Abstract
Nodal Malignant Lymphoma (with Comments on Extranodal Malignant Lymphoma and Metastatic Cancer): this chapter outlines the incidence, risk factors, clinical presentation, investigations, treatments and prognosis of cancer relating to lymph nodes. These features are correlated with the core data that are required to make corresponding histopathology reports of a consistently high quality, available in an appropriate timeframe, and clinically relevant to patient management and prognosis. Summary details of the common cancers given at this site include: gross description, histological types, tumour grade/differentiation, extent of local tumour spread, lymphovascular involvement, and the status of excision margins. Current WHO Classifications of Malignant Tumours and relevant staging are referenced. Notes are provided on other associated pathology, contemporary use of immunohistochemistry, updates on the role of evolving molecular tests, and the use of these ancillary techniques as biomarkers in diagnosis, and prediction of prognosis and treatment response.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
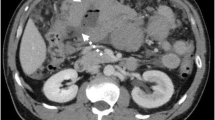
Representing 5–7% of all cancers and 55% of haematological malignancies with an increasing incidence , malignant lymphoma presents as persistent, mobile, rubbery and non-tender lymphadenopathy with or without associated systemic symptoms such as weight loss, itch or night sweats. Investigation is by full blood picture (infections/leukaemias), serology (infections/autoimmune diseases), fine needle aspiration cytology (FNAC: to exclude metastatic cancer) and biopsy. Clinical staging is by CT/PET/MRI scans appropriate to the clinical context, bone marrow aspirate and trephine biopsy.
In the UK contemporary guidance from the Royal College of Pathologists and the NHS National Cancer Action Team indicates concordance of diagnosis for malignant lymphomas of less than 85%. It is advised that diagnosis should be in accordance with the WHO 2016 classification of haematopoietic neoplasms and within the remit of a specialist integrated haematological malignancy diagnostic service covering a catchment population of at least two million. There should be a single integrated report encompassing the requisite specialist morphological expertise, immunohistochemistry, flow cytometry, cytogenetics, in situ hybridization and molecular diagnostics. Local arrangements will require at least prompt referral through the cancer network to the appropriate haematological malignancy diagnostic team. Underpinning this will be the ongoing need for general diagnostic pathologists to competently recognize the wide range of haematolymphoid pathology so that relevant and expeditious clinicopathological referrals are made.
Gross Description and Morphological Recognition
Specimen
-
FNAC/needle biopsy core/excisional biopsy/regional lymphadenectomy.
-
Regional lymphadenectomy comprises part of a formal cancer resection operation. This can either be for removal of a primary malignant lymphoma, e.g. gastrectomy, or, where malignant lymphoma is found incidentally in a resection for a primary carcinoma, e.g. in the mesorectal nodes of an anterior resection for rectal cancer.
-
Size (mm) and weight (g)
-
Colour, consistency, necrosis.
The preferred specimen for diagnosis, subtyping and grading of nodal malignant lymphoma is an excisional lymph node biopsy carefully taken by an experienced surgeon to ensure representation of disease and avoidance of traumatic artifact. Submission of the specimen fresh to the laboratory allows material to be collected for flow cytometry, cytogenetics, and imprints to be made, to which a wide panel of immunohistochemical antibodies or FISH probes can be applied some of which are more effective than on formalin fixed paraffin processed tissue sections. E.g. the demonstration of light chain restriction. Tissue can also be harvested for molecular and genetic techniques. Triaging of FNA and core biopsy samples for morphology, and ancillary studies is helped by rapid on site evaluation of the specimen (ROSE) . Needle core samples should be blocked in individual cassettes and spare serial sections requested to allow selective panels of immunohistochemistry or FISH to be performed. Knowledge of the broad diagnostic categories of haematological diseases is helpful in maximizing information from small samples. Morphological classification is generally based on well fixed, thin slices, processed through to paraffin with high quality 4 μm H&E sections. Core biopsy may be the only option if the patient is unwell or the lesion is relatively inaccessible, e.g. mediastinal or para-aortic lymphadenopathy. Allowances must be made in interpretation for underestimation of nuclear size, sampling error and artifact. Confirmation of lymphomatous (or other) malignancy is the prime objective and further comments on subtyping and grading given with care and only if definitely demonstrable. Despite these considerations a positive diagnosis can be given in a significant percentage of cases. Importantly, interpretation should be in light of the clinical context, i.e. the presence of palpable or radiologically proven significant regional or systemic lymphadenopathy, and the absence of any obvious carcinoma primary site. Tumour heterogeneity must also be borne in mind. The same principles apply to FNAC, which is excellent at excluding inflammatory lymphadenopathy, e.g. abscess or sarcoidosis, and non-lymphomatous cancer (e.g. metastatic squamous cell carcinoma, breast carcinoma or malignant melanoma). It is also reasonably robust at designating Hodgkin’s and high-grade non-Hodgkin’s malignant lymphoma. Morphology is the starting point and principal diagnostic criterion when assessing excisional lymph node biopsies, core biopsies and FNAC but is supplemented by immunohistochemical antibody panels targeted at the various diagnostic options, e.g. a small lymphoid cell proliferation (lymphocytic lymphoma versus mantle cell lymphoma etc.). In addition, flow cytometry and molecular tests including PCR for gene rearrangements, FISH for chromosomal abnormalities and mutation tests (single/multiplex or next generation sequencing) can be important in determining a diagnosis and its attendant treatment and prognosis. Limited needle sampling techniques can also be used in patients with a previous biopsy proven tissue diagnosis of malignant lymphoma and in whom recurrence is suspected. However, possible transformation of grade must be considered and even change of malignant lymphoma type, e.g. small lymphocytic lymphoma to Hodgkin’s malignant lymphoma, or Richter‘s transformation to diffuse large B cell malignant lymphoma. A range of inflammatory and neoplastic lymph node pathology may also be encountered secondary to chemotherapy and immunosuppression, e.g. tuberculosis, EBV (Epstein Barr Virus) driven lymphoproliferation, and various malignant lymphomas.
A systematic approach to excisional lymph node biopsies will allow the majority to be categorised as specific inflammatory pathology, benign or malignant, and the latter as haematolymphoid or non-haematolymphoid in character. Diagnostic morphological clues to malignant lymphoma are architectural and cytological.
Architectural descriptors are: diffuse, follicular, nodular, marginal zone, sinusoidal, paracortical, and angiocentric/angioinvasive distributions.
Cytological descriptors are: cell size (small, medium (the size of a histiocyte nucleus), large), the relative proportions of the cell populations, specific cytomorphological features, and cellular proliferative activity (mitoses, apoptosis, Ki-67 index). Various malignant lymphomas are also characterized by a typical host connective tissue and/or cellular inflammatory response.
Low Power Magnification
-
Capsular/extracapsular spillage of lymphoid tissue
-
Capsular thickening and banded septal fibrosis or hyaline sclerosis
-
Loss of sinusoids with either compression or filling due to a cellular infiltrate (preservation of sinuses is occasionally seen)
-
Alteration in follicular architecture with changes in
-
Distribution: proliferation in the medulla
-
Size and shape: relative uniformity of appearance
-
Definition: loss of the mantle zone- germinal centre interface/“filling up” of the germinal centre/loss of tingible body macrophages
-
Absence: the architecture may be completely effaced by a diffuse infiltrate
-
-
Prominent post capillary venules.
High Power Magnification
-
Presence of a background polymorphous inflammatory cellular infiltrate, e.g. eosinophils, plasma cells and histiocytes (epithelioid in character ± granulomas)
-
Alterations in the proportions of the normal cellular constituents
-
Dominance of any mono- or dual cell populations
-
Presence of atypical lymphoid cells
-
Nuclei: enlargement/irregularity/hyperchromasia/bi- or polylobation/mummification/apoptosis
-
Nucleoli: single/multiple/central/peripheral/eosinophilic/basophilic/Dutcher inclusions
-
Cytoplasm: clear/vacuolar/eosinophilic/scant/plentiful/paranuclear hof.
-
A morphological diagnostic short list should be created, e.g. mixed cellularity Hodgkin’s lymphoma versus T cell malignant lymphoma versus T cell rich large B cell malignant lymphoma, and a targeted immunohistochemical antibody panel used. The determination of cell lineage is a prerequisite for diagnosis. In the majority of cases immunohistochemistry will confirm the preliminary diagnosis, but will in a minority lead to its modification and either a refinement within or revision of diagnostic category. A pitfall for the unwary is aberrant expression of T cell antigens by a B cell malignant lymphoma and vice versa, e.g. expression of CD5 in small lymphocytic lymphoma/ chronic lymphocytic leukaemia. Clonality and gene rearrangement studies, either by immunohistochemistry, flow cytometry or molecular techniques can be important in confirming the neoplastic character of the B and T cell populations. Another relevant ancillary technique in various clinical settings is in situ hybridization for EBERs (Epstein Barr virus Encoded RNAs). Patient age, disease site and distribution also contribute to making a correct diagnosis, e.g. nodular lymphocyte predominant Hodgkin lymphoma usually presents in younger patients and as solitary or localized lymphadenopathy rather than extensive disease.
Histological Type and Differentiation/Grade
Therapeutic and prognostic distinction is made between Hodgkin and non-Hodgkin malignant lymphomas (HL/NHLs), with a significant proportion of the former being reclassified as variants of the latter on the basis of improved immunophenotyping. Within classical Hodgkin malignant lymphoma there are several subtypes from nodular sclerosis and lymphocyte rich through mixed cellularity to lymphocyte depleted, with nodular sclerosis divided into two subtypes that are of prognostic significance in limited stage disease. In non-Hodgkin lymphoma , indolent tumours often have a follicular pattern and are composed of small cells while aggressive lesions are usually diffuse with proliferation of medium to large cells or blasts. The morphological spectrum can predict the likelihood of untreated disease progression from indolence to aggressive behaviour, but paradoxically often does not correlate with extent of disease stage, chemoresponsiveness, long term disease free survival and potential for cure. For example, grade 1/2 follicular lymphoma is often of extensive distribution (stage IV), indolent in behaviour, yet incurable and ultimately fatal at 5–10 years after diagnosis. Morphology and immunophenotyping can identify most low and high-grade lymphomas, e.g. mantle cell lymphoma, mediastinal large B cell lymphoma and lymphoblastic lymphoma. In recent years, cell of origin as identified by immunohistochemistry or gene expression profiling and elucidation of the genetic and mutational landscape of lymphomas has led to upfront molecular testing for accurate diagnosis, treatment and prognosis.
Non-Hodgkin’s Malignant Lymphoma
Non-Hodgkin’s malignant lymphoma (NHL) is classified according to the WHO 2016 system (Table 35.1) which defines each disease by its morphology, immunophenotype, genetic characteristics, proposed normal counterpart and clinical features. It is reproducible, with prognostic and therapeutic implications. Broad categories are malignant lymphomas of B, T or NK (natural killer) cell types. Malignant lymphomas and leukaemias are both included as many haematolymphoid neoplasms have both solid and fluid circulatory phases. Prognosis relates to stage of disease, treatment protocols and individual disease biology.
Hodgkin’s Malignant Lymphoma
WHO Classification
Comprising nodular lymphocyte predominant Hodgkin lymphoma (NLPHL—a B cell lymphoma), and classic Hodgkin lymphomas encompassing nodular sclerosis, lymphocyte rich, mixed cellularity and lymphocyte depleted variants. Hodgkin lymphoma is a tumour of abnormal B-cell lineage.
Lymphocyte and Histiocyte (L and H) Predominant: Multilobated “Popcorn” Cell
-
Nodular:a B cell lymphoma of early stage (cervical, axilla, groin), predominantly in young men and low-grade indolent behaviour (80% 10 year survival) with a 4% risk of diffuse large B cell change. Some association with progressive transformation of germinal centres.
-
Diffuse: a controversial category with overlap between lymphocyte rich classic Hodgkin lymphoma, vaguely nodular lymphocyte predominant Hodgkin, and exclusion of other entities such as T cell/histiocyte rich large B cell NHL.
Overlap of nodular and diffuse patterns exists; diffuseness is a poor prognostic feature.
Classic Hodgkin lymphoma includes nodular sclerosis, lymphocyte rich, mixed cellularity and lymphocyte depleted categories. They vary in their clinical features, growth pattern, degree of fibrosis, background cells, tumour cell numbers and atypia, and, frequency of EBV infection.
Nodular Sclerosis: Lacunar Cell
-
Female adolescents, young adult preponderance. Mediastinal or cervical involvement and either localised disease or high stage at presentation. Moderately aggressive but curable.
-
Birefringent fibrous bands (capsular and intranodal septa) with mixed inflammatory cell nodules containing lacunar cells, or, cellular phase (rich in lacunar cells, scant fibrosis)
-
∗Type 1.
-
∗Type 2: lymphocyte depletion or pleomorphism of R-S (Reed Sternberg ) cells in more than 25% of nodules. An alternative descriptor is syncytial variant (sheets/clusters of R-S cells with central necrosis and a polymorph infiltrate).
-
∗Grade 1/grade 2 British National Lymphoma Investigation (BNLI). These types and grades are not prognostically relevant or independent of stage.
-
Mixed Cellularity: Reed Sternberg Cell
-
Male adults, high stage disease at presentation: lymph nodes, spleen, liver ± bone marrow. Moderately aggressive but curable.
-
R-S cells of classic type in a mixed inflammatory background. A category of exclusion in that no specific features of other subtypes are present.
Lymphocyte Rich Classic
-
Scattered R-S cells against a nodular or diffuse background of small lymphocytes but no polymorphs. Reactive lymphoid follicles are present.
Lymphocyte Depleted
-
Older patients , high stage disease at presentation, aggressive, association with HIV.
-
R-S cells ± pleomorphism; diffuse fibrosis (fibroblasts obscure scattered R-S cells) and reticular variants (cellular, pleomorphic R-S cells).
Other Features
-
Follicular and interfollicular Hodgkin cell with a high epithelioid cell content (granulomas).
-
R-S cells: classic mirror image, binucleated cell with prominent, inclusion -like eosinophilic nucleolus (“owl’s eye” appearance) characteristic of the mixed cellularity and lymphocyte depleted categories. Mononuclear, polylobated and necrobiotic (mummified) forms are also common. Lacunar cells (nodular sclerosis) can be mono-, bi- or polylobated (± necrobiotic), with characteristic perinuclear artifactual cytoplasmic retraction and clarity. Mononuclear cells tend to be termed Hodgkin cells. Hodgkin/R-S cells are derived from germinal centre B cells with monoclonal, non-functional immunoglobulin gene rearrangements.
Immunophenotype
Nodular lymphocyte predominant Hodgkin lymphoma
-
Popcorn cells: CD45/CD20/CD79a/EMA/J chain/bcl-6 positive, CD30 weak or negative, CD15 negative, EBV negative. Nuclear transcription factors Oct2/BoB1 positive.
-
Small lymphocytes: nodules of B cells (CD20) and intervening T cells (CD3).
-
Rosettes: CD57/CD4 positive T cell rosettes around the popcorn cells.
Classic Hodgkin lymphoma
-
R-S cells: CD15/CD30 positive in 75%/90% of cases respectively, EBV (variable-10–70% 60–70% of cases), CD20/79a ±, CD45/ALK negative. MUM1/PAX5 positive. CD15 positivity can be weak and focal, limited to the Golgi apparatus in 15% of cases.
-
Small lymphocytes: T cells (CD3/CD4).
In Hodgkin lymphoma the heterogeneous cellular background (comprising 90% of the tissue) is an important part of the diagnosis: small lymphocytes, eosinophils, neutrophils, fibroblasts, histiocytes and follicular dendritic cells. Note that this cytokinetic diathesis is also seen in T cell NHLs and T cell rich B cell NHLs. Another differential diagnosis with which there can be overlap is anaplastic large cell lymphoma. Other features are progressive transformation of germinal centres (particularly associated with NLPHL), granulomas, necrosis, interfollicular plasma cells and reactive follicular hyperplasia, all of which should prompt a careful search for R-S cells.
Differential Diagnoses in Haematolymphoid Pathology
Relatively common diagnostic difficulties in lymph node assessment are:
-
Follicular hyperplasia vs. follicular lymphoma
-
Follicular hyperplasia vs. partial nodal involvement by in situ follicular lymphoma
-
Progressive transformation of germinal centres vs. NLPHL
-
T cell hyperplasia vs. dermatopathic lymphadenopathy vs. T cell lymphoma
-
Histological underestimation of aggressiveness in small lymphoid cell infiltrates, e.g. mantle cell or lymphoblastic lymphomas
-
Burkitt lymphoma vs. Burkitt-like diffuse large B cell lymphoma
-
Hodgkin lymphoma vs. anaplastic large cell lymphoma, and subtle infiltration of sinusoids by the latter
-
Interfollicular Hodgkin lymphoma
-
Anaplastic large cell lymphoma vs. metastatic carcinoma, malignant melanoma or germ cell tumour
-
Post immunosuppression lymphoproliferative disorders.
Important non-malignant differential diagnoses for malignant lymphoma are Castleman’s disease (hyaline vascular and plasma cell variants), drug induced (e.g. phenytoin) and viral reactive hyperplasia with paracortical transformation (e.g. herpesvirus, infectious mononucleosis), and necrotising and granulomatous lymphadenitis (Kikuchi’s, toxoplasmosis, tuberculosis, sarcoidosis). A clinical history of immunosuppression in EBV driven lymphoid proliferations must always be borne in mind.
Extent of Local Tumour Spread
Part of node or whole node.
Extracapsular into adjacent soft tissues or organ parenchyma.
A TNM classification is not used as the primary site of origin is often uncertain and attribution of N and M stages would therefore be arbitrary.
Staging often requires extensive imaging including CT/PET scan as well as bone marrow examination.
Stage: Modified Ann Arbor system |
I Single lymph node region or localised extralymphatic site/organ |
II Two or more lymph node regions on same side of the diaphragm or single localised extralymphatic site/organ and its regional lymph nodes ± other lymph node regions on the same side of the diaphragm |
III Lymph node regions on both sides of the diaphragm ± a localised extralymphatic site/organ or spleen |
IV Disseminated (multifocal) involvement of one or more extralymphatic organs ± regional lymph node involvement, or single extralymphatic organ and non-regional nodes. Includes any involvement of liver, bone marrow, lungs or cerebrospinal fluid |
A without weight loss/fever/sweats |
B with weight loss/fever/sweats: |
Fever >38 °C |
Night sweats |
Weight loss >10% of body weight within the previous 6 months. |
Subscripts e.g. IIIE denotes stage III with Extranodal disease |
IIIS denotes stage III with splenic involvement |
III3 denotes stage III with involvement of 3 lymph node regions: > 2 is prognostically adverse. |
Lymph node regions: head, neck, face |
Intrathoracic |
Intraabdominal |
Axilla/arm |
Groin/leg |
Pelvis |
Other major structures of the lymphatic system are the spleen, thymus, Waldeyer’s ring (palatine, lingual and pharyngeal tonsils), vermiform appendix and ileal Peyer’s patches. Bone marrow, skin, liver, lung, pleura and gonads are sites with relatively low volumes of lymphoid tissue.
Bilateral involvement of axilla/arm or inguinal/leg regions is considered as involvement of two separate regions.
Direct spread of lymphoma into adjacent tissues or organs does not alter the classification, e.g. gastric lymphoma into pancreas and with involved perigastric lymph nodes is stage IIE.
Involvement of two or more discontinuous segments of gastrointestinal tract is multifocal and classified as stage IV, e.g. stomach and ileum. However multifocal involvement of a single extralymphatic organ is IE.
Involvement of both organs of a paired site, e.g. lungs is also IE. Regional nodes for an extranodal lymphoma are those relevant to that particular site, e.g. gastric lymphoma—perigastric, left gastric, common hepatic, splenic and coeliac nodes (Figs. 35.1, 35.2, 35.3, 35.4, and 35.5).
Staging laparotomy has been replaced by assessment of clinical and radiological parameters, e.g. peripheral blood differential cell counts, clinical chemistry including LDH, and imaging for hepatosplenomegaly, involved lymph node sites and other organ involvement. Bone marrow biopsy remains part of normal staging. Bone marrow involvement in Hodgkin lymphoma is characterized by the presence of Hodgkin cells in a typical fibroinflammatory stroma; nodular lymphoid aggregates or granulomas per se are not sufficient for a positive diagnosis of Hodgkin lymphoma. Bone marrow involvement by NHL can be diffuse, nodular or focal, and paratrabecular infiltration is a characteristic site of distribution.
Lymphovascular Invasion
Vessel wall invasion and destructive angiocentricity can be a useful indicator of malignancy in NHL and in specific subtypes, e.g. nasal angiocentric T/NK cell lymphoma.
Immunophenotype
In general an antibody panel is used with both expected positive and negative antibodies , and, two antibodies per lineage. Select combinations are targeted at determining the nature of the various lymphoid proliferations, e.g. follicular (follicular lymphoma vs. reactive hyperplasia), small cell (CLL/SLL vs. mantle cell lymphoma), and large cell (HL vs. NHL vs. ALCL). Interpretation must take into account artifacts such as poor fixation or lymph node necrosis following FNAC. In the latter, expression of nuclear antigens is affected first and T cell stains can give false positive results in inflammatory debris. Some antigens such as CD20 retain remarkably robust expression. Expression must also be appropriate to the antibody concerned, e.g. localization to the nucleus, cytoplasm or cell membrane. Suitable in built positive, and, external positive and negative controls are used. Interpretation must also account for expression in physiological cell populations in the test tissue. High quality thin sections are required to aid visualisation and interpretation of applied antibodies. Commonly used antibodies available for formalin fixed, paraffin embedded sections are:
CD45 | Pan lymphoid marker (Leucocyte Common Antigen) and excellent in the characterisation of a poorly differentiated malignant tumour, e.g. malignant lymphoma vs. carcinoma vs. malignant melanoma. |
CD20 | Mature B cell marker (and some cases of plasma cell myeloma).Lymphoma cell positivity is a marker for specific anti-CD20 immunotherapy. |
CD79a | As for CD20 but also less mature (pre B: lymphoblastic) cells and plasma cell tumours. |
CD3 | Pan T cell marker. |
CD5 | T cell marker and aberrant consistent expression in some B cell lymphoma (small lymphocytic, mantle cell lymphomas). |
CD4, CD8: | T cell subsets of use in some T cell proliferations e.g. mycosis fungoides. Other T cell markers include CD45R0 (UCHL1), CD43 (MT1), CD2, CD7, CD28, CD57 and TIA-1. |
CD10 | Lymphoblastic lymphoma (CALLA), Burkitt lymphoma and follicular lymphoma. Also with CD5 and CD23 in the diagnosis of small B cell lymphomas (lymphocytic CD5/CD23+: mantle cell CD5+: follicle centre cell CD10+). 40-50% of DLBCL are CD10 positive and referred to as germinal centre phenotype. |
CD15, CD30 | Classic Hodgkin lymphoma R-S cells. CD30 is also positive in ALCL, a proportion of DLBCLs, embryonal carcinoma and malignant melanoma. CD15 is positive in some large T cell lymphomas. |
CD56, CD57 | Natural killer (NK) cells e.g. angiocentric sinonasal lymphoma. Also T cells and plasma cell myeloma/AML (CD56). |
CD68 | Macrophages, cells of granulocytic lineage. |
CD 38/138 | Plasma cells and multiple myeloma (usually CD45/20 negative; CD79a±). Other low grade B cell lymphomas (CD38+ CLL has a worse prognosis). |
CD123 | Hairy cell leukaemia, AML. |
κ, λ light chains | Immunoglobulin light chain restriction is difficult to demonstrate satisfactorily in paraffin sections but more easily shown on fresh imprint preparations or by in situ hybridisation. |
CD21, CD23 | Follicular dendritic cells. CD23 also stains most B cell lymphocytic lymphomas, some follicular and DLBCLs. |
bcl-1/cyclin D1 | Mantle cell lymphoma with the t(11:14) translocation. A nuclear epitope. Also variably positive in hairy cell leukaemia and plasma cell myeloma cases. p27kip1 is positive in cyclin D1 negative mantle cell lymphoma. |
bcl-2 | An apoptosis regulator: positive in many B cell lymphomas, strongly expressed in 80–85% follicular lymphoma. Also normal B, T cells and negative in reactive germinal centres. Strong expression is adverse in DLBCLs. |
bcl-6 | Follicular lymphoma, Burkitt lymphoma and a large proportion of DLBCLs. A transcription factor in the nuclei of germinal centre cells. |
Ki-67/MIB-1 | Nuclear proliferation marker useful for identifying high-grade lymphomas e.g. Burkitt (98–100%), lymphoblastic lymphoma (also TdT positive), and DLBCL with a high proliferation fraction. Its distribution in the germinal centre is helpful in distinguishing reactive lymphoid hyperplasia (shows polarity with staining in the dark zone) from follicular lymphoma (lower level of staining than reactive hyperplasia and lacks polarity). |
EBV | LMP-1 (latent membrane protein) antibody is positive in a proportion of R-S cells in HL. In situ hybridisation is more sensitive with a higher rate (60–70%) of positivity. |
TdT | Terminal deoxynucleotidyltransferase is positive in precursor B and T cell lymphoblastic lymphomas. A nuclear epitope. |
CD1a | Langerhans cell histiocytosis, cortical thymic T cells. |
ALK-1/ (CD246) | Nucleophosmin-anaplastic lymphoma kinase fusion protein associated with the ALK-1 gene t(2:5) translocation and good prognosis ALCLs. |
C-MYC | Identifies an aggressive subset of DLBCLs that are less responsive to usual chemotherapy agents. |
MUM1 | A nuclear proliferation/differentiation epitope positive in post germinal centre B cells. It is of prognostic value in DLBCLs and stains classic R-S cells. |
PAX5 | A nuclear B-cell transcription factor expressed in B lymphoctyes and weakly in R-S cells; absent in plasma cells. |
Oct2/BoB1 | B cell transcription factors positive in the nuclei of NLPHL L and H popcorn cells. Also in DLBCL. |
EMA | Plasma cells, ALCL, NLPHL L and H cells. |
Lysozyme | (muramidase/myeloperoxidase)—granulocytic and myeloid cell lineages. AML: also CD34, CD43, CD68, CD117, neutrophil elastase and chloroacetate esterase. |
p53 | A prognostic marker in various lymphoid neoplasms and MDS/AML. |
p21 | A prognostic marker in multiple myeloma. |
PD1, CXCL13, ICOS & bcl6 | Valuable in identification of follicular T-cell helper cells |
S100 | Interdigitating reticulum cells, Langerhans cells. |
Factor VIII/ CD61 | Markers of megakaryocytes. |
Molecular Techniques
Immunoglobulin receptor (heavy and light chain restriction) and T cell receptor (TCR) gene rearrangements using polymerase chain reaction are of use in difficult diagnostic cases, e.g. follicular hyperplasia vs. follicular lymphoma, or T zone reactive hyperplasia vs. malignant lymphoma. Also, where immunohistochemistry has been equivocal (e.g. dubious cyclin D1 staining in mantle cell lymphoma) chromosomal studies for specific translocations have a role to play. These techniques vary in their applicability to fresh tissue and routine paraffin sections and suitable arrangements for prompt tissue transportation and referral on a regional network basis should be put in place. A majority of malignant lymphomas can be provisionally diagnosed without these techniques but their role is rapidly evolving in importance with respect to diagnostic confirmation, prognostication and therapy.
The evolution of new generation robust antibodies applicable to paraffin sections with unmasking of antigenic sites by antigen retrieval methods and more sensitive visualization techniques has led to considerable reclassification of malignant lymphomas and emergence of new entities. The full spectrum of NHL widens viz. T cell NHL, anaplastic large cell NHL, T cell rich B cell lymphoma (<10% CD20 positive large cells on a background of CD3 small lymphocytes). Unusually composite (HL/NHL) and gray zone (HL/DLBCL and HL/ALCL) cases also occur. It is important that a panel of antibodies is used and markers assessed in combination. The WHO 2016 classification includes several established lymphomas (e.g. lymphoplasmacytic lymphoma) and provisional entities such as Burkitt-like lymphoma with 11q aberration in which the molecular abnormality is a disease defining characteristic feature. There is an explicit recognition of the need to incorporate genetic findings in diagnosis and management of diffuse large B-cell lymphoma. Thus morphology and immunohistochemistry are routinely supplemented by molecular studies such as FISH, clonality assessment and mutation tests. Gene expression profiling and next generation sequencing (NGS) are currently restricted to large tertiary referral centres. Molecular test results need careful correlation with morphology and immunophenotype. Clonality does not always correlate with malignant lymphoma; it has been demonstrated in some inflammatory skin (e.g. eczema vs. mycosis fungoides), salivary and gastric biopsies. Pathogenic mutations and chromosomal abnormalities are sometimes found in normal people and in patients lacking firm clinical evidence of disease.
Formalin fixation and high quality, thin (2–4 μm) paraffin sections are adequate for morphological characterisation in most cases. Fixation should be sufficient (24–36 h) but not excessive as this may mask antigenic sites.
The majority (60–70%) of NHLs are diffuse large B cell lymphomas and follicular lymphoma.
Characteristic Lymphomas
Precursor B Cell Lymphoblastic Lymphoma/Leukaemia
-
Presents as childhood leukaemia or occasionally solid tumour (skin, bone, lymph node) and relapses in the central nervous system or testis.
-
75% survival in childhood but <50% in adults. Aggressive but potentially curable by multiagent chemotherapy.
-
Medium sized round, mitotically active lymphoid cells with small nucleolus.
-
CD79a, CD10, TdT, CD99±, Ki-67 > 95%, CD20±.
Small Lymphocytic Lymphoma/Chronic Lymphocytic Leukaemia (CLL)
-
5–10% of lymphomas occurring in older adults with diffuse lymph node, bone marrow and blood involvement, and hepatosplenomegaly.
-
Indolent and incurable with 5–10 year survival even without treatment but ultimately fatal.
-
Small lymphocytes with pale proliferation centres (para-immunoblasts/prolymphocytes)
-
CD45, CD20, CD5, CD23, LEF1, bcl-2, Ki-67 < 20%. Cyclin D1 and CD10 negative.
-
Richter’s transformation to large cell lymphoma in 3–5% of cases. Worse prognosis cases are CD38 positive.
-
occasional cases have Hodgkin like cells (CD30/15+) and < 1% develop classic HL.
Lymphoplasmacytic Lymphoma
-
1–2% of cases and in the elderly involving bone marrow, nodes and spleen. Indolent course with a median survival of 5–10 years.
-
Monoclonal IgM serum paraprotein with hyperviscosity symptoms and autoimmune/cryoglobulinemia phenomena.
-
Small lymphocytes, plasmacytoid cells and plasma cells.
-
Intranuclear Dutcher and cytoplasmic Russell bodies.
-
CD45, CD20, VS38 positive and CD5/CD10/CD23 negative.
-
MYD88 L265P mutation positive by PCR in more than 90% cases.
Marginal Zone Lymphoma of MALT (Mucosa Associated Lymphoid Tissue)
-
8% of NHLs, stomach 50% of cases, also salivary gland, lung, thyroid, orbit and skin. Multiple extranodal sites in 25–45% of cases. 80% are stage I or II disease and indolent. Many are cured by local excision, or antibiotic therapy in gastric MALToma .
-
Usually extranodal associated with chronic autoimmune or antigenic stimulation.
-
Centrocyte like cells, lymphocytes, plasma cells (scattered immunoblast and centroblast like cells).
-
Destructive lymphoepithelial lesions, reactive germinal centres and follicular colonisation by the lymphoma cells.
-
CD45, CD20 positive but CD5/10/23 negative.
-
Lymph node variant is monocytoid B cell lymphoma: indolent (60–80% 5 year survival) but has potential for large cell transformation.
-
Gastric MALT with t(11:18) confers resistance to anti-Helicobacter treatment.
-
Splenic marginal zone lymphoma: splenomegaly, lymphocytosis, stage III/IV disease.
Hairy Cell Leukaemia
-
Rare, elderly in the bone marrow, spleen and lymph nodes. Typically marked splenomegaly with pancytopaenia. 10 year survival >90%.
-
“fried egg” perinuclear cytoplasmic clarity with prominent cell boundaries.
-
CD45, CD20, CD72(DBA44), CD123, tartrate resistant acid phosphatase (TRAP) positive, cyclin D1 ± and BRAF.
-
BRAFV600E mutation positive.
Mantle Cell Lymphoma
-
6% of NHLs predominantly in older adult males (75%).
-
Extensive disease including spleen, bone marrow, Waldeyer’s ring ± bowel involvement (multiple lymphomatous polyposis).
-
Monomorphic small to medium sized irregular nuclei (centrocytic). Rare blastoid and pleomorphic variants.
-
Diffuse with vague architectural nodularity.
-
CD45, CD20, and typically CD5, cyclin D1, SOX11 and CD43 positive (t11;14 positive).
-
CD10, CD23, bcl-6 negative. Cyclin D1 negative (also t11;14 negative) cases can be p27kip1 positive; these are usually CD5 and SOX11 positive.
-
Aggressive with mean survival of 3–5 years. A high Ki-67 index (>30%) is prognostically adverse.
-
An indolent variant of mantle cell lymphoma is recognized; these patients have peripheral blood and bone marrow or spleen involvement with no evidence of lymphadenopathy. Some patients have overlapping features with conventional mantle cell lymphoma.
Follicular Lymphoma
-
30% of adult NHLs and transformation to DLBCL is relatively common.
-
Patterns: follicular, follicular and diffuse, diffuse (see Table 35.1)
-
Cell types: centroblasts with large open nuclei, multiple small peripheral basophilic nucleoli, variable cytoplasm; Centrocytes with medium sized irregular nuclei.
-
Grade: 1/2/3 according to the number of centroblasts per high power field (see Table 35.1). Grade 3 has a high Ki-67 and 50% may be bcl-2 negative—it is high-grade requiring immunochemotherapy and is to be distinguished from low-grade (grade 1/2) disease.
-
CD45, CD20, CD10 (60%), bcl-2 (t14:18; 70–95%), bcl-6.
-
Usually CD21/23 positive and CD5 negative (20% positive).
-
High stage disease at presentation (splenomegaly and bone marrow involvement in 40% of cases), and indolent time course, but late relapse (5–10 years) with large cell transformation in 25–35% of cases to DLBCL.
-
Pattern and grade can vary within a lymph node necessitating adequate sampling.
Diffuse Large B Cell Lymphoma (DLBCL)
-
30% of adult NHLs, 40% are extranodal (especially stomach, skin, central nervous system, bone, testis, etc.). Forms a rapidly growing mass in older patients which usually arises de-novo, or, occasionally from low-grade B cell NHL. Aggressive but potentially curable—immunochemotherapy has improved outlook considerably.
-
Centroblasts, immunoblasts (prominent central nucleolus), bi−/polylobated, cleaved, anaplastic large cell (ALK+), plasmablastic (HIV+) forms, basophilic cytoplasm.
-
Aggressive variants: T cell/histocyte rich, mediastinal/thymic, intravascular, primary effusion (chronic inflammation associated), primary central nervous system.
-
CD45, CD20, CD79a, Ki-67 40–90%, CD10 (30–60%), bcl-2 (30%), bcl-6 (60–90%), CD5/23/CD30/CD43 ±. MUM1(35–65%).
-
Strong bcl-2 expression is adverse.
-
Gene expression profiling (GEP) identifies two types: germinal centre (52%); non germinal centre (activate d B-cell phenotype and unclassifiable 48%). Immunohistochemistry is a surrogate and demonstrates up to 85% concordance with the classification based on GEP. Approximately 10% DLBCL demonstrate C-MYC gene rearrangement and poorer prognosis.
-
Hans algorithm : DLBCLs of germinal centre origin (CD10+, or, CD10−/bcl-6 +/MUM1-) are of better prognosis (76% 5 year survival) than those of non-germinal centre origin (CD10−/bcl-6- or, CD10−/bcl-6+/MUM1+: 34% 5 year survival). “Germinal centre markers ” include CD10, bcl-6, CD21 and CD23 while MUM-1 (Interferon Regulating Factor 4: IRF4) is expressed by post germinal centre destined B cells.
-
Strong and diffuse MYC protein overexpression correlates with MYC gene translocation.
-
Primary testicular and CNS DLBCL are usually of non germinal centre phenotype and often demonstrate MYD88 L265P mutations.
Burkitt Lymphoma
-
1–2.5% of NHLs.
-
Childhood or young adult: endemic/sporadic/HIV related (EBV: 95%/15–20%/30–40% of cases respectively).
-
Jaw and orbit (early childhood/endemic), or abdomen (ileocaecal/late childhood or ovaries/young adult/sporadic) and breasts with risk of central nervous system involvement.
-
Monomorphic, medium -sized lymphoid cells, multiple small central nucleoli, basophilic cytoplasm.
-
Mitoses, apoptosis, “starry-sky” pattern.
-
CD79a, CD20, CD10, bcl-6, Ki-67 98–100%, and bcl-2/TdT/CD5/23 negative.
-
t(8:14) and t(2:8)/t (8:22) variants by FISH in paraffin sections or karyotyping in fresh tissue.
-
Requires aggressive polychemotherapy and is potentially curable: 90% in low stage disease, 60–80% with advanced disease, children better than adults.
-
Burkitt like morphology and the C-MYC rearrangement are not specific to this lymphoma. Aggressive B-cell lymphoma with MYC rearrangement, transformed follicular lymphoma with MYC and bcl2 rearrangments (so called ‘double hit’ lymphoma, ‘triple hit’ if MYC, bcl6, and bcl2 rearrangements identified) and Burkitt-like lymphoma with 11q aberration require FISH and/or additional molecular testing for diagnosis.
Precursor T Lymphoblastic Lymphoma/Leukaemia
-
Expresses CD3, Ki-67 > 95%, TdT.
-
Presents in childhood/adolescence as leukaemia or a mediastinal mass (also lymph nodes, skin, liver, spleen, central nervous system, gonads).
-
Aggressive with 20–30% 5 year survival but potentially curable.
Angioimmunoblastic T Cell Lymphoma
-
Neoplasm of follicular T-helper cells and constitutes up to 25% of all T-NHL in adults.
-
Clinical features include fever, skin rash and generalized lymphadenopathy associated with laboratory abnormalities such as raised ESR, polyclonal hypergammaglobulinemia and anaemia.
-
Tumour cells are CD3, CD5 and CD7 positive with variable expression of follicular T-helper cell antigens such as CD4, CD10, CXCL13, ICOS and PD1.
-
Expanded extra-follicular dendritic meshwork, high endothelial venules and EBV positive B immunoblasts are other characteristic findings.
-
Clonal TCR rearrangement is present in the majority of cases. Expansion of the EBV positive B-cell population with clonal immunoglobulin receptor rearrangements may be seen in a subset of cases and result in a B-cell lymphoma.
-
Aggressive disease with median survival of 2 years.
Mycosis Fungoides
-
Cutaneous patch, plaque and tumour stages with or without lymph node involvement.
-
Indolent but stage related and can transform to high-grade NHL of large cell type.
-
Several biopsies over time may be required before diagnosis is made
-
Usually CD3, CD5, TCRαβ and CD4+/CD8−; loss of CD7 is common and large cell transformation is associated with CD30 positivity.
Sézary Syndrome
-
Defined by the triad of erythroderma, lymphadenopathy and peripheral blood involvement by clonally related neoplastic T cells with cerebriform nuclei (Sézary cells). Histologic features can be similar to mycosis fungoides. The tumour cells are typically PD-1 positive.
Subcutaneous Panniculitis Like T Cell Lymphoma
-
Nodules trunk/extremities, CD3, CD8, TCRαβ.
-
80% 5 year survival but sometimes haemophagocytic syndrome supervenes with poor prognosis.
Enteropathy Associated T Cell Lymphoma
-
Type 1—pleomorphic, small to medium or large and anaplastic cells
-
CD3 positive, associated gluten enteropathy or ulcerative jejunitis.
-
Aggressive and in adults presents with abdominal pain, mass, ulceration or perforation, or a change in responsiveness to a gluten free diet.
-
Type 2—monomorphic , CD8, CD56 and CD3 positive cells; not associated with celiac disease.
Hepatosplenic Gamma Delta T Cell Lymphoma
-
Male adolescents and young adults (some following immunosuppressive treatment for inflammatory bowel disease, transplant, etc.).
-
Aggressive and relapses despite treatment with survival <2 years.
-
Liver, spleen, bone marrow and lymph node sinus involvement.
-
CD3+, CD4/8−, γδ TCR, often CD56 positive.
Peripheral T Cell Lymphoma, Unspecified
-
10% of NHLs and 30% of T cell NHLs. Diagnosed if cases are not classifiable as one of the previously described specific entities (i.e. Precursor T lymphoblastic lymphoma/leukaemia, Angioimmunoblastic T Cell Lymphoma, Mycosis Fungoides, Sézary syndrome, Subcutaneous Panniculitis Like T Cell Lymphoma, Enteropathy Associated T Cell Lymphoma, Hepatosplenic Gamma Delta T Cell Lymphoma).
-
Adults. Generalised lymph node or extranodal disease at presentation with involvement of skin, subcutaneous tissue, viscera and spleen. Aggressive with relapses and median survival of 2–3 years.
-
Interfollicular/paracortical or diffuse infiltrate.
-
Variable nuclear morphology from medium sized cells with minimal atypia to large blast-like pleomorphic cells, “crows-feet” appearance with irregular nuclear contours.
-
Cytoplasmic clearing.
-
Accompanying eosinophils, histiocytes and vascularity with prominent post capillary venules.
-
Lymphoepithelioid variant (Lennert lymphoma).
-
Usually CD3, CD4, CD5 and TCR gene rearrangement positive, variable expression of CD7/CD8/CD15/CD30/CD56/TIA-1.
-
Worse prognosis than B cell lymphomas.
Extranodal NK/T Cell Lymphoma, Nasal Type
-
Nasal type is the prototypic presentation. Also seen in any organ system including skin and soft tissues. Aggressive with 30–40% survival.
-
Polymorphic inflammatory infiltrate of granulocytes which may obscure the tumour cells.
-
Variably sized minimally atypical to markedly pleomorphic or blastic lymphoid cells.
-
Angiocentric and destructive.
-
Usually CD2, CD56, CD16, CD3 (cytoplasmic) and EBER-ISH positive, TCR germline, STAT3 and STAT5 mutations in 40% cases. Cytoplasmic but not surface CD3. Also ± CD57, perforin, granzyme B, TIA-1.
Anaplastic Large Cell Lymphoma (ALCL)
-
2.5% of NHLs in adults and 10–20% of childhood malignant lymphomas.
-
Elderly and young (25% < 20 years): ALK negative and ALK positive/male predominance.
-
May also follow mycosis fungoides, lymphomatous papulosis or HL.
-
Cohesive, sinusoidal growth pattern of “epithelioid” cells mimicking carcinoma, malignant melanoma and germ cell tumour.
-
Large pleomorphic nuclei, multiple nucleoli, polylobated forms, “hallmark cells” with horseshoe or reniform nucleus; rarely small cell variant.
-
CD30, and, EMA/CD45/CD3 ±, CD2+, CD4 more often positive than CD8.
-
Mainly T (60–70% TCR), and null (20–30%) cell types. 90% have clonal TCR rearrangements.
-
12–50% of adult cases are t(2:5) and ALK-1 positivity confers a good prognosis (80% 5 year survival) despite presentation with stage III/IV disease. ALK-1 negative cases have 40% 5 year survival.
-
Recently, breast implant associated ALCL has been described. This presents as a seroma a number of years following breast implant/reconstruction. The tumour cells are mostly confined to the seroma fluid and rarely penetrate the capsule, involve regional lymph nodes or spread to distant sites. Seroma cytology and imaging are critical for this diagnosis.
Granulocytic (Myeloid) Sarcoma
-
Myelomonocytic markers are CD68, myeloperoxidase, chloroactetate esterase, neutrophil elastase, lysozmye, CD15, CD34, CD43, CD117.
-
Megakaryocytic component: CD61, factor VIII.
-
If a tumour looks like a malignant lymphoma but does not show appropriate immunohistochemical marking, think of granulocytic (myeloid) sarcoma.
Extranodal Lymphoma
Of NHLs, 25–40% are extranodal, defined as when a NHL presents with the main bulk of disease at an extranodal site usually necessitating the direction of treatment primarily to that site. In order of decreasing frequency sites of occurrence are
-
Gastrointestinal tract (especially stomach then small intestine)
-
Skin
-
Waldeyer’s ring
-
Salivary gland
-
Thymus
-
Orbit
-
Thyroid
-
Lung
-
Testis
-
Breast
-
Bone
A majority are aggressive large B cell lymphomas although T cell lesions also occur (cutaneous T cell lymphoma, enteropathy associated T cell lymphoma, subcutaneous panniculitis like T cell lymphoma, NK/T cell nasal lymphoma). Their incidence is rising partly due to increased recognition and abandonment of terms such as pseudolymphoma, but also because of aetiological factors, e.g. HIV, immunosuppression after transplantation or chemotherapy, autoimmune diseases (e.g. systemic lupus erythematosis), and chronic infections (H. pylorii, EBV, hepatitis C virus).
Many remain localised to the extranodal site. However a significant proportion present as or undergo high-grade transformation and when they metastasise typically do so to other extranodal sites. This site homing can be explained by the embryological development and circulation of mucosa associated lymphoid tissue (MALT) . The low-grade MALTomas often arise from a background of chronic antigenic stimulation:
Gastric MALT lymphoma | H. pylori gastritis |
Thyroid MALT lymphoma | Hashimoto’s thyroiditis |
Salivary gland MALT lymphoma | Lympho(myo-)epithelial sialadenitis/Sjögren’s syndrome |
They normally comprise a sheeted or nodular infiltrate of centrocyte like cells, destructive lymphoepithelial lesions and sometimes monotypic plasma cell immunoglobulin expression. Interfollicular infiltration or follicular colonisation of reactive follicles by the neoplastic cells is characteristic. There is often a component of blast cells and the immunophenotype is one of exclusion in that they are CD5 and cyclin-D1 negative ruling out mantle cell lymphoma and other small B lymphoproliferative disorders. Other extranodal lymphomas have diverse morphology and immunophenotype correlating with the full spectrum of the WHO classification, although the lymph node based categories are not consistently transferable to extranodal sites.
Immunosuppressed post transplant (solid organs or bone marrow) patients are prone to a wide spectrum of nodal/extranodal polyclonal and monoclonal B/T cell lymphoproliferative disorders (PTLD: post-transplant lymphoproliferative disorder). The latter is either non-destructive: plasmacytic hyperplasia/infectious mononucleosis like, or destructive: polymorphic B cell hyperplasia/polymorphic B cell lymphoma. Early PTLD is more likely to be EBV positive while late PTLD is usually EBV negative. Monomorphic PTLD resembles conventional B or T-cell lymphoma and Hodgkin lymphoma. In general monomorphic/monoclonal lesions require multi-modality therapy while polymorphic/polyclonal lesions may regress without therapy or following elimination of EBV positive B-cells. However, even apparent high-grade lymphoma may potentially regress if immunosuppressant therapy is decreased. Whole blood and/or tissue expression of EBV are ascertained and clinical response to reduction of immunosuppressants is assessed prior to escalation of therapy. PTLD like findings can also be present in patients receiving chronic immunosuppression therapy for autoimmune diseases.
Prognosis
For some malignant lymphomas watchful waiting is the initial course of action and treatment is only instigated once the patient is symptomatic. Otherwise, immuno-chemotherapy and radiotherapy, autologous or allogeneic bone marrow transplant are the principal treatment modalities for malignant lymphoma. However, surgical excision is often involved for definitive subtyping in primary lymph node disease or for removal of a bleeding or obstructing tumour mass and primary diagnosis of extranodal malignant lymphoma, e.g. gastric lymphoma. Prognosis relates to lymphoma type/grade (small cell and nodular are better than large cell and diffuse), and stage of disease. Low-grade or indolent nodal malignant lymphomas have a high frequency (>80% at presentation) of bone marrow and peripheral blood involvement. They are incurable pursuing a protracted time course and multiple relapses with potential for blastic or high grade transformation (e.g. CLL: 23% risk at 8 years). High-grade or aggressive lymphomas develop bone marrow or peripheral involvement as an indication of advanced disease and the latter are known to have high fatality rates. Overall, four broad prognostic categories are identified in NHL, although outlook does vary within individual types e.g.:
NHL type | 5 year survival |
|---|---|
1. Anaplastic large cell/MALT/follicular | >80% |
2. Nodal marginal zone/small lymphocytic/lymphoplasmacytoid | 60–80% |
3. Mediastinal B cell/large B cell/Burkitt’s | 30–70% |
4. T lymphoblastic/peripheral T cell/mantle cell | <50% |
Hodgkin lymphoma (HL) is relatively radiotherapy and chemotherapy responsive. Prognosis relates to stage of disease more than histological subtype. Average 5 year survival and cure rates for HL are 75% with worse outcome for older patients (>40–50 years), disease of advanced stage (i.e. more than one anatomical site), involvement of the mediastinum by a large mass (>1/3 of the widest thoracic diameter), spleen or extranodal sites.
There is evidence that early (confined to the mucosa), gastric MALToma is potentially reversible on removal of the ongoing antigenic stimulus, i.e. antibiotic treatment of H. pylori. However, lesions with deep submucosal or muscle invasion require chemotherapy supplemented by surgery if there are local mass effects, e.g. bleeding or pyloric outlet stenosis. High grade transformation of MALT lymphoma us usually treated by immunochemotherapy.
T cell lymphomas form a minority of NHL (10–15%) and tend to have a worse prognosis than B cell lesions. Their cytological features are not particularly reliable at defining disease entities or clinical course, which is more dependent on tumour site and clinical setting. Involvement of extranodal sites and relapse is not infrequent with typically an aggressive disease course, e.g. enteropathy associated T cell lymphoma and extra nodal T/NK lymphoma. Cutaneous ALCL has a favourable prognosis while that of systemic ALCL with skin involvement is poor: 50% present with stage III/IV disease and there is a 65–85% 5 year survival rate but relapse is high (30–60%).
Similarly some B cell lymphomas have site specific characteristics and clinical features, e.g. mantle cell lymphoma in the gut (lymphomatous polyposis) or mediastinal diffuse large B cell lymphoma – young females with a rapidly enlarging mediastinal mass associated with superior vena cava syndrome. A large (>10 cm) mass and extramediastinal spread indicate poor prognosis. Generally adverse prognostic factors in NHLs are:
-
Age > 60 years.
-
Male gender.
-
Systemic symptoms (fever >38 °C, weight loss >10%, night sweats).
-
Poor performance status.
-
Anaemia
-
Elevated serum LDH.
-
Tumour bulk:
-
5–10 cm (stage I/II); >10 cm (stage III/IV)
-
Large mediastinal mass
-
Palpable abdominal mass
-
Combined paraortic and pelvic nodal disease.
-
Combinations of these parameters can be scored clinically using the international prognostic index (IPI) for various NHLs (e.g. FLIPI for follicular lymphoma) for risk stratification and 5 year survival figures.
Other Malignancy
Carcinoma, germ cell tumours and malignant melanoma frequently metastasise to lymph nodes and are seen either in diagnostic biopsies (or FNAC) in patients with lymphadenopathy, or in regional lymph node resections in patients with known cancer. Spread of malignant mesothelioma or sarcoma to lymph nodes is unusual although it does occur, e.g. alveolar rhabdomyosarcoma, epithelioid sarcoma, synovial sarcoma. Assessment is by routine morphology supplemented by ancillary techniques, e.g. immunohistochemistry and molecular methods, although it should be noted that the significance of nodal micrometastases in a number of cancers is still not resolved. Metastases are initially in the subcapsular sinus network expanding to partial or complete nodal effacement with potential for extracapsular spread. Anatomical site of involvement can be a clue as to the origin of the cancer, e.g. neck (cancer of the upper aerodigestive tract, lung, breast, salivary glands or thyroid gland), supraclavicular fossa (lung, stomach, prostate, testis, ovary or breast cancer), axilla (breast, lung cancer or malignant melanoma), groin (cancer of the perineum or perianal area, cutaneous melanoma and rarely the pelvis) and retroperitoneum (germ cell tumour, genitourinary cancers). The metastatic deposit may be necrotic or cystic (e.g. squamous cell carcinoma of the head and neck, germ cell tumour in the retroperitoneum), resemble the primary lesion or be more or less well differentiated. Cell cohesion with nesting, necrosis, focal or sinusoidal distribution, solid lymphatic plugs of tumour and plentiful cytoplasm favour non-lymphomatous neoplasia although this is not always the case, e.g. ALCL or DLBCL. In this respect a broad but basic panel of antibodies is crucial for accurate designation (e.g. cytokeratins, CD45, CD30, OCT3/4, S100, melan-A, chromogranin) occasionally supplemented by histochemistry (e.g. PAS diastase resistant mucin positivity, an organoid pattern of reticulin fibres). Some metastases also induce characteristic inflammatory responses, e.g. squamous cell carcinoma of head and neck, large cell lung cancer and nasopharyngeal carcinoma (lymphocytes, leukaemoid reaction, eosinophils, granulomas) even mimicking HL. Some diagnostic clues are:
Malignant melanoma | Cell nests, eosinophilic nucleolus, spindle/epithelioid cells, melanin pigment, S100, HMB-45, melan-A, SOX10. |
Germ cell tumour | Midline (mediastinum or retroperitoneum), elevated serum βHCG or AFP (± tissue expression), PLAP/CD117 (seminoma), cytokeratins/CD30 (embryonal carcinoma). Also SALL4 and OCT3/4 (except yolk sac tumour). |
Lobular breast cancer | Sinusoidal infiltrate of sheeted, non-cohesive small cells, intracytoplasmic lumina, cytokeratins (CAM 5.2, AE1/AE3, CK7), GCDFP-15 and ER positive. Metastatic ductal cancer often has a nested pattern of larger cells with variable ER/HER2 positivity (Grade 1 or 2 tumours will have a tubular component). |
Small cell carcinoma | Small (×2–3 the size of a lymphocyte), round to fusiform cells, granular chromatin, inconspicuous nucleolus, moulding, crush and DNA artifact, ± paranuclear dot CAM 5.2, and chromogranin/synaptophysin/CD56/TTF-1 (Merkel cell carcinoma is CK 20 positive). In addition to positivity with the above markers other metastatic neuroendocrine tumours (e.g. carcinoid, large cell neuroendocrine carcinoma) show stronger chromogranin and cytokeratin expression than small cell carcinoma. |
Lung adenocarcinoma | Variably glandular or tubulopapillary, CK7/TTF-1/napsin-A/CEA/BerEP4/MOC31. |
Thyroid carcinoma | Papillae, characteristic nuclei (overlapping, optically clear, grooves), psammoma bodies, CK7/TTF-1 and thyroglobulin/CK19. |
Colorectal adenocarcinoma | Glandular with segmental and dirty necrosis, CK20/CEA/CDX-2/βcatenin. |
Upper gastrointestinal and pancreaticobiliary adenocarcinoma | Tubuloacinar, tall columnar cells with clear cytoplasm, CK7/CEA/CA19-9/± CK20/CDX-2). |
Ovarian carcinoma | Serous (tubulopapillary, psammoma bodies, CK7/CA125/WT-1/p16), or mucinous (glandular, CK7, ± CK20/CA125). |
Uterine adenocarcinoma | Endometrioid (CK7/vimentin/ER) or serous (CK7/p53/Ki-67/HMGA2/PTEN/AMACR). |
Prostate adenocarcinoma | Acinar or cribriform, PSA m/p, PSAP. |
Bladder carcinoma | Nested (squamoid) or micropapillary, CK7/CK20/34βE12/CK5/6/uroplakin III. |
The reader is referred to the Introduction for further discussion of the use of immunohistochemistry. Regardless, there are approximately 3–5% cancers of unknown primary origin wherein despite extensive imaging and pathological examination, a primary site is not found. These require expert review and discussion at specialised MDT.
References
Alizadeh AA, Eisen MB, Davis RE. Distinct types of large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503–11.
Attygalle AD, Cabeçadas J, Gaulard P, et al. Peripheral T-cell and NK-cell lymphomas and their mimics; taking a step forward—report on the lymphoma workshop of the XVIth meeting of the European Association for Haematopathology and the Society for Hematopathology. Histopathology. 2014;64:171–99.
Brown D, Gatter K, Natkunam Y. Bone marrow diagnosis: an illustrated guide. Hoboken, NJ: Wiley Blackwell; 2006.
Brunning RD, Arber DA. Bone marrow. Chapter 23. In: Rosai J, editor. Rosai and Ackerman’s surgical pathology. 10th ed. Amsterdam: Elsevier; 2011.
Campo E, Chott A, Kinney MC, Leoncini L, Meijer CJLM, Papadimitriou CS, Piris MA, Stein H, Swerdlow SH. Update on extranodal lymphomas. Conclusions of the workshop held by the EAHP and the SH in Thessaloniki, Greece. Histopathology. 2006;48:481–504.
Chan JKC. Tumours of the lymphoreticular system, including spleen and thymus. In: Fletcher CDM, editor. Diagnostic histopathology of tumours, vol. 2. 3rd ed. London: Harcourt; 2007. p. 1139–310.
De Kerviler E, Guermazi A, Zagdanski AM, et al. Image-guided core-needle biopsy in patients with suspected or recurrent lymphoma. Cancer. 2000;89:647–52.
Dojcinov SD, Venkataraman G, Pittaluga S, et al. Age-related EBV-associated lymphoproliferative disorders in the Western population: a spectrum of reactive lymphoid hyperplasia and lymphoma. Blood. 2011;117:4726–35.
Du M-Q, Bacon CM, Isaacson PG. Kaposi sarcoma-associated herpesvirus/human herpesvirus 8 and lymphoproliferative disorders. J Clin Pathol. 2007;60:1350–7.
Rosai J. Lymph nodes, spleen. Chapter 22. In: Goldblum J, Lamps L, McKenney J, Myers J, editors. Rosai and Ackerman’s surgical pathology. 11th ed. Amsterdam: Elsevier; 2017.
Grogg KL, Miller RF, Dogan A. HIV infection and lymphoma. J Clin Pathol. 2007;60:1365–72.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma immunohistochemistry using a tissue microarray. Blood. 2004;103:275–82.
Hart A, Lechowicz MJ. Breast implant-associated anaplastic large cell lymphoma: treatment experience in 53 patients. Blood. 2013;122:5089.
Intlekofer AM, Joffe E, Batlevi CL, et al. Integrated DNA/RNA targeted genomic profiling of diffuse large B-cell lymphoma using a clinical assay. Blood Cancer J. 2018;8:60.
Kapatai G, Murray P. Contribution of the Epstein-Barr virus to the molecular pathogenesis of Hodgkin lymphoma. J Clin Pathol. 2007;60:1342–9.
Kocjan C. Cytological and molecular diagnosis of lymphoma. ACP best practice no 185. J Clin Pathol. 2005;58:561–7.
Leoncini L, Delsol G, Gascoyne RD, Harris NL, Pileri SA, Piris MA, Stein H. Aggressive B-cell lymphomas: a review based on the workshop of the XI meeting of the European Association for Haematopathology. Histopathology. 2005;46:241–55.
Maes B, De Wolf-Peeters C. Marginal zone cell lymphoma—an update on recent advances. Histopathology. 2002;40:117–26.
Matutes E. Adult T-cell leukaemia/lymphoma. J Clin Pathol. 2007;60:1373–7.
Műller-Hermelink HK, Zettl A, Pfeifer W, Ott G. Pathology of lymphoma progression. Histopathology. 2001;38:285–306.
O’Malley DP, George TI, Orazi A, editors. Benign and reactive conditions of lymph node and spleen. Washington DC: ARP Press; 2009.
Oudejans JJ, van der Walk P. Diagnostic brief. Immunohistochemical classification of B cell neoplasms. J Clin Pathol. 2003;56:193.
Prakash S, Swerdlow SH. Nodal aggressive B-cell lymphomas: a diagnostic approach. J Clin Pathol. 2007;60:1076–85.
Sagaert X, De Wolf-Peeters C. Anaplastic large cell lymphoma. Curr Diagn Pathol. 2003;9:252–8.
Salaverria I, Martin-Guerrero I, Wagener R, et al. A recurrent 11q aberration pattern characterizes a subset of MYC-negative high-grade B-cell lymphomas resembling Burkitt lymphoma. Blood. 2014;123:1187–98.
Sehn LH, Berry B, Chhanabhai M, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109:1857–61.
Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J. WHO classification of tumours of haemopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2017.
Tapia G, Lopez R, Munoz-Marmol AM, Mate JL, Sanz C, Marginet R, Navarro J-T, Ribera J-M, Ariza A. Immunohistochemical detection of MYC protein correlates with MYC gene status in aggressive B cell lymphomas. Histopathology. 2011;59:672–8.
Taylor CR. Hodgkin’s disease is a non-Hodgkin’s lymphoma. Hum Pathol. 2005;36:1–4.
The National Cancer Action Team and The Royal College of Pathologists. Additional best practice commissioning guidance for developing haematology diagnostic services. (in line with the NICE improving outcomes guidance for haemato-oncology). http://www.rcpath.org/publications-media/publications
The Royal College of Pathologists. Standards for specialist laboratory integration and dataset for the histopathological reporting of lymphomas. 2015. https://www.rcpath.org/uploads/assets/uploaded/dc15eefa-4b49-461d-a292fa44a6541e03.pdf.
The Royal College of Pathologists. Standards and datasets for reporting cancers. Dataset for histopathological reporting of cancer of unknown primary (CUP) or malignancy of unknown primary origin (UO). 2018. www.rcpath.org/uploads/assets/uploaded/d060a31a-b4b5-4e05-8396b65125b7fa87.pdf.
Tiacci E, Trifonov V, Schiavoni G, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011;364:2305–15.
Treon SP, Xu L, Yang G, et al. MYD88L265P somatic mutation in Waldenstrom’s macroglobulinemia. N Engl J Med. 2012;367:826–33.
Warnke RA, Weiss LM, Chan JKC, Cleary ML, Dorfman RF. Tumors of the lymph nodes and spleen. Atlas of tumor pathology, vol. 3. Washington, DC: AFIP; 1995.
Willemze R, Cerroni L, Kempf W, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood. 2019;133:1703–14. https://doi.org/10.1182/blood-2018-11-881268.
Wilkins BS, Wright DH. Illustrated pathology of the spleen. Cambridge: Cambridge University Press; 2000. p. 1–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Venkatraman, L. (2020). Nodal Malignant Lymphoma (With Comments on Extranodal Malignant Lymphoma and Metastatic Cancer). In: Boyle, D., Allen, D. (eds) Histopathology Reporting. Springer, Cham. https://doi.org/10.1007/978-3-030-27828-1_35
Download citation
DOI: https://doi.org/10.1007/978-3-030-27828-1_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27827-4
Online ISBN: 978-3-030-27828-1
eBook Packages: MedicineMedicine (R0)