Abstract
The assessment and airway planning of patients with airway pathology can be challenging as the current bedside airway assessment tools are often inadequate due to their low sensitivity and specificity. Almost all of these patients would have had a multi-plane computerised tomography (CT) of the head and neck as part of the diagnostic process. In addition to this many would also have had a flexible nasal endoscopy with an associated hand-drawing by the surgeon or a still image in the notes. With three-dimensional (3-D) reconstruction and virtual endoscopy (VE) performed either by the radiologist, anaesthetist or surgeon on an Apple Mac workstation with easily available software such as OsiriX® and HOROS, an inside simulated view of the airway or the pathology can be obtained. This can then be utilised to formulate an airway management plan. Three-dimensional reconstruction of the patient’s head and neck anatomy gives a better understanding of how it is affected by pathology in and around the upper airway. This well-established tool has already shown its value in diagnosing intra-luminal lesions of the airway and bronchial tree and there is now growing evidence demonstrating the benefits of this technology in visualising and mapping out an airway management plan in patients with head and neck pathology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Airway planning
- Airway pathology
- (3-D) reconstruction
- Virtual endoscopy (VE)
- Head and neck pathology
- Upper airway imaging
5.1 Introduction
The assessment and airway planning of patients with airway pathology can be challenging as the current bedside airway assessment tools are often inadequate due to their low sensitivity and specificity. Almost all of these patients would have had a multi-plane computerised tomography (CT) of the head and neck as part of the diagnostic process. In addition to this, many would also have had a flexible nasal endoscopy with an associated hand-drawing by the surgeon or a still image in the notes. With three-dimensional (3-D) reconstruction and virtual endoscopy (VE) performed by either the radiologist, the anaesthetist or the surgeon on an Apple Mac workstation with easily available software such as OsiriX® and HOROS, an inside simulated view of the airway or the pathology can be obtained. This can then be utilised to formulate an airway management plan. Three-dimensional reconstruction of the patient’s head and neck anatomy gives a better understanding of how it is affected by pathology in and around the upper airway. This well-established tool has already shown its value in diagnosing intra-luminal lesions of the airway and bronchial tree, and there is now growing evidence demonstrating the benefits of this technology in visualising and mapping out an airway management plan in patients with head and neck pathology.
5.2 Assessment Tools for Airway Management
Predicting difficulty with mask ventilation, intubation or both is notoriously challenging for the anaesthetist, lacking as we are in tests of sufficient sensitivity and specificity to identify those patients at greatest risk.
These difficulties are more pronounced when attempting to plan appropriate airway management for patients with airway pathology, where the disease state, or indeed its treatment, can introduce further challenges.
The Fourth National Audit Project (NAP4) [1], published in the UK in 2011, demonstrated that patients with head and neck pathology accounted for 40% of patients suffering from serious morbidity and mortality during airway management, with key features being a failure to adequately assess the airway preoperatively, or to adapt the best anaesthetic technique to suit the patient’s condition. In several cases, radiological imaging was available prior to theatre, which would have alerted the anaesthetist to the difficulty ahead if it had been reviewed appropriately. It was postulated that unfamiliarity with interpreting images such as CT scans may partly explain why this did not occur in some cases.
Many patients with airway pathology, for example neoplastic disease in the glottic region, are likely to need advanced airway management techniques such as videolaryngoscopy, awake tracheal intubation or even a primary tracheostomy. NAP 4 highlighted several cases where patients were exposed to harm due to suboptimal airway management when an awake tracheal bronchoscopic intubation or tracheostomy under local anaesthesia was indicated, but not performed first-line. An accurate judgement of which technique is most likely to result in the rapid, atraumatic and safe securement of the airway reduces the morbidity suffered by the patient, and the stress suffered by the anaesthetist.
Many organisations including the American Society of Anaesthesiologists (ASA) and World Health Organization (WHO) [2, 3] recommend a systematic airway assessment be performed prior to induction of anaesthesia, although consensus on what this should entail and the evidence that doing so improves outcomes, is lacking.
However, patients with head and neck pathology by their very nature should arouse suspicions of difficulty with the airway, and tend to have undergone several relevant diagnostic investigations prior to surgery, which are of benefit to the anaesthetist planning the airway management.
Virtual endoscopy offers particular advantages in such cases, utilising computer software to transform CT images of the head and neck into 3-D “fly-through videos” of the patient’s airway anatomy in a format familiar to the anaesthetist who practices flexible bronchoscopic intubation. This allows the anaesthetist to determine preoperatively the degree of distortion and narrowing caused by any infective, inflammatory or neoplastic process and make a judgement as to whether ventilation and intubation can be performed in the asleep patient, or whether an awake technique utilising a flexible bronchoscope or tracheostomy is more appropriate. If flexible bronchoscopic intubation is deemed the technique of choice, the anaesthetist can plan the best route to take and can anticipate at which level of the airway difficulty may be encountered.
5.2.1 Airway Assessment
The airway assessment of the patient with head and neck pathology begins as for any other patient undergoing anaesthesia, with a targeted history and simple bedside tests.
5.2.2 History
Important symptoms to illicit when taking a pre-anaesthetic history for a patient with pathology in the airway include dyspnoea—on exertion, at rest or worsened by the supine position; dysphagia, to solids and/or liquids, and is coughing provoked which may suggest aspiration; voice change, such as hoarseness or weakness of the voice, or the “hot potato” quality suggestive of base-of-tongue lesions; difficulty with mouth opening due to pain or true trismus. The time scale over which symptoms have developed, and whether they are static or progressive is important. A more rapid progression will of course be expected in acute, infective pathologies of the airway as compared to those of a malignant process. If a patient’s dyspnoea or hoarseness has progressed since their last imaging or surgical review, one should be wary that this is likely to be accompanied by anatomical deterioration of the airway. A history of relevant treatment, such as previous head and neck surgery or radiotherapy, is also very pertinent.
5.2.3 External Examination
A general external examination may yield information about generic challenges for airway management, such as the presence of a beard or obesity. There may also be disease-specific signs, such as facial or neck swellings caused by infection, tumour or lymphadenopathy or a visible goitre. The classic woody texture and appearance of radiotherapy treatment may be apparent, along with the scars and tissue flaps from previous surgery. Patients with slowly progressive disease can appear deceptively lacking in symptoms, as their respiratory muscles adapt and compensate for the progressive narrowing of the airway; the severity of their airway obstruction may only reveal itself with the induction of anaesthesia and the resultant loss of skeletal muscle tone [4].
5.2.3.1 Mouth Opening, Inter-Incisor Gap and Mallampati
The ability to open the mouth is the most ubiquitous component of the airway assessment, allowing the anaesthetist to gauge the ease of access for airway instrumentation. The inter-incisor gap (IIG) is the most reproducible measure of mouth-opening, with a distance of less than 3 cm being suggestive of difficulty with direct laryngoscopy [5]. Some of the more streamlined videolaryngoscope blades can be inserted with an IIG of 2 cm [6], and successful insertion of supraglottic airway devices has been reported with an IIG below this [7].
With the mouth open and the tongue protruded maximally, the modified Mallampati score can be assessed. This compares the relative size of the tongue to that of the oral cavity, and a grading of 1–4 assigned depending on the structures visible to the assessor sitting opposite to the patient.
A Class 1 Mallampati view means that the soft palate and entirety of the uvula are visible, while a Class 4 view means that only the hard palate is visible to the observer. In Mallampati’s original paper [8], 80% of those with a Mallampati Class 1 view had a Grade 1 view of the glottis at laryngoscopy, with the remainder a grade 2 view, with higher Mallampati classes showing increasingly higher rates of poorer glottic visualisation. However, if used in isolation, the Mallampati test has been shown to be an unreliable predictor of the difficult airway with varied inter-observer reproducibility [9].
Performing a Mallampati assessment can be of value in patients with head and neck disease, as looking into the oral cavity can reveal the presence of an abscess, tumour or other soft tissue swelling. An inability to protrude the tongue can suggest disease process in the tongue base or submandibular space, which is a red flag for difficult laryngoscopy.
5.2.3.2 Jaw Protrusion and Upper Lip Bite Test
Difficult laryngoscopy is more likely in patients with retrognathic mandibles or prominent maxillary incisors. An assessment of the patient’s ability to prognath the jaw will highlight either of these deficiencies and also assess the temporo-mandibular joint. Jaw protrusion is defined as Grade A when the incisors of the mandible protrude beyond those of the maxilla, Grade B when the incisors meet and Grade C when the maxillary incisors protrude beyond the mandible. An alternative is to ask the patient to bite their upper lip and assess whether they are able to get above the vermillion border of the upper lip with the lower incisors. This test has shown variable sensitivity and specificity for predicting difficult laryngoscopy when compared to the Mallampati assessment [10, 11].
5.2.3.3 Thyromental and Sternomental Distance
The thyromental distance (TMD) is the distance from the cephalad border of the thyroid cartilage to the mental protuberance of the mandible, with the head held in extension. The sternomental distance is that between the sternal notch and the mental protuberance. Distances of less than 6.5 cm and 12.5 cm, respectively, are associated with difficult direct laryngoscopy. The World Health Organization advocates the combination of Mallampati with TMD as the most useful way of identifying patients at risk of difficult intubation [3]. A modification of the TMD by working out its ratio to the patient’s height has been shown to be more accurate than the TMD itself at predicting difficult laryngoscopy [12, 13].
5.2.3.4 Neck Movements
Assessing whether a patient can adequately flex the cervical spine and extend at the atlanto-axial joint indicates their ability to adopt the optimal position for mask ventilation and direct laryngoscopy. It also allows an opportunity to assess the landmarks for cricothyroidotomy, and the ability to position the patient with full cervical spine extension should front of neck access be required electively or in an emergency. Previous radiotherapy to the neck can have a detrimental effect on the ability to flex the neck and palpate the necessary cartilaginous landmarks.
5.2.3.5 Multivariate Scoring Systems
As each of the tests outlined above has limited specificity and sensitivity when used in isolation, various attempts have been made to combine these components together to form a scoring system with a greater positive predictive value.
One of the first such scoring systems was the Wilson Score, which assesses the patient’s weight, cervical spine flexibility, inter-incisor gap, retrognathism and prominent maxillary incisors [14]. The more unfavourable each component, the higher the score it attracts. A total score below 5 is reported to be reassuring for straightforward direct laryngoscopy, while a score greater than 7 warns of severe difficulty.
5.2.3.6 Simplified Airway Risk Index (SARI)
A more recently developed system is the Simplified Airway Risk Index (SARI) [15]. Again, this uses a weighted scoring system, and the factors assessed are mouth opening, thyromental distance, Mallampati score, neck movements, prognathic ability, weight and history of previous difficult intubation. However, a large, prospective Scandinavian trial detected no statistically significant change in the number of unanticipated or straightforward intubations when the SARI tool was compared with non-standardised airway assessment [16].
With the limitations that these simple bedside tests have in identifying the potentially difficult airway, the importance of imaging investigations in the planning of airway management for patients with head and neck pathology is emphasised.
5.3 Imaging of the Airway
Preoperative investigations can assist the anaesthetist by confirming the presence of any pathological abnormality detected during history and examination, and providing further information of the location and extent of disease. This allows us to make a more informed judgement as to how the airway pathology in question may impact on our ability to intubate, ventilate or both, and adjust our plan accordingly. The majority of airway investigations comprise some form of static radiological imaging, but some dynamic, real-time assessment can also be obtained by flexible nasendoscopy (Fig. 5.1) (Movie 5.1).
X-ray can provide useful information for airway assessment. Soft tissue views of the neck are informative in cases of suspected foreign body inhalation, as they may confirm the nature of the object and the level and extent of any resulting airway obstruction.
A chest radiograph may offer further information, such as distal airway obstruction or collapse and air trapping. A plain chest film may also reveal pathologies such as deviation or narrowing of the trachea, which may prompt further investigations such as nasoendoscopy or a CT scan.
A lateral c-spine radiograph, taken with the head in a neutral position, allows measurement of the distance between the C1 spinous process and the occiput. A distance less than 5 mm is suggestive of intubation difficulty [5].
Information can be gleaned from orthopantomograms (panoramic views) such as the presence of facial fractures. This can increase the likelihood of difficult mask ventilation and laryngoscopy due to the disruption of the anatomy and tissue swelling.
5.3.1 Ultrasound
The introduction of anatomical assessment with the help of ultrasound imaging in anaesthesia has been one of the more recent technological advances in this field. The increasing use of ultrasound has been accredited to its proven established clinical efficacy, cost-effectiveness and practicality as it allows anaesthetists to evaluate often complex and varied anatomy.
Ultrasound imaging can contribute to anatomical information that would otherwise not be evident on routine clinical screening tests for assessment of difficult laryngoscopy, e.g. thickness of anterior soft tissue on the neck, oedema and tumours. One of the primary uses of ultrasound is for the identification of the cricothyroid membrane. Additionally, it is employed for the discovery of midline vessels in gauging suitability for percutaneous tracheostomy. It also allows an assessment of vocal cord mobility.
Current literature suggests the novel use of ultrasound for predicting difficult intubation has been growing. Hui et al. describe a method of imaging oropharyngeal and laryngeal structures by performing sublingual ultrasound on the floor of the mouth [17, 18]. This produces sagittal views permitting visualisation of the base of tongue, hyoid bone and suprahyoid muscles. They postulate that failure to visualise the hyoid bone may indicate difficulty with intubation, as this suggests a more caudal placement of the hyoid which can be caused by a relatively short mandibular ramus or a more hypopharyngeal position of the tongue. Oesophageal intubation can be easily determined by an ultrasound probe when placed 1 in. above the suprasternal notch, and the double trachea sign is easy to be seen and more diagnostic.
Ultrasound use has gained popularity; however, more extensive validation is required. Advantages of ultrasound imaging are as follows: it is safe; there is no use of ionising radiation or contrast agent; it is non-invasive, portable, widely available, painless and easily reproducible, and moreover gives real-time dynamic images. Although considered safer compared to other imaging modalities, exposure in terms of intensity and time should be limited as much as possible, as high-energy ultrasound can cause heating of the tissues. There is also a recognised learning curve for ultrasoud assessement of the airway, which requires training and practice to overcome.
5.3.2 Computed Tomography (CT)
Computed tomography scans have significantly enhanced the assessment of patients with complex airway pathology. Joint discussion between the head and neck/ENT surgeon and radiologist aids the interpretation of images with regard to the source of pathology, staging of neoplasms and severity of any stenosis, or any subglottic/retrosternal extension.
The CT scan, whilst providing extensive clinical information and aiding in diagnosis, to the extent of pathology, carries certain risks to patients, namely, exposure to ionising radiation, allergy to contrast and deterioration of renal function in patients with poor renal function when contrast is used.
5.3.3 Magnetic Resonance Imaging (MRI)
MRI is useful for delineating soft tissue pathology; however, the ability of many patients with multiple comorbidities to lie flat for prolonged periods can be a limiting factor for their use. The lack of radiation compared to CT scan is a huge advantage. Multi-planar reformations (MPR) in sagittal and coronal planes are more useful in indicating stenosis, as well as the degree of airway distortion, and in delineating airway anatomy than individual coronal slice images [3].
5.3.4 Nasendoscopy
Nasendoscopy is versatile in the fact that it is generally well tolerated and can be performed at pre-assessment clinic, in the ward setting and before induction of anaesthesia (Fig. 5.1). It is performed using a small-diameter flexible nasendoscope, and allows the operator to visualise the upper airway anatomy and identify any abnormalities. As the patient is awake and spontaneously breathing during the procedure and retains the ability to phonate various sounds, nasendoscopy allows a dynamic assessment of the position and movement of the vocal cords.
The procedure is commonly performed as part of the patient’s assessment in the head and neck clinic, and the surgeons will usually document any pathology seen on a diagram in the patient’s case notes so that other clinicians can refer to it, although still images or video recordings can also be taken and stored for reference. It is highly beneficial for the anaesthetist to perform or be present at the time of nasendoscopy rather than rely on these methods of documentation, as this allows a fuller assessment of the patient’s upper airway anatomy and the ease with which a view of the glottis can be obtained with a flexible bronchoscope [19]. The procedure provides information on the bearing that a lesion will have on direct laryngoscopy, fibre-optic intubation, intubation and even direct tracheal access, and this information can be assimilated into the airway plan (Movie 5.1).
5.3.5 Radiographs
5.4 3-D Reconstruction and Virtual Endoscopy and Applications in Airway Pathology
In obstructing airway pathology, the assessment of the airway beyond what can be seen on examination is difficult, and therefore, advanced imaging can be helpful. Often nasendosopy is performed if tolerated and is a valuable tool in understanding the degree of airway compromise. In most cases, a CT scan of the head and neck will be performed; this provides extra information for the surgeon and the anaesthetist. Viewing of airway pathology on two-dimensional imaging such as CT slices and making an accurate identification of the size and location of the pathology can be a challenging task for the anaesthetist.
Modern post-processing software techniques such as 3-D volume rendering provide added diagnostic value to two-dimensional CT scans [20, 21]. Sharing the 3-D images enhances communication amongst clinicians and also improves procedural planning. The software tools are available to radiologists but often underutilised as they are slightly more time consuming and not all radiologists are familiar with them. Also the additional reconstruction is often not routinely requested. With newer software such as OsiriX® and Horos, the reconstruction has become easier and available to specialists outside radiology. The usefulness in the diagnostic process and airway management has been shown in the literature [22]. Virtual endoscopy and 3-D reconstruction also enhance communication amongst different specialities such as ENT and head and neck surgeons, radiologists, anaesthetists and also possibly the patient. It is important to understand that VE and 3-D reconstruction of the airway do not provide new information to the original CT scans but rather a complementary way of viewing the same data set. All the images and movies at our centre are created using the Osirix software (Osirix Viewer 9.5, Pixmeo Sarl, Bernex, Switzerland). Other software such as Horos (Horosproject.org, Nimble Co. LLC d/b/a Purview in Annapolis, MD, USA) and RadiAnt (Medixant 2009) used by the radiologists are equally accurate.
5.4.1 3-D Reconstruction
3-D reconstruction of the air–tissue interface is another application of post-processing software. This external 3-D rendering creates a 3-D model of the air-filled spaces that can be rotated in every direction and exported as an image (Fig. 5.2) or a movie format (see Movie 5.2). Pathology within the airway or external lesions can be visualised by showing a narrowing of the air-filled spaces (Fig. 5.2).
With these techniques, subglottic lesions and abnormalities such as deviation of the trachea and long narrow stenosis can be appreciated better than those with a 2-D format or even virtual endoscopy.
5.4.1.1 Example
The three-dimensional aspect of an airway tumour can be better appreciated in the movie format. The extent of the obstruction of this adenoid cystic supraglottic tumour is shown in Movie 5.2 in the linked video files.
5.4.2 Virtual Endoscopy
Virtual endoscopy is another application of volume-rendering techniques whereby a virtual camera can be moved inside a hollow organ lumen. In airway assessment, this can be done in a similar way to moving a flexible bronchoscope through the patient’s airway and down into the trachea. A focal point, which can be moved in every direction through the lumen, determines the pathway. Several points are saved and computed to create a movie that can be viewed and shared. The advantage of VE in addition to conventional airway imaging is that it is non-invasive whereas flexible nasendoscopy is therefore not always tolerated by the patient. Also, VE does not require any additional radiation, as the CT scans are already part of the diagnostic process. By visualising the airway from the inside and thereby simulating an awake flexible bronchoscopic examination, the airway management can be planned in advance. Also, the virtual camera can move beyond the vocal cords and establish a retrograde view in a downward to upward direction.
5.4.2.1 Clinical Applications of VE
Virtual simulation training has good evidence as a tool to improve technical skills in the training of physicians [23, 24, 25].
NAP 4 has shown that patients with pathology of the head and neck have a higher proportion of complications during airway management as well as more severe complications than any other patient cohorts [1]. The evaluation and the subsequent airway management plan tend to be more challenging in patients with obstructing airway lesions [26]. As mentioned above, the usual methods of clinical airway assessment can be misleading or falsely reassuring or in fact be influenced by the airway pathology such as a dental abscess causing poor mouth opening.
Airway pathology can involve one or several parts of the supraglottic, glottic and subglottic larynx, and correctly pinpointing the location and extent of the lesion can be difficult for most anaesthetists [26, 27]. Advanced imaging of the airway such as helical CT scans or MRI can help to visualise the obstructing airway pathology (OAP). When available and performed close to the time of surgery, flexible nasendoscopy evaluation of the airway can change airway management [19]. Nasendoscopy is routinely done by the otolaryngologists if tolerated by the patient, but it is not always available to the anaesthetist. Also, the small calibre nasal endoscope can be passed after topicalisation of the nose to visualise structures down as far as the vocal cords and not beyond, and is not always available in theatre.
Other than nasal endoscopy, CT scans or MRI of the head and neck needs to be reviewed. Because of the two-dimensional aspect of these images and the way they need to be reviewed, it is not always easy to clearly identify the level of the obstructing airway pathology and quantify the impact onto the airway patency, especially by practitioners who have not been formally trained to do so. The endoscopic view of the airway is a view that anaesthetists are more familiar with as done during standard laryngoscopy, video-laryngoscopy or awake tracheal intubation using a flexible bronschoscope. Virtual endoscopy provides such a view of the airway from the patient’s CT scans with no extra radiation as these images will have already been obtained during the diagnostic process. These virtual endoscopy views have been shown to accurately represent intraluminal lesions [28,29,30,31,32,33,34,35,36,37] and in fact are used in other specialities such as radiology and thoracic surgery to diagnose pathology in head and neck and the bronchial tree. More recent evidence shows that having virtual endoscopy views in addition to CT images improves the anaesthetist’s diagnostic accuracy [22]. It has also been shown that they influence the airway plan. In the study by El-Boghdadly et al., the changes that were made to the airway management plan after viewing the virtual endoscopy video were mostly to a more cautious approach and that was not dependent on the anaesthetist’s level of experience with managing patients with OAP.
5.4.2.2 Example 1
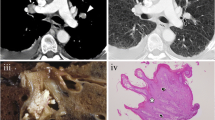
This is an example of a glottic tumour involving the arytenoid cartilages. In Movie 5.3, the glottic tumour can be seen (Figs. 5.3 and 5.4).
5.4.2.3 Example 2
This is an example of a large supraglottic obstructing airway pathology arising from the right valleculla and pushing the epiglottis over to the left. The similar appearance of the large smooth-surfaced lesion wrapping around the epiglottis and obstructing the laryngeal inlet can be seen on the image taken from the flexible bronchoscopic airway assessment (Fig. 5.5) as well as from the virtual endoscopy (Fig. 5.6). In the VE video (Movie 5.4), a patent pathway can be seen beyond the lesion, which favours a possible awake tracheal intubation using a flexible bronschoscope.
5.4.2.4 Example 3
The following example is a patient with a base of tongue tumour and the abnormally shaped epiglottis can be seen on the movie (Movie 5.5) as well as on the images (Figs. 5.7 and 5.8).
5.4.3 Limitations of VE and 3-D Reconstruction
One of the limitations of VE and 3-D reconstruction is that it is based on static CT images in a supine position. In some cases, the supine position results in collapse of the airway and thus can give an appearance of the airway that is worser than it actually is. Also, it would be difficult to obtain a full VE run through down to the trachea if parts of the airway are collapsed, and there is no actual lumen for the virtual camera to go through. 3-D reconstruction of the air-filled spaces will still be possible but might give the impression of a more severe narrowing of the airway. This could be overcome by manoeuvres such as Valsalva or blowing through a straw during the CT scan, which is done in some institutions [38].
The CT images are not always taken just prior to surgery and anaesthesia induction; therefore, caution should be taken in case the obstructing airway pathology has worsened or even improved.
Another limitation is the availability of the appropriate software and hardware as well as the CT scans. Radiologists can upon request reconstruct VE videos and a 3-D model of the air-filled spaces using the hospital’s hardware and software and accessing the scans through the Patient Archive and Communication System (PACS). The downside of that is that radiologists do not always know what the anaesthetist is looking for to plan the airway, and some communication between specialities is required.
OsiriX® viewer and HOROS is a computer software program for Apple computer systems and that can be used to view Digital Imaging and Communications in Medicine DICOM data files as well as reconstruct VE and 3-D models of the airway in a user-friendly way. Most users without prior experience can create a video in 20 min whereas more experienced users are able to reconstruct VE in around 2 min.
5.5 3-D Printing in Airway Pathology
One must also consider the use of 3-D printed models, particularly of patients with airway pathology. These models, once printed from the patient’s CT data, can not only be used in the assessment of the airway but also provide valuable anatomical information when they have been scoped by the anaesthetist pre-operatively. Manoeuvres of the flexible bronchoscope required to negotiate airway pathology can be practiced on the model without causing any airway trauma, with the added advantage that the operator will experience physical feedback, which is absent from VE. The creation of these models may also help in the teaching and training of fibre-optic intubation. There are, however, some areas of difficulty that need to be overcome such as cost and time required to produce each model, universal access to the software used to create the models and establishing the most appropriate materials to make the models.
5.6 Training Uses for Virtual Reality
Not only are 3-D reconstruction images useful for pre-emptive airway management planning, but the images are also of value for education and training. Both novice and expert airway anaesthetists can study the images, predict what aspects of airway management may be challenging and propose a strategy, which can be compared to how the case unfolded clinically.
There is precedent for the use of virtual reality in airway training, for example, the Operating Room Simulation (ORSIM)® System (Airway Simulation Limited, Auckland, New Zealand.) The ORSIM® comprises a replica bronchoscope associated with a sensor device, which communicates with a laptop configured with the ORSIM software package [25]. Users select a training package which displays on screen a high-fidelity, real-time run through a simulated patient’s airway, and allows them to practice the endoscopy skills required to successfully navigate the airway. There are a variety of simulations to run, from normal airways through to complex airway pathology. The program will then give the operator feedback on the time taken for the procedure, whether hypoxia occurred during the procedure, and how often the simulated bronchoscope collided with soft tissues. The use of this system offers practitioners the opportunity to gain skills and experience in airway endoscopy in the safety of the virtual reality environment.
5.7 Summary
3-D reconstruction and VE volume rendering of CT images of the airway can provide anaesthetists with an alternative view of the airway in patients with head and neck pathology. This way of assessing the airway in a complex group of patients allows us to better appreciate how the pathology may affect safe airway management and appears to influence us into formulating safer airway planning.
References
Cook T, Woodall N, Frerk C. 4th National Audit Project (NAP 4) of the Royal College of Anaesthetists and The Difficult Airway Society, Major Complications of Airway Management in the United Kingdom, Report and Findings; 2011.
Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. https://doi.org/10.1097/ALN.0b013e31827773b2.. Accessed 25 Mar 2018
Gawande A, Weiser T. Airway assessment. In:WHO Guidelines for Safe Surgery. Geneva: World Health Organisation; 2009. p. 29.. http://apps.who.int/iris/bitstream/handle/10665/44185/9789241598552_eng.pdf;jsessionid=170625B22-DD3F86FABAB55892724F269?sequence=1. Accessed 25 Mar 2018.
Ahmed-Nusrath A. Anaesthesia for head and neck cancer surgery. BJA Educ. 2017;17(12):383–9.
Crawley SM, Dalton AJ. Predicting the difficult airway. BJA Educ. 2015;15(5):253–7.
Karalapillai D, Darvall J, Mandeville J, Ellard L, Graham J, Weinberg L. A review of video laryngoscopes relevant to the intensive care unit. Indian J Crit Care Med. 2014;18(7):442–52.
Maltby JR, Loken RG, Beriault MT, Archer DE. Laryngeal mask airway with mouth opening less than 20 mm. Can J Anaesth. 1995;42(12):1140–2.
Mallampati SR, Gatt S, Gugino L, et al. A clinical sign to predict difficult tracheal intubation:a prospective study. Can Anaesth Soc J. 1985;32(4):29–34.
Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the mallampati tests to predict the difficult airway. Anesth Analg. 2006;102(6):1867–78.
Khan Z, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a simple new technique) with modified mallampati classification in predicting difficulty in endotracheal intubation: a prospective blinded study. Anesth Analg. 2003;96(2):595–9.
Hester C, Dietrich S, White S, Secrest J, Lindgren K, Smith T. A comparison of preoperative airway assessment techniques: the modified Mallampati and the upper lip bite test. AANA J. 2007;75(3):177–82.
Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient's height to thyromental distance improves prediction of difficult laryngoscopy. Anaesth Intensive Care. 2002;30(6):763–5.
Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–5.
Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61(2):211–6.
El-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–204.
Nørskov AK, Wetterslev J, Rosenstock CV, Afshari A, Astrup G, Jakobsen JC, et al. Effects of using the simplified airway risk index vs usual airway assessment on unanticipated difficult tracheal intubation - a cluster randomized trial with 64,273 participants. Br J Anaesth. 2016;116(5):680–9.
Hui CM, Tsui BC. Sublingual ultrasound as an assessment method for predicting difficult intubation: a pilot study. Anaesthesia. 2014;69:314–20.
Erzi T, Gewurtz G, Sessler DI, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58:1111–4.
Rosenblatt W, Ianus AI, Sukhupragarn W, Fickenscher A, Sasaki C. Preoperative endoscopic airway examination (PEAE) provides superior airway information and may reduce the use of unnecessary awake intubation. Anesth Analg. 2011;112:602–7.
Rosset A, Spadola L, Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imaging. 2004;17:205–16.
Ahmad I, Millhoff B, John M, Andi K, Oakley R. Virtual endoscopy—a new assessment tool in difficult airway management. J Clin Anesth. 2015;27:508–13.
El-Boghdadly K, Onwochei DN, Millhoff B, Ahmad I. The effect of virtual endoscopy on diagnostic accuracy and airway management strategies in patients with head and neck pathology: a prospective cohort study. Can J Anaesth. 2017 Nov;64(11):1101–10.
Boet S, Naik VN, Diemunsch PA. Virtual simulation training for fibreoptic intubation. Can J Anesth. 2009;56:87–8.
Boet S, Bould MD, Schaeffer R, et al. Learning fibreoptic intubation with a virtual computer program transfers to ‘hands on’ improvement. Eur J Anaesthesiol. 2010;27:31–5.
Baker PA, Weller JM, Baker MJ, et al. Evaluating the ORSIM_simulator for assessment of anaesthetists’ skills in flexible bronchoscopy: aspects of validity and reliability. Br J Anaesth. 2016;117:i87–91.
Law JA, Morris IR, Malpas G. Obstructing pathology of the upper airway in a post-NAP4 world: time to wake up to its optimal management. Can J Anaesth. 2017;64(11):1087–97. https://doi.org/10.1007/s12630-017-0928-7.
Norskov AK, Rosenstock CV, Wetterslev J, Astrup G, Afshari A, Lundstrom LH. Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish anaesthesia database. Anaesthesia. 2015;70:272–81.
Finkelstein SE, Schrump DS, Nguyen DM, Hewitt SM, Kunst TF, Summers RM. Comparative evaluation of super high-resolution CT scan and virtual bronchoscopy for the detection of tracheobronchial malignancies. Chest. 2003;124:1834–40.
Boiselle P, Reynolds KF, Ernst A. Multiplanar and threedimensional imaging of the central airways with multidetector CT. AJR Am J Roentgenol. 2002;179:301–8.
Men S, Ecevit MC, Topc¸u I, Kabakci N, Erdag TK, Sutay S. Diagnostic contribution of virtual endoscopy in diseases of the upper airways. J Digit Imaging. 2007;20:67–71.
Walshe P, Hamilton S, McShane D, McConn Walsh R, Walsh MA, Timon C. The potential of virtual laryngoscopy in the assessment of vocal cord lesions. Clin Otolaryngol Allied Sci. 2002;27:98–100.
Summers RM, Shaw DJ, Shelhamer JH. CT virtual bronchoscopy of simulated endobronchial lesions: effect of scanning, reconstruction, and display settings and potential pitfalls. AJR Am J Roentgenol. 1998;170:947–50.
Summers RM, Aggarwal NR, Sneller MC, et al. CT virtual bronchoscopy of the central airways in patients with Wegener’s granulomatosis. Chest. 2002;121:242–50.
De Wever W, Vandecaveye V, Lanciotti S, Verschakelen JA. Multidetector CT-generated virtual bronchoscopy: an illustrated review of the potential clinical indications. Eur Respir J. 2004;23:776–82.
Bauer TL, Steiner KV. Virtual bronchoscopy: clinical applications and limitations. Surg Oncol Clin N Am. 2007;16:323–8.
Rogalla P, Nischwitz A, Gottschalk S, Huitema A, Kaschke O, Hamm B. Virtual endoscopy of the nose and paranasal sinuses. Eur Radiol. 1998;8:946–50.
Burke AJ, Vining DJ, McGuirt WF Jr, Postma G, Browne JD. Evaluation of airway obstruction using virtual endoscopy. Laryngoscope. 2000;110:23–9.
P H, Blum A, Toussaint B, Troufleau P, Stines J, Roland J. Dynamic maneuvers in local staging of head and neck malignancies with current imaging techniques: principles and clinical applications. Radiographics. 2003;23(5):1201–13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
5.1 Electronic Supplementary Material
Real-time assessment of the upper airway obtained by flexible naso-endoscopy (the main editor is the one appearing in the video). (MP4 120839 kb)
Volume-rendering technique TTP showing the level and extent of the trans-glottic indentation and displacement of the airway by the mass lesion (MP4 3192 kb)
Glottic tumour involving the arytenoid cartilages seen by VE movie (MP4 3325 kb)
Large supraglottic obstructing airway pathology arising from the right vallecula and pushing the epiglottis over to the left proved by VE movie (MP4 4262 kb)
VE of a patient with a base of tongue tumour and the abnormally shaped epiglottis (MP4 3469 kb)
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ahmad, I., Millhoff, B., Muldoon, S., Jeyarajah, K. (2019). Virtual Endoscopy and 3-D Reconstruction in Patients with Airway Pathology. In: Shallik, N.A., Moustafa, A.H., Marcus, M.A.E. (eds) Virtual Endoscopy and 3D Reconstruction in the Airways. Springer, Cham. https://doi.org/10.1007/978-3-030-23253-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-23253-5_5
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23252-8
Online ISBN: 978-3-030-23253-5
eBook Packages: MedicineMedicine (R0)