Abstract
The family of chemical structures that interact with a cannabinoid receptor are broadly termed cannabinoids. Traditionally known for their psychotropic effects and their use as palliative medicine in cancer, cannabinoids are very versatile and are known to interact with several orphan receptors besides cannabinoid receptors (CBR) in the body. Recent studies have shown that several key pathways involved in cell growth, differentiation and, even metabolism and apoptosis crosstalk with cannabinoid signaling. Several of these pathways including AKT, EGFR, and mTOR are known to contribute to tumor development and metastasis, and cannabinoids may reverse their effects, thereby by inducing apoptosis, autophagy and modulating the immune system. In this book chapter, we explore how cannabinoids regulate diverse signaling mechanisms in cancer and immune cells within the tumor microenvironment and whether they impart a therapeutic effect. We also provide some important insight into the role of cannabinoids in cellular and whole body metabolism in the context of tumor inhibition. Finally, we highlight recent and ongoing clinical trials that include cannabinoids as a therapeutic strategy and several combinational approaches towards novel therapeutic opportunities in several invasive cancer conditions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
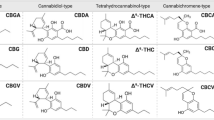
Cannabinoids have typically been assumed to originate from the plant Cannabis, however , broadly speaking cannabinoids are the group of chemical structures that mainly act in the body through cannabinoid receptors (CB); CB1 (Central receptor) and CB2 (Peripheral receptor) [1, 2]. They can be divided into different groups based on their source of origin as plant derived cannabinoids (phytocannabinoids), endogenously produced cannabinoids (endocannabinoids) and chemically produced synthetic cannabinoids. They all represent a broad range of ligands that interact with the CB receptors termed cannabinoids.
Amongst the several phytocannabinoids, Δ9-tetrahydrocannabinol (THC) is the main psychoactive compound . These compounds are responsible for many physiological effects such as euphoria, pain relief and anti-inflammatory activities [3].
Endogenous ligands like anandamide (AEA) and arachindonoylglycerol (2-AG) interact with CB as part of the endocannabinoid system [4]. Majority of the CB are expressed in neural tissues as CB1 receptor, and are known to modulate the central nervous system. CB2 receptors are predominantly expressed in immune cells and thus can modulate both the innate and adaptive immune systems [5,6,7,8] Interestingly, cannabinoids bind not only to classical receptors (CB1 and CB2), but also to certain orphan receptors and ion channels like transient receptor potential vanilloid-2 (TRVP2) and peroxisome proliferator-activated receptors (PPAR) [9] (Table 4.1).
4.2 Cannabinoids and Cancer Signaling
Several studies have suggested that cannabidiol and THC directly inhibit cancer cells growth by activation of diverse signaling pathways associated with apoptosis, proliferation, angiogenesis and metastasis [10, 11]. A schematic representation of these pathways is presented in Fig. 4.1 [12]. Previously, it has been reported that THC mediates its pro-apoptotic effect in tumor cells by increased synthesis of the proapoptotic sphingolipid ceramides [13]. In glioma cells, ceramide-dependent upregulation of the stress protein p8 induced apoptosis via the upregulation of the endoplasmic reticulum (ER) stress related gene Activating Transcription Factor 4 (ATF-4), C/EBP homologous protein (CHOP) and Tribbles homolog 3 (TRB3) [14]. It was also found the ceramide can induce apoptosis in leukemic cells by regulation of p38 MAPK signaling. Experimental studies also revealed that THC causes apoptosis in leukemia T cells by downregulation of Raf-1/mitogen-activated protein kinase/ERK kinase pathway and thus, leads to translocation of BCL2 Associated Agonist of Cell Death (BAD) to mitochondria [15]. On the other hand, it can activate apoptosis in colorectal cancer cells by inhibition of RAS-MAPK/ERK and PI3K-AKT survival signaling cascades accompanied by activation of the pro-apoptotic BAD [16].
Most interestingly, THC promotes autophagy mediated apoptosis by inducing ceramide accumulation via Tribbles homolog 3 dependent inhibition of the AKT/mTORC1 complex axis in human glioma [4] and in hepatocellular carcinoma [17] cells. The combined administration of THC and temozolomide was also found to exert a strong anti-tumoral effect in-vivo in in glioma mouse model [18]. THC treatment was also reported to inhibit the proliferation of breast cancer cells by activating the CB2 receptors with subsequent arrest of cell cycle in G2-M phase via downregulation of Cyclin-Dependent Kinase 1 (CDC2) protein [19] or modulation of JunD (a member of the AP-1 transcription factor family) [20] It also upregulated several PPAR dependent signaling pathways in cancer cells [21].
Additionally, further study confirmed that cannabidiol inhibited cancer cell viability and proliferation, which was reversed in-vitro in the presence of blockers of either CB2, Transient Receptor Potential Vanilloid 1 (TRPV1) or melastatin-related transient receptor potential (TRPM), cyclooxygenase-2 (COX-2) or PPAR and in tumor derived primary culture from a patient with non-small cell lung cancer in presence of PPAR antagonists [22, 23]. Our research group demonstrated that cannabinoid mediate its anti-proliferative effects in highly aggressive human breast cancer cells in part, by inhibition of epidermal growth factor (EGF), NF-kB, extracellular signal–regulated kinases/AKT (ERK/AKT) and matrix metalloproteinase 2 and 9 signaling pathways [24]. Cannabinoid also reduces angiogenesis in both tumor and endothelial cells . Experimental evidence suggested that cannabinoid treatment also suppresses the expressions of pro-angiogenic gene (COX-2) and decreases the secretion of prostaglandin E2 (PGE2) [25]. Furthermore, it is reported that anandamide showed decreased phosphorylation of focal adhesion-associated protein kinases, which are components of cell adhesion machinery, and influence their migration [26].
Furthermore, the treatment of THC also inhibits the growth of Lewis lung adenocarcinoma via inhibition of DNA synthesis [27]. It has also been found that THC suppresses the growth and metastasis of A549 and SW-1573 (human lung cancer cell lines) both in-vitro and in-vivo by inhibition of epidermal growth factor-induced phosphorylation of ERK1/2, c-Jun-NH2-kinase1/2 and Akt [27, 28]. Recently, research studies from our group also revealed that CB2-specific synthetic cannabinoids, JWH-015 inhibits CXCL-12 induced migration and invasion by suppressing the phosphorylation of ERK and C-X-C chemokine receptor type 4 (CXCR4) polymerization [29]. It was also reported that the treatment of cannabinoids induces apoptosis in different malignant immune cells (Jurkat and EL-4) in lymphomas and leukemia’s [30] via mitochondria mediated ROS pathway and activation of different caspases [31].
4.3 Cannabinoids and the Immune System
Presently, many advanced therapeutic approaches have been developed to treat different cancers which mainly include surgery, radiation and chemotherapy, endocrine therapy, or targeted therapy. Although, these therapies have decreased breast cancer specific mortality, they have also shown dramatic failures due to the emergence of drug resistance, relapse, multi-organ metastasis and subsequently death [32, 33]. Recently, it has been reported that the tumor microenvironment (TME) plays an essential role in regulating the stemness and drug resistance of cancer cells. TME play important roles in tumor initiation, development, invasion, and metastasis. TME is basically comprised of cancer cells, endothelial cells , fibroblasts and different types of immune cells known as tumor associated macrophages (TAMs).
TAMS have been shown to secrete different types of growth factors which can regulate TME and thus support cancer growth and subsequent metastasis [34]. Moreover, it has also been reported that M2 macrophages, which can secrete a diverse array of essential growth factors, can promote invasion and metastasis of cancer cells into multiple organs [34]. Recently, research findings have shown that the in-vivo treatment of Cannabidiol inhibits the recruitment of total macrophages and especially, M2 macrophage populations in tumor stroma as well as in lung metastatic nodules [24]. In this study, Zhu et al. demonstrated that that the in-vitro treatment of 4T1.2 cells with cannabinoid inhibited the secretion of specific cytokines such as CCL3 and GM-CSF in its condition medium (CM) as compared to CM of vehicle control. The CM harvested from cannabinoid treated 4T1.2 cells also significantly reduced the migration of mouse monocytic cells, RAW 264.7, comparatively to CM collected from vehicle control [24].
Furthermore, research findings also showed that the cannabinoid treatment inhibited the M2 macrophages induced epithelial mesenchymal transition (EMT) in non-small cell lung cancer (NSCLC) cells via downregulation of EGFR signaling cascade [35,36,37]. It has been reported that TAM can secrete EGF like ligands which can activate EFGR pathway and thus can cause increased EMT in cancer cells [38]. In addition, it has been shown that the treatment of JWH-015 inhibits the EMT induction by suppressing the activation of EGFR signaling in NSCLC cells both in-vitro and in-vivo systems. The treatment of JHW-015 also reduced the expression of proliferative marker (Ki67), angiogenic marker (CD-31), EMT markers (N-Cadherin, Snail and Slug) and also inhibited the infiltration of CD11b/F4/80/CD206 M2 macrophages into tumor. Investigation of these interactions and signaling has led to novel insights in the cannabinoids-mediated modulation of TME in cancer [39].
It has also been reported that the treatment of cannabinoids induces the conversion of T helper 1 cell (Th1) to T helper 2 cell (Th2) subpopulations by activating the expression of interleukin (IL), IL-10, and TGF-β and also decreases the production of TH1 cytokines (IL-2, IL-12 and Interferon-γ) [40] [41]. On the other hand, IL-10 and TGF-β play significant roles in mediating the THC induced suppression of anti-tumor immunity, and abrogation of either cytokine alone is sufficient to reverse the detrimental effect of THC. The study suggests that THC promotes tumorigenicity and limits immunogenicity in-vivo by upregulating the potent immune inhibitory cytokines [42].
THC has also been reported to modulate the activity of different immune cells such as macrophages, NK cells and T lymphocytes. THC and other cannabinoid agonists may exert their immune modulating effects through the disruption of Th1 to Th2 conversion [43]. THC mediates these effects by inhibiting the production of type-1 cytokines and promoting type-2 cytokine production by lymphocytes [44]). The synthetic analogues of cannabinoid were also reported to suppress the proliferation of T cells by inhibiting the production of IFN-γ. So overall, several studies show that cannabinoid and its different synthetic analogues can modulate host immunity and thus, it can regulate tumor growth and metastasis in different human malignancies [45].
4.4 Cannabinoids in Cellular Metabolism
Aberration of cellular metabolism is a hallmark feature of solid tumors as well as leukemic cancers [46,47,48]. For several decades, cancer associated metabolism has been defined in context of the Warburg effect, which suggests that highly proliferative cancer cells are entirely dependent on glycolysis rather than the mitochondria driven oxidative phosphorylation for their energetics. Since Warburg’s initial observations, research has questioned the dogma of the Warburg effect and helped to establish the significant contributions of metabolic reprogramming in mitochondrial function, and cellular energetics in cancer cell survival, metastasis, and even drug resistance [49,50,51]. Moreover, recent experimental and epidemiological research has also implicated whole body metabolism and changes induced by factors such as high fat diet, particularly obesity, in the development of a pro-tumor microenvironment [52] [53]. This has led to a greater interest in targeting cellular metabolic pathways, such as the 5′ AMP-activated protein kinase (AMPK), protein kinase C (PKC), and mammalian target of rapamycin (mTOR) pathways [54,55,56], Although PKC inhibitors have been successfully tested in the experimental setting, the efficacy of these inhibitors as monotherapy against cancer has been limited to B-cell lymphoma malignancy [57] Similarly, targeting other individual pathways, including mTOR, AKT and AMPK have had limited success in eliciting anti-tumor activity. Another product of cellular metabolism, particularly in cancer cells is reactive oxygen species (ROS). ROS are thought to further contribute to inflammatory pathways and damage cellular macromolecules and nucleotides, particularly DNA, thus potentially perpetuating cancer survival and metastasis [58].
Meanwhile, growing body of research in cannabinoids indicates a close mechanistic link between cannabinoids and metabolism. Cannabinoids have primarily been investigated as palliative therapy for individuals with advanced cancer. In this section, we hope to provide an overview of current literature linking cannabinoids and their anti-tumor activity mediated through metabolism and metabolic pathways, thereby shedding light on the potential of cannabinoids as a therapy against cancer.
For several decades, the link between metabolic syndrome and obesity, and cancer has sparked interest in whole body metabolism in patients with cancer. Fatty acid oxidation by tumor cells is often linked with various cancers, including prostate cancer, breast cancer, pancreatic cancer, etc. [59,60,61]. Fatty acid oxidation, mediated through the mitochondria, is a highly energetic process linked with high ROS generation. Experimental studies have shown that an inhibition of mitochondrial metabolism and a switch to glycolytic energy generation in tumors is linked with better prognosis as well as drug response [62]. Mitochondrial uncoupling is also critically important in inducing programmed cell death, thus making this shift from mitochondrial respiration to glycolysis in tumor cells a key therapeutic target [63].
It has also been observed that patients with cancer undergo greater loss of lean mass rather than fat mass, which in turn is linked with poor outcome and quality of life. Lean mass loss in patients with cancer can be regulated by protein nutritional support, however, the course of therapies often leads to loss of appetite, which greatly impact nutrition in these patients [64]. This is partially benefitted by cannabinoids, as cannabinoids enhance appetite through Ghrelin receptor interaction. Ghrelin receptor, a receptor for the anabolic hormone Ghrelin, is expressed is all vital organs. It is known to modulate appetite, fat accumulation and energy expenditure. Moreover, the synthetic cannabinoids HU210, impacts cellular energy metabolism via Gherlin receptor interaction [65].
In spite of its central role in nutrient sensing and metabolic regulation, AMPK appears to have both pro-tumor and anti-tumor effects. On one hand, AMPK promotes this metabolic plasticity through promotion of fatty acid oxidation, while on the other hand AMPK is closely linked with tumor suppressors p53 and tuberous sclerosis complex (TSC2) [55]. While a thorough investigation of AMPK subunits and variants involved in various solid tumors and leukemia has never been performed, several studies indicate reduced AMPK activity in lung cancer, colorectal cancer, breast cancer, ovarian cancer, hepatic cancer, etc. [1, 60, 66,67,68,69]. Interestingly, AMPK activation in cancer models, including hepatoma, has been shown to inhibit PPAR-gamma and PCG-1alpha leading to a decrease in fatty acid oxidation [70] The effect of the mitochondrial inhibitor, metformin, in patients with breast cancer is also shown to be mediated by AMPK [71].
Although not as extensively investigated in different models and cancers, synthetic cannabinoids arachidonoyl cyclopropamide (APCA) and GW405833 have been shown to inhibit mitochondrial metabolism and induce AMPK-dependent autophagy in pancreatic cancer cells [72]. Cannabinoid receptor cross-talk with AMPK is well documented in several tissues and is linked with reduction in mitochondrial biogenesis, thus disrupting mitochondrial metabolism [73]. Another systemic effect of Cannabinoids on metabolism as well as their anti-tumor activity may be exerted through the insulin signaling pathway. The key factors downstream of insulin-insulin receptor interaction such as AKT, mitogen activated protein kinase kinase 1/2 (MEK1/2) and ERK are known to contribute to cell proliferation, motility, and cancer cell survival. Cannabinoids have been shown to induce hepatic insulin resistance and multiple studies report that Cannabinoids inhibit insulin receptor signaling in pancreatic beta cells showing direct interaction between the CB1 receptor and insulin signaling [74, 75]. This is an entirely new and therapeutically sound avenue to alter crucial cell survival pathways with minimal toxicity to healthy cells.
Cancer cells have high energy needs to maintain proliferation and migration. Cannabinoids are known to inhibit mitochondrial energetics leading to autophagy [76] In pancreatic cancer cells, in combination with Gemcitabine, APCA is known to induce ROS-mediated autophagy, once again suggesting the possible role of mitochondrial electron transport chain uncoupling in response to Cannabinoids, thus directly affecting cancer cell death [77].
Cannabinoid may also potentially induce anti-tumor activity via immune cell, particularly macrophages. It has been observed that the activation of CB1 by ACEA in macrophages, which modulates ROS production, is dependent on the phosphorylation of p38-mitogen-activated protein kinase (p38-MAPK). This is known to lead to tumor necrosis factor-α and monocyte chemoattractant protein-1 expression, thus enhancing a pro-inflammatory phenotype [78]. Nevertheless, the direct effects of Cannabinoids on macrophage phenotype and function have not been thoroughly tested.
Finally, it is important to note that in the present epidemic of metabolic diseases and obesity that drive various cancers, phytocannabinoids, particularly THC, act in a manner similar to metformin. Metformin is a mild inhibitor of complex 1 of the mitochondria, and therefore is thought to play an important role in metabolic reprogramming. While long term use of metformin has been linked with risk of cardiomyopathy, the effect of chronic use of phytocannabinoids and synthetic cannabinoids on systemic health, while predictable based on several studies, may need to be performed specifically in the context of cancer survivor cohorts [79].
4.5 Recent Advances of Cannabinoids in Clinical Trials
The use and understanding of mechanisms of cannabinoids in context of tumors are almost completely limited to preclinical studies. Nevertheless, its lower toxicity led it to the first clinical application of THC on humans, conducted on nine terminal patients with recurrent glioblastoma and resistant to standard chemotherapy [85]. THC was administered intra-tumorally and dose was determined to be safe and without any psychoactive effects [80]. Furthermore, this study also confirmed the anti-proliferative action and induction of apoptosis induced by THC, however, further studies are needed to determine the correct dosage or any potent systemic interaction [80]. There have been some clinical trials currently ongoing or recently completed using combinatorial treatments of nabiximols and temozolomide in patients with recurrent glioblastoma (NCT01812603, NCT01812616). Another clinical study was conducted using Cannabidoil as a single regimen on different solid tumor patients (NCT02255292). In addition, many recent clinical studies also underscore the promising therapeutic potential of one of the synthetic cannabinoids, dexanabinol, in patients with different solid tumors or brain cancer, compared with other healthy subjects (NCT01489826, NCT01654497, and NCT02054754).
4.6 Concluding Remarks
In summary, cannabinoid modulates the tumor growth and metastasis in different human malignancies by regulating different signaling cascades linked with proliferation, survival, angiogenesis and metastatic spread of cancer cells. It can also regulate the TME by regulating different types of immune cells associated with pro and anti-tumor immunity. Cannabinoid may induce ROS generation and lower mitochondrial activity in cancer cells, leading to autophagy and cell death. Cannabinoid also cross-talks with cellular metabolism via AMPK and mTOR, subsequently enhancing cancer cell death. Overall, application of cannabinoid will have high translational significance and impact for developing novel immune and metabolic-based therapies directed against different metastatic cancers with minimal to low side effects.
Abbreviations
- 2-AG:
-
2-arachindonoylglycerol
- AEA:
-
anandamide
- AMPK:
-
5′ AMP-activated protein kinase
- CBD:
-
cannabinoids
- CBR:
-
cannabinoid receptor
- COX-2:
-
cyclooxygenase-2
- CXCL:
-
C-X-C motif chemokine ligand
- EGFR:
-
epidermal growth factor receptor
- EMT:
-
epithelial to mesenchymal transition
- E:R:
-
endoplasmic reticulum
- mTOR:
-
mammalian target of rapamycin
- PPAR:
-
peroxisome proliferator-activated receptors
- ROS:
-
reactive oxygen species
- TAMs:
-
tumor associated macrophages
- THC:
-
Δ9-tetrahydrocannabinol
- TME:
-
tumor microenvironment
- TRPV2:
-
transient receptor potential cation channel subfamily V member 2.
References
Navarro G, Varani K, Reyes-Resina I, Sanchez de Medina V, Rivas-Santisteban R, Sanchez-Carnerero Callado C, Vincenzi F, Casano S, Ferreiro-Vera C, Canela EI, Borea PA, Nadal X, Franco R (2018) Cannabigerol action at cannabinoid CB1 and CB2 receptors and at CB1-CB2 heteroreceptor complexes. Front Pharmacol 9:632
Wang J, Wang Y, Tong M, Pan H, Li D (2019) New prospect for cancer cachexia: medical cannabinoid. J Cancer 10:716–720
Kramer JL (2015) Medical marijuana for cancer. CA Cancer J Clin 65:109–122
Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, Greasley PJ, Hansen HS, Kunos G, Mackie K, Mechoulam R, Ross RA (2010) International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB(1) and CB(2). Pharmacol Rev 62:588–631
Fernandez-Ruiz J, Romero J, Velasco G, Tolon RM, Ramos JA, Guzman M (2007) Cannabinoid CB2 receptor: a new target for controlling neural cell survival? Trends Pharmacol Sci 28:39–45
Katona I, Freund TF (2008) Endocannabinoid signaling as a synaptic circuit breaker in neurological disease. Nat Med 14:923–930
Stempel AV, Stumpf A, Zhang HY, Ozdogan T, Pannasch U, Theis AK, Otte DM, Wojtalla A, Racz I, Ponomarenko A, Xi ZX, Zimmer A, Schmitz D (2016) Cannabinoid Type 2 receptors mediate a cell type-specific plasticity in the hippocampus. Neuron 90:795–809
Li X, Hua T, Vemuri K, Ho JH, Wu Y, Wu L, Popov P, Benchama O, Zvonok N, Locke K, Qu L, Han GW, Iyer MR, Cinar R, Coffey NJ, Wang J, Wu M, Katritch V, Zhao S, Kunos G, Bohn LM, Makriyannis A, Stevens RC, Liu ZJ (2019) Crystal structure of the human cannabinoid receptor CB2. Cell 176:459–67.e13
Davis MP (2016) Cannabinoids for symptom management and cancer therapy: the evidence. J Natl Compr Cancer Netw 14:915–922
Fowler CJ (2015) Delta(9) -tetrahydrocannabinol and cannabidiol as potential curative agents for cancer: a critical examination of the preclinical literature. Clin Pharmacol Ther 97:587–596
Solinas M, Massi P, Cantelmo AR, Cattaneo MG, Cammarota R, Bartolini D, Cinquina V, Valenti M, Vicentini LM, Noonan DM, Albini A, Parolaro D (2012) Cannabidiol inhibits angiogenesis by multiple mechanisms. Br J Pharmacol 167:1218–1231
Panatier A, Vallee J, Haber M, Murai KK, Lacaille JC, Robitaille R (2011) Astrocytes are endogenous regulators of basal transmission at central synapses. Cell 146:785–798
Galve-Roperh I, Sanchez C, Cortes ML, Gomez del Pulgar T, Izquierdo M, Guzman M (2000) Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat Med 6:313–319
Carracedo A, Lorente M, Egia A, Blazquez C, Garcia S, Giroux V, Malicet C, Villuendas R, Gironella M, Gonzalez-Feria L, Piris MA, Iovanna JL, Guzman M, Velasco G (2006) The stress-regulated protein p8 mediates cannabinoid-induced apoptosis of tumor cells. Cancer Cell 9:301–312
Jia W, Hegde VL, Singh NP, Sisco D, Grant S, Nagarkatti M, Nagarkatti PS (2006) Delta9-tetrahydrocannabinol-induced apoptosis in Jurkat leukemia T cells is regulated by translocation of Bad to mitochondria. Mol Cancer Res 4:549–562
Greenhough A, Patsos HA, Williams AC, Paraskeva C (2007) The cannabinoid delta(9)-tetrahydrocannabinol inhibits RAS-MAPK and PI3K-AKT survival signalling and induces BAD-mediated apoptosis in colorectal cancer cells. Int J Cancer 121:2172–2180
Vara D, Salazar M, Olea-Herrero N, Guzman M, Velasco G, Diaz-Laviada I (2011) Anti-tumoral action of cannabinoids on hepatocellular carcinoma: role of AMPK-dependent activation of autophagy. Cell Death Differ 18:1099–1111
Torres S, Lorente M, Rodriguez-Fornes F, Hernandez-Tiedra S, Salazar M, Garcia-Taboada E, Barcia J, Guzman M, Velasco G (2011) A combined preclinical therapy of cannabinoids and temozolomide against glioma. Mol Cancer Ther 10:90–103
Caffarel MM, Sarrio D, Palacios J, Guzman M, Sanchez C (2006) Delta9-tetrahydrocannabinol inhibits cell cycle progression in human breast cancer cells through Cdc2 regulation. Cancer Res 66:6615–6621
Caffarel MM, Moreno-Bueno G, Cerutti C, Palacios J, Guzman M, Mechta-Grigoriou F, Sanchez C (2008) JunD is involved in the antiproliferative effect of Delta9-tetrahydrocannabinol on human breast cancer cells. Oncogene 27:5033–5044
Vara D, Morell C, Rodriguez-Henche N, Diaz-Laviada I (2013) Involvement of PPARgamma in the antitumoral action of cannabinoids on hepatocellular carcinoma. Cell Death Dis 4:e618
McAllister SD, Soroceanu L, Desprez PY (2015) The antitumor activity of plant-derived non-psychoactive cannabinoids. J NeuroImmune Pharmacol 10:255–267
Ramer R, Heinemann K, Merkord J, Rohde H, Salamon A, Linnebacher M, Hinz B (2013) COX-2 and PPAR-gamma confer cannabidiol-induced apoptosis of human lung cancer cells. Mol Cancer Ther 12:69–82
Elbaz M, Nasser MW, Ravi J, Wani NA, Ahirwar DK, Zhao H, Oghumu S, Satoskar AR, Shilo K, Carson WE 3rd, Ganju RK (2015) Modulation of the tumor microenvironment and inhibition of EGF/EGFR pathway: novel anti-tumor mechanisms of Cannabidiol in breast cancer. Mol Oncol 9:906–919
Qamri Z, Preet A, Nasser MW, Bass CE, Leone G, Barsky SH, Ganju RK (2009) Synthetic cannabinoid receptor agonists inhibit tumor growth and metastasis of breast cancer. Mol Cancer Ther 8:3117–3129
Grimaldi C, Pisanti S, Laezza C, Malfitano AM, Santoro A, Vitale M, Caruso MG, Notarnicola M, Iacuzzo I, Portella G, Di Marzo V, Bifulco M (2006) Anandamide inhibits adhesion and migration of breast cancer cells. Exp Cell Res 312:363–373
Preet A, Ganju RK, Groopman JE (2008) Delta9-Tetrahydrocannabinol inhibits epithelial growth factor-induced lung cancer cell migration in vitro as well as its growth and metastasis in vivo. Oncogene 27:339–346
Guzman M (2003) Cannabinoids: potential anticancer agents. Nat Rev Cancer 3:745–755
Nasser MW, Qamri Z, Deol YS, Smith D, Shilo K, Zou X, Ganju RK (2011) Crosstalk between chemokine receptor CXCR4 and cannabinoid receptor CB2 in modulating breast cancer growth and invasion. PLoS One 6:e23901
Lombard C, Nagarkatti M, Nagarkatti P (2007) CB2 cannabinoid receptor agonist, JWH-015, triggers apoptosis in immune cells: potential role for CB2-selective ligands as immunosuppressive agents. Clin Immunol 122:259–270
McKallip RJ, Jia W, Schlomer J, Warren JW, Nagarkatti PS, Nagarkatti M (2006) Cannabidiol-induced apoptosis in human leukemia cells: a novel role of cannabidiol in the regulation of p22phox and Nox4 expression. Mol Pharmacol 70:897–908
Tajbakhsh A, Mokhtari-Zaer A, Rezaee M, Afzaljavan F, Rivandi M, Hassanian SM, Ferns GA, Pasdar A, Avan A (2017) Therapeutic potentials of BDNF/TrkB in breast cancer; current status and perspectives. J Cell Biochem 118:2502–2515
Binabaj MM, Bahrami A, ShahidSales S, Joodi M, Joudi Mashhad M, Hassanian SM, Anvari K, Avan A (2018) The prognostic value of MGMT promoter methylation in glioblastoma: a meta-analysis of clinical trials. J Cell Physiol 233:378–386
Qian BZ, Pollard JW (2010) Macrophage diversity enhances tumor progression and metastasis. Cell 141:39–51
Lin CY, Lin CJ, Chen KH, Wu JC, Huang SH, Wang SM (2006) Macrophage activation increases the invasive properties of hepatoma cells by destabilization of the adherens junction. FEBS Lett 580:3042–3050
Ruffell B, Affara NI, Coussens LM (2012) Differential macrophage programming in the tumor microenvironment. Trends Immunol 33:119–126
Liu CY, Xu JY, Shi XY, Huang W, Ruan TY, Xie P, Ding JL (2013) M2-polarized tumor-associated macrophages promoted epithelial-mesenchymal transition in pancreatic cancer cells, partially through TLR4/IL-10 signaling pathway. Lab Investig 93:844–854
Chanmee T, Ontong P, Konno K, Itano N (2014) Tumor-associated macrophages as major players in the tumor microenvironment. Cancers (Basel) 6:1670–1690
Ravi J, Elbaz M, Wani NA, Nasser MW, Ganju RK (2016) Cannabinoid receptor-2 agonist inhibits macrophage induced EMT in non-small cell lung cancer by downregulation of EGFR pathway. Mol Carcinog 55:2063–2076
Croxford JL, Yamamura T (2005) Cannabinoids and the immune system: potential for the treatment of inflammatory diseases? J Neuroimmunol 166:3–18
Borner C, Smida M, Hollt V, Schraven B, Kraus J (2009) Cannabinoid receptor type 1- and 2-mediated increase in cyclic AMP inhibits T cell receptor-triggered signaling. J Biol Chem 284:35450–35460
Zhu LX, Sharma S, Stolina M, Gardner B, Roth MD, Tashkin DP, Dubinett SM (2000) Delta-9-tetrahydrocannabinol inhibits antitumor immunity by a CB2 receptor-mediated, cytokine-dependent pathway. J Immunol 165:373–380
Jenny M, Schrocksnadel S, Uberall F, Fuchs D (2010) The potential role of cannabinoids in modulating serotonergic signaling by their influence on tryptophan metabolism. Pharmaceuticals (Basel) 3:2647–2660
Newton CA, Klein TW, Friedman H (1994) Secondary immunity to Legionella pneumophila and Th1 activity are suppressed by delta-9-tetrahydrocannabinol injection. Infect Immun 62:4015–4020
Vieweg J, Su Z, Dahm P, Kusmartsev S (2007) Reversal of tumor-mediated immunosuppression. Clin Cancer Res 13:727s–732s
Chen WL, Wang JH, Zhao AH, Xu X, Wang YH, Chen TL, Li JM, Mi JQ, Zhu YM, Liu YF, Wang YY, Jin J, Huang H, Wu DP, Li Y, Yan XJ, Yan JS, Li JY, Wang S, Huang XJ, Wang BS, Chen Z, Chen SJ, Jia W (2014) A distinct glucose metabolism signature of acute myeloid leukemia with prognostic value. Blood 124:1645–1654
Staubert C, Bhuiyan H, Lindahl A, Broom OJ, Zhu Y, Islam S, Linnarsson S, Lehtio J, Nordstrom A (2015) Rewired metabolism in drug-resistant leukemia cells: a metabolic switch hallmarked by reduced dependence on exogenous glutamine. J Biol Chem 290:8348–8359
Vander Heiden MG, DeBerardinis RJ (2017) Understanding the intersections between metabolism and cancer biology. Cell 168:657–669
Pavlova NN, Thompson CB (2016) The emerging hallmarks of cancer metabolism. Cell Metab 23:27–47
Bosc C, Selak MA, Sarry JE (2017) Resistance is futile: targeting mitochondrial energetics and metabolism to overcome drug resistance in cancer treatment. Cell Metab 26:705–707
Anderson RG, Ghiraldeli LP, Pardee TS (2018) Mitochondria in cancer metabolism, an organelle whose time has come? Biochim Biophys Acta Rev Cancer 1870:96–102
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348:1625–1638
Goodwin PJ (2015) Obesity, insulin resistance and breast cancer outcomes. Breast 24(Suppl 2):S56–S59
Koivunen J, Aaltonen V, Peltonen J (2006) Protein kinase C (PKC) family in cancer progression. Cancer Lett 235:1–10
Faubert B, Vincent EE, Poffenberger MC, Jones RG (2015) The AMP-activated protein kinase (AMPK) and cancer: many faces of a metabolic regulator. Cancer Lett 356:165–170
Cooke M, Magimaidas A, Casado-Medrano V, Kazanietz MG (2017) Protein kinase C in cancer: the top five unanswered questions. Mol Carcinog 56:1531–1542
Yap TA, Bjerke L, Clarke PA, Workman P (2015) Drugging PI3K in cancer: refining targets and therapeutic strategies. Curr Opin Pharmacol 23:98–107
Panieri E, Santoro MM (2016) ROS homeostasis and metabolism: a dangerous liason in cancer cells. Cell Death Dis 7:e2253
Legaspi A, Jeevanandam M, Starnes HF Jr, Brennan MF (1987) Whole body lipid and energy metabolism in the cancer patient. Metabolism 36:958–963
Liu Y (2006) Fatty acid oxidation is a dominant bioenergetic pathway in prostate cancer. Prostate Cancer Prostatic Dis 9:230–234
Bian Y, Yu Y, Wang S, Li L (2015) Up-regulation of fatty acid synthase induced by EGFR/ERK activation promotes tumor growth in pancreatic cancer. Biochem Biophys Res Commun 463:612–617
Xu RH, Pelicano H, Zhou Y, Carew JS, Feng L, Bhalla KN, Keating MJ, Huang P (2005) Inhibition of glycolysis in cancer cells: a novel strategy to overcome drug resistance associated with mitochondrial respiratory defect and hypoxia. Cancer Res 65:613–621
Kumar R, Coronel L, Somalanka B, Raju A, Aning OA, An O, Ho YS, Chen S, Mak SY, Hor PY, Yang H, Lakshmanan M, Itoh H, Tan SY, Lim YK, Wong APC, Chew SH, Huynh TH, Goh BC, Lim CY, Tergaonkar V, Cheok CF (2018) Mitochondrial uncoupling reveals a novel therapeutic opportunity for p53-defective cancers. Nat Commun 9:3931
Burt ME, Stein TP, Schwade JG, Brennan MF (1984) Whole-body protein metabolism in cancer-bearing patients. Effect of total parenteral nutrition and associated serum insulin response. Cancer 53:1246–1252
Lim CT, Kola B, Feltrin D, Perez-Tilve D, Tschop MH, Grossman AB, Korbonits M (2013) Ghrelin and cannabinoids require the ghrelin receptor to affect cellular energy metabolism. Mol Cell Endocrinol 365:303–308
Ding L, Getz G, Wheeler DA, Mardis ER, McLellan MD, Cibulskis K, Sougnez C, Greulich H, Muzny DM, Morgan MB, Fulton L, Fulton RS, Zhang Q, Wendl MC, Lawrence MS, Larson DE, Chen K, Dooling DJ, Sabo A, Hawes AC, Shen H, Jhangiani SN, Lewis LR, Hall O, Zhu Y, Mathew T, Ren Y, Yao J, Scherer SE, Clerc K, Metcalf GA, Ng B, Milosavljevic A, Gonzalez-Garay ML, Osborne JR, Meyer R, Shi X, Tang Y, Koboldt DC, Lin L, Abbott R, Miner TL, Pohl C, Fewell G, Haipek C, Schmidt H, Dunford-Shore BH, Kraja A, Crosby SD, Sawyer CS, Vickery T, Sander S, Robinson J, Winckler W, Baldwin J, Chirieac LR, Dutt A, Fennell T, Hanna M, Johnson BE, Onofrio RC, Thomas RK, Tonon G, Weir BA, Zhao X, Ziaugra L, Zody MC, Giordano T, Orringer MB, Roth JA, Spitz MR, Wistuba II, Ozenberger B, Good PJ, Chang AC, Beer DG, Watson MA, Ladanyi M, Broderick S, Yoshizawa A, Travis WD, Pao W, Province MA, Weinstock GM, Varmus HE, Gabriel SB, Lander ES, Gibbs RA, Meyerson M, Wilson RK (2008) Somatic mutations affect key pathways in lung adenocarcinoma. Nature 455:1069–1075
Phoenix KN, Vumbaca F, Claffey KP (2009) Therapeutic metformin/AMPK activation promotes the angiogenic phenotype in the ERalpha negative MDA-MB-435 breast cancer model. Breast Cancer Res Treat 113:101–111
Baba Y, Nosho K, Shima K, Meyerhardt JA, Chan AT, Engelman JA, Cantley LC, Loda M, Giovannucci E, Fuchs CS, Ogino S (2010) Prognostic significance of AMP-activated protein kinase expression and modifying effect of MAPK3/1 in colorectal cancer. Br J Cancer 103:1025–1033
William WN, Kim JS, Liu DD, Solis L, Behrens C, Lee JJ, Lippman SM, Kim ES, Hong WK, Wistuba II, Lee HY (2012) The impact of phosphorylated AMP-activated protein kinase expression on lung cancer survival. Ann Oncol 23:78–85
Sozio MS, Lu C, Zeng Y, Liangpunsakul S, Crabb DW (2011) Activated AMPK inhibits PPAR-{alpha} and PPAR-{gamma} transcriptional activity in hepatoma cells. Am J Physiol Gastrointest Liver Physiol 301:G739–G747
Currie E, Schulze A, Zechner R, Walther TC, Farese RV Jr (2013) Cellular fatty acid metabolism and cancer. Cell Metab 18:153–161
Dando I, Donadelli M, Costanzo C, Dalla Pozza E, D’Alessandro A, Zolla L, Palmieri M (2013) Cannabinoids inhibit energetic metabolism and induce AMPK-dependent autophagy in pancreatic cancer cells. Cell Death Dis 4:e664
Tedesco L, Valerio A, Dossena M, Cardile A, Ragni M, Pagano C, Pagotto U, Carruba MO, Vettor R, Nisoli E (2010) Cannabinoid receptor stimulation impairs mitochondrial biogenesis in mouse white adipose tissue, muscle, and liver: the role of eNOS, p38 MAPK, and AMPK pathways. Diabetes 59:2826–2836
Kim W, Doyle ME, Liu Z, Lao Q, Shin YK, Carlson OD, Kim HS, Thomas S, Napora JK, Lee EK, Moaddel R, Wang Y, Maudsley S, Martin B, Kulkarni RN, Egan JM (2011) Cannabinoids inhibit insulin receptor signaling in pancreatic beta-cells. Diabetes 60:1198–1209
Liu J, Zhou L, Xiong K, Godlewski G, Mukhopadhyay B, Tam J, Yin S, Gao P, Shan X, Pickel J, Bataller R, O’Hare J, Scherer T, Buettner C, Kunos G (2012) Hepatic cannabinoid receptor-1 mediates diet-induced insulin resistance via inhibition of insulin signaling and clearance in mice. Gastroenterology 142:1218–1228.e1
Singh N, Hroudova J, Fisar Z (2015) Cannabinoid-induced changes in the activity of electron transport chain complexes of brain mitochondria. J Mol Neurosci 56:926–931
Donadelli M, Dando I, Zaniboni T, Costanzo C, Dalla Pozza E, Scupoli MT, Scarpa A, Zappavigna S, Marra M, Abbruzzese A, Bifulco M, Caraglia M, Palmieri M (2011) Gemcitabine/cannabinoid combination triggers autophagy in pancreatic cancer cells through a ROS-mediated mechanism. Cell Death Dis 2:e152
Han KH, Lim S, Ryu J, Lee CW, Kim Y, Kang JH, Kang SS, Ahn YK, Park CS, Kim JJ (2009) CB1 and CB2 cannabinoid receptors differentially regulate the production of reactive oxygen species by macrophages. Cardiovasc Res 84:378–386
Hall W, Christie M, Currow D (2005) Cannabinoids and cancer: causation, remediation, and palliation. Lancet Oncol 6:35–42
Guzman M, Duarte MJ, Blazquez C, Ravina J, Rosa MC, Galve-Roperh I, Sanchez C, Velasco G, Gonzalez-Feria L (2006) A pilot clinical study of Delta9-tetrahydrocannabinol in patients with recurrent glioblastoma multiforme. Br J Cancer 95:197–203
Acknowledgements
This work is supported in part by the Department of Defense Level II Breakthrough Award and Pelotonia IDEA Award.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Das, S., Kaul, K., Mishra, S., Charan, M., Ganju, R.K. (2019). Cannabinoid Signaling in Cancer. In: Bukiya, A. (eds) Recent Advances in Cannabinoid Physiology and Pathology. Advances in Experimental Medicine and Biology, vol 1162. Springer, Cham. https://doi.org/10.1007/978-3-030-21737-2_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-21737-2_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21736-5
Online ISBN: 978-3-030-21737-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)