the dysregulated indirect pathway in PD. The dopaminergic deficit from nigrostriatal neuron degeneration leads to a hyperinhibited GPe, disinhibited STN, hyperactive GPi/SNR, and reduced thalamocortical output that produces the cardinal parkinsonian symptoms [47]. Subthalamotomies in nonhuman primates normalized GPi/SNr outputs and relieved akinesia, bradykinesia, tremor, and rigidity [48]. Metabolic studies confirmed that STN lesions suppress GPi/SNr activity, which influenced downstream pontine and thalamic activity through the first postoperative year [49, 50].
Deep Brain Stimulation Versus Ablation
To select the most appropriate neurosurgical technique to manage parkinsonian patients, the unique risks and benefits of DBS and ablation should guide decision-making. Though unilateral pallidotomy appears as safe and as effective as pallidal DBS, bilateral ablations appear to be less safe than bilateral DBS implantations due to a higher incidence of speech complications [51, 52]. Though both thalamotomy and VIM DBS demonstrated comparable increases in clinician rating scales for PD and quality of life, the improved DBS side effect profile makes it a superior option for most patients [53, 54].
Despite the merits of DBS, ablation remains a viable alternative and may be considered first-line in select patients. For experienced neurosurgeons, ablations are more straightforward procedures of shorter duration. General anesthesia is not required in lesioning, but is needed for DBS pulse generator implantation [55]. DBS implantation also requires significant follow-up for optimal programming, monitoring, and equipment replacement—these combined costs increase the ultimate price of DBS far above ablation [56]. With lesioning, patients need not be concerned with bulky hardware that is susceptible to infection, migration, malfunction, fracture, or failure reported at rates as high as 49% [57, 58]. Patients who required DBS explant due to hardware complications like infection or migration may also be appropriate candidates for ablation after sufficient recovery and appropriate evaluation [59]. Lastly, DBS is contraindicated in patients with immunodeficiency or autoimmune disorders [60].
Indications and Contraindications
The optimal candidate for ablation has had medically refractory idiopathic PD for 5–10 years with levodopa-responsive motor symptoms of tremor, rigidity, bradykinesia, and drug-induced dyskinesias. In practice, these patient’s symptoms should be more lateralized since pallidotomy is generally only done unilaterally. Patients should undergo rigorous neurologic and psychologic evaluation by a specialized movement disorders team in order to exclude patients with alternative diagnoses of supranuclear palsy, multiple system atrophy, and parkinsonism secondary to multifocal ischemic white matter disease—conditions with poorer prognoses that demonstrate minimal improvement after an ablation [61,62,63]. Patients with dementia, severe depression, psychosis, encephalitis, recent neuroleptic exposure, head trauma, or recent vascular disease should also be excluded [64]. Despite evidence that most patients experience only temporary speech disturbances, speech disorders remain a relevant contraindication. Thalamotomy presents a greater risk than pallidotomy for developing speech complications including hypoprosodia, changed enunciation, speech arrest, and lack of initiative to speak. Speech disturbances are much greater after bilateral ablations than unilateral ablations, both of which exceed the incidence after DBS surgeries [65, 66].
Pallidotomy
Asymmetric medically resistant idiopathic non-tremor-dominant PD patients whose motor symptoms had previously been levodopa-responsive achieve the greatest therapeutic benefit [67, 68]. Though painful dystonias, marked ON/OFF fluctuations, and bradykinesia respond very well, the greatest improvement is seen in dyskinesia reduction and OFF-period disability. Tremor may respond less well to pallidotomy, although most patients are substantially improved [69]. Postural instability and autonomic dysfunction rarely improve and have also worsened occasionally, so severe ataxia, serious gait problems, orthostatic hypotension, or severe gastrointestinal or genitourinary symptoms of autonomic dysfunction are relative contraindications [70]. Younger patients (<60 years old) derive greater benefit than older patients (>70 years old) though pallidotomies have been performed safely on patients from 30 to 82. Increased time since PD diagnosis also predicts poorer response [64]. Structural abnormalities and lentiform hypometabolism on FDG-PET are relative contraindications [58]. Several studies report increased risks in bilateral pallidotomy though others have safely performed staged bilateral pallidotomies without incurring additional complications; therefore, patients with severe bilateral symptoms should undergo bilateral DBS, but can sometimes be considered for staged bilateral pallidotomy [71, 72].
Thalamotomy
Patients with unilateral or asymmetric tremor-dominant medically refractory PD may experience greater benefit from thalamotomy [73]. Thalamotomy produces excellent reductions in tremor and moderate alleviation of rigidity; however, thalamic lesions typically have little to no impact on bradykinesia, micrographia, hypophonia, and gait [49]. Extending the lesion anteriorly to include the ventral oralis posterior can improve rigidity and levodopa-induced dyskinesias [74]. Bilateral thalamotomies have been associated with higher rates of hypophonia, dysarthria, swallowing difficulties, and worsened bradykinesia; so patients with bilateral tremor might benefit more from bilateral DBS [75, 76].
Subthalamotomy
Due to the historical association of STN damage with hemiballismus, subthalamotomies were not considered as a surgical option. This philosophy slowly shifted with increased understanding of the STN’s role in PD, due to several case reports of STN strokes improving parkinsonian tremor, and after early success with DBS stimulation to the STN [30, 77, 78]. Still only rarely performed, radiofrequency subthalamotomy may be considered in advanced, medically refractory relatively asymmetrical PD with disabling dyskinesias [79].
Surgical Procedures
Preoperative Evaluation
A comprehensive multidisciplinary movement disorders team of neurosurgeons, neurologists, psychiatrists, psychologists, and neuroradiologists should evaluate all patients. Their screening consists of a brain MRI, neuropsychological and ophthalmologic testing, as well as a thorough discussion of anticipated risks and benefits. The diagnosis of idiopathic PD must be confirmed to prevent ablating patients whose poor prognosis or comorbid conditions would thwart therapeutic benefit. A detailed history and physical examination might include Unified Parkinson’s Disease Rating Scale, Schwab and England scale, Hoehn and Yahr scale, and the SF-36 health survey to quantify overall disability. Prior to surgery, medical management should be optimized, mood or psychiatric disorders must be treated, and the cognitive state of the patient should be assessed. Standard preoperative screening and bloodwork is performed, and agents that alter clotting characteristics should be discontinued at least 5 days prior to surgery.
Stereotactic Radiofrequency Lesioning
Radiofrequency ablations of the pallidum, thalamus, and subthalamus share similar procedural steps with the notable exceptions of lesion location and microelectrode recording/macrostimulation characteristics. This overview describes the general technique for any stereotactic radiofrequency lesion [59, 80, 81].
Preparation for Surgery
Antiparkinson and antitremor medications are withheld overnight to facilitate microelectrode mapping, prevent medication-induced dyskinesias from dislodging the frame, and allow for direct assessment of clinical response. Benzodiazepines, anxiolytics, and other sedating agents are avoided to ensure adequate monitoring of motor symptoms and for full patient cooperation during the surgery. Propofol or midazolam can be used sparingly if a head tremor interferes with stereotactic image acquisition. IV access is established ipsilaterally to the side of lesion generation for complete freedom of movement in the extremity of interest. Oxygen is supplied by nasal cannula. EKG, pulse oximetry, and blood pressure are monitored and maintained in the normal range. Bladder catheterization is not routinely performed.
An MRI-compatible stereotactic frame is typically applied under local anesthesia with or without conscious sedation; however, frameless systems have been adapted for these procedures. General anesthesia can be used in patients with severe symptoms or anxiety.
Stereotactic Imaging
Modern imaging techniques have enabled demarcation of GPi and STN borders, but thalamic nuclei are not well visualized on 1.5–3T MRI scanners. There are two main target planning methodologies that utilize different combinations of images—“direct” and “indirect.” In “direct” target planning, the patient undergoes a sagittal T1-weighted MRI after frame application to identify the anterior commissure (AC) and posterior commissure (PC) and measure AC-PC length. The basal ganglia and thalamus, which lie in the AC-PC plane, are subsequently imaged using T2 sequences for GPi and SWI sequences for STN. For patients with contraindications to MRI, a stereotactic CT or ventriculography may be used for “indirect” targeting to estimate the AC-PC length and midcommissural points [75]. CT images alone are not suitable for target identification as their anatomical resolution is not sufficient for adequate target identification; however, a volumetric CT scan may be co-registered with a previous MRI without a frame if an MRI cannot be obtained.
Patient-specific atlases or probabilistic atlases based on large previous data sets can also be used as aids in target identification or verification. Furthermore, diffusion tensor imaging studies have been proposed to personalize target identification [82]. Images are imported into a neuronavigation computer workstation with stereotactic targeting software that calculates optimal trajectories as defined by the entry and lesion targets.
The pallidotomy target is typically 2–3 mm anterior to the midcommissural point, 4–6 mm below the intercommissural line, and 19–22 mm lateral to the midline of the third ventricle; however, these measurements are adjusted based on the patient’s unique anatomy. The lesion location lies behind the mammillary bodies’ posterior margin and superolateral to the optic tract; the limbic and associative territories of the pallidum, the optic tract, and the internal capsule should be avoided (Fig. 19.1) [83, 84].
The thalamotomy target, VIM nucleus, is usually 25% of the AC-PC length anterior to the posterior commissure point, 11 mm lateral to the third ventricle wall and at the level of the AC-PC (Fig. 19.2) [85].
The optimal STN target, dorsolateral motor region, is 2–3 mm posterior to the midcommissural point, 11–12 mm lateral to the AC-PC, and 4–5 mm inferior to the AC-PC plane [86, 87].
Surgical Technique
After prophylactic antibiotic administration, patients are positioned comfortably in a supine semi-sitting position to encourage full cooperation during the procedure. Draping must cover the field sufficiently without interfering with intraoperative assessment. A local anesthetic numbs the scalp, and a parasagittal incision is made to place a pallidotomy burr hole 3 cm from midline in the midpupillary line and 1–2 cm anterior to the coronal suture or a thalamotomy burr hole 3 cm from midline at the level of the coronal suture. An entry point is selected to avoid venous, sulcal, and ventricular penetration. The pallidotomy entry point is placed more anterolaterally in front of the coronal suture, while the thalamotomy entry point is about the level of the coronal suture. The dura and pia are coagulated to minimize bleeding during electrode placement. The stereotactic arc is then positioned and the electrode guide tube is lowered into the burr hole. The burr hole is filled with fibrin glue or the skin is temporarily closed with nylon sutures to minimize CSF loss and brain settling.
Microelectrode Recording and Macrostimulation
To confirm the trajectory, define target borders, and refine lesion location, macrostimulation and/or microelectrode recording may be performed. Microelectrode recording was used in 46.2% of pallidotomies, and macroelectrode stimulation was performed in 53.8% of pallidotomies from 1992 to 1999 [63]. For microelectrode recording, a microdrive platform is mounted to the frame to precisely drive in a microelectrode, which records activity from individual neurons. Analyzing the neuronal activity of various cell types enables the creation of a detailed map of the basal ganglia and thalamic nuclei for precise targeting; however, specialized expertise, specific equipment, and time for analysis is required. Faster but less precise, a macroelectrode with an exposed tip for stimulation can be used independently or sequentially after microelectrode recording. A square wave pulse is applied at 0–5 volts at 2 Hz for motor thresholds and at 50–75 Hz for visual thresholds, and the patient is monitored for signs of symptom relief, neurologic impairments, or abnormal sensations.
Lesion Generation
The radiofrequency generator conducts heat through a probe with an exposed tip to create a lesion at the target. During both the test lesions and ablation process, speech and sensorimotor functions are continuously monitored. In pallidotomies, visual fields are also monitored. A test lesion is performed at 42–46 °C for 60 seconds, and the permanent lesion is produced by gradually increasing the temperature from 60 to 75 °C for 60 seconds [63]. For pallidotomy, additional lesions are made at 2 mm and 4 mm above the target (Fig. 19.3). For thalamotomy lesions, the initial lesion is placed at the intercomissural plane and a second lesion placed 2 mm superior to the first (Fig. 19.4). A balance must be struck when determining overall lesion size between symptomatic relief and side effects or complications. Lesion size varies also based on procedure type—pallidotomy lesions often measure 6 mm in height and 4 mm in diameter, and thalamotomy lesions measure 4–6 mm in diameter [55, 88]. After ablating the target, the electrode is withdrawn, and the burr hole is filled with Gelfoam and bone dust prior to closing the scalp, removing the frame, and covering with sterile dressing.
Postoperative Care
Patients usually return to their room after a short period of observation. Mild analgesics are typically sufficient to manage postoperative pain though special care is taken to manage blood pressure to minimize hemorrhage risk. Patients are monitored overnight and undergo an MRI prior to discharge to verify lesion location and exclude complications.
MRI-Guided Focused Ultrasound (MRgFUS) Lesioning
Although Fry et al. first proposed ultrasound as a surgical option for PD in 1958, his technique required a craniotomy to directly access the site of interest [89]. Since that time, numerous technological discoveries paved the way for the development of the newest noninvasive neurosurgical technique currently undergoing Phase III clinical trials: MRgFUS [90,91,92,93]. The physics concept of focused sonication serves as the basis for this therapy: sound energy in the form of an ultrasound wave transmitted through the skull is transformed to thermal energy at the target site. No incisions or burr holes are required to precisely create permanent lesions. A thermal dose of 57 °C for 1 second denatures all proteins and causes death of all cells; the equivalent thermal dose is a function of exposed area and length of exposure [94].
Preoperative screening and surgical preparation remains the same as for radiofrequency ablation. The patient’s head is first completely shaved and then fixed in an MRI-compatible stereotactic frame with local anesthetic similarly to radiofrequency ablation procedures. An elastic diaphragm is stretched around the head and connected to the transducer before being filled with degassed and chilled water. Performed in an MRI suite, MRgFUS uses real-time MRI for accurate localization, treatment planning, and thermal dosing control throughout the procedure [95]. Intraoperative MRI scans are fused to the preoperative CT scan for proper skull correction as the skull density alters the thermal energy that reaches the lesion site [96]. The VIM thalamotomy target is one quarter of the AC-PC length anterior to PC, 14 mm lateral to midline or 11 mm from the third ventricle wall if the ventricle is enlarged and 1–2 mm above the AC-PC plane [83]. The pallidotomy target is reported to be 22 mm lateral from midline, 3–4 mm anterior from the AC-PC line midpoint, and 2–3 mm inferior to the intercommissural line [84].
MRgFUS is divided into three phases. During the first stage, MR thermography at lower energies (41–46 °C) is used to confirm the sonication target in sagittal, axial, and coronal planes. In the second stage, energy is gradually increased (46–50 °C) while the patient is monitored for symptom relief and adverse effects. The third and final stage consists of ablation—incrementally, energy is increased through either larger sonication intensity not to exceed 60 °C or prolonged sonication duration (Fig. 19.5). The procedure is typically performed as an outpatient procedure [83, 97].
Gamma Knife (GK) Lesioning
Though introduced as a neurosurgical technique for functional disorders in 1951 by Lars Leksell, stereotactic radiosurgery for PD remains less preferable than DBS and radiofrequency lesioning because of the significant delay in symptomatic improvement and less predictable adverse events [98, 99]. Its application is limited to patient preference and to poor surgical candidates with severe cardiac or respiratory disease, taking chronic anticoagulation, medically noncompliant, and the elderly. Cobalt-60 gamma units produce multiple beams of photon energy that are focused through 4 mm collimator openings. This ionizing radiation produces free radicals; both gamma radiation and free radicals damage tissue and mutate DNA to induce necrosis at the target site [100, 101]. Incisions and burr holes are not required for lesion generation and no head shave is needed.
As described above for radiofrequency ablations, patients should undergo rigorous preoperative screening and surgical preparation; the movement disorders team should also include radiation oncologists and medical physicists. The patient’s head is first fixed in a stereotactic frame, and a high-resolution MRI is obtained and then loaded onto a computer with dose-planning software. Individual doses were determined jointly by the neurosurgeon, radiation oncologist, and medical physicist, ranging from 120 to 180 Gy in pallidotomies and 120 to 160 Gy in thalamotomies. Follow-up imaging is performed several months after discharge when the GK results would be visible [91, 92].
Surgical Results
Clinical Outcome
Pallidotomy
Pallidotomy has been evaluated in numerous retrospective case series, several prospective uncontrolled trials, and a few controlled, randomized, blinded clinical trials [102, 103]. Alkhani et al. summarized the results of nearly 2000 PD patients who had received radiofrequency pallidotomies in 40 centers in 12 countries published between 1992 and 1999. In 263 of 1959 patients, pre- and postoperative contralateral dyskinesia scores were documented: mean scores increased by 67.7% from 2.2 +/− 0.6 to 0.71 +/− 0.45 with improvement sustained at 6 months (73.5% of 94 assessed patients) and 12 months (86.4% of 71 assessed patients) [63]. Patients also achieve significant reductions in contralateral symptoms of rigidity, tremor, and bradykinesia during OFF periods with some ipsilateral changes. Changes during the ON periods are less pronounced [26, 78]. Not only are the symptoms better during the OFF periods, but patients report reduced duration of OFF hours per day [65, 95]. The impact on gait remains obscured by conflicting results as some patients describe improved or unchanged gait, while others complain of worsening gait and postural instability [104, 105]. Speech dysfunction worsens in patients with preoperative moderate and severe dysarthria, while mildly dysarthric patients are more likely to experience some benefit to speech after pallidotomy [106].
Thalamotomy
The majority of patients achieve complete or near-complete extremity tremor arrest with little impact on bradykinesia, gait, or executive function [107, 108]. Persistence of tremor relief remains a controversial topic since some patients report sustained benefits over a decade of follow-up, while others have observed a steady decline to preoperative function as compared to baseline. Although the length of benefit from thalamotomy continues to be debated, there does appear to be consensus that thalamotomy does not alter disease progression [109]. Some demonstrate sustained improvements in rigidity opposite to lesion side; however, optimal improvement of rigidity occurs with lesions in the Vop thalamus [59]. Thalamotomy’s impact on levodopa-induced dyskinesias was initially controversial with some early publications purported that lesioning prevented their development and others reporting minimal dyskinesia reduction [110]. It appears that the overall dyskinesia reduction was the result of reduced daily levodopa requirements after the surgery. Furthermore, ventralis oralis anterior and posterior have been found to be more appropriate lesioning targets to reduce dyskinesias [111].
MRI-Guided Focused Ultrasound (MRgFUS) Lesioning
Though few case reports of MRgFUS pallidotomy have been published, early results demonstrate similar improvements to radiofrequency pallidotomy in the first 6 months: improved ON and OFF motor scores and reduced levodopa-induced dyskinesias [84, 112]. MRgFUS VIM thalamotomy has been studied more rigorously and been shown to greatly improve tremor in patients with medically refractory tremor-dominant PD in the setting of a placebo response [85]. Alleviating tremor significantly improves quality of life scores through increased ability to complete activities of daily living [113, 114].
Gamma Knife (GK) Lesioning
Elaimy et al. summarized the 14 publications on 79 patients who received GK pallidotomy and 477 patients who received GK thalamotomy for movement disorders. Patients rarely undergo GK pallidotomy due to the controversy surrounding the procedure’s efficacy and safety; improvements in bradykinesia, rigidity, and dyskinesia range from 0% to 87%. Although none of the 4 patients in the smallest case series received therapeutic benefit and only 33% of the 18 patients in the intermediate-sized series improved, 2 larger studies of 28 and 29 patients reported 64.3–65.5% reported bradykinesia/rigidity improvements and 85.7–86.8% experienced reduced dyskinesias. GK thalamotomy for tremor has reportedly produced 80–100% improvement in 455 patients with essential tremor, PD, and multiple sclerosis with onset of improvement ranging from 1 week to 1 year [92].
Subthalamotomy
Subthalamotomies produce contralateral tremor arrest, bilateral reductions in bradykinesia and rigidity in the ON and OFF states, and improvements in freezing, postural stability, and facial expression. In comparison with pallidotomy and thalamotomy, subthalamotomy significantly decreases medication needs, which slows medication-induced dyskinesia development and reduces disability [28, 86]. Bilateral procedures demonstrated greater improvements in scores for tremor, bradykinesia, and rigidity on both sides [29].
Complications
Pallidotomy
Alkhani and Lozano’s systematic review of 1564 pallidotomy patients provides the most comprehensive analysis of adverse events. Hemorrhage is the most serious complication of radiofrequency pallidotomy and occurs in 1.7% of patients with a mortality rate of 0.4%. It is clear that hemorrhage occurs more commonly with MER-guided procedures. Overall estimated morbidity rate was 23.1% with a 14.3% permanent morbidity rate. The most common complications were (1) weakness that developed in 5.3% and persisted in 2.2%, (2) speech disorders (dysarthria, hypophonia) that occurred in 4.5% and persisted in 2.9%, and (3) visual field deficits that affected 2% and persisted in 1.5% of patients [63]. Most patients do not experience significant cognitive or psychiatric impairment though the elderly are more prone to transient postoperative confusion or somnolence [64, 115]. Several studies indicate temporary mild changes to cognition, memory, and executive function; left-sided lesions may decrease verbal fluency or frontal lobe functions, while right-sided lesions may improve frontal functions [116, 117].
Thalamotomy
As in pallidotomy, mortality rates are low (0.4–9%), and intracranial hemorrhage, which represents the most significant complication of thalamotomy, has been reported in 1.5–6% of patients, again more commonly with MER-guided procedures [118]. Patients report dysarthria, hypophonia, dysphagia, or aphasia with only a subset reporting persistent complications and an even smaller fraction reporting the adverse effects were a source of disability [119]. Historically patients experienced weakness or hemiparesis at rates of 1.7–26% though modern stereotactic techniques seem to have reduced the incidence and most resolve without subsequent treatment [15, 111]. Patients also report temporary perioral or appendicular paresthesias and numbness [120]. Thalamotomy appears to have limited cognitive sequelae of reduced verbal fluency and minor memory impairment; however, some patients experience improvements in verbal memory [121, 122]. Rare complications include infection, thalamic pain syndromes, neglect, dysphagia, sialorrhea, blepharospasm, dystonia, ataxia, hyperkinesia, and hypotonia [111].
MRI-Guided Focused Ultrasound (MRgFUS) Lesioning
The noninvasive technique of MRgFUS represents a major benefit as compared to other neurosurgical interventions for movement disorders—those benefits are most visibly manifested through reduced rates of serious complications. Though larger trials are necessary to confirm the results of the MRgFUS thalamotomy clinical trial, its outcomes are the most current understanding of MRgFUS complication rates in PD. During early trials, internal capsule heating induced mild hemiparesis that eventually improved to near-baseline. The majority of adverse results are temporary and of lower acuity and consist of persistent mild ataxia (5%), orofacial paresthesias (27%), finger paresthesias (5%), and temporary ataxia (35%)—the majority resolved by 12 months. Headache (65%) and dizziness/vertigo (42%) occur only during the procedure with complete resolution upon exiting the MRI suite [85]. Several other minor complications arise at lower rates: nausea, pin-site discomfort, taste disturbances, dyskinesias, subjective speech disturbance, anxiety, fatigue, weight gain, transient hypertension, facial asymmetry, and minor impulsivity [83, 86].
Gamma Knife (GK) Lesioning
In both GK pallidotomy and thalamotomy, a diverse and unpredictable side effects profile develops in the same delayed fashion as clinical benefit with a wide reported range of 0.4–50%. The larger studies of 28 and 29 patients reported complication rates of 3.4–3.6%, the intermediate series of 18 patients reported a 50% complication rate, and the smallest case series of 4 reported 25%. Complications included visual field deficiencies, dysphagia, dysarthria, hemiparesis, hemianesthesia, dementia, and psychosis. In the nine studies on GK thalamotomy, complication rates ranged from 0% to 16.7% though one outlier published a 46.7% complication rate. Complications included hemorrhage, edema, hemiparesis, sensory and motor impairments, dysarthria, dysphagia, and disordered balance [92]. Two hypotheses postulate causes for the increased rates of adverse events in GK pallidotomy versus thalamotomy: (1) pallidal perforating arteries supply more diverse downstream effects than thalamic vessels, and (2) iron accumulates in the pallidum with age, thus increasing the concentration of metallic products susceptible to acting as free radical catalysts that induce greater damage [91, 123].
Subthalamotomy
Subthalamotomies produce contralateral tremor arrest, bilateral reductions in bradykinesia and rigidity in the ON and OFF states, and improvements in freezing, postural stability, and facial expression. In comparison with pallidotomy and thalamotomy, subthalamotomy significantly decreases medication needs, which slows medication-induced dyskinesia development and reduces disability [28, 86]. Bilateral procedures demonstrated greater improvements in scores for tremor, bradykinesia, and rigidity on both sides [29].
A pilot study of ten patients reported results of unilateral MRgFUS subthalamotomy with a lesion target of 3 mm posterior, 12 mm lateral, and 4 mm inferior to the midcommissural point. Results demonstrated improvements of hemibody motor scores for rigidity, akinesia, and tremor by 53% in the OFF state and 47% in the ON state through the first 6 months. Complications included dyskinesias, speech disturbances, anxiety, weight gain, gait ataxia, pin-site pain, transient hypertension, facial asymmetry, and impulsivity [86]. A small case series of 13 patients targeting the pallidothalamic tract guided by tractography also showed equivalent benefit to patients as from radiofrequency lesioning with reduced risk of adverse events—total motor score improvements of 60.9% without postoperative neurologic complications [124].
Conclusion
Radiofrequency ablation procedures have been established as an efficacious and safe surgical option for parkinsonian patients with suboptimal symptom control or levodopa-induced dyskinesias who had previously responded to levodopa therapy. Pallidotomy provides substantial therapeutic relief of tremor, bradykinesia, rigidity, and dyskinesias with some risk of weakness, speech alterations, and visual field deficits. Thalamotomy provides near-complete arrest of tremor with some risk of paresthesias, weakness, and dysarthria. GK has also been shown to effectively produce lesions though in a delayed fashion with less predictable side effects particularly after pallidotomies. Though longer-term and larger studies of MRgFUS lesioning are needed to confirm early results, the novel noninvasive technique’s initial experience suggests an important role in the functional neurosurgery armamentarium.
References
Parkinson J. An essay on the shaking palsy. J Neuropsychiatry Clin Neurosci. 2002;14(2):223–36.
Duker AP, Espay AJ. Surgical treatment of Parkinson disease: past, present, and future. Neurol Clin. 2013;31(3):799–808.
Bucy PC, Case TJ. Tremor: physiologic mechanism and abolition by surgical means. Arch Neurol Psychiatr. 1939;41(4):721–46.
Walker AE. Cerebral pedunculotomy for the relief of involuntary movements: II. Parkinsonian tremor. J Nerv Ment Dis. 1952;116(6):766–75.
Baltuch GH, Stern MB, editors. Deep brain stimulation for Parkinson’s disease. Boca Raton: CRC Press; 2007.
Putnam TJ. Relief from unilateral paralysis agitans by section of the pyramidal tract. Arch Neurol. 1938;40:1049–50.
Oliver L. Surgery in Parkinson’s disease division of lateral pyramidal tract for tremor. Lancet. 1949;253(6561):910–3.
Puusepp L. Cordotomia posterior lateralis (fasc. Burdachi) on account of trembling and hypertonia of the muscles in the hand. Folia Neuropath Estonia. 1930;10:62–4.
Gardner WJ, Williams GH. Interruption of the sympathetic nerve supply to the brain—effect on Parkinson’s syndrome. Arch Neurol Psychiatr. 1949;61(4):413–21.
Cooper IS. Ligation of the anterior choroidal artery for involuntary movements-parkinsonism. Psychiatry Q. 1953;27(1–4):317–9.
Cooper IS. Surgical alleviation of parkinsonism: effects of occlusion of the anterior choroidal artery. J Am Geriatr Soc. 1954;2(11):691–718.
Meyers R. Surgical procedure for postencephalitic tremor, with notes on the physiology of premotor fibers. Arch Neurol Psychiatr. 1940;44:455–9.
Meyers R. Surgical experiments in the therapy of certain ‘extrapyramidal’ diseases: a current evaluation. Acta Psychiatr Neurol Suppl. 1951;67:1–42.
Spiegel EA, Wycis HT, Marks M, Lee AJ. Stereotaxic apparatus for operations on the human brain. Science. 1947;106(2754):349–50.
Waltz JM, Riklan M, Stellar S, Cooper IS. Cryothalamectomy for Parkinson’s disease a statistical analysis. Neurology. 1966;16(10):994.
Obrador S. A simplified neurosurgical technique for approaching and damaging the region of the globus pallidus in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1957;20(1):47.
Fry WJ, Meyers R. Ultrasonic method of modifying brain structures. Stereotact Funct Neurosurg. 1962;22(3–5):315–27.
Cooper IS, Bravo G. Chemopallidectomy and chemothalamectomy. J Neurosurg. 1958;15(3):244–50.
Guridi J, Lozano AM. A brief history of pallidotomy. Neurosurgery. 1997;41(5):1169–83.
Cooper IS. Surgical treatment of parkinsonism. Annu Rev Med. 1965;16(1):309–30.
Narabayashi H. Parkinsonian tremor and nucleus ventralis intermedius of the human thalamus. Prog Clin Neurophysiol. 1978;5:165–72.
Bertrand CMA. Pneumotaxic technique for producing localized cerebral lesions: and its use in the treatment of Parkinson’s disease. J Neurosurg. 1958;15(3):251–64.
Speelman JD, Bosch DA. Resurgence of functional neurosurgery for Parkinson’s disease: a historical perspective. Mov Disord. 1998;13(3):582–8.
Marsden CD, Parkes JD. Success and problems of long-term levodopa therapy in Parkinson’s disease. Lancet. 1977;309(8007):345–9.
Laitinen LV, Bergenheim AT, Hariz MI. Ventroposterolateral pallidotomy can abolish all parkinsonian symptoms. Stereotact Funct Neurosurg. 1992;58(1–4):14–21.
Laitinen LV. Pallidotomy for Parkinson’s disease. Neurosurg Clin. 1995;6(1):105–12.
Merello M, Starkstein S, Nouzeilles MI, Kuzis G, Leiguarda R. Bilateral pallidotomy for treatment of Parkinson’s disease induced corticobulbar syndrome and psychic akinesia avoidable by globus pallidus lesion combined with contralateral stimulation. J Neurol Neurosurg Psychiatry. 2001;71(5):611–4.
Obeso JA, Alvarez LM, Macias RJ, Guridi J, Teijeiro J, Juncos JL, Rodriguez MC, Ramos E, Linazasoro GJ, Gorospe A, DeLong MR. Lesion of the subthalamic nucleus (STN) in Parkinson’s disease (PD). Neurology. 1997;48(3):12003.
Heywood P, Gill SS. Bilateral dorsolateral subthalamotomy for advanced Parkinson’s disease. Lancet. 1997;350(9086):1224.
Kleiner-Fisman G, Herzog J, Fisman DN, Tamma F, Lyons KE, Pahwa R, Lang AE, Deuschl G. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord. 2006;21(S14):S290–304.
Tomaszewski KJ, Holloway RG. Deep brain stimulation in the treatment of Parkinson’s disease a cost-effectiveness analysis. Neurology. 2001;57(4):663–71.
Higuchi Y, Matsuda S, Serizawa T. Gamma knife radiosurgery in movement disorders: indications and limitations. Mov Disord. 2017;32(1):28–35.
Christian E, Yu C, Apuzzo ML. Focused ultrasound: relevant history and prospects for the addition of mechanical energy to the neurosurgical armamentarium. World Neurosurg. 2014;82(3–4):354–65.
Lozano CS, Tam J, Lozano AM. The changing landscape of surgery for Parkinson’s disease. Mov Disord. 2018;33(1):36–47.
Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001;16(3):448–58.
Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci. 1986;9(1):357–81.
Alexander GE, Crutcher MD. Functional architecture of basal ganglia circuits: neural substrates of parallel processing. Trends Neurosci. 1990;13(7):266–71.
Smith Y, Bevan MD, Shink E, Bolam JP. Microcircuitry of the direct and indirect pathways of the basal ganglia. Neuroscience. 1998;86(2):353–87.
Crossman AR. Functional anatomy of movement disorders. J Anat. 2000;196(4):519–25.
Obeso JA, Rodriguez-Oroz MC, Rodriguez M, Lanciego JL, Artieda J, Gonzalo N, Olanow CW. Pathophysiology of the basal ganglia in Parkinson’s disease. Trends Neurosci. 2000;23:S8–19.
Miller WC, DeLong MR. Parkinsonian symptomatology an anatomical and physiological analysis. Ann N Y Acad Sci. 1988;515(1):287–302.
Jasper HH. Thalamic units involved in somatic sensation and voluntary and involuntary movements in man. Thalamus. 1966:365–90.
Deuschl G, Raethjen J, Baron R, Lindemann M, Wilms H, Krack P. The pathophysiology of parkinsonian tremor: a review. J Neurol. 2000;247(5):V33–48.
Eidelberg D, Moeller JR, Ishikawa T, Dhawan V, Spetsieris P, Silbersweig D, Stern E, Woods RP, Fazzini E, Dogali M, Beric A. Regional metabolic correlates of surgical outcomes following unilateral pallidotomy for parkinson’s disease. Ann Neurol. 1996;39(4):450–9.
Henselmans JM, de Jong BM, Pruim J, Staal MJ, Rutgers AW, Haaxma R. Acute effects of thalamotomy and pallidotomy on regional cerebral metabolism, evaluated by PET. Clin Neurol Neurosurg. 2000;102(2):84–90.
Boecker H, Wills AJ, Ceballos-Baumann A, Samuel M, Thomas DG, Marsden CD, Brooks DJ. Stereotactic thalamotomy in tremor-dominant Parkinson’s disease: an H215O PET motor activation study. Ann Neurol. 1997;41(1):108–11.
Bergman H, Wichmann T, DeLong MR. Reversal of experimental parkinsonism by lesions of the subthalamic nucleus. Science. 1990;249(4975):1436–8.
Aziz TZ, Peggs D, Sambrook MA, Crossman AR. Lesion of the subthalamic nucleus for the alleviation of 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine (MPTP)-induced parkinsonism in the primate. Mov Disord. 1991;6(4):288–92.
Su PC, Ma Y, Fukuda M, Mentis MJ, Tseng HM, Yen RF, Liu HM, Moeller JR, Eidelberg D. Metabolic changes following subthalamotomy for advanced Parkinson’s disease. Ann Neurol. 2001;50(4):514–20.
Trošt M, Su PC, Barnes A, Su SL, Yen RF, Tseng HM, Ma Y, Eidelberg D. Evolving metabolic changes during the first postoperative year after subthalamotomy. J Neurosurg. 2003;99(5):872–8.
Kumar R, Lozano AM, Montgomery E, Lang AE. Pallidotomy and deep brain stimulation of the pallidum and subthalamic nucleus in advanced Parkinson’s disease. Mov Disord. 1998;13:73–82.
Blomstedt P, Hariz GM, Hariz MI. Pallidotomy versus pallidal stimulation. Parkinsonism Relat Disord. 2006;12(5):296–301.
Tasker RR. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg Neurol. 1998;49(2):145–53.
Blomstedt P, Hariz MI. Are complications less common in deep brain stimulation than in ablative procedures for movement disorders? Stereotact Funct Neurosurg. 2006;84(2–3):72–81.
Gross RE. What happened to posteroventral pallidotomy for Parkinson’s disease and dystonia? Neurotherapeutics. 2008;5(2):281–93.
McIntosh E, Gray A, Aziz T. Estimating the costs of surgical innovations: the case for subthalamic nucleus stimulation in the treatment of advanced Parkinson’s disease. Mov Disord. 2003;18(9):993–9.
Hariz MI. Complications of deep brain stimulation surgery. Mov Disord. 2002;17(S3):S162–6.
Oh MY, Abosch A, Kim SH, Lang AE, Lozano AM. Long-term hardware-related complications of deep brain stimulation. Neurosurgery. 2002;50(6):1268–76.
Lokuketagoda J, Gross R. Thalamotomy and pallidotomy. In: Jandial R, McCormick P, Black PM, editors. Core techniques in operative neurosurgery E-book: expert consult-online. Amsterdam: Elsevier Health Sciences; 2011. p. 290–300.
Hooper AK, Okun MS, Foote KD, Fernandez HH, Jacobson C, Zeilman P, Romrell J, Rodriguez RL. Clinical cases where lesion therapy was chosen over deep brain stimulation. Stereotact Funct Neurosurg. 2008;86(3):147–52.
Alterman RL, Kelly P, Sterio D, Fazzini E, Eidelberg D, Perrine K, Beric A. Selection criteria for unilateral posteroventral pallidotomy. In: Advances in stereotactic and functional neurosurgery 12. Vienna: Springer; 1997. p. 18–23.
Alterman RL, Kelly PJ. Pallidotomy technique and results: the New York University experience. Neurosurg Clin N Am. 1998;9(2):337–44.
Tasker RR, Siqueira J, Hawrylyshyn P, Organ LW. What happened to VIM thalamotomy for Parkinson’s disease? Stereotact Funct Neurosurg. 1983;46(1–4):68–83.
Bronstein JM, DeSalles A, DeLong MR. Stereotactic pallidotomy in the treatment of Parkinson disease: an expert opinion. Arch Neurol. 1999;56(9):1064–9.
Alomar S, King NK, Tam J, Bari AA, Hamani C, Lozano AM. Speech and language adverse effects after thalamotomy and deep brain stimulation in patients with movement disorders: a meta-analysis. Mov Disord. 2017;32(1):53–63.
Uitti RJ, Wharen RE Jr, Duffy JR, Lucas JA, Schneider SL, Rippeth JD, Wszolek ZK, Obwegeser AA, Turk MF, Atkinson EJ. Unilateral pallidotomy for Parkinson’s disease: speech, motor, and neuropsychological outcome measurements. Parkinsonism Relat Disord. 2000;6(3):133–43.
Alkhani A, Lozano AM. Pallidotomy for Parkinson disease: a review of contemporary literature. J Neurosurg. 2001;94(1):43–9.
Van Horn G, Hassenbusch SJ, Zouridakis G, Mullani NA, Wilde MC, Papanicolaou AC. Pallidotomy: a comparison of responders and nonresponders. Neurosurgery. 2001;48(2):263–73.
Iacono RP, Shima F, Lonser RR, Kuniyoshi S, Maeda G, Yamada S. The results, indications, and physiology of posteroventral pallidotomy for patients with Parkinson’s disease. Neurosurgery. 1995;36(6):1118–25.
Lozano AM, Lang AE. Pallidotomy for Parkinson’s disease. Neurosurg Clin N Am. 1998;9(2):325–36.
De Bie RM, Schuurman PR, Esselink RA, Bosch DA, Speelman JD. Bilateral pallidotomy in Parkinson’s disease: a retrospective study. Mov Disord. 2002;17(3):533–8.
Counihan TJ, Shinobu LA, Eskandar EN, Cosgrove GR, Penney JB Jr. Outcomes following staged bilateral pallidotomy in advanced Parkinson’s disease. Neurology. 2001;56(6):799–802.
Tasker RR. Thalamotomy. Neurosurg Clin N Am. 1990;1(4):841–64.
Narabayashi HI, Yokochi FU, Nakajima YA. Levodopa-induced dyskinesia and thalamotomy. J Neurol Neurosurg Psychiatry. 1984;47(8):831–9.
Matsumoto K, Asano T, Baba T, Miyamoto T, Ohmoto T. Long-term follow-up results of bilateral thalamotomy for parkinsonism. Stereotact Funct Neurosurg. 1976;39(3–4):257–60.
Hallett M, Litvan I. Evaluation of surgery for Parkinson’s disease: a report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 1999;53(9):1910.
Vidaković A, Dragasević N, Kostić VS. Hemiballism: report of 25 cases. J Neurol Neurosurg Psychiatry. 1994;57(8):945–9.
Yamada A, Takeuchi H, Miki H. Unilateral abolition of parkinsonian rigidity after subthalamic nucleus hemorrhage. Clin Neurol. 1992;32(8):887–9.
Patel NK, Heywood P, O’Sullivan K, McCarter R, Love S, Gill SS. Unilateral subthalamotomy in the treatment of Parkinson’s disease. Brain. 2003;126(5):1136–45.
Gross RE, Stern MA, Lazarus JT. Ablative procedures for Parkinson’s disease. In: Winn HR, editor. Youmans neurological surgery E-book. Amsterdam: Elsevier Health Sciences; 2011. p. 610–8.
Walter BL, Vitek JL. Surgical treatment for Parkinson’s disease. Lancet Neurol. 2004;3(12):719–28.
See AA, King NK. Improving surgical outcome using diffusion tensor imaging techniques in deep brain stimulation. Front Surg. 2017;4:54.
Eskandar EN, Shinobu LA, Penney JB, Cosgrove GR, Counihan TJ. Stereotactic pallidotomy performed without using microelectrode guidance in patients with Parkinson’s disease: surgical technique and 2-year results. J Neurosurg. 2000;92(3):375–83.
Laitinen LV, Bergenheim AT, Hariz MI. Leksell’s posteroventral pallidotomy in the treatment of Parkinson’s disease. J Neurosurg. 1992;76(1):53–61.
Tasker RR, Yamashiro K, Lenz F, Dostrovsky JO. Thalamotomy for Parkinson’s disease: microelectrode technique. In: Modern stereotactic neurosurgery. Boston: Springer; 1988. p. 297–314.
Alvarez L, Macias R, Guridi J, Lopez G, Alvarez E, Maragoto C, Teijeiro J, Torres A, Pavon N, Rodriguez-Oroz MC, Ochoa L. Dorsal subthalamotomy for Parkinson’s disease. Mov Disord. 2001;16(1):72–8.
Rodriguez-Rojas R, Carballo-Barreda M, Alvarez L, Guridi J, Pavon N, Garcia-Maeso I, Macías R, Rodriguez-Oroz MC, Obeso JA. Subthalamotomy for Parkinson’s disease: clinical outcome and topography of lesions. J Neurol Neurosurg Psychiatry. 2018;89(6):572–8.
Lozano A, Hutchison W, Kiss Z, et al. Methods for microelectrode-guided posteroventral pallidotomy. J Neurosurg. 1996;84(2):194–202. 153.
Fry WJ. Use of intense ultrasound in neurological research. Am J Phys Med. 1958;37(3):143–7.
Schlesinger I, Sinai A, Zaaroor M. MRI-guided focused ultrasound in Parkinson’s disease: a review. Parkinson’s Dis. 2017;2017:8124624.
Na YC, Chang WS, Jung HH, Kweon EJ, Chang JW. Unilateral magnetic resonance–guided focused ultrasound pallidotomy for Parkinson disease. Neurology. 2015;85(6):549–51.
Bond AE, Shah BB, Huss DS, Dallapiazza RF, Warren A, Harrison MB, Sperling SA, Wang XQ, Gwinn R, Witt J, Ro S. Safety and efficacy of focused ultrasound thalamotomy for patients with medication-refractory, tremor-dominant Parkinson disease: a randomized clinical trial. JAMA Neurol. 2017;74(12):1412–8.
Martínez-Fernández R, Rodríguez-Rojas R, del Álamo M, Hernández-Fernández F, Pineda-Pardo JA, Dileone M, Alonso-Frech F, Foffani G, Obeso I, Gasca-Salas C, de Luis-Pastor E. Focused ultrasound subthalamotomy in patients with asymmetric Parkinson’s disease: a pilot study. Lancet Neurol. 2018;17(1):54–63.
Sapareto SA, Dewey WC. Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys. 1984;10(6):787–800.
Chung AH, Jolesz FA, Hynynen K. Thermal dosimetry of a focused ultrasound beam in vivo by magnetic resonance imaging. Med Phys. 1999;26(9):2017–26.
Chang WS, Jung HH, Zadicario E, Rachmilevitch I, Tlusty T, Vitek S, Chang JW. Factors associated with successful magnetic resonance-guided focused ultrasound treatment: efficiency of acoustic energy delivery through the skull. J Neurosurg. 2016;124(2):411–6.
Zaaroor M, Sinai A, Goldsher D, Eran A, Nassar M, Schlesinger I. Magnetic resonance–guided focused ultrasound thalamotomy for tremor: a report of 30 Parkinson’s disease and essential tremor cases. J Neurosurg. 2018;128(1):202–10.
Duma CM. Movement disorder radiosurgery–planning, physics and complication avoidance. In: Radiosurgery and pathological fundamentals, vol. 20. Basel: Karger Publishers; 2007. p. 249–66.
Elaimy AL, Arthurs BJ, Lamoreaux WT, Demakas JJ, Mackay AR, Fairbanks RK, Greeley DR, Cooke BS, Lee CM. Gamma knife radiosurgery for movement disorders: a concise review of the literature. World J Surg Oncol. 2010;8(1):61.
Wu A, Lindner G, Maitz AH, Kalend AM, Lunsford LD, Flickinger JC, Bloomer WD. Physics of gamma knife approach on convergent beams in stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 1990;18(4):941–9.
Ganz J. Gamma knife neurosurgery. New York: Springer Science & Business Media; 2010.
Merello M, Nouzeilles MI, Cammarota A, Betti O, Leiguarda R. Comparison of 1-year follow-up evaluations of patients with indication for pallidotomy who did not undergo surgery versus patients with Parkinson’s disease who did undergo pallidotomy: a case control study. Neurosurgery. 1999;44(3):461–7.
de Bie RM, de Haan RJ, Nijssen PC, Rutgers AW, Beute GN, Bosch DA, Haaxma R, Schmand B, Schuurman PR, Staal MJ, Speelman JD. Unilateral pallidotomy in Parkinson’s disease: a randomised, single-blind, multicentre trial. Lancet. 1999;354(9191):1665–9.
Bastian AJ, Kelly VE, Perlmutter JS, Mink JW. Effects of pallidotomy and levodopa on walking and reaching movements in Parkinson’s disease. Mov Disord. 2003;18(9):1008–17.
Hagiwara N, Hashimoto T, Ikeda SI. Static balance impairment and its change after pallidotomy in Parkinson’s disease. Mov Disord. 2004;19(4):437–45.
Schulz GM, Greer M, Friedman W. Changes in vocal intensity in Parkinson’s disease following pallidotomy surgery. J Voice. 2000;14(4):589–606.
Narabayashi H, Maeda T, Yokochi F. Long-term follow-up study of nucleus ventralis intermedius and ventrolateralis thalamotomy using a microelectrode technique in parkinsonism. Stereotact Funct Neurosurg. 1987;50(1–6):330–7.
Kelly PJ, Gillingham FJ. The long-term results of stereotaxic surgery and L-dopa therapy in patients with Parkinson’s disease: a 10-year follow-up study. J Neurosurg. 1980;53(3):332–7.
Diederich N, Goetz CG, Stebbins GT, Klawans HL, Nittner K, Koulosakis A, Sanker P, Sturm V. Blinded evaluation confirms long-term asymmetric effect of unilateral thalamotomy or subthalamotomy on tremor in Parkinson’s disease. Neurology. 1992;42(7):1311.
Cardoso F, Jankovic J, Grossman RG, Hamilton WJ. Outcome after stereotactic thalamotomy for dystonia and hemiballismus. Neurosurgery. 1995;36(3):501–8.
Guridi J, Obeso JA, Rodriguez-Oroz MC, Lozano AM, Manrique M. L-dopa-induced dyskinesia and stereotactic surgery for Parkinson’s disease. Neurosurgery. 2008;62(2):311–25.
Chang JW. Magnetic resonance guided focused ultrasound pallidotomy for Parkinson’s disease. J Ther Ultrasound. 2015;3(S1):O5.
Schlesinger I. MRI guided focused ultrasound thalamotomy for moderate-to-severe tremor in Parkinson’s disease. Parkinson’s Dis. 2015;2015:219149.
Sperling SA, Shah BB, Barrett MJ, Bond AE, Huss DS, Mejia JA, Elias WJ. Focused ultrasound thalamotomy in Parkinson disease: nonmotor outcomes and quality of life. Neurology. 2018;91(14):e1275–84.
Lozano AM, Lang AE, Galvez-Jimenez N, Miyasaki J, Duff J, Hutchison WD, Dostrovsky JO. Effect of GPi pallidotomy on motor function in Parkinson’s disease. Lancet. 1995;346(8987):1383–7.
Demakis GJ, Mercury MG, Sweet JJ, Rezak M, Eller T, Vergenz S. Motor and cognitive sequelae of unilateral pallidotomy in intractable Parkinson’s disease: electronic measurement of motor steadiness is a useful outcome measure. J Clin Exp Neuropsychol. 2002;24(5):655–63.
Lacritz LH, Cullum CM, Frol AB, Dewey RB Jr, Giller CA. Neuropsychological outcome following unilateral stereotactic pallidotomy in intractable Parkinson’s disease. Brain Cogn. 2000;42(3):364–78.
Louw DF, Burchiel KJ. Ablative therapy for movement disorders: complications in the treatment of movement disorders. Neurosurg Clin N Am. 1998;9(2):367–74.
Bell DS. Speech functions of the thalamus inferred from the effects of thalamotomy. Brain. 1968;91(4):619–38.
Wester K, Hauglie-Hanssen E. Stereotaxic thalamotomy--experiences from the levodopa era. J Neurol Neurosurg Psychiatry. 1990;53(5):427–30.
Rossitch E Jr, Zeidman SM, Nashold BS Jr, Horner J, Walker J, Osborne D, Bullard DE. Evaluation of memory and language function pre-and postthalamotomy with an attempt to define those patients at risk for postoperative dysfunction. Surg Neurol. 1988;29(1):11–6.
Hugdahl K, Wester K. Neurocognitive correlates of stereotactic thalamotomy and thalamic stimulation in parkinsonian patients. Brain Cogn. 2000;42(2):231–52.
Duma CM, Deane J. The treatment of movement disorders using gamma knife stereotactic radiosurgery. Neurosurg Clin N Am. 1999;10(2):379–89.
Magara A, Bühler R, Moser D, Kowalski M, Pourtehrani P, Jeanmonod D. First experience with MR-guided focused ultrasound in the treatment of Parkinson’s disease. J Ther Ultrasound. 2014;2(1):11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rotter, J., Cosgrove, G.R. (2020). Parkinson’s Disease: Lesions. In: Pouratian, N., Sheth, S. (eds) Stereotactic and Functional Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-030-34906-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-34906-6_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34905-9
Online ISBN: 978-3-030-34906-6
eBook Packages: MedicineMedicine (R0)