Abstract
Vitreo-retinal surgical techniques have transformed since the introduction of pars plana vitrectomy in 1970. Advancements include smaller gauge instrumentation, faster cut rates, improved illumination methods, wider-field viewing systems, and the use of various tamponade agents and perfluorocarbon.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vitreo-retinal surgery
- Vitrectomy
- Cannula-trocar
- Wide-angle viewing
- Lensectomy
- Perfluorocarbon
- Subretinal injection
- Scleral buckle
- Tamponade
- Retinal detachment
History of Vitrectomy
“Open sky” vitrectomy technique, termed diapupillary resection, was described by Tsugio Dodo for partial removal of a vitreous hemorrhage from a patient in Japan in 1955 [1, 2]. However, the Western world likely did not hear about this technique until 1968 when David Kasner also described an “open sky” technique for vitreous removal using cellulose sponges and scissors. This technique was initially used to address vitreous loss during cataract surgery (Fig. 7.1) and subsequently used to remove opacified vitreous in the setting of amyloidosis [3].
The introduction of modern pars plana vitrectomy (PPV) is generally credited to Robert Machemer (Fig. 7.2) as he was responsible for developing the first automated system for vitreous removal with controlled intraocular pressure in 1970 [4]. Machemer and Helmut Buettner initially designed a vitrectomy device with a drill bit and tiny electric motor encased in a blunt hypodermic needle. Suction was added to remove the vitreous more effectively, and an infusion tube was soldered to the outside of the hypodermic needle to prevent globe collapse [5]. Machemer performed his first PPV on April 20, 1970 on a diabetic patient with a non-clearing vitreous hemorrhage and visual acuity improved from 2/200 to 20/50 [4]. Subsequently, a collaboration between Jean-Marie Parel (Fig. 7.3a) and Machemer led to the development of the vitreous infusion suction cutter (VISC, Fig. 7.3b) and the fiberoptic endoillumination used in early PPV. The VISC was developed as an instrument which cut vitreous, removed debris from the eye by suction, while simultaneously infusing Ringer’s solution [6, 7]. Early vitrectomy was performed using a VISC that was 17 gauge and 1.5 mm in diameter inserted through a 2.1 mm scleral incision [6, 8].
In 1971, Gholam Peyman (Fig. 7.4a) described a technique using a vitrophage (Fig. 7.4b) to remove and replace the vitreous [9]. In 1974, Conor O’Malley and Ralph Heintz developed the first three port 20-gauge pars plana vitrectomy system, separating the components of vitreous cutting, infusion, and illumination [10]. In 1985, Machemer and Dyson Hickingbotham introduced the first 20-gaugetrocar/cannula system to allow for easier passage and interchangeability of instruments in an attempt to reduce the risk of iatrogenic retinal tears or retinal detachment [11]. Subsequently, 20-gauge vitrectomy became standard treatment for decades.
In 1990, Eugene de Juan and Hickingbotham developed 25-gauge vitrectomy instrumentation, including a vitreous cutter, microscissors, and vitreous membrane dissector. At that time, use of 25 gauge instruments was limited to select cases requiring high precision due to slow vitreous removal speeds [12]. Peyman described a 23 gauge vitrectomy system in 1990 [13]. In 2002, Gildo Fujii introduced a 25 gauge operating system, the Transconjunctival Sutureless Vitrectomy System, allowing for self-sealing transconjunctival sclerotomies. This method popularized the widespread use of small gauge PPV [14, 15]. In 2005, Claus Eckardt introduced 23 gauge instrumentation as an alternative to 25 gauge PPV [16]. Yusuke Oshima pioneered a 27 gauge vitrectomy system in 2010 [17].
When PPV was first utilized it was generally reserved for the more severe, selected cases, such as non-clearing vitreous hemorrhage and complex retinal detachment [18]. However, evolution of vitreoretinal ancillary equipment and surgical techniques has allowed increases in the utilization of vitrectomy and indications for vitrectomy surgery (Table 7.1). Today, PPV is the most commonly performed surgical procedure by retinal specialists.
Perioperative Considerations
Vitrectomy can be performed with general or local anesthesia, including regional with or without topical anesthesia [19]. Traditionally, vitrectomy was more often performed with general anesthesia, but recently local anesthesia is also popular [20]. General anesthesia may be used when the procedure is expected to be long or painful. Additionally, patients with claustrophobia, anxiety, or dementia may benefit from surgery with general anesthesia. However, use of general anesthesia decreases turnover time, increases procedural costs, and has increased systemic risks compared to local anesthesia with monitored anesthesia care [21].
Regional block with monitored anesthesia care allows the patient to remain awake during the procedure. Several methods of local anesthesia may been used, including retrobulbar, peribulbar, sub-Tenon’s, and topical anesthesia [20]. Retrobulbar anesthesia generally provides excellent anesthesia and akinesia but is associated with small risks of retrobulbar hemorrhage and scleral perforation [22]. Peribulbar anesthesia is associated with fewer risks but is somewhat less effective than retrobulbar anesthesia and may require a longer time to produce adequate effects. Sub-Tenon’s anesthesia is administered in the posterior sub-Tenon’s space and provides rapid anesthesia and akinesia [22]. Topical anesthesia involves the use of anesthetic drops on the ocular surface. It has been reported effective in select patients for vitreoretinal surgery [23]. However, due to relatively long procedure times for most vitreoretinal surgery, it has not been widely adopted. In-office PPV with local anesthesia has also been reported, but is not widely practiced [24].
Vitrectomy Systems
Berkeley Bioengineering in 1974 developed the first three-port, 20G system known as the Ocutome 800 (Fig. 7.5). It had a lightweight pneumatic probe with axial cutting and surgeon foot pedal controlled on-off aspiration. It was followed by the Coopervision Ocutome 8000, which had the first linear aspiration system, integrated light source, and connected fragmenter. These early companies are no longer in existence or are not involved in vitrectomy surgical instruments. Another early vitrectomy system was the MID Labs MicroVit system, which produced the first high-quality disposable pneumatic cutter [25]. The Daisy (Storz) (Fig. 7.6) was introduced in 1986 and had multiple functions including irrigation/aspiration, anterior and posterior vitrectomy, bipolar coagulation, automated scissors, illumination, air exchange and phacoemulsification and fragmentation. The Daisy was followed by the Premiere system. Storz was acquired by Bausch + Lomb in 1997, and the combined organization produced the Millennium Microsurgical System (Fig. 7.7) that year. Also in 1997, Alcon introduced the Accurus (Fig. 7.8).
Currently, the most commonly used vitrectomy systems include the Constellation (Alcon, 2008), Enhanced Visual Acuity (EVA, DORC, Zuidland, the Netherlands, 2015), and the Stellaris PC/Stellaris Elite (Bausch + Lomb, Bridgewater, NJ, USA, 2010/2017). The Constellation vitrectomy system (Fig. 7.9) has a dual pneumatic vitreous cutter with increased cut rates up to 10,000 cpm, radiofrequency identification recognition technology to regulate light intensity based upon the probe gauge size, surgeon-controlled duty cycle, integrated laser, and torsional anterior segment phacoemulsification. The Constellation has capacity for 20, 23, 25, and 27 gauge instrumentation. The EVA vitrectomy system (Fig. 7.10) utilizes a two-dimensional vitreous cutter with a cut rate of up to 16,000 cpm, high flow infusion cannula, and instrumentation for 23, 25, and 27 gauge vitrectomy.
The Stellaris PC (Fig. 7.11), has vitreous cutters with cut rates of up to 5000 cpm. It also has a dual light source, color filters for differentiated viewing, and instrumentation for 20, 23, and 25 gauge vitrectomy [26]. The Stellaris Elite Vision Enhancement System (Bausch + Lomb, 2017), offers single port 20, 23, and 25 gauge vitreous cutters with cut rates up to 7500 cpm, and bi-blade 25 and 27 gauge vitrectomy cutters which cut in two directions per cycle with cut rates up to 15,000 cpm. The Stellaris Elite (Fig. 7.12) is also compatible with the ultrasound vitreous cutter, which uses ultrasound energy to liquefy vitreous (instead of cutting it with the traditional guillotine cutter) and remove it using a port that is continuously open. The equivalent cut rate of the hypersonic vitrector (Fig. 7.13) is up to 1.7 million cpm.
Cannula-Trocar Systems
After the mid-1970s, PPV was largely performed with 20 gauge instrumentation, requiring conjunctival incisions and sclerotomies measuring approximately 0.9 mm in diameter. With 20G surgery trochars were optional. More recently, the growing use of transconjunctival small-gauge has necessitated the use of cannulated sclerotomies. Fujii first reported a 25 gauge transconjunctival sutureless vitrectomy system using microtrocars and cannulas in 2002 [14, 15]. The use of smaller gauge vitrectomy instrumentation has reduced the scleral incision diameter to 0.72 mm for 23 gauge, 0.55 mm for 25 gauge, and 0.40 mm for 27 gauge (Fig. 7.14) [14, 16, 17].
Advantages of cannulas include maintaining the alignment between the conjunctiva and sclera, minimizing wound border trauma and allowing easier and faster interchangeability of instrument and infusion sites [27]. Less traumatic insertion and removal of instruments is thought to contribute to a decreased risk of iatrogenic retinal tears. Additional benefits of the cannula-trocar system include increased likelihood of self-sealing sclerotomy closure, decreased post-operative discomfort, decreased risk of inflammatory reaction secondary to suture use, and post-operative atrophy and thinning of the sclerotomy site [28]. However, the relatively small internal diameter of the cannula sleeve limits the radius of curvature of smaller gauge intraocular scissors and results in decreased efficiency of intraocular scissors for membrane cutting and dissection compared to intraocular scissors used in 20 gauge vitrectomy [29]. Currently, most vitreoretinal procedures are performed with 23 or 25 gauge transconjunctival cannula-trocar systems, and 20G vitrectomy systems are usually limited to select cases, such as severe posterior segment trauma or intraocular foreign body [30].
Valved cannulas have become popular since they minimize egress of fluid and eliminate the need for cannula plugs during instrument exchange. The practical advantages of valved cannulas are more stable intraocular fluidics and improved control of intraocular pressure. Valved cannulas are reported to be comparable to their non-valved counterparts with regards to functional and anatomical outcomes as well as post-operative complications. Valved cannulas can have the disadvantage of increased friction between the instrument and valve and difficult insertion of soft or flexible tip instruments [31, 32]. A valved cannula design can also cause intraocular pressure build-up during air-silicone oil exchange, and venting extensions have been introduced to prevent this.
Viewing Systems
Microscopes
Enhancements in the optics and illumination of operating microscopes contribute to optimization of the retina surgeon’s view. In 1954, Littmann produced the earliest modern operating microscope with a constant working distance and the ability to change magnification with a revolving Galilean turret, and paraxial illumination [33]. The Galilean turret allowed for different magnifications at a constant working distance, with lenses selected by turning a knob. Paraxial illumination utilized light tubes with bulbs attached to the mounting of the body of the microscope to illuminate the field of view and focus light at the working distance for the microscope, providing better depth perception for surgeons. The ability to move the microscope in the x- and y-axis and control the movement through a foot pedal were major advancements that improved visualization for vitreous surgery, developed by Parel and Machemer in the 1970s (Fig. 7.15) [34]. An additional advancement was incorporating a beam splitter to provide coaxial viewing for through additional oculars to allow for assistant observation through the microscope (Fig. 7.16) [34]. Over the next several decades, ocular microscopes continued to become more sophisticated with improved light sources and optics to enable improved viewing of the vitreous and retina.
A recent advancement in microscopes for vitreoretinal surgery is the availability of intraoperative real-time optical coherence tomography (OCT) integrated into the surgical microscope. Currently, OCT-integrated microscopes are available from Carl Zeiss Meditec (Fig. 7.17, Jena, Germany) and Leica Microsystems (Bannockburn, IL, US). Potential uses advantages of intraoperative OCT include confirmation of epiretinal and internal limiting membrane removal and potentially better visualization of membrane peeling in select cases without using retinal dyes [35].
Lenses
Historically, vitreoretinal surgery was performed with planoconcave or biconcave lenses under an operating microscope, which gave a limited field of view, approximately 20–35° (Fig. 7.18) [36]. Prism lenses were used to increase the field of view to 60° [37]. Wide-angle viewing systems that are now available provide increased visualization and access to the peripheral vitreous and retina. Wide-angle viewing systems provide a panoramic view of the retina through the principles of binocular indirect ophthalmoscopy and may require an image inverter mounted on the operating microscope. The two main types of wide-angle viewing systems are contact and noncontact (Table 7.2) [38,39,40,41,42].
Contact lens wide-angle viewing systems provide better image resolution, contrast, and stereopsis than noncontact systems. With direct contact with the cornea, they eliminate corneal aberrations and minimize reflective surfaces [38, 39]. The lenses are either fixed into place using a ring sutured to the sclera or they are held in place by a skilled assistant [39, 43]. The field of view and magnification vary depending upon the lens used.
Noncontact wide-field viewing systems use a lens that is placed above the cornea producing an inverted image, and they use an internal or separate prism system to reinvert the image. The field of view can be adjusted by changing the distance between the lens and the corneal surface [44]. The noncontact wide-angle viewing system does not require an assistant to hold the lens. The cornea must be coated with a viscoelastic material or be constantly irrigated to avoid corneal dehydration. Condensation on the lens, but this can be avoided with proper draping [39].
Three-Dimensional Viewing
Recently, three-dimensional (3-D) viewing techniques for vitreoretinal surgery were introduced as an alternative to traditional viewing through microscope oculars. With 3-D viewing systems, images from the microsurgical field are displayed on a flat screen via a 3-D camera. The microscope head must still be positioned properly, but visualization is independent of the oculars and requires the use of 3-D glasses for stereopsis. The single display allows multiple observers to view the 3-D surgical field. Through digital amplification of camera signals, lower illumination settings can be used, which can potentially reduce risks of phototoxicity [45]. 3-D viewing also has the potential to improve ergonomics compared to conventional binocular microsurgery [46]. The Ngenuity (Fig. 7.19, Alcon, 2016) is the only commercially available system currently.
Illumination and Filters
Initial vitrectomy was performed with coaxial light from the operating microscope and later a modified slit-lamp affixed to the operating microscope (Fig. 7.20) [47]. In order to deliver intraocular illumination, Machemer and Parel placed fiberoptics around the VISC cutter (Fig. 7.21a) in 1974 and Peyman mounted a separate fiberoptic light source attached to the vitrophage cutter in 1976 (Fig. 7.21b) [7, 48]. However, as early as 1974 the concept of separating the light source from the vitrector was introduced, by O’Malley and Heintz; this is currently standard practice for vitrectomy surgery [10]. The first light probes used halogen bulbs [49]. In order to improve illumination, xenon light sources were introduced. Theoretically the short wavelength of light emitted by xenon lamps could increase the rate of photochemical damage [50]. Light-emitting diode (LED) light sources coupled with smaller gauge instrumentation have the potential to allow reduction of the total amount retinal light exposure and can be used without a fiber [51]. A mercury vapor illuminator (Synergetics Inc., O’Fallon, Missouri, USA) was developed to provide powerful illumination and uses a dual-output pathway from one mercury vapor bulb with spherical reflectors adapted to generate homogenized illumination and sharpen the focus light spot. Spectral filters, also known as pass filters, have been introduced to eliminate hazardous wavelengths from the emission spectrum of light probes [52]. Many modern endoillumination devices have built in some variant of a yellow pass filter to screen lower wavelengths [50].
The structure of the light probes also determines the field of illumination. Straight light probes provide a field of view of 50–80°. Mid-field light probes provide a field of view of 90–110° [53,54,55]. Wide-angle light probes provide a field of view of up to 135–140°. Chandelier light sources illuminate from a greater distance than conventional light probes, reducing the risk of photochemical damage. Additionally, the use of chandeliers frees up the surgeon’s hand from having to hold the light source and allows bimanual manipulation during surgery [56].
Chromovitrectomy
Chromovitrectomy refers to the use of dyes during vitreoretinal surgery to aid in the identification of preretinal membranes or tissues [57]. The concept was introduced by Kazauki Kadonosono in 2000 when he reported the use of indocyanine green (ICG) to stain the internal limiting membrane (ILM) in macular hole surgery to improve ILM visualization and facilitate its removal [58]. However, suspected toxicity to the neuroretina and retinal pigment epithelium from ICG use has been reported and observed to be dependent upon the dye concentration, osmolarity of the solvent solutions, length of dye exposure time, and vitrectomy endolight illumination time [59]. Membrane Blue (trypan blue 0.15%, DORC, Zuidland, the Netherlands) is a dye that is FDA-approved for epiretinal membrane (ERM)/ILM peeling but is generally not as effective as ICG. Brilliant blue G is also used for this ERM/ILM peeling, but it is not FDA-approved for this indication. Triamcinolone acetonide is used to stain the vitreous to ensure complete removal of the vitreous during surgery and can stain ERMs, but is not FDA-approved [60]. Triesence® (Alcon, Fort Worth, TX, USA) is a preservative-free preparation of triamcinolone acetonide that is FDA-approved for intraocular use including use for vitreous visualization in intraocular surgery.
Lensectomy and Phacoemulsification
Pars plana lensectomy or phacoemulsification from an anterior approach can be performed during or prior to vitrectomy when visualization of the fundus is limited due to dense cataract. Modern vitrectomy systems have the capability to perform pars plana vitrectomy as well as anterior segment phacoemulsification. However, many surgeons prefer to use pars plana lensectomy, especially when the crystalline lens is severely subluxated or dislocated, or there is retained lens material in the vitreous cavity. Historically pars plana lensectomy has been performed with the use of a 20 gauge fragmatome, requiring a conjunctival peritomy, a 20 gauge sclerotomy, and suture-closure of wounds [61,62,63,64,65,66,67,68]. Since the advent of smaller gauge transconjunctival vitrectomy, many retina surgeons use a combination of smaller gauge vitrectomy instrumentation and either enlarge one sclerotomy or create a separate sclerotomy for a larger gauge fragmatome instrument [69]. The Constellation Vision System (Alcon) uses a 20 gauge fragmatome, while both the EVA (DORC) and Stellaris PC/Elite (Bauch + Lomb) systems now have the option of a 23 gauge fragmatome for removal of lens material (Fig. 7.22) [70, 71]. The vitreous cutter can also be used for lens removal but this may require a longer time for dense cataract material.
Instrumentation
The evolution of vitrectomy surgery and its applications is closely linked to the development of new instrumentation. While many retinal surgeons were key developers of various different instruments, Steve Charles has been one of the most influential developers of instruments and surgical techniques (Fig. 7.23).
Forceps
Various different forceps have been designed for different purposes in vitreoretinal surgery. Internal limiting membrane (ILM) forceps are designed with a small platform at the tip, which can be used to remove ILM through the pinch-peel technique or in combination with scrapers. Serrated forceps are designed to provide a stronger grip on tissues, for manipulation of thick and heavy membranes, such as those encountered in proliferative vitreoretinopathy or severe proliferative diabetic retinopathy. Micro-textured grasping forceps are designed to provide a strong grip on less thick or heavy membranes, while producing less tissue trauma [27].
Membrane Scrapers
Bausch + Lomb has developed multiple membrane scrapers, including the Tano and variations on this device [72]. The Extendible Diamond Dusted Sweeper (DORC) is a similar membrane scraper to the Tano instrument. The FINESSE Flex Loop (Alcon) is a nitinol flexible extendible loop scraper that can be used to create an edge to lift the ILM or an epiretinal membrane [73]. The force applied to the retina by the can be adjusted based upon whether the loop is partially or fully extended [74].
Scissors
Horizontal scissors are used to cut retinal bands and tractional components near the retinal surface. Illuminated horizontal scissors are available from some manufacturers, which are useful during bimanual surgery and minimize the need for chandelier placement. Vertical scissors can have a sharp anterior edge to optimize close dissection, tissue segmentation, and delamination techniques. Vertical scissors are used in complex proliferative cases with multiplane tractional bands. Curved or angled scissors follow the contour of the eye to minimize retinal trauma and are better for segmentation and delamination [27, 74].
Extrusion Cannulas
Soft-tip extrusion cannulas are useful to allow a more complete removal of fluid by enabling closer approach to the retinal tissue than the cutter. Newer soft-tip cannulas have retractable tips for greater ease with insertion through a valved cannula. Backflush cannulas allow for active and passive aspiration of fluid (not vitreous). Furthermore, the backflush feature can be used if retinal incarceration occurs at the tip and can be used to disperse blood settled on the retina [75, 76].
Endolasers
Endolasers are used in vitreoretinal surgery to perform pan-retinal photocoagulation, laser to the edges of retinal breaks, cauterize bleeding vessels, ablate retinal and choroidal tumors, and perform endophotocyclocoagulation [77]. Early endolasers were straight, but newer endolasers with a curved tip are now available for easier access to the far periphery. Articulating endolasers allow continuously adjustable articulation up to 45° and improves access to the far periphery. The probe is semi-rigid, which makes insertion through a valved cannula easier. Illuminated laser probes are available in curved or extendable forms and can potentially improve peripheral viewing during laser and facilitate simultaneous depression and laser without the help of an assistant or the need for chandelier illumination. Aspirating laser probes provide the capacity for simultaneous endolaser and aspiration, which minimizes the need for instrument exchanges and potentially decreases total surgical time.
Diathermy
The most common uses for diathermy in vitreoretinal surgery is to cauterize bleeding retinal vessels for hemostasis and to create drainage retinotomies. External diathermy application to a leaking sclerotomy has been reported effective in sealing the surgical wound [78,79,80].
Perfluorocarbon Liquid
Stanley Chang (1987) introduced low viscosity fluorocarbons as an intraoperative adjunct during vitreous surgery for retinal detachments (Fig. 7.24) [81]. The high density and specific gravity of perfluorocarbon liquid allows reattachment of the retina and unrolling of retinal folds without having to use operating bed which enabled prone positioning of patients during the surgical repair (Fig. 7.25). Perfluorocarbon liquid can also prevent the need for a drainage retinotomy to drain subretinal fluid. For these reasons, perfluorocarbons have become used in the treatment of giant retinal tears and proliferative vitreoretinopathy. Additionally, the optical clarity of perfluorocarbon liquid allows for surgical manipulation beneath it, such as “floating” crystalline lens fragments off the macula for subsequent lensectomy. Its immiscibility with water provides a clear operating fluid in the setting of intraoperative hemorrhage. Perfluorocarbons are biologically inert, but evidence indicates that they are toxic when retained in the eye for longer periods of time [82]. Despite some concerns of toxicity, some studies have demonstrated benefit from using perfluorocarbon liquids as short term tamponade agents, ranging from 7 days to 3 months, in patients with inferior or complex retinal detachments [83,84,85,86]. Subretinal perfluorocarbon in the fovea is visually significant and generally requires removal.
Subretinal Injections
Subretinal injections are performed for several indications. Subretinal tissue plasminogen activator (tPA) with or without air has been reported to displace submacular hemorrhage [87,88,89,90,91,92,93]. More recently, gene therapy through subretinal delivery of a viral vector has been performed effectively for with specific retinal dystrophies [94,95,96,97]. Luxturna (Voretigene neparvovec-rzyl, Spark Therapeutics Inc., Philadelphia, Pennsylvania, USA) is an FDA approved subretinal gene therapy for patients with inherited retinal disease due to mutations in both copies of the RPE65 gene. Subretinal injection of human embryonic stem cell (HESC) and induced pluripotent stem cell (iPSC)-derived RPE cells/sheets for macular degeneration have been performed in clinical trials [98,99,100,101]. There are multiple reusable and disposable small cannulas (as small as 41 gauge) that are available for subretinal injection through trocars. New instruments are being developed to facilitate subretinal RPE cell sheet delivery [102].
Scleral Buckling
Scleral buckling (SB) can be used to treat primary rhegmatogenous retinal detachments, most commonly in phakic eyes [103]. Scleral buckling involves placement of solid or porous silicone buckling elements—encircling, radial, or both—in order to support equatorial or pre-equatorial breaks and reduce traction from the peripheral vitreous. The elements are either sutured to the sclera or placed through scleral tunnels [104]. Once closure of the retinal breaks is achieved, the retinal pigment epithelium pump removes subretinal fluid resulting in retinal reattachment [105, 106]. The breaks can be sealed with cryopexy and gas tamponade can be used to aid retina reattachment. SB may be combined with PPV. A prospective randomized clinical trial of 681 eyes with medium complexity rhegmatogenous retinal detachments showed that SB showed a benefit with regards to visual improvement in phakic eyes, but PPV had a better anatomic outcome in pseudophakic patients compared to SB [105]. In cases of proliferative vitreoretinopathy, the combination allows support of the vitreous base and the ability to address membranes and/or perform a retinectomy. One retrospective study found the combination of PPV and SB to lead to better outcomes than PPV alone in retinal detachments that were at risk to develop PVR [107].
Numerous intrascleral implants have been used in scleral buckling surgery, including polyethylene, silicone, and gelatin implants. In 1985, episcleral hydrogel implants (MIRAgel, MIRA Inc., Waltham, Massachusetts, USA) were introduced as an alternative to silicone for treatment of rhegmatogenous retinal detachment. The material was thought to have the potential to decrease risk of scleral erosion due to its soft, pliable characteristics. However, after several years, it was discovered that the hydrolytic degradation of the MIRAgel material caused progressive swelling of the explant and subsequent strabismus, ptosis, scleral erosion, conjunctivitis, and infection [108]. These implants are no longer used.
In one study of 728 eyes that underwent scleral buckling, the incidence of erosion was analyzed based upon the type of implant used. The study found that erosion occurred in 62.3% of eyes with polyethylene tubes compared with 3.8% in eyes with solid silicone implants with silicone circling bands. The use of solid silicone implants and circling bands has greatly reduced the issue of implant erosion [109].
Chandelier-assisted SB uses chandelier endoillumination and a wide-angle fundus viewing system in lieu of an indirect ophthalmoscope. The advantages of this technique are better visualization, improved ergonomics, and increased familiarity for predominantly vitrectomy trained surgeons [110]. However, chandelier insertion carries the risk of cataract from lens touch, and new breaks from vitreous traction during eye manipulation [111, 112]. Use of an illuminated scleral depressor is a novel technique to improve localization of retinal breaks. This method uses a 20G light pipe with a bent tip as an illuminated scleral depressor to see the break in greater detail and screen suspect areas [110].
Tamponade Agents
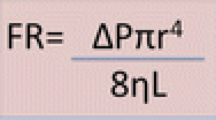
Tamponade agents are used to provide surface tension across retinal breaks in vitrectomy for rhegmatogenous retinal detachment repair. They prevent further fluid flow into the subretinal space until the retinopexy via photocoagulation or cryopexy provides a permanent seal. Gases and silicone oil (SO) are the most commonly used classes of tamponade agents. The use of tamponade agents for the treatment of retinal detachment was first described in 1911 by Joh Ohm who successfully treated two patients with intravitreal sterile air [113]. In 1962, Paul Cibis described the use of liquid silicone for the management of retinal detachment [114]. The use of inert expansile gas sulfur hexafluoride (SF6) was described in 1973 by Edward Norton as a vitreous substitute [115].
Currently, the most common gas tamponades in the US are air, SF6, and perfluoropropane (C3F8) [116]. Air is nonexpansile. SF6 100% expands two times over 1–2 days and C3F8 100% expands about four times over 3–4 days [117]. Small volumes (0.5 cm3 or less) of undiluted gas are generally used for pneumatic retinopexy. Diluted gas to fill the vitreous cavity is typically used for PPV at non-expansile concentrations (SF6 20% and C3F8 14%). Gas tamponade agents resorb spontaneously from the vitreous cavity over an average period of 5–7 days for air, 2 weeks for SF6 20%, and 8 weeks for C3F8 [118].
The Silicone Study was a prospective multicenter randomized clinical trial that compared 1000 centistoke silicone oil to SF6 20% or C3F8 14% in patients with retinal detachment associated with proliferative vitreoretinopathy, which reported that anatomic and visual outcomes after 1 year was significantly better with SO compared to SF6 and not significantly different for SO compared to C3F8 [119]. A 6-year follow up of the Silicone Study reported that, among subjects whose macula was attached at 36 months, there were no significant anatomic or visual outcome differences among SO, SF6, and C3F8 groups [119]. The European Vitreo-Retinal Society (EVRS) Retinal Detachment Study reported no significant difference in failure rate between tamponade with gas versus SO in patients with proliferative vitreoretinopathy [120].
In the USA, the most commonly used viscosities of silicone oils are 1000 and 5000 centistokes [121]. Due to the lower specific gravity of gases (0.001 g/mL) and silicone oils (0.97 g/mL) compared to vitreous (1.005–1.008 g/mL), these tamponade agents float in the vitreous cavity [122]. For this reason, gases and SO provide less effective tamponade for inferior breaks without a full fill of the vitreous cavity. Heavier-than-water tamponades, such as heavy silicone oils and perfluorocarbon liquids, are used as tamponade agents for inferior retinal breaks [123,124,125,126,127]. Heavy silicone oils are available for clinical use in many nations but not the United States.
Postoperative Considerations and Complications
Over the years PPV has evolved with the development of smaller and faster vitrectomy systems. Transconjunctival small-gauge instruments have provided the advantages of decreased operating time, self-sealing scleral wounds, decreased postoperative pain and inflammation, decreased astigmatism, and faster visual recovery over traditional 20 gauge instruments [128,129,130,131,132]. PPV and SB are now typically outpatient procedures with follow up 1 day after surgery. However, alternative postoperative visits on the same day as surgery and 3 or more days after surgery have been reported [133, 134].
Overall, PPV has one of the lowest rates of endophthalmitis among intraocular surgical procedures [135]. As small-gauge transconjunctival PPV gained popularity, concerns arose about increased rates of endophthalmitis with 25 gauge transconjunctival sutureless vitrectomy. A retrospective study in 2007 examined 8600 PPV patients and reported a 12-fold higher incidence of endophthalmitis in 25 gauge PPV compared to 20 gauge PPV [136]. However, later studies reported no significant difference in endophthalmitis rates between 20 gauge PPV and small incision vitrectomy [137, 138].
With regards to post-operative retinal detachment complications, a retrospective study of 2432 vitrectomies reported a similar incidence of post-surgical retinal detachment after sutureless 23 gauge and 25 gauge PPV compared to 20 gauge PPV [139]. Another retrospective study of 4274 vitrectomies comparing intraoperative complications of 23 gauge versus 20 gauge PPV showed that 23 gauge PPV had a lower risk of choroidal hemorrhage and iatrogenic retinal tears compared to 20 gauge PPV, especially for eyes with rhegmatogenous retinal detachment [140].
Other post-operative complications of vitrectomy include cataract progression, cystoid macular edema, hypotony, and sympathetic ophthalmia [141, 142].
Future Advancements in Vitreo-Retinal Surgery
Recent developments in vitreo-retinal surgery have led to advances in surgeon capabilities, visual outcomes, and patient safety. Robotic vitreo-retinal surgery is a rapidly emerging technology within this domain. Early robotic vitreo-retinal surgical techniques have been aimed at tremor cancellation, improved precision, enhanced dexterity, force sensing and micron-scale distance sensing [143,144,145,146,147]. The use of robotics in vitreo-retinal surgery has been limited by the lack of broad clinical experience among potential users and challenges to implementation.
Four-dimensional (4-D) OCT imaging has been introduced recently for use intraoperatively to provide enhanced visualization of volumetric tissue deformation. It has been used in vitreo-retinal surgical cases for macular hold, ERM, myopic foveal schisis, diabetic macular edema, and retinal detachment. 4-D OCT imaging has the potential to provide enhanced intraoperative visualization from multiple perspectives, precise determination of instrument distance from the retina, and visualization of retinal contour deformation during and after surgical manipulation. This technology is presently limited by image quality and resolution [148].
Summary
Vitreoretinal surgical techniques have evolved in the last 50 years largely due to the development and evolution of PPV. Developments include smaller gauge instrumentation, faster cut speeds, enhanced illumination techniques, microscopes, and perfluorocarbon liquids. These advancements have improved the safety and efficacy of vitrectomy and allowed surgeons to more effectively treat a wide variety of conditions, including complications of diabetic retinopathy, macular holes, and retinal detachments.
References
Dodo T. Diapupillary resection of vitreous opacity. Nippon Ganka Gakkai Zasshi. 1955;59:1737–45.
Dodo T, Okuzawa Y, Baba N. [Trans-pupillary resection of vitreous body opacity]. Ganka. 1969;11(1):38–44.
Kasner D, Miller GR, Taylor WH, Sever RJ, Norton EW. Surgical treatment of amyloidosis of the vitreous. Trans Am Acad Ophthalmol Otolaryngol. 1968;72(3):410–8.
Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971;75(4):813–20.
Machemer R. Reminiscences after 25 years of pars plana vitrectomy. Am J Ophthalmol. 1995;119(4):505–10.
Machemer R, Parel JM, Buettner H. A new concept for vitreous surgery. I. Instrumentation. Am J Ophthalmol. 1972;73(1):1–7.
Parel JM, Machemer R, Aumayr W. A new concept for vitreous surgery. 4. Improvements in instrumentation and illumination. Am J Ophthalmol. 1974;77(1):6–12.
Machemer R. A new concept for vitreous surgery. 2. Surgical technique and complications. Am J Ophthalmol. 1972;74(6):1022–33.
Peyman GA, Dodich NA. Experimental vitrectomy: instrumentation and surgical technique. Arch Ophthalmol. 1971;86(5):548–51.
O’Malley C, Heintz RM. Vitrectomy with an alternative instrument system. Ann Ophthalmol. 1975;7(4):585–8, 591–4.
Machemer R, Hickingbotham D. The three-port microcannular system for closed vitrectomy. Am J Ophthalmol. 1985;100(4):590–2.
de Juan E, Hickingbotham D. Refinements in microinstrumentation for vitreous surgery. Am J Ophthalmol. 1990;109(2):218–20.
Peyman GA. A miniaturized vitrectomy system for vitreous and retinal biopsy. Can J Ophthalmol. 1990;25(6):285–6.
Fujii GY, De Juan E, Humayun MS, Pieramici DJ, Chang TS, Awh C, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–12; discussion 1813.
Fujii GY, De Juan E, Humayun MS, Chang TS, Pieramici DJ, Barnes A, et al. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology. 2002;109(10):1814–20.
Eckardt C. Transconjunctival sutureless 23-gauge vitrectomy. Retina. 2005;25(2):208–11.
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y. A 27-gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology. 2010;117(1):93–102.e2.
Machemer R, Norton EW. A new concept for vitreous surgery. 3. Indications and results. Am J Ophthalmol. 1972;74(6):1034–56.
Wilson D, Barr CC. Outpatient and abbreviated hospitalization for vitreoretinal surgery. Ophthalmic Surg. 1990;21(2):119–22.
Newsom RS, Wainwright AC, Canning CR. Local anaesthesia for 1221 vitreoretinal procedures. Br J Ophthalmol. 2001;85(2):225–7.
Huang JJ, Fogel S, Leavell M. Cost analysis in vitrectomy: monitored anesthesia care and general anesthesia. AANA J. 2001;69(2):111–3.
Wong DH. Regional anaesthesia for intraocular surgery. Can J Anaesth. 1993;40(7):635–57.
Celiker H, Karabas L, Sahin O. A comparison of topical or retrobulbar anesthesia for 23-gauge posterior vitrectomy. J Ophthalmol. 2014;2014:237028.
Trujillo-Sanchez GP, Gonzalez-De La Rosa A, Navarro-Partida J, Haro-Morlett L, Altamirano-Vallejo JC, Santos A. Feasibility and safety of vitrectomy under topical anesthesia in an office-based setting. Indian J Ophthalmol. 2018;66(8):1136–40.
Narendran V, Kothari AR, editors. Vitreoretinal surgery systems. In: Principles and practice of vitreoretinal surgery. 1st ed. Philadelphia: Jaypee Brothers Medical Publishers Ltd; 2014. p. 53–6.
Lai TYY. Machines and cutters: Stellaris PC. Dev Ophthalmol. 2014;54:8–16.
Charles S, Calzada J, Wood B, editors. 25-Gauge vitrectomy. In: Vitreous microsurgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 103–11.
Mohamed S, Claes C, Tsang CW. Review of small gauge vitrectomy: progress and innovations. J Ophthalmol. 2017;2017:6285869.
Nagpal M, Paranjpe G, Jain P, Videkar R. Advances in small-gauge vitrectomy. Taiwan J Ophthalmol. 2012;2(1):6.
Osawa S, Oshima Y. 27-Gauge vitrectomy. Dev Ophthalmol. 2014;54:54–62.
Oellers P, Stinnett S, Hahn P. Valved versus nonvalved cannula small-gauge pars plana vitrectomy for repair of retinal detachments with Grade C proliferative vitreoretinopathy. Clin Ophthalmol. 2016;10:1001–6.
Oellers P, Stinnett S, Mruthyunjaya P, Hahn P. Small-gauge valved versus nonvalved cannula pars plana vitrectomy for retinal detachment repair. Retina. 2016;36(4):744–9.
Littmann H. [A new surgical microscope]. Klin Monatsblatter Augenheilkd Augenarztliche Fortbild. 1954;124(4):473–6.
Parel JM, Machemer R, Aumayr W. A new concept for vitreous surgery. 5. An automated operating microscope. Am J Ophthalmol. 1974;77(2):161–8.
Hattenbach L-O, Framme C, Junker B, Pielen A, Agostini H, Maier M. [Intraoperative real-time OCT in macular surgery]. Ophthalmologe. 2016;113(8):656–62.
Landers MB, Stefánsson E, Wolbarsht ML. The optics of vitreous surgery. Am J Ophthalmol. 1981;91(5):611–4.
Bovey EH, Gonvers M. A new device for noncontact wide-angle viewing of the fundus during vitrectomy. Arch Ophthalmol. 1995;113(12):1572–3.
Chalam KV, Shah VA. Optics of wide-angle panoramic viewing system-assisted vitreous surgery. Surv Ophthalmol. 2004;49(4):437–45.
Inoue M. Wide-angle viewing system. Dev Ophthalmol. 2014;54:87–91.
Chihara T, Kita M. New type of antidrying lens for vitreous surgery with a noncontact wide-angle viewing system. Clin Ophthalmol. 2013;7:353–5.
Ohji M, Tada E, Futamura H. Combining a contact lens and wide-angle viewing system for a wider fundus view. Retina. 2011;31(9):1958–60.
Ohno H. Combined use of high-reflective index vitrectomy meniscus contact lens and a noncontact wide-angle viewing system in vitreous surgery. Clin Ophthalmol. 2011;5:1109–11.
Shah VA, Chalam KV. Self-stabilizing wide-angle contact lens for vitreous surgery. Retina. 2003;23(5):667–9.
Mateo C, Burés-Jelstrup A. Contact versus noncontact wide-field viewing systems: why not have the best of both worlds? Retina. 2018;38(4):854–6.
Adam MK, Thornton S, Regillo CD, Park C, Ho AC, Hsu J. Minimal endoillumination levels and display luminous emittance during three-dimensional heads-up vitreoretinal surgery. Retina. 2017;37(9):1746–9.
Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina. 2016;36(1):137–47.
Machemer R. The development of pars plana vitrectomy: a personal account. Graefes Arch Clin Exp Ophthalmol. 1995;233(8):453–68.
Peyman GA. Improved vitrectomy illumination system. Am J Ophthalmol. 1976;81(1):99–100.
Sakaguchi H, Oshima Y. Considering the illumination choices in vitreoretinal surgery. Retin Physician. 2012;9:26–31.
Chow DR. The evolution of endoillumination. Dev Ophthalmol. 2014;54:77–86.
Koelbl PS, Lingenfelder C, Spraul CW, Kampmeier J, Koch FH, Kim YK, et al. An intraocular micro light-emitting diode device for endo-illumination during pars plana vitrectomy. Eur J Ophthalmol. 2019;29(1):75–81. https://doi.org/10.1177/1120672118757618.
Henrich PB, Valmaggia C, Lang C, Cattin PC. The price for reduced light toxicity: do endoilluminator spectral filters decrease color contrast during Brilliant Blue G-assisted chromovitrectomy? Graefes Arch Clin Exp Ophthalmol. 2014;252(3):367–74.
Witmer MT, Dugel PU. Machines and cutters: constellation. In: Oh H, Oshima Y, editors. Microincision vitrectomy surgery: emerging techniques and technology. New York: Karger Medical and Scientific Publishers; 2014. p. 1–7.
Lai TYY. Machines and cutters: Stellaris PC. In: Oh H, Oshima Y, editors. Microincision vitrectomy surgery: emerging techniques and technology. New York: Karger Medical and Scientific Publishers; 2014. p. 8–16.
Morales-Canton V, Kawakami-Campos PA. Machines and cutters: VersaVIT—potential and perspectives of office-based vitrectomy. In: Oh H, Oshima Y, editors. Microincision vitrectomy surgery: emerging techniques and technology. New York: Karger Medical and Scientific Publishers; 2014. p. 17–22.
Seider MI, Nomides REK, Hahn P, Mruthyunjaya P, Mahmoud TH. Scleral buckling with chandelier illumination. J Ophthalmic Vis Res. 2016;11(3):304–9.
Rodrigues EB, Meyer CH, Kroll P. Chromovitrectomy: a new field in vitreoretinal surgery. Graefes Arch Clin Exp Ophthalmol. 2005;243(4):291–3.
Kadonosono K, Itoh N, Uchio E, Nakamura S, Ohno S. Staining of internal limiting membrane in macular hole surgery. Arch Ophthalmol. 2000;118(8):1116–8.
Grisanti S, Altvater A, Peters S. Safety parameters for indocyanine green in vitreoretinal surgery. Dev Ophthalmol. 2008;42:43–68.
Al-Halafi AM. Chromovitrectomy: update. Saudi J Ophthalmol. 2013;27(4):271–6.
Margherio RR, Margherio AR, Pendergast SD, Williams GA, Garretson BR, Strong LE, et al. Vitrectomy for retained lens fragments after phacoemulsification. Ophthalmology. 1997;104(9):1426–32.
Ho SF, Zaman A. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments after phacoemulsification. J Cataract Refract Surg. 2007;33(12):2106–10.
Hansson LJ, Larsson J. Vitrectomy for retained lens fragments in the vitreous after phacoemulsification. J Cataract Refract Surg. 2002;28(6):1007–11.
Borne MJ, Tasman W, Regillo C, Malecha M, Sarin L. Outcomes of vitrectomy for retained lens fragments. Ophthalmology. 1996;103(6):971–6.
Scott IU, Flynn HW Jr, Smiddy WE, Murray TG, Moore JK, Lemus DR, et al. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments. Ophthalmology. 2003;110(8):1567–72.
Ho LY, Doft BH, Wang L, Bunker CH. Clinical predictors and outcomes of pars plana vitrectomy for retained lens material after cataract extraction. Am J Ophthalmol. 2009;147(4):587–594.e1.
Kadonosono K, Yamakawa T, Uchio E, Yanagi Y, Tamaki Y, Araie M. Comparison of visual function after epiretinal membrane removal by 20-gauge and 25-gauge vitrectomy. Am J Ophthalmol. 2006;142(3):513–5.
Chang C-J, Chang Y-H, Chiang S-Y, Lin L-T. Comparison of clear corneal phacoemulsification combined with 25-gauge transconjunctival sutureless vitrectomy and standard 20-gauge vitrectomy for patients with cataract and vitreoretinal diseases. J Cataract Refract Surg. 2005;31(6):1198–207.
Cho M, Chan RP. 23-gauge pars plana vitrectomy for management of posteriorly dislocated crystalline lens. Clin Ophthalmol. 2011;5:1737–43.
Arevalo JF, Berrocal MH, Arias JD, Banaee T. Minimally invasive vitreoretinal surgery: is sutureless vitrectomy the future of vitreoretinal surgery? J Ophthalmic Vis Res. 2011;6(2):136–44.
Shah GK, Ho VY. Vitrectomy platforms go to the next level. Retina Spec [Internet]. 2016. http://www.retina-specialist.com/article/noninfectious-uveitis-enriching-our-toolbox-1. [Cited 2018 Sept 17].
Kuhn F, Mester V, Berta A. The Tano Diamond Dusted Membrane Scraper: indications and contraindications. Acta Ophthalmol Scand. 1998;76(6):754–5.
Hsu J. Nitinol flex loop-assisted retrieval and sutureless intrascleral refixation of a dislocated intraocular lens implant. Retin Cases Brief Rep. 2018; E-pub before print.
Charles S, Calzada J, Wood B, editors. General posterior segment techniques. In: Vitreous microsurgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 45–75.
Villegas V, Murray T. Know your retinal surgery toolbox. Retin Physician. 2018;15:24–9.
Charles S, Calzada J, Wood B, editors. Vitrectomy for retinal detachment. In: Vitreous microsurgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 135–8.
Kuhn F. Endolaser. In: Kuhn F, editor. Vitreoretinal surgery: strategies and tactics [Internet]. Cham: Springer International Publishing; 2016. p. 263–76. https://doi.org/10.1007/978-3-319-19479-0_30. [Cited 2018 Sept 24].
Barak Y, Lee ES, Schaal S. Sealing effect of external diathermy on leaking sclerotomies after small-gauge vitrectomy: a clinicopathological report. JAMA Ophthalmol. 2014;132(7):891–2.
Reibaldi M, Longo A, Reibaldi A, Avitabile T, Pulvirenti A, Lippolis G, et al. Diathermy of leaking sclerotomies after 23-gauge transconjunctival pars plana vitrectomy: a prospective study. Retina. 2013;33(5):939–45.
Jusufbegovic D, Ozkok A, Schaal S. Intraoperative optical coherence tomography validates the immediate efficacy of external diathermy in sealing 25-gauge sclerotomy wounds. Retina. 2017;37(2):402–4.
Chang S. Low viscosity liquid fluorochemicals in vitreous surgery. Am J Ophthalmol. 1987;103(1):38–43.
Georgalas I, Ladas I, Tservakis I, Taliantzis S, Gotzaridis E, Papaconstantinou D, et al. Perfluorocarbon liquids in vitreoretinal surgery: a review of applications and toxicity. Cutan Ocul Toxicol. 2011;30(4):251–62.
Randolph JC, Diaz RI, Sigler EJ, Calzada JI, Charles S. 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for the repair of giant retinal tears. Graefes Arch Clin Exp Ophthalmol. 2016;254(2):253–7.
Eiger-Moscovich M, Gershoni A, Axer-Siegel R, Weinberger D, Ehrlich R. Short-term vitreoretinal tamponade with heavy liquid following surgery for giant retinal tear. Curr Eye Res. 2017;42(7):1074–8.
Zhang Z, Wei Y, Jiang X, Zhang S. Surgical outcomes of 27-gauge pars plana vitrectomy with short-term postoperative tamponade of perfluorocarbon liquid for repair of giant retinal tears. Int Ophthalmol. 2018;38(4):1505–13.
Mikhail MA, Mangioris G, Best RM, McGimpsey S, Chan WC. Management of giant retinal tears with vitrectomy and perfluorocarbon liquid postoperatively as a short-term tamponade. Eye. 2017;31(9):1290–5.
Kamei M, Tano Y. Tissue plasminogen activator-assisted vitrectomy: surgical drainage of submacular hemorrhage. Dev Ophthalmol. 2009;44:82–8.
Vander JF. Tissue plasminogen activator irrigation to facilitate removal of subretinal hemorrhage during vitrectomy. Ophthalmic Surg. 1992;23(5):361–3.
Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol. 1996;121(3):267–75.
Moriarty AP, McAllister IL, Constable IJ. Initial clinical experience with tissue plasminogen activator (tPA) assisted removal of submacular haemorrhage. Eye. 1995;9(Pt 5):582–8.
Moisseiev E, Ben Ami T, Barak A. Vitrectomy and subretinal injection of tissue plasminogen activator for large submacular hemorrhage secondary to AMD. Eur J Ophthalmol. 2014;24(6):925–31.
Peyman GA, Nelson NC, Alturki W, Blinder KJ, Paris CL, Desai UR, et al. Tissue plasminogen activating factor assisted removal of subretinal hemorrhage. Ophthalmic Surg. 1991;22(10):575–82.
Lim JI, Drews-Botsch C, Sternberg P, Capone A, Aaberg TM. Submacular hemorrhage removal. Ophthalmology. 1995;102(9):1393–9.
Ghazi NG, Abboud EB, Nowilaty SR, Alkuraya H, Alhommadi A, Cai H, et al. Treatment of retinitis pigmentosa due to MERTK mutations by ocular subretinal injection of adeno-associated virus gene vector: results of a phase I trial. Hum Genet. 2016;135(3):327–43.
Testa F, Maguire AM, Rossi S, Pierce EA, Melillo P, Marshall K, et al. Three-year follow-up after unilateral subretinal delivery of adeno-associated virus in patients with Leber congenital Amaurosis type 2. Ophthalmology. 2013;120(6):1283–91.
Mühlfriedel R, Michalakis S, Garcia Garrido M, Biel M, Seeliger MW. Optimized technique for subretinal injections in mice. Methods Mol Biol. 2013;935:343–9.
Ikeda Y, Yonemitsu Y, Miyazaki M, Kohno R-I, Murakami Y, Murata T, et al. Stable retinal gene expression in nonhuman primates via subretinal injection of SIVagm-based lentiviral vectors. Hum Gene Ther. 2009;20(6):573–9.
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385(9967):509–16.
da Cruz L, Fynes K, Georgiadis O, Kerby J, Luo YH, Ahmado A, et al. Phase 1 clinical study of an embryonic stem cell–derived retinal pigment epithelium patch in age-related macular degeneration. Nat Biotechnol. 2018;36(4):328.
Mandai M, Watanabe A, Kurimoto Y, Hirami Y, Morinaga C, Daimon T, et al. Autologous induced stem-cell–derived retinal cells for macular degeneration. N Engl J Med. 2017;376(11):1038–46.
Kashani AH, Lebkowski JS, Rahhal FM, Avery RL, Salehi-Had H, Dang W, et al. A bioengineered retinal pigment epithelial monolayer for advanced, dry age-related macular degeneration. Sci Transl Med. 2018;10(435):eaao4097.
Kamao H, Mandai M, Okamoto S, Sakai N, Suga A, Sugita S, et al. Characterization of human induced pluripotent stem cell-derived retinal pigment epithelium cell sheets aiming for clinical application. Stem Cell Rep. 2014;2(2):205–18.
Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51(1):15–31.
Gomaa AR, Elbaha SM. Applying sutureless encircling number 41 band and transscleral chandelier-assisted laser retinopexy for scleral buckling procedure. J Ophthalmol. 2017;2017:4671305.
Heimann H, Hellmich M, Bornfeld N, Bartz-Schmidt KU, Hilgers RD, Foerster MH. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment (SPR Study): design issues and implications. SPR Study report no. 1. Graefes Arch Clin Exp Ophthalmol. 2001;239(8):567–74.
Foster WJ, Dowla N, Joshi SY, Nikolaou M. The fluid mechanics of scleral buckling surgery for the repair of retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2010;248(1):31–6.
Storey P, Alshareef R, Khuthaila M, London N, Leiby B, DeCroos C, et al. Pars plana vitrectomy and scleral buckle versus pars plana vitrectomy alone for patients with rhegmatogenous retinal detachment at high risk for proliferative vitreoretinopathy. Retina. 2014;34(10):1945–51.
Crama N, Klevering BJ. The removal of hydrogel explants: an analysis of 467 consecutive cases. Ophthalmology. 2016;123(1):32–8.
Yoshizumi MO, Friberg T. Erosion of implants in retinal detachment surgery. Ann Ophthalmol. 1983;15(5):430–4.
Shanmugam PM, Ramanjulu R, Mishra KCD, Sagar P. Novel techniques in scleral buckling. Indian J Ophthalmol. 2018;66(7):909–15.
Hu Y, Si S, Xu K, Chen H, Han L, Wang X, et al. Outcomes of scleral buckling using chandelier endoillumination. Acta Ophthalmol (Copenh). 2017;95(6):591–4.
Imai H, Tagami M, Azumi A. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol. 2015;9:2103–7.
Ohm J. Über die Behandlung der Netzhautablösung durch operative Entleerung der subretinalen Flüssigkeit und Einspritzung von Luft in den Glaskörper [On the treatment of retinal detachment by surgical evacuation of subretinal fluid and injection of air into the vitreous]. Albrecht Von Graefes Arch Für Ophthalmol. 1911;79(3):442–50.
Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol. 1962;68:590–9.
Norton EW. Intraocular gas in the management of selected retinal detachments. Trans Am Acad Ophthalmol Otolaryngol. 1973;77(2):OP85–98.
Mohamed S, Lai TY. Intraocular gas in vitreoretinal surgery. Hong Kong J Ophthalmol. 2010;14(1):8–13.
Kreissig I. The perfluorocarbon gases. In: A practical guide to minimal surgery for retinal detachment. 1st ed. Stuttgart: Thieme; 2000. p. 129–32.
Williamson TH. Principles of internal tamponade. In: Vitreoretinal surgery [Internet]. 2nd ed. Berlin: Springer; 2013. p. 61–87. //www.springer.com/us/book/9783642318719. [Cited 2018 Sept 16].
Abrams GW, Azen SP, McCuen BW, Flynn HW, Lai MY, Ryan SJ. Vitrectomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy: results of additional and long-term follow-up. Silicone Study report 11. Arch Ophthalmol. 1997;115(3):335–44.
Adelman RA, Parnes AJ, Sipperley JO, Ducournau D, European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of complex retinal detachments: the European vitreo-retinal society retinal detachment study report 2. Ophthalmology. 2013;120(9):1809–13.
Foster WJ. Vitreous substitutes. Expert Rev Ophthalmol. 2008;3(2):211–8.
Cazabon S, Hillier RJ, Wong D. Heavy silicone oil: a “novel” intraocular tamponade agent. Optom Vis Sci. 2011;88(6):772–5.
Rizzo S, Romagnoli MC, Genovesi-Ebert F, Belting C. Surgical results of heavy silicone oil HWS-45 3000 as internal tamponade for inferior retinal detachment with PVR: a pilot study. Graefes Arch Clin Exp Ophthalmol. 2011;249(3):361–7.
Er H. Primary heavy silicone oil usage in inferior rhegmatogenous retinal detachment. Ophthalmologica. 2010;224(2):122–5.
Levasseur SD, Schendel S, Machuck RWA, Dhanda D. High-density silicone oil Densiron-68 as an intraocular tamponade for primary inferior retinal detachments. Retina. 2013;33(3):627–33.
Reza AT. Postoperative Perfluro-N-Octane tamponade for complex retinal detachment surgery. Bangladesh Med Res Counc Bull. 2014;40(2):63–9.
Sigler EJ, Randolph JC, Calzada JI, Charles S. Pars plana vitrectomy with medium-term postoperative perfluoro-N-octane for recurrent inferior retinal detachment complicated by advanced proliferative vitreoretinopathy. Retina. 2013;33(4):791–7.
Rizzo S, Genovesi-Ebert F, Murri S, Belting C, Vento A, Cresti F, et al. 25-gauge, sutureless vitrectomy and standard 20-gauge pars plana vitrectomy in idiopathic epiretinal membrane surgery: a comparative pilot study. Graefes Arch Clin Exp Ophthalmol. 2006;244(4):472–9.
Khan MA, Kuley A, Riemann CD, Berrocal MH, Lakhanpal RR, Hsu J, et al. Long-term visual outcomes and safety profile of 27-gauge pars plana vitrectomy for posterior segment disease. Ophthalmology. 2018;125(3):423–31.
Tayyab H, Khan AA, Sadiq MAA, Karamat I. Comparison of 23 gauge transconjunctival releasable suture vitrectomy with standard 20 gauge vitrectomy. Pak J Med Sci. 2018;34(2):328–32.
Xia F, Jiang Y-Q. Clinical outcomes of 23-gauge vitrectomy may be better than 20-gauge vitrectomy for retinal detachment repair. Mol Vis. 2015;21:893–900.
Ho J, Grabowska A, Ugarte M, Muqit MM. A comparison of 23-gauge and 20-gauge vitrectomy for proliferative sickle cell retinopathy—clinical outcomes and surgical management. Eye (Lond). 2018;32(9):1449–54.
Ho VY, Shah GK. Short-and long-term outcomes of vitreoretinal surgeries with deferred first postoperative visits at day 3 or later. J Vitreoretinal Dis. 2017;1(2):126–32.
Ringeisen AL, Parke DW. Reconsidering the postoperative day 0 visit for retina surgery. Ophthalmic Surg Lasers Imaging Retina. 2018;49(9):e52–6.
Rahmani S, Eliott D. Postoperative endophthalmitis: a review of risk factors, prophylaxis, incidence, microbiology, treatment, and outcomes. Semin Ophthalmol. 2018;33(1):95–101.
Kunimoto DY, Kaiser RS, Wills Eye Retina Service. Incidence of endophthalmitis after 20- and 25-gauge vitrectomy. Ophthalmology. 2007;114(12):2133–7.
Scott IU, Flynn HW Jr, Acar N, Dev S, Shaikh S, Mittra RA, et al. Incidence of endophthalmitis after 20-gauge vs 23-gauge vs 25-gauge pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2011;249(3):377–80.
Wu L, Berrocal MH, Arévalo JF, Carpentier C, Rodriguez FJ, Alezzandrini A, et al. Endophthalmitis after pars plana vitrectomy: results of the Pan American Collaborative Retina Study Group. Retina. 2011;31(4):673–8.
Rizzo S, Belting C, Genovesi-Ebert F, di Bartolo E. Incidence of retinal detachment after small-incision, sutureless pars plana vitrectomy compared with conventional 20-gauge vitrectomy in macular hole and epiretinal membrane surgery. Retina. 2010;30(7):1065–71.
Neffendorf JE, Gupta B, Williamson TH. Intraoperative complications of patients undergoing small-gauge and 20-gauge vitrectomy: a database study of 4,274 procedures. Eur J Ophthalmol. 2017;27(2):226–30.
Gass JD. Sympathetic ophthalmia following vitrectomy. Am J Ophthalmol. 1982;93(5):552–8.
Gupta OPI, Weichel ED, Regillo CD, Fineman MS, Kaiser RS, Ho AC, et al. Postoperative complications associated with 25-gauge pars plana vitrectomy. Ophthalmic Surg Lasers Imaging. 2007;38(4):270–5.
Roizenblatt M, Edwards TL, Gehlbach PL. Robot-assisted vitreoretinal surgery: current perspectives. Robot Surg. 2018;5:1–11.
Gonenc B, Handa J, Gehlbach P, Taylor RH, Iordachita I. A comparative study for robot assisted vitreoretinal surgery: micron vs. the steady-hand robot. IEEE Int Conf Robot Autom. 2013;2013:4832–7.
Balicki M, Xia T, Jung MY, Deguet A, Vagvolgyi B, Kazanzides P, Taylor R. Prototyping a hybrid cooperative and tele-robotic surgical system for retinal microsurgery. MIDAS J. 2011; E-pub Dec 2011.
Gonenc B, Handa J, Gehlbach P, Taylor RH, Iordachita I. Design of 3-DOF force sensing micro-forceps for robot assisted vitreoretinal surgery. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:5686–9.
Edwards TL, Xue K, Meenink HCM, Beelen MJ, Naus GJL, Simunovic MP, et al. First-in-human study of the safety and viability of intraocular robotic surgery. Nat Biomed Eng. 2018;2:649–56.
Carrasco-Zevallos OM, Keller B, Viehland C, Shen L, Seider MI, Izatt JA, et al. Optical coherence tomography for retinal surgery: perioperative analysis to real-time four-dimensional image-guided surgery. Invest Ophthalmol Vis Sci. 2016;57(9):OCT37–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Idrees, S., Kuriyan, A.E., Schwartz, S.G., Parel, JM., Flynn, H.W. (2020). Recent Developments in Vitreo-Retinal Surgery. In: Grzybowski, A. (eds) Current Concepts in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-030-25389-9_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-25389-9_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25388-2
Online ISBN: 978-3-030-25389-9
eBook Packages: MedicineMedicine (R0)