Abstract
In this chapter, we review evidence supporting the tuberculosis (TB) disease spectrum, rather than dichotomous categories of latent M. tuberculosis infection (LTBI) and active disease, as TB pathophysiology is important when considering TB prevention and treatment. We also describe the impact of immunocompromising conditions, specifically human immunodeficiency virus (HIV) infection, along the TB disease spectrum. We review the indications for treatment of LTBI among people living with HIV (PLWH) and the evidence behind the LTBI treatment regimens currently recommended by the World Health Organization and the United States Centers for Disease Control and Prevention. Lastly, we discuss the importance of antiretroviral therapy (ART) in addition to anti-mycobacterial therapy for the prevention of TB among PLWH, as well as the drug-drug interactions with concomitant antiretroviral therapy and LTBI treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tuberculosis disease spectrum
- Latent M. tuberculosis infection
- Tuberculin skin test
- Interferon gamma release assay
- Human immunodeficiency virus
- Antiretroviral therapy
- Isoniazid
- Rifampicin
- Rifabutin
- Rifapentine
- Directly observed therapy
Latent TB Infection and TB Disease: A Spectrum
Traditionally, tuberculosis (TB) has been viewed as a dichotomous disease entity in which a person with TB has either latent TB infection (LTBI) or active TB disease. LTBI is classically defined as evidence of an immunologic response to M. tuberculosis (Mtb) antigens via an in vivo tuberculin skin test (TST) or an in vitro interferon-gamma release assay (IGRA) in the absence of other signs and/or symptoms of TB disease. Active TB disease has been distinguished from LTBI by the presence of objective signs and/or symptoms of TB disease, such as cough, fever, night sweats, hemoptysis, and weight loss. However, evidence of an immunologic response to Mtb antigens via either a TST or IGRA is not required for the diagnosis of active TB disease. Importantly, the TST and IGRA are unable to distinguish between LTBI and active TB disease.
More recent evidence suggests that TB is a spectrum of disease pathology, and not simply a dichotomous disease entity. In 2009, Young and colleagues proposed a novel paradigm that involved a spectrum of responses to and control of Mtb infection (Fig. 1): (1) an innate immune response in which Mtb infection is eliminated without priming of antigen-specific T-cells; (2) an acquired immune response in which infection is eliminated with T-cell priming; (3) quiescent infection during which bacteria can persist in a non-replicating form and infection is controlled; (4) active infection in which bacteria are replicating at a sub-clinical level (i.e. asymptomatic) that is controlled by the immune response and; (5) clinical disease in which overt signs and symptoms are observed due to bacterial replication despite immune responses [1]. There is in vitro, non-human primate, and clinical human evidence to support this concept of a spectrum of TB disease pathology, as discussed below.
A spectrum of responses to tuberculosis infection (Adapted from Young et al. Trends in Microbiology 2009) [1]
First, the elimination of Mtb infection by the innate immune response, without T-cell priming via an acquired immune response, is supported by the finding that some healthy people who are repeatedly exposed to TB do not develop a positive TST or IGRA [2,3,4,5]. In addition to never becoming infected, another explanation for this finding is that current tests are unable to detect the host’s acquired immune response. The latter could be due in part to the imperfect sensitivity of the TST or the IGRA , particularly when the host’s immune system is compromised (e.g. human immunodeficiency virus [HIV]) [6,7,8,9]. Another possible explanation is that some people exposed to TB do not need an acquired immune response for bacterial elimination. For example, a person might expectorate Mtb bacilli before the immune system is exposed. Alternatively, the innate immune response (via neutrophils or macrophages) could eliminate Mtb without necessitating an acquired immune response [10, 11].
Second, elimination of Mtb infection by the acquired immune response is supported by the finding that some people with a positive IGRA revert to negative on subsequent testing, and never develop a positive TST. Although some reversions may be related to the sub-optimal reproducibility of the IGRA using current cutoffs for a positive result [12, 13], elimination of Mtb infection via transient activation of the acquired immune response may also revert an IGRA from positive to negative [14].
While in vivo evidence is lacking, there is in vitro evidence that Mtb can persist in a non-replicating form, as seen in quiescent infection. This dormant state has been described using the Wayne model, in which bacilli are deprived of oxygen [15]. Oxygen-deprived bacilli upregulate genes controlled by two sensor kinases (dosS and dosT) and a response regulator (dosR) [16, 17]. The dosR response regulator includes genes involved in triglyceride synthesis, which are required when the bacilli shift their carbon source from glucose to fatty acids [18, 19]. With more prolonged oxygen deprivation, many genes responsible for transcriptional regulation are induced [20]. Dormant bacteria may be resuscitated, either randomly or due to unknown signals, and serve as “scouts” which test the conditions of the local environment. If these scouts are not cleared by the immune system (e.g., immunocompromised states, including HIV-infection), they will continue to replicate and signal the remainder of the dormant bacilli to replicate which, in turn, leads to sub-clinical and clinical TB disease. These scout signals may take the form of a protein called Rpf (resuscitation promoting factor), which has been shown to increase the recovery of Mtb from the sputum of patients with active TB [21].
Sub-clinical TB disease occurs in the macaque TB model, which may most closely resemble the human TB disease spectrum. Monkeys with sub-clinical TB, termed “percolators”, are clinically normal but may have positive cultures for Mtb months and even up to 1 year after infection with Mtb [22]. Sub-clinical TB is also well-described in humans, particularly among people living with HIV [23]. Perhaps the best human example of the transition from subclinical to clinical TB disease is provided by treatment of people living with HIV with antiretroviral therapy (ART). A vigorous recovery of T cell responses on ART has been associated with unmasking of sub-clinical TB in the setting of immune reconstitution inflammatory syndrome (IRIS) [24, 25].
Understanding this spectrum of TB disease is important when considering treatment for latent Mtb infection. Based on this paradigm, persons diagnosed with LTBI represent a heterogenous group of individuals—those who have already cleared the infection, are infected with bacilli in a non-replicating form, or infected with actively replicating bacilli but have no overt signs or symptoms of clinical disease. Therefore, anti-tuberculous drugs may be effective because non-replicating bacilli can be targeted by affecting cell wall maintenance and repair, or because Mtb bacilli periodically replicate (e.g. “scouts”) and this is inhibited by the drugs. An improved understanding of the TB disease spectrum is critical for future TB drug development.
Immunocompromise in the setting of HIV-infection likely has effects all along this disease spectrum. First, PLWH may be unable to mount an adequate innate or acquired immune response, leaving them less likely to clear infection following exposure compared to HIV-negative persons. Second, PLWH may also be unable to clear “scouts” that signal other dormant bacilli to replicate and cause sub-clinical or clinical TB disease following infection. Thirdly, PLWH and severe immunocompromise may not progress from subclinical to clinical TB for long periods of time. In contrast, the progression from subclinical to clinical TB may be accelerated among PLWH in the setting of antiretroviral therapy initiation and immune reconstitution.
Treatment of Latent TB Infection with Anti-TB Therapy
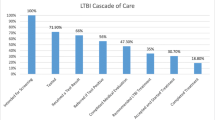
There are several regimens available for the treatment of LTBI among people living with HIV (Table 1). Currently in the US, guidelines recommend testing for latent TB infection using TST or IGRA at the time of HIV diagnosis, regardless of epidemiological risk factors for TB exposure. PLWH, CD4+ counts <200 cells/μL, and negative tests for LTBI should be retested once they have started antiretroviral therapy (ART) and CD4+ counts are over 200 cells/μL. Annual testing (using TST) is only recommended for PLWH if they are at high risk for repeated/ongoing exposure to people with active TB [31]. In the US, treatment for LTBI is only recommended for PLWH who test positive for LTBI [28,29,30]. According to the WHO guidelines, PLWH who have an unknown or positive TST (and are unlikely to have active TB) are recommended to receive treatment for latent TB infection. HIV-negative persons are recommended to receive treatment if they are household contacts of a person with pulmonary TB or if they belong to other at-risk groups [26, 27].
Isoniazid
Isoniazid (INH) monotherapy is endorsed as an LTBI treatment option by both the World Health Organization (WHO) [26, 27] and the United States Centers for Disease Control and Prevention (CDC) [28,29,30]. The WHO guidelines recommend INH daily for 6 months regardless of HIV-status, in countries with either high or low TB incidence, as a strong recommendation. In contrast, the CDC recommends INH daily for 9 months, regardless of HIV-status. The CDC endorses isoniazid for 6 months as an alternative regimen. There are no special antiretroviral therapy considerations during INH monotherapy for LTBI.
Randomized trials have shown that both 6 and 12 months of INH, when compared to placebo, significantly reduce the incidence of TB disease in both HIV-negative [32,33,34] and HIV-positive populations [35, 36]. Only one trial, conducted by the International Union Against Tuberculosis (IUAT) among an HIV-negative population, was designed to compare 6 vs. 12 months of INH. This study showed a 65% efficacy of 6 months of INH and 75% efficacy of 12 months of INH during 5 years of follow-up [33]. The 6-month INH regimen has not been directly compared to 12 months duration in clinical trials among HIV-positive populations.
Data on direct comparisons of treatment pairs for the outcome of active TB are lacking for 9-months compared to either 6 or 12 months. Through a network meta-analysis, indirect evidence regarding these comparisons is available. For example, although 9 months of INH has not been directly compared to either 6 or 12 months, all three have been compared to no treatment and both 6 and 12 months have been compared to placebo, allowing indirect comparisons to be made. Using network meta-analysis, the odds ratio for active TB was 0.65 (95% Credible Interval [Crl] 0.50–0.83) for 6 months INH, 0.75 (95% Crl 0.35–1.62) for 9 months INH, and 0.50 (95% Crl 0.41–0.62) for 12–72 months INH compared to placebo. The 95% credible intervals for all INH durations are overlapping, indicating no significant differences in the prevention of active TB. Stratifying results by HIV-status revealed no statistically significant difference in effect estimates for all INH durations [37]. In addition to these data, the WHO Guideline Development Group (GDG) considered programmatic feasibility, resource requirements, and patient acceptability in their preference for 6 over 9 months of INH. The 6-month regimen is more cost-effective than the 12-month regimen [38].
Data supporting the CDC’s recommendation for 9-month INH duration over the 6-month duration are largely extrapolated from two studies including only HIV-negative persons, neither of which were designed to directly compare various INH durations. A post-hoc analysis of a randomized trial conducted by the US Public Health Service [34] showed that among persons believed to have taken at least 80% of INH therapy, TB rates dropped 68% if INH was taken for 10–12 months and only 16% when taken for less than 10 months when compared to placebo [32]. Another post-hoc analysis was conducted using data from the Bethel Isoniazid Studies [39, 40] and included participants who had taken a wide range of INH durations, from none up to 24 months. TB case rates per 100 persons were plotted against the duration of INH in months and the observed points were fitted with a simple curve. This curve approached horizontal at approximately 9–10 months duration [41]. However, the CDC also notes that cost-effectiveness may be a consideration for the 6-month duration depending on the local health department conditions.
Continuous Isoniazid
A treatment duration of at least 36 months (or continuous isoniazid) is recommended by the WHO for PLWH who have either a positive TST, or unknown TST result in settings with high TB incidence and high rates of Mtb transmission, as defined by national authorities. It was recognized by the GDG that PLWH with a positive TST (or unknown TST result) as well as those receiving antiretroviral therapy (ART) are more likely to benefit [42]. This is a conditional recommendation with low-quality evidence based largely on the results of a systematic review including three studies conducted in Botswana, South Africa, and India [43]. Compared to 6 months of INH, patients receiving continuous isoniazid had a 38% lower risk of active TB (relative risk [RR] 0.62, 95% CI 0.42–0.89) [43]. Among those with a positive TST there was a 49% lower risk of active TB (RR 0.51, 95% CI 0.30–0.86) and a 50% lower risk of mortality (RR 0.50, 95% CI 0.27–0.91) [43]. Among those with a negative TST there was no significant decrease in active TB or mortality, although the point estimate indicated a reduction in TB incidence of 27% [43]. All but one of these studies excluded participants eligible for ART [44]. In this study, those PLWH with a positive TST receiving continuous isoniazid and 360 days of ART had a 96% lower risk of active TB than those PLWH with a positive TST who received only 6 months of isoniazid and no ART (adjusted hazard ratio [aHR] 0.04, 95% CI 0.005–0.35). Among those with a positive TST receiving 6-months of isoniazid and 360 days of ART, the reduction in the risk of active TB was only 50% (aHR 0.50, 95% CI 0.26–0.97) compared to TST-positive participants receiving 6-months of isoniazid but not receiving ART [44].
Two of the studies found no statistically significant increase in adverse events in the continuous isoniazid group [44, 45]; a third study reported an increase in grade 3 or 4 adverse events (32 vs. 9.5%, RR 3.41, 95% CI 2.28–5.09) [46], but meta-analysis was not preformed due to study heterogeneity [43]. The pooled relative risk of study drug discontinuation due to adverse events was 5.96 (95% CI 4.12–8.62) for the continuous isoniazid group compared to the 6-month treatment duration group [43].
Only one of the studies included in this meta-analysis reported data on adherence [46]. The proportion of patients who reported or were observed taking more than 90% of their assigned treatment regimen in the allotted time frame were 84% in the 6-month isoniazid arm and 89% in the continuous isoniazid arm. In the continuous arm, the median treatment duration was 3.3 years (IQR 2.1–4.3 years). The proportion of patients who had to permanently discontinue medication was highest for the continuous isoniazid arm (36.5%) compared to the rifapentine-isoniazid arm (1.8%), rifampicin-isoniazid arm (3.8%), and 6-month isoniazid arm (1.9%). Similarly, this was the only study included in the meta-analysis which reported resistance rates for incident TB cases in both the continuous and 6-month isoniazid groups [46]. They found 1 case of isoniazid resistance in the continuous isoniazid arm and no cases in the 6-month arm (RR 5.96, 95% CI 0.24–146). The other two studies reported that the observed rate of INH resistance in incident cases was similar between the continuous and 6-month isoniazid groups, and not different from the expected rate of INH resistance in the population [44, 45].
Data on the cost-effectiveness of continuous isoniazid are limited. One study utilized data from a National Institute for Research in Tuberculosis clinical trial conducted in India in conjunction with a previously published model of TB and HIV co-infection [47]. Compared to no preventive therapy, 6 months of isoniazid increased life expectancy by 0.8 months at a lifetime cost per person of $57,00 US dollars; continuous isoniazid increased life expectancy by 1.0 months at a lifetime per person cost of $5,780 US dollars. The incremental cost-effectiveness ratio (ICER) for continuous isoniazid was $4,290 per year of life saved compared to $1,140 for 6 months of isoniazid. The WHO Commission on Macroeconomics and Health suggests that a regimen is cost-effective if the incremental cost-effectiveness ratio is <3 times the Gross Domestic Product (GDP) per capita ($2,490 US dollars in India in 2009) making the 6-month isoniazid regimen (ICER $1,140) cost-effective and the continuous isoniazid regimen (ICER $4,290) not cost-effective [47]. A second study developed a decision-analytic model utilizing previously published data with health care costs from South Africa [48]. This study also considered varying antiretroviral coverage (55% versus 90%), presence of infection control practices, type of TB diagnostic algorithms (sputum smear and chest radiography versus Xpert MTB/RIF), and presence of intensified case finding in addition to isoniazid duration (6 versus 36 months) in the strategies evaluated. The 36-month strategy was most cost-effective when packaged together with expanded ART provision (90%), infection control, Xpert MTB/RIF, and intensified TB case finding. The incremental cost-effectiveness ratio (ICER) per TB case averted was $28,936 US dollars [48]. A third study, also utilizing a decision-analytic model, used primary data and key results from a clinical trial conducted in Botswana [44]. This study considered TST results in the decision to provide isoniazid and a CD4+ lymphocyte cut-off of 250 and 500 cells/ μL in the decision to provide ART in addition to isoniazid duration (6 versus 36 months). Providing 36 months of isoniazid to only TST-positive PLWH and providing ART only when CD4+ counts were <250 cells/μL was the most cost-effective strategy with respect to ICER per TB case averted ($1,612 US dollars) and ICER per death averted ($2,418) [49].
The WHO GDG noted that consideration be given to the increased resource needs for implementation of continuous isoniazid at the programmatic level, as it is known that global implementation of the 6-month regimen among PLWH is low. The preference for TST before starting therapy was recognized as a possible barrier. Additionally, the committee expressed concerns about lower completion rates and adherence with a longer regimen as well as the development of isoniazid resistance. Continued research on operationalizing continuous isoniazid among PLWH is needed.
Rifamycin-Containing Regimens
There are several rifamycin-containing regimens available as options for treatment of LTBI and endorsed by the WHO and/or CDC as discussed below.
Rifampicin
The WHO guidelines recommend daily rifampicin for 3–4 months as an alternative to isoniazid monotherapy in countries with low TB incidence [26, 27]. The CDC guidelines also recommend daily rifampicin for 4 months as an alternative regimen [28]. Rifampicin-containing regimens must be prescribed with caution to PLWH in high-burden settings. This population has a higher possibility of sub-clinical or undiagnosed TB, which if treated with monotherapy could result in rifampicin resistance.
In addition, there are several drug-drug interactions between rifampicin and ART. Currently, a non-nucleoside reverse transcriptase inhibitor (NNRTI) plus two nucleoside reverse transcriptase inhibitors (NRTIs) is the recommended first-line ART regimen with rifampicin-based therapy. The preferred NRTI backbone is abacavir (ABC), zidovudine (AZT), or tenofovir (TDF) with either lamivudine (3TC) or emtricitabine (FTC). The preferred NNRTI is efavirenz (600 mg) although nevirapine can be considered for patients with an intolerance or contraindication to efavirenz [50,51,52]. Nevirapine induces its own metabolism and is, therefore, initiated using a lead-in dose of 200 mg/day for 2 weeks before increasing to full doses of 400 mg/day. Rifampicin can also lower serum nevirapine levels in addition to this auto-induction [53]. When evaluated in clinical trials, nevirapine with lead-in dosing has been shown to be associated with low serum nevirapine concentrations, decreased antiviral efficacy, emergence of drug resistance, and death [54,55,56,57]. Therefore, experts suggest starting nevirapine at full-dose when it is co-administered with rifampicin [50, 51]. However, when compared to efavirenz , even full-dose nevirapine has been shown to be associated with poor virologic outcomes and higher rates of discontinuation due to toxicity [58]. These data strengthen the preference for efavirenz over nevirapine as the NNRTI of choice during rifampicin co-administration.
Integrase inhibitor-based regimens are now increasingly used as first-line therapy, including in resource-limited settings. Raltegravir and dolutegravir are metabolized mainly by uridine 5′-diphospho-glucuonosyltransferase 1A1, which is induced by rifampicin. Co-administration of these agents with rifampicin reduces serum levels of both drugs. For this reason, rifabutin is preferred over rifampicin by the CDC guidelines. However, there are emerging data that rifampicin may be co-administered with raltegravir if doses are increased to 800 mg twice daily [59,60,61] or with dolutegravir if doses are increased to 50 mg twice daily [62, 63]. Based on these data and expert opinion, the CDC currently favors the increased dose of raltegravir and dolutegravir when co-administered with rifampicin until further data are available [51]. Additional details on drug-drug interactions between rifampicin and integrase inhibitors can be found in the chapter on pharmacologic considerations during the co-treatment of HIV and TB.
In a network meta-analysis of studies including both HIV-negative and HIV-positive persons, rifampicin monotherapy was effective at preventing active TB when compared to placebo (OR 0.41, 95% CI 0.19–0.85). Rifampicin monotherapy had a lower odds of hepatotoxicity than either 6 or 9-months of isoniazid. The odds ratio for hepatotoxicity with rifampicin monotherapy was 0.03 (95% CI 0.00–0.48) compared to 6-months isoniazid and 0.17 (95% CI 0.06–0.47) compared to 9-months of isoniazid. Stratifying results by HIV-status revealed no statistically significant difference in effect estimates [37].
Since the publication of this meta-analysis, the first randomized controlled trial investigating the effectiveness of 4 months of rifampicin (and compared to 9 months of isoniazid) has been published. Participants were eligible if they were 18 years of age or older, and had a positive TST. Among 6012 participants enrolled, 242 (4.0%) were HIV-positive. There were 3443 participants enrolled in the rifampicin group; 4 developed confirmed active TB and 4 developed clinically diagnosed active TB over 7732 person-years of follow-up. Among 3416 participants enrolled in the isoniazid group, 4 developed confirmed active TB and 5 developed clinically diagnosed active TB over 7652 person-years of follow-up. The rate difference for rifampicin minus isoniazid was <0.01 cases/100 p-y (95% CI −0.14 to 0.16) for confirmed active TB and < 0.01 cases/100 p-y (95% CI −0.23 to 0.22) for confirmed or clinically diagnosed TB. The upper bound of the 95% confidence interval was below the prespecified noninferiority margin of 0.75; thus the 4-month rifampicin regimen was noninferior to 9 months of isoniazid. Treatment completion was better for rifampicin compared to isoniazid (rate difference 15.1%, 95% CI 12.7 to 17.4%). There were fewer grade 3–5 adverse events (rate difference − 1.1%, 95% CI −1.9—0.4%) and fewer grade 3–5 hepatotoxicity events (rate difference −1.2%, 95% CI −1.7 to −0.7%) for rifampicin compared to isoniazid.
Rifabutin
The CDC guidelines note that rifabutin can be substituted for rifampicin among PLWH on ART regimens that are known to interact with rifampicin, such as protease-inhibitor (PI) based or integrase inhibitor based ART [28]. Rifabutin is not recommended in the WHO LTBI treatment guidelines [26, 27]. Although rifabutin is a less potent inducer of CYP isoenzymes, rifabutin itself is metabolized by CYP3A enzymes. Co-administration with PI-based ART, therefore, leads to CYP3A inhibition and increased serum rifabutin levels. Experts suggest decreasing rifabutin doses to 150 mg daily when co-administered with PI-based ART [64]. If rifabutin is not available, double dose lopinavir/ritonavir is the only PI that can be used with rifampicin although these patients must be monitored closely for hepatotoxicity. No dose adjustments are required when rifabutin is co-administered with either raltegravir or dolutegravir.
Rifabutin has been evaluated in a phase II pilot study including 44 participants with LTBI and HIV co-infection . Participants were eligible if they were TST positive adults with confirmed HIV-infection; they were excluded if CD4+ counts were < 200 cells/μL. Participants were randomized to receive either rifabutin 300 mg and isoniazid 750 mg twice weekly for three months (arm 1, n = 16), rifabutin 600 mg and isoniazid 750 mg twice weekly for three months (arm 2, n = 14), or isoniazid 300 mg daily for 6 months (arm 3, n = 14). The study was terminated early prior to reaching enrollment goals by the pharmaceutical sponsor. Three, one, and four subjects did not complete treatment in arms 1, 2, and 3, respectively. Adverse events were reported for four, nine, and seven participants in arms 1, 2, and 3, respectively. During follow-up two cases of active TB were identified (both in the isoniazid monotherapy arm) [65].
Rifampicin and Isoniazid
The WHO guidelines recommend rifampicin plus isoniazid daily for 3 months as an alternative to isoniazid monotherapy in countries with a low TB incidence [26, 27]. ART considerations when using this regimen are the same as those for rifampicin monotherapy as described above.
In a network meta-analysis of studies including both HIV-negative and HIV-positive persons, rifampicin plus isoniazid was effective in preventing active TB when compared to placebo (OR 0.53, 95% CI 0.36–0.78). Furthermore, when using standard meta-analysis methods for direct pairwise comparisons between regimens, rifampicin plus isoniazid did not differ from isoniazid of any duration with respect to prevention of active TB. Rifampicin plus isoniazid also did not differ from isoniazid of either 6 or 9-months in duration with respect to the development of hepatotoxicity. Stratifying results by HIV-status revealed no statistically significant difference in effect estimates [37].
Isoniazid and Rifapentine
The WHO guidelines recommend rifapentine plus isoniazid weekly for 12 weeks (3HP) in countries with a low TB incidence (strong recommendation) and those with a high TB incidence (conditional recommendation) [26, 27]. The CDC guidelines first recommended 3HP among PLWH in December 2011 if they were otherwise healthy and not taking antiretroviral therapy and if 3HP was given by directly-observed therapy [29]. This recommendation was based largely on the results of the PREVENT TB trial which compared 3HP given weekly by directly observed therapy to 9H given daily by self-administered therapy [66]. The primary endpoint was active TB and the non-inferiority margin was 0.75%. There were 403 PLWH enrolled in the United States, Brazil, Spain, Peru, Canada, and Hong Kong; median CD4+ count was 495 (IQR 389–675 cells/μL). Participants receiving or planning to initiate ART during the first 90 days after enrollment were excluded. Cumulative TB rates were 1.01% in the 3HP arm and 3.50% in the 9H arm (rate difference − 2.49, upper 95% CI of the difference 0.60%). Treatment completion was higher in the 3HP arm compared to the 9H arm (89% versus 64%, p < 0.001). Discontinuation of study drug due to adverse events was similar (3% in 3HP arm versus 4% in 9H arm, p = 0.79) [66].
In June 2018, these recommendations were updated to also include PLWH who were taking efavirenz or raltegravir-based ART. Moreover, self-administered therapy was now an allowed mode of administration in the United States based on local resources and patient characteristics [30]. The inclusion of PLWH taking standard dose efavirenz or raltegravir-based ART were based on pharmacokinetic studies [67, 68]. Co-administration of dolutegravir and rifapentine is not currently recommended, but some pharmacokinetic data on this topic are discussed in the chapter on pharmacologic considerations during co-treatment of HIV and TB. Self-administered 3HP was evaluated in the iAdhere study, which compared that administration method to directly-observed therapy [69]. The primary endpoint was treatment completion and the non-inferiority margin was 15%. Among 1002 participants enrolled in the United States, Spain, Hong Kong, and South Africa, 11 (1.1%) were known to be HIV-positive. Overall, treatment completion was 87% (95% CI 83–91%) in the direct observation group, 74% (95% CI 70–79%) in the self-administration group, and 76% (95% CI 71%–81%) in the self-administration with text message reminders group. In the United States, treatment completion was 85% (95% CI 81–89%), 78% (95% CI 73%–83%) and 77% (95% CI 71–82%), respectively. Therefore, treatment completion of self-administered therapy was non-inferior to directly observed therapy in the United States but not overall or outside of the United States [69].
This short course regimen (3HP) has been evaluated in a cost-effectiveness study in both high- and low-burden settings. Using a cohort of PLWH in a Ugandan HIV clinic, 3HP was estimated to avert 9 cases of TB and 1 death for every 1000 PLWH on ART when compared to isoniazid monotherapy [70]. Incremental cost effectiveness was estimated at $9,402 US dollars per disability-adjusted life year averted. In this model, the cost-effectiveness of 3HP was highly dependent on the cost of rifapentine, completion of treatment, and the prevalence of LTBI. The authors concluded that in comparison to isoniazid monotherapy, that 3HP would only be cost-effective in this high burden setting if the price of rifapentine was reduced and treatment completion rates were high (>85%) [70]. In a US setting, the cost-effectiveness of 3HP was initially evaluated using a cost per dose of 3HP of $12.31 US dollars [71]. In this analysis, 3HP was estimated to avert 5.2 cases of TB for every 1000 people treated. The 3HP regimen would cost $21,525 and $4,294 more per TB case prevented compared to 9H from a health system and societal perspective; it would cost $4,565 and $911 per quality adjusted life year, respectively. In the US, activities costing <$50,000/QALY gained are generally considered to be cost-effective [71]. These estimates were updated after the price of rifapentine was reduced and the cost per dose of 3HP dropped to $6 [72]. In the updated analysis, the cost to the health system per TB case averted by 3HP decreased to $8,816 and the cost to the health system per QALY gained decreased to $1,879. Additionally the authors estimated that switching from 9H to self-administered 3HP would lead to an additional $141 saved per individual treated from a health system perspective and $231 saved per individual treated from a societal perspective. Therefore, in low burden settings the 3HP regimen was deemed to be cost-effective when compared to 9H, with additional savings following the reduction in rifapentine pricing and ability to provide self-administered therapy [72].
The BRIEF-TB trial conducted by the AIDS Clinical Trial Group evaluated an ultra-short 1-month course of daily self-administered rifapentine and isoniazid for treatment of LTBI among PLWH [73]. Participants were eligible if they were at least 13 years old and lived in a high burden TB setting or were TST/IGRA positive. Concomitant ART with an efavirenz or nevirapine based regimen was allowed. Participants were stratified by ART status and CD4+ count and randomized to either 9 months of isoniazid 300 mg daily or one month of weight based-rifapentine plus isoniazid 300 mg daily. The primary outcome was a combined endpoint of active TB, death due to TB, and death due to unknown causes. There were 3000 participants; 50% were on ART and median CD4+ count was 470 cells/ μL (IQR 346–635 cells/μL). Only 634 (21%) had a positive TST/IGRA. A non-inferiority margin of 1.25/100 person-years was set based on an assumed 2.0/100 p-y incidence of the primary endpoint in the 9H arm. The incidence of the primary endpoint was 0.69/100 person-years in the 1HP arm and 0.72/100 p-y in the 9H arm (IR difference − 0.025, upper 95% CI 0.31). Since the upper bound of the 95% CI was below the non-inferiority margin, the 1HP regimen was deemed non-inferior to the 9H regimen. There was no difference in serious adverse events between arms (5.6% 1HP versus 7.1% 9H, p = 0.1). There was a higher incidence of targeted safety events in the 9H arm (5.1/100 p-y) compared to the 1HP arm (3.3/100 p-y, p = 0.03). Treatment completion was higher in the 1HP arm compared to the 9H arm (97% versus 90%, p < 0.01). There was one case of rifampicin-resistance TB in each arm and 1 case of isoniazid-resistant TB in the 9H arm [73]. Additional studies conducted in low-burden TB settings and on the pharmacokinetics of integrase inhibitors when co-administered with daily rifapentine dosing are needed.
Rifapentine was approved by the US Food and Drug Administration for the treatment of latent TB in 2014. Despite the drop in price as discussed above, the drug has not been widely registered outside the US, raising concerns for global access to rifapentine. In 2015, the 20th World Health Organization (WHO) meeting on the selection and use of essential medications recommended the addition of Rifapnetine to the WHO Model List of Essential Medications (EML) [74]. The addition of a medication to the EML often leads to increased demand from country governments and subsequently stimulates drug manufacturers to invest in registration in these countries.
Effect of Antiretroviral Therapy in Preventing the Progression of Latent TB Infection
Many studies have demonstrated the protective effect of ART on the incidence of active TB disease. In 2012, a systematic review and meta-analysis was conducted which included randomized controlled trials, prospective cohort studies, and retrospective cohort studies if they compared TB incidence by ART status among HIV-positive adults for a median of at least 6 months in developing countries [75]. The authors found that ART was strongly associated with a reduction in TB incidence regardless of CD4+ count: HR 0.16 (95% CI 0.07–0.36) for CD4+ <200, HR 0.34 (95% CI 0.19–0.60) for CD4+ 200–350, HR 0.43 (95% CI 0.30–0.63) for CD4+ >350, and HR 0.35 (95% CI 0.28–0.44) for any CD4+ count [75].
Following the publication of this systematic review an additional clinical trial using a 2-by-2 factorial design was conducted to assess the benefits of early ART, 6-months of isoniazid preventive therapy, or both among PLWH in Ivory Coast – the TEMPRANO trial [76]. Participants were included if they had CD4+ counts <800 cells/μL and did not meet criteria for ART initiation according to WHO guidelines. They were randomly assigned to deferred ART (ART initiation per WHO guidelines), deferred ART plus isoniazid, early ART (immediate ART initiation), or early ART plus isoniazid. The primary endpoint was a composite endpoint including AIDS, non-AIDS defining cancer, non-AIDS defining bacterial disease, or death from any cause at 30 months. There were 2056 participants enrolled and followed for 4757 person-years. Tuberculosis accounted for 42% of the 204 primary endpoints observed. Early ART initiation was associated with a decreased incidence of TB (aHR 0.50, 95% CI 0.32–0.79) compared to deferred ART initiation among all patients. When stratified by baseline CD4+ count, early ART initiation was associated with a similar decrease in TB incidence for those with baseline CD4+ count <500 cells/μL (aHR 0.48, 95% CI 0.27–0.87) and a trend toward a decreased incidence for those with a baseline CD4+ count >500 cells/μL (aHR 0.54, 95% CI 0.26–1.09). Isoniazid preventive therapy was associated with a decreased incidence of TB overall (aHR 0.44, 95% CI 0.28–0.69), regardless of baseline CD4+ count (aHR 0.42 [95% CI 0.23–0.76] for CD4 < 500 cells/μL and aHR 0.47 [95% CI 0.23–0.97] for CD4 > 500 cells/μL). The group who received both early ART plus isoniazid had the fewest number of TB events (n = 11), followed by those who received deferred ART plus isoniazid (n = 16), early ART alone (n = 17), and deferred ART alone (n = 41) [76]. Participants who completed this trial follow-up were invited to participate in additional post-trial phase. The primary endopoint of this post-trial phase was death due to any cause from the time of inclusion in the parent trial. The hazard ratio of death was 0.63 (95% CI 0.41–0.97) after adjusting for ART timing and 0.61 (95% CI 0.39–0.94) after adjusting for ART timing, CD4+ count, and other patient characteristics [77]. These data suggest that there is additive benefit of ART and isoniazid preventive therapy in the prevention of TB.
In summary, tuberculosis is likely a spectrum of disease rather than a dichotomous condition of latent infection or active disease; the spectrum is impacted by immunocompromising conditions, particularly HIV infection. Both antiretroviral therapy and anti-mycobacterial therapy are important for the treatment of LTBI. Several anti-mycobacterial regimens are endorsed by the World Health Organization and US Centers for Disease Control and Prevention for treatment of latent TB infection among PLWH, although LTBI treatment options are limited by drug-drug interactions with antiretroviral drugs. Further research is needed to advance our understanding the TB disease spectrum, to develop novel and shorter, well-tolerated anti-mycobacterial treatment regimens, and to better characterize the interactions of anti-mycobacterial and antiretroviral drugs.
References
Young DB, Gideon HP, Wilkinson RJ (2009) Eliminating latent tuberculosis. Trends Microbiol 17(5):183–188
Stead WW (1995) Management of health care workers after inadvertent exposure to tuberculosis: a guide for the use of preventive therapy. Ann Intern Med 122(12):906–912
Joshi R, Reingold AL, Menzies D, Pai M (2006) Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. PLoS Med 3(12):e494
Morrison J, Pai M, Hopewell PC (2008) Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 8(6):359–368
Stein CM, Nsereko M, Malone LL, Okware B, Kisingo H, Nalukwago S et al (2018) Long-term stability of resistance to latent M. tuberculosis infection in highly exposed TB household contacts in Kampala, Uganda. Clin Infect Dis
Santin M, Munoz L, Rigau D (2012) Interferon-gamma release assays for the diagnosis of tuberculosis and tuberculosis infection in HIV-infected adults: a systematic review and meta-analysis. PLoS One 7(3):e32482
Chen J, Zhang R, Wang J, Liu L, Zheng Y, Shen Y et al (2011) Interferon-gamma release assays for the diagnosis of active tuberculosis in HIV-infected patients: a systematic review and meta-analysis. PLoS One 6(11):e26827
Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC et al (2011) Interferon-gamma release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis. J Infect Dis 204(Suppl 4):S1120–S1129
Cattamanchi A, Smith R, Steingart KR, Metcalfe JZ, Date A, Coleman C et al (2011) Interferon-gamma release assays for the diagnosis of latent tuberculosis infection in HIV-infected individuals: a systematic review and meta-analysis. J Acquir Immune Defic Syndr 56(3):230–238
Martineau AR, Newton SM, Wilkinson KA, Kampmann B, Hall BM, Nawroly N et al (2007) Neutrophil-mediated innate immune resistance to mycobacteria. J Clin Invest 117(7):1988–1994
Clay H, Volkman HE, Ramakrishnan L (2008) Tumor necrosis factor signaling mediates resistance to mycobacteria by inhibiting bacterial growth and macrophage death. Immunity 29(2):283–294
van Zyl-Smit RN, Pai M, Peprah K, Meldau R, Kieck J, Juritz J et al (2009) Within-subject variability and boosting of T-cell interferon-gamma responses after tuberculin skin testing. Am J Respir Crit Care Med 180(1):49–58
van Zyl-Smit RN, Zwerling A, Dheda K, Pai M (2009) Within-subject variability of interferon-g assay results for tuberculosis and boosting effect of tuberculin skin testing: a systematic review. PLoS One 4(12):e8517
Pai M, Joshi R, Dogra S, Zwerling AA, Gajalakshmi D, Goswami K et al (2009) T-cell assay conversions and reversions among household contacts of tuberculosis patients in rural India. Int J Tuberc Lung Dis 13(1):84–92
Wayne LG, Lin KY (1982) Glyoxylate metabolism and adaptation of Mycobacterium tuberculosis to survival under anaerobic conditions. Infect Immun 37(3):1042–1049
Roberts DM, Liao RP, Wisedchaisri G, Hol WG, Sherman DR (2004) Two sensor kinases contribute to the hypoxic response of Mycobacterium tuberculosis. J Biol Chem 279(22):23082–23087
Sherman DR, Voskuil M, Schnappinger D, Liao R, Harrell MI, Schoolnik GK (2001) Regulation of the Mycobacterium tuberculosis hypoxic response gene encoding alpha -crystallin. Proc Natl Acad Sci U S A 98(13):7534–7539
McKinney JD, Honer zu Bentrup K, Munoz-Elias EJ, Miczak A, Chen B, Chan WT et al (2000) Persistence of Mycobacterium tuberculosis in macrophages and mice requires the glyoxylate shunt enzyme isocitrate lyase. Nature 406(6797):735–738
Reed MB, Gagneux S, Deriemer K, Small PM, Barry CE, 3rd. The W-Beijing lineage of Mycobacterium tuberculosis overproduces triglycerides and has the DosR dormancy regulon constitutively upregulated. J Bacteriol 2007;189(7):2583–2589
Rustad TR, Harrell MI, Liao R, Sherman DR (2008) The enduring hypoxic response of Mycobacterium tuberculosis. PLoS One 3(1):e1502
Chao MC, Rubin EJ (2010) Letting sleeping dos lie: does dormancy play a role in tuberculosis? Annu Rev Microbiol 64:293–311
Lin PL, Rodgers M, Smith L, Bigbee M, Myers A, Bigbee C et al (2009) Quantitative comparison of active and latent tuberculosis in the cynomolgus macaque model. Infect Immun 77(10):4631–4642
Mtei L, Matee M, Herfort O, Bakari M, Horsburgh CR, Waddell R et al (2005) High rates of clinical and subclinical tuberculosis among HIV-infected ambulatory subjects in Tanzania. Clin Infect Dis 40(10):1500–1507
Sterling TR, Pham PA, Chaisson RE (2010) HIV infection-related tuberculosis: clinical manifestations and treatment. Clin Infect Dis 50(Suppl 3):S223–S230
Meintjes G, Lawn SD, Scano F, Maartens G, French MA, Worodria W et al (2008) Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis 8(8):516–523
World Health Organization. Guidelines on the management of latent tuberculosis infection. 2015
World Health Organization. Latent tuberculosis infection: Updated and consolidated guidelines for programmatic management 2018
American Thoracic Society (2000) Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep 49(RR-6):1–51
Centers for Disease Control and Prevention (2011) Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent Mycobacterium tuberculosis infection. MMWR Morb Mortal Wkly Rep 60(48):1650–1653
Borisov AS, Bamrah Morris S, Njie GJ, Winston CA, Burton D, Goldberg S et al (2018) Update of recommendations for use of once-weekly isoniazid-rifapentine regimen to treat latent Mycobacterium tuberculosis infection. MMWR Morb Mortal Wkly Rep 67(25):723–726
Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed April 8, 2019
Ferebee SH (1970) Controlled chemoprophylaxis trials in tuberculosis. A general review. Bibl Tuberc 26:28–106
International Union Against Tuberculosis Committee on Prophylaxis (1982) Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. Bull World Health Organ 60(4):555–564
Ferebee SH, Mount FW (1962) Tuberculosis morbidity in a controlled trial of the prophylactic use of isoniazid among household contacts. Am Rev Respir Dis 85:490–510
Bucher HC, Griffith LE, Guyatt GH, Sudre P, Naef M, Sendi P et al (1999) Isoniazid prophylaxis for tuberculosis in HIV infection: a meta-analysis of randomized controlled trials. AIDS 13(4):501–507
Akolo C, Adetifa I, Shepperd S, Volmink J (2010) Treatment of latent tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev 1:CD000171
Zenner D, Beer N, Harris RJ, Lipman MC, Stagg HR, van der Werf MJ (2017) Treatment of latent tuberculosis infection: an updated network meta-analysis. Ann Intern Med 167(4):248–255
Snider DE Jr, Caras GJ, Koplan JP (1986) Preventive therapy with isoniazid. Cost-effectiveness of different durations of therapy. JAMA 255(12):1579–1583
Comstock GW, Baum C, Snider DE Jr (1979) Isoniazid prophylaxis among Alaskan Eskimos: a final report of the bethel isoniazid studies. Am Rev Respir Dis 119(5):827–830
Comstock GW, Ferebee SH (1967) Hammes LM. A controlled trial of community-wide isoniazid prophylaxis in Alaska. Am Rev Respir Dis 95(6):935–943
Comstock GW (1999) How much isoniazid is needed for prevention of tuberculosis among immunocompetent adults? Int J Tuberc Lung Dis 3(10):847–850
World Healt Organization. Recommendation on 36 months isoniazid preventive therapy to adult and adolescents living with HIV in resource-constrained and high TB- and HIV-prevalence settings. 2015
Den Boon S, Matteelli A, Ford N, Getahun H (2016) Continuous isoniazid for the treatment of latent tuberculosis infection in people living with HIV. AIDS 30(5):797–801
Samandari T, Agizew TB, Nyirenda S, Tedla Z, Sibanda T, Shang N et al (2011) 6-month versus 36-month isoniazid preventive treatment for tuberculosis in adults with HIV infection in Botswana: a randomised, double-blind, placebo-controlled trial. Lancet 377(9777):1588–1598
Swaminathan S, Menon PA, Gopalan N, Perumal V, Santhanakrishnan RK, Ramachandran R et al (2012) Efficacy of a six-month versus a 36-month regimen for prevention of tuberculosis in HIV-infected persons in India: a randomized clinical trial. PLoS One 7(12):e47400
Martinson NA, Barnes GL, Moulton LH, Msandiwa R, Hausler H, Ram M et al (2011) New regimens to prevent tuberculosis in adults with HIV infection. N Engl J Med 365(1):11–20
Pho MT, Swaminathan S, Kumarasamy N, Losina E, Ponnuraja C, Uhler LM et al (2012) The cost-effectiveness of tuberculosis preventive therapy for HIV-infected individuals in southern India: a trial-based analysis. PLoS One 7(4):e36001
Gupta S, Abimbola T, Date A, Suthar AB, Bennett R, Sangrujee N et al (2014) Cost-effectiveness of the Three I's for HIV/TB and ART to prevent TB among people living with HIV. Int J Tuberc Lung Dis 18(10):1159–1165
Smith T, Samandari T, Abimbola T, Marston B, Sangrujee N (2015) Implementation and operational research: cost-effectiveness of antiretroviral therapy and isoniazid prophylaxis to reduce tuberculosis and death in people living With HIV in Botswana. J Acquir Immune Defic Syndr 70(3):e84–e93
World Health Organization (2009) Treatment of tuberculosis guidelines. In: 4th ed.
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A et al (2016) Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis 63(7):e147–ee95
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. Department of Health and Human Services. Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed April 8, 2019
Cohen K, van Cutsem G, Boulle A, McIlleron H, Goemaere E, Smith PJ et al (2008) Effect of rifampicin-based antitubercular therapy on nevirapine plasma concentrations in South African adults with HIV-associated tuberculosis. J Antimicrob Chemother 61(2):389–393
van Oosterhout JJ, Kumwenda JJ, Beadsworth M, Mateyu G, Longwe T, Burger DM et al (2007) Nevirapine-based antiretroviral therapy started early in the course of tuberculosis treatment in adult Malawians. Antivir Ther 12(4):515–521
Boulle A, Van Cutsem G, Cohen K, Hilderbrand K, Mathee S, Abrahams M et al (2008) Outcomes of nevirapine- and efavirenz-based antiretroviral therapy when coadministered with rifampicin-based antitubercular therapy. JAMA 300(5):530–539
Avihingsanon A, Manosuthi W, Kantipong P, Chuchotaworn C, Moolphate S, Sakornjun W et al (2008) Pharmacokinetics and 48-week efficacy of nevirapine: 400 mg versus 600 mg per day in HIV-tuberculosis coinfection receiving rifampicin. Antivir Ther 13(4):529–536
Swaminathan S, Padmapriyadarsini C, Venkatesan P, Narendran G, Ramesh Kumar S, Iliayas S et al (2011) Efficacy and safety of once-daily nevirapine- or efavirenz-based antiretroviral therapy in HIV-associated tuberculosis: a randomized clinical trial. Clin Infect Dis 53(7):716–724
Bonnet M, Bhatt N, Baudin E, Silva C, Michon C, Taburet AM et al (2013) Nevirapine versus efavirenz for patients co-infected with HIV and tuberculosis: a randomised non-inferiority trial. Lancet Infect Dis 13(4):303–312
Grinsztejn B, De Castro N, Arnold V, Veloso VG, Morgado M, Pilotto JH et al (2014) Raltegravir for the treatment of patients co-infected with HIV and tuberculosis (ANRS 12 180 Reflate TB): a multicentre, phase 2, non-comparative, open-label, randomised trial. Lancet Infect Dis 14(6):459–467
Taburet AM, Sauvageon H, Grinsztejn B, Assuied A, Veloso V, Pilotto JH et al (2015) Pharmacokinetics of raltegravir in HIV-infected patients on rifampicin-based antitubercular therapy. Clin Infect Dis 61(8):1328–1335
Wenning LA, Hanley WD, Brainard DM, Petry AS, Ghosh K, Jin B et al (2009) Effect of rifampin, a potent inducer of drug-metabolizing enzymes, on the pharmacokinetics of raltegravir. Antimicrob Agents Chemother 53(7):2852–2856
Dooley KE, Sayre P, Borland J, Purdy E, Chen S, Song I et al (2013) Safety, tolerability, and pharmacokinetics of the HIV integrase inhibitor dolutegravir given twice daily with rifampin or once daily with rifabutin: results of a phase 1 study among healthy subjects. J Acquir Immune Defic Syndr 62(1):21–27
Dooley KE, Kaplan R, Mwelase N, Grinsztejn B, Ticona E, Lacerda M et al (2019) Dolutegravir-based antiretroviral therapy for patients co-infected with tuberculosis and HIV: a multicenter, noncomparative, open-label, randomized trial. In: Clin Infect Dis
Loeliger A, Suthar AB, Ripin D, Glaziou P, O'Brien M, Renaud-Thery F et al (2012) Protease inhibitor-containing antiretroviral treatment and tuberculosis: can rifabutin fill the breach? Int J Tuberc Lung Dis 16(1):6–15
Matteelli A, Olliaro P, Signorini L, Cadeo G, Scalzini A, Bonazzi L et al (1999) Tolerability of twice-weekly rifabutin-isoniazid combinations versus daily isoniazid for latent tuberculosis in HIV-infected subjects: a pilot study. Int J Tuberc Lung Dis 3(11):1043–1046
Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E et al (2011) Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med 365(23):2155–2166
Podany AT, Bao Y, Swindells S, Chaisson RE, Andersen JW, Mwelase T et al (2015) Efavirenz pharmacokinetics and pharmacodynamics in HIV-infected persons receiving rifapentine and isoniazid for tuberculosis prevention. Clin Infect Dis 61(8):1322–1327
Weiner M, Egelund EF, Engle M, Kiser M, Prihoda TJ, Gelfond JA et al (2014) Pharmacokinetic interaction of rifapentine and raltegravir in healthy volunteers. J Antimicrob Chemother 69(4):1079–1085
Belknap R, Holland D, Feng PJ, Millet JP, Cayla JA, Martinson NA et al (2017) Self-administered versus directly observed once-weekly isoniazid and rifapentine treatment of latent tuberculosis infection: a randomized trial. Ann Intern Med 167(10):689–697
Johnson KT, Churchyard GJ, Sohn H, Dowdy DW (2018) Cost-effectiveness of preventive therapy for tuberculosis with isoniazid and rifapentine versus isoniazid alone in high-burden settings. Clin Infect Dis 67(7):1072–1078
Shepardson D, Marks SM, Chesson H, Kerrigan A, Holland DP, Scott N et al (2013) Cost-effectiveness of a 12-dose regimen for treating latent tuberculous infection in the United States. Int J Tuberc Lung Dis 17(12):1531–1537
Shepardson D, MacKenzie WR (2014) Update on cost-effectiveness of a 12-dose regimen for latent tuberculous infection at new rifapentine prices. Int J Tuberc Lung Dis 18(6):751
Swindells S, Rramchandani R, Gupta A, Benson CA, Leon-Cruz JT, Mwelase N et al (2019) One month of rifapentine plus isoniazid to prevent HIV-related tuberculosis. N Engl J Med 380(11):1001–1011
Organization WH. Report of the WHO Expert Committee, 2015 (including the 19th WHO Model List of Essential Medicines and the 5th WHO Model List of Essential Medicines for Children)
Suthar AB, Lawn SD, del Amo J, Getahun H, Dye C, Sculier D et al (2012) Antiretroviral therapy for prevention of tuberculosis in adults with HIV: a systematic review and meta-analysis. PLoS Med 9(7):e1001270
TEMPRANO ANRS 12136 Study Group (2015) Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med 373(9):808–822
Badje A, Moh R, Gabillard D, Guehi C, Kabran M, Ntakpe JB et al (2017) Effect of isoniazid preventive therapy on risk of death in west African, HIV-infected adults with high CD4 cell counts: long-term follow-up of the Temprano ANRS 12136 trial. Lancet Glob Health 5(11):e1080–e10e9
Acknowledgements
No additional assistance outside the efforts of the authors was contributed for this article. Sources of funding include the National Institutes of Health (P30 AI110527). Both authors report no conflicts of interest with respect to this work.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pettit, A.C., Sterling, T.R. (2019). Recent Advances in the Treatment of Latent Tuberculosis Infection Among Adults Living with HIV Infection. In: Sereti, I., Bisson, G.P., Meintjes, G. (eds) HIV and Tuberculosis. Springer, Cham. https://doi.org/10.1007/978-3-030-29108-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-29108-2_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29107-5
Online ISBN: 978-3-030-29108-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)