Abstract
Decision-makers strive to reduce health-care costs, improve capacity, and get the best value for every dollar spent in health care. Recently, the published literature has shown the value of enhanced recovery after surgery (ERAS) guidelines from an economic perspective and looked at the return on investment of ERAS programs. Given the initial investment needed to successfully implement an ERAS program, there is value in providing a robust business case for managers and decision-makers. The business case must clearly address the clinical advantages and improvements for patients and clinicians as well as the metrics and value proposition for the site. The challenge is often that the metrics important to decision-makers differ from (or need to be expressed differently than) the metrics important to clinicians. The ability to build a case that clearly conveys the value proposition to both parties is critical to ERAS implementation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- ERAS implementation
- Implementation barriers
- Implementation enablers
- Business case for ERAS
- Multiple guidelines
- Economic value
- Transformational investment
- Value proposition
- Measurable improvement
- Capacity gains
Introduction
Decision-makers strive to reduce health-care costs, improve capacity, and get the best value for every dollar spent in health care. There is ample evidence reported in the literature of health systems achieving major gains, clinically and economically, by implementing a single guideline that modifies perioperative decisions (preoperative, intraoperative, and postoperative). These guidelines have potential to transform perioperative management of ALL surgical patients; however, there is limited documentation of the spread and scale of enhanced recovery after surgery (ERAS) protocols across clinical sites and health systems. Similarly, little information is available about the potential impact on surgical programs and health systems of implementing multiple guidelines across multiple sites. Recently, the published literature has shown the value of ERAS guidelines from an economic perspective and looked at the return on investment of ERAS programs. More can be done to evaluate and expand the economic value—within hospitals and post discharge. Building a case for widespread implementation of ERAS guidelines, and supporting change within health systems, requires a focused approach, a clear implementation and evaluation framework, and a robust business case that conveys the potential impact. These elements are essential to enable evidence-based decision-making about transformational investments.
The Evidence for ERAS
Improving the quality and performance of health care is one of the main challenges facing health systems and governments worldwide. International guidelines for enhanced recovery after surgery (ERAS) have existed for 15 years with well-documented evidence of improvements for individual patients and specific surgical populations [1,2,3,4]. ERAS guidelines outline a series of evidence-informed practices (preoperative, intraoperative, and postoperative) aimed at mitigating adverse effects of surgery using a team-based approach. These practices have been associated with accelerated recovery, resulting in reduced complications and hospital lengths of stay (LOS), fewer readmissions, improved patient experience, and no associated increases in health services utilization [3, 5,6,7,8].
There is ample evidence that ERAS protocols improve patient care and experience and provide economic value to health systems. Across the globe, health systems are adopting a Quadruple Aim approach to improve system performance (patient and provider satisfaction, improved clinical outcomes, and economic value for the health system). Yet, even more health systems would benefit if they adopted ERAS programs within their hospitals [9]. This surgical transformation has been shown to significantly improve system performance—clinically and financially—for almost every major surgical procedure in many centers around the world [10].
Despite this success, uptake is slow, and we know there are millions more surgical patients worldwide who could benefit from ERAS programs. While this observation is noted, it is unclear what the barriers are to advancing uptake and is, therefore, a potential area for further inquiry and research. The evidence does show that by adopting ERAS guidelines, decision-makers can affect positive individual and surgical population outcomes while reducing complications and per-unit costs and freeing up capacity through reduced lengths of stay, readmissions, and overall health services utilization. The evidence points to a health system’s potential to magnify these benefits by systematically implementing the existing research findings and looking at methods to spread and scale ERAS protocols to all surgical patients.
Large-Scale Implementation of Multiple ERAS Guidelines
Few health systems have attempted to implement multiple guidelines system-wide. The United Kingdom’s Enhanced Recovery Partnership Programme (ERPP) included multiple guidelines across multiple sites with good outcomes for surgical patients and the system itself [11]. They describe a system-wide attempt to implement multiple guidelines for several surgical disciplines including orthopedic, urology, colorectal, and gynecologic procedures. Although they did see a positive impact, the authors concluded that a stringent implementation process should be in place to ensure compliance with the guidelines beyond the implementation phase [11]. The Netherlands implemented the ERAS International© Society Colorectal Guideline, using what developed into the ERAS® Society Implementation Program, across 33 sites with results similar to those reported by others in the literature [11, 12]. The ERAS® Society’s implementation approach is modeled after the Institute for Healthcare Improvement’s (IHI) learning collaborative methodology and assists teams with education, data, and process improvements to guide the ERAS implementation at the site [11, 13].
In Canada, in the Province of Alberta, Alberta Health Services (AHS) has implemented multiple ERAS® Society guidelines across nine major sites and nine program areas. AHS adopted the ERAS® Society approach by using the evidence-based guidelines and implementation plans based on IHI methodology and adopting the ERAS International© Society’s Interactive Audit System (EIAS) for data collection, audit, and feedback. Results from Alberta have been very positive and show value across all Quadruple Aim goals: patient and provider satisfaction, improved clinical outcomes, and economic value for the health system [3, 5, 14, 15].
Barriers and Enablers of ERAS Implementation
Gramlich et al. studied the implementation of ERAS protocols across six colorectal sites to better understand the barriers and enablers to implementation and to maximize guideline compliance [3]. High compliance was identified as being important to achieving results, especially when considering the use of multiple guidelines within and across surgical centers [16, 17]. They used two frameworks to guide their review: (1) the Theoretical Domains Framework (TDF) and (2) the Quality Enhancement Research Initiative (QUERI) Framework [18, 19]. The team applied rigorous methods for implementation that not only led to behavior change and helped sustain that change but also has supported the development of spread and scale opportunities within Alberta [3, 20,21,22].
Mapping barriers and facilitators across the different domains—patient, provider, and system—provides insight into the change strategies that might best drive compliance [3]. McLeod et al. identified four key ingredients for successful guideline adoption: (1) clinical champions, (2) good communication and collaboration, (3) organizational management, and (4) use of audit and feedback processes and standardization of orders [23]. This research is in keeping with work done by Pearsall et al. who looked at barriers and facilitators to ERAS implementation across four hospital sites [17]. They identified barriers to implementation that included limited financial and human resources to ensure audit and feedback, absence of change management strategies and supports for standardization (e.g., standardized order sets), poor communication and collaboration, and absence of clinician or organizational champions. These elements were considered essential to affect change. Standardized patient education and family involvement in the process were also identified as important components. This information is critical to successfully spread and scale ERAS guidelines as implementation is complex and typically requires multiple strategies to achieve the objectives. Unfortunately, there is no “one-size-fits-all” approach, and it is important to understand what is required to change behavior at the provider level, site level, and system level. For example, customized audit and feedback of individual performance based on compliance with ERAS practices and protocols might be helpful at a provider level. At the site level, the approach (e.g., standardized fasting guidelines as part of preadmission process) may be different than what is required at the system level (e.g., standardized patient education materials for all sites and standardized education for all staff across the health system).
Monitoring Compliance and Outcomes
Audit and feedback mechanisms are an important component of the implementation program as they provide a means of regularly evaluating outcomes (e.g., LOS, surgical complications, and patient-reported outcome measures) and compliance with ERAS guidelines [3]. While some programs have adopted the ERAS® Society Interactive Audit System (EIAS), several methods of measuring ERAS impact have been used worldwide with little evidence to suggest one method is superior. The essential ingredient to successful implementation is measurement and feedback that provides meaningful data to measure improvements in practice and key outcomes. Moreover, it is necessary to clearly outline those planned improvements in the business case that are proposed to decision-makers. Measurement and feedback are important as tools to manage both the individual patient progress and team progress; the EIAS system was designed to provide near-real-time feedback to clinicians and teams. When instituting the EIAS, teams could use the feedback to manage individual patient progress and to better understand where the team had achieved compliance with the ERAS elements. Studies have shown that high levels of compliance with ERAS guidelines provide better results [16] and can help sustain the clinical and economic gains achieved. It may be surprising for decision-makers that a sum of relatively simple perioperative measures, such as early mobilization and oral nutrition, impacts patient outcomes to the extent that has been documented. However, these results highlight the importance of engaging health-care providers in refining and implementing standards and processes that lead to quality improvements and better value over time [24,25,26].
Developing a Model for Spread and Scale
In evaluating barriers and facilitators of ERAS implementation, Gramlich et al. developed a model to spread and scale ERAS protocols [3]. The model suggests that strategies to achieve compliance with ERAS guidelines can be applied across many surgical areas to support widespread implementation. The model includes four elements (Fig. 61.1):
-
Nutrition
-
Mobilization
-
Fluid management—including modern fasting guidelines and carbohydrate loading
-
Pain and symptom control
The model highlights patient-focused information and education as an important enabler to successful spread and scale. This finding is consistent with several studies that have reported the need for better patient and family education and involvement—especially in the preoperative and postoperative phases of the surgical experience. However, there is little evidence that these changes have made their way into clinical systems. Few studies have reported any patient-reported outcomes, and this is viewed as a shortcoming of the ERAS evaluation. Patient-centered care is an important concept among health providers, and most health systems monitor patient-reported outcomes as part of their quality management systems. The absence of patient-reported outcomes is currently a gap in the ERAS literature and evaluation tools and an area for future research, especially for recovery beyond the postoperative stay [17, 27].
Considering and Preparing a Business Case for ERAS Implementation
Given the initial investment needed to successfully implement an ERAS program (i.e., to develop evidence-based guidelines, an implementation approach, and a measurement system to ensure audit and feedback), there is value in providing a robust business case for managers and decision-makers. The business case must clearly address the clinical advantages and improvements for patients and clinicians as well as the metrics and value proposition for the site. The challenge is often that the metrics important to decision-makers differ from (or need to be expressed differently than) the metrics important to clinicians. The ability to build a case that clearly conveys the value proposition to both parties is critical to ERAS implementation.
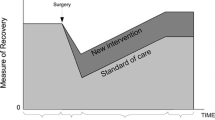
To demonstrate impact while describing the value to the organization, the business case must consider the patient, providers, organization, and the overall health system [3]. However, even when evidence is expressed in economic terms, health administrators have found it difficult to relate these gains to real system savings. Most of these gains are described in terms of freed-up capacity (bed days saved), improved productivity (decreased readmissions), improved safety (reduced complications), and cost-effectiveness (health system savings and greater value for each dollar invested).
Given the capacity strains and economic pressures that most institutions experience, gains in capacity are typically short-lived because freed-up surgical inpatient beds are rapidly filled by the ever-increasing demand of other programs and services. This masks the impact of ERAS, making it appear somewhat theoretical; without the ability to close surgical beds, the clinical gains do not necessarily translate into real cash savings for the system. So for many decision-makers (especially those with relatively fixed, global budgets), the case for investing in ERAS may be more difficult to justify from a financial perspective despite the positive clinical gains.
Making the case for more investment into ERAS is challenging, and it can help to take a broad and long-term view. As more complex patients are treated in hospitals with surgery, and the increasing cost to add more physical capacity is prohibitive, administrators must seek innovative solutions that can advance productivity and capacity gains within existing hospital footprints. While innovative solutions (such as the ERAS ingredients) cannot be expected to reduce total health-care expenditures in absolute terms, they do, however, have the potential to free up a significant amount of capacity that may enable health systems to significantly increase surgical throughput. Doing so results in the provision of more timely hospital service to other patient populations. The potential to significantly increase patient throughput with existing hospital capacity could be realized by deploying the innovative solution at scale. For instance, by applying the key ERAS ingredients to all surgical patients at a particular hospital, it may be possible to provide decision-makers with a credible quantitative forecast that shows that more patients can be treated within the existing hospital capacity at a fraction of the cost of the next-best (though economically unlikely) alternative—that is, of adding more physical capacity. Clinical appropriateness (using evidence-based guidelines) and improving care efficiency (reducing unwarranted variation and cost) are fundamental drivers to transformational change and to becoming a high-performing health system—something that the case for ERAS has proven.
Building the Case for ERAS in Alberta
Alberta Health Services (AHS) is Canada’s first province-wide, fully integrated health system. Created in 2008, AHS is responsible for delivering health services to more than 4 million people. In June 2012, AHS introduced Strategic Clinical Networks™ (SCNs), which are collaborative teams of clinicians, researchers, and stakeholders to advance innovation across the province’s health system. Specifically, their mandate and goals are to achieve best outcomes; seek greatest value for money; and engage clinicians, patients, and health providers in all aspects of the work. SCNs are led by clinicians, driven by clinical needs, based on measurement and best evidence, and supported by research expertise, infrastructure, quality improvement, and analytic resources [28].
Quantifying the value or return on investment (ROI) of quality and patient safety initiatives is part of the SCN mandate as a means of becoming a higher-performing health system. In Alberta, more than 275,000 surgical procedures are performed annually in 58 surgical facilities, with 16 of these performing 85% of major surgical procedures in the province [5, 15, 29]. Given the mandate of the SCNs, the diabetes, obesity and nutrition, and the surgery SCNs built a business case and demonstration project to implement the ERAS® Society’s international guidelines [24]. Since 2013, AHS has implemented multiple ERAS guidelines at nine sites and across nine program areas. Clinical and economic evaluations have shown improvements associated with accelerated recovery, including reduced complications, shorter length of stays, improved patient experience, and reduced health service utilization [5, 14, 15]. Alberta showed that the health system savings were estimated at $2,290,000 (range $1,191,000–$3,391,000); after factoring the project costs of implementing ERAS, the net cost savings of ERAS was $1768 (range from $920 to $2619) per patient. In terms of the value proposition associated with this investment, the analysis demonstrated that every $1 invested in ERAS programs would bring about $4 in value to the system [5].
For AHS, maximizing value is a fundamental principle to creating high performance in the health system. Specifically, AHS has described organizational value as a function of:
-
Quality, safety, and outcomes
-
Process improvements
-
Timing of expected benefits
-
Budget/financial impact
-
System readiness
-
Value for money
Therefore, to build the business case for ERAS, these six dimensions must be described and, where possible, quantified to best understand the overall value that a particular innovation contributes to the system. As ERAS results in a lower cost per patient (quality, safety, and outcomes), it is logical to assume that from a spread and scale perspective, the more patients enrolled, the more organizational value will be created. Important factors for ERAS long-term success are changes in management of care processes and time investment to form multidisciplinary and interprofessional ERAS teams along with the use of continuous audit and feedback.
Building the case for ERAS started by developing a change proposal that focused on “doing the right thing” by identifying and proposing an approach that addressed the quantifiable gap in health system performance. From there, the SCNs developed a high-quality operational and financial plan to make the solution work in practice. To achieve this, the team developed a framework (with support from AHS’s innovation and research management and finance teams) that provides a comprehensive plan that supported both clinical implementation and decision-maker requirements.
The framework (Fig. 61.2) consists of five components:
- Step 1.:
-
Problem Identification—Identify the specific problem to focus on, defined as the gap between current performance and potential performance. Use a quantifiable measure that relates to the organization’s goals and priorities (e.g., Quadruple Aim).
- Step 2.:
-
Option Analysis—Review and select a solution from a range of options. Evaluate the options based on clinical input and research findings. The analysis should include a well-supported estimate of the magnitude of the potential impact in terms of the quantifiable measure (identified in Step 1) and be based on evidence in the literature (e.g., ERAS international guidelines).
- Step 3.:
-
Preliminary Projections—Use available data to complete a preliminary forecast of projected performance improvement, showing how the gap between current and potential performance (from Step 1) will be reduced. In Alberta, the findings from the UK study provided options (Step 2) and data from which to estimate the order of magnitude that could be achieved with full-system implementation. This data was used to estimate potential benefit that would accrue to Alberta Health Services (AHS), based on Alberta surgical volumes.
- Step 4.:
-
Operational and Financial Impact Assessment (OFIA)—Evaluate the anticipated impacts of implementing the solution on the health-care system by conducting a detailed OFIA. The OFIA should be informed by consultation with expert representatives of sites, services, and units that would be potentially affected by the implementation. The OFIA should also outline plans to mitigate any adverse impacts on other areas of the system.
- Step 5.:
-
Business Case Development—Describe the potential benefits and costs of implementation (i.e., the value proposition), include a clear recommendation, and request a decision. The business case should also summarize all managerial actions (e.g., financial transfers, policy changes, communications support) necessary to support implementation and include a plan to review the implementation decision at a defined time and according to the project’s performance (based on quantitative measures defined in the business case).
A business case for transformational investments must provide clear and complete information about the project for decision-makers at a level of detail that enables them to understand exactly (1) what the project offers in terms of progress toward their goals and (2) what is needed in terms of system resources to deliver on that promise.
ERAS Implementation to Date in Alberta
As mentioned, AHS has implemented ERAS guidelines at nine sites in nine program areas. Alberta’s three major teaching hospitals have adopted multiple guidelines in several surgical program areas, including orthopedics, gynecology, liver, major head and neck oncology, colorectal, pancreas, cystectomy, and breast reconstruction. Several of the surgeons in Alberta have been part of, or have led the development and testing of, the international guidelines [15, 30,31,32,33], and there are plans underway for further guideline development.
The AHS investment in ERAS has been a direct result of having a clear and compelling case for change and a comprehensive implementation plan. The implementation plan was built as a result of research conducted in Alberta to understand the barriers and facilitators of multiple guideline implementations. This research was supported by a Partnership for Research and Innovation in the Health System (PRIHS) grant. Important ingredients that contributed to success included the surgeon, anesthesia and local administrative champions, standardized approaches for education and implementation, and a robust audit and feedback capability. A systems perspective and structured approach to communications across multiple sites was also considered critical to the project’s success [3, 15].
In building the case for investment in ERAS, there is compelling evidence published on the value of single-protocol implementation. However, if there is an inability to utilize the freed capacity/resources as the fuel to sustain continued transformative change, then, unfortunately over time, compliance with the guidelines can be expected to deteriorate. In an environment of increasing scarcity and scrutiny of health-care budgets, non-compliance can occur if efficiency gains are completely utilized toward other priorities during corporate budgeting processes. This ultimately can cause increased pressure, staff workload, change fatigue, and operational risk, and it also may inhibit quality improvement. An approach that may help find the balance between fueling continued transformative change and other organizational priorities is adopting a benefits sharing approach.
Incenting Change and Quality Improvement Through Benefit Sharing
In Alberta, the Institute for Health Economics (IHE) conducted a rapid review to understand how health systems were building incentives and policy to recognize and reward quality improvement efforts [34]. The review revealed two main types of incentives: those described as “gain sharing” and those described as “shared savings.” Gain sharing is defined as an arrangement with employees where the organization shares a portion of the savings (cost reductions) attributable to the efforts of those employees and where the rewards are allocated back to teams or individuals based on the improvements. Gain sharing includes concepts such as pay-for-performance, global payments, bundled payments, and pay-for-coordination payments geared at promoting provider accountability [34]. Many of these efforts have been introduced across several health systems within European countries, with limited published literature on the outcomes/outputs of these efforts.
With the recently adopted Affordable Care Act in the United States, accountable care organizations (ACOs) and payment schemes to reward better outcomes have proliferated. The major risks and benefits associated with gain-sharing methods include complicated payment schemes, difficulty with the attribution of outcomes, and potential conflicts with providing monetary payback to individual providers. Gain-sharing programs require measurable and clearly stated goals, transparent data sharing among stakeholders, and safeguards against inappropriate referrals or reductions in care quality [34].
Alternatively, shared savings (also referred to as benefits sharing) is described as an approach that links an organizations’ planning and budgeting process to employee-created, operation-led performance improvements. There are two types:
-
One-sided (upside) risk model: Providers (usually hospitals or physician practices) would provide decision -makers with specific plans/proposals that would have them retain within their clinical business unit some pre-defined portion (either a specific amount or a particular proportion) of planned operational or financial performance gains in the event that those planned gains were actually realized. The proposal would outline how the business unit would be able to fuel further performance improvements (i.e., to create further value) as a direct result of retaining these gains. While business units would be allowed to propose the retention of some of the planned gains actually realized, they would not, however, be subject to any sanctions or penalties in the event that they were not able to achieve planned performance gains.
-
Two-sided (upside and downside) risk model: Under this type of arrangement, providers would be able to provide decision-makers with specific plans/proposals that would have them retain within their clinical business unit some predetermined portion of planned gains to fuel further performance improvements. Similar to the one-sided (upside) risk model discussed above, providers would be allowed to propose the retention of some of the planned gains actually realized. Unlike the one-sided (upside) risk model, however, the two-sided risk model would make the provider more accountable for the realization of planned results in that their proposal would be expected to specify the mechanism by which the decision-maker would recover a portion of the investment in the event that actual, measurable performance improvement was materially less than planned [34].
In the IHE review, shared savings are described as models that “encourage collaboration among providers to reduce the use of health services and improve quality in a population over time. This reimbursement strategy is well suited to the ethos of ACOs because it incentivizes providers to develop effective primary care prevention and population health management strategies, with the aim of decreasing utilization by avoiding hospital admissions, reducing readmissions, and improving care coordination” [34]. Because of its focus on clinical improvement, the shared savings approach (especially the balanced two-sided risk model, above) encourages providers to “do the right thing” and then provides the financing mechanism to “make it work.”
There is little published literature on the use of incentives to drive quality improvements in health systems. The largest number of studies comes from the United States as a result of the policy changes in their system related to the Affordable Care Act . “In Canada there is no ACO equivalent, and it is rare for front-line workers to be given responsibility for initiating change or to be compensated directly for such efforts [35]. Although the highly regulated nature of Canada’s provincial health systems is a potential barrier to gain sharing and shared savings initiatives, there are examples in both Ontario and Alberta Health Services that are experimenting with these approaches” [34].
Alberta Health Services has recently adopted a benefit-sharing strategy as part of its annual resource allocation and budgeting process for the province. Under the new approach, clinical teams that propose the adoption of innovative solutions to drive measurable improvements can apply for benefits sharing. Under benefits sharing, benefits are not automatically taken back into the corporate budgeting process and used for other organizational purposes, but rather are a source of capacity or resources (i.e., fuel) to enable clinical programs across AHS (including the program leading the innovation) to reinvest some or all of those measured gains to help them improve organizational value (i.e., manage their business) by enabling them to manage priority clinical pressures and improve quality or patient outcomes. AHS notes that efficiency gains are those that are predominantly nonmonetary benefits (e.g., cost avoidance, freed capacity, productivity gains) especially in the short term due to the issue of passive reallocation where the redeployment of capacity/resources freed by one particular clinical program area is simply exhausted by other programs which consume that capacity without specific approvals or plans. In order to ensure that providers share in both upside and downside risk, the AHS approach will require programs to track actual performance against the original improvement forecast contained in the business case as a feedback mechanism that will help inform the subsequent budget cycle. Over a longer time horizon, possible real budget adjustments may occur at this step, which would translate capacity gains into actual monetary savings enabling the reallocation of resources to achieve other organizational priorities (clinical and nonclinical).
For ERAS, the case for change was funded by AHS, and the organization has reacted positively with respect to the return (i.e., measured benefits) that it has realized on its investment in ERAS. Moreover, several clinicians have stepped up to drive the change clinically and through their contributions to the international guideline development. With the progress that has been made in guideline implementation, it is now the time to apply shared savings principles, the newest concept of ERAS for all , ensuring that all surgical patients across the province are exposed to the guideline fundamentals. Using Gramlich et al.’s work on barriers and facilitators, the business case for change will address issues at the individual, site, and system levels. Using the AHS framework for change proposals (outlined previously), we can now better articulate the benefits that can be expected, understand what clinical and operational changes are required to enable teams to sustain operational and financial performance results, and compare those results to the site-specific deployment plans originally set out in the business case.
Conclusion
In conclusion, the ability to spread and scale ERAS international guidelines is promising, and health systems should consider how to spread and scale this innovation to ensure ERAS for all. In doing so, the ability to demonstrate surgical transformation and the value proposition associated with the investment will likely emerge. However, in building the case for change, a robust methodology is recommended to help decision-makers better understand the value that can be created for the health system through the planned deployment of this innovative solution. By clearly articulating and quantifying expected operational and financial results, it will be easier for providers and decision-makers to identify and agree upon strategies for sustaining performance results over the longer term.
Little research has been published about the implementation of multiple guidelines across multiple sites and what levers are being used to maintain or improve outcomes. Studies that examine multiple guideline implementation and return on investment are necessary to better describe the value and the process required to achieve system-wide adoption and change. Furthermore, while some studies outline the value of single-protocol adoption, the impacts beyond the hospital have been poorly studied. Nonetheless, there is promise that ERAS implementation not only produces acute care value but also has an impact on overall health system utilization.
Finally, the role of patients as part of the ERAS team and the ability to better measure and understand their reported outcomes and experience would also add strength to a business case for change. For example, decision-makers require a comprehensive picture of the expected value that will be created should they decide to finance the continued deployment of the ERAS guidelines to all surgical patients in Alberta. This picture can be created by putting together a robust operational and financial forecast of future performance and documenting the case for change and how the health systems will incent performance in order to achieve and sustain planned gains.
References
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–41.
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8.
Gramlich LM, Sheppard CE, Wasylak T, Gilmour LE, Ljungqvist O, Basualdo-Hammond C, et al. Implementation of enhanced recovery after surgery; a strategy to transform surgical care across a health system. Implement Sci. 2017;12(1):67.
Adamina M, Kehlet H, Tomlinson GA, Senagore AJ, Delaney CP. Enhanced recovery pathways optimize health outcomes and resource utilization: A meta-analysis of randomized controlled trials in colorectal surgery. Surgery. 2011;149(6):830–40.
Thanh NX, Chuck AW, Wasylak T, Lawrence J, Faris P, Ljungqvist O, et al. An economic evaluation of the Enhanced Recovery After Surgery (ERAS) multisite implementation program for colorectal surgery in Alberta. Can J Surg. 2016;59(6):415–21.
Roulin D, Donadini A, Gander S, Griesser AC, Blanc C, Hübner M, et al. Cost-effectiveness of the implementation of an enhanced recovery protocol for colorectal surgery. Br J Surg. 2013;100(8):1108–14.
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced reovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24(3):466–77.
Dautremont JF, Rudmik LR, Yeung J, Asante T, Nakoneshny SC, Hoy M, et al. Cost-effectiveness analysis of a postoperative clinical care pathway in head and neck surgery with microvascular recirculation. J Otolaryngol Head Neck Surg. 2013;42:59.
Sikka R, Morath JM, Leape L. The Quadruple Aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10.
Stowers MD, Lemanu DP, Hill AG. Health economics in enhanced recovery after surgery programs. Can J Anaesth. 2015;62(2):219–30.
Simpson JC, Moonesinghe SR, Grocott MP, Kuper M, McMeeking A, Oliver CM, et al. National Enhanced Recovery Partnership Advisory Board. Enhanced recovery from surgery in the UK: an audit of the enhanced recovery partnership program 2009–2012. Br J Anaesth. 2015;115(4):560–8.
Gillissen F, Hoff C, Maessen JM, Winkens B, Teeuwen JH, von Meyenfeldt MF, et al. Structured Syncronyous Implementation of an enhanced recovery program in elective colonic surgery in 33 hospitals in the Netherlands. World J Surg. 2013;37(5):1082–93.
Institute for Healthcare Improvement. The Breakthrough Series: IHI’s collaborative model for achieving breakthrough improvement. IHI Innovation Series White Paper. Boston: Institute for Healthcare Improvement. 2003.
Nelson G, Kiyang LN, Crumley ET, Chuck A, Nguyen T, Faris P, et al. Implementation of enhanced recovery after surgery (ERAS) across a provincial healthcare system: the ERAS Alberta Colorectal Surgery Experience. World J Surg. 2016;40(5):1092–103.
Bisch SP, Wells T, Gramlich L, Faris P, Wang X, Tran DT, et al. Enhanced recovery in gynecologic oncology: system-wide implementation and audit leads to improved value and patient outcomes. Gynecol Oncol. 2018;151(1):117–23.
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J, Enhanced Recovery After Surgery Study Group. Adherence to the enhanced recovery after suregery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146(5):571–7.
Pearsall EA, Meghji Z, Pitzul KB, Aarts MA, McKenzie M, McLeod RS, et al. A qualitative study to understand the barriers and facilitators in implementing an enhanced recovery after surgery program. Ann Surg. 2015;261(1):92–6.
Stetler CB, McQueen L, Demakis J, Mittman BS. An organizational frameworkand strategic implmentation for system-level changeto enhance research-based practice: QUERI Series. Implement Sci. 2008;3:30.
Birken SA, Powell BJ, Presseau J, Kirk MA, Lorencatto F, Gould NJ, et al. Combined use of the Consolidated Framework for Implementation Research (CFIR) and the Theoretical Domains Framework(TDF): a systematic review. Implement Sci. 2017;12(1):2.
Brehaut JC, Colquhoun HL, Eva KW, Carroll K, Sales A, Michie S, et al. Practice feedback interventions; 15 suggestions for optimizing effectiveness. Ann Intern Med. 2016;164(6):435–41.
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovation within service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629.
McLeod RS, Aarts MA, Chung F, Eskicioglu C, Forbes SS, Conn LG, et al. Development of an enhanced recovery after surgery guideline and implementation strategy based on the knowledge-to-action cycle. Ann Surg. 2015;262(6):1016–25.
Noseworthy T, Wasylak T, O’Neill BJ. Strategic clinical networks: Alberta’s response to the triple aim. Healthc Pap. 2016;15(3):49–54.
Verma A, Bhatia SA. Policy framework for health systems to promote triple aim innovation. Healthc Pap. 2016;15(3):9–23.
Bernstein JA, Friedman C, Jacobson P, Rubin JC. Ensuring public health’s future in a national-scale learning health system. Am J Prev Med. 2015;48(4):480–7.
Gillis C, Gill M, Marlett N, MacKean G, GermAnn K, Gilmour L, et al. Patients as partners in enhanced recovery after surgery: a qualitative patient-led study. BMJ Open. 2017;7(6):e017002.
Noseworthy T, Wasylak T, O’Neill B. Strategic clinical networks in Alberta: structures, processes and early outcomes. Healthc Manage Forum. 2015;28(6):262–4.
Nelson G, Kiyang LN, Chuck A, Thanh NX, Gramlich LM. Cost impact analysis of Enhanced Recovery After Surgery program implementation in Alberta colon cancer patients. Curr Oncol. 2016;23(3):e221–7.
Nelson G, Altman AD, Nick A, Meyer LA, Ramirez PT, Achtari C, et al. Guidelines for pre-and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations – Part 1. Gynecol Oncol. 2016;140(2):313–22.
Nelson G, Altman AD, Nick A, Meyer LA, Ramirez PT, Achtari C, et al. Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations – Part II. Gynecol Oncol. 2016;140(2):323–32.
Dort JC, Farwell DG, Findlay M, Huber GF, Kerr P, Shea-Budgell MA, et al. Optimal perioperative care in major head and neck cancer surgery with free flap reconstruction. JAMA Otolaryngol Head Neck Surg. 2017;143(3):292–303.
Temple-Oberle C, Shea-Budgell MA, Tan M, Semple JL, Schrag C, Barreto M, Blondeel P, Hamming J, Dayan J, Ljungqvist O, ERAS Society. Consensus review of optimal perioperative care in breast reconstruction: Enhanced Recovery after Surgery (ERAS) Society Recommendations. Plast Reconstr Surg. 2017;139(5):1056e–71e.
Scott A, Tjosvold L, Chojecki D. Gainsharing and shared savings strategies in the healthcare setting: evidence for effectiveness. Edmonton, Alberta, Canada: Institute of Health Economics, November 18, 2016. Available from: https://www.ihe.ca/advanced-search/gainsharing-and-shared-savings-strategies-in-the-healthcare-setting-evidence-for-effectiveness.
Bear R. Heads up: there are lessons for Canada in U.S. health care reform. Healthy Debate. December 5, 2012. Available from: https://healthydebate.ca/opinions/heads-up-there-may-be-lessons-for-canada-in-u-s-health-care-reform.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wasylak, T., Osiowy, K., Chuck, A. (2020). Enhanced Recovery After Surgery – Making the Business Case: Economics – The Alberta Experience. In: Ljungqvist, O., Francis, N., Urman, R. (eds) Enhanced Recovery After Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-33443-7_61
Download citation
DOI: https://doi.org/10.1007/978-3-030-33443-7_61
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-33442-0
Online ISBN: 978-3-030-33443-7
eBook Packages: MedicineMedicine (R0)