Abstract
Diagnosis of superficial colorectal neoplasms [1] increases as a result of the effort and adoption of screening and surveillance programs. Most of superficial neoplasms of the gastrointestinal tract with limited risk of lymph node (LN) metastasis are locally excised by endoscopic resection (ER), with 5-year survival rates similar to those of surgery, lower mortality and morbidity, and greater cost-effective ratio [2–4]. Multicenter studies show that mortality of surgery is 1% and 2% for low anterior resection and right hemicolectomy, respectively [5, 6], and these data are confirmed by a National Surgical Quality Improvement Program [4]. However, major postoperative adverse events rate occur in 15% of the cases with 8% readmissions, 4% redo surgeries, and 2% colostomies or ileostomies. Conversely, ER of large neoplasms has a much lower (0.1%) mortality rate both in a review of 6440 patients [7] and a prospective study of 1050 advanced lesions. Moreover, ER has a very low morbidity rate [8], and age is not an independent risk fact [9, 10], although severe comorbidities should be cautiously considered [11]. ER and surgery in the treatment algorithm of colorectal neoplasms are complementary according to the risk of LN metastasis, difficulty gradients of resection, and quality of life.
Similar content being viewed by others
References
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58:S3–43
Keswani RN, Law R, Ciolino JD et al (2016) Adverse events after surgery for nonmalignant colon polyps are common and associated with increased length of stay and costs. Gastrointest Endosc 84:296–303. e1
Yu JX, Russell WA, Ching JH et al (2019) Cost effectiveness of endoscopic resection vs transanal resection of complex benign rectal polyps. Clin Gastroenterol Hepatol 17:2740–2748. e6
Peery AF, Shaheen NJ, Cools KS et al (2018) Morbidity and mortality after surgery for nonmalignant colorectal polyps. Gastrointest Endosc 87:243–250. e2
Kobayashi H, Miyata H, Gotoh M et al (2014) Risk model for right hemicolectomy based on 19,070 Japanese patients in the national clinical database. J Gastroenterol 49:1047–1055
Matsubara N, Miyata H, Gotoh M et al (2014) Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large-scale clinical database. Dis Colon Rectum 57:1075–1081
Hassan C, Repici A, Sharma P et al (2016) Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut 65:806–820
Ahlenstiel G, Hourigan LF, Brown G et al (2014) Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc 80:668–676
Uraoka T, Higashi R, Kato J et al (2011) Colorectal endoscopic submucosal dissection for elderly patients at least 80 years of age. Surg Endosc 25:3000–3007
Tamai N, Saito Y, Sakamoto T, Nakajima T, Matsuda T, Tajiri H (2012) Safety and efficacy of colorectal endoscopic submucosal dissection in elders: clinical and follow-up outcomes. Int J Color Dis 27:1493–1499
Abdelmessih R, Packey CD, Lawlor G (2016) Endoscopy in the elderly: a cautionary approach, when to stop. Curr Treat Options Gastroenterol 14:305–314
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Schlemper RJ, Riddell RH, Kato Y et al (2000) The Vienna classification of gastrointestinal epithelial neoplasia. Gut 47:251–255
Weiser MR (2018) AJCC 8th edition: colorectal cancer. Ann Surg Oncol 25:1454–1455
Ueno H, Mochizuki H, Hashiguchi Y et al (2004) Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology 127:385–394
Ferlitsch M, Moss A, Hassan C et al (2017) Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 49:270–297
Kaltenbach T, Anderson JC, Burke CA et al (2020) Endoscopic removal of Colorectal lesions-recommendations by the US multi-society task force on Colorectal Cancer. Gastrointest Endosc 91:486–519
Tanaka S, Kashida H, Saito Y et al (2020) Japan Gastroenterological Endoscopy Society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 32:219–239
Bosch SL, Teerenstra S, de Wilt JH, Cunningham C, Nagtegaal ID (2013) Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 45:827–834
Brown IS, Bettington ML, Bettington A, Miller G, Rosty C (2016) Adverse histological features in malignant colorectal polyps: a contemporary series of 239 cases. J Clin Pathol 69:292–299
Hassan C, Zullo A, Risio M, Rossini FP, Morini S (2005) Histologic risk factors and clinical outcome in colorectal malignant polyp: a pooled-data analysis. Dis Colon Rectum 48:1588–1596
Kimura T, Yamamoto E, Yamano HO et al (2012) A novel pit pattern identifies the precursor of colorectal cancer derived from sessile serrated adenoma. Am J Gastroenterol 107:460–469
Emmanuel A, Lapa C, Ghosh A et al (2019) Risk factors for early and late adenoma recurrence after advanced colorectal endoscopic resection at an expert Western center. Gastrointest Endosc 90:127–136
Ishiguro A, Uno Y, Ishiguro Y, Munakata A, Morita T (1999) Correlation of lifting versus non-lifting and microscopic depth of invasion in early colorectal cancer. Gastrointest Endosc 50:329–333
Uno Y, Munakata A (1994) The non-lifting sign of invasive colon cancer. Gastrointest Endosc 40:485–489
Kobayashi N, Saito Y, Sano Y et al (2007) Determining the treatment strategy for colorectal neoplastic lesions: endoscopic assessment or the non-lifting sign for diagnosing invasion depth? Endoscopy 39:701–705
Uraoka T, Saito Y, Matsuda T et al (2006) Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut 55:1592–1597
Moss A, Bourke MJ, Williams SJ et al (2011) Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 140:1909–1918
Kudo S (1993) Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy 25:455–461
Yamada M, Saito Y, Sakamoto T et al (2016) Endoscopic predictors of deep submucosal invasion in colorectal laterally spreading tumors. Endoscopy 48:456–464
Burgess NG, Hourigan LF, Zanati SA et al (2017) Risk stratification for covert invasive cancer among patients referred for colonic endoscopic mucosal resection: a large multicenter cohort. Gastroenterology 153:732–742. e1
Tanaka S, Kaltenbach T, Chayama K, Soetikno R (2006) High-magnification colonoscopy (with videos). Gastrointest Endosc 64:604–613
Ikematsu H, Saito Y, Yamano H (2011) Comparative evaluation of endoscopic factors from conventional colonoscopy and narrow-band imaging of colorectal lesions. Dig Endosc 23(Suppl 1):95–100
Hewett DG, Kaltenbach T, Sano Y et al (2012) Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology 143:599–607. e1
Tanaka S, Sano Y (2011) Aim to unify the narrow band imaging (NBI) magnifying classification for colorectal tumors: current status in Japan from a summary of the consensus symposium in the 79th Annual Meeting of the Japan Gastroenterological Endoscopy Society. Dig Endosc 23(Suppl 1):131–139
Kudo S, Rubio CA, Teixeira CR, Kashida H, Kogure E (2001) Pit pattern in colorectal neoplasia: endoscopic magnifying view. Endoscopy 33:367–373
Sano Y, Tanaka S, Kudo SE et al (2016) Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI expert team. Dig Endosc 28:526–533
Matsuda T, Fujii T, Saito Y et al (2008) Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol 103:2700–2706
Bianco MA, Rotondano G, Marmo R et al (2006) Predictive value of magnification chromoendoscopy for diagnosing invasive neoplasia in nonpolypoid colorectal lesions and stratifying patients for endoscopic resection or surgery. Endoscopy 38:470–476
Sakamoto T, Saito Y, Nakajima T, Matsuda T (2011) Comparison of magnifying chromoendoscopy and narrow-band imaging in estimation of early colorectal cancer invasion depth: a pilot study. Dig Endosc 23:118–123
Fu KI, Kato S, Sano Y et al (2008) Staging of early colorectal cancers: magnifying colonoscopy versus endoscopic ultrasonography for estimation of depth of invasion. Dig Dis Sci 53:1886–1892
Sumimoto K, Tanaka S, Shigita K et al (2017) Clinical impact and characteristics of the narrow-band imaging magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI expert team. Gastrointest Endosc 85:816–821
Deyhle P, Jenny S, Fumagalli I (1973) Endoscopic polypectomy in the proximal colon. A diagnostic, therapeutic (and preventive?) intervention. Dtsch Med Wochenschr 98:219–220
Moss A, Williams SJ, Hourigan LF et al (2015) Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian colonic EMR (ACE) study. Gut 64:57–65
Ono H, Kondo H, Gotoda T et al (2001) Endoscopic mucosal resection for treatment of early gastric cancer. Gut 48:225–229
Gotoda T, Yanagisawa A, Sasako M et al (2000) Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer 3:219–225
Tanaka S, Oka S, Kaneko I et al (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Saito Y, Uraoka T, Yamaguchi Y et al (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Tanaka S, Tamegai Y, Tsuda S, Saito Y, Yahagi N, Yamano HO (2010) Multicenter questionnaire survey on the current situation of colorectal endoscopic submucosal dissection in Japan. Dig Endosc 22(Suppl 1):S2–S8
Saito Y, Fukuzawa M, Matsuda T et al (2010) Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24:343–352
Lee EJ, Lee JB, Lee SH, Youk EG (2012) Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg Endosc 26:2220–2230
Lee EJ, Lee JB, Lee SH et al (2013) Endoscopic submucosal dissection for colorectal tumors – 1,000 colorectal ESD cases: one specialized institute’s experiences. Surg Endosc 27:31–39
Niimi K, Fujishiro M, Kodashima S et al (2010) Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 42:723–729
Saito Y, Sakamoto T, Nakajima T, Matsuda T, Colorectal ESD (2014) Current indications and latest technical advances. Gastrointest Endosc Clin N Am 24:245–255
Jayanna M, Burgess NG, Singh R et al (2016) Cost Analysis of Endoscopic Mucosal Resection vs Surgery for Large Laterally Spreading Colorectal Lesions. Clin Gastroenterol Hepatol 14:271–278. e1–2
Heldwein W, Dollhopf M, Rosch T et al (2005) The Munich Polypectomy study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy 37:1116–1122
Nawata Y, Homma K, Suzuki Y (2014) Retrospective study of technical aspects and complications of endoscopic submucosal dissection for large superficial colorectal tumors. Dig Endosc 26:552–555
Tanaka S, Oka S, Chayama K (2008) Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol 43:641–651
Tanaka S, Kashida H, Saito Y et al (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27:417–434
Hotta K, Oyama T, Shinohara T et al (2010) Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc 22:302–306
Sakamoto T, Saito Y, Fukunaga S, Nakajima T, Matsuda T (2011) Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum 54:1307–1312
Bhatt A, Abe S, Kumaravel A, Vargo J, Saito Y (2015) Indications and techniques for endoscopic submucosal dissection. Am J Gastroenterol 110:784–791
Asayama N, Oka S, Tanaka S, Hayashi N, Arihiro K, Chayama K (2015) Endoscopic submucosal dissection as total excisional biopsy for clinical T1 colorectal carcinoma. Digestion 91:64–69
Fuccio L, Hassan C, Ponchon T et al (2017) Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc 86:74–86. e17
Iacopini F, Bella A, Costamagna G et al (2012) Stepwise training in rectal and colonic endoscopic submucosal dissection with differentiated learning curves. Gastrointest Endosc 76:1188–1196
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T et al (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 47:829–854
Shiga H, Endo K, Kuroha M et al (2014) Endoscopic submucosal dissection for colorectal neoplasia during the clinical learning curve. Surg Endosc 28:2120–2128
Probst A, Ebigbo A, Markl B et al (2017) Endoscopic submucosal dissection for early rectal neoplasia: experience from a European center. Endoscopy 49:222–232
Iacopini F, Saito Y, Bella A et al (2017) Colorectal endoscopic submucosal dissection: predictors and neoplasm-related gradients of difficulty. Endosc Int Open 5:E839–EE46
Heitman SJ, Bourke MJ (2017) Endoscopic submucosal dissection and EMR for large colorectal polyps: "the perfect is the enemy of good". Gastrointest Endosc 86:87–89
Bahin FF, Heitman SJ, Rasouli KN et al (2018) Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions: a cost-effectiveness analysis. Gut 67:1965–1973
Peery AF, Cools KS, Strassle PD et al (2018) Increasing rates of surgery for patients with nonmalignant colorectal polyps in the United States. Gastroenterology 154:1352–1360. e3
Benson AB 3rd, Venook AP, Cederquist L et al (2017) Colon cancer, version 1.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 15:370–398
Rahmi G, Tanaka S, Ohara Y et al (2015) Efficacy of endoscopic submucosal dissection for residual or recurrent superficial colorectal tumors after endoscopic mucosal resection. J Dig Dis 16:14–21
Oka S, Tanaka S, Saito Y et al (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707
Barendse R, Musters G, Fockens P et al (2014) Endoscopic mucosal resection of large rectal adenomas in the era of centralization: results of a multicenter collaboration. United European Gastroenterol J 2:497–504
Nakajima T, Saito Y, Tanaka S et al (2013) Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc 27:3262–3270
Khashab M, Eid E, Rusche M, Rex DK (2009) Incidence and predictors of "late" recurrences after endoscopic piecemeal resection of large sessile adenomas. Gastrointest Endosc 70:344–349
Knabe M, Pohl J, Gerges C, Ell C, Neuhaus H, Schumacher B (2014) Standardized long-term follow-up after endoscopic resection of large, nonpedunculated colorectal lesions: a prospective two-center study. Am J Gastroenterol 109:183–189
Tate DJ, Desomer L, Klein A et al (2017) Adenoma recurrence after piecemeal colonic EMR is predictable: the Sydney EMR recurrence tool. Gastrointest Endosc 85:647–656. e6
Swan MP, Bourke MJ, Alexander S, Moss A, Williams SJ (2009) Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc 70:1128–1136
Bahin FF, Pellise M, Williams SJ, Bourke MJ (2016) Extended endoscopic mucosal resection does not reduce recurrence compared with standard endoscopic mucosal resection of large laterally spreading colorectal lesions. Gastrointest Endosc 84:997–1006. e1
Desomer L, Tutticci N, Tate DJ, Williams SJ, McLeod D, Bourke MJ (2017) A standardized imaging protocol is accurate in detecting recurrence after EMR. Gastrointest Endosc 85:518–526
Veerappan SG, Ormonde D, Yusoff IF, Raftopoulos SC (2014) Hot avulsion: a modification of an existing technique for management of nonlifting areas of a polyp (with video). Gastrointest Endosc 80:884–888
Saito Y, Uraoka T, Matsuda T et al (2007) A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc 65:537–542
Kikuchi T, Fu KI, Saito Y et al (2010) Transcutaneous monitoring of partial pressure of carbon dioxide during endoscopic submucosal dissection of early colorectal neoplasia with carbon dioxide insufflation: a prospective study. Surg Endosc 24:2231–2235
Sanchez-Yague A, Kaltenbach T, Yamamoto H, Anglemyer A, Inoue H, Soetikno R (2012) The endoscopic cap that can (with videos). Gastrointest Endosc 76:169–178. e1–2
Toyonaga T, Man IM, Fujita T et al (2010) The performance of a novel ball-tipped flush knife for endoscopic submucosal dissection: a case-control study. Aliment Pharmacol Ther 32:908–915
Saito Y, Sylvia Wu SY, Ego M, Abe S (2019) Colorectal endoscopic submucosal dissection with use of a bipolar and insulated tip knife. VideoGIE 4:314–318
Yamamoto K, Michida T, Nishida T, Hayashi S, Naito M, Ito T (2015) Colorectal endoscopic submucosal dissection: recent technical advances for safe and successful procedures. World J Gastrointest Endosc 7:1114–1128
Honma K, Kobayashi M, Watanabe H et al (2010) Endoscopic submucosal dissection for colorectal neoplasia. Dig Endosc 22:307–311
Han SJ, Jung Y, Cho YS et al (2018) Clinical effectiveness of submucosal injection with indigo carmine mixed solution for Colon endoscopic mucosal resection. Dig Dis Sci 63:775–780
Yamamoto H, Yahagi N, Oyama T et al (2008) Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid "cushion" in endoscopic resection for gastric neoplasms: a prospective multicenter trial. Gastrointest Endosc 67:830–839
Yandrapu H, Desai M, Siddique S et al (2017) Normal saline solution versus other viscous solutions for submucosal injection during endoscopic mucosal resection: a systematic review and meta-analysis. Gastrointest Endosc 85:693–699
Fujishiro M, Yahagi N, Nakamura M et al (2006) Successful outcomes of a novel endoscopic treatment for GI tumors: endoscopic submucosal dissection with a mixture of high-molecular-weight hyaluronic acid, glycerin, and sugar. Gastrointest Endosc 63:243–249
Kishihara T, Chino A, Uragami N et al (2012) Usefulness of sodium hyaluronate solution in colorectal endoscopic mucosal resection. Dig Endosc 24:348–352
Takeuchi Y, Uedo N, Ishihara R et al (2010) Efficacy of an endo-knife with a water-jet function (Flushknife) for endoscopic submucosal dissection of superficial colorectal neoplasms. Am J Gastroenterol 105:314–322
Nagata K, Shimizu M (2012) Pathological evaluation of gastrointestinal endoscopic submucosal dissection materials based on Japanese guidelines. World J Gastrointest Endosc 4:489–499
Yamasaki Y, Takeuchi Y, Uedo N et al (2018) Efficacy of traction-assisted colorectal endoscopic submucosal dissection using a clip-and-thread technique: a prospective randomized study. Dig Endosc 30:467–476
Ide D, Saito S, Ohya TR et al (2019) Colorectal endoscopic submucosal dissection can be efficiently performed by a trainee with use of a simple traction device and expert supervision. Endosc Int Open 7:E824–EE32
Hayashi Y, Sunada K, Takahashi H et al (2014) Pocket-creation method of endoscopic submucosal dissection to achieve en bloc resection of giant colorectal subpedunculated neoplastic lesions. Endoscopy 46(Suppl 1 UCTN):E421–E422
Hayashi Y, Miura Y, Yamamoto H (2015) Pocket-creation method for the safe, reliable, and efficient endoscopic submucosal dissection of colorectal lateral spreading tumors. Dig Endosc 27:534–535
Sakamoto H, Hayashi Y, Miura Y et al (2017) Pocket-creation method facilitates endoscopic submucosal dissection of colorectal laterally spreading tumors, non-granular type. Endosc Int Open 5:E123–E1E9
Yamashina T, Nemoto D, Hayashi Y et al (2020) Prospective randomized trial comparing the pocket-creation method and conventional method of colorectal endoscopic submucosal dissection. Gastrointest Endosc 92:368–379
Yamamoto K, Hayashi S, Nakabori T, Shibuya M, Ichiba M, Inada M (2012) Endoscopic submucosal dissection using endoclips to assist in mucosal flap formation (novel technique: "clip flap method"). Endoscopy 44(Suppl 2 UCTN):E334–E335
Oyama T (2012) Counter traction makes endoscopic submucosal dissection easier. Clin Endosc 45:375–378
Ota R, Doyama H, Tsuji K, Yamada S (2015) Deep colonic endoscopic submucosal dissection using a modified clip and snare method incorporating a pre-looping technique. BMJ Case Rep 2015
Saito Y, Emura F, Matsuda T et al (2005) A new sinker-assisted endoscopic submucosal dissection for colorectal cancer. Gastrointest Endosc 62:297–301
Sakamoto N, Osada T, Shibuya T et al (2009) Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video). Gastrointest Endosc 69:1370–1374
Osada T, Sakamoto N, Shibuya T et al (2008) "Loops-attached rubber band" facilitation of endoscopic submucosal dissection of superficial colorectal neoplasm. Endoscopy 40(Suppl 2):E101–E102
Mori H, Kobara H, Nishiyama N, Fujihara S, Matsunaga T, Masaki T (2017) Novel effective and repeatedly available ring-thread counter traction for safer colorectal endoscopic submucosal dissection. Surg Endosc 31:3040–3047
Parra-Blanco A, Nicolas D, Arnau MR, Gimeno-Garcia AZ, Rodrigo L, Quintero E (2011) Gastric endoscopic submucosal dissection assisted by a new traction method: the clip-band technique. A feasibility study in a porcine model (with video). Gastrointest Endosc 74:1137–1141
Ritsuno H, Sakamoto N, Osada T et al (2014) Prospective clinical trial of traction device-assisted endoscopic submucosal dissection of large superficial colorectal tumors using the S-O clip. Surg Endosc 28:3143–3149
Jacques J, Charissoux A, Bordillon P et al (2019) High proficiency of colonic endoscopic submucosal dissection in Europe thanks to countertraction strategy using a double clip and rubber band. Endosc Int Open 7:E1166–E1E74
Saito Y, Sumiyama K, Chiu PW (2017) Robot assisted tumor resection devices. Expert Rev Med Devices 14:657–662
Kantsevoy SV, Bitner M, Piskun G (2016) New endoscopic platform for endoluminal en bloc tissue resection in the gastrointestinal tract (with videos). Surg Endosc 30:3145–3151
Sharma S, Momose K, Hara H et al (2019) Facilitating endoscopic submucosal dissection: double balloon endolumenal platform significantly improves dissection time compared with conventional technique (with video). Surg Endosc 33:315–321
Jacques J, Chaussade S, Ponchon T et al (2019) Endoscopic submucosal dissection or endoscopic mucosal resection for large colorectal laterally spreading lesions? Scientific and economic data are still lacking. Gut 68:577–578
Shah SL, Sharma S, Dawod Q et al (2018) Double-balloon platform-assisted rectal endoscopic submucosal dissection. Endoscopy 50:E252–E2E3
Chiu PW, Phee SJ, Bhandari P et al (2015) Enhancing proficiency in performing endoscopic submucosal dissection (ESD) by using a prototype robotic endoscope. Endosc Int Open 3:E439–E442
Wang Z, Phee SJ, Lomanto D et al (2012) Endoscopic submucosal dissection of gastric lesions by using a master and slave transluminal endoscopic robot: an animal survival study. Endoscopy 44:690–694
Turiani Hourneaux de Moura D, Aihara H, Jirapinyo P et al (2019) Robot-assisted endoscopic submucosal dissection versus conventional ESD for colorectal lesions: outcomes of a randomized pilot study in endoscopists without prior ESD experience (with video). Gastrointest Endosc 90:290–298
Okamoto Y, Nakadate R, Nakamura S et al (2019) Colorectal endoscopic submucosal dissection using novel articulating devices: a comparative study in a live porcine model. Surg Endosc 33:651–657
Nanda KS, Tutticci N, Burgess NG, Sonson R, Williams SJ, Bourke MJ (2015) Endoscopic mucosal resection of laterally spreading lesions involving the ileocecal valve: technique, risk factors for failure, and outcomes. Endoscopy 47:710–718
Ponugoti PL, Broadley HM, Garcia J, Rex DK (2019) Endoscopic management of large ileocecal valve lesions over an 18-year interval. Endosc Int Open 7:E1646–E1E51
Ishii N, Setoyama T, Matsuda M et al (2010) Superficial tumors involving terminal ileum treated by endoscopic submucosal dissection. Clin J Gastroenterol 3:226–229
Yoshizaki T, Toyonaga T, Tanaka S et al (2016) Feasibility and safety of endoscopic submucosal dissection for lesions involving the ileocecal valve. Endoscopy 48:639–645
Ishii N, Itoh T, Horiki N et al (2010) Endoscopic submucosal dissection with a combination of small-caliber-tip transparent hood and flex knife for large superficial colorectal neoplasias including ileocecal lesions. Surg Endosc 24:1941–1947
Gurram KC, Ly E, Zhang X et al (2020) A novel technique of endoscopic submucosal dissection for circumferential ileocecal valve adenomas with terminal ileum involvement: the "doughnut resection" (with videos). Surg Endosc 34:1417–1424
Takahashi K, Ito T, Sato T et al (2017) Endoscopic submucosal dissection for depressed-type early adenocarcinoma of the terminal ileum. Intern Med 56:1153–1156
Sasajima K, Chinzei R, Takahashi M, Koushima Y, Watanabe H (2015) Endoscopic submucosal dissection for an early ileal cancer. Gastrointest Endosc 81:1031–1032. discussion 2-3
Iacopini F, Saito Y, Gotoda T, Grossi C, Costamagna G (2016) Endoscopic submucosal dissection of a nonpolypoid superficial neoplasm of the terminal ileum. Endoscopy 48(Suppl 1 UCTN):E57–E58
Jacob H, Toyonaga T, Ohara Y et al (2016) Endoscopic submucosal dissection of cecal lesions in proximity to the appendiceal orifice. Endoscopy 48:829–836
Tashima T, Ohata K, Nonaka K et al (2017) Endoscopic submucosal dissection for laterally spreading tumors involving the appendiceal orifice. Surg Endosc 31:5444–5450
Boda K, Oka S, Tanaka S et al (2018) Short-term outcomes of endoscopic submucosal dissection for superficial cecal tumors: a comparison between extension and nonextension into the appendiceal orifice. Ther Adv Gastroenterol 11:1756284818772794
Oung B, Rivory J, Chabrun E et al (2020) ESD with double clips and rubber band traction of neoplastic lesions developed in the appendiceal orifice is effective and safe. Endosc Int Open 8:E388–EE95
Iacopini F, Gotoda T, Montagnese F, Andrei F, Saito Y (2017) Underwater endoscopic submucosal dissection of a nonpolypoid superficial tumor spreading into the appendix. VideoGIE 2:82–84
Takeda T, Murakami T, Sakamoto N et al (2013) Traction device to remove an adenoma in the appendiceal orifice by endoscopic submucosal dissection. Endoscopy 45(Suppl 2 UCTN):E239–E240
Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD (2016) Underwater EMR of adenomas of the appendiceal orifice (with video). Gastrointest Endosc 83:638–642
Holt BA, Bassan MS, Sexton A, Williams SJ, Bourke MJ (2014) Advanced mucosal neoplasia of the anorectal junction: endoscopic resection technique and outcomes (with videos). Gastrointest Endosc 79:119–126
Kiriyama S, Saito Y, Matsuda T et al (2011) Comparing endoscopic submucosal dissection with transanal resection for non-invasive rectal tumor: a retrospective study. J Gastroenterol Hepatol 26:1028–1033
Park SU, Min YW, Shin JU et al (2012) Endoscopic submucosal dissection or transanal endoscopic microsurgery for nonpolypoid rectal high grade dysplasia and submucosa-invading rectal cancer. Endoscopy 44:1031–1036
Nakadoi K, Tanaka S, Hayashi N et al (2012) Clinical outcomes of endoscopic submucosal dissection for rectal tumor close to the dentate line. Gastrointest Endosc 76:444–450
Imai K, Hotta K, Yamaguchi Y et al (2015) Safety and efficacy of endoscopic submucosal dissection of rectal tumors extending to the dentate line. Endoscopy 47:529–532
Tamaru Y, Oka S, Tanaka S et al (2016) Endoscopic submucosal dissection for anorectal tumor with hemorrhoids close to the dentate line: a multicenter study of Hiroshima GI endoscopy study group. Surg Endosc 30:4425–4431
Tanaka S, Toyonaga T, Morita Y et al (2016) Feasibility and safety of endoscopic submucosal dissection for lower rectal tumors with hemorrhoids. World J Gastroenterol 22:6268–6275
Matsumoto S, Mashima H (2017) The efficacy of endoscopic submucosal dissection for colorectal tumors extending to the dentate line. Int J Color Dis 32:831–837
Probst A, Ebigbo A, Markl B et al (2018) Endoscopic submucosal dissection for rectal neoplasia extending to the dentate line: European experience. Endosc Int Open 6:E1355–E1E62
Roland D, Rahmi G, Perez-Cuadrado-Robles E et al (2020) Endoscopic submucosal dissection in rectal tumors extending or not to the dentate line: a comparative analysis. Dig Liver Dis 52:296–300
Abe S, Sakamoto T, Takamaru H et al (2016) Stenosis rates after endoscopic submucosal dissection of large rectal tumors involving greater than three quarters of the luminal circumference. Surg Endosc 30:5459–5464
Matsumoto S, Uehara T, Mashima H (2019) Construction of a preoperative scoring system to predict the difficulty level of colorectal endoscopic submucosal dissection. PLoS One 14:e0219096
Matsumoto A, Tanaka S, Oba S et al (2010) Outcome of endoscopic submucosal dissection for colorectal tumors accompanied by fibrosis. Scand J Gastroenterol 45:1329–1337
Hurlstone DP, Shorthouse AJ, Brown SR, Tiffin N, Cross SS (2008) Salvage endoscopic submucosal dissection for residual or local recurrent intraepithelial neoplasia in the colorectum: a prospective analysis. Color Dis 10:891–897
Kuroki Y, Hoteya S, Mitani T et al (2010) Endoscopic submucosal dissection for residual/locally recurrent lesions after endoscopic therapy for colorectal tumors. J Gastroenterol Hepatol 25:1747–1753
Sakamoto T, Saito Y, Matsuda T, Fukunaga S, Nakajima T, Fujii T (2011) Treatment strategy for recurrent or residual colorectal tumors after endoscopic resection. Surg Endosc 25:255–260
Yoshida N, Naito Y, Yasuda R et al (2018) The efficacy of the pocket-creation method for cases with severe fibrosis in colorectal endoscopic submucosal dissection. Endosc Int Open 6:E975–EE83
Kobayashi R, Hirasawa K, Ikeda R et al (2017) The feasibility of colorectal endoscopic submucosal dissection for the treatment of residual or recurrent tumor localized in therapeutic scar tissue. Endosc Int Open 5:E1242–E1E50
Hurlstone DP, Sanders DS, Atkinson R et al (2007) Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut 56:838–846
Smith LA, Baraza W, Tiffin N, Cross SS, Hurlstone DP (2008) Endoscopic resection of adenoma-like mass in chronic ulcerative colitis using a combined endoscopic mucosal resection and cap assisted submucosal dissection technique. Inflamm Bowel Dis 14:1380–1386
Iacopini F, Saito Y, Yamada M et al (2015) Curative endoscopic submucosal dissection of large nonpolypoid superficial neoplasms in ulcerative colitis (with videos). Gastrointest Endosc 82:734–738
Suzuki N, Toyonaga T, East JE (2017) Endoscopic submucosal dissection of colitis-related dysplasia. Endoscopy 49:1237–1242
Kinoshita S, Uraoka T, Nishizawa T et al (2018) The role of colorectal endoscopic submucosal dissection in patients with ulcerative colitis. Gastrointest Endosc 87:1079–1084
Yang DH, Kim J, Song EM et al (2019) Outcomes of ulcerative colitis-associated dysplasia patients referred for potential endoscopic submucosal dissection. J Gastroenterol Hepatol 34:1581–1589
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Appendix
Appendix
Patients with cecal neoplasms involving the appendix have been considered candidates for laparoscopic surgery. Actually, neoplasms at the appendix should be classified as: Type 0, in proximity to but not in contact with the appendiceal orifice; Type 1, at the border but not entering into orifice; Type 2, entering into the orifice with visible margins on inspection of the appendiceal lumen; Type 3, entering the orifice deeply with no visible margins [133]. Type 0 neoplasms should be considered as cecal neoplasms. After case reports, Jacob et al. [133] retrospectively reported their ESD experience on a large cohort of patients (Table 6) with an en bloc resection rate of 83% for Type 2 lesions. Another retrospective center study found similar ESD outcomes [134].
Difficulties for ER at the appendix are: highly prevalent SM fibrosis; the very narrow appendiceal lumen that may preclude the visualization of neoplasm margins (a prerequisite to perform a complete resection); difficulty in maintaining an adequate luminal distension; potential development of a delayed appendicitis. Type 3 lesions should not undergo ER unless the patient had a previous appendectomy or the endoscopist believes there is a reasonable chance that a complete resection can be carried out. Perforations are more frequent in these cases leading to surgery in almost a quarter of cases [136]. The technical strategy has not been standardized, and different methods have been proposed: a tapered transparent distal attachment can be useful to partially intubate the appendix [134, 135, 137], traction methods can be useful [136, 138]; water immersion may be more effective in maintaining the distension of the appendiceal lumen [137, 139].
Ano-Rectal Junction
The perineal rectum is characterized by: a narrow lumen at the anal sphincter that makes visualization and operability difficult; abundant blood vessels and hemorrhoids; squamous epithelium rich in sensory nerves. Holt et al. [140] showed that EMR at the ano-rectal junction (ARJ) is almost always piecemeal with a high 22% recurrence rate. The disadvantages of piecemeal EMR at the ARJ are even more relevant that in other locations: incomplete resections and scarring recurrences becomes even more difficult to be visualized and retreated; inaccurate T1 cancer microstaging leads to the unnecessary demolitive surgery. Due to these limitations, tumors at the ARJ have been mainly resected by transanal surgical approach with suboptimal outcomes: high recurrence rates ranging from ranging from 23% to 31% [141], and complications, such as temporary ileostomy in some cases [142]. Recent data indicate that ESD at the ARJ is successful (Table 7), although operation times are longer [143,144,145], and curative resection rates are lower due to burning artifacts at the anal side of the specimen since mucosal incision is often conducted below the dentate line.
Technical points for ESD at the ARJ are: a tapered transparent hood may be more effective than straight ones to maintain a good visual field into the anal canal; injection of 1% lidocaine (100 mg/10 mL) on the anal side reduces pain while dissecting at the ARJ; SM dissection should be conducted just above the muscularis propria to shut off vessels that penetrate vertically and supply hemorrhoids. Specific adverse events of ER at the ARJ are a postoperative anal pain in 16–18% of patients that can be managed by oral non-steroidal anti-inflammatory drugs, and a proctostenosis if resection is circumferential [150]. The risk of delayed bleeding of ESD at the ARJ is similar to that of rectal ESD, and not increased by hemorrhoids .
Nonlifting Lesions
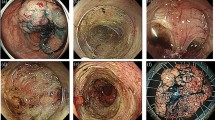
Neoplasms may have a positive non-lifting sign due to: (1) carcinomatous SM invasion; (2) scars of previous biopsies and/or resection attempts; and (3) specific morphologies. Biopsies should never be performed when ER is possible. Difficult neoplasms should be referred to high-volume referral centers: the first attempt at ER should be associated with the highest rate of success; an attempt to see if ER might be possible should be avoided. If SM invasive neoplasms with a positive nonlifting sign should not undergo ER, nonlifting intramucosal neoplasms are a specific ESD indication: EMR has a high failure rate in these cases since the snare slips over. However, severe and/or diffuse SM fibrosis is the most important prognostic of difficulty for ESD [69, 151], and its presence need to be assessed preoperatively: residual neoplasms have visible scars; naïve non-granular and bulky morphologies have a high prevalence of SM fibrosis. Matsumoto et al. [152] classified SM fibrosis in: F0, no fibrosis, blue transparent layer; F1, mild fibrosis, white web-like structures in the blue submucosal layers; F2, severe fibrosis, white muscular structure without blue transparent layer. F0–1 and F2 neoplasms showed significantly different en bloc resection rates (84% vs. 33%) and perforation rates (17% vs. 11%). Subsequent studies confirmed the negative impact of severe fibrosis on ESD outcomes: longer operating time, lower en bloc resection and complete resection rates, and higher discontinuance and perforation rates (Table 8).
A unique technique is required for ESD of nonlifting neoplasms, the main issue being the facilitation of the SM access. The PCM was found to be advantageous for ESD of F2 neoplasms with higher en bloc and complete resection rates, and lower operating time [156]. Mucosal incision should be performed at a larger distance so that dissection can be initiated into nonfibrotic SM tissue in order to create the lesion flap and a facilitated SM access. The colonic localization represents an addition difficulty and increases the risk for perforation. Previous histological results are determinant before planning ER of residual or local recurrent lesions.
Inflammatory Bowel Disease
Patients with inflammatory bowel disease (IBD) have an increased risk of colorectal dysplasia and cancer. Endoscopic resection is appropriate when complete, synchronous invisible dysplasia is absent in the adjacent mucosa and in the whole colitic mucosa. Although this assumption is evidence-based for patients with small (<10 mm) polypoid neoplasms, it remains to be established if large (>20 mm), nonpolypoid IBD neoplasms can undergo ER without a high risk of metachronous cancer. Piecemeal EMR is associated with high incomplete resection rates and the need of salvage surgery [158, 159], which often means total colectomy due to the chronic inflammation cancer field effect. ESD is the only possibility, as indicated in all guidelines, but it has been evaluated only recently in few small experiences. The first study by Iacopini et al. [160] comprised 10 patients underwent ESD in Italy and Japan. ESD resulted highly successful, and no metachronous cancer and/or invisible dysplasia developed during the short follow-up (median 24 months). Similar results have been reported by other studies (Table 9).
ESD in IBD is difficult. SM fibrosis is highly prevalent due to long-standing chronic inflammation, and also because most neoplasms are submitted to multiple biopsies and/or attempts of resection before being referred for ESD in expert centers. Delineation of neoplasm margins may be extremely difficult and requires prolonged times, the best high-definition scope, chromoendoscopy by narrow band imaging and dye application with acetic acid and indigo carmine. Magnification may be helpful. IBD neoplasms may show the coexistence of adenomatous and nonadenomatous patterns (hyperplastic and inflammatory), so that there could be overlap features of lesion margins and the background mucosa. The ESD strategy should be modified to include peripheral dot markings 5 mm beyond the lesion margins as for gastric ESD; mucosal incision be performed at a wider distance from neoplasm edges to guarantee a wide rim of normal mucosa and exclude adjacent invisible dysplasia that is pivotal to confirm a curative resection. Finally, endoscopists and patients should strictly adhere to strict long-term follow-ups .
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this entry
Cite this entry
Iacopini, F., Saito, Y. (2021). Endoscopic Submucosal Dissection of Colorectal Lesions. In: Testoni, P.A., Inoue, H., Wallace, M.B. (eds) Gastrointestinal and Pancreatico-Biliary Diseases: Advanced Diagnostic and Therapeutic Endoscopy. Springer, Cham. https://doi.org/10.1007/978-3-030-29964-4_19-1
Download citation
DOI: https://doi.org/10.1007/978-3-030-29964-4_19-1
Received:
Accepted:
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29964-4
Online ISBN: 978-3-030-29964-4
eBook Packages: Springer Reference MedicineReference Module Medicine