Abstract
The main objective of airway reconstruction is to establish a patent laryngeal airway without the need of a tracheostomy tube as well as being able to support respiration, airway protection, and voicing (Kelchner et al. Pediatric voice: a modern, collaborative approach to care. San Diego: Plural Publishing; 2014). To achieve these goals, several surgical techniques may be used to either expand the airway diameter, remove the stenosed segment, or slide the airway. The most common airway expansion procedure is laryngotracheoplasty (LTP) with anterior and/or posterior costal cartilage grafts, while the most common resection procedure is cricotracheal resection (CTR). Slide tracheoplasty improves the airway diameter by sliding one segment of the airway onto the other, effectively doubling the size of the slid section. Each of these procedures has its advantages and disadvantages regarding surgical correction of the stenotic airway. Similarly, these techniques, as well as the initial airway injury, impact voice outcome to different degrees.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Dysphonia after laryngotracheal reconstruction
- Laryngotracheal reconstruction dysphonia
- Airway reconstruction
- Laryngotracheoplasty
- Slide tracheoplasty
- Cricotracheal resection
Overview
The main objective of airway reconstruction is to establish a patent laryngeal airway without the need of a tracheostomy tube as well as being able to support respiration, airway protection, and voicing [1]. To achieve these goals, several surgical techniques may be used to either expand the airway diameter, remove the stenosed segment, or slide the airway. The most common airway expansion procedure is laryngotracheoplasty (LTP) with anterior and/or posterior costal cartilage grafts, while the most common resection procedure is cricotracheal resection (CTR). Slide tracheoplasty improves the airway diameter by sliding one segment of the airway onto the other, effectively doubling the size of the slid section. Each of these procedures has its advantages and disadvantages regarding surgical correction of the stenotic airway. Similarly, these techniques, as well as the initial airway injury, impact voice outcome to different degrees.
Childhood dysphonia is associated with social withdrawal and depression and has negative influences on emotional, educational, and occupational outcomes. Moreover, it has been reported that teachers have a negative bias toward adolescents who have a voice disorder [2]. Ultimately, voice disorders may lead to psychosocial problems that will affect patients over their lifetime, specifically their career choices and their long-term quality of life [3]. Once a patent airway has been secured, efforts should be made to improve patient’s voice and overall quality of life as it can have significant effects on their well-being.
Patients with airway disorders represent a unique subset of patients. The majority of them have undergone numerous hospitalizations, were premature, and are typically involved in multiple complex medical and surgical interventions. When caring for pediatric airway patients, consideration of additional interventions should be individualized, which requires a thorough and complete workup. Voice evaluation provides further crucial, detailed functional information that can specifically direct the management of ongoing airway problems and voice problems.
Definitions
Supraglottic Phonation
Supraglottic phonation implies the patient is voicing by means of supraglottic rather than glottic vibration [4]. The source of vibration from the supraglottic tissues may vary across patients and may include any of the following structures or combination of structures: the ventricular folds, the aryepiglottic folds with or without the petiole, and the interarytenoid mucosa. The sound generated from these structures results in a distinct, perceptually low-pitched, rough voice quality. Patterns of supraglottic compression are typically documented as either lateral-medial (medial movement of the ventricular folds during true vocal fold phonation) or anterior-posterior (anterior movement of the arytenoid cartilages toward the petiole) [4] (Fig. 40.1).
Posterior Glottic Diastasis
Posterior glottic diastasis is suspected in patients with a history of airway expansion or prolonged intubation who present with breathy dysphonia. Rigid endoscopy is performed to confirm the presence of a broad posterior cricoid plate and interarytenoid space contributing to a persistent posterior keyhole aperture (Fig. 40.2).
Laryngotracheoplasty (LTP)
LTP is a surgical procedure to expand the airway diameter by placing an anterior and/or posterior costal cartilage graft (ACCG, APCCG, PCCG), most often costal cartilage or thyroid ala cartilage. This procedure can be performed as a double-stage surgery (placement of a tracheostomy) or as a single-stage surgery (removal or non-placement of a tracheostomy). Multiple factors may impact voice outcomes, such as prelaryngeal muscle dissection during surgery, baseline subglottic stenosis severity, and laryngeal nerve injury.
Cricotracheal Resection (CTR)
CTR involves the excision of the anterolateral cricoid plate and anastomosis of the distal tracheal ring to the proximal thyroid ala with suture lines placed in the posterior cricoid mucosa to reapproximate the trachealis to the more proximal cricoid plate [5]. This procedure should be reserved for experienced surgeons as results are highly surgeon dependent. Furthermore, this procedure may significantly alter the voice. In particular, CTR decreases the fundamental frequency of connected speech and vowel phonation and changes the acoustic signal type [6].
Slide Tracheoplasty
Slide tracheoplasty is a surgery to increase tracheal diameter. The trachea is opened anteriorly and posteriorly. It is then slid up onto itself and reconnected to make the trachea shorter, but wider. This procedure is classically performed for long-segment congenital tracheal stenosis. Limited data exist regarding specific voice outcomes after such procedures, but vocal fold paralysis has been reported in approximately 5% of patients [7].
Epidemiology
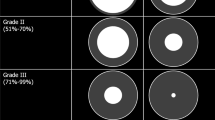
Voice disturbance following airway reconstruction is not uncommon; more than half of children who undergo airway surgery are reported to have postoperative dysphonia, which is often described as severe [3]. Parents and patients concerns about normalization of the airway and removal of the tracheostomy often overshadow initial concerns about voice outcome and dysphonia. Concerns about voice become more relevant during middle school and high school. Typically, children in these age groups are moving from one environment to another and therefore encountering novel situations where their abnormal voice becomes more relevant. Consequently, in our experience, children in these age groups are more likely to seek care related to their dysphonic voice. Additional benefits of early voice evaluation include counseling about potential voice problems post reconstruction. Risk factors for poor voice outcomes after an airway reconstruction are numerus and include [8, 9]:
-
Complete laryngofissure
-
Cricotracheal resection
-
Posterior grafting
-
Higher grade of subglottic stenosis (SGS)
-
Revision airway surgery
-
History of multiple airway reconstructions
Patients with low-grade stenosis (grade 1–2), single-stage procedure, and fewer comorbidities are less likely to have post-reconstruction dysphonia [9, 10].
Pathophysiology
Post-reconstruction dysphonia is multifactorial and occurs in more than half of patients. Postsurgical causes of dysphonia include, but are not limited to:
-
Abnormal vocal fold mobility
-
Persistent subglottic stenosis
-
Anterior commissure blunting
-
Posterior glottic diastasis
-
Prolapsed petiole
-
Vertical asymmetry of vocal folds
-
Vocal fold scaring
-
Supraglottic compression
Dysphonia after airway reconstruction may depend on the baseline airway problem and the type of surgery performed. Glottic incompetence is often a problem, either secondary to vocal fold immobilization due to laryngeal nerve dysfunction, cricoarytenoid fixation, or glottic diastasis with a posterior graft. With vocal fold immobility and cricoarytenoid fixation, patients often compensate with supraglottic phonation, using their ventricular folds to produce voice [11]. Such compensatory compression patterns and alternate sources of vibration used by these children often result in moderate to severe dysphonia. These patients also typically complain of breathiness, strain, and fatigue. Additionally, patients may have difficulty modulating or creating sound due to excessive scarring and/or injury to the prelaryngeal muscles during dissection for their airway reconstruction [5]. A complete laryngofissure violates the anterior commissure and depending on postoperative healing or long-term changes during pubertal growth may result in off-level vocal folds, anterior commissure blunting, or petiole prolapse (Fig. 40.3) [12, 13].
As previously mentioned, CTR will frequently lead to a more severe degree of dysphonia. This is partly explained by either the removal of the cricothyroid muscle and obliteration of the cricothyroid membrane [5]. Moreover, there is a possibility of arytenoid prolapse (Fig. 40.4) due to destabilization of the cricoarytenoid joint or vocal fold paralysis secondary to recurrent laryngeal nerve injury during surgery.
Presentation
Most patients will report some degree of dysphonia after airway reconstruction. Typically, voice outcomes after airway reconstruction include roughness, breathiness, supraglottic phonation, or inappropriate pitch [1, 14]. These children often present when they are becoming more social or making decisions about future careers. In younger children (ages 5–10 years), issues may arise as children begin participation in sports and other social activities. As children reach middle school age, they may have more issues related to being in multiple different classroom settings with different peer groups and teachers who are not familiar with their voice. Concerns include peers noticing this dysphonia as well as difficulty being heard in a noisy environment, embarrassment about their voices, and reduced willingness to participate in class [15]. In adolescents, the voice is important for social interactions, defining their identity, and determining their future occupation. Teenagers report embarrassment and fear of peer responses to their voice, as well as frustration and social isolation [15].
Otolaryngologist and Speech-Language Pathologist Approach
Patients with dysphonia after airway reconstruction are typically complex, and there are a variety of parameters that must be evaluated. As such, the evaluation is best performed in a multidisciplinary fashion with both an otolaryngologist and speech-language pathologist well-versed in voice pathology. Multidisciplinary voice evaluation frequently influences the course of treatment for patients with airway reconstruction and dysphonia [14, 16].
History
The history for these patients is largely obtained from the parents, but the child’s perspective is also very important when discussing the management of voice concerns. Many children will have had voice issues throughout their life related to prior intubations, scarring in the airway, and prior surgical interventions. At the time of presentation for voice evaluation, it is necessary to determine the child’s airway history including intubation history, history or presence of a tracheostomy, and prior surgical interventions. Furthermore, attention should also focus on current medications and relevant comorbidities such as pulmonary or swallowing disorders. Details of the surgical interventions performed, such as if anterior or posterior grafts were placed or if a laryngofissure was performed, are useful in helping predict potential causes of the dysphonia. Reviewing operative notes and operative videos, if available, may also be helpful to determine potential causes of the dysphonia.
As with any history, the clinicians should determine the nature and course of the dysphonia, alleviating and aggravating factors, and if prior interventions (e.g., voice therapy, injections, surgery) have been attempted. If they have had prior interventions, the specifics of those and their outcomes should be elicited. The family’s perception of the voice quality (e.g., weak, breathy, rough, raspy, harsh, deep) and how it is affecting the child’s quality of life in all environments (e.g., home, school, social, work) is important. Families will sometimes report that the child has “two voices” – typically a weaker one (presumably the glottic voice) and a stronger but deeper one (presumably a supraglottic voice). They may describe this as a “duck” voice or “superhero” voice. For a younger preverbal patient, a formal preoperative voice evaluation may be challenging; however, the breathing pattern, presence of stridor, and babbling can be documented.
Indices such as the pediatric Voice Handicap Index (pVHI) [17] or Voice-Related Quality of Life (VRQL) [18] can assist in elucidating the perceived impact of dysphonia. Similar factors that may cause laryngeal irritation and exacerbate voice problems in other patients, such as laryngopharyngeal reflux, allergic rhinitis, chronic cough, asthma, sleep-disordered breathing, smoke exposure, and vocal misuse/overuse, must be evaluated, as well.
Additionally, operating on the larynx can significantly and disparately impact voice, airway, and swallowing. As such, the current airway status (e.g., tracheostomy, decannulated), presence of stridor or dyspnea on exertion, and time of last airway evaluation should be noted. Lastly, patients who undergo open airway reconstruction are also likely to experience some degree of postoperative dysphagia symptoms and delayed return to oral intake. Cough, choking events, and aspiration pneumonias should be documented. The patient’s current feeding status and swallowing safety should also be assessed.
Examination
The examination is typically completed in conjunction with the speech-language pathologist. Combined evaluation has been proven to be beneficial for decision-making regarding voice management and potential surgical interventions [14]. A general head and neck examination should be completed. Special attention should be paid to the intelligibility, voice quality, effort for voice production, and voice range. Specific perceptual instruments, such as the grade, roughness, breathiness, asthenia, and strain (GRBAS) [19] scale or Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V) [20], are used to document the quality and severity of the dysphonia. These scales assist in establishing a baseline and monitoring progress over time. Interestingly, a prior study showed only weak-to-fair correlation between the parent-reported pVHI and expert ratings of voice quality using the CAPE-V [21]. The presence of diplophonia and if two discrete voices can be elicited should be documented.
The otolaryngologist should pay attention to the presence of stridor or respiratory distress; however, most children presenting for voice evaluation after airway reconstruction have typically overcome this challenge. Finally, patients who have undergone airway reconstruction may have other factors that can affect their voice outcome or ability to participate in therapy, such as syndromes, other congenital abnormalities, or developmental delay that should be noted.
Instrumental Assessment
Endoscopic Evaluation
Laryngoscopy and videostroboscopy should be performed. Again, the speech-language pathologist and otolaryngologist serve complimentary roles. Depending on the child’s age, ability to cooperate, and anatomy, flexible transnasal and/or rigid transoral 70-degree stroboscopy may be completed. Whereas one or the other is often adequate for evaluation of common laryngeal lesions, both transnasal and transoral exams may be necessary to fully evaluate the anatomy and function in these post-airway reconstruction patients. The use of a distal chip telescope will improve image quality, and recording the examination is useful for reference. Careful attention should be paid to attempting to determine the sound generator for phonation (e.g., glottic or supraglottic or both), presence of a posterior glottic gap, if the vocal folds are level, the degree of scarring, the mobility of the vocal folds and arytenoids, and the degree of effort/strain with vocalization. Of note, examination of the glottis during phonation is often difficult due to the degree of supraglottic collapse and/or squeeze seen in these patients as well as postsurgical anatomical variation. Parameters of vibratory patterns should also be evaluated via stroboscopic exam.
Rigid endoscopy in the operating room alone is not adequate for evaluation of vocal pathology. However, the mobility of the arytenoids, presence of posterior glottic scarring or diastasis, and other structural anomalies can be assessed and may add important information to the clinical picture.
Acoustic and Aerodynamic Evaluation
Post-airway reconstruction patients should undergo acoustic and aerodynamic evaluation. This is typically completed by the speech-language pathologist, and detailed descriptions of these exams can be found in other chapters. Briefly, acoustic analysis provides information regarding the fundamental frequency; jitter, shimmer, and noise-to-harmonic ratio; and frequency range and may also include spectral/cepstral measures such as cepstral peak prominence. Aerodynamic measures provide information regarding glottal efficiency by determining the average airflow rate and estimated subglottic pressures. Not all patients will be able to produce a type I (periodic) signal and a measurement of fundamental frequency. Common features seen in post-airway reconstruction patients are a lower pitch and reduced pitch range, breathiness, and a reduced maximum phonation time [14]. These assessments help provide a baseline and can be used to measure response to voice or surgical therapies over time. A prior study suggests that the majority of children are able to complete the acoustic and aerodynamic assessments with a significant proportion of post-airway reconstruction patients having severe dysphonia [22]. Recording enough voicing segments may be challenging and sometimes impossible; protocols should be tailored to the patient’s capability.
Other Modalities
Dynamic voice computed tomography (CT) has been described but is not yet widely available. This CT is performed with the patient holding a sustained /i/. The CT does not require contrast and is a relatively low dose of radiation (same as a general head CT). The main benefit of the voice CT is that it allows for evaluation of the glottis during phonation. As previously mentioned, this is often difficult to assess endoscopically due to the supraglottic structures. This exam is particularly useful for evaluating the degree of glottic gap during phonation (Fig. 40.5), but cannot evaluate the mucosal wave.
High-speed videography is another tool that is still largely used in a research setting, but is also used in some clinical settings. This exam can provide extremely detailed information regarding the mucosal wave and sound generator with higher reliability when compared with traditional videostroboscopy (Fig. 40.6) [4]. Limitations of this exam, however, include the availability of the equipment and the massive amount of storage space required for the data obtained for even very short examinations.
Ultrasound for evaluation of the supraglottic and glottic structures has also been described by some pediatric voice specialists. While the presence of cartilage grafts may alter visibility to a degree, the larynx does not typically calcify until around 40 years of age making this a viable tool in children.
Differential Diagnosis
The differential diagnosis for a child presenting with dysphonia after airway reconstruction is broad. While more typical laryngeal pathology (e.g., nodules, cysts, polyps, papilloma) may be present, the post-airway reconstruction vocal pathology is typically more complex. The dysphonia may relate to scarring in the subglottis, glottis, or supraglottis, arytenoid prolapse or fixation, vocal fold atrophy, vocal fold scar, or vocal fold vertical asymmetry preventing an adequate mucosal wave, anterior commissure blunting, posterior glottic diastasis, and the compensatory use of supraglottic structures for phonation. Furthermore, patients with history of airway reconstruction often have several comorbidities, such as pulmonary and neurologic disorders that can also impact voice quality. Often, a combination of these pathologies can be identified.
Management
Understanding the family and patient’s motivations for voice evaluation and how it is impacting the child’s day-to-day life is important in helping the family determine goals of therapy and/or surgical interventions. Not every patient will have the same needs or goals for their voice. Additionally, as opposed to the airway procedures these children underwent in their youth, voice interventions are more about quality of life; thus, a discussion with both the patient and family about their goals and expectations is crucial. For example, a young girl using a supraglottic voice may desire a more feminine-sounding voice. In that case, transitioning to a glottic voice may be more appropriate even if it is slightly weaker or breathier. On the other hand, if the patient is a young male whose goal is a louder voice, finding ways to help him use the supraglottic voice may be more appropriate. Additionally, some patients may not be bothered by their voice at initial evaluation. It is important to discuss with the families that voice interventions are not a “now-or-never” option. The child and family committing to voice therapy and perceiving a need for change will improve adherence to exercises. If surgery is to be undertaken, children of adequate age and maturity should be included in the discussion as voice is such an integral part of a person’s identity.
Management of these patients typically involves voice therapy alone, before surgery, and/or after surgery. Voice therapy can help the child access and use the supraglottic and/or glottic voice more easily when appropriate. Prior studies have shown that some children can achieve periodic vibration when phonating with non-glottic structures suggesting that in appropriate children, therapy can help achieve a better adapted and more acceptable supraglottic voice [14].
Initial surgical intervention should be tailored to the anatomic considerations of the patient. This often includes injection laryngoplasty, which can help improve a glottic or a supraglottic voice. Injection in the typical location, however, may be more difficult due to scarring, and, in some cases, an intracordal injection is required. Other procedures have been described specifically for posterior glottic diastasis including laryngofissure with partial posterior cricoid reduction, endoscopic pharyngoepiglottic-aryepiglottic fold advancement-rotation flap with interarytenoid interposition, interarytenoid submucosal implant augmentation [23], buccal flap augmentation [24], and endoscopic posterior cricoid reduction [25]. The following section will focus specifically on the latter intervention for posterior glottic diastasis. As awareness of post-airway reconstruction dysphonia increases, surgeons should certainly think more critically when performing airway procedures. Some strategies to help minimize the impact on voice include avoiding a complete laryngofissure when possible, meticulous reapproximation of the vocal folds in the setting of complete laryngofissure, and creating appropriately-sized (not oversized) posterior grafts when they are indicated.
Operative Approach
This section will focus on a surgical approach to posterior glottic diastasis: endoscopic posterior cricoid reduction.
Indications
Endoscopic posterior cricoid reduction is a surgical procedure to address posterior glottic diastasis. This may be caused by prior intubation and/or prior airway reconstruction, particularly when posterior grafts are placed. Patients with posterior glottic diastasis, as demonstrated on endoscopy and/or dynamic voice CT, who cannot obtain an adequate voice with voice therapy, whose voice is impacting their quality of life, and who do not have concerns for airway compromise, are candidates for this procedure. The ability to obtain adequate exposure endoscopically is also a consideration.
Key Aspects of the Consent Process
The procedure includes suspension microlaryngoscopy, use of a CO2 laser, and reduction in the size of the airway. Risks associated with each of those should be discussed. For suspension microlaryngoscopy, the risk of injury to the lips, teeth, and gums should be noted. Additionally, there is potential for dysgeusia or hyperextension injury to the neck. With use of a CO2 laser, risk of eye injury, burns to head and neck structures, and the risk of airway fire should be acknowledged. With the posterior cricoid split, there is a risk of tracheoesophageal fistula and potential need to open the neck for repair should it occur. Finally, the family and patient should understand the balance of voice, airway, and swallowing. It should be explicitly stated that making in reducing the glottic inlet to help improve the voice, there is an inherent decrease of the airway diameter. While care is taken to minimize the risk, there may be airway compromise and need for future airway interventions, including intubation, tracheostomy, and/or revision airway reconstruction. Additionally, the voice may fail to improve despite the surgical intervention, and other therapies may still be required (including voice therapy and/or additional surgical interventions).
Equipment
Traditional suspension laryngoscopy equipment should be available. Additionally, a CO2 laser, laser technician, and laser safety equipment should be available. While the procedure can be performed with cold instrumentation, in the senior author’s experience, it is advantageous to have the laser for this case.
Steps (Fig. 40.7)
-
1.
Patient Positioning and Preparation
Discussion with the anesthesia team regarding preference for spontaneous ventilation and low oxygen levels while the laser is in use should be performed prior to the procedure. The patient is brought to the operating room and placed in the supine position on the operating table. Perioperative antibiotic prophylaxis (e.g., cephalexin) is given at induction. The patient should undergo initial rigid microlaryngoscopy and bronchoscopy (MLB) with a dental guard, an appropriately sized Phillips blade, and a rigid Hopkins rod 0-degree telescope. Laryngotracheal anesthesia should be employed. Sizing of the airway should be performed pre- and postoperatively with endotracheal tubes. Photodocumentation should be employed throughout the case.
-
2.
Exposure
After the initial MLB has been performed, the patient should be placed in suspension with the largest Lindholm laryngoscope the patient can accommodate. If the exposure is not adequate with this, taping of the anterior neck to provide constant cricoid pressure or a different laryngoscope (such as a Zeitels universal modular glottiscope placed in the laryngeal vestibule) may be employed. Furthermore, a shoulder roll may give some additional degree of exposure.
-
3.
Injection
Once adequate exposure is obtained, the posterior cricoid can be palpated. An orotracheal injector is then used to inject 1% lidocaine with 1:100,000 epinephrine into the posterior cricoid plate to assist with hemostasis.
-
4.
Laser Precautions
While allowing time for the local anesthetic to work, standard laser precautions should be instituted. The patient’s eyes should be taped with silk tape and wet eye pads and the skin covered with wet towels. All room staff should have adequate eye protection. The windows to the room should be covered and signs placed on each entrance warning that the laser is in use. The microscope should be appropriately prepared for use with the laser, and a smoke evacuator should be turned on. The accuracy of the laser beam must be ensured off the field. Communication should be instituted with the anesthesia team regarding safe oxygen levels. A basin of water or saline should be available on the scrub table in case of fire.
-
5.
Cricoid Reduction
Once all necessary laser precautions have been instituted, the operating microscope is brought into the field. The posterior split and reduction are then performed using the CO2 laser (SurgiTouch+ set at 16 W, 2 mm depth, and approximately 1.6 mm circle shape). The surgeon should have a predetermined width of reduction planned and size the laser shape accordingly. Care should be taken to stay in a straight line in the midline when performing the split and to not take a wider segment than planned. This can be completed with a D-knife or Blitzer knife if the CO2 laser is not available. The surgeon should confirm that the split extends the full length of the cricoid by using a vocal fold spreader to distract the cricoid laterally. The posterior common party wall should be respected throughout the dissection and carefully inspected afterward to ensure a tracheoesophageal fistula is not created. The microscope and the zero-degree telescope can be used for visualization throughout this process, as needed. Afrin-soaked pledgets may then be used to attain hemostasis.
-
6.
Refinement of the Cricoid Split
The edges of the split should be refined as needed using the CO2 laser (with a straight line instead of a circle) to allow for excellent midline approximation. Once the laser is no longer required, it may be helpful to communicate to the anesthesia team that the oxygen level can be increased. At this point, attention is turned to suture repair of the cricoid.
-
7.
Cricoid Closure
Using an endoscopic needle driver and 4-0 PDS suture on an RB-1 needle, the cricoid is reapproximated in the midline with simple interrupted sutures. A distal suture is placed followed by a proximal suture. Two sutures are typically adequate for closure. A post-procedure photograph should be taken, and the patient can then be taken out of suspension.
-
8.
Final Bronchoscopy
The larynx should again be exposed with the Phillips blade and repeat sizing of the airway performed using endotracheal tubes.
-
9.
Final Tips
-
Intermittent intubation may be employed throughout the case.
-
Excellent communication with the anesthesia team is helpful.
-
Size the airway before and after the procedure.
-
Make sure the midline split is both midline and straight. Right-handed surgeons will tend to veer to the right and left-handed surgeons veer to the left.
-
Zeitels universal modular glottiscope often provides excellent exposure for more difficult cases.
-
Endoscopic cricoid reduction. (a) Preoperative view of the posterior glottic diastasis (b) Closer look at the preoperative glottic diastasis. (c) CO2 laser cricoid split with vocal folds spreader in place demonstrating the split cricoid and the preserved posterior wall. (d) Endoscopic sutures of the posterior cricoid plate. (e) Postoperative view of the glottis at 1 week. (f) Postoperative view of the subglottic area at 1 week
Postoperative Management and Follow-Up
The patient should be admitted for overnight observation with airway monitoring to either an “airway stepdown” unit or the intensive care unit. Acetaminophen and ibuprofen can be employed for pain control along with oxycodone as needed for severe pain. The senior author allows the use of ketorolac on postoperative day 1, if needed. The patient should be on antibiotic prophylaxis (amoxicillin-clavulanate) and a proton pump inhibitor for 7 days and 1 month postoperatively, respectively. The patient can be orally fed after the procedure. Ideally, the patient should not receive corticosteroids that may inhibit adequate healing. A repeat microlaryngoscopy and bronchoscopy is performed one week postoperatively to ensure adequate healing of the cricoid.
Emerging and Evolving Techniques of the Future
Innovative technologies exist to optimize the evaluation of these complex patients prior surgery.
-
As already mentioned, high-speed videoendoscopy improves the ability to rate tissue vibratory characteristics when compared with videolaryngoscopy in children with supraglottic phonation. This information may allow better understanding of the underlying mechanisms of voice production in these individuals, leading to improved therapeutic and surgical recommendations [4].
-
Predicting the impact of the surgery on airway dynamics may decrease morbidity and improve overall quality of care for these complex patients. Cine magnetic resonance imaging (MRI) combined with computational fluid dynamics (CFD) has been reported to model the airflow through the dynamic airway in complex airway cases. CFD modeling might reveal the specific portions of pressure and energy losses in both inhalation and exhalation, allowing targeted interventions for these specific locations.
-
Also, the use of dynamic voice CT may provide complementary information to the videostroboscopy [26, 27]. For patients with complex airway history, the pattern of laryngeal closure could be detected more frequently compared to the standard endoscopic examination. Moreover, the location of gap closure and the vertical closure pattern of the glottis may have a better yield with the dynamic voice CT scan. Dynamic voice CT shows promise as an additional tool for evaluation of patients with a history of complex airway procedures by providing complementary information that might alter surgical decision-making.
References
Kelchner LN, Brehm SB, Weinrich BD. Pediatric voice: a modern, collaborative approach to care. San Diego: Plural Publishing; 2014.
Zacharias S, Kelchner LN, Creaghead N. Teachers’ perceptions of adolescent females with voice disorders. Lang Speech Hear Serv Sch. 2013;44:174–82.
De Alarcon A. Voice outcomes after pediatric airway reconstruction. Laryngoscope. 2012;122(Suppl 4):S84–6.
Zacharias SR, Myer CM 4th, Meinzen-Derr J, Kelchner L, Deliyski DD, de Alarcón A. Comparison of videostroboscopy and high-speed videoendoscopy in evaluation of supraglottic phonation. Ann Otol Rhinol Laryngol. 2016;125(10):829–37.
Rutter MJ, Link DT, Hartley BE, Cotton RT. Arytenoid prolapse as a consequence of cricotracheal resection in children. Ann Otol Rhinol Laryngol. 2001;110(3):210–4. PubMed ID: 11269763.
Houlton JJ, de Alarcon A, Johnson K, et al. Voice outcomes following adults cricotracheal resection. Laryngoscope. 2011;121(9):1910–4.
Stewart AJ, Butler CR, Muthialu N. Swallowing outcomes in children after slide tracheoplasty. Int J Pediatr Otorhinolaryngol. 2018;108:85–90.
Bailey CM, Clary RA, Pengilly A, Albert DM. Voice quality following laryngotracheal reconstruction. Int J Pediatr Otorhinolaryngol. 1995;32. Supple:S93–5.
Zalzal GH, Loomis SR, Fisher M. Laryngeal reconstruction in children. Assessment of vocal quality. Arch Otolaryngol Head Neck Surg. 1993;119(5):504–7.
Smith ME, Marsh JH, Cotton RT, Myer CM 3rd. Voice problems after pediatric laryngotracheal reconstruction: videolaryngostroboscopic, acoustic, and perceptual assessment. Int J Pediatr Otorhinolaryngol. 1993;25(1–3):173–81.
Kelchner LN, Weinrich B, Brehm SM, Tabangin ME, de Alarcon A. Characterization of supraglottic phonation in children after airway reconstruction. Ann Otol Rhinol Laryngol. 2010;119(6):383–90.
Bergeron M, de Alarcon A, Hart CK, Rutter MJ. Factors associated with epiglottic petiole prolapse repositioning success. Laryngoscope. 2018. [epub ahead of print].
Bergeron M, de Alarcon A, Hart CK, Rutter MJ. Outcomes of prophylactic epiglottic petiole suspension at the time of complete laryngofissure. Otolaryngol Head Neck Surg. 2019. [epub ahead of print].
Krival K, Kelchner LN, Weinrich B, Baker SE, Lee L, Middendorf JH, Zur KB. Vibratory source, vocal quality and fundamental frequency following pediatric laryngotracheal reconstruction. Int J Pediatr Otorhinolaryngol. 2007;71(8):1261–9.
Connor NP, Cohen SB, Theis SM, Thibeault SL, Heatley DG, Bless DM. Attitudes of children with dysphonia. J Voice: Off J Voice Found. 2008;22(2):197–209.
Bergeron M, Kelchner L, Weinrich B, et al. Influence of preoperative voice assessment on treatment plan prior to airway surgery. Laryngoscope. 2018;128(12):2858–63.
Zur KB, Cotton S, Kelchner L, Baker S, Weinrich B, Lee L. Pediatric voice handicap index (pVHI): a new tool for evaluating pediatric dysphonia. Int J Pediatr Otorhinolaryngol Ireland. 2007;71:77–82.
Boseley ME, Cunningham MJ, Volk MS, Hartnick CJ. Validation of the pediatric voice-related quality-of-life survey. Arch Otolaryngol Head Neck Surg. 132. United States2006:717–20.
Hirano M. Clinical examination of voice. New York: Springer-Verlag; 1981.
American Speech Language and Hearing Association (ASHA). CAPE-V procedures and form. Available from: https://www.asha.org/uploadedFiles/ASHA/SIG/03/CAPE-V-Procedures-and-Form.pdf.
de Alarcon A, Brehm SB, Kelchner LN, Meinzen-Derr J, Middendorf J, Weinrich B. Comparison of pediatric voice handicap index scores with perceptual voice analysis in patients following airway reconstruction. Ann Otol Rhinol Laryngol. 2009;118(8):581–6.
Brehm SB, Weinrich B, Zieser M, Kelchner L, Middendorf J, Elluru R, de Alarcon A. Aerodynamic and acoustic assessment in children following airway reconstruction: an assessment of feasibility. Int J Pediatr Otorhinolaryngol. 2009;73(7):1019–23.
Zeitels SM, de Alarcon A, Burns JA, Lopez-Guerra G, Hillman RE. Posterior glottic diastasis: mechanically deceptive and often overlooked. Ann Otol Rhinol Laryngol. 2011;120(2):71–80.
Helman SN, Karle W, Pitman MJ. Management of posterior glottal insufficiency with use of a buccal graft. Ann Otol Rhinol Laryngol. 2017;126(2):159–62.
Sidell DR, Zacharias S, Balakrishnan K, Rutter MJ, de Alarcón A. Surgical management of posterior glottic diastasis in children. Ann Otol Rhinol Laryngol. 2015;124(1):72–8.
Bergeron M, Fleck RJ, Middlebrook C, et al. Preliminary assessment of dynamic voice CT in post-airway reconstruction patients. Otolaryngol Head Neck Surg. 2018;159(3):516–21.
Bergeron M, Fleck RJ, Zacharias S, Tabangin M, de Alarcón A. The value of dynamic voice CT scan for complex airway patients undergoing voice surgery. Ann Otol Rhinol Laryngol. 2019 [under review].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bergeron, M., Wilcox, L.J., de Alarcon, A. (2020). Dysphonia After Laryngotracheal Reconstruction. In: McMurray, J., Hoffman, M., Braden, M. (eds) Multidisciplinary Management of Pediatric Voice and Swallowing Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-26191-7_40
Download citation
DOI: https://doi.org/10.1007/978-3-030-26191-7_40
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-26190-0
Online ISBN: 978-3-030-26191-7
eBook Packages: MedicineMedicine (R0)