Abstract
Purpose
To compare agreement between conventional B-mode ultrasound (US) and compression sonoelastography (SEL) of the common extensor tendons of the elbow with histological evaluation.
Materials and methods
Twenty-six common extensor tendons were evaluated in 17 cadavers (11 females, median age 85 years and 6 males, median age 80 years). B-mode US was graded into: Grade 1, homogeneous fibrillar pattern; grade 2, hypoechoic areas and/or calcifications <30%; and grade 3 > 30%. SEL was graded into: Grade 1 indicated blue (hardest) to green (hard); grade 2 yellow (soft); and grade 3 red (softest). B-mode US, SEL, and a combined grading score incorporating both were compared to histological findings in 76 biopsies.
Results
Histological alterations were detected in 55/76 biopsies. Both modalities showed similar results (sensitivity, specificity, and accuracy 84%, 81%, and 83% for B-mode US versus 85%, 86%, and 86% for SEL, respectively, P > 0.3). However, a combination of both resulted in significant improvement in sensitivity (96%, P < 0.02) without significant change in specificity (81%, P < 0.3), yielding an improved overall accuracy (92%).
Conclusion
Combined imaging of the extensor tendons with both modalities is superior to either modality alone for predicting the presence of pathologic findings on histology.
Key Points
• Combination of B-mode US and SEL proved efficiency in diagnosing lateral epicondylitis.
• Combination of B-mode US and SEL in lateral epicondylitis correlates to histology.
• Combination of both modalities provides improved sensitivity without loss of specificity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lateral epicondylitis (LE), a condition known as tennis elbow, is a commonly diagnosed elbow pathology with a prevalence rate of 1.3% in the general population, which is increased in manual workers and tennis players [1–6]. Overuse of the common extensor tendon is the major aetiology of LE. LE commonly presents as lateral elbow pain that is aggravated by repetitive use of the extensor muscles of the wrist during daily activities and job related functions [5–7].
Diagnosis of LE is primarily based upon clinical assessment. The role of imaging is to confirm the clinical diagnosis, to exclude other possible causes of lateral elbow pain and to determine disease severity [2, 3, 6, 8, 9].
Compression sonoelastography (SEL) is an ultrasound (US)-based imaging technique for assessing tissue elasticity. Differences in tissue stiffness can be measured by differential speckle displacement in the setting of an externally applied force [10]. Preliminary studies using SEL have demonstrated promising results in various musculoskeletal (MSK) diseases [11, 12]. Although there is good correlation between SEL and conventional US for the diagnosis of LE, the accuracy of SEL has surpassed conventional US in studies that use clinical diagnosis as the reference standard [8, 13]. To the best of our knowledge just one study has correlated B-mode US to the histological structure of the common extensor tendons just for few cases showing that the most common ultrasound appearance of lateral epicondylitis were focal hypoechoic areas in the deep part of the tendon, which were identified at surgery and corresponded histologically to collagen degeneration with fibroblastic proliferation [1]. The present study was performed to correlate B-mode US and SEL findings with histological assessment of common extensor tendon of the cadaveric elbow.
Materials and methods
Our institutional review board approved this cadaveric study, with informed consent provided according to the last wills of the donors, who had dedicated their bodies to human studies and died between November 2013 and June 2014. All cadavers were in legal custody of the anatomy department of the university.
Cadavers
We examined 26 common extensor tendons from 26 elbow joints in 17 cadavers. The study population included 11 female cadavers (median age 85 years; age range: 71–101 years) and six male cadavers (median age 80 years; age range: 70 – 88 years). All cadavers were examined within 30 h after death (median 16 h; range: 6–27.5 h) and were neither frozen nor embalmed.
We did not have information regarding prior medical and surgical history or regarding prior elbow injuries for these cadavers.
US and SEL
All examinations were performed by using a linear array transducer (18-5 MHz frequency range) (EUP-L75; Hitachi Medical Corporation, Tokyo, Japan). Optimization of transducer coupling was achieved with copious amounts of contact US gel.
For evaluation of the common extensor tendon, the cadaver was placed in supine position with adduction and internal rotation of the arm; the palm of the hand was rested on the abdomen, resulting in elbow flexion of 90 degrees. This position will put the examined tendon in a relaxed position, which is important for optimization of the examination in order to avoid tendon stress [14]. This was also in line with the recommendations of the European Society of Skeletal Radiology (ESSR). For the purpose of our study, the common extensor tendon was divided into three portions [8]: anterior, middle, and posterior portions.
B-mode US images were obtained in longitudinal planes for each portion of the common extensor tendon, and graded by one radiologist (AK) who had 15 years of experience in MSK US. We proposed a grading system as follows: grade 1 indicated a normal appearing tendon with homogeneous parallel fibrillar pattern; grade 2 indicated bulge of the tendon and/or hypoechoic areas and/or calcifications <30% of the tendon; and grade 3 indicated hypoechoic areas and/or calcifications >30% of the tendon with or without tendon thickening. Grade 1 was considered normal and grades 2 and 3 abnormal.
A second operator (MA) who had 5 years of experience with SEL performed SEL examinations immediately after the B-mode US. The second operator was blinded to the results of B-mode US. The SEL examination was performed with the technique of strain imaging, by applying gentle repetitive compression with the hand-held transducer at a rate of one compression per second with no stand-off pad. The elastogram was displayed in a rectangular region of interest (ROI) on the screen, adjusted to include the entire common extensor tendon and surrounding tissues with the subcutaneous fat and part of the radius bone. The elastogram was displayed as a translucent colour-coded real-time image superimposed on B-mode image. The colour-code corresponds to the relative tissue stiffness within the ROI; red indicated soft, blue indicated hard, and green and yellow indicated medium elasticity. The strength of compression was adjusted based upon a strain indicator on the screen according to the technique of De Zordo et al. [8].
Elastograms were constructed with the same optimal settings throughout the study as suggested by Havre et al. [10]. The US probe was held perpendicular to the tendon to minimize anisotropy.
Care was taken throughout the study to apply the same settings to all cadavers and hold the probe perpendicular to the common extensor tendon with appropriate pressure to avoid shifting. At least five successive compression-relaxation cycles were obtained to ensure reproducibility of the results. Images were saved as cine loops in the memory of the US device. Representative images were obtained from the middle of the compression-relaxation cycle for grading. Based on the grading system of De Zordo et al. [8], we proposed our grading system as follows: grade 1 indicated blue and/or green colour of tendon substance; grade 2, yellow and/or red spots <30% of tendon substance; and grade 3, yellow and/or red spots > 30% of tendon substance. Grade 1 was considered normal and grades 2 and 3 abnormal.
In addition to the independent assessments based on B-mode US and SEL, we created a combination score which was computed as the maximum of the B-mode and SEL scores. The B-mode score, the SEL score and the combined imaging score were each compared to histological findings based upon tendon biopsy.
Biopsy
Biopsy was performed in each third of the common extensor tendon under US guidance by the second examiner, who performed SEL examinations. When an abnormality was detected with B-mode US or SEL, biopsy was taken from the site of the abnormality. For any tendon third with no abnormality detected by B-mode US or SEL, a random biopsy of each tendon third was performed. The biopsy was performed by using a 14-gauge × 16-cm biopsy needle (Bard Max-Core; Bard Peripheral Vascular, Inc., Tempe, AZ, USA), which was advanced through a coaxial 13-gauge × 7.8-cm needle (Bard Tru-Guide, Bard Peripheral Vascular, Inc., Tempe, AZ, USA). The coaxial needle was used to pierce the skin and position the biopsy needle as close to the tendon as possible. The biopsy needle tip was advanced to the tendon surface, where it was fired under US guidance.
One biopsy core was obtained from each tendon third (anterior, middle, and posterior) in each of the examined common extensor tendons. We obtained 78 biopsy specimens from 78 tendon thirds; however, two of the biopsy cores were excluded from our analysis because of insufficient biopsy material.
Histological evaluation
The biopsy specimens were put into 4% formalin, incubated for 24 h and embedded in paraffin. Each specimen was cut along the long axis of the tissue sample into 7-10 um-thick slices, which were stained with haematoxylin-eosin (the standard stain). A histology specialist with 30 years of histology experience (GK), who was blinded to B-mode US and SEL findings, examined each specimen.
The following tendon alterations were considered as histopathologic signs of tendinopathy incorporated in a grading system used for histological evaluation as follows: grade 1 indicated samples without histological alterations (parallel collagen fibrils, no fatty infiltration, and no capillary proliferation); grade 2 indicated samples with mild tendinopathy (accumulation of peripheral blood mononuclear cells: lymphocytes, monocytes, and granulocytes among the fibrils, termed inflammatory infiltrate; signs of neoangiogenesis, termed capillary proliferation; inclusion of fatty vacuoles, termed fatty degeneration); and grade 3 indicated moderate or severe tendinopathy (alteration of collagen fibres with loosening of the bonds and fluid aggregation within tendons, termed loss of parallel collagen structure; and necrotic areas, termed necrosis). For statistical analysis, Grade 1 was considered normal and grades 2 and 3 as abnormal.
Statistical analysis
The concordance of US grading with histology was assessed by using κ analysis with a quadratic weighting, as well as by calculation of the equivalent intraclass correlation coefficient (Stata 12.1; StataCorp, College Station, TX, USA). The intraclass correlation with histology was calculated for B-mode US, SEL, and the combined approach. A bootstrap technique was used to estimate the standard error for each intraclass correlation coefficient, followed by a Wald test for differences among the intraclass correlation values. A P-value less than 0.05 was used to define a statistically significant result.
Sensitivity and specificity were computed with SPSS software, version 13.0 (SPSS, Chicago, IL, USA). Because B-mode, SEL, and the combined score were obtained from the same cadaver population, estimates of sensitivity and specificity were compared with a McNemar Chi square for marginal homogeneity. P < .05 was considered to indicate a statistically significant difference.
Results
The results are presented in Table 1. Histological abnormalities were detected in 72% (55/76) of all biopsies, which were distributed as follows: inflammatory infiltrate was the most commonly found (82%, 45/55), followed by capillary proliferation (47%, 26/55) and fatty degeneration (44%, 24/55). Loss of parallel collagen structure (16%, 9/55) and necrosis (2%, 1/55) were less commonly detected alterations.
The distribution of B-mode US and SEL findings are tabulated by grade of histological abnormality in Tables 2 and 3, demonstrating that each B-mode US and SEL grade increases with increasing grade of histological abnormality.
Kappa analysis demonstrated κ = 0.63 for B-mode US with histology, κ = 0.71 for SEL with histology and κ = 0.78 for the combination of B-mode US with SEL. The difference between the intraclass correlation coefficients was not significant for B-mode US and SEL. However, the intraclass correlation for the combined test was significantly better than either B-mode US (P = 0.002) or SEL (P = 0.03), suggesting that the combination of B-mode US with SEL provided the best agreement with histology.
Using histological analysis as the reference standard for all tendon thirds, the sensitivity, specificity, and accuracy of B-mode US and SEL demonstrated similar results. For B-mode US the sensitivity, specificity and accuracy were, respectively, 84% (95% CI: 72%, 91%), 81% (95% CI: 60%, 92%), and 83% (95% CI: 73%, 90%). For SEL the sensitivity, specificity and accuracy were, respectively, 85% (95% CI: 74%, 92%), 86% (95% CI: 65%, 95%), and 86% (95% CI: 76%, 92%). The combination of both imaging modalities resulted in significant improvement of sensitivity, which registered 96% (95% CI: 88%, 99%), as compared with either B-mode US (P < 0.01) or SEL (P < 0.02). There was no significant change in specificity which was 81% (95% CI: 60%, 92%). Overall accuracy was improved to 92% (95% CI: 84%, 96%) (Figs. 1, 2 and 3).
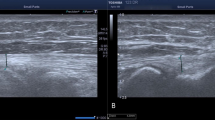
Example of normal cadaveric common extensor tendon. a, B-mode US image at anterior third of common extensor tendon insertion of right elbow in longitudinal plane. White stars = Homogeneous fibrillar pattern graded as normal appearing (grade 1). b, SEL image at same level as a. White stars = Blue-green elastogram area (grade 1) indicates hard tissue (normal), which is the site for the biopsy. According to the settings by the used machine red indicates softest structures, blue indicates hardest structures, and yellow and green indicate structures of intermediate elasticity. c, Histologic image obtained with haematoxylin and eosin stain shows parallel collagen fibrils, no fatty infiltration, and no capillary proliferation (grade 1)
Example of degenerative cadaveric common extensor tendon. a, B-mode US image at posterior third of common extensor tendon of left elbow in longitudinal plane. White X = wavy fibrillar echotexture with mucoid degeneration and loss of echogenicity (grade 2). b, SEL image at same level as a. White X = Green-yellow elastogram area (grade 2) indicates abnormal softening, where biopsy was subsequently performed. According to the settings by the used machine red indicates softest structures, blue indicates hardest structures, and yellow and green indicate structures of intermediate elasticity). c, Histologic image obtained with haematoxylin and eosin stain shows neovascularisation, alteration of the fibrillar structure with wavy outline (grade 2)
Example of degenerative cadaveric common extensor tendon. a, B-mode US image at middle third of common extensor tendon of left elbow in longitudinal plane. White X = Fatty degeneration and small hypoechoic areas (grade 2). b, SEL image at same level as a. White X = Green-Red elastogram area (grade 3) representing abnormal softening, where biopsy was subsequently performed. According to the settings by the used machine red indicates softest structures, blue indicates hardest structures, and yellow and green indicate structures of intermediate elasticity. c, Histologic image obtained with haematoxylin and eosin stain shows loss of parallel collagen structure, multiple fatty infiltrates, areas of fat necrosis, and neovascularisation (grade 3)
Discussion
Lateral epicondylitis (LE) is a common disorder characterized by lateral elbow pain and functional impairment. Microtrauma to the common extensor tendon is the main aetiology [15]. Diagnosis of LE is based on clinical assessment, with US or magnetic resonance imaging performed mainly for patients with refractory and or confounding symptoms [6, 13]. The role of imaging is either to confirm the diagnosis, to exclude other possible causes or to grade disease severity.
In a recent review of literature Latham et al. [7] reported a wide range of sensitivities (64-100%) and specificities (36–100%) for lateral epicondylitis diagnosis.
SEL as a relatively new modality is capable of determining tissue elasticity. Previous research has shown excellent reliability of SEL technique in the diagnosis of different MSK pathologies and its better performance than B-mode ultrasound in some circumstances [8, 11, 16, 17].
Several recent MSK studies suggested better results with SEL as compared with conventional B-mode US for LE diagnosis. B-mode evaluation is limited by the similarity in echogenicity between healthy normal tissues and tissues affected by degenerative disease [8, 15, 18]. De Zordo et al. [8] published a study in 2009 showing significant differences of common extensor tendon elastograms between healthy volunteers and patients with lateral epicondylitis. The reported sensitivity, specificity, and accuracy of SEL in this study were 100%, 89%, and 94%, respectively, compared to clinical examination as the gold standard for diagnosis. A semi-quantitative approach in addition to the elastogram qualitative approach was used in another study by Kocyigit et al. [15], they evaluated lateral epicondylitis by ultrasound, colour Doppler, and SEL and considered contra lateral elbows as controls. They reported significant correlation between strain ratio of the medial portion of the affected tendon and symptom duration (rho = 0.61, P = 0.010) and nocturnal pain as well (rho = 0.522, P = 0.031). Interobserver agreement was substantial for colour scales (к = 0.74, P = 0.001) and strain ratio (ICC = 0.61, P = 0.031)
To the best of our knowledge one previous study assessed the role of SEL versus B-mode US based with correlation to histology in the Achilles tendon, SEL could depict histological degeneration in 100% of Achilles tendon thirds, but B-mode ultrasound depicted it in only 86% [16].
In the current study, both conventional B-mode US and SEL showed similar results regarding the main calculated parameters (sensitivity, specificity, and accuracy) when correlated to histological findings. In concordance with the previous studies [8, 15, 18], we showed the feasibility and effectiveness of SEL in diagnosing LE of the elbow, though there was no significant difference between SEL and conventional B-mode US.
A combined test using both B-mode and SEL imaging, demonstrated improved agreement with histological degeneration (as demonstrated by kappa analysis), which was reflected by the significant increase in sensitivity.
The improved accuracy obtained by combining SEL with B-mode US suggests that SEL should be used as an adjunct tool to conventional B-mode US for evaluation of LE of the elbow, as advocated in the results of Giyoung et al. [18] and Kocyigit et al. [15].
Despite the usefulness of CDUS in diagnosing LE showing increased vascularity in symptomatic tendons [19], we could not evaluate its utility for improving the results in our study, as it was conducted on cadavers.
Our study was confronted with several additional limitations. First, we used subjective grading of SEL rather than using an objective quantification. We did not use strain ratio quantification as was done by Ahn et al. [13], nor shear wave elastography [20], which would allow elastogram quantification.
Second, differences in SEL findings may be expected between cadavers and in vivo tendons as a result of difference in vascular supply, hydration, or temperature. We investigated all cadavers as quickly as possible (and always within 30 h) after death in order to minimize post-mortem changes that might impact our results.
Third, the relatively small number of cadavers included in our study was another limitation. In order to increase our sample size, we examined both common extensor tendons whenever possible and divided each tendon into thirds with independent biopsies from each third. We recognize that although the pathology may be different in different tendons or different areas of a single tendon, the “clustered” observations from a single cadaver are not truly independent. It is for this reason that we chose to use a bootstrap method to estimate the standard error of the intraclass correlation coefficients for statistical comparison, as the bootstrap method makes no assumptions regarding the underlying variance structure of the sample. In a future study, a larger sample size that would allow truly independent observations would be preferred.
Fourth, there was a lack of medical history of involved cadavers, as we just got our study subjects from the anatomy department and we did not have any connection to their originating departments.
Fifth, each examination was done by one examiner, so we did not calculate for interrater reliability, as each cadaver examination including B-mode US and SEL, as well as biopsy took long time, which made repeated examination for each modality by second examiner not possible.
Sixth, conducting the study on cadavers may be the cause of the increased age range and mean age with inability to define the main cause of the tendon changes either degenerative tendinopathy or inflammatory changes (epicondylitis), but this was mandatory in order to be able to perform tendon biopsy.
In summary, our results confirm the results of previous studies suggesting that SEL can facilitate conventional US [8, 15, 18] in evaluating and diagnosing LE of the elbow. Combining SEL with B-mode US will improve the accuracy and robustness of LE diagnosis.
Abbreviations
- LE:
-
Lateral epicondylitis
- SEL:
-
Sonoelastography
- US:
-
Ultrasound
- MSK:
-
Musculoskeletal
- B-mode US:
-
B-mode ultrasound
- ROI:
-
Region of interest
References
Connell D, Burke F, Coombes P et al (2001) Sonographic examination of lateral epicondylitis. AJR 176:777–82
Miller TT, Shapiro MA, Schultz E, Kalish PE (2002) Comparison of sonography and MRI for diagnosing epicondylitis.JClin. Ultrasound 30:193–202
Levin D, Nazarian LN, Miller TT et al (2005) Lateral epicondylitis of the elbow: US findings. Radiology 237:230–4
Jaen-Diaz JI, Cerezo-Lopez E, Lopez-de CF et al (2010) Sonographic findings for the common extensor tendon of the elbow in the general population. J Ultrasound Med 29:1717–24
Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M (2006) Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 164:1065–74
Walz DM, Newman JS, Konin GP, Ross G (2010) Epicondylitis: pathogenesis, imaging, and treatment. Radiographics 30:167–84
Latham SK, Smith TO (2014) The diagnostic test accuracy of ultrasound for the detection of lateral epicondylitis: a systematic review and meta-analysis. Orthop Traumatol Surg Res 100:281–6
De Zordo T, Lill SR, Fink C et al (2009) Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. AJR 193:180–5
Dones VC III, Grimmer K, Thoirs K, Suarez CG, Luker J (2014) The diagnostic validity of musculoskeletal ultrasound in lateral epicondylalgia: a systematic review. BMC Med Imaging 14:10
Havre RF, Elde E, Gilja OH et al (2008) Freehand real-time elastography: impact of scanning parameters on image quality and in vitro intra- and interobserver validations. Ultrasound Med Biol 34:1638–50
Klauser AS, Miyamoto H, Bellmann-Weiler R, Feuchtner GM, Wick MC, Jaschke WR (2014) Sonoelastography: musculoskeletal applications. Radiology 272:622–33
Klauser AS, Faschingbauer R, Jaschke WR (2010) Is sonoelastography of value in assessing tendons? Semin Musculoskelet Radiol 14:323–33
Ahn KS, Kang CH, Hong SJ, Jeong WK (2014) Ultrasound elastography of lateral epicondylosis: clinical feasibility of quantitative elastographic measurements. AJR 202:1094–9
Ooi CC, Malliaras P, Schneider ME, Connell DA (2014) “Soft, hard, or just right” applications and limitations of axial-strain sonoelastography and shear-wave elastography in the assessment of tendon injuries. Skelet Radiol 43:1–12
Kocyigit F, Kuyucu E, Kocyigit A et al (2016) Association of real-time sonoelastography findings with clinical parameters in lateral epicondylitis. Rheumatol Int 36:91–100
Klauser AS, Miyamoto H, Tamegger M et al (2013) Achilles tendon assessed with sonoelastography: histologic agreement. Radiology 267:837–42
Miyamoto H, Halpern EJ, Kastlunger M et al (2014) Carpal tunnel syndrome: diagnosis by means of median nerve elasticity--improved diagnostic accuracy of US with sonoelastography. Radiology 270:481–6
Giyoung P, Dongrak K, Junghyun P (2014) Diagnostic confidence of sonoelastography as adjunct to greyscale ultrasonography in lateral elbow tendinopathy. Chin Med J 127:3110–5
Khoury V, Cardinal É (2009) “Tenomalacia”: a new sonographic sign of tendinopathy? Eur Radiol 19:144–6
Rosskopf AB, Ehrmann C, Buck FM, Gerber C, Fluck M, Pfirrmann CW (2016) Quantitative shear-wave US elastography of the supraspinatus muscle: reliability of the method and relation to tendon integrity and muscle quality. Radiology 278:465–74
Acknowledgements
The scientific guarantor of this publication is Andrea S Klauser. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was not indicated as this work was conducted on cadavers, who dedicated their bodies for research after death according to their will and they signed this consent form before death. Written informed consent was obtained from all subjects in this study. Methodology: Prospective, Diagnostic or prognostic study, Performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klauser, A.S., Pamminger, M., Halpern, E.J. et al. Extensor tendinopathy of the elbow assessed with sonoelastography: histologic correlation. Eur Radiol 27, 3460–3466 (2017). https://doi.org/10.1007/s00330-016-4711-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4711-x