Abstract
In this chapter we describe a standardized approach for robotic colonic resections from the splenic flexure to the peritoneal reflection (i.e., left colectomy) for benign and malignant diseases. Advantages and pitfalls of the robotic technique are highlighted. Potential intraoperative difficulties and complications are also addressed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction and Rationale
It is widely accepted that compared with open operations, minimally invasive abdominal surgery is superior in nearly every aspect: reduced pain, faster return of bowel function, reduced length of hospital stay, lower overall cost of care, improved cosmesis, lower hernia rates, and quicker return to work [1]. This holds true for most laparoscopic operations and is therefore the reason that the laparoscopy has become the gold standard for a large part of elective and emergent operations. The same clinical benefits are seen in patients undergoing minimally invasive colorectal operations but with the added benefit of equivalent oncologic benefits and a trend towards improved cancer-related survival in at least one randomized controlled trial (RCT) comparing open and laparoscopic resection for colon cancer [2]. However, despite the known benefits and widespread availability of laparoscopy [3], adoption has remained relatively low, with rates of laparoscopic colectomy reaching 55.4% based on the most recent data from the National Inpatient Sample database [4, 5]. The adoption is low even considering an increase in worldwide prevalance of left-sided colonic pathology [6]. Slow adoption can be partly explained by the complexity of colorectal operations, which require control and ligation of one or more major vascular pedicles, mastery of the relevant anatomical landmarks, careful dissection and manipulation of tumor specimens, and familiarity with all the steps required to construct an adequate anastomosis.
Continued advances in minimally invasive technologies have led to the development of robotic platforms in the hope that the ergonomic benefits of a robotic platform, combined with wristed instruments and 3D visualization, would help mitigate some the technical challenges of laparoscopy, thereby increasing adoption of minimally invasive surgery (MIS) while reducing conversion rates. This rise in pathology has likewise encouraged surgeons to incorporate instruments and technology to bridge the gaps that laparoscopic surgery was unable to fill.
This chapter will describe various techniques and strategies for robotic left-sided colonic resections, with emphasis on best practices based on tumor location and tumor pathology.
Indications and Contradictions
There are no absolute contraindications to a robotic approach for left-sided colorectal resection. In fact, in recent years, absolute contraindications to minimally invasive approaches in “high-risk” patients have been challenged, such as prior abdominal surgery and obesity [7]. Authors now advocate for the use of minimally invasive surgery when possible, even in “high-risk” patients based on the benefits derived from reduced physiologic stress and postoperative morbidity. Similarly, robotic colorectal operations may also be offered to all patients undergoing left-sided colon resections. Relative contraindications to robotic surgery include the following:
-
Hemodynamic instability
-
Inability to tolerate insufflations: e.g., due to cardiopulmonary disease
-
Inability to access the abdominal cavity safely: e.g., intense adhesive burden from previous surgery, intraperitoneal mesh placement
-
Inability to adequately insufflate: e.g., abdominoplasty, bowel obstruction causing over distension of bowel
-
Tumor-related issues: e.g., size of tumor larger than incision required for laparotomy, local extension into adjacent structures that would require a multidisciplinary approach where other surgical teams are not proficient in reconstructive procedures using a minimally invasive approach
Principles and Quality Benchmarks
The critical steps to be completed during minimally invasive resection of malignant and benign left-sided pathology are outlined below.
Malignant Diseases
-
1.
Dissection along embryologic planes of the parietal and visceral peritoneal layer to the root of the mesentery and avoiding retroperitoneal structures and the left ureter (complete mesocolic excision)
-
2.
Identification and dissection of the inferior mesenteric artery (IMA) with selective ligation of the IMA at its origin or just distal to the junction of the left colic artery resulting in adequate lymph node yield for malignant diseases (minimum of 12 lymph nodes)
-
3.
Adequate proximal and distal tumoral margins of healthy, non-affected colon of 5–10 cm
-
4.
Adequate colonic mobilization with technical ability for complete splenic flexure mobilization and high ligation of the inferior mesenteric vein (IMV) if necessary for a tension-free anastomosis
Benign Diseases
-
1.
Definition of the appropriate extent of the resection as defined by the nature of the disease: for example, for a resection in diverticulitis cases, it is necessary to precisely identify and divide the colon at the rectosigmoid junction (coalescence of the teniae) to avoid retaining distal sigmoid colon with an increased risk of recurrent diverticulitis.
-
2.
Proximal division of the colon where the bowel is healthy.
-
3.
Definition of an appropriate degree of devascularization: Unless there is strong confirmation about the benign nature of the disease, the same oncological vascular dissection should be performed as for known malignant disease; if the disease is confirmed to benign, a less aggressive and blood supply-sparing dissection may be sufficient as the lymph node harvest is not of relevance.
Preoperative Planning, Patient Workup, and Optimization
Patients with left-sided pathologies are – like for any major surgical intervention – evaluated for relevant comorbidities and optimized accordingly. Special attention is paid to obese patients, where a thorough pulmonary evaluation is needed to rule out underlying diseases such as chronic obstructive pulmonary disease which can be associated with difficulties with ventilation during prolonged periods in Trendelenburg position.
Computer tomography of the chest, abdomen, and pelvis is obtained for tumor staging. It further provides important strategic information about pathology itself as well as about the configuration of the colon, its redundancy, and the level of the splenic flexure.
Preoperative complete colonoscopy or alternative colon evaluation is necessary to exclude secondary pathology and possible for tattooing if the tumor location is not otherwise reliably defined.
Individual hospital and institutional specific enhanced recovery protocols determine further preoperative optimization . These frequently include prehabilitation, nutritional supplements, patient education, and bowel preparation with oral antibiotics.
Operative Setup
Patient Positioning
The patient is placed in the modified lithotomy position with both arms tucked in neutral position along the torso. The legs are placed in stirrups such that they can be moved from a 0-degree angle at the hip level to an elevated position when access to the anus is needed.
To minimize sliding when the patient is placed in steep Trendelenburg position, an anti-sliding pad should be used. Alternatively, a beanbag with respective external stabilizers may be helpful. Shoulder brackets should be used with caution to avoid damage to the brachial plexus. The patient is further secured to the table by means of safety straps across the upper chest. Testing the various positions before prepping the patient may be helpful to identify instabilities.
Room Setup
It is important to optimize the limited space and arrange the various items in the room , such as operating table, towers, robot, accessory equipment, room lights, anesthesia equipment, sterile trays, colonoscopy cart, etc. The arrangement needs coordination in such a fashion that adequate space is available to access the robotic arms and execute an unrestricted and sterile exchange of instruments once the patient is prepped and draped.
The assistant surgeon will be on the right side of the patient and can help with instrument changes, retraction, suctioning, and irrigation as needed. The scrub tech is also on the right side next to the assistant surgeon.
Operative Technique
Trocar Placement
Planning the trocar outline should take into consideration the extent of the planned colon dissection, the midpoint between the most proximal and the most distal point, the optimal site for an accessory port as well as the specimen extraction site. Trocar sites should be marked onto the patient’s skin using a sterile pen after draping. Abdominal access, CO2 insufflation and initial camera insertion are completed in the usual fashion using safe practice guidelines.
Si® Robot (Intuitive Surgical, Sunnyvale, CA, USA)
When using the Si system, the ports should be placed along a curve and be approximately 20 cm away from the target and 10 cm apart in order to avoid clashing of the robotic arms. The ports/arms are labeled C for the camera and 1, 2, and 3 for trocars going right to the left. The specimen extraction and anvil insertion site may be planned at one of the existing ports or as a separate small Pfannenstiel incision in the suprapubic region.
A typical trocar setup for a robotic low anterior resection (LAR) is illustrated in Fig. 19.1a. The camera is placed through a periumbilical 12 mm laparoscopic trocar. A 12 mm robotic trocar (arm 1) is placed in the right lower quadrant making sure not to injure the inferior epigastric vessels. A more medial position facilitates access to the deep pelvis, whereas a more lateral position is appropriate if the extent of the dissection ends at the pelvic inlet. One 8 mm robotic trocar (arm 2) is placed in the left upper quadrant on the midclavicular line between ribs and the iliac crest, and another 8 mm trocar (arm 3) is placed in the left lower quadrant (position 3A). For splenic flexure mobilization, a right upper quadrant 8 mm trocar may temporarily be used for arm 3 (position 3B). An accessory 5 mm port is placed in the right upper quadrant to be used by the bedside assistant.
Figure 19.1b shows a modification of the trocar outline when the entire left side (left and sigmoid colon) is the target of the operation.
Xi® Robot (Intuitive Surgical, Sunnyvale, CA, USA)
For the Xi system , the ports have a different layout and should be placed on a straight line from left upper to right lower quadrant. The slope of the line may be steeper if the splenic flexure needs to be taken down and flatter if that step is not anticipated. The space between arms should be an equal distance of 6–8 cm. In contrast to the previous setting, the ports/arms in the Xi are labeled as 1–4 from left to right (Fig. 19.2). The standard robotic port including the one for the camera is 8 mm; stapler insertion requires a 12 mm port (typically arm 4) with an 8 mm reducer when used for the other instruments. The specimen extraction and anvil insertion site may be planned as one of the existing ports or as a separate small Pfannenstiel incision in the suprapubic region.
Docking of the Robot
After trocar placement, the patient is positioned in Trendelenburg and with the left side up just enough to move the small bowel out of the pelvis and expose the root of the left colon mesentery.
Si Robot
The Si robot has less flexibility, and the cart needs to be docked in an oblique angle (approximately 30 degrees) from the left hip. The base of the robotic cart is aligned parallel to a virtual line between the most outer trocars in the left flank and right lower quadrant (Fig. 19.1a). It is important to position the left leg in the stirrup such that it will not interfere with the robotic arm movements after the patient is positioned in Trendelenburg position and tilted to the right. The Si system will allow reasonable access to two quadrants involved in the operation. If the ports are configured for a lower pelvic operation, access to the pelvis and a portion of the left hemi-abdomen will be possible without repositioning. If the splenic flexure needs to be mobilized, three options exist: [1] arm 3a is undocked and rotated into the 3b position (Fig. 19.1a), [2] the robotic cart may need to be redocked over the left shoulder, or [3] the splenic flexure is mobilized laparoscopically. Once the Si robot has been docked, it needs to be manually targeted to the area of interest.
Xi Robot
As the Xi robot has a central boom that allows for 360 degrees rotation, it can be docked from any direction, typically though from the left. First, the boom is centered and then docked to the camera port (arm 3) only. The camera is inserted and pointed at the surgical target. The boom and the other arms are automatically optimized using the integrated targeting function. The other arms are docked and adequately spaced.
Instrument Insertion
Instruments should be carefully inserted, best under visual control or by testing the direction first by means of a nontraumatic laparoscopic peanut. With either system, the right hand typically controls an energy device (monopolar scissors, hook, or bipolar vessel sealer) through the right lower quadrant port. The left hand directs two retracting instruments (fenestrated bipolar forceps, Cadiere forceps or tip up, fenestrated graspers). These instruments are frequently adjusted utilizing the foot switch to allow for optimal traction and countertraction. Much of the exposure is achievable without the assistant surgeon and is considered one of the major benefits of robotic compared to laparoscopic approaches.
CME Dissection of the Colon Mesentery and Isolation of the Mesenteric Root
When the goal is to perform an oncological resection, the procedure follows the same steps as described for the laparoscopic approach. Please refer to Chap. 11 on Principles of Complete Mesocolic Excision (CME) for Colon Cancer.
Depending on the location of the pathology and whether left colectomy is performed for benign or malignant indications, different levels of vascular dissection are needed. The dissection usually commences with retracting the rectosigmoid colon upwards to tent up the inferior mesenteric artery (IMA) pedicle towards the anterior abdominal wall (Fig. 19.3). The two robotic arms from the left side and a laparoscopic grasper through the assistant trocar can be utilized to achieve optimal tension on the peritoneum. This will allow CO2 dissection to better identify the dissection planes defined by embryological anatomy. Wide scoring of the peritoneum overlying the base of the left colon mesentery starts at the peritoneal groove on the right side of the lateral mesorectum and continues towards the inferior border of the inferior mesentery artery (Fig. 19.4). Subsequent adjustment of the robotic arms with lifting the rectosigmoid colon and by passive upwards retraction with the instrument shafts from beneath the colon wall will expose the areolar tissue between the sigmoid colon mesentery and all retroperitoneal structures. This dissection continues from medial to lateral until the IMA and inferior mesenteric vein (IMV) are completely mobilized, the left ureter is identified close to the mesenteric root, the hypogastric nerves identified and preserved, and the lateral peritoneal reflection is reached. The dissection is performed along the embryological planes of the visceral and parietal peritoneum to yield an intact mesocolon (complete mesocolic excision).
At this point, the decision has to be made whether the IMV will be ligated next to the artery or higher near the duodenum (see Fig. 19.5, which demonstrates high ligation of the IMV). This step is most commonly used during low anterior resection (LAR) and will be described in detail in Chap. 24 on Robotic Low Anterior Resection. The entire pedicle is encircled, and high ligation of the IMA and IMV is performed with the robotic vessel sealer or stapler after being individually dissected and skeletonized. Alternatively, the left colic artery can be preserved and ligation of the superior rectal artery only performed just distal to its runoff.
With few exceptions, it is recommended to follow the natural planes regardless of the indication for left colectomy. The ability to consistently and intentionally dissect, isolate, and divide the IMA, left colic artery, and superior rectal artery is invaluable and mandatory for malignant disease. Even for confirmed benign disease, dissection along these planes is often easier and less bloody than dissecting through the mesentery. In addition, a high ligation increases colon mobility which is needed for lower anastomoses.
A non-anatomic “wedge resection” along the bowel wall may on occasion be preferable in proven benign disease with severely altered anatomy (Crohn’s colitis, severe diverticulitis) and is technically facilitated using vessel sealing devices. For more details and techniques, please refer to Chap. 5 on Laparoscopic Left Colon Resection for Complex Inflammatory Bowel Disease.
The dissection continues with a medial to lateral mobilization of the descending colon mesentery off Gerota’s fascia. If the splenic flexure is mobilized for a tension-free anastomosis, the inferior border of the distal pancreas should be recognized to maintain the dissection plane anteriorly (Fig. 19.6). The sigmoid and descending colon is now retracted medially to divide a thin remaining layer of peritoneum along the line of Toldt. This dissection is continuous from lateral to medial for the splenocolic ligament. Alternatively, the lesser sac is entered from medially, and the omentum and splenocolic ligament are divided starting from the distal transverse colon (Fig. 19.7). Upon complete mobilization of the descending colon and the splenic flexure, the peritoneum lateral to the rectosigmoid junction is scored, and a window is created using blunt dissection along the posterior wall of the colon. This allows transection of the rectosigmoid colon with a robotic stapler through the right lower quadrant port. The remaining mesentery is divided to the planned proximal transection. Bowel perfusion can be assessed with indocyanine green injection and the fluorescence imaging mode of the robotic camera. For additional details on perfusion assessment for left-sided anastomoses, refer to Chap. 29 on Minimizing Colorectal Anastomotic Leaks.
Extracorporeal Anastomosis
Multiple extraction sites can be selected for extracorporeal anastomosis and mostly used are a Pfannenstiel or a lower midline incision. A small wound protector is inserted prior to specimen exteriorization to help reduce the risk of wound infection. The anvil of the EEA stapler is placed into the descending colon and secured with a purse string suture. An end-to-end or end-to-side anastomosis to the rectum is then created with the EEA stapler.
Intracorporeal Anastomosis
The robotic approach simplifies intracorporeal anastomosis (ICA) , which has the benefits of moving the specimen extraction sites off the midline to decrease the risk of incisional hernia. The most commonly used extraction site is an extension of the right lower quadrant stapler port. A small wound protector is placed after enlarging the 12 mm trocar site, and the anvil of the EEA stapler is placed intra-abdominally.
For a side-to-end anastomosis, an enterotomy is created on the specimen side, i.e., just distal to the planned level of transection on the proximal colon. The anvil can be manipulated spike-first through the anterior wall of the descending colon. The spike is pushed laterally through the proximal bowel wall after incising the wall over the tip of the anvil. The anvil spike should be located approximately 5 cm above the planned transection site on the proximal colon. The initial enterotomy is closed with a running suture to avoid spillage of content from the specimen. The colon is transected with the robotic stapler just proximal to this closure.
Alternatively, a true end-to-end anastomosis can be created as well. The bowel is transected with the stapler first, the proximal staple line is excised, and a purse string suture is placed. The anvil (secured with a string) is inserted backwards with the tip aiming distally, and the purse string is tied.
Pitfalls, Intraoperative Difficulties, and Complications
Instrument Collisions
Instrument collisions are frequently related to suboptimal trocar placement too close to each other in relation to the target. The idea of laparoscopic triangulation should always be the underlying principle for trocar placement. It is always recommended that the surgeon walks from the console to the bedside to inspect and analyze the reason for the collisions. If the adjustment of the robotic arms and elbow joints do not improve the instrument movement, the surgeon should not hesitate to consider repositioning the trocars.
Inadequate Colon Length and Morbid Obesity
Morbid obesity and inadequate colon length can go hand in hand due to thickened and foreshortened mesentery. The short and fatty mesentery makes it significantly difficult to safely identify, isolate, and divide the inferior mesenteric artery/vein, left colic vessels, and superior rectal artery. In addition, small bowel loops tend to slide back into the surgical field and cannot be kept out of the pelvis and away from the mesenteric root for adequate visualization of the inferior mesenteric pedicle. Furthermore, the steep Trendelenburg position might not be tolerated from the anesthesia perspective when the massive weight pushes onto the diaphragm. At the same time, benefits of a minimal invasive approach are more pronounced in the morbidly obese specifically as it relates to the abdominal wall and wound complications.
Achieving additional colon length can be achieved using multiple strategies. High ligation of the IMA close to the junction to the aorta will help relieve tension on the descending colon after the descending colon mesentery is mobilized from the retroperitoneum and Gerota’s fascia. The next step consists in ligation of the IMV close to the duodenum, followed by medial to lateral splenic flexure mobilization over the inferior border of the pancreas. Care must be taken to avoid avulsion and interruption of the marginal artery along the entire colon. If there is still inadequate length, the omentum is taken off the transverse colon; the middle colic vessels may have to be sacrificed unless the plan of an anastomosis is abandoned. In any such challenging case, it is helpful to check the perfusion of the colon with the integrated fluorescence imaging technology using intravenous injection of indocyanine green.
These are difficult situations that require experience and sound clinical judgment as it relates to the implications of further vascular division , including that of the middle colic vessels. Rather than blindly continue, this may be a moment to reconsider the goals and progress of the surgery and evaluate whether conversion to laparoscopy or an open approach would be justified.
Bleeding
Bleeding is often related to non-anatomical tissue and mesenteric dissection. Precise dissection is easier to perform due to the three instrument traction, countertraction, and dissection. Clear identification and circumferential dissection of all major vessels is paramount before attempted division. If bleeding is encountered at the mesenteric root, a third arm is helpful to immediately occlude proximally, while the other instruments can help suction and identify the exact source. Repeat attempt at controlling the proximal vessel can be attempted, but early conversion and laparotomy is sometimes mandatory before massive blood loss ensues. Surgeons and operating room teams should be prepared and trained for emergent robotic undocking for vascular injuries.
Anastomotic Leak
Intraoperative anastomotic leaks are almost always due to technical difficulties and complications. Even though genuine failure of the EEA stapler can occur, more often leaks are due to technical issues. Proximal colon anvil placement could be impaired from a loose proximal purse string suture, incorporation of a diverticulum, or uneven bowel wall thickness from the suture placement. It is important to recognize a suboptimal purse string suture and redo it, or alternatively place the anvil through the antimesenteric wall of the colon and perform a side-to-end anastomosis (Baker type).
Distally, the passage of the EEA stapler through the rectum can cause unrecognized serosal or even full-thickness injuries of the rectal wall often seen anteriorly. It is advised not to force the stapler through the rectum but rather perform a limited rectal mobilization, specifically posteriorly. Posterior rectal mobilization straightens out the rectum and allows the stapler to advance more easily.
An alternative is to place the spike through the anterior rectum distal and away from the blind staple line for an end-to-side stapled anastomosis (reversed Baker Type).
If the anastomosis is found to be suboptimal or faulty, as evidenced by either a positive air leak test, incomplete anastomotic doughnut , or endoscopic inspection, the options are (1) to reinforce the anastomosis (with/without diversion), (2) to redo the entire anastomosis, or (3) to abandon the anastomosis and convert to a Hartmann’s procedure.
Outcomes
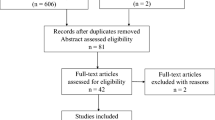
Several studies have been published examining the outcomes for robotic versus laparoscopic versus open colectomy in patients undergoing resection for both malignant and benign disease [8,9,10]. In general, robotic and laparoscopic surgery take longer than open operations, but they are both associated with improved short-term outcomes , shorter length of stay, fewer 30-day complications, and equivalent long-term oncologic results. In a comprehensive meta-analysis analyzing 40 peer-reviewed studies with varying study designs, Sheng and colleagues [9] compared robotic surgery to laparoscopic surgery in oncologic resections. They noted that blood loss, complication rate, mortality rate, bleeding rate, and ileus rate were all lowest in the robotic group. The authors also demonstrated that wound infection rate for laparoscopic resections was lowest, but this was statistically similar to the robotic group. Notably, both minimally invasive approaches were superior to the open approach with regard to reducing wound infections.
Fewer conversions to open surgery are also a clear benefit of left-sided robotic colonic resections [10]. Robotic colorectal surgery has been associated with a nearly 50% reduction in open conversion when compared to equivalent laparoscopic operations (15.1 vs. 7.6%, p < 0.001) [11]. These lower conversions translate into improved clinical outcomes such as decreased length of stay, fewer 30-day complications, and a reduction in overall cost of care [11]. Alva and colleagues has performed an exhaustive review of the currently published data regarding clinical outcomes in laparoscopic versus robotic colorectal surgical cases and is summarized in Table 19.1 [12].
Conclusions
A robotic approach to a sigmoid and left colectomy has several technical advantages compared to a laparoscopic approach. The addition of a third surgeon-controlled instrument arm allows optimal traction and countertraction. In combination with improved stable and 3D visualization and wristed instruments, consistent dissection along embryologic and anatomic planes and precise visualization, mapping, and dissection of the left-sided mesenteric vessels allow consistent oncologic resections for malignant disease. Intracorporeal anastomosis is facilitated allowing off midline extraction of the specimen with decreased incisional hernia rates.
References
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–9.
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for Colon cancer. Ann Surg. 2008;248(1):1–7.
Blackmore AE, Ching MT, Tang CL. Evolution of laparoscopy in colorectal surgery: an evidence-based review. World J Gastroenterol. 2014;20(17):4926–33.
Abu Gazala M, Wexner S. Adoption rates for laparoscopy in colorectal surgery: why are they lagging behind? Ann Laparosc Endosc Surg. 2018. http://ales.amegroups.com/article/view/4625/5418.
Yeo HL, Isaacs AJ, Abelson JS, Milsom JW, Sedrakyan A. Comparison of open, laparoscopic, and robotic colectomies using a large National Database: outcomes and trends related to surgery center volume. Dis Colon Rectum. 2016;59:535–42.
Bharucha A, Parthasarathy G, Ditah I, Fletcher J, Ewelukwa O, Pendlimari R, et al. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol. 2015;110(11):1589–96.
Marks J, Kawun U, Hamdan W, Marks G. Redefining contraindications to laparoscopic colorectal resection for high-risk patients. Surg Endosc. 2008;22(8):1899–904.
Ragupathi M, Ramos-Valadez DI, Patel CB, Haas EM. Robotic-assisted laparoscopic surgery for recurrent diverticulitis: experience in consecutive cases and a review of the literature. Surg Endosc. 2011;25(1):199–206.
Sheng S, Zhao T, Wang X. Comparison of robot-assisted surgery, laparoscopic-assisted surgery, and open surgery for the treatment of colorectal cancer: a network meta-analysis. Medicine (Baltimore). 2018;97(34):e11817.
Bhama AR, Obias V, Welch KB, Vandewarker JF, Cleary RK. A comparison of laparoscopic and robotic colorectal surgery outcomes using the American College of Surgeons—National Surgical Improvement Program (ACS-NSQIP) database. Surg Endosc. 2016;30:1576–84.
Cleary RK, Mullard AJ, Ferraro J, Regenbogen SE. The cost of conversion in robotic and laparoscopic colorectal surgery. Surg Endosc. 2018;32(3):1515–24.
Alva S. Laparoscopic vs robotic surgery in colorectal cases. World J Laparosc Surg. 2018;11(1):43–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)
About this chapter
Cite this chapter
Soliman, M.K., Bardakcioglu, O. (2020). Robotic Left-Sided Colon Resections: Unique Considerations and Optimal Setup. In: Sylla, P., Kaiser, A., Popowich, D. (eds) The SAGES Manual of Colorectal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-24812-3_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-24812-3_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-24811-6
Online ISBN: 978-3-030-24812-3
eBook Packages: MedicineMedicine (R0)