Abstract
Cryopreservation is a technique that can keep sperm alive indefinitely, enabling the conservation of male fertility. It involves the cooling of semen samples and their storage at −196 °C in liquid nitrogen. At this temperature all metabolic processes are arrested. Sperm cryopreservation is of fundamental importance for patients undergoing medical or surgical treatments that could induce sterility, such as cancer patients about to undergo genotoxic chemotherapy or radiotherapy, as it offers these patients not only the hope of future fertility but also psychological support in dealing with the various stages of the treatment protocols.
Despite its importance for assisted reproduction technology (ART) and its success in terms of babies born, this procedure can cause cell damage and impaired sperm function. Various studies have evaluated the impact of cryopreservation on chromatin structure, albeit with contradictory results. Some, but not all, authors found significant sperm DNA damage after cryopreservation. However, studies attempting to explain the mechanisms involved in the aetiology of cryopreservation-induced DNA damage are still limited. Some reported an increase in sperm with activated caspases after cryopreservation, while others found an increase in the percentage of oxidative DNA damage. There is still little and contradictory information on the mechanism of the generation of DNA fragmentation after cryopreservation. A number of defensive strategies against cryoinjuries have been proposed in the last decade. Most studies focused on supplementing cryoprotectant medium with various antioxidant molecules, all aimed at minimising oxidative damage and thus improving sperm recovery. Despite the promising results, identification of the ideal antioxidant treatment method is still hampered by the heterogeneity of the studies, which describe the use of different antioxidant regimens at different concentrations or in different combinations. For this reason, additional studies are needed to further investigate the use of antioxidants, individually and in combination, in the cryopreservation of human sperm, to determine the most beneficial conditions for optimal sperm recovery and preservation of fertility.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Semen cryopreservation
- Sperm DNA damage
- Male fertility preservation
- Antioxidant supplementation
- Cryoprotectant
Sperm Cryopreservation
Cryopreservation is a technique that can keep sperm alive indefinitely, thus enabling male fertility to be conserved. It is of fundamental importance for patients undergoing medical or surgical treatments that could induce sterility, such as cancer patients about to undergo genotoxic chemotherapy or radiotherapy. Testicular cancer and Hodgkin’s and non-Hodgkin’s disease are the most common conditions in patients cryopreserving their sperm, as they mainly affect males of childbearing age. Despite their serious disease, sperm cryopreservation offers these patients the hope of future fertility; this is not only reassuring in relation to their possibility of fatherhood but is also a psychological support when dealing with the various stages of the treatment protocols, as it permits them to envision the prospect of their survival (Saito et al. 2005).
Advances in cancer treatments and increasingly sophisticated assisted reproduction techniques (ART) have opened up new possibilities for infertile men; cryopreservation is thus also indicated even for severely damaged sperm that would have had no reproductive capacity in the pre-ICSI era. Given the potential importance of reproduction for these patients, who are often young and childless, it is essential that this option is recommended by specialists and offered as quickly and efficiently as possible. Cancer patients must thus be informed of this possibility before undergoing any treatment that might have an irreversible effect on their ability to father a child, and cryopreservation must be performed before beginning any such treatment.
Sperm Cryobiology
The ability to store cells indefinitely in a state of ‘suspended animation’ was a pivotal event in reproductive medicine. In the last 60 years, the cryobiology of gametes, testicular tissue, embryos and, recently, ovarian tissue has been studied in parallel to the development of ART. The first attempt at freezing semen dates back to 1776, when abbot Lazzaro Spallanzani reported that sperm could be stored by cooling in snow. In 1800, Paolo Mantegazza came up with the idea of the sperm bank, to ensure the continued linage of soldiers going off to war. Discussion of cryopreservation began when Rostand in 1946 and Polge in 1949 discovered that glycerol could act as a cryoprotectant, while in 1953 Bunge and Sherman reported three pregnancies after insemination with sperm that had been treated with glycerol and frozen in dry ice. The discovery that glycerol protected sperm cells from freezing damage enabled human semen to be stored in dry ice at −78 °C (Polge et al. 1949; Bunge and Sherman 1953; Bunge et al. 1954). However, later studies by Sherman (1963) demonstrated that sperm stored in liquid nitrogen at −196 °C could be kept even longer and, moreover, conserved flagellar movement after thawing. In fact, molecular movements, and hence the biochemical processes of cell metabolism, stop at extremely low temperatures, recommencing once the cell has thawed.
Cell life depends on the simultaneous interactions of various chemical reactions, kept in balance through homoeostatic control mechanisms. Long-term storage is thus only possible by minimising these reactions by lowering the temperature until life is ‘cryogenically suspended’. In liquid nitrogen at −196 °C, no chemical reaction can take place as there is insufficient thermal energy at this temperature. In fact, below −130 °C, water exists in a crystalline or vitreous state, in which its viscosity is so high as to limit its diffusion (Mazur 1984). The chemical and physical phenomena which arise during cooling of cells and tissues affect the viability of the system, reducing enzyme activity and active transport mechanisms, changing membrane conformation and causing transmembrane ion loss.
However, the main problem the cell must overcome during cooling is the transition of water to ice. Water plays an important role in cell life, acting as an intra- and extracellular carrier of hydrophilic structures such as proteins, metabolites and ions. During freeze-thaw phase changes, the concentrations of solutes in intra- and extracellular aqueous solutions vary considerably. Such intra- and extracellular changes are the greatest biological problem encountered with freezing. In fact, the solutes in the aqueous medium in which the cells are suspended take its freezing point down to −10 to −15 °C, i.e. below that of pure water (0 °C). At these low temperatures, the water in the extracellular environment freezes, increasing the concentration of the solutes. This generates osmotic pressure, causing solvent to flow through the plasma membrane, from inside to outside the cell. This extracellular need for water leads to a reduction in cell volume and then to dehydration, a process which is essential to protect cells from the formation of intracellular ice, which can cause them to die. However, this intense dehydration process can reach a point of no return (at about 40% of the original cell volume), at which the cell suffers permanent damage.
The extent of dehydration depends mainly on the cooling rate. If the cell is cooled very quickly, dehydration may not be complete and intracellular ice crystals can form. In this case, there is no osmosis or volume change, but on thawing there may be mechanical damage to the membrane and subcellular organelles. In contrast, if the cell is cooled very slowly, extracellular water freezes before intracellular water, due to the protective effect of the cell membrane. The extracellular environment thus becomes hypertonic, causing water to flow from inside to outside the cell, resulting in excessive dehydration.
During thawing, reverse osmosis takes place. As soon as the water passes from the solid to the liquid state, the concentration of extracellular solutes drops steadily, and the cells rehydrate to compensate for the different extra- and intracellular concentrations.
Cell survival after freezing/thawing thus depends on the ability to minimise the formation of intracellular ice crystals. It should therefore be optimised by establishing a cooling rate which enables the cell to remain in equilibrium with the extracellular solution. An intermediate rate is needed: fast enough not to cause excessive solute concentration but slow enough to avoid intracellular crystallisation.
The ability of a cell to survive freezing also depends on its shape, size, water content, permeability and membrane lipid composition. Human sperm can tolerate a series of temperature variations and are fairly resistant to damage caused by rapid cooling, due to the unsaturated fatty acids in the lipid bilayer (65–70% phospholipids – side chains of docosahexaenoic acid), which lead to high membrane fluidity (Clarke et al. 2003); their small cell size; and the compact cellular organisation of the head. Their low water content (around 50%) may also make them more resistant than other cells to freezing damage. Nevertheless, motility is generally reduced by 30–50% upon thawing.
Cryoprotectant media containing low molecular weight compounds that modify the cell environment are used to try to obviate these problems. By replacing the water content, they keep the extracellular environment in the liquid phase even when the temperature drops below freezing point. These substances have been defined as ‘any additive which can be provided to cells before freezing and yields a higher post-thaw survival than can be obtained in its absence’ (Karow 1974). Although the chemical composition of these cryoprotectants differs, they are all highly water soluble and have a concentration-dependent toxicity. They work directly on the cell membrane through electrostatic interactions, lowering the freezing point of the solution and modifying the intra- and extracellular environment as their displacement of the water reduces both the formation of ice crystals and the quantity of salt and solutes in the liquid phase.
There are two main classes of cryoprotectants:
-
Permeating cryoprotectants , which penetrate the cell membrane. This class includes dimethyl sulfoxide (DMSO), glycerol, 1,2-propanediol (PROH) and ethylene glycol. These hydrophilic substances have a molecular weight of <400 Da and cross the membrane very easily, creating an osmotic gradient and causing water to leave the cell by lowering the freezing point even further.
-
Non-permeating cryoprotectants , which do not cross the cell membrane. These include sucrose, fructose, glucose, dextrose, starch, lipoproteins and polyvinylpyrrolidone (PVP). These large molecules with a molecular weight of >1000 Da increase the concentration of extracellular solutes, thus generating an osmotic gradient that causes water to leave the cell, causing dehydration before freezing takes place.
Glycerol is the most commonly used cryoprotectant for human sperm. It acts on the membrane structure, the permeability and stability of the lipid bilayer, the association of surface proteins and cell metabolism (Fabbri et al. 2004). However, Sherman (1990) showed that the use of glycerol alone can damage the plasma membrane, the inner acrosomal membrane, the nucleus and the mitochondrial cristae. Other substances such as DMSO and PROH were used subsequently, but with little success, due to their harmful effects on human sperm.
Almost all cryoprotectant media contain glycerol, to protect against thermal shock; sugars, which provide the sperm with energy and optimise osmolarity and hydrogen ion concentration; egg yolk, which improves the fluidity of the cytoplasmic membrane, provides structural and functional protection and, through its lipoprotein content, safeguards sperm integrity; and antibiotics, to protect against any microorganisms that might be present. Cryopreservation is carried out in nitrogen vapour with one of two techniques, leading to either slow or fast freezing.
Cryopreservation Methods
Rapid freezing
Rapid freezing was first proposed by Sherman (1990). It does not require automatic equipment. The most common technique is vertical freezing, carried out in cryogenic containers of a suitable size. Semen samples are diluted with cryoprotectant media and left to equilibrate at 37 °C for 10 minutes. The suspension is aspirated with a vacuum pump into 300 or 500 μL straws. The straws are sealed and placed in nitrogen vapour for 8 minutes and then immersed in liquid nitrogen at −196 °C. Nitrogen vapour contains a thermal gradient depending on the distance from the surface of the liquid nitrogen and the volume of underlying liquid. The straws are placed 15–20 cm above the liquid (Fabbri et al. 2004) and are then slowly lowered to reach the surface before being raised once more. This gives a fast freezing rate (about 20 °C/min). Following this phase, the straws are plunged in liquid nitrogen.
Slow freezing
This was proposed by Behrman and Sawada (1966). It uses automatic equipment which takes cells from room temperature to the storage temperature at a controlled rate. The sample is first diluted with cryoprotectant and then taken from room temperature to 5 °C at a rate of 0.5–1 °C/min (Mahadevan and Trounson 1984). The temperature is then lowered to −80 °C at 1–10 °C/min, and finally the sample is plunged in liquid nitrogen (Thachil and Jewett 1981). However, this method can cause ice crystals to form if the freezing rate is too fast or too slow.
In both of these methods, the cells are exposed to cryoprotectant before freezing to protect them from cooling damage. This stage is called conditioning. The efficacy of cryoprotectant is a function of how long the cryoprotectant and the cells have to interact and the temperature at which this exposure takes place. For this reason, cryoprotectant medium is added drop by drop and mixed gently to avoid osmotic stress and the mixture incubated at 37 °C for 10 to 15 minutes to allow the cells and medium to equilibrate. Another important point is that the thawing techniques must enable the cells to recover their normal biological activities, minimising fast temperature changes as much as possible. For this reason, the straws are extracted very slowly, to enable a thermal equilibrium between the cells and the external environment to be reached. Different protocols can be used: (1) straws are kept at room temperature for 10 minutes and then incubated at 37 °C for 10 minutes; (2) straws are placed in a thermostatic bath at 37 °C for 10 minutes; and (3) straws are thawed at room temperature (22 °C) for 15 min.
Effect of Cryopreservation on DNA Integrity
Damage can take place not only during freezing but also during thawing. On thawing, ice crystals can cause mechanical damage to the subcellular organelles. Various studies have shown that the damage induced by cryopreservation can affect the integrity of the plasma membrane (Arav et al. 1996; Zeron et al. 1999), which contains phospholipids and cholesterol (Giraud et al. 2000). The latter authors showed that the freeze-thaw process induces a rigidifying effect on the sperm membrane and suggested that the adaptability of mammalian sperm to freeze-thaw-induced stress, and hence its ability to withstand cryopreservation, might depend on the fluidity of its membrane, which is in turn modulated by the membrane’s lipid composition (Giraud et al. 2000).
Human and rabbit sperm are less sensitive to cryopreservation than sperm from other animals, such as rams and bulls, due to the different lipid composition of the sperm plasma membrane (Bailey et al. 2000). In bull and ram sperm, the membrane contains less cholesterol and a higher ratio of unsaturated and saturated fatty acids than found in human sperm. Nevertheless, during cryopreservation of human sperm, the cooling process can cause a membrane lipid phase change as well as functional damage to the intramembrane proteins responsible for ion transport (Oehninger et al. 2000). The sperm plasma membrane contains a glycocalyx of oligosaccharide chains bound to intramembrane proteins and lipids. Cryopreservation can have adverse effects on the composition of carbohydrates in the glycocalyx, thus interfering with the function of intramembrane proteins (Benoff 1997) and with other physiological functions such as immunological protection (Cross and Overstreet 1987) and acrosome reaction (Lassalle and Testart 1994).
Cryopreservation also has adverse effects on sperm motility and speed, due to membrane swelling and acrosome degeneration. Fatty acids, which are abundant in the sperm membrane (Halliwell and Gutterridge 1984), are also vulnerable to peroxidation; this can not only damage the plasma membrane but also cause a loss of intracellular enzymes and inhibit oxidative phosphorylation (White 1993). The mitochondrial membrane is in fact susceptible to damage at low temperatures, and a change in membrane fluidity can affect its potential and cause the release of reactive oxygen species (ROS) (Said et al. 2010).
Given that the antioxidant activity of sperm is also reduced by cryopreservation, it is clear that sperm are susceptible to ROS damage (Lasso et al. 1994). This damage may involve single- or double-DNA strand breakage. Various studies have examined how ROS form during cryopreservation and thawing. Mazzilli et al. (1995) studied 45 subjects for the presence of ROS in sperm selected by swim-up before and after cryopreservation in liquid nitrogen. After cryopreservation, 42.2% of samples showed an increase in ROS and 20% an increase in free radicals, which were absent prior to freezing. The study suggested that cryopreservation procedures can induce or increase ROS production in some semen samples. After thawing, samples with ROS showed reduced motility and viability in comparison with ROS-free samples. High ROS concentrations and the loss of antioxidants can also trigger apoptosis (Wang et al. 2003).
Thawing can also cause sperm DNA damage. In fact, some studies have shown that DNA fragmentation increases during the first 4 hours after thawing. For this reason, sperm should be used rapidly after thawing (Gosálvez et al. 2009).
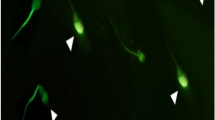
The various studies of DNA integrity after cryopreservation and thawing produced conflicting results. Some, but not all, authors found significant sperm DNA damage after cryopreservation. Spanò et al. (1999) evaluated sperm chromatin damage in 19 normozoospermic subjects using sperm chromatin structure assay (SCSA). This technique exploits the properties of the metachromatic fluorescent dye acridine orange to reveal the susceptibility of double-stranded DNA to denaturation induced by acid stress. Each sample was divided into three aliquots: the first aliquot was evaluated without further processing; the second underwent swim-up (post-rise spermatozoa); and the third was stored according to standard cryopreservation techniques in liquid nitrogen at −196 °C. In addition, an aliquot of the cryopreserved sample underwent a further swim-up procedure after thawing (post-rise spermatozoa after cryopreservation). The DNA damage observed in fresh samples increased in sperm thawed after cryopreservation. This increase may be indicative of the physical stresses the cryopreserved samples experienced, leading to chromatin deterioration in some of the spermatozoa in the native sample. On the other hand, the migrated sperm population (post-rise spermatozoa and post-rise after cryopreservation) exhibited a general improvement in DNA integrity compared with the unselected populations. These authors demonstrated that swim-up techniques select a subpopulation of highly motile cells with better sperm chromatin features, as evaluated by SCSA. Post-rise spermatozoa (from fresh and cryopreserved semen) are therefore characterised by superior and more homogeneous chromatin structure characteristics than those of unselected fresh (and, in the vast majority of cases, also cryopreserved) semen samples. The authors suggested that when performed correctly cryopreservation does not damage spermatozoa per se, but can enhance any defects already present in the sperm population.
This result is consistent with the findings of Oehninger et al. (2000) who reported that the severity of sperm damage after cryopreservation was higher in infertile men, and the extent of the damage was correlated with the degree of oligoasthenoteratozoospermia. Poor-quality semen samples are more susceptible to DNA damage and cell death after cryopreservation than semen samples with normal parameters (Borges et al. 2007).
Donnelly et al. (2001a) studied the effects of cryopreservation on chromatin integrity by Comet assay in 17 fertile and 40 infertile men. Each sample was divided into four aliquots: fresh semen, cryopreserved semen, freshly prepared by density gradient spermatozoa and cryopreserved prepared spermatozoa. In fertile controls, there were no significant differences in DNA damage between the unprocessed semen sample and sperm separated by discontinuous Percoll gradient. The sperm of these subjects was therefore resistant to damage from freezing. However, for the infertile subjects, there was a significant (24%) reduction in chromatin integrity after freezing/thawing of semen samples, reaching 40% in selected sperm. There is in fact less chromatin condensation in poor-quality sperm, making their DNA potentially susceptible to nuclease and polymerase action (Bianchi et al. 1993) or to fragmentation (Gorczyca et al. 1993). Infertile men are well known to have a higher percentage of sperm with fragmented DNA than fertile men (Sun et al. 1997; Lopes et al. 1998). The authors also found a significant reduction in normal forms after cryopreservation in both semen samples and selected sperm from both fertile and infertile subjects, but did not find any correlation between morphology and chromatin integrity. As in previous studies (Hammadeh et al. 1999), this study found that the cryopreservation of sperm from fertile and infertile subjects affected sperm morphology, while sperm DNA from semen samples from fertile men was more resistant to damage. In other words, the genotype and phenotype of human sperm were not equally affected by cryopreservation. In contrast, subsequent studies (Kalthur et al. 2008) showed that morphologically abnormal sperm were more sensitive to DNA damage induced by cryopreservation in liquid nitrogen. These authors evaluated chromatin integrity pre- and post-cryopreservation in 20 normozoospermic and 24 teratozoospermic semen samples using the Comet assay and acridine orange test. Prior to freezing, 17.5% of sperm from normozoospermic and 24.9% from teratozoospermic samples were denatured; post-thawing, this percentage was three times higher in teratozoospermic samples than in normozoospermic samples.
These results can be explained by the fact that abnormal sperm, as demonstrated by several studies, are a major source of free radicals. The cryopreservation-induced ROS level may thus be higher in abnormal than in morphologically normal sperm. The importance of oxygen radicals in the cryopreservation process is confirmed by various studies which show that sperm in seminal plasma seem to be more resistant to the shock of cryopreservation than gradient-selected sperm. This could be due to the presence in the seminal plasma of antioxidant enzymes such as superoxide dismutase and catalase and scavengers such as albumin and taurine, which remove the ROS (Donnelly et al. 2001a).
Confirmation of this hypothesis comes from another study by Donnelly et al. (2001b) carried out on semen samples from 40 infertile patients. For each sample, an aliquot of fresh semen was frozen unprepared, while other aliquots were prepared by Percoll density centrifugation or direct swim-up procedure. The authors compared fresh and frozen semen and prepared sperm (frozen with or without the addition of seminal plasma) from the same ejaculate. Sperm frozen unprepared in seminal fluid appeared more resistant to freezing damage than frozen prepared sperm. Moreover, the DNA of sperm prepared either by Percoll density centrifugation or by swim-up and frozen with additional seminal plasma appeared to be more resistant to freezing damage than the DNA of semen or prepared sperm (without seminal plasma) from the same ejaculate. These data suggest that the abundant presence of antioxidants in seminal plasma protects DNA integrity against freezing. Furthermore, De Paula et al. (2006) demonstrated by TUNEL assay an increase in post-cryopreservation apoptotic fragmentation in both 47 oligozoospermic and 30 normozoospermic subjects. According to these authors, cryopreservation induces fragmentation independently of sperm concentration, as the increase was similar in both groups. Another study by Ngamwuttiwong and Kunathikom (2007) found a decrease in sperm chromatin integrity on acridine orange testing in 20 men from infertile couples after 6 months of sperm cryopreservation.
Overall, various studies in the literature have evaluated the impact of cryopreservation on chromatin structure, albeit with contradictory results; this may be due to small caseloads, different freezing procedures, different methods for assessment of DNA integrity and different semen preparation techniques (Di Santo et al. 2012).
However, studies attempting to explain the mechanisms involved in the aetiology of cryopreservation-induced DNA damage are still limited. Some reported an increase in sperm with activated caspases after cryopreservation, while others found an increase in the percentage of oxidative DNA damage. Studies in animal models showed that cryopreservation induces an increase in apoptotic events, such as modification of mitochondrial membrane potential, activation of caspases and externalisation of phosphatidylserine. Duru et al. (2001) reported an increase in the percentage of sperm with membrane translocation of phosphatidylserine after cryopreservation in both fertile and infertile patients, but this was not associated with impaired sperm integrity. Paasch et al. (2004) achieved the same results, demonstrating in 11 pools of cryopreserved semen samples and 9 pools of fresh semen samples that cryopreservation was significantly associated with the activation of caspases 3, 8 and 9 and impaired mitochondrial membrane potential, but not with any impairment of DNA integrity evaluated by TUNEL. Although caspase activation following cryopreservation and thawing is observed in mature and immature sperm exhibiting cytoplasmic droplets, this mechanism differs in annexin V-positive and annexin V-negative sperm. The authors concluded that ‘cryopreservation and thawing triggers activated caspase activity in spermatozoa by a mechanism that may be linked to the translocation of phosphatidylserine to the surface of the cell’. Unfortunately, the paper does not clearly explain if the cryopreserved and fresh samples derived from the same pools.
These interactions suggest that cryopreservation and thawing trigger the caspase activation through mechanisms possibly linked to membrane translocation of phosphatidylserine. However, more recent studies suggest that DNA fragmentation may be associated with increased cryopreservation-induced oxidative stress rather than caspase activation and apoptosis (Thomson et al. 2009). These authors compared the percentage of sperm with fragmented DNA, the percentage of 8-oxo-7,8-dihydro-2’deoxyguanosine (8OHdG) and the percentage of positive caspases in semen samples from infertile patients before and after cryopreservation. There was an increase in the percentage of DNA fragmentation, oxidative damage and caspase activation after cryopreservation. In fresh semen, there was a correlation between caspase-positive cells and DNA fragmentation and between 8OHdG and DNA fragmentation, due to the simultaneous nature of the two pathways unified by ROS production by abnormal sperm (Thomson et al. 2009). In contrast, there was a negative correlation between caspase-positive cells and DNA fragmentation after thawing, suggesting that cryopreservation could induce DNA fragmentation independently of caspase activation and that this process probably takes place in non-apoptotic cells.
Here too, ROS seem to play an important role in the pathophysiology of DNA damage in human sperm. Zribi et al. (2010) evaluated sperm DNA fragmentation by TUNEL and oxidative damage by flow cytometric analysis of 8OHdG in 15 semen samples pre- and post-cryopreservation. The increased fragmentation induced by cryopreservation was associated with a small increase in the percentage of sperm with oxidative damage.
More recently, Amor et al. (2018) reported that the cryopreservation process not only affects semen parameters but also induces DNA fragmentation and mitochondrial DNA damage in spermatozoa from both fertile and subfertile men. Freeze-thawing reduced sperm viability, total motility and membrane integrity in fertile men, with a significant mean increase in DNA fragmentation (from 14.8% to 27.5% with TUNEL) and in caspase-3 staining (from 5.8% to 7.3%). Similar results were seen in the subfertile group, with a significant increase in both DNA fragmentation (from 19.8% to 29.5%) and caspase-3 staining (from 7.5% to 10.2%). Finally, Lusignan et al. (2018) evaluated the impact of different freezing methods on sperm DNA and chromatin structure assessed by two assays, SCSA and TUNEL, in semen samples from normozoospermic, oligoasthenoteratozoospermic and teratozoospermic men. There was a significant increase in post-thaw TUNEL scores in all three categories for all the freezing methods, while there was no significant change in the DNA fragmentation index (DFI) on SCSA. The authors thus suggested that freeze-thawing had a negative impact on DNA quality regardless of the freezing method and that TUNEL was sensitive enough to detect such damage.
In conclusion, the effect of cryopreservation and thawing follows different pathways, such as amplification of defects already present in the sperm cell, which could activate apoptotic mechanisms, or DNA repair enzyme defects, as well as oxidative stress (Zribi et al. 2010).
Various studies have focused on the effects of cryopreservation on sperm DNA damage; however, there is still no consensus. Some studies found sperm DNA damage after cryopreservation (Thomson et al. 2009; Zribi et al. 2010; Amor et al. 2018), while others did not (Duru et al. 2001; Paasch et al. 2004) (Table 9.1).
Poor-quality semen samples seem to be more susceptible to DNA damage (Spanò et al. 1999; Oehninger et al. 2000; Kalthur et al. 2008) although De Paula et al. (2006) and Amor et al. (2018) reported that cryopreservation induces DNA fragmentation independently of semen quality. However, the use of different cryopreservation methods and of different techniques to assess sperm DNA damage (TUNEL, SCSA or Comet assay) confounds the issue. For this reason, more studies are needed to establish the true importance of such damage, especially in order to improve the results of ART.
Strategies to Prevent Cryopreservation Injuries
Although the cryopreservation of human semen is an important technique routinely employed in the clinical management of male infertility, it can induce changes in sperm function, and the risk of cryodamage is still a major issue. A number of defensive strategies against cryoinjuries have been proposed in the last decade, such as antifreeze proteins (AFPs) (Hezavehei et al. 2018), seminal plasma protein (Pini et al. 2018) and gangliosides (Gavella and Lipovac 2013), although most literature reports have focused on the role of antioxidants.
The cryopreservation process may result in adverse changes in membrane lipid composition, acrosome status, sperm motility and viability, as well as an increase in sperm DNA damage (Donnelly et al. 2001b; Medeiros et al. 2002; O’Connell et al. 2002; Hezavehei et al. 2018). Most of these deleterious effects are due to the reactive oxygen species (ROS) generated during cryopreservation (Agarwal and Majzoub 2017; Bui et al. 2018). Under normal conditions, spermatozoa and seminal plasma possess a number of antioxidant systems that scavenge ROS and prevent internal cellular damage, thus neutralising the detrimental effects of ROS. The imbalance between the presence of ROS and sperm antioxidant activity is considered an important cause of sperm cryodamage (Amidi et al. 2016).
Components of the human reproductive system contain antioxidants that are either endogenously formed or acquired from dietary sources. In males, antioxidants are found in the testis, epididymis, secretions of the male accessory organs and seminal plasma (Agarwal et al. 2014a). Based on their chemical structure, antioxidants may be enzymatic and non-enzymatic. Enzymatic (natural) antioxidants include catalase, superoxide dismutase (SOD) and glutathione reductase (GSH), while non-enzymatic antioxidants consist of radical scavengers such as vitamin E (α-tocopherol), vitamin C (ascorbic acid), cysteine, carnitine, melatonin, polyphenols and natural extracts (Tan et al. 2000; Stojanović et al. 2001; Meamar et al. 2012; Agarwal et al. 2014b).
Extensive research has been conducted to study the effect of antioxidant therapy in improving male fertility and pregnancy rates (Agarwal et al. 2004; Ahmadi et al. 2016; Majzoub and Agarwal 2018). Different types of cryoprotective media, mostly supplemented with antioxidants, have been designed in recent years to attempt to overcome the cell damage caused by cryopreservation. Antioxidants have generally proved beneficial in reversing the sperm dysfunction caused by oxidative stress, suggesting that antioxidant supplementation has a protective effect on ROS-induced sperm cryoinjury (Agarwal et al. 2014a; Amidi et al. 2016; Hezavehei et al. 2018).
Enzymatic Antioxidants
Catalase
Catalase is a ubiquitous antioxidant enzyme mostly found in cellular peroxisomes and involved in the detoxification of hydrogen peroxide (H2O2), by decomposing it to oxygen and water. Catalase originating mainly from the prostate gland is found in seminal fluid and motile spermatozoa (Jeulin et al. 1989). In 2008, Chi et al. investigated how the addition of catalase to a sperm preparation medium affected the functional parameters of the spermatozoa, finding reduced ROS and DNA fragmentation levels and an increased acrosome reaction rate in spermatozoa from normozoospermic men. Other studies have also found that catalase supplementation of cryomedia improves freeze-thaw outcomes. Li et al. (2010) found that both catalase (200 and 400 IU/mL) and ascorbate (300 mM) supplementation in cryomedia reduced ROS levels, thereby protecting against cryodamage. More recently, Moubasher et al. (2013) also demonstrated that catalase supplementation was associated with a higher percentage of progressive motility and improved sperm viability and DNA integrity.
Superoxide Dismutase
Superoxide dismutases (SODs) are metalloenzymes that convert superoxide to hydrogen peroxide. Murawski et al. (2007) found a significantly lower semen SOD activity in oligoasthenozoospermic cases when compared to normozoospermic men. SOD activity in seminal plasma is also positively associated with sperm concentration and overall motility (Yan et al. 2014). Co-supplementation of cryopreserved spermatozoa with catalase and SOD results in higher post-thaw motility and viability. It may also help prevent sperm membrane lipid peroxidation by ROS, thus allowing good sperm parameter recovery after freeze-thaw procedures (Rossi et al. 2001). Recent research has suggested that cell-permeable enzyme-mimetic agents may help reduce intracellular ROS levels. For example, manganese (III) meso-tetrakis (MnTE) is a mimetic agent which can convert superoxide to H2O2. Shafiei et al. (2015) suggested that the addition of MnTE or catalase to commercial optimised media improves post-thaw goat semen function.
Glutathione
The glutathione enzymatic family comprises reduced glutathione (GSH) , glutathione peroxidase (GPx , isoforms Gpx 1 to GPx 6), glutathione S-transferase (GST) and glutathione reductase (GR). Glutathione is a sulphur-containing tripeptide present in both a reduced (GSH) and an oxidative (GSSG) form. The sulfhydryl groups of GSH protect cells against oxidants, electrophiles and free radicals (Agarwal et al. 2006). The addition of GSH to both freezing and thawing extenders improved post-thaw boar sperm quality, stabilised the nucleoprotein structure and improved both in vivo and in vitro fertilising ability (Estrada et al. 2014). The greatest improvement was seen when freezing and thawing media were supplemented with both GSH and l-ascorbic acid (Giaretta et al. 2015). The addition of GSH also improved the post-thaw quality of ram semen. Zeitoun and Al-Damegh (2014) found that adding 1–2 mM glutathione to ram semen extender increased GPX and SOD activity, reduced free radicals and improved the post-thaw sperm survival rate.
Gadea et al. (2011) reported a reduction of up to 64% in GSH content after freeze-thawing, indicating that the antioxidant defence system is challenged by sperm cryopreservation. These authors also showed that the addition of GSH to freezing and thawing media reduced ROS levels and improved the motility of human spermatozoa. More recently, Ghorbani et al. (2016) also investigated GSH supplementation in human sperm cryopreservation, demonstrating that after thawing, cryovials supplemented with 5 mM of GSH showed greater sperm viability than the control samples. These cryovials also showed reduced sperm lipid peroxidation and DNA fragmentation and a lower H2O2 and O2− content than the controls.
Non-enzymatic Antioxidants
Vitamin E (a-Tocopherol/Trolox)
Vitamin E is a potent chain-breaking lipophilic antioxidant, residing on the cell membrane, which can break the covalent links formed by ROS between fatty acid side chains in membrane lipids. It quenches free hydroxyl radicals and superoxide anions, thereby reducing ROS-induced lipid peroxidation in the plasma membrane. The most active form, alpha-tocopherol, quenches hydrogen peroxide, superoxide anions and hydroxyl anions and breaks peroxidation chain reactions (Agarwal et al. 2004; Majzoub and Agarwal 2018).
Geva et al. (1996) were the first to demonstrate an improved fertilisation rate after 1 month of treatment with vitamin E (200 mg/day) for fertile normozoospermic men who had low fertilisation rates in previous IVF cycles. Greco et al. (2005a) showed that daily treatment with 1 g of vitamin C and 1 g of vitamin E improved the success rate of intracytoplasmic sperm injection (ICSI) and reduced sperm DNA fragmentation.
Taylor et al. (2009) found that supplementation of semen cryopreservation medium with 200 μmol of vitamin E significantly improved post-thaw motility but not viability or the degree of DNA fragmentation. The authors associated the positive effect of vitamin E supplementation with age: the effects were better in men over 40 years of age. Finally, Kalthur et al. (2011) demonstrated that supplementation of cryoprotective medium with vitamin E (5 mM) not only improved post-thaw sperm motility but also helped maintain sperm DNA integrity in normozoospermic and asthenozoospermic samples.
Trolox is a water-soluble vitamin E analogue with powerful antioxidant properties. Trolox supplementation (40 μM) significantly improved post-thaw human semen quality, especially progressive motility (Minaei et al. 2012). Nekoonam et al. (2016) supported the use of Trolox as a freezing extender supplement to improve the quality of cryopreserved human sperm. The authors investigated DNA integrity, mitochondrial function as expressed by its membrane potential (MMP) and phosphatidylserine externalisation, an early marker of apoptosis, in sperm cells following freeze-thawing in normozoospermic men and oligozoospermic patients. Sperm frozen in extender with Trolox had a higher MMP and lower DNA fragmentation and phosphatidylserine externalisation in both groups , though the most effective dose differed between normozoospermic and oligozoospermic semen samples (80 and 20 μM, respectively).
Vitamin C
Vitamin C (ascorbic acid) is a water-soluble vitamin freely available in fruits and vegetables, whose antioxidant properties offer many beneficial effects (Alahmar 2018). Ascorbate reduces H2O2-induced DNA damage, recycles inactive vitamin E and reduces lipid peroxidation (Donnelly et al. 1999; Sierens et al. 2002). Vitamin C is the principal antioxidant in the seminal plasma of fertile men, contributing up to 65% of its total chain-breaking antioxidant capacity. The concentration of ascorbate in seminal plasma is 10 times greater than in blood plasma (Agarwal et al. 2004). Several studies have reported a significant improvement in sperm quality after vitamin C supplementation (Akmal et al. 2006; Kobori et al. 2014; Cyrus et al. 2015; Eslamian et al. 2017). As reported above, Greco et al. (2005b) demonstrated in ejaculated spermatozoa from 64 infertile men that DNA fragmentation was reduced by oral treatment with 1 g vitamin C and 1 g vitamin E daily for 2 months. Song et al. (2006) found that ascorbic acid levels in semen were directly correlated with the percentage of morphologically normal spermatozoa and negatively correlated with the DNA fragmentation index. Similarly, Fanaei et al. (2014) reported that vitamin C supplementation of culture media reduced lipid peroxidation and DNA damage while improving sperm motility and viability. Branco et al. (2010) demonstrated that 10 mM ascorbic acid added to semen samples from infertile men prior to adding cryomedia prevents DNA damage. Finally, Jenkins et al. (2011) found that supplementation of cryomedium with ascorbic acid-2-glucoside (AA2G), a stabilised form of ascorbate , protected the post-thaw motility of human sperm.
L-Carnitine
L-carnitine is a highly polar water-soluble quaternary amine. It is biologically important for the mitochondrial β-oxidation of long-chain fatty acids and the generation of ATP. In eukaryotic metabolism, its main function is to promote the translocation of fatty acids across the mitochondrial inner membrane as β-hydroxyl O-acyl esters of L-carnitine. Its concentration in epididymal plasma and spermatozoa is 2000-fold higher than in circulating blood. In the epididymal lumen, the initiation of sperm motility occurs in parallel to increasing L-carnitine levels (Enomoto et al. 2002). Carnitines also have antioxidant properties, thus protecting against ROS (Gülçin 2006).
In seminal plasma, L-carnitine plays an essential role in maintaining male fertility, and its beneficial effects on sperm parameters are well known (Agarwal and Said 2004; Ahmed et al. 2011). Combination therapy with L-carnitine and acetyl-L-carnitine improves sperm quality in men with asthenozoospermia, as demonstrated by Lenzi et al. (2004) in a double-blind placebo-controlled trial investigating the effects of L-carnitine supplements in 56 men with idiopathic oligoasthenoteratozoospermia, in which the intervention group received 2 g/day of L-carnitine and 1 g/day of L-acetyl carnitine for 6 months. Similarly, in a randomised double-blind trial of 59 men with idiopathic oligoasthenoteratozoospermia, Balercia et al. (2005) demonstrated that the administration of L-carnitine and acetyl-L-carnitine improved the sperm kinetic features and the total oxyradical scavenging capacity of the seminal fluid in patients with idiopathic asthenozoospermia.
Banihani et al. (2014) recently found that the use of cryopreservation medium supplemented with l-carnitine for cryopreservation of semen samples from infertile patients improved post-thaw sperm motility and viability but had no protective effect on sperm DNA oxidative damage in comparison with semen samples frozen and thawed without l-carnitine.
L-Cysteine
L-cysteine is a low molecular weight non-essential amino acid containing thiol. It penetrates the cell membrane to participate in intracellular GSH biosynthesis (Amidi et al. 2016). Uysal and Bucak (2007) reported that L-cysteine enhanced intracellular GSH biosynthesis and protected proteins, DNA and membrane lipids through the direct radical scavenging ability of GSH. L-cysteine protects the spermatozoa of various mammalian species against cryodamage, including boars (Chanapiwat et al. 2009), bulls (Sariözkan et al. 2009), buffalos (Topraggaleh et al. 2014), goats (Memon et al. 2012) and rams (Coyan et al. 2011). Zhu et al. (2017) recently found that the addition of L-cysteine to freezing extender for the cryopreservation of rabbit semen enhanced antioxidant GSH content and glutathione peroxidase activity, lowering ROS levels and lipid peroxidation.
Melatonin
Melatonin , a derivative of tryptophan, is mainly secreted by the pineal gland and contributes to the regulation of different physiological events, such as the seasonal and circadian rhythms of mammals (Reiter et al. 2009). It is a potent endogenous free radical scavenger, independently of its many receptor-mediated effects (Tan et al. 2000). Human seminal fluid contains melatonin, and spermatozoa reportedly possess a melatonin receptor (Ortiz et al. 2011). Several studies have reported the beneficial effects of melatonin on spermatozoa. In adult rats with experimentally induced unilateral varicocele, it prevented testicular damage by stimulating antioxidant enzyme activity and reducing NO levels (Semercioz et al. 2003), while Sönmez et al. (2007) observed that it protected rat spermatozoa from the adverse effects of the pro-oxidative agent homocysteine.
Gavella and Lipovac (2000) investigated the ability of melatonin to suppress experimentally induced lipid peroxidation in semen samples from 41 infertile men. They found that it relieved the sperm mitochondrial oxidative stress caused by ROS, although it was 40-fold less efficient than Trolox. Melatonin has also been shown to protect spermatozoa from oxidative stress-induced apoptosis. Espino et al. (2010) evaluated its effect on H2O2-treated (10 μM) ejaculated human spermatozoa from 20 healthy donors, concluding that its free radical scavenging action subverted the pro-apoptotic action induced by H2O2. Several studies report that melatonin protects animal spermatozoa from the adverse effects of ROS during cryopreservation (Succu et al. 2011; Ashrafi et al. 2013). In humans, Karimfar et al. (2015) demonstrated that semen extender supplemented with melatonin (0.01 mM) significantly increased post-thaw motility and viability and reduced intracellular ROS and malondialdehyde levels in cryopreserved sperm.
Quercetin and Resveratrol
Resveratrol is a non-flavonoid and quercetin a flavonoid polyphenol. They are described as powerful antioxidants with a similar effect, resulting from their ability to inhibit ROS formation by enzymatic and non-enzymatic systems, especially NADPH-oxidase and NADH-dependent oxidoreductase (Stojanović et al. 2001).
Resveratrol is a natural phytoalexin with antioxidant properties which has different biological activities, including anti-inflammatory, antiviral and antitumorigenic activities. It is found in many plant species, especially grapes, and in red wine. Garcez et al. (2010) studied the effects of resveratrol supplementation in cryopreservation medium for human semen, demonstrating that it inhibited post-thaw oxidative damage, although it did not prevent post-thaw loss of motility (Garcez et al. 2010). Shabani Nashtaei et al. (2018) recently demonstrated in 22 normozoospermic semen samples that the addition of resveratrol before cryopreservation led to a significant reduction in the incidence of post-thaw sperm DNA fragmentation. The authors suggested that its protective effects against cryopreservation-induced oxidative stress may be mediated through activation of AMP-activated protein kinase (AMPK), an evolutionary conserved serine/threonine kinase that controls cell metabolism and acts as a key sensor of cell energy status through the stimulation of catabolic processes and inhibition of anabolic processes (Hardie et al. 2006).
Quercetin is a dietary flavonoid found in various vegetables, fruits, seeds and nuts, as well as in tea and red wine. It scavenges reactive species and hydroxyl radicals, thereby providing beneficial anticarcinogenic, anti-inflammatory and antimicrobial properties (Boots et al. 2008).
Quercetin helps protect against H2O2-mediated sperm damage in rats by reducing lipid peroxidation and increasing the sperm’s antioxidant defences (Ben Abdallah et al. 2011). Supplementation of semen extender with quercetin also had beneficial antioxidant properties on the post-thaw characteristics of semen from bulls (Avdatek et al. 2018), horses (Seifi-Jamadi et al. 2016), boars (Kim et al. 2014) and rams (Silva et al. 2012). In humans, Zribi et al. (2012) showed that the addition of quercetin (50 μM) to the cryoprotective medium enhanced sperm motility and viability and reduced post-thaw DNA damage.
Although flavonoid compounds exhibit strong antioxidant properties in vitro, their effects are minimised in vivo due to their low water solubility, weak absorption and lower bioavailability. Moretti et al. (2016) tested the ability of quercetin-loaded liposomes compared to quercetin alone in preventing oxidative stress induced in vitro in swim-up-selected human spermatozoa. Quercetin-loaded liposomes did not affect sperm viability and motility even at high concentrations, but were less efficient than quercetin alone at protecting spermatozoa from lipid peroxidation. Although quercetin alone appeared more effective at reducing oxidative stress, the authors suggested further investigations were needed on the use of liposomes to carry compounds into spermatozoa.
Natural Extracts (Opuntia ficus-indica and Genistein)
Opuntia ficus-indica (OFI) is a pear cactus whose extract contains a cocktail of antioxidants including ascorbic acid, polyphenols, carotenoids, taurine and several types of flavonoids, in particular quercetin. Meamar et al. (2012) evaluated whether the addition of OFI extract to cryopreservation medium would protect sperm from the deleterious effects of cryopreservation in comparison with the antioxidant resveratrol. They found that both substances had a slight but statistically significant protective effect against sperm DNA fragmentation.
Genistein is an isoflavone found in soya and other legumes. The structure of isoflavones, a class of phytoestrogens, resembles the steroid hormone 17β-oestradiol, and isoflavones can bind to the oestrogen receptor. However, their physiological effects are not confined to oestrogen modulation, and isoflavones have been reported to inhibit angiogenesis and cell proliferation and induce cancer cell differentiation. In addition, they may function as antioxidant species (Zielonka et al. 2003). Sierens et al. (2002) demonstrated that pretreatment with genistein at doses of 0.01–100 μmol/l significantly protected sperm DNA against oxidative damage. The addition of 50 μM or 100 μM of genistein to the cryoprotectant also had a significant protective effect on cryopreservation-induced DNA fragmentation in post-thaw human spermatozoa (Thomson et al. 2009). Martinez-Soto et al. (2010) confirmed that genistein has antioxidant properties in post-thaw spermatozoa, finding reduced cryopreservation-induced ROS production and DNA damage and improved sperm motility with a concentration of 1–10 μM.
In summary, cryopreservation may lead to changes in sperm structure and function secondary to the state of oxidative stress induced by the freeze-thaw process. Several studies focused on supplementing cryoprotectant medium with various antioxidant molecules, all aimed at minimising oxidative damage and thus improving sperm recovery. Despite the promising results, identification of the ideal antioxidant treatment method is still hampered by the heterogeneity of the studies, which describe the use of different antioxidant regimens at different concentrations or in different combinations. For this reason, additional studies are needed to further investigate the use of antioxidants, individually and in combination, in the cryopreservation of human sperm, to determine the most beneficial conditions for optimal sperm recovery and preservation of fertility.
References
Agarwal A, Majzoub A (2017) Role of antioxidants in assisted reproductive techniques. World J Mens Health 35:77–93
Agarwal A, Said TM (2004) Carnitines and male infertility. Reprod Biomed Online 8:376–384
Agarwal A, Nallella KP, Allamaneni SS, Said TM (2004) Role of antioxidants in treatment of male infertility: an overview of the literature. Reprod Biomed Online 8:616–627
Agarwal A, Gupta S, Sikka S (2006) The role of free radicals and antioxidants in reproduction. Curr Opin Obstet Gynecol 18:325–332
Agarwal A, Durairajanayagam D, du Plessis SS (2014a) Utility of antioxidants during assisted reproductive techniques: an evidence based review. Reprod Biol Endocrinol 24:112
Agarwal A, Virk G, Ong C, du Plessis SS (2014b) Effect of oxidative stress on male reproduction. World J Mens Health 32(1):17
Ahmadi S, Bashiri R, Ghadiri-Anari A, Nadjarzadeh A (2016) Antioxidant supplements and semen parameters: an evidence based review. Int J Reprod Biomed (Yazd) 14:729–736
Ahmed SD, Karira KA, Jagdesh, Ahsan S (2011) Role of L-carnitine in male infertility. J Pak Med Assoc 61:732–736
Akmal M, Qadri JQ, Al-Waili NS, Thangal S, Haq A, Saloom KY (2006) Improvement in human semen quality after oral supplementation of vitamin C. J Med Food 9:440–442
Alahmar AT (2018) The effects of oral antioxidants on the semen of men with idiopathic oligoasthenoteratozoospermia. Clin Exp Reprod Med 45:57–66
Amidi F, Pazhohan A, Shabani Nashtaei M, Khodarahmian M, Nekoonam S (2016) The role of antioxidants in sperm freezing: a review. Cell Tissue Bank 17:745–756
Amor H, Zeyad A, Alkhaled Y, Laqqan M, Saad A, Ben Ali H, Hammadeh ME (2018) Relationship between nuclear DNA fragmentation, mitochondrial DNA damage and standard sperm parameters in spermatozoa of fertile and sub-fertile men before and after freeze-thawing procedure. Andrologia 50:e12998
Arav A, Zeron Y, Leslie SB, Behboodi E, Anderson GB, Crowe JH (1996) Phase transition temperature and chilling sensitivity of bovine oocytes. Cryobiology 33:589–599
Ashrafi I, Kohram H, Ardabili FF (2013) Antioxidative effects of melatonin on kinetics, microscopic and oxidative parameters of cryopreserved bull spermatozoa. Anim Reprod Sci 139:25–30
Avdatek F, Yeni D, İnanç ME, Çil B, Tuncer BP, Türkmen R, Taşdemir U (2018) Supplementation of quercetin for advanced DNA integrity in bull semen cryopreservation. Andrologia, Feb 7
Bailey JL, Bilodeau JF, Cormier N (2000) Semen cryopreservation in domestic animals: a damaging and capacitating phenomenon. J Androl 21:1–7
Balercia G, Regoli F, Armeni T, Koverech A, Mantero F, Boscaro M (2005) Placebo-controlled double-blind randomized trial on the use of l-carnitine, l-acetylcarnitine, or combined l-carnitine and l-acetylcarnitine in men with idiopathic asthenozoospermia. Fertil Steril 84:662–671
Banihani S, Agarwal A, Sharma R, Bayachou M (2014) Cryoprotective effect of l-carnitine on motility, vitality and DNA oxidation of human spermatozoa. Andrologia 46:637–641
Behrman SJ, Sawada Y (1966) Heterologous and homologous insemination with human semen frozen and stored in a liquid-nitrogen refrigerator. Fertil Steril 17:457–466
Ben Abdallah F, Zribi N, Ammar-Keskes L (2011) Antioxidative potential of Quercetin against hydrogen peroxide induced oxidative stress in spermatozoa in vitro. Andrologia 43:261–265
Benoff S (1997) Carbohydrates and fertilization: an overview. Mol Hum Reprod 3:599–637
Bianchi PG, Manicardi GC, Bizzaro D, Bianchi U, Sakkas D (1993) Effect of deoxyribonucleic acid protamination on fluorochrome staining and in situ nick-translation of murine and human mature spermatozoa. Biol Reprod 49:1083–1088
Boots AW, Haenen GR, Bast A (2008) Health effects of quercetin: from antioxidant to nutraceutical. Eur J Pharmacol 585:325–337
Borges E Jr, Rossi LM, Locambo de Freitas CV, Guilherme P, Bonetti TC, Iaconelli A, Pasqualotto FF (2007) Fertilization and pregnancy outcome after intracytoplasmic injection with fresh or cryopreserved ejaculated spermatozoa. Fertil Steril 87:316–320
Branco CS, Garcez ME, Pasqualotto FF, Erdtman B, Salvador M (2010) Resveratrol and ascorbic acid prevent DNA damage induced by cryopreservation in human semen. Cryobiology 60:235–237
Bui AD, Sharma R, Henkel R, Agarwal A (2018) Reactive oxygen species impact on sperm DNA and its role in male infertility. Andrologia 50:e13012
Bunge RG, Sherman JK (1953) Fertilizing capacity of frozen human spermatozoa. Nature 172:767–768
Bunge RG, Keettel WC, Sherman JK (1954) Clinical use of frozen semen: report of four cases. Fertil Steril 5:520–529
Chanapiwat P, Kaeoket K, Tummaruk P (2009) Effects of DHA-enriched hen egg yolk and L-cysteine supplementation on quality of cryopreserved boar semen. Asian J Androl 11:600–608
Chi HJ, Kim JH, Ryu CS, Lee JY, Park JS, Chung DY, Choi SY, Kim MH, Chun EK, Roh SI (2008) Protective effect of antioxidant supplementation in sperm-preparation medium against oxidative stress in human spermatozoa. Hum Reprod 23:1023–1028
Clarke GN, Liu DY, Baker HW (2003) Improved sperm cryopreservation using cold cryoprotectant. Reprod Fertil Dev 15:377–381
Coyan K, Başpınar N, Bucak MN, Akalın PP (2011) Effects of cysteine and ergothioneine on post-thawed Merino ram sperm and biochemical parameters. Cryobiology 63:1–6
Cross NL, Overstreet JW (1987) Glycoconjugates of the human sperm surface: distribution and alterations that accompany capacitation in vitro. Gamete Res 16:23–35
Cyrus A, Kabir A, Goodarzi D, Moghimi M (2015) The effect of adjuvant vitamin C after varicocele surgery on sperm quality and quantity in infertile men: a double blind placebo controlled clinical trial. Int Braz J Urol 41:230–238
De Paula TS, Bertolla RP, Spaine DM, Cunha MA, Schor N, Cedenho AP (2006) Effect of cryopreservation on sperm apoptotic deoxyribonucleic acid fragmentation in patients with oligozoospermia. Fertil Steril 86:597–600
Di Santo M, Tarozzi N, Nadalini M, Borini A (2012) Human sperm cryopreservation: update on techniques, effect on DNA integrity, and implications for ART. Adv Urol 2012:854837
Donnelly ET, McClure N, Lewis SE (1999) The effect of ascorbate and alpha-tocopherol supplementation in vitro on DNA integrity and hydrogen peroxide-induced DNA damage in human spermatozoa. Mutagenesis 14:505–512
Donnelly ET, Steele EK, McClure N, Lewis SE (2001a) Assessment of DNA integrity and morphology of ejaculated spermatozoa from fertile and infertile men before and after cryopreservation. Hum Reprod 16:1191–1199
Donnelly ET, McClure N, Lewis SE (2001b) Cryopreservation of human semen and prepared sperm: effects on motility parameters and DNA integrity. Fertil Steril 76:892–900
Duru NK, Morshedi MS, Schuffner A, Oehninger S (2001) Cryopreservation-Thawing of fractionated human spermatozoa is associated with membrane phosphatidylserine externalization and not DNA fragmentation. J Androl 22:646–651
Enomoto A, Wempe MF, Tsuchida H, Shin HJ, Cha SH, Anzai N, Goto A, Sakamoto A, Niwa T, Kanai Y, Anders MW, Endou H (2002) Molecular identification of a novel carnitine transporter specific to human testis. Insights into the mechanism of carnitine recognition. J Biol Chem 277:36262–36271
Eslamian G, Amirjannati N, Rashidkhani B, Sadeghi MR, Hekmatdoost A (2017) Nutrient patterns and asthenozoospermia: a case-control study. Andrologia 49:e12624
Espino J, Bejarano I, Ortiz A, Lozano GM, García JF, Pariente JA, Rodríguez AB (2010) Melatonin as a potential tool against oxidative damage and apoptosis in ejaculated human spermatozoa. Fertil Steril 94:1915–1917
Estrada E, Rodríguez-Gil JE, Rocha LG, Balasch S, Bonet S, Yeste M (2014) Supplementing cryopreservation media with reduced glutathione increases fertility and prolificacy of sows inseminated with frozen-thawed boar semen. Andrology 2:88–99
Fabbri R, Ciotti P, Di Tommaso B, Magrini O, Notarangelo L, Porcu E, Contro E, Venturosi S (2004) Tecniche di crioconservazione riproduttiva. Riv Ital Ostet Ginecol 3:33–41
Fanaei H, Khayat S, Halvaei I, Ramezani V, Azizi Y, Kasaeian A, Mardaneh J, Parvizi MR, Akrami M (2014) Effects of ascorbic acid on sperm motility, viability, acrosome reaction and DNA integrity in teratozoospermic samples. Iranian J Reprod Med 12:103–110
Gadea J, Molla M, Selles E, Marco MA, Garcia-Vazquez FA, Gardon JC (2011) Reduced glutathione content in human sperm is decreased after cryopreservation: effect of the addition of reduced glutathione to the freezing and thawing extenders. Cryobiology 62:40–46
Garcez ME, dos Santos Branco C, Lara LV, Pasqualotto FF, Salvador M (2010) Effects of resveratrol supplementation on cryopreservation medium of human semen. Fertil Steril 94:2118–2121
Gavella M, Lipovac V (2000) Antioxidative effect of melatonin on human spermatozoa. Arch Androl 44:23–27
Gavella M, Lipovac V (2013) Protective effects of exogenous gangliosides on ROS-induced changes in human spermatozoa. Asian J Androl 15:375–381
Geva E, Bartoov B, Zabludovsky N, Lessing J, Lerner-Geva L, Amit A (1996) The effect of antioxidant treatment on human spermatozoa and fertilization rate in an in vitro fertilization program. Fertil Steril 66:430–434
Ghorbani M, Vatannejad A, Khodadadi I, Amiri I, Tavilani H (2016) Protective effects of glutathione supplementation against oxidative stress during cryopreservation of human spermatozoa. Cryo Letters 37:34–40
Giaretta E, Estrada E, Bucci D, Spinaci M, Rodríguez-Gil JE, Yeste M (2015) Combining reduced glutathione and ascorbic acid has supplementary beneficial effects on boar sperm cryotolerance. Theriogenology 83:399–407
Giraud MN, Motta C, Boucher D, Grizard G (2000) Membrane fluidity predicts the outcome of cryopreservation of human spermatozoa. Hum Reprod 15:2160–2164
Gorczyca W, Traganos F, Jesionowska H, Darzynkiewicz Z (1993) Presence of DNA strand breaks and increased sensitivity of DNA in situ to denaturation in abnormal human sperm cells: analogy to apoptosis of somatic cells. Exp Cell Res 207:202–205
Gosálvez J, Cortés-Gutierez E, López-Fernández C, Fernández JL, Caballero P, Nuñez R (2009) Sperm deoxyribonucleic acid fragmentation dynamics in fertile donors. Fertil Steril 92:170–173
Greco E, Romano S, Iacobelli M, Ferrero S, Baroni E, Minasi MG, Ubaldi F, Rienzi L, Tesarik J (2005a) ICSI in cases of sperm DNA damage: beneficial effect of oral antioxidant treatment. Hum Reprod 20:2590–2594
Greco E, Iacobelli M, Rienzi L, Ubaldi F, Ferrero S, Tesarik J (2005b) Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J Androl 26:349–353
Gülçin I (2006) Antioxidant and antiradical activities of L-carnitine. Life Sci 78:803–811
Halliwell B, Gutterridge J (1984) Lipid peroxidation, oxygen radicals, cell damage and antioxidant therapy. Lancet 231:1396–1397
Hammadeh ME, Askari AS, Georg T, Rosenbaum P, Schmidt W (1999) Effect of freeze-thawing procedure on chromatin stability, morphological alteration and membrane integrity of human spermatozoa in fertile and subfertile men. Int J Androl 22:155–162
Hardie DG, Hawley SA, Scott JW (2006) AMP-activated protein kinase – development of the energy sensor concept. J Physiol 574:7–15
Hezavehei M, Sharafi M, Kouchesfahani HM, Henkel R, Agarwal A, Esmaeili V, Shahverdi A (2018) Sperm cryopreservation: a review on current molecular cryobiology and advanced approaches. Reprod Biomed Online 37:327–339
Jenkins TG, Aston KI, Carrell DT (2011) Supplementation of cryomedium with ascorbic acid-2-glucoside (AA2G) improves human sperm post-thaw motility. Fertil Steril 95:2001–2004
Jeulin C, Soufir JC, Weber P, Laval-Martin D, Calvayrac R (1989) Catalase activity in human spermatozoa and seminal plasma. Gamete Res 24:185–196
Thachil JV, Jewett MAS (1981) Preservation techniques for human semen. Fertil Steril 35:546–548
Kalthur G, Adiga SK, Upadhya D, Rao S, Kumar P (2008) Effect of cryopreservation on sperm DNA integrity in patients with teratosperm. Fertil Steril 89:1723–1727
Kalthur G, Raj S, Thiyagarajan A, Kumar S, Kumar P, Adiga SK (2011) Vitamin E supplementation in semen-freezing medium improves the motility and protects sperm from freeze-thaw–induced DNA damage. Fertil Steril 95:1149–1151
Karimfar MH, Niazvand F, Haghani K, Ghafourian S, Shirazi R, Bakhtiyari S (2015) The protective effects of melatonin against cryopreservation induced oxidative stress in human sperm. Int J Immunopathol Pharmacol 28:69–76
Karow AM Jr (1974) Cryopreservation: pharmacological considerations. In: Karow AM, Abouna GJ, Humphries AL (eds) Organ preservation for transplantation. Little Brown, Boston, pp 86–107
Kim TH, Yuh IS, Park IC, Cheong HT, Kim JT, Park JK, Yang BK (2014) Effects of quercetin and genistein on boar sperm characteristics and porcine IVF embryo developments. J Embrio Transfer 29:141–148
Kobori Y, Ota S, Sato R, Yagi H, Soh S, Arai G, Okada H (2014) Antioxidant cosupplementation therapy with vitamin C, vitamin E, and coenzyme Q10 in patients with oligoasthenozoospermia. Arch Ital Urol Androl 86:1–4
Lassalle B, Testart J (1994) Human zona pellucida recognition associated with removal of sialic acid from human sperm surface. J Reprod Fertil 101:703–711
Lasso JL, Noiles EE, Alvarez JG, Storey BT (1994) Mechanism of superoxide dismutase loss from human sperm cells during cryopreservation. J Androl 15:255–265
Lenzi A, Sgrò P, Salacone P (2004) A placebo-controlled double-blind randomized trial of the use of combined L-carnitine and L-acetylcarnitine treatment in men with asthenozoospermia. Fertil Steril 8:1578–1584
Li Z, Lin Q, Liu R, Xiao W, Liu W (2010) Protective effects of ascorbate and catalase on human spermatozoa during cryopreservation. J Androl 31:437–444
Lopes S, Sun JG, Jurisicova A, Meriano J, Casper RF (1998) Sperm deoxyribonucleic acid fragmentation is increased in poor-quality semen samples and correlates with failed fertilization in intracytoplasmic sperm injection. Fertil Steril 69:528–532
Lusignan MF, Li X, Herrero B, Delbes G, Chan PTK (2018) Effects of different cryopreservation methods on DNA integrity and sperm chromatin quality in men. Andrology 6:829
Mahadevan M, Trounson AO (1984) Effect of cooling, freezing and thawing rates and storage conditions on preservation of human spermatozoa. Andrologia 16:52–60
Majzoub A, Agarwal A (2018) Systematic review of antioxidant types and doses in male infertility: benefits on semen parameters, advanced sperm function, assisted reproduction and live-birth rate. Arab J Urol 16:113–124
Martinez-Soto JC, De Dioshourcade J, Gutiérrez-Adán A, Landeras JL, Gadea J (2010) Effect of genistein supplementation of thawing medium on characteristics of frozen human spermatozoa. Asian J Androl 12:431–441
Mazur P (1984) Freezing of living cells: mechanisms and implications. Am J Physiol 247(3 Pt 1):C125–C142
Mazzilli F, Rossi T, Sabatini L, Pulcinelli FM, Rapone S, Dondero F, Gazzaniga PP (1995) Human sperm cryopreservation and reactive oxygen species (ROS) production. Acta Eur Fertil 26:145–148
Meamar M, Zribi N, Cambi M, Tamburrino L, Marchiani S, Filimberti E, Fino MG, Biggeri A, Menezo Y, Forti G, Baldi E, Muratori M (2012) Sperm DNA fragmentation induced by cryopreservation: new insights and effect of a natural extract from Opuntia ficus-indica. Fertil Steril 98:326–333
Medeiros CM, Forell F, Oliveira AT, Rodrigues JL (2002) Current status of sperm cryopreservation: why isn’t it better? Theriogenology 57:327–344
Memon AA, Wahid H, Rosnina Y, Goh YM, Ebrahimi M, Nadia FM (2012) Effect of antioxidants on post thaw microscopic, oxidative stress parameter and fertility of Boer goat spermatozoa in Tris egg yolk glycerol extender. Anim Reprod Sci 136:55–60
Minaei MB, Barbarestani M, Nekoonam S, Abdolvahabi MA, Takzare N, Asadi MH, Hedayatpour A, Amidi F (2012) Effect of Trolox addition to cryopreservation media on human sperm motility. Iran J Reprod Med 10:99–104
Moretti E, Mazzi L, Bonechi C, Salvatici MC, Iacoponi F, Rossi C, Collodel G (2016) Effect of Quercetin-loaded liposomes on induced oxidative stress in human spermatozoa. Reprod Toxicol 60:140–147
Moubasher AE, El Din AM, Ali ME, El-sherif WT, Gaber HD (2013) Catalase improves motility, vitality and DNA integrity of cryopreserved human spermatozoa. Andrologia 45:135–139
Murawski M, Saczko J, Marcinkowska A, Chwiłkowska A, Gryboś M, Banaś T (2007) Evaluation of superoxide dismutase activity and its impact on semen quality parameters of infertile men. Folia Histochem Cytobiol 45(Suppl 1):S123–S126
Nekoonam S, Nashtaei MS, Zangi BM, Amidi F (2016) Effect of Trolox on sperm quality in normozospermia and oligozospermia during cryopreservation. Cryobiology 72:106–111
Ngamwuttiwong T, Kunathikom S (2007) Evaluation of cryoinjury of sperm chromatin according to liquid nitrogen vapour method (I). J Med Assoc Thai 90:224–228
O’Connell M, McClure N, Lewis SE (2002) The effects of cryopreservation on sperm morphology, motility and mitochondrial function. Hum Reprod 17:704–709
Oehninger S, Duru NK, Srisombut C, Morshedi M (2000) Assessment of sperm cryodamage and strategies to improve outcome. Mol Cell Endocrinol 169:3–10
Ortiz A, Espino J, Bejarano I, Lozano GM, Monllor F, García JF, Pariente JA, Rodríguez AB (2011) High endogenous melatonin concentrations enhance sperm quality and short-term in vitro exposure to melatonin improves aspects of sperm motility. J Pineal Res 50:132–139
Paasch U, Sharma RK, Gupta AK, Grunewald S, Mascha EJ, Thomas AJ Jr, Glander HJ, Agarwal A (2004) Cryopreservation and thawing is associated with varying extent of activation of apoptotic machinery in subsets of ejaculated human spermatozoa. Biol Reprod 71:1828–1837
Pini T, Leahy T, de Graaf SP (2018) Sublethal sperm freezing damage: Manifestations and solutions. Theriogenology 118:172–181
Polge C, Smith AU, Parkes AS (1949) Revival of spermatozoa after vitrification and dehydration at low temperatures. Nature 164:666
Reiter RJ, Tan DX, Manchester LC, Paredes SD, Mayo JC, Sainz RM (2009) Melatonin and reproduction revisited. Biol Reprod 81:445–456
Rossi T, Mazzilli F, Delfino M, Dondero F (2001) Improved human sperm recovery using superoxide dismutase and catalase supplementation in semen cryopreservation procedure. Cell Tissue Bank 2:9–13
Rostand J (1946) Glycerine et resistance du sperm aux basses temperature. CR Acad Sci Paris 222:1524
Said TM, Gaglani A, Agarwal A (2010) Implication of apoptosis in sperm cryoinjury. Reprod Biomed Online 21:456–462
Saito K, Suzuki K, Iwasaki A, Yumura Y, Kubota Y (2005) Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer 104:521–524
Sariözkan S, Bucak MN, Tuncer PB, Ulutaş PA, Bilgen A (2009) The influence of cysteine and taurine on microscopic-oxidative stress parameters and fertilizing ability of bull semen following cryopreservation. Cryobiology 58:134–138
Seifi-Jamadi A, Kohram H, Shahneh AZ, Ansari M, Macías-García B (2016) Quercetin ameliorate motility in frozen-thawed Türkmen stallions sperm. J Equine Vet Sci 45:73–77
Semercioz A, Onur R, Ogras S, Orhan I (2003) Effects of melatonin on testicular tissue nitric oxide level and antioxidant enzyme activities in experimentally induced left varicocele. Neuro Endocrinol Lett 24:86–90
Shabani Nashtaei M, Nekoonam S, Naji M, Bakhshalizadeh S, Amidi F (2018) Cryoprotective effect of resveratrol on DNA damage and crucial human sperm messenger RNAs, possibly through 5' AMP-activated protein kinase activation. Cell Tissue Bank 19:87–95
Shafiei M, Forouzanfar M, Hosseini SM, Esfahani MH (2015) The effect of superoxide dismutase mimetic and catalase on the quality of postthawed goat semen. Theriogenology 83:1321–1327
Sherman JK (1963) Improved methods of preservation of human spermatozoa by freezing and freeze-drying. Fertil Steril 14:49–64
Sherman JF (1990) Cryopreservation of human semen. In: Keel B, Webster BW (eds) Handbook of the laboratory diagnosis and treatment of infertility. CRC Press, Boca Raton/Ann Arbor/Boston, pp 229–260
Sierens J, Hartley J, Campbell M, Leathem A, Woodside J (2002) In vitro isoflavone supplementation reduces hydrogen peroxide-induced DNA damage in sperm. Teratog Carcinog Mutagen 22:227–234
Silva EC, Cajueiro JF, Silva SV, Soares PC, Guerra MM (2012) Effect of antioxidants resveratrol and quercetin on in vitro evaluation of frozen ram sperm. Theriogenology 77:1722–1726
Song GJ, Norkus EP, Lewis V (2006) Relationship between seminal ascorbic acid and sperm DNA integrity in infertile men. Int J Androl 29:569–575
Sönmez M, Yüce A, Türk G (2007) The protective effect of melatonin and Vitamin E on antioxidant enzyme activities and epididymal sperm characteristics of homocysteine treated male rats. Reprod Toxicol 23:226–231
Spanò M, Cordelli E, Leter G, Lombardo F, Lenzi A, Gandini L (1999) Nuclear chromatin variations in human spermatozoa undergoing swim-up and cryopreservation evaluated by the flow cytometric sperm chromatin structure assay. Mol Hum Reprod 5:29–37
Stojanović S, Sprinz H, Brede O (2001) Efficiency and mechanism of the antioxidant action of trans-resveratrol and its analogues in the radical liposome oxidation. Arch Biochem Biophys 391:79–89
Succu S, Berlinguer F, Pasciu V, Satta V, Leoni GG, Naitana S (2011) Melatonin protects ram spermatozoa from cryopreservation injuries in a dose-dependent manner. J Pineal Res 50:310–318
Sun JG, Jurisicova A, Casper RF (1997) Detection of deoxyribonucleic acid fragmentation in human sperm: correlation with fertilization in vitro. Biol Reprod 56:602–607
Tan DX, Manchester LC, Reiter RJ, Qi WB, Karbownik M, Calvo JR (2000) Significance of melatonin in antioxidative defense system: reactions and products. Biol Signals Recept 9:137–159
Taylor K, Roberts P, Sanders K, Burton P (2009) Effect of antioxidant supplementation of cryopreservation medium on post-thaw integrity of human spermatozoa. Reprod Biomed Online 18:184–189
Thomson LK, Fleming SD, Aitken RJ, De Iuliis GN, Zieschang JA, Clark AM (2009) Cryopreservation-induced human sperm DNA damage is predominantly mediated by oxidative stress rather than apoptosis. Hum Reprod 24:2061–2070
Topraggaleh TR, Shahverdi A, Rastegarnia A, Ebrahimi B, Shafiepour V, Sharbatoghli M, Esmaeili V, Janzamin E (2014) Effect of cysteine and glutamine added to extender on post-thaw sperm functional parameters of buffalo bull. Andrologia 46:777–783
Uysal O, Bucak MN (2007) Effects of oxidized glutathione, bovine serum albumin, cysteine and lycopene on the quality of frozen-thawed ram semen. Acta Vet Brno 76:383–390
Wang X, Sharma RK, Sikka SC, Thomas AJ, Falcone T, Agarwal A (2003) Oxidative stress is associated with increased apoptosis leading to spermatozoa DNA damage in patients with male factor infertility. Fertil Steril 80:531–535
White IG (1993) Lipids and calcium uptake of sperm in relation to cold shock and preservation: a review. Reprod Fertil Dev 5:639–658
Yan L, Liu J, Wu S, Zhang S, Ji G, Gu A (2014) Seminal superoxide dismutase activity and its relationship with semen quality and SOD gene polymorphism. J Assist Reprod Genet 31:549–554
Zeitoun MM, Al-Damegh MA (2014) Effect of nonenzymatic antioxidants on sperm motility and survival relative to free radicals and antioxidant enzymes of chilled-stored ram semen. Open J Anim Sci 5:50
Zeron Y, Pearl M, Borochov A, Arav A (1999) Kinetic and temporal factors influence chilling injury to germinal vesicle and mature bovine oocytes. Cryobiology 38:35–42
Zhu Z, Ren Z, Fan X, Pan Y, Lv S, Pan C, Lei A, Zeng W (2017) Cysteine protects rabbit spermatozoa against reactive oxygen species-induced damages. PLoS One 12:e0181110
Zielonka J, Gebicki J, Grynkiewicz G (2003) Radical scavenging properties of genistein. Free Radic Biol Med 35:958–965
Zribi N, Feki Chakroun N, El Euch H, Gargouri J, Bahloul A, Ammar Keskes L (2010) Effects of cryopreservation on human sperm deoxyribonucleic acid integrity. Fertil Steril 93:159–166
Zribi N, Feki Chakroun N, Ben Abdallah F, Elleuch H, Sellami A, Rebai T, Fakhfakh F, Keskes LA (2012) Effect of freezing-thawing process and quercetin on human sperm survival and DNA integrity. Cryobiology 65:326–331
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Paoli, D., Pelloni, M., Lenzi, A., Lombardo, F. (2019). Cryopreservation of Sperm: Effects on Chromatin and Strategies to Prevent Them. In: Baldi, E., Muratori, M. (eds) Genetic Damage in Human Spermatozoa. Advances in Experimental Medicine and Biology, vol 1166. Springer, Cham. https://doi.org/10.1007/978-3-030-21664-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-21664-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21663-4
Online ISBN: 978-3-030-21664-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)