Abstract
In the past 20 years, musculoskeletal ultrasound has accumulated important evidence supporting its role for the assessment and treatment monitoring of several inflammatory rheumatic diseases.
The expanding applications of this imaging modality include many examinations that are new to pediatric rheumatologists but are known to the adult colleagues.
In this chapter, we present an introduction of some of these more sophisticated imaging technologies, such as three-dimensional ultrasound, elastography, and fusion imaging as well as their potential clinical impact in assessing pediatric musculoskeletal disorders. Three-dimensional US (B-mode and Doppler imaging) offers objective quantification of synovial proliferation and vascularity, and it can improve the assessment accuracy of bone erosions due to its multiplanar view (longitudinal, transverse, and coronal planes) as well as three-dimensional reconstruction. Elastography offers tissue elasticity evaluation by measurement of tissue displacement in terms of tissue stiffness changes, promising improved assessment of tendon pathology. However, it is still looking for its role in juvenile inflammatory myopathies. Fusion imaging is an exciting development that displays simultaneously in the monitor, the ultrasound image, and the corresponding computed tomography/magnetic resonance imaging scan. This technique is considered helpful in guiding challenging intra-articular injections.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
In relatively recent years, ultrasound (US) imaging has progressed rapidly improving the diagnostic accuracy in several rheumatic conditions, and it is currently considered a first-line research tool for several musculoskeletal diseases. Better transducer technology is now available increasing B-mode image quality as well as information from Doppler imaging. Additionally, new US technologies such as three-dimensional (3D) US, elastography (ES), and fusion imaging (FI) are able to increase the traditional role of US. The purpose of this chapter is to bring this new technology closer to pediatric rheumatologist and to summarize some of its possible clinical applications.
Content
Three-Dimensional Ultrasound (3D US)
In the clinical setting, this technology has been mostly used in obstetrics [1,2,3], urology [4], and cardiology [5]. In recent years, it has also demonstrated its potential role in some adult rheumatologic conditions such as rheumatoid arthritis (RA) [6], spondyloarthritis (SPA) [7], and rotator cuff pathology [8]. There are several 3D US image acquisition techniques [9].In rheumatological practice, a volumetric probe (a large footprint probe that covers a relatively wide anatomical area) (Fig. 20.1) is used in order to obtain a 3D US image in an automatic manner and in a few seconds. The image acquisition, in both grayscale and power Doppler (PD) modes, is performed by an automatic sweeping scan movement of the piezoelectric crystals located inside the probe. This technique offers virtual operator independence due to transducer automated sweeping. In order to generate the US images, the operator places the volumetric probe with a steady hand on the chosen anatomical area which is covered by a generous layer of acoustic gel and then presses the acquisition button. After 4 s, the ultrasound images are ready to be examined on longitudinal, transverse, and coronal planes and on 3D reconstruction as well. The stored US images are also available to be examined at any time and without the presence of the patient. It is important to stress that even though 3D US seems to be not operator dependent, the diagnostic quality of the US volumetric images is influenced by the ultrasonographer knowledge of anatomic landmarks, the correct placement of the probe, the use of an appropriate amount of acoustic gel, and finally the avoidance of probe movement. A very recent study where 31 RA patients underwent examination of seven joints (491 anatomic sites) by 2D and 3D US for synovitis and tenosynovitis in B and PD modes and erosions in B-mode revealed that 15% of the 3D scans could not be properly evaluated due to technical issues with the image acquisition (nonachievement of minimum standard of image quality) [10]. Although image acquisition time is shorter than with 2D US, image reconstruction and interpretation can be time-consuming, and its accurate evaluation still depends on previous training. The 3D PDUS is considered a reliable imaging technique due to its capability to assess synovial vascularity in inflamed wrists of RA patients when compared with clinical symptoms and the gold standard contrast-enhanced magnetic resonance imaging (MRI) [11]. 3D PDUS allows the spatial demonstration of synovial blood vessels in the peri- and intra-articular region of inflamed joints in patients with RA [12]. Furthermore, several studies have confirmed good-to-excellent agreement in both qualitative and semiquantitative assessments of joint inflammation and bone erosions between 3D US and conventional 2D US when examining RA hand and wrist joints [10, 13,14,15]. Acebes et al. [10] found that a higher level of agreement was attained for patient global scores than for individual joints. Naredo et al. [15] reported that 3D US may even improve the reliability for inflammatory changes of the hand and wrist in patients with RA, but they did not show a significant inter-modality agreement for bone erosions. A recent study [16] that investigated the performance of 3D US in the detection of bone erosions in hand and wrist joints of radiographically nonerosive RA patients compared to computed tomography (CT) as the reference method revealed that 3D US exhibited a sensitivity of 90% and a specificity of 55% in identifying erosive patients, suggesting that the majority of erosive patients identified by 3D US were correctly classified. However, more than 50% of the cortical breaks detected with 3D US were not considerate CT true erosions showing that at a single erosion level, misclassification can occur on 3D US. Contrary to Naredo et al. [15], Lai et al. [17] did not find any relevant advantage of a 3D transducer with respect to the 2D US assessment in wrist inflammation in RA patients. Due to the possible observation of synovial blood vessels and angiogenesis in patients with synovitis by 3D PDUS imaging, this method can play a key role in monitoring anti-inflammatory and biological therapy in RA as shown by some studies [18,19,20,21]. Another important advantage for therapy monitoring which has a major impact on follow-up examinations of synovitis is the fact that due to the sweep over the entire joint, the 3D imaging provides a true 3D perspective of the whole anatomical region which can be processed immediately for objective quantification (Fig. 20.2). In the case of conventional 2D US, only the directly accessible part of the inflamed joint region can be imaged. Four-dimensional US (real-time 3D US)-guided biopsy is feasible and can improve visualization of biopsy procedures by using multiplanar views as shown by [22]. Although the accuracy is comparable to that of conventional 2D biopsy, this technique may be helpful for biopsy of lesions with close relation to relevant anatomical structures. It’s relevant to stress that a potential use of this technique imaging may be in guiding synovial and tenosynovial biopsies. In spondyloarthritis (SPA), similar findings comparing conventional 2D and 3D US have been shown for Achilles tendon involvement [7] as well as for the presence and change of calcaneal bone erosions [23]. Further studies are needed to validate this technique in psoriatic arthritis. Regarding the pediatric population and the musculoskeletal (MSK) system, there are a number of studies on the potential applications of this method mainly in infant hip dysplasia [24,25,26,27]. 3D US can display the full acetabular shape, improving the assessment accuracy of developmental dysplasia of the hip. To date, there is no data in the medical literature about this innovative technique and its use in the diagnosis and/or follow-up of inflammatory arthritis in children. One important limitation of the application of this imaging tool is the size and shape of the 3D transducer which can decrease its ability to study the MSK system of this age range. Another disadvantage is the fact that the image acquisition process does not allow for movement, thus preventing the possibility of obtaining a dynamic image which is an essential part of the examination of tendons in children and adults. Even though its image resolution is inferior to conventional 2D US, 3D US can be used for training and education, as it is an ideal tool to demonstrate complex anatomy and vasculature (Fig. 20.3) and the 3D volume can be virtually rescanned without the patient’s presence. The improvement of transducer technology with higher resolution and smaller size may allow pediatric MSK 3D US to become a promising imaging tool for assisting the diagnosis and follow-up of some of the pediatric rheumatologic diseases (Fig. 20.4).
3D data of synovitis of the right knee of a 3-year-old girl with juvenile idiopathic arthritis. Each image is a mosaic of nine ultrasound images showing mild suprapatellar pouch enlargement due to synovitis. (a) One transverse view of the one in the upper left corner and eight longitudinal views parallel to each other and distance of 2.5 mm between each other; (b) one longitudinal view of the one in the upper left corner and eight transverse views parallel to each other and distance of 2.5 mm between each other;(c) one longitudinal view of the one in the upper left corner and eight coronal views parallel to each other and distance of 2.5 mm between each other. (Courtesy of E. Filippucci, MD)
Ultrasound Elastography (Sonoelastography)
Ultrasound is an essential tool in medical imaging. New recent applications as elastography (ES) can contribute to the assessment of rheumatic diseases. In addition to the information obtained from B-mode and Doppler ultrasonography, ES can provide a different form of tissue evaluation as it may show pathologic changes before its detection on B-mode imaging. Besides that, since the pathological and the surrounding healthy tissue may often present the same echogenicity on conventional US, it is sometimes difficult to distinguish between them [28].
Tissue elasticity assessment by ES is based on the principle that tissue compression produces strain (displacement) which is lower in harder and less compressible tissues and higher in softer and more compressible ones [29].
There are currently two main methods used to perform ES in the clinical setting: strain or compression ES (the most common one) and shear-wave ES . Essentially, strain ES measures the elasticity of the tissue through the collection of US echo data before and after a slight compression applied from the transducer by repetitive manual pressure and, thus, a qualitative, color-coded strain map termed elastogram is obtained. Different grades of elasticity are frequently super-imposed on the related B-mode image in order to show anatomical localization using diverse coloring (yellow to red in soft tissues and green and blue representing hard ones). A potential disadvantage of this image modality is the variability in the pressure applied to the tissue, which might affect reproducibility. Tissue shifting due to unilateral compression is another relevant issue; the use of a gel standoff pad can help to reduce this problem. It is recommended to apply at least three cycles of compression and decompression for an ideal assessment [30]; however, it is important to stress that repeated compressions may cause excessive preload of the tissues modifying tissue elasticity. To address this problem, there is a visual indicator scale on the machine that monitors the relationship between pressure exerted and tissue strain. If the pressure decreases or increases below a certain level, the pattern of the elasticity image changes considerably.
Unlike strain elastography, shear-wave elastography allows the determination of the actual tissue elasticity since it applies a vibration to tissues through a focused US pulse generated by a linear transducer, which by itself provides a local stress generating tissue displacement without the need for manual compression. The vibration within the tissues creates shear waves (transverse waves) which are perpendicular to the US pulse and propagate faster in stiffer tissues. A quantitative color-coded elastogram on the US screen displays shear-wave velocities in meters per second or tissue elasticity in kilopascals [31]. Shear-wave ES is thus likely to be more objective and reproducible than strain ES due to direct assessment of tissue elasticity, with the possibility to obtain quantitative measurements. A major limitation of this imaging tool is the fact that very deep (>9 cm from the skin) or very superficial structures cannot be assessed [32]. Shallow depths may be compensated by using a gel standoff pad.
Additionally, shear-wave ES is sensitive to transducer pressure and angle similar to strain ES [33]. Shear-wave measurements are potentially affected by the way the anatomical structure is evaluated (long vs short axis) due to anisotropy as well as the size and shape of the region of interest. The heating generated by the repetitive use of the shear-wave ES may modify the measurements and cause tissue damage. This is compensated by a cooling delay. Finally, cystic structures are not well analyzed owing to the fact that shear waves are not generated within fluids [34]. Tissue elasticity changes caused by tumors have already been evaluated in breast [35,36,37,38], thyroid [39, 40], and prostate cancers [41, 42]. Despite the recent advances in tumor diagnosis with ES, biopsy still remains the gold standard. However, it is now considered the standard imaging tool in the assessment of liver fibrosis, even, replacing biopsy in many cases [43].
Recently, ES has been proven useful in the evaluation of rheumatic disorders such as tendinosis [44] (Achilles tendon [45, 46], supraspinatus tendon [47], common extensor tendon of the elbow [48], SPA (Achilles tendon abnormalities) [49]), polymyalgia rheumatica (subacromial-subdeltoid bursitis) [50], carpal tunnel syndrome [51], Sjögren’s syndrome (salivary tissue assessment) [52], gout (gouty arthritis) [53], adhesive capsulitis of the shoulder (coracohumeral ligament) [54], and inflammatory myopathies [55, 56]. Regarding systemic sclerosis (SSc), a very recent systematic review about US assessment of the skin in SSc which included three studies on strain ES and three studies on shear-wave ES showed significantly higher shear-wave velocities in SSc patients than in controls [57]. To date, there is little information regarding the elastographic appearance of the synovium in rheumatoid arthritis. Recently, a cross-sectional study presented as a poster (FRI0525—Sammel AM et al. 2016) evaluated nine patients with low to moderate activity of RA and five controls with shear-wave elastography of the MCP joints. The authors found significantly lower maximum shear-wave velocity in RA patients than in controls (6.38 m/s vs 6.99 m/s p = 0.042). In MSK disorders in children, ES has been mostly used to evaluate muscle elasticity in healthy subjects (at rest and after exercise) [58] and in patients with congenital muscle torticollis [59, 60], cerebral palsy [61], myositis [56], and in Bethlem myopathy, a congenital muscle dystrophy [62].Regarding cerebral palsy, ES was equally used to guide botulinum toxin injections into contracted muscle fibers, identified as hard (blue) on the elastogram [63]. A recent study [56] that evaluated inflammatory myopathies (dermatomyositis (41,2%), polymyositis (29,4%), systemic lupus erythematosus overlap (11.8%), juvenile dermatomyositis (5.9%), mixed connective tissue disease (5.9%), and RA overlap (5.9%)) by physical examination, imaging (MRI and strain ES), and histopathology showed alteration in the normal muscle elastogram, with predominance of stiff appearance of pathological muscles. Besides that, the authors also found a correlation between sonographic stiffness and the inflammatory changes on muscle biopsy suggesting that strain ES could be an important tool in identifying and measuring the degree of muscular inflammation. In contrast, Berko N et al. [64] who evaluated the performance of strain ES in the diagnosis of juvenile idiopathic inflammatory myopathy compared to MRI showed no association between abnormal muscle appearance on the elastogram and muscle edema detected on MRI (P > 0.999). Muscle elasticity was assessed based on a comparison with previously published findings of muscle elasticity in a cohort of normal children of similar age and gender [58]. The areas of signal abnormality seen on MRI in patients with active inflammatory myopathy correspond to areas of muscle edema. A possible explanation for the absence of correlation between ES and MRI is the fact that sonoelastography might not be able to detect small changes in fluid related to muscle inflammation seen on MRI as well as the smaller area of the muscle able to be evaluated with ES. Patients with JDM often have heterogeneous areas of affected muscle, and therefore it is possible that the area of muscle analyzed on the ES studies was not an area of active disease.
Other potential limitations of strain ES in assessing skeletal muscles are related to reproducibility, and it is possible that other ES tools, such as shear-wave ES and magnetic resonance elastography [65], may be useful in the assessment of muscular diseases. However, it is important to note that understanding and interpreting color elastograms and shear-wave velocities requires knowledge of the basic ultrasound physics of shear-wave ES. More research is needed to establish the role of ES in assessing myositis and other muscle disorders. To date, this image modality is unlikely to replace muscle biopsy for the diagnosis of muscular pathologies.
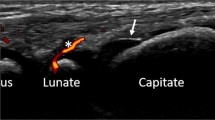
Fusion Imaging
Another interesting approach is the fusion imaging (FI) which software may be integrated into high-end US machines. This imaging modality overlaps information from previously performed computed tomography (CT) or MRI on to real-time image acquisition by US scanning with better illustrations of bony and certain soft-tissue lesions. This is particularly promising for intra-articular guided infiltrations, improving injection accuracy, especially into the sacroiliac joints. Bony landmarks are provided by the CT scan and the needle placement is guided by real-time US [66]. With respect to rheumatic diseases, the FI applications have already been evaluated in the hand and wrist joints of patients with RA and osteoarthritis [67] and in shoulder pathology [68].
Regarding the pediatric population, the major limitations to the use of this technology are the difficulty that children have to tolerate MRI exam without sedation and the well-established risk for developing a radiation-related cancer when exposed to CT scan. However, young patients with chronic sacroiliitis who require several infiltrations of the sacroiliac joints already have the necessary information from previously performed CT scan reducing repeated radiation exposure [66].
Conclusion
New developments in US imaging such as 3D US and ES have potential applications in pediatric rheumatic diseases. An interdisciplinary approach between pediatric rheumatologists and radiologists is essential to spread information on the advantages of using such imaging tools. This cooperation might certainly result in optimal patient management. Besides that, despite all advances in imaging diagnosis, much remains to be done regarding pediatric rheumatology.
References
Tonni G, Araujo Junior E. Three-dimensional ultrasound in obstetrics practice: myth or reality? Rev Bras Ginecol Obstet. 2014;36(4):143–5.
Goncalves LF, Lee W, Espinoza J, Romero R. Three- and 4-dimensional ultrasound in obstetric practice: does it help? J Ultrasound Med. 2005;24(12):1599–624.
Kurjak A, Miskovic B, Andonotopo W, Stanojevic M, Azumendi G, Vrcic H. How useful is 3D and 4D ultrasound in perinatal medicine? J Perinat Med. 2007;35(1):10–27.
Cool DW, Connolly MJ, Sherebrin S, Eagleson R, Izawa JI, Amann J, et al. Repeat prostate biopsy accuracy: simulator-based comparison of two- and three-dimensional transrectal US modalities. Radiology. 2010;254(2):587–94.
Surkova E, Muraru D, Aruta P, Romeo G, Bidviene J, Cherata D, et al. Current clinical applications of three-dimensional echocardiography: when the technique makes the difference. Curr Cardiol Rep. 2016;18(11):109.
Filippucci E, Meenagh G, Epis O, Iagnocco A, Riente L, Delle Sedie A, et al. Ultrasound imaging for the rheumatologist. XIII. New trends. Three-dimensional ultrasonography. Clin Exp Rheumatol. 2008;26(1):1–4.
Iagnocco A, Riente L, Delle Sedie A, Filippucci E, Salaffi F, Meenagh G, et al. Ultrasound imaging for the rheumatologist. XXII. Achilles tendon involvement in spondyloarthritis. A multi-Centre study using high frequency volumetric probe. Clin Exp Rheumatol. 2009;27(4):547–51.
Wallny TA, Schild RL, Schulze Bertelsbeck D, Hansmann ME, Kraft CN. Three-dimensional ultrasonography in the diagnosis of rotator cuff lesions. Ultrasound Med Biol. 2001;27(6):745–9.
Downey DB, Fenster A, Williams JC. Clinical utility of three-dimensional US. Radiographics. 2000;20(2):559–71.
Acebes C, McKay N, Ciechomska A, Alcorn N, Harvie JP, Robson B, et al. Level of agreement between three-dimensional volumetric ultrasound and real-time conventional ultrasound in the assessment of synovitis, tenosynovitis and erosions in rheumatoid arthritis patients. Rheumatol Int. 2017;37(2):197–205.
Strunk J, Klingenberger P, Strube K, Bachmann G, Muller-Ladner U, Kluge A. Three-dimensional Doppler sonographic vascular imaging in regions with increased MR enhancement in inflamed wrists of patients with rheumatoid arthritis. Joint Bone Spine. 2006;73(5):518–22.
Strunk J, Lange U. Three-dimensional power Doppler sonographic visualization of synovial angiogenesis in rheumatoid arthritis. J Rheumatol. 2004;31(5):1004–6.
Filippucci E, Meenagh G, De Agustin JJ, De Miguel E, Iagnocco A, Mayordomo L, et al. Level of agreement between rheumatologists on US image acquisition using a 3D volumetric probe. Clin Exp Rheumatol. 2007;25(1):116.
Filippucci E, Meenagh G, Delle Sedie A, Salaffi F, Riente L, Iagnocco A, et al. Ultrasound imaging for the rheumatologist. XX. Sonographic assessment of hand and wrist joint involvement in rheumatoid arthritis: comparison between two- and three-dimensional ultrasonography. Clin Exp Rheumatol. 2009;27(2):197–200.
Naredo E, Moller I, Acebes C, Batlle-Gualda E, Brito E, de Agustin JJ, et al. Three-dimensional volumetric ultrasonography. Does it improve reliabililty of musculoskeletal ultrasound? Clin Exp Rheumatol. 2010;28(1):79–82.
Peluso G, Bosello SL, Gremese E, Mirone L, Di Gregorio F, Di Molfetta V, et al. Detection of bone erosions in early rheumatoid arthritis: 3D ultrasonography versus computed tomography. Clin Rheumatol. 2015;34(7):1181–6.
Lai KL, Chen DY, Chen YH, Huang WN, Hsieh TY, Hsieh CW, et al. Assessment of wrist joint inflammation in patients with rheumatoid arthritis by quantitative two- and three-dimensional power Doppler ultrasonography. Clin Exp Rheumatol. 2014;32(5):674–9.
Meenagh G, Filippucci E, Abbattista T, Busilacchi P, Grassi W. Three-dimensional power Doppler sonography in short-term therapy monitoring of rheumatoid synovitis. Rheumatology (Oxford). 2007;46(11):1736.
Strunk J, Strube K, Muller-Ladner U, Lange U. Three dimensional power Doppler ultrasonography confirms early reduction of synovial perfusion after intra-articular steroid injection. Ann Rheum Dis. 2006;65(3):411–2.
Strunk J, Strube K, Rumbaur C, Lange U, Muller-Ladner U. Interobserver agreement in two- and three-dimensional power Doppler sonographic assessment of synovial vascularity during anti-inflammatory treatment in patients with rheumatoid arthritis. Ultraschall Med. 2007;28(4):409–15.
Naredo E, Acebes C, Brito E, de Agustin JJ, de Miguel E, Mayordomo L, et al. Three-dimensional volumetric ultrasound: a valid method for blinded assessment of response to therapy in rheumatoid arthritis. J Rheumatol. 2013;40(3):253–60.
Albrecht H, Stroszczynski C, Felix R, Hunerbein M. Real time 3D (4D) ultrasound-guided percutaneous biopsy of solid tumours. Ultraschall Med. 2006;27(4):324–8.
de Miguel E, Falcao S, Castillo C, Plasencia C, Garcia M, Branco JC, et al. Enthesis erosion in spondyloarthritis is not a persistent structural lesion. Ann Rheum Dis. 2011;70(11):2008–10.
Diederichs C, Heath A, Hareendranathan AR, Zonoobi D, Kuntze G, Dulai S, et al. Cross-modality validation of acetabular surface models using 3-d ultrasound versus magnetic resonance imaging in normal and dysplastic infant hips. Ultrasound Med Biol. 2016;42(9):2308–14.
Mabee MG, Hareendranathan AR, Thompson RB, Dulai S, Jaremko JL. An index for diagnosing infant hip dysplasia using 3-D ultrasound: the acetabular contact angle. Pediatr Radiol. 2016;46(7):1023–31.
Jaremko JL, Mabee M, Swami VG, Jamieson L, Chow K, Thompson RB. Potential for change in US diagnosis of hip dysplasia solely caused by changes in probe orientation: patterns of alpha-angle variation revealed by using three-dimensional US. Radiology. 2014;273(3):870–8.
Hareendranathan AR, Zonoobi D, Mabee M, Diederichs C, Punithakumar K, Noga M, et al. Semiautomatic classification of acetabular shape from three-dimensional ultrasound for diagnosis of infant hip dysplasia using geometric features. Int J Comput Assist Radiol Surg. 2017;12(3):439–47.
Frey H. Realtime elastography. A new ultrasound procedure for the reconstruction of tissue elasticity. Radiologe. 2003;43(10):850–5.
Garra BS. Imaging and estimation of tissue elasticity by ultrasound. Ultrasound Q. 2007;23(4):255–68.
Klauser AS, Faschingbauer R, Jaschke WR. Is sonoelastography of value in assessing tendons? Semin Musculoskelet Radiol. 2010;14(3):323–33.
Taljanovic MS, Gimber LH, Becker GW, Latt LD, Klauser AS, Melville DM, et al. Shear-wave elastography: basic physics and musculoskeletal applications. Radiographics. 2017;37(3):855–70.
Winn N, Lalam R, Cassar-Pullicino V. Sonoelastography in the musculoskeletal system: current role and future directions. World J Radiol. 2016;8(11):868–79.
Kot BC, Zhang ZJ, Lee AW, Leung VY, Fu SN. Elastic modulus of muscle and tendon with shear wave ultrasound elastography: variations with different technical settings. PLoS One. 2012;7(8):e44348.
Elkateb Hachemi M, Calle S, Remenieras JP. Transient displacement induced in shear wave elastography: comparison between analytical results and ultrasound measurements. Ultrasonics. 2006;44(Suppl 1):e221–5.
Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239(2):341–50.
Evans A, Whelehan P, Thomson K, McLean D, Brauer K, Purdie C, et al. Invasive breast cancer: relationship between shear-wave elastographic findings and histologic prognostic factors. Radiology. 2012;263(3):673–7.
Tozaki M, Isobe S, Sakamoto M. Combination of elastography and tissue quantification using the acoustic radiation force impulse (ARFI) technology for differential diagnosis of breast masses. Jpn J Radiol. 2012;30(8):659–70.
Carlsen J, Ewertsen C, Sletting S, Vejborg I, Schafer FK, Cosgrove D, et al. Ultrasound elastography in breast cancer diagnosis. Ultraschall Med. 2015;36(6):550–62; quiz 63-5.
Bojunga J, Dauth N, Berner C, Meyer G, Holzer K, Voelkl L, et al. Acoustic radiation force impulse imaging for differentiation of thyroid nodules. PLoS One. 2012;7(8):e42735.
Azizi G, Keller JM, Mayo ML, Piper K, Puett D, Earp KM, et al. Thyroid nodules and shear wave elastography: a new tool in thyroid cancer detection. Ultrasound Med Biol. 2015;41(11):2855–65.
Correas JM, Tissier AM, Khairoune A, Vassiliu V, Mejean A, Helenon O, et al. Prostate cancer: diagnostic performance of real-time shear-wave elastography. Radiology. 2015;275(1):280–9.
Woo S, Suh CH, Kim SY, Cho JY, Kim SH. Shear-wave elastography for detection of prostate cancer: a systematic review and diagnostic meta-analysis. AJR Am J Roentgenol. 2017;209(4):806–14.
Barr RG, Ferraioli G, Palmeri ML, Goodman ZD, Garcia-Tsao G, Rubin J, et al. Elastography assessment of liver fibrosis: society of radiologists in ultrasound consensus conference statement. Ultrasound Q. 2016;32(2):94–107.
Fusini F, Langella F, Busilacchi A, Tudisco C, Gigante A, Masse A, et al. Real-time sonoelastography: principles and clinical applications in tendon disorders. A systematic review. Muscles Ligaments Tendons J. 2017;7(3):467–77.
De Zordo T, Chhem R, Smekal V, Feuchtner G, Reindl M, Fink C, et al. Real-time sonoelastography: findings in patients with symptomatic achilles tendons and comparison to healthy volunteers. Ultraschall Med. 2010;31(4):394–400.
Tan S, Kudas S, Ozcan AS, Ipek A, Karaoglanoglu M, Arslan H, et al. Real-time sonoelastography of the Achilles tendon: pattern description in healthy subjects and patients with surgically repaired complete ruptures. Skelet Radiol. 2012;41(9):1067–72.
Lee SU, Joo SY, Kim SK, Lee SH, Park SR, Jeong C. Real-time sonoelastography in the diagnosis of rotator cuff tendinopathy. J Shoulder Elb Surg. 2016;25(5):723–9.
Klauser AS, Pamminger M, Halpern EJ, Abd Ellah MMH, Moriggl B, Taljanovic MS, et al. Extensor tendinopathy of the elbow assessed with sonoelastography: histologic correlation. Eur Radiol. 2017;27(8):3460–6.
Turan A, Tufan A, Mercan R, Teber MA, Tezcan ME, Bitik B, et al. Real-time sonoelastography of Achilles tendon in patients with ankylosing spondylitis. Skelet Radiol. 2013;42(8):1113–8.
Silvestri E, Garlaschi G, Bartolini B, Minetti G, Schettini D, D’Auria MC, et al. Sonoelastography can help in the localization of soft tissue damage in polymyalgia rheumatica (PMR). Clin Exp Rheumatol. 2007;25(5):796.
Orman G, Ozben S, Huseyinoglu N, Duymus M, Orman KG. Ultrasound elastographic evaluation in the diagnosis of carpal tunnel syndrome: initial findings. Ultrasound Med Biol. 2013;39(7):1184–9.
Hofauer B, Mansour N, Heiser C, Gahleitner C, Thuermel K, Bas M, et al. Sonoelastographic modalities in the evaluation of salivary gland characteristics in Sjogren’s syndrome. Ultrasound Med Biol. 2016;42(9):2130–9.
Tang Y, Yan F, Yang Y, Xiang X, Wang L, Zhang L, et al. Value of shear wave Elastography in the diagnosis of gouty and non-gouty arthritis. Ultrasound Med Biol. 2017;43(5):884–92.
Wu CH, Chen WS, Wang TG. Elasticity of the Coracohumeral ligament in patients with adhesive capsulitis of the shoulder. Radiology. 2016;278(2):458–64.
Botar-Jid C, Damian L, Dudea SM, Vasilescu D, Rednic S, Badea R. The contribution of ultrasonography and sonoelastography in assessment of myositis. Med Ultrason. 2010;12(2):120–6.
Song Y, Lee S, Yoo DH, Jang KS, Bae J. Strain sonoelastography of inflammatory myopathies: comparison with clinical examination, magnetic resonance imaging and pathologic findings. Br J Radiol. 2016;89(1065):20160283.
Santiago T, Santiago M, Ruaro B, Salvador MJ, Cutolo M, da Silva JAP. Ultrasonography for the assessment of skin in systemic sclerosis: a systematic review. Arthritis Care Res (Hoboken). 2018;
Berko NS, Fitzgerald EF, Amaral TD, Payares M, Levin TL. Ultrasound elastography in children: establishing the normal range of muscle elasticity. Pediatr Radiol. 2014;44(2):158–63.
Lee SY, Park HJ, Choi YJ, Choi SH, Kook SH, Rho MH, et al. Value of adding sonoelastography to conventional ultrasound in patients with congenital muscular torticollis. Pediatr Radiol. 2013;43(12):1566–72.
Park GY, Kwon DR, Kwon DG. Shear wave sonoelastography in infants with congenital muscular torticollis. Medicine (Baltimore). 2018;97(6):e9818.
Kwon DR, Park GY, Lee SU, Chung I. Spastic cerebral palsy in children: dynamic sonoelastographic findings of medial gastrocnemius. Radiology. 2012;263(3):794–801.
Drakonaki EE, Allen GM. Magnetic resonance imaging, ultrasound and real-time ultrasound elastography of the thigh muscles in congenital muscle dystrophy. Skelet Radiol. 2010;39(4):391–6.
Vasilescu D, Vasilescu D, Dudea S, Botar-Jid C, Sfrangeu S, Cosma D. Sonoelastography contribution in cerebral palsy spasticity treatment assessment, preliminary report: a systematic review of the literature apropos of seven patients. Med Ultrason. 2010;12(4):306–10.
Berko NS, Hay A, Sterba Y, Wahezi D, Levin TL. Efficacy of ultrasound elastography in detecting active myositis in children: can it replace MRI? Pediatr Radiol. 2015;45(10):1522–8.
McCullough MB, Domire ZJ, Reed AM, Amin S, Ytterberg SR, Chen Q, et al. Evaluation of muscles affected by myositis using magnetic resonance elastography. Muscle Nerve. 2011;43(4):585–90.
Klauser AS, De Zordo T, Feuchtner GM, Djedovic G, Weiler RB, Faschingbauer R, et al. Fusion of real-time US with CT images to guide sacroiliac joint injection in vitro and in vivo. Radiology. 2010;256(2):547–53.
Iagnocco A, Perella C, D’Agostino MA, Sabatini E, Valesini G, Conaghan PG. Magnetic resonance and ultrasonography real-time fusion imaging of the hand and wrist in osteoarthritis and rheumatoid arthritis. Rheumatology (Oxford). 2011;50(8):1409–13.
Liu J, Zhan W, Zhou M, Zhang X, Hu Y, Zhu Y. The feasibility study of US-MRI virtual navigation in the shoulder. Clin Imaging. 2012;36(6):803–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bruns, A. (2020). Advances in Pediatric Musculoskeletal Ultrasonography. In: El Miedany, Y. (eds) Pediatric Musculoskeletal Ultrasonography. Springer, Cham. https://doi.org/10.1007/978-3-030-17824-6_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-17824-6_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-17823-9
Online ISBN: 978-3-030-17824-6
eBook Packages: MedicineMedicine (R0)