Opinion statement
Vestibular rehabilitation of persons with peripheral and central vestibular disorders requires a thorough evaluation and a customized plan of care. Collaboration of the various members of the treatment team optimizes outcomes. Early intervention appears to be better than referring patients who have developed chronic symptoms of balance loss, dizziness, anxiety, and depression. There is a body of emerging evidence that supports that the central nervous system has the capability to reweigh sensory inputs in order to improve function. There continues to be a dearth of knowledge related to how to treat persons with otolithic dysfunction as compared to those with semicircular canal damage. With the use of vestibular rehabilitation, patients are less likely to fall, are less dizzy, balance and gait improve, and quality of life is enhanced. Recent Cochrane reviews and a clinical practice guideline support the use of vestibular rehabilitation for persons with vestibular dysfunction. Typical symptoms and their management including dysregulated gait, falling, fear of falling, increased sway in standing, visual blurring, symptoms with complex visual scenes in the periphery, and weakness are all discussed with ideas for intervention. Any patient with a vestibular disorder may benefit from a trial of vestibular rehabilitation. A discussion of recent evidence and innovations related to vestibular rehabilitation is also included.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular rehabilitation has been practiced for almost 70 years [1, 2], yet evidence related to its efficacy and effectiveness has exponentially increased over the last 10–15 years [3–38, 39•, 40]. A recent Cochrane review reports that there is moderate to strong evidence to support the use of vestibular rehabilitation for persons with vestibular disorders [41••]. Authors of a systematic review suggest that there was moderate evidence to support balance and gaze stability type exercises in persons with bilateral vestibular loss based on level II and III evidence [42]. Vestibular rehabilitation typically consists of the provision of a customized exercise program targeted toward the patient’s specific needs. Patient education and psychological support are also key elements to optimal recovery. Anxiety and fear can be associated with dizziness and balance dysfunction in humans and in animal models, ultimately affecting quality of life [43–45].
Home exercises are almost always incorporated into the persons care plan in order to optimize the effectiveness of the exercise program. Exercises are typically chosen to specifically address the person’s goals and are incorporated as much as possible into functional activities in order to maximize exercise compliance [46]. The frequency, optimal treatment duration, and total number of physical therapy visits for best results are unknown. The clinical practice guideline (CPG) for vestibular hypofunction suggests that the number of visits may need to be varied based on comorbidities that can affect movement and psychologic functioning [47••].
Factors that affect recovery
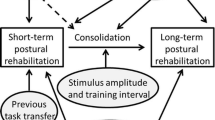
Movement is essential for recovery of function in persons with vestibular disorders. Evidence suggests that rehabilitation programs should be active [48, 49], should begin early after vestibular insult, focus on optimizing plasticity within the brain, be customized especially related to the persons sensory and motor abilities plus cognitive functioning, be progressed with care, be designed to decrease stress and anxiety, be motivating, plus be progressed via changes in the context of the task and the background environment [50]. Negative factors that affect recovery include migraines, sensory loss, visual comorbidities, cognition, sensitivity to motion, psychologic factors, and comorbid central pathology.
A list of common symptoms reported in persons with vestibular disorders is included in Table 1. Patient diagnosis and laboratory findings are very important in determining prognosis, yet even with the same diagnosis/lab findings, the presenting symptoms and functional limitations are variable from person to person. Common symptoms that will be discussed in persons with vestibular disorders include dysregulated gait, falling, fear of falling, impaired ability to stand with excess sway, visual blurring with head movement, increased symptoms with movement in the periphery, and weakness.
Dysregulated gait of persons with peripheral and central vestibular disorders
Gait speed alone is a powerful marker of patient health, regardless of diagnosis [51]. Generally, people who walk faster are healthier and live longer [51]. Persons with vestibular disorders have disordered gait [52, 53]. At the completion of a vestibular rehab program, persons with vestibular disorders generally walk faster and with less variability [37, 54, 55].
Head movements during gait are particularly difficult for persons with vestibular disorders as they often veer with head movement and become dizzy. Overall, walking with head movements increases instability in persons with vestibular disorders [56], but head movements need to be encouraged as patients can develop cervical pain from trying not to move their heads. Cervical range of motion can be affected adversely which can negatively affect function in persons with vestibular disorders.
Persons with unilateral and bilateral vestibular loss often walk “en bloc” with trunk and neck stiffness in order to minimize the amount of head movement during gait. When they move their head during gait, many patients become unstable and lose their balance plus can experience dizziness. The head/trunk stiffness may be a result of the decreased vestibulo-ocular reflex (VOR) gain, which will result in visual blurring with head movement. The disordered strategy of attempting to keep the body stiff during walking is one that is actively managed with a good rehab program. Exercises to increase trunk/head movement are encouraged in order to improve the VOR gain, to decrease pain from trying to keep the body/head rigid, and to improve overall gait function [46].
A new intervention to improve gait in older adults includes the “On the Move” exercise program designed by Brach et al. to enhance the rhythm of a person’s gait [57–59]. The exercises consist of movements performed while standing and walking whereby the person is asked to move forward, backward, and to the side over and around objects in a rhythmical fashion with variable practice. The concept is to teach the older adult to “relearn” how to move efficiently during gait and to incorporate normal timing into their ambulation. Although not tested with persons with vestibular disorders, persons with dizziness and balance problems often experience gait instability during the performance of active head movements and may benefit from this new exercise program.
Augmented feedback including auditory, vibrotactile, and somatosensory feedback have shown some promising results with persons with vestibular disorders during standing trials and gait. Basta et al. [60] demonstrated that tandem walking with auditory feedback improved postural control during tandem walking on a foam surface compared to others who performed the same exercises with no feedback. Others have attempted to utilize auditory and vibrotactile feedback to aide in postural control with persons with vestibular disorders [61–63]. Vibrotactile feedback can enhance postural control and improve gait [64, 65]. A recent development is the use of a smart phone which delivers vibrotactile cues as a balance aide [66]. The goal of vibrotactile feedback is to decrease a person’s fall risk and improve their walking, yet there continue to be concerns about whether vibrotactile feedback will make people more “stiff” during gait.
Falls in persons with vestibular disorders and older adults
Falls occur in persons with vestibular disorders. There is emerging evidence having a vestibular disorders and falling are related [67, 68]. There was a 12-fold increase in the odds of falling in persons over the age of 40 who had reported dizziness within the last year [67]. Balance rehabilitation has been shown to reduce the risk of falling in older persons [19, 69, 70]. Several authors have reported that persons with vestibular disorders are at less risk for falling after rehabilitation [7, 16, 19, 22, 26, 37].
Arhythmicity of gait has been related to falls in seniors [58, 71, 72]. It is not clear if falls and arhythmicity of gait are related in persons with vestibular disorders; however, it is clear that persons with vestibular disorders have less smooth gait when asked to walk while moving their heads, especially in the yaw and pitch planes compared with control subjects [73]. Generally, instability of gait during head movement in the pitch plane is more related to reported falls in persons with vestibular disorders [73].
Interestingly, of the tests and measures that Verreeck et al. utilized, the number of step outs during tandem walking clearly differentiated the older adults (those ≥50 years of age) who underwent rehab versus the group that were provided with the home exercise program [38]. One of the problems often noted in vestibular rehabilitation is that there is a ceiling effect on many of the gait and balance measures, especially in younger subjects [65, 74]. Noting the number of step outs during tandem walking may add value in discriminating if a person is improving [38]. Another possible means to assess fall risk in older adults with multisensory dizziness and need for rehabilitation is via the head shake test. Vestibular asymmetry, as measured via the head shake test, has been related to increased risk of falls [75, 76].
There is promising evidence that vestibular rehabilitation can reduce falls in persons with vestibular hypofunction and benign paroxysmal positional vertigo (BPPV) [38, 77]. One year after performance of the canalith repositioning maneuver, subjects reported fewer falls than the year prior to repositioning [78]. Performing a careful fall history is imperative during the examination of a person with a vestibular disorder.
Reduction in the number of falls can be achieved thru balance/strengthening exercises and/or Tai Chi, although the exercise programs must be of sufficient duration to effectively change strength and balance. Early efforts of the use of Tai Chi with persons with vestibular disorders demonstrated improvements in balance but no changes in perceived dizziness with the exercise program [22].
Exercises designed to challenge a person’s balance are indicated in order to reduce fall risk. Sitting exercises are not nearly as effective at decreasing falls as exercises in upright stance or gait, as balance is not generally challenged during supported sitting exercises. Reaching outside of one’s base of support is essential for persons with vestibular disorders in order to maximize their functional capabilities and in order to learn how far they can optimally move without a loss of postural control.
Fear of falling
Although little has been written about fear of falling specifically in persons with vestibular disorders, it is a concern. Fear of falling is primarily a concern in older persons with vestibular disorders but can be a consideration in younger patients. Fear of falling limits peoples’ willingness to move and participate in their communities. Persons with bilateral vestibular hypofunction fall frequently compared to age-matched controls, and persons with central vestibular disorders are at higher risk for falling because of their neurologic comorbidities [56]. The most utilized instrument in the vestibular literature to quantify fear of falling is the Activities-specific Balance Confidence (ABC) scale [79], although the Falls Efficacy Scale International (FES-I), which is commonly used in Europe, was recently validated for persons living with vestibular disorders [80].
Mounting evidence suggests that secondary factors such as fear and anxiety will affect long-term rehab outcomes if persons do not move after a vestibular event [81, 82]. Depression has also been noted in persons with vestibular disorders [81–83], possibly as a result of their lack of movement and fear of becoming dizzy or falling when they move.
Asking a patient if they are afraid of falling appears to have little value. A yes/no answer does not seem to probe deep enough to provide the clinician with valuable information. The use of scales like the ABC and the FES-I assists in quantifying their fear and is also helpful for goal setting. The goal of a physical therapy intervention program is to decrease fear of falling. If people feel more confident, the hope is that they are more willing to move and participate in their communities.
Working on reaching and moving toward the person’s limits of stability is a strategy often used to decrease fear of falling. One works on reaching in all directions in various standing positions in order to improve the person’s ability to control their center of mass in various positions. One also can have the patient hold objects and have them stand on different support surfaces in a safe and protected environment. As people learn to move more effectively, generally, their fear of falling appears to decrease. There does not appear yet to be a direct relationship between decreasing people’s fear of falling and falls themselves.
Providing all patients at risk for falling with strategies to minimize their risk of falling is advised including having adequate lighting in their homes, decreasing clutter, and rearranging items so that they do not have to excessively reach for commonly used objects that could challenge their balance [84].
Impaired ability to stand without excess sway
An inability to stand without excessive sway is seen more in persons with central or psychiatric disorders than persons with peripheral vestibular disorders. Mal de Debarquement, persons with anxiety disorders, or cerebellar stroke are some examples of conditions where the person will most likely have the feeling of increased sway in standing. Mal de Debarquement is a condition where people feel that they are continuing to move after travel on a boat, car, train, or an airplane and their symptoms persist. Customized optokinetic stimuli as a rehabilitative tool hold promise for persons living with Mal de Debarquement [85]. It is unclear what the mechanism is for recovery for persons with Mal de Debarquement with the use of the optokinetic stimuli that matches their perceived movement frequency.
Subthreshold mechanical noise (vibration) has also been shown to decrease postural sway and improve gait in a laboratory setting in older adults, those with stroke, and persons with somatosensory deficits [86–88]. Sensory aides, if they can be produced for the masses, may have utility for persons with vestibular disorders who have impaired postural control.
There is preliminary evidence that persons with anxiety disorders can decrease postural sway with exercise [89, 90]. The use of maximizing distal somatosensory inputs in order to “ground” the person appears to aid in recovery of persons with anxiety-related dizziness. It appeared that many of the subjects utilized visual inputs rather than the combination of visual, vestibular, and proprioceptive cues for postural control.
Excessive sway in standing can also be seen in persons with anxiety or malingering. The difference between the two can be difficult to determine. Excessive, rhythmic sway has been associated on posturography with malingering [91] but also can be seen with persons with anxiety disorders [92]. Larrosa et al. recently reported that a high percentage of persons with work-related dizziness and imbalance had abnormal posturography and videonystagmography test findings [93]. Care must be exercised in using abnormal posturography as the gold standard to determine if malingering is present [93].
Getting the patient to understand what is “normal” versus “excessive” sway is the first step to functional recovery. The physical therapy exercise program attempts to get the patient to recalibrate what normal sway is over time through visual, verbal, and tactile feedback. Simple games like the Wii balance system may also help people to understand that their sway is excessive and also make the retraining fun.
Visual blurring with head movements/visual compensation for vestibular insults
In persons with both peripheral and central vestibular disorders, head movements can often increase dizziness. Persons with central pathology may be dizzy constantly, but constant dizziness is rare in persons with peripheral pathology at rest unless they are in the acute phase. The VOR gain is often reduced in persons with peripheral vestibular hypofunction such as a neuritis or labyrinthitis. When they move their head quickly, the visual scene blurs. As a strategy to minimize visual blurring, a patient may choose to not move their head. Only thru active head movement does the VOR gain increase. Patients are typically provided with exercises to increase the VOR gain by focusing on a target and actively moving their head in either the pitch, yaw, or roll planes with the target in focus in various stances and also during gait.
Central plasticity has been seen in persons with bilateral loss. The visual cortex was more active in persons with bilateral loss when assessed via functional MRI (fMRI) compared to control subjects during optokintic stimulation, suggesting that sensory reweighting had occurred [94]. With the use of fMRI, it was determined that vision was substituting for vestibular loss in persons with bilateral dysfunction. During rehabilitation, physical therapists attempt to reweigh sensory inputs and teach people to use vision to compensate for vestibular loss.
There are times when sensory reweighting or using another visual pathway to decrease the visual blurring may be the optimal recovery strategy. Training the saccadic system to assist with compensation of the VOR [95, 96] suggests that those persons who learn quickly to use a saccade (i.e., a covert saccade) during active head movement compensate faster. With an overt saccade, the saccade occurs after head movement and is seen as a catch-up saccade at the bedside (i.e., +head impulse test [HIT]) whereas with a covert saccade, the eye movement occurs during head movement—these short latency compensatory saccades can mask vestibular loss and make the HIT appear normal.
In a case report of a person with unilateral vestibular hypofunction, as VOR gain increased, the saccadic number and magnitude of the saccades decreased [97]. In healthy subjects, one can unilaterally train the VOR without an increase toward the non-adapting side [98]. If it is possible to successfully only retrain the VOR on the involved side in persons with vestibular disorders, visual blurring may be reduced faster facilitating recovery after a vestibular event. In addition, this device could prevent a VOR gain on the normal side which might result in faster compensation. An ongoing clinical trial will help to answer the question of the value of training only the involved side during active head movement.
Presently, rehabilitation for visual blurring includes head movements in various positions and at different speeds within their tolerance in an attempt to increase the VOR gain. Generally, persons should be back at their baseline symptoms approximately 20–30 min after the termination of the exercise session.
Symptoms with complex visual scenes in the periphery
A select group of patients with vestibular disorders complain of an increase in dizziness and disorientation with exposure to complex visual scenes such as grocery stores, stripes on the walls, and even lighting filtering in through blinds. The newly coined term for this “symptom complex” is persistent postural perceptual dizziness [99]. Other terms previously used in the literature include visual vertigo [100], space and motion symptoms [101], height vertigo [102], and chronic subjective dizziness [92]. Persons with migraines can present with similar symptoms when exposed to visually complex scenes. Rehabilitation has been shown to be effective in persons with migraine dizziness [39•].
Bittar and Lins suggested that 68 % of their subjects with persistent postural perceptual dizziness improved with serotonin reuptake inhibitors [99]. Pavlou et al. have recently suggested that persons with reduced stereopsis or double vision with near fixation may predispose them after a vestibular event to develop problems with complex visual scenes [103••]. Relying primarily on vision after a vestibular disorder continues to be a negative predictor of successful rehabilitation [100, 104]. Winkler and Ciuffreda [105] reported that Dizziness Handicap Inventory (DHI) scores were an average of 52 in persons with vestibular disorders and motion sensitivity versus 25 in persons with only vestibular dysfunction (higher DHI scores are worse).
Training with varying visual backgrounds appears to be effective as a rehabilitative tool. Various forms of virtual reality have been used for treatment intervention, yet the evidence is not clear as to virtual reality being “better” than traditional rehabilitation [23, 33, 54]. Use of virtual reality training, such as the use of the Wii balance platform, may add value as the exercises are fun and the system provides feedback about the person’s performance (knowledge of results) [23]. It appears that people without disease can perform virtual exercises in the home with the use of a virtual platform, suggesting that this may be a viable option in the future for vestibular rehabilitation [106]. In addition, the use of optokinetic exercises with the use of a DVD for home use has also been shown to be effective in persons with uncompensated vestibular loss [28].
Other simple treatment ideas include gradual exposure to a disco ball (more room light to less room light), and no head movement progressing to head movement with the disco ball moving have been attempted and appear to have value [28]. Increasing the difficulty of the visual scene must be done slowly over sessions. Persons with head trauma including concussion, binocular vision deficits, those with migraines, and some patients with uncompensated peripheral vestibular disorders appear to benefit from habituation exercises. Patients with motion sensitivity can be some of the most difficult to treat. Exercise may need to be combined with medication to decrease their sensitivity to the exposure to motion in the periphery.
Weakness
In older adults, sarcopenia is common and many persons with vestibular disorders are older. There is a 30 % decline in muscle mass between 20 and 80 years of age [107]. Reduction in muscle mass is the most important contributing factor to decline in muscle strength [108]. Younger people with vestibular disorders do not complain of muscle weakness, but muscle strength can affect postural control in older adults [109]. Strengthening is a component of all upright and gait exercises with an emphasis on the distal musculature. Increasing lower extremity strength and decreasing pain, especially in the ankle and the foot, will allow for enhanced postural control in older adults [110, 111]. As a good percentage of persons with balance and vestibular disorders are older, this strategy is often utilized in physical therapy in order to decrease risk of falling and to optimize function.
Overall benefits of vestibular rehabilitation
In the last 10 years, studies have been conducted to highlight the value of the vestibular rehabilitation using various outcome measures in persons with vestibular disorders [3–38, 39•, 40, 54]. Most of the studies report positive effects of vestibular rehabilitation on dizziness, vertigo, postural instability, gait, risk of fall, ADLs, and quality of life in persons with peripheral, central, or mixed vestibular disorders.
Vestibular rehabilitation programs often are multidisciplinary as patients may have special needs. Members of the team can include physical therapists, audiologists, a neuro-otologist, neurologist, psychologist, or a psychiatrist.
Exercise prescription
Exercise prescription for persons with balance and vestibular disorders is complex. The exercise prescription depends on the deficits that the patient exhibits, rather than the presenting diagnosis. Klatt et al. [46] recently suggested that exercises be divided into six different categories including firm static standing, standing on a foam pad, gait, modified center of gravity exercises, VOR adaptation exercises, and weight shifting. In addition, the environment, dual tasking, eyes open versus closed, speed, and other factors will affect exercise performance. There were over 800 different exercises proposed based on the above parameters. Patient response to the exercise dictates the exercise progression. Generally, patients are told to perform their exercises two to three times per day, especially the VOR exercises.
The otolith organs and rehabilitation
The semicircular canals provide inputs related to angular acceleration, and the otolith organs (utricle and saccule) provide information about linear acceleration. Few rehab studies exist that have utilized only persons with either utricular and/or saccular damage [26, 112]. With vestibular disorders, vertigo is a common complaint versus with otolith disorders; a head tilt is often noted. Auditory feedback improved postural control in persons with otolithic only disease [60]. Control subjects performed the same exercises without the auditory feedback and showed no improvement in balance [60]. In contrast, Murray et al. [26] compared persons with canal versus canal and otolithic dysfunction and reported no differences in balance and reports of dizziness between the two groups after vestibular rehab.
Since the otolith organ detects motion relative to changes in gravity, interventions have including components such as bouncing and jumping, yet they have not appeared to be any more effective than traditional vestibular rehabilitation exercises. It is unclear how a person’s rehabilitation program should be managed differently if they have otolithic disease with or without semicircular disease damage. Presently, people with otolithic disease are treated based on their functional deficits. Diagnostic tests such as the ocular vestibular evoked myogenic potential (oVEMP), which is a test of the utricle and the cervical VEMP (a test of the saccule), plus subjective visual vertical (a test of the utricle) assist with identifying the underlying pathology in the otolith organs.
Innovations related to vestibular rehabilitation
A surgically implanted vestibular prosthetic device is being developed and may have a profound effect on vestibular rehabilitation for persons with bilateral vestibular loss and those possibly with uncompensated, chronic vestibulopathy [113–115]. The vestibular prosthesis is designed to provide a signal to the CNS that can be interpreted as an angular acceleration input in place of the defective semicircular canal(s). Like the cochlear implant, persons will most likely need to “learn” how to utilize the new signal from the implant. At least five centers around the world are working on optimizing their design and functionality of the vestibular implant. Rehab protocols will need to be developed so that persons can quickly and efficiently learn how to retrain the brain to utilize the new inputs. The vestibular prosthesis has moved beyond the laboratory into human experiments with promising findings, although there have been reports of hearing loss with the surgical procedure [115]. Similar to cochlear implant programs, retraining the brain will be critical in optimizing success of this developing technology. With cochlear implant programs, adequate “retraining” is essential and it may be similar for the vestibular implant that retraining the brain how to effectively utilize the new signals will be required for the end user to effectively use the vestibular prosthesis.
Phone and computer apps can provide reports of eye/head exercise compliance. Successful programs already exist in the laboratory and will be utilized clinically in the near future [116, 117]. Velocity of head movement, duration of the exercises, time of day that the exercises were performed, neck range of motion, the frequency of head turning plus self-reported dizziness ratings can all be downloaded and reported to the clinician with ease [117].
Tablet and smartphone technology is being used to videotape patients performing their exercises so that they can remember what they have been instructed to do on their own devices. They can also use their technology (smartphone) to recheck the exercise prescription to ensure that they are doing the exercises correctly. Other physical therapists are using exercise programs with computer-simulated models mimicking the exercises that they have been prescribed in the hopes of promoting optimal exercise compliance and accuracy of performance of the exercise prescription.
Patients with dizziness and balance disorders must move in order to improve their function. Physical therapists often combine cognitive behavioral therapy into their interventions, which may make physical therapy with the patient more effective than handing the person a sheet of exercises to perform. The human interaction for persons with uncompensated vestibular disorders appears to have added value.
Conclusion
Vestibular rehabilitation enhances recovery after vestibular dysfunction. There is increasing evidence that the central nervous system has the capability to compensate for vestibular dysfunction and reweight sensory inputs. Early referral for vestibular rehabilitation results in enhanced quality of life, decreases in reports of dizziness, improved postural control, plus less anxiety about their dizziness and balance deficits.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cawthorne T. The physiological basis for head exercises. J Chart Soc Physiother. 1944;3:106–7.
Cooksey FS. Rehabilitation in vestibular injuries. Proc R Soc Med. 1946;39.
Badaracco C, Labini FS, Meli A, De Angelis E, Tufarelli D. Vestibular rehabilitation outcomes in chronic vertiginous patients through computerized dynamic visual acuity and gaze stabilization test. Otol Neurotol. 2007;28(6):809–13.
Badke MB, Miedaner JA, Shea TA, Grove CR, Pyle GM. Effects of vestibular and balance rehabilitation on sensory organization and dizziness handicap. Ann Oto Rhinol Laryn. 2005;114(1):48–54.
Bjerlemo B, Kollen L, Boderos I, Kreuter M, Moller C. Recovery after early vestibular rehabilitation in patients with acute unilateral vestibular loss. Audiol Med. 2006;4:117–23.
Cakrt O, Chovanec M, Funda T, Kalitova P, Betka J, Zverina E, et al. Exercise with visual feedback improves postural stability after vestibular schwannoma surgery. Eur Arch Oto-Rhino-L. 2010;267(9):1355–60.
Chen PY, Hsieh WL, Wei SH, Kao CL. Interactive wiimote gaze stabilization exercise training system for patients with vestibular hypofunction. J Neuroeng Rehabil. 2012;9:77.
Clendaniel RA. The effects of habituation and gaze stability exercises in the treatment of unilateral vestibular hypofunction: a preliminary results. J Neurol Phys Ther. 2010;34(2):111–6.
Donmez B, Akdal G. Vestibular rehabilitation in unilateral peripheral vestibulopathy: a preliminary report. J Neurol Sci Turk. 2008;25(2):128–35.
Enticott JC, O'Leary SJ, Briggs RJS. Effects of vestibulo-ocular reflex exercises on vestibular compensation after vestibular schwannoma surgery. Otol Neurotol. 2005;26(2):265–9.
Enticott JC, Vitkovic JJ, Reid B, O'Neill P, Paine M. Vestibular rehabilitation in individuals with inner-ear dysfunction: a pilot study. Audiol Neuro Otol. 2008;13(1):19–28.
Gabilan YPL, Perracini MR, Munhoz MSL, Gananc FF. Aquatic physiotherapy for vestibular rehabilitation in patients with unilateral vestibular hypofunction: exploratory prospective study. J Vestibul Res Equil. 2008;18(2–3):139–46.
Giray M, Kirazli Y, Karapolat H, Celebisoy N, Bilgen C, Kirazli T. Short-term effects of vestibular rehabilitation in patients with chronic unilateral vestibular dysfunction: a randomized controlled study. Arch Phys Med Rehabil. 2009;90(8):1325–31.
Goudakos JK, Markou KD, Psillas G, Vital V, Tsaligopoulos M. Corticosteroids and vestibular exercises in vestibular neuritis single-blind randomized clinical trial. Jama Otolaryngol. 2014;140(5):434–40.
Kammerlind ASC, Ledin TRE, Odkvist LM, Skargren EIB. Effects of home training and additional physical therapy on recovery after acute unilateral vestibular loss—a randomized study. Clin Rehabil. 2005;19(1):54–62.
Kao CL, Chen LK, Chern CM, Hsu LC, Chen CC, Hwang SJ. Rehabilitation outcome in home-based versus supervised exercise programs for chronically dizzy patients. Arch Gerontol Geriatr. 2010;51(3):264–7.
Kao CL, Tsai KL, Cheng YY, Kuo CH, Lee SD, Chan RC. Vestibular rehabilitation ameliorates chronic dizziness through the axis. Front Aging Neurosci. 2014;6.
Kvale A, Wilhelmsen K, Fiske HA. Physical findings in patients with dizziness undergoing a group exercise programme. Physiother Res Int: J Res Clin Phys Ther. 2008;13(3):162–75.
Maciaszek J, Osinski W. Effect of Tai Chi on Body Balance: Randomized Controlled Trial in Elderly Men with Dizziness. Am J Chin Med. 2012;40(2):245–53.
Mantello EB, Moriguti JC, Rodrigues-Junior AL, Ferrioli E. Vestibular rehabilitation's effect over the quality of life of geriatric patients with labyrinth disease. Braz J Otorhinolaryngol. 2008;74(2):172–80.
Marioni G, Fermo S, Zanon D, Broi N, Staffieri A. Early rehabilitation for unilateral peripheral vestibular disorders: a prospective, randomized investigation using computerized posturography. Eur Arch Oto-Rhino-L. 2013;270(2):425–35.
McGibbon CA, Krebs DE, Parker SW, Scarborough DM, Wayne PM, Wolf SL. Tai Chi and vestibular rehabilitation improve vestibulopathic gait via different neuromuscular mechanisms: Preliminary report. Bmc Neurol. 2005;5.
Meldrum D, Herdman S, Vance R, Murray D, Malone K, Duffy D, et al. Effectiveness of conventional versus virtual reality-based balance exercises in vestibular rehabilitation for unilateral peripheral vestibular loss: results of a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(7):1319–28.
Mohammad MT, Whitney SL, Sparto PJ, Jennings JR, Furman JM. Perceptual and motor inhibition in individuals with vestibular disorders. J Neurol Phys Ther. 2010;34(2):76–81.
Morozetti PG, Gananca CF, Chiari BM. Comparison of different protocols for vestibular rehabilitation in patients with peripheral vestibular disorders. J Soc Bras Fonoaudiol. 2011;23(1):44–50.
Murray KJ, Hill K, Phillips B, Waterston J. Does otolith organ dysfunction influence outcomes after a customized program of vestibular rehabilitation? J Neurol Phys Ther. 2010;34(2):70–5.
Patatas OH, Gananca CF, Gananca FF. Quality of life of individuals submitted to vestibular rehabilitation. Braz J Otorhinolaryngol. 2009;75(3):387–94.
Pavlou M, Bronstein AM, Davies RA. Randomized trial of supervised versus unsupervised optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabil Neural Repair. 2013;27(3):208–18.
Rocha Junior PR, da Peres Silva A, Garbi FP, Frizzo AC, Valenti VE. Effects of physiotherapy on balance and unilateral vestibular hypofunction in vertiginous elderly. Int Arch Med. 2014;7(1):8.
Rossi-Izquierdo M, Santos-Perez S, Rubio-Rodriguez JP, Lirola-Delgado A, Zubizarreta-Gutierrez A, Roman-Rodriguez ES, et al. What is the optimal number of treatment sessions of vestibular rehabilitation? Eur Arch Oto-Rhino-L. 2014;271(2):275–80.
Rossi-Izquierdo M, Santos-Perez S, Soto-Varela A. What is the most effective vestibular rehabilitation technique in patients with unilateral peripheral vestibular disorders? Eur Arch Oto-Rhino-L. 2011;268(11):1569–74.
Smaerup M, Gronvall E, Larsen SB, Laessoe U, Henriksen JJ, Damsgaard EM. Computer-assisted training as a complement in rehabilitation of patients with chronic vestibular dizziness—a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(3):395–401.
Sparrer I, Thien ADD, Ilgner J, Westhofen M. Vestibular rehabilitation using the Nintendo (R) Wii Balance Board—a user-friendly alternative for central nervous compensation. Acta Oto-Laryngol. 2013;133(3):239–45.
Tee LH. Functional outcomes after customized vestibular rehabilitation in subjects with chronic vestibular dysfunction. Physiother Singapore. 2010;13(2):4–7.
Teggi R, Caldirola D, Fabiano B, Recanati P, Bussi M. Rehabilitation after acute vestibular disorders. J Laryngol Otol. 2009;123(4):397–402.
Venosa AR, Bittar RS. Vestibular rehabilitation exercises in acute vertigo. Laryngoscope. 2007;117(8):1482–7.
Verdecchia DH, Mendoza M, Sanguineti F, Binetti AC. Outcomes after vestibular rehabilitation and Wii(R) therapy in patients with chronic unilateral vestibular hypofunction. Acta Otorrinolaringol Esp. 2014;65(6):339–45.
Vereeck L, Wuyts FL, Truijen S, De Valck C, de Heyning PHV. The effect of early customized vestibular rehabilitation on balance after acoustic neuroma resection. Clin Rehabil. 2008;22(8):698–713.
Vitkovic J, Winoto A, Rance G, Dowell R, Paine M. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol. 2013;260(12):3039–48. People with and without migraine dizziness appear to improve after completion of a vestibular rehabiliation program.
Yeh SC, Chen S, Wang PC, Su MC, Chang CH, Tsai PY. Interactive 3-dimensional virtual reality rehabilitation for patients with chronic imbalance and vestibular dysfunction. Technol Health Care. 2014;22(6):915–21.
McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015;1, CD005397. The paper provides the most current review related to peripheral vestibular hypofunction inclusive of BPPV.
Porciuncula F, Johnson CC, Glickman LB. The effect of vestibular rehabilitation on adults with bilateral vestibular hypofunction: a systematic review. J Vestib Res: Equilib Orientation. 2012;22(5–6):283–98.
Nagaratnam N, Ip J, Bou-Haidar P. The vestibular dysfunction and anxiety disorder interface: a descriptive study with special reference to the elderly. Arch Gerontol Geriatr. 2005;40(3):253–64.
Shefer S, Gordon C, Avraham KB, Mintz M. Balance deficit enhances anxiety and balance training decreases anxiety in vestibular mutant mice. Behav Brain Res. 2015;276:76–83.
Simon NM, Pollack MH, Tuby KS, Stern TA. Dizziness and panic disorder: a review of the association between vestibular dysfunction and anxiety. Ann Clin Psychiatry: Off J Am Acad Clin Psychiatrists. 1998;10(2):75–80.
Klatt BN, Carender WJ, Lin CC, Alsubaie SF, Kinnaird CR, Sienko KH, et al. A conceptual framework for the progression of balance exercises in persons with balance and vestibular disorders. Phys Med Rehabil Int. 2015;2:4.
Hall CD, Herdman SD, Whitney SL, Cass SP, Clendaniel RA, Fife TD, et al. Vestibular rehabilitation for peripheral vestibular hypofunction: an evidence-based clinical practice guideline J Neurol Phys Ther. 2016;In press. The paper is the first clinical practice guidelilne generated related to peripehral vestibular hypofunction.
Curthoys IS. Vestibular compensation and substitution. Curr Opin Neurol. 2000;13(1):27–30.
Gauchard GC, Parietti-Winkler C, Lion A, Simon C, Perrin PP. Impact of pre-operative regular physical activity on balance control compensation after vestibular schwannoma surgery. Gait Posture. 2013;37(1):82–7.
Lacour M, Bernard-Demanze L. Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Front Neurol. 2014;5:285.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–8.
Arnold SA, Stewart AM, Moor HM, Karl RC, Reneker JC. The effectiveness of vestibular rehabilitation interventions in treating unilateral peripheral vestibular disorders: a systematic review. Physiotherapy research international : the journal for researchers and clinicians in physical therapy. 2015.
Ricci NA, Aratani MC, Caovilla HH, Gananca FF. Effects of Vestibular Rehabilitation on Balance Control in Older People with Chronic Dizziness: A Randomized Clinical Trial. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2015.
Alahmari KA, Sparto PJ, Marchetti GF, Redfern MS, Furman JM, Whitney SL. Comparison of virtual reality based therapy with customized vestibular physical therapy for the treatment of vestibular disorders. IEEE Trans Neural Syst Rehabil Eng: Publ IEEE Eng Med Biol Soc. 2014;22(2):389–99.
Saman Y, Bamiou DE, Murdin L, Tsioulos K, Davies R, Dutia MB, et al. Balance, falls risk, and related disability in untreated vestibular schwannoma patients. J Neurol Surg Part B, Skull Base. 2014;75(5):332–8.
Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with vestibular deficits. AmJOtol. 2000;21(6):847–51.
Brach JS, Francois SJ, VanSwearingen JM, Gilmore S, Perera S, Studenski SA. Translation of a motor learning walking rehabilitation program into a group-based exercise program for community-dwelling older adults. PM R. 2015.
Brach JS, Lowry K, Perera S, Hornyak V, Wert D, Studenski SA, et al. Improving motor control in walking: a randomized clinical trial in older adults with subclinical walking difficulty. Arch Phys Med Rehabil. 2015;96(3):388–94.
Brach JS, Van Swearingen JM, Perera S, Wert DM, Studenski S. Motor learning versus standard walking exercise in older adults with subclinical gait dysfunction: a randomized clinical trial. J Am Geriatr Soc. 2013;61(11):1879–86.
Basta D, Singbartl F, Todt I, Clarke A, Ernst A. Vestibular rehabilitation by auditory feedback in otolith disorders. Gait Posture. 2008;28(3):397–404.
Allum JH, Carpenter MG, Horslen BC, Davis JR, Honegger F, Tang KS, et al. Improving impaired balance function: real-time versus carry-over effects of prosthetic feedback. Conf Proc: Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf. 2011;2011:1314–8.
Horlings CG, Carpenter MG, Honegger F, Allum JH. Vestibular and proprioceptive contributions to human balance corrections: aiding these with prosthetic feedback. Ann N Y Acad Sci. 2009;1164:1–12.
Dozza M, Horak FB, Chiari L. Auditory biofeedback substitutes for loss of sensory information in maintaining stance. Exp Brain Res. 2007;178(1):37–48.
Sienko KH, Balkwill MD, Oddsson LI, Wall 3rd C. The effect of vibrotactile feedback on postural sway during locomotor activities. J Neuroeng Rehabil. 2013;10:93.
Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther. 2004;84(10):906–18.
Lee BC, Kim J, Chen S, Sienko KH. Cell phone based balance trainer. J Neuroeng Rehabil. 2012;9:10.
Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med. 2009;169(10):938–44.
Liao WL, Chang TP, Chen HJ, Kao CH. Benign paroxysmal positional vertigo is associated with an increased risk of fracture: a population-based cohort study. J Orthop Sports Phys Ther. 2015;45(5):406–12.
Avin KG, Hanke TA, Kirk-Sanchez N, McDonough CM, Shubert TE, Hardage J, et al. Management of falls in community-dwelling older adults: clinical guidance statement from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association. Phys Ther. 2015;95(6):815–34.
Moreland J, Richardson J, Chan D, O'Neill J, Bellissimo A, Grum R, et al. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49(2):93–116.
Lowry KA, Vanswearingen JM, Perera S, Studenski SA, Brach JS. Walking smoothness is associated with self-reported function after accounting for gait speed. J Gerontol Ser A Biol Med Sci. 2013;68(10):1286–90.
Rosso AL, Olson Hunt MJ, Yang M, Brach JS, Harris TB, Newman AB, et al. Higher step length variability indicates lower gray matter integrity of selected regions in older adults. Gait Posture. 2014;40(1):225–30.
Whitney SL, Marchetti GF, Schade A, Wrisley DM. The sensitivity and specificity of the Timed "Up & Go" and the Dynamic Gait Index for self-reported falls in persons with vestibular disorders. J Vestib Res: Equilib Orientation. 2004;14(5):397–409.
Alsalaheen BA, Whitney SL, Marchetti GF, Furman JM, Kontos AP, Collins MW, et al. Performance of high school adolescents on functional gait and balance measures. Pediatric Phys Ther: Off Publ Section Pediatr Am Phys Ther Assoc. 2014;26(2):191–9.
Ekvall Hansson E, Dahlberg LE, Magnusson M. Vestibular rehabilitation affects vestibular asymmetry among patients with fall-related wrist fractures—a randomized controlled trial. Gerontology. 2015;61(4):310–8.
Ekvall Hansson E, Magnusson M. Vestibular asymmetry predicts falls among elderly patients with multi-sensory dizziness. BMC Geriatr. 2013;13:77.
Hall CD, Schubert MC, Herdman SJ. Prediction of fall risk reduction as measured by dynamic gait index in individuals with unilateral vestibular hypofunction. Otol Neurotol. 2004;25(5):746–51.
Gananca FF, Gazzola JM, Gananca CF, Caovilla HH, Gananca MM, Cruz OL. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2010;76(1):113–20.
Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34.
Morgan MT, Friscia LA, Whitney SL, Furman JM, Sparto PJ. Reliability and validity of the Falls Efficacy Scale-International (FES-I) in individuals with dizziness and imbalance. Otol Neurotol. 2013;34(6):1104–8.
Bigelow RT, Semenov YR, du Lac S, Hoffman HJ, Agrawal Y. Vestibular vertigo and comorbid cognitive and psychiatric impairment: the 2008 National Health Interview Survey. Journal of neurology, neurosurgery, and psychiatry. 2015.
Yuan Q, Yu L, Shi D, Ke X, Zhang H. Anxiety and depression among patients with different types of vestibular peripheral vertigo. Medicine. 2015;94(5), e453.
Kanzaki J, Goto F. Psychiatric disorders in patients with dizziness and Meniere's disease. Acta Otolaryngol. 2015;135(5):447–50.
Hill AM, Etherton-Beer C, Haines TP. Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge—a pilot randomized controlled trial. PLoS ONE. 2013;8(5), e63450.
Dai M, Cohen B, Smouha E, Cho C. Readaptation of the vestibulo-ocular reflex relieves the mal de debarquement syndrome. Front Neurol. 2014;5:124.
Liu W, Lipsitz LA, Montero-Odasso M, Bean J, Kerrigan DC, Collins JJ. Noise-enhanced vibrotactile sensitivity in older adults, patients with stroke, and patients with diabetic neuropathy. Arch Phys Med Rehabil. 2002;83(2):171–6.
Priplata AA, Niemi JB, Harry JD, Lipsitz LA, Collins JJ. Vibrating insoles and balance control in elderly people. Lancet. 2003;362(9390):1123–4.
Priplata AA, Patritti BL, Niemi JB, Hughes R, Gravelle DC, Lipsitz LA, et al. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann Neurol. 2006;59(1):4–12.
Jacob RG, Whitney SL, Detweiler-Shostak G, Furman JM. Vestibular rehabilitation for patients with agoraphobia and vestibular dysfunction: a pilot study. J Anxiety Disord. 2001;15(1–2):131–46.
Whitney SL, Jacob RG, Sparto PJ, Olshansky EF, Detweiler-Shostak G, Brown EL, et al. Acrophobia and pathological height vertigo: indications for vestibular physical therapy? Phys Ther. 2005;85(5):443–58.
Mallinson AI, Longridge NS. A new set of criteria for evaluating malingering in work-related vestibular injury. Otol Neurotol. 2005;26(4):686–90.
Staab JP. Chronic dizziness: the interface between psychiatry and neuro-otology. Curr Opin Neurol. 2006;19(1):41–8.
Larrosa F, Dura MJ, Menacho J, Gonzalez-Sabate L, Cordon A, Hernandez A, et al. Aphysiologic performance on dynamic posturography in work-related patients. Eur Arch Oto-Rhino-Laryngol: Off J Eur Fed Oto-Rhino-Laryngol Soc. 2013;270(1):93–7.
Dieterich M, Bauermann T, Best C, Stoeter P, Schlindwein P. Evidence for cortical visual substitution of chronic bilateral vestibular failure (an fMRI study). Brain : J Neurol. 2007;130(Pt 8):2108–16.
Mantokoudis G, Schubert MC, Tehrani AS, Wong AL, Agrawal Y. Early adaptation and compensation of clinical vestibular responses after unilateral vestibular deafferentation surgery. Otol Neurotol. 2014;35(1):148–54.
Schubert MC, Zee DS. Saccade and vestibular ocular motor adaptation. Restor Neurol Neurosci. 2010;28(1):9–18.
Schubert MC, Migliaccio AA, Della Santina CC. Modification of compensatory saccades after aVOR gain recovery. J Vestib Res: Equilib Orientation. 2006;16(6):285–91.
Migliaccio AA, Schubert MC. Pilot study of a new rehabilitation tool: improved unilateral short-term adaptation of the human angular vestibulo-ocular reflex. Otol Neurotol. 2014;35(10):e310–6.
Bittar RS, Lins EM. Clinical characteristics of patients with persistent postural-perceptual dizziness. Braz J Otorhinolaryngol. 2015;81(3):276–82.
Bronstein A. Visual symptoms and vertigo. Neurol Clin. 2005;23(3):705–13. v-vi.
Jacob R, Woody SR, Clark DB, Lilienfeld SO, Hirsch BE, Kucera GD, et al. Discomfort with space and motion: a possible marker of vestibular dysfunction assessed by the Situational Characteristics Questionnaire. J Psychopathol Behav Assess. 1993;15(4):299–324.
Brandt T, Bles W, Arnold F, Kapteyn TS. Height vertigo and human posture. Adv Otorhinolaryngol. 1979;25:88–92.
Pavlou M, Acheson J, Nicolaou D, Fraser CL, Bronstein AM, Davies RA. Effect of developmental binocular vision abnormalities on visual vertigo symptoms and treatment outcome. J Neurol Phys Ther. 2015;39(4):215–24. The results of the paper provide support for the concept that persons with binoculare visual abnormalities take longer to get better after a vestiublar injury.
Bronstein AM, Golding JF, Gresty MA. Vertigo and dizziness from environmental motion: visual vertigo, motion sickness, and drivers' disorientation. Semin Neurol. 2013;33(3):219–30.
Winkler PA, Ciuffreda KJ. Ocular fixation, vestibular dysfunction, and visual motion hypersensitivity. Optometry. 2009;80(9):502–12.
Gonzalez-Franco M, Gilroy S, Moore JO. Empowering patients to perform physical therapy at home. Conf Proc: Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf. 2014;2014:6308–11.
Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R. Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol (1985). 2000;88(4):1321–6.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Ng TP, Feng L, Nyunt MS, Feng L, Niti M, Tan BY, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med. 2015;128(11):1225–36. e1.
Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. ISB Clinical Biomechanics Award 2009: toe weakness and deformity increase the risk of falls in older people. Clin Biomech (Bristol, Avon). 2009;24(10):787–91.
Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. Cross-sectional analysis of foot function, functional ability, and health-related quality of life in older people with disabling foot pain. Arthritis Care Res (Hoboken). 2011;63(11):1592–8.
Murray KJ, Hill KD, Phillips B, Waterston J. The influence of otolith dysfunction on the clinical presentation of people with a peripheral vestibular disorder. Phys Ther. 2007;87(2):143–52.
Lewis RF. Vestibular prostheses investigated in animal models. ORL; J Oto-Rhino-Laryngol Relat Spec. 2015;77(4):219–26.
Phillips C, Ling L, Oxford T, Nowack A, Nie K, Rubinstein JT, et al. Longitudinal performance of an implantable vestibular prosthesis. Hear Res. 2015;322:200–11.
Phillips JO, Ling L, Nie K, Jameyson E, Phillips CM, Nowack AL, et al. Vestibular implantation and longitudinal electrical stimulation of the semicircular canal afferents in human subjects. J Neurophysiol. 2015;113(10):3866–92.
Bhatti PT, Herdman SJ, Roy SD, Hall CD, Tusa RJ. A prototype head-motion monitoring system for in-home vestibular rehabilitation therapy. Journal of bioengineering & biomedical science. 2011;Suppl 1.
Huang K, Sparto PJ, Kiesler S, Siewiorek DP, Smailagic A. iPod-based in-home system for monitoring gaze-stabilization exercise compliance of individuals with vestibular hypofunction. J Neuroeng Rehabil. 2014;11:69.
Acknowledgments
The project was financially supported by King Saud University, through the Vice Deanship of Research Chairs, Rehabilitation Research Chair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Susan L. Whitney, Ahmad H. Alghadir, and Shahnawaz Anwer declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurologic Ophthalmology and Otology
Rights and permissions
About this article
Cite this article
Whitney, S.L., Alghadir, A.H. & Anwer, S. Recent Evidence About the Effectiveness of Vestibular Rehabilitation. Curr Treat Options Neurol 18, 13 (2016). https://doi.org/10.1007/s11940-016-0395-4
Published:
DOI: https://doi.org/10.1007/s11940-016-0395-4