Abstract
The digital workflow for surgical rehabilitation with dental implants can help prevent complications, achieve more predictable outcomes, and render implant surgery more accessible for dentists and patients alike. The digital workflow for implant surgery consists of three steps, image acquisition, virtual planning, and implant placement using surgical guides. Digital images acquired by cone beam computerized tomography (CBCT) and intraoral scanning can help recreate the patient’s condition in the computer. This information is then used to plan for optimized implant placement. The digital plan is then executed clinically with the aid of a digital surgical guide, a template that help the clinician place the implants at the exact site as planned in the computer. This chapter explains in details how implant surgery is planned and executed using a digital workflow.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The advent of dental implant therapy was one of the most important advancements in the field of dentistry in the last 40 years. Since its conception, dental implant therapy has become one of the most predictable ways to replace missing teeth. However, as a result of its increased popularity, the number of problems related to lack of proper three-dimensional positioning of the implants installed by professionals has also largely increased. To manage this issue, implant dentistry has recently seen an emergence of the digital workflow for virtual surgical planning. This includes digital impressions and models, the advent of CAD/CAM (computer-assisted design and computer-assisted manufacturing) technology, and imaging software to diagnose and plan surgeries for different dental implant systems. As a result of these developments, dental implant surgeries have become more predictable, safer, faster, and more comfortable for the patients. Digital implant impressions and image-guided surgery have revolutionized implant placement surgeries and bone graft procedures and have led to the possibility of customizing prosthetic abutments and restorations by using specific digital design computer software.
2 Radiographic Analysis
2.1 The Advent of CBCT for Dental Implant Planning
In the early days, radiographic images were used solely to perform linear measurements of the implant site and to identify vital anatomical structures that need to be avoided during implant site drilling such as the incisive canal, maxillary sinus and nasal floor in the maxillae, as well as the mandibular canal, the mental foramina, and the fossa, in the mandible. A safety margin of 1–2 mm should be left between the implant hole and these structures.
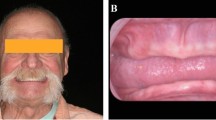
Upon its introduction to implant dentistry, the CBCT was initially used to generate images, which were printed on film or paper, for chairside assessment. Such method involved the use of schematic templates prepared by oral and maxillofacial radiologists, to show surgeons optimal implant positions on cross-sectional images. Nowadays, such templates are also available as 2D digital images (Fig. 9.1). However, this type of images does not allow navigation and true 3D analysis of entire volumes.
Basically, the CBCT scan should be used to determine the three-dimensional location of the abovementioned anatomical structures, as well as the amount of alveolar bone available. For this purpose, two linear measurements are required to be displayed in the parasagittal images (i.e., cross-sectional cuts along the alveolar ridge) for each edentulous site planned to be rehabilitated with dental implants. Such measurements are (a) the alveolar ridge height, extending from the alveolar crest to the closest anatomical structure to be avoided, used to determine implant length, and (b) the alveolar ridge buccal-lingual width, which should be done in the level planned to insert the implant body (i.e., the level where the implant platform should start). Such measurement will be used in the choice of the most appropriate diameter of the implant, considering that a minimum buccal plate width should always be left in order to prevent buccal bone resorption after implant placement.
2.2 Implant Planning Software
In contrast with printed CBCT images or JPG files, implant planning software allows for interactive 3D assessment to achieve accurate implant surgical planning (Fig. 9.2). 3D multiplanar reconstructions generated from CBCT (axial, coronal, and sagittal) may also include a curved plane (i.e., coronal panoramic images) and a series of cross-sectional images of the alveolar ridge (named parasagittal images). Although some implant planning software can read original DICOM images, most of them require conversion of the DICOM file into a specific file extension. Images from each plane are shown in different windows containing axes that indicate the location of the current images on the other planes. With such imaging setup, the surgeon is able to perform an entire 3D assessment of the implant site. Implant planning software usually include tools for virtual implant placement in the planned site within the alveolar bone. The 3D position of the implant can then be optimized and refined in both multiplanar images and 3D reconstructed models.
Implant position should always be determined according to a prosthetic rehabilitation plan developed beforehand. Currently, this can be done with a conventional workflow (i.e., using a diagnostic wax-up) or with a digital workflow (i.e., using a digital prosthetic planning performed on STL files from intraoral scanners—Fig. 9.3). At the same time, similarly to the use of printed CBCT, virtual dental implant surgical planning must take into consideration the 3D dimensions of the underlying bone, such as vertical and buccal-lingual dimensions measured in the cross-sectional images of the implant site. As a rule of thumb, bone volume should allow for a safety distance of at least 1.5 mm between implants and adjacent teeth, 3 mm between adjacent implants, and 1–2 mm between implant and buccal and lingual plates and other surrounding vital structures.
Digital diagnostic wax-up of the case depicted in Fig. 9.1 (Exocad software, DentalCAD, Darmstadt, Germany)
3 Digital Impression
3.1 Intraoral Scanning
One of the main technologies that has increased accuracy and precision of image-guided surgeries is intraoral scanning. As previously discussed in this book, the process of intraoral scanning allows for a digital impression of the patient’s dental arches. This procedure recreates a virtual 3D model of the patient’s dental arch that includes both teeth and soft tissue.
Intraoral scanners (IOS) are devices that project a light source (either laser or structured light) onto the object to be scanned in order to capture direct optical impressions of the oral cavity [1, 2]. IOS devices are composed of a computer and a handheld camera. All images captured by IOS imaging sensors are processed by a specific scanning software resulting in 3D surface models (i.e., triangulated mesh, presented as STL files).
The first dental scanner for intraoral use was introduced in the early 1980s. Today, there is a wide range of models and brands of intraoral scanners available in the market. Intraoral scanning devices such as 3M™Mobile True Definition Scanner, Carestream Dental CS3500® and CS3600®, Dental Wings® DWIO, Sirona CEREC® Omnicam, Planmeca PlanScan®, and 3Shape Trios® are among the most popular on the current world market.
In the field of digital implant dentistry, IOS can be used prior to implant placement to enable digital implant planning and image-guided surgery or after implant osseointegration to enable digital implant impression. Digital implant planning requires integration of IOS STL images with CBCT original DICOM images. Digital implant impression requires the use of implant scanbodies for transferring the 3D implant position.
Using IOS for digital optical impression has many advantages and disadvantages (see Table 9.1). The digital impression technique is more comfortable, patient friendly, and faster than conventional impressions [1, 2]. It is also a more efficient technique requiring shorter preparation and retake time, as compared with conventional implant impressions [2,3,4]. The most widely used file format by IOS devices is the open STL or STL-like locked file. The STL file format encodes only the surface geometry of a 3D object.
Dental tissues present many reflective surfaces, such as enamel or polished prosthetic surfaces, that could cause light overexposure and disrupt scanning. To prevent this issue, practitioners could change the orientation of the camera to increase light diffusion. Another strategy employed by some systems would be the use of cameras with polarizing filters [5] or applying a 20–40 μm powder coating during the digitizing process to reduce reflectivity. Theoretically, the powder thickness could vary between operators and reduce file accuracy, although the software of the IOS is capable of taking an average thickness into consideration [6]. On the other hand, the use of powder could be relatively uncomfortable for patients, and it complicates scanning when it gets contaminated with saliva [4]. Indeed, powder-free IOS are recommended for full-arch impressions to avoid the issue of maintaining powder coating on all teeth for the whole scan duration [7].
According to the ISO 5725, accuracy is assessed by two measurement methods: trueness and precision [8, 9]. Trueness refers to the closeness of agreement between the arithmetic mean after obtaining a large number of test results and the true or accepted value of reference. Precision, in turn, refers to the closeness of agreement between all test results. In this context, the trueness and precision of IOS technologies for partial impressions range between 20 and 48 μm and between 4 and 16 μm, respectively [1, 10,11,12,13,14]. Thus, current IOS devices are well adapted for clinical practice, with at least similar accuracy to conventional impression methods [7, 13, 14]. Nevertheless, intraoral scanning accuracy also depends on operator handling during execution of the procedure. In this context, more training and adherence scanning protocols can also help obtaining more accurate 3D digital models. Also, the accuracy of digital implant impressions with IOS is comparable to conventional impression for both single and multiple implant cases; however, when it comes to fully edentulous cases, the accuracy is lower and may vary across devices.
3.2 Extraoral Scanners (EOS)
Extraoral scanners are dental scanning equipments that use an optical technology similar to intraoral scanners to digitize a gypsum model obtained by a conventional impression. Such methodology can also be considered an effective alternative to conventional dental impressions [15]. Nevertheless, alterations suffered by the gypsum models obtained by the conventional impressions may interfere in the accuracy of the digital models obtained by the scanning process. When compared, intraoral and extraoral scans do not show significant differences in quality and accuracy of the digital models obtained. Therefore, intraoral scans are the preferred option to obtain digital models, since the reduced number of steps minimizes the risk of acquisition errors.
3.3 Bite and Occlusal Relationship Registration
Prosthetic rehabilitation procedures commonly require registration of the intermaxillary relationship. However, this clinical step may be complex and has been described as a common source of error due to inadequate behavior of bite registration materials. In contrast, intermaxillary registration for digital impressions using IOS only requires an additional vestibular acquisition of the occluding teeth [16]. Only one left and one right lateral occlusal registration are required [16, 17]. Such acquisitions enable alignment of images of both maxillary and mandibular arches by means of an image matching process. For this purpose, the software algorithm recognizes coincident areas positioned in multiple planes.
4 Design
Digital surgical guides are templates designed for guided drilling, which are custom-made for each patient’s prosthetic and surgical plan to ensure highly accurate drilling and implant placement [18]. This enables reliable transfer of the surgical plan from digital images to the actual surgical field, which translates to optimal implant positioning and highly predictable prosthetic outcomes. This also allows for better soft tissue management, emergence profile, and final prosthetic morphology [19]. In certain cases, implants can be loaded in the same appointment of surgical placement by using immediate loading systems such as the “Immediate Smile” or “All-on-4” protocols [20, 21].
In order to design accurate surgical guides, 3D images from STL files obtained from intraoral scanning are merged with CBCT DICOM files. The intraoral scanning and tomographic data allows for virtual planning of the prosthetic replacement and implant surgery, respectively. As a result of this process, an optimal surgical guide is created (Fig. 9.4).
4.1 Image-Guided Surgery Planning Software
In the current market, there are several different software dedicated for image-guided surgical planning. Each of them has specific strengths and weaknesses. Most of these software programs are not developed by the CBCT manufacturers, such as Simplant (Materialise Dental Inc., Glen Burnie, MD, USA), Invivo5 (Anatomage, San Jose, CA, USA), NobelClinician (Nobel Biocare, Goteborg, Sweden), OnDemand3D (Cybermed Inc., Seoul, Korea), Virtual Implant Placement software (BioHorizons, Inc., Birmingham, AL, USA), coDiagnostiX (Dental Wings Inc., Montreal, CA, USA), Blue Sky Plan (Blue Sky Bio, LLC, Grayslake, IL, USA), and Implant Studio® (3Shape, Copenhagen, Denmark), among others.
Most of these software allow access to a library of various dental implant brands and types enabling appropriate choices based on each professional’s clinical experience and preferences.
In general, there seems to be no significant differences in accuracy among the different software systems, although just a few have an integrated prosthetic module so the temporary crowns can be printed or milled at the surgical planning step.
4.2 File Superimposition and Anatomical Structure Identification
As mentioned earlier, modern implant planning software allow to merge STL files from either IOS or EOS with images from CBCT scans. In this procedure, geometries of the key structures are automatically recognized. The resulting images and files can be used to plan the implant treatment and fabricate models and surgical guides. Most software packages require advanced knowledge to benefit from the full potential of this technology.
Software systems that allow file merging such as Implant Studio® (3Shape, Copenhagen, Denmark) enable the operator to combine images either automatically or manually. The automatic algorithm depends on the software development and similar geometries structures, whereas combining manually requires the selection of similar points of reference on both files (DICOM and STL), as shown in Fig. 9.5.
Either automatic or manual superimposition method provides a color bar analysis of 3D merging accuracy. Quantitative deviation values represented by colors can also be assessed, as seen in Fig. 9.6.
An important issue is that metal artifacts on CBCT scans commonly interfere on merging quality analysis and consequently on the imaging superimposition step. In this case, manual superimposition is generally required. Figures 9.7 and 9.8 show a case with significant metal artifacts, before and after performing manual superimposition.
Different analysis methods can be applied to ensure accuracy of manual superimposition. As introduced before, color bar analysis is a visual method by which quantitative alignment accuracy information can be obtained by selecting aleatory points over the model (Figs. 9.9 and 9.10); another method for achieving superimposition accuracy is the use of transversal slice selection, by which it is possible to evaluate file merging by selecting planes of slicing on the merged 3D model, as seen in Figs. 9.11 and 9.12.
Image-guided software also have additional tools for better identifying anatomical structures such as the mandibular canal. By using panoramic, sagittal, and axial views, some software virtually reconstructs the inferior alveolar nerve (Fig. 9.13). The image-guided software will warn the professional about implants virtually placed in areas too close to the nerve (Fig. 9.14).
4.3 Virtual Prosthetic and Dental Implant Planning
The ultimate objective of placing dental implants is to support a final prosthetic restoration. In other words, patients seek teeth and not implants; thus a restorative-driven mind-set should always be maintained. The prosthetic treatment should be designed to restore esthetic, function, and occlusal stability while considering implant position and angulation.
Ideally, the implants should be placed at least 1.5 mm away from adjacent teeth, 3.0 mm away from adjacent implants, and 2.0 mm away from adjacent anatomical structures (mandibular canal, etc.); some planning software have those parameters set by default (1.5 mm radial and 2.00 mm apical distances); however they can be individualized if needed, as seen in Fig. 9.15.
Also, the implants should be placed in alignment with the occlusal forces in order to avoid eccentric loading. Since axial implant occlusal loading is desirable, 3D implant inclination should be planned taking into consideration the position of the antagonist arch, aiming for a balanced occlusion, which can be digitally assessed and planned beforehand [16, 17]. This is why the opposing arch should be included in the digital impression, either intraoral or extraoral scans.
Virtual planning software for image-guided implant surgery usually include multiple prosthodontic-related tools to create pre-designed crowns and bridges. The shape of these virtual prosthetic restorations can be edited in the computer, in order to prepare the exact design of the prosthesis intended as final restoration (Fig. 9.15). If prosthodontic-related tools are not available, an additional software dedicated exclusively to digital prosthetic planning should be used.
Ultimately, an optimal digital treatment plan should combine endosseous implant placement that respects patient’s anatomy, with prosthetic rehabilitation that is able to restore patient’s esthetics, function, and occlusal stability. Once the implant position is determined according to the prosthetic needs of the patient, the dental professional can proceed with the fabrication of a surgical guide that can transfer the digital treatment plan to the patient’s oral cavity. Such surgical guide is generally designed by the image-guided surgery software to have a shape allowing for stability in the patient’s mouth during surgery. Surgical guides are designed with metal sleeves to guide the drills during implant site preparation, ensuring implant placement in the exact region virtually planned. Such metal drills generally have the diameter of the implant to be placed or the diameter of the last drill to be used for implant site preparation. Additional metal rings can be applied for diameter reduction of the metal sleeves for using the initial thinner drills.
There are a number of different digital workflow systems for image-guided implant surgery in the market. One of them is compatible with some implant systems such as Straumann (Institut Straumann, Basel, Switzerland) and is composed of three software of the same company (Dental Wings Inc., Montreal, Canada). The first software is mainly used for working with STL files from intraoral scanning (Dental Wings Open System). The second is used for virtual implant planning (Dental Wings coDiagnostiX ®), and the third is used to communicate between the first two software (Dental Wings Synergy ®), enabling combination of STL and DICOM files, as well as visualization of the integrated treatment planning in the first two software (Fig. 9.16). Such CAD/CAM system has been validated in the literature [22]. Both virtual implant (Fig. 9.17) and prosthetic planning can be also visualized in the software dedicated to work with intraoral scanning (Fig. 9.18). This will be followed by surgical guide design and CAD/CAM fabrication (Fig. 9.19) and, finally, image-guided implant surgery (Figs. 9.20, 9.21, 9.22, and 9.23).
Visualization of both virtual implant and prosthetic planning of the case depicted in Fig. 9.4, using the software dedicated for intraoral scanning (Dental Wings Open System)
4.4 Types of Surgical Guides
Digital implant dentistry requires the combination of radiological and intraoral data in order to proceed with virtual implant planning and subsequently design the surgical guide in the form of an STL file for final manufacturing. Digital surgical guides can be divided into three categories according to the type of support they use for stabilization in the oral cavity [16, 17, 23]. First, there are tooth-supported guides, which make use of the remaining teeth to anchor the surgical guide in place; second, there are mucosa-supported guides, which get support solely on the soft tissues; and third, there are bone-supported guides, which are fixed directly into the bone. Surgical guides supported by both mucosa and bone can be stabilized with fixation pins that are inserted directly into the bone. Research has shown that both mucosa- and tooth-supported guides offer reliable accuracy, while bone-supported ones seem to be less accurate [24, 25].
5 Fabrication of Surgical Guides
After designing them virtually, digital surgical guides can be fabricated using 3D printing additive processed like rapid prototyping (RP) or subtractive manufacturing methods such as computer numerical control (CNC) machining and milling. See details underneath [24, 26].
5.1 Subtractive Manufacturing (CNC Milling Machine)
For subtractive manufacturing, the surgical guide design produced with the designing software is converted into milling strips for the CAM processing and finally loaded into the milling device [27]. This involves computation to control CNC milling, including features such as sequencing, milling tools, and tool motion direction and magnitude. Due to the anatomical variances of dental restoration, the milling machines usually have burs with different sizes. The accuracy of milling is usually within 10 μm [28, 29].
The milling machines used to prepare surgical guides have at least three axes of movement (X, Y, and Z) such the inLab (Sirona), Lava (3M ESPE), and Cercon brain (DeguDent) systems. However some more costly devices can have additional axes of movement to allow for the fabrication of more complex structures. With a five-axis milling device, in addition to the three spatial dimensions and the rotatable tension bridge (fourth axis), there is also the possibility of rotating the milling spindle (fifth axis) [28, 30, 31].
5.2 Additive Manufacturing (3D Printing Rapid Prototyping)
As explained above, 3D printing was initially set up to increase the speed of prototype manufacturing in the manufacturing industry. Recently, different types of 3D printing have been used for different applications in the fields of medicine [32] and dentistry [33, 34].
Additive 3D printing techniques include SLA, digital light projection (DLP), jet (PolyJet/ProJet) printing, and direct laser metal sintering (DLMS)/selective laser sintering (SLS).
SLA technique uses ultraviolet (UV) laser for layer-by-layer polymerization of materials. Such technique is used for manufacturing dental models from UV-sensitive liquid resins. DLP uses visible light projection for polymerization and is used for the manufacture of dental models, from visible light-sensitive resins, wax, and composite materials. After the material is printed, it is cured using a light-emitting diode lamp [35]. In addition, polymethyl methacrylate (PMMA) can also be used in the DLP technique [36]. Jet (PolyJet/ProJet) printing involves a series of ink-jet printheads and small pieces of material jetted onto support material and create each layer of the part. Next, each jetted layer is hardened by using a UV lamp or heating. This technique is used for the manufacture of dental models and for surgical drill guides. DLMS/SLS is a powder-based technique in which a high-power laser beam is used to hit the powder, resulting in melt and fusion of the powder particles. Such technique is used for the manufacture of copings, dental models, and surgical guides made from cobalt-chrome, palladium chrome, and nylon [35, 37].
5.3 Manufacturing Accuracy
Production of the fine details by milling is largely dependent on the diameter of the smallest milling bur, which usually is around 1 mm [11, 24]. On the other hand, bur diameter seems not to influence milling accuracy [38, 39]. Drilling compensation features have been found to produce small fit errors, dramatically increasing the internal gap between surgical guide and teeth or mucosa surface. Excessive cement space results in a loose fitting surgical guide that may affect the accuracy of seating, thus resulting in loss of guide retention [40].
Milling accuracy is also affected by materials properties. Excessive hardness of materials may lead to surface chipping and chattering, especially under high feed rates, high cutting speed, and deficient cooling [41, 42]. Such cutting conditions may also cause excessive vibrations and exert thermal and mechanical stresses, contributing to dimensional distortions on the workpiece, especially around thin edges [43].
Among the advantages of additive manufacturing is the production of detailed and customized workpieces that fit patient hard and/or soft tissues [32, 33]. The workpieces can be edited in regard to morphology details, sharp corners, undercuts, or voids. Such features may be also useful for manufacturing facial prostheses. Since no drilling tool is involved, no compensation feature is needed, in contrast with subtractive manufacturing. However, due to the steps of production involving sequential layering, the external surface tends to have stepped and coarse morphology [44]. Such stepping adversely affects surface texture and overall dimensional accuracy of the workpiece [44] and could be a clinical issue if the prosthesis is not polished or veneered [45, 46]. Vertical walls were minimally affected by stepping, while the corrugated or sloping surfaces are more prominently influenced [47]. Therefore, concerns have also been raised regarding the accuracy of prosthetic occlusal surfaces produced with this technique [48]. The accuracy of additive technique is dependent on layer thickness and the width of curing beam. The thinner the layers are and the narrower the curing beam is, the more accurate the final product will be. On the other hand, an increasing number of layers and reduction of beam diameter exponentially increase fabrication time [44, 49, 50].
6 Surgical Procedure
Image-guided surgeries can be performed with either flap or flapless techniques depending on the amount of keratinized tissue and on the type of surgical guide to be used (Figs. 9.21, 9.22, 9.23, and 9.24). To use a surgical template for guided surgery, a special drill kit is necessary. This kit may include a tissue punch, drill sleeves, and drills of various lengths and diameters. Such drills are compatible with specific surgical guides and dental implant manufacturers.
For a flapless approach, the first step is to remove soft tissue with a punch drill to allow access to the underlying bony crest; for the flap approach, a conventional flap is performed on the ridge. Subsequently, preparation of the implant sites is done using drills of increasing diameters. Drilling is always guided in terms of placement, angle, and depth by the surgical guide. As explained before, angle and depth control during the use of thinner drills is achieved with a series of diameter reducers positioned inside the metal sleeves. As the size of the drill increases, the diameter reducers are changed until the final diameter is reached, as determined during surgical planning.
Implant insertion and tightening can then be performed either with the implant motor or a torque wrench through the template, hence with the surgical guide in position. On completion of implant placement, the surgical guide can be removed from the oral cavity. The dentist is then able to check the depth of the implants in relation to the mucosa. X-Rays of the intraoral implants can be taken right away, and either healing screws or temporary abutments and PMMA restorations can be placed and adjusted in case of immediate loading.
7 Clinical Evidence
There are still a small number of articles in the literature comparing and addressing the accuracy of different digital workflow systems for image-guided implant surgery. Scientific evidence, however, have recently confirmed the usefulness of such methodologies for implant placement in partially edentulous patients. For such cases, implants can be placed with flapless surgery following a computer-assisted planning procedure with minimal deviation rates, as compared with the respective planned positions [51].
A systematic review of nine different computer-assisted (static) guided implant systems shows that the clinical performance of these systems achieves an implant survival rate of 97.3% after a 12-month follow-up. However, there are still no sufficient scientific evidence suggesting that computer-assisted surgery is superior to conventional procedures in terms of safety, outcomes, morbidity, or efficiency [52].
Another systematic review concluded that image-guided surgery with digital workflow leads to less self-reported pain and swelling, as compared with conventional workflow [53]. Static digital implant surgery offers higher patient satisfaction and less discomfort and complications compared to the conventional methodology. In addition, flapless digital implant surgery leads to less postoperative pain in full-arch cases than open-flap procedures. However, implants with flapless digital workflow may be placed outside the area with keratinized mucosa, which needs to be carefully assessed during treatment planning [54].
Two other recent systematic reviews verified that, although accuracy of CBCT measurements and image-guided surgery are clinically acceptable for most cases, CBCT images can be affected by patient motion and metallic artifacts [55, 56]. Since measurements can be slightly under- or overestimated, a safety margin of at least 2 mm should be always respected, when working with CBCT measurements for implant planning and CBCT-based image-guided surgery. A recent consensus report on digital technology by the International Team of Implantology (ITI) assessed the highest impact-factor reviews on differences in accuracy between conventional and digital workflow for implant surgeries [54]. The accuracy of CBCT measurements can vary across different types of software; nonetheless using a digital workflow, it is expected to have a mean 3D deviation of 1.2 mm at the implant entry point, as well as a vertical discrepancy in final implant position of up to 1.13 mm.
One of the perspectives for future research of digital implant surgery is the advent of CAD/CAM technology to create cutting and grafting guides for maxillofacial and reconstructive surgeries [57]. In addition, flapless implant surgery seems to be a viable option in cases of reconstructions with free flaps after tumor resection or gunshot trauma, despite that some complications have been reported and many challenges remain. A high degree of patient satisfaction has been reported. Nonetheless, there is still only limited research available in the literature on image-guided surgery involving bone regeneration procedures. The feasibility of retrieving onlay autogenous bone grafts with guides has been recently confirmed. However, future clinical trials would still be recommended to address the accuracy and precision of such methodology.
In conclusion, considering the current accuracy of IOS and CBCT measurements, static implant image-guided surgery should be only considered as an additional tool that can be used for comprehensive diagnosis, treatment planning, and surgical procedures.
8 Conclusions
The use of guided dental implant surgery raises concerns regarding cost- effectiveness and professional responsibility. A high initial investment and an increase in operating costs are the major challenges for the advent of a complete digital workflow in implant dentistry, especially for developing countries. Also, this novel workflow requires well-qualified personnel to manage a more sophisticated operation that otherwise would not yield the desired results. Nonetheless, despite these challenges the abovementioned technologies save time, and in full-arch implant rehabilitations, the literature shows that computer-guided implant surgery is much more accurate than freehand surgery.
Digital implant dentistry also implies a change in professional accountability. Traditionally, dental professionals can be held responsible for poor treatment outcomes cause by using inferior techniques when well-proven superior methods are available. This concept could eventually be applied to traditional and digital implantology.
Despite its already great precision, computer-assisted implant surgery seems not yet to have reached its full evolution. It is still undergoing continuous improvements, in relation to the equipment for capturing diagnostic images, the planning software, and the surgical instrument and templates used in the technique.
References
Gjelvold B, Chrcanovic BR, Korduner EK, Collin-Bagewitz I, Kisch J. Intraoral digital impression technique compared to conventional impression technique. A randomized clinical trial. J Prosthodont. 2016;25(4):282–7.
Burhardt L, Livas C, Kerdijk W, Meer WJ v d, Ren Y. Treatment comfort, time perception, and preference for conventional and digital impression techniques: a comparative study in young patients. Am J Orthod Dentofac Orthop. 2016;150(2):261–7.
Lee SJ, Gallucci GO. Digital vs. conventional implant impressions: efficiency outcomes. Clin Oral Implants Res. 2013;24(1):111–5.
Joda T, Brägger U. Patient-centered outcomes comparing digital and conventional implant impression procedures: a randomized crossover trial. Clin Oral Implants Res. 2016;27(12):e185–9.
Burgner J, Simpson AL, Fitzpatrick JM, et al. A study on the theoretical and practical accuracy of conoscopic holography-based surface measurements: toward image registration in minimally invasive surgery. Int J Med Robot. 2013;9(2):190–203.
da Costa JB, Pelogia F, Hagedorn B, Ferracane JL. Evaluation of different methods of optical impression making on the marginal gap of onlays created with CEREC 3D. Oper Dent. 2010;35(3):324–9.
Zimmermann M, Mehl A, Mörmann WH, Reich S. Intraoral scanning systems – a current overview. Int J Comput Dent. 2015;18(2):101–29.
Menditto A, Patriarca M, Magnusson B. Understanding the meaning of accuracy, trueness and precision. Accred Qual Assur. 2007;12(1):45–7.
Ender A, Mehl A. Accuracy of complete-arch dental impressions: a new method of measuring trueness and precision. J Prosthet Dent. 2013;109(2):121–8.
Vecsei B, Joós-Kovács G, Borbély J, Hermann P. Comparison of the accuracy of direct and indirect three-dimensional digitizing processes for CAD/CAM systems – an in vitro study. J Prosthodont Res. 2017;61(2):177–84.
Jacob HB, Wyatt GD, Buschang PH. Reliability and validity of intraoral and extraoral scanners. Prog Orthod. 2015;16:38.
Ender A, Attin T, Mehl A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent. 2016;115(3):313–20.
Ahlholm P, Sipilä K, Vallittu P, Jakonen M, Kotiranta U. Digital versus conventional impressions in fixed prosthodontics: a review. J Prosthodont. 2016;27:35–41.
Ting-Shu S, Jian S. Intraoral digital impression technique: a review. J Prosthodont. 2015;24(4):313–21.
Atia MA, El-Gheriani AA, Ferguson DJ. Validity of 3 shape scanner techniques: a comparison with the actual plaster study casts. Biom Biostat Int J. 2015;2(2):00026. https://doi.org/10.15406/bbij.2015.02.00026.
Solaberrieta E, Garmendia A, Brizuela A, Otegi JR, Pradies G, Szentpétery A. Intraoral digital impressions for virtual occlusal records: section quantity and dimensions. Biomed Res Int. 2016;2016:7.
Solaberrieta E, Arias A, Brizuela A, Garikano X, Pradies G. Determining the requirements, section quantity, and dimension of the virtual occlusal record. J Prosthet Dent. 2016;115(1):52–6.
Guerrero ME, Jacobs R, Loubele M, et al. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig. 2006;10(1):1–7.
van Steenberghe D, Naert I, Andersson M, et al. A custom template and definitive prosthesis allowing immediate implant loading in the maxilla: a clinical report. Int J Oral Maxillofac Implants. 2002;17(5):663–70.
Johansson BR, Friberg B, Nilson H. Digitally planned, immediately loaded dental implants with prefabricated prostheses in the reconstruction of edentulous maxillae: a 1-year prospective, multicenter study. Clin Implant Dent Relat Res. 2009;11(3):194–200.
Cassetta M. Accuracy of a computer-aided implant surgical technique. Int J Periodontics Restorative Dent. 2013;33(3):317–25.
Sannino G, Gloria F, Schiavetti R, Ottria L, Barlattani A. Dental wings CAD/CAM system precision: an internal and marginal fit sperimental analisys. Oral Implantol. 2009;2(3):11–20.
Ritter L, Reiz SD, Rothamel D, et al. Registration accuracy of three-dimensional surface and cone beam computed tomography data for virtual implant planning. Clin Oral Implants Res. 2012;23(4):447–52.
Di Giacomo GA, Cury PR, de Araujo NS, Sendyk WR, Sendyk CL. Clinical application of stereolithographic surgical guides for implant placement: preliminary results. J Periodontol. 2005;76:503–7.
Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, Morimoto S, Sesma N, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(5):602–12.
Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18:571–7.
Andersson M, Carlsson L, Persson M, Bergmann B. Accuracy of machine milling and spark erosion with a CAD/CAM system. J Prosthet Dent. 1996;76(2):187–93.
Rekow ED, Erdman AG, Riley DR, Klamecki B. CAD/CAM for dental restorations—some of the curious challenges. IEEE Trans Biomed Eng. 1991;38(4):314–8.
Abduo J, Lyons K, Bennamoun M. Trends in computer-aided manufacturing in prosthodontics: a review of the available streams. Int J Dent. 2014;2014:783948.
Beuer F, Schweiger J, Edelhoff D. Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J. 2008;204(9):505–11.
Kanazawa M, Inokoshi M, Minakuchi S, Ohbayashi N. Trial of a CAD/CAM system for fabricating complete dentures. Dent Mater J. 2011;30(1):93–6.
Webb PA. A review of rapid prototyping (RP) techniques in the medical and biomedical sector. J Med Eng Technol. 2000;24(4):149–53.
Davis BK. The role of technology in facial prosthetics. Curr Opin Otolaryngol Head Neck Surg. 2010;18(4):332–40.
Van Noort R. The future of dental devices is digital. Dent Mater. 2012;28(1):3–12.
Hazeveld A, Huddleston Slater JJ, Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am J Orthod Dentofac Orthop. 2014;145:108–15.
Brkic B, France N, Clare AT, Sutcliffe CJ, Chalker PR, Taylor S. Development of quadrupole mass spectrometers using rapid prototyping technology. J Am Soc Mass Spectrom. 2009;20:1359–65.
Örtorp A, Jönsson D, Mouhsen A, Vult von Steyern P. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011;27(4):356–63.
Bornemann G, Lemelson S, Luthardt R. Innovative method for the analysis of the internal 3D fitting accuracy of Cerec-3 crowns. Int J Comput Dent. 2002;5(2–3):177–82.
Tinschert J, Natt G, Hassenpflug S, Spiekermann H. Status of current CAD/CAM technology in dental medicine. Int J Comput Dent. 2004;7(1):25–45.
Wassell RW, Barker D, Steele JG. Crowns and other extra-coronal restorations: try-in and cementation of crowns. Br Dent J. 2002;193(1):17–20.
Ezugwu EO, Bonney J, Yamane Y. An overview of the machinability of aeroengine alloys. J Mater Process Technol. 2003;134(2):233–53.
Abele E, Frohlich B. High speed milling of titanium alloys. Adv Prod Eng Manag. 2008;3(3):131–40.
Terminasov YS, Yakhontov AG. Distortion of lattice structure of metals by grinding. Metal Sci Heat Treat Metals. 1959;1(5):19–23.
Choi SH, Chan AMM. A virtual prototyping system for rapid product development. Comput Aided Design. 2004;36(5):401–12.
Williams RJ, Bibb R, Eggbeer D, Collis J. Use of CAD/CAM technology to fabricate a removable partial denture framework. J Prosthet Dent. 2006;96(2):96–9.
Williams RJ, Bibb R, Rafik T. A technique for fabricating patterns for removable partial denture frameworks using digitized casts and electronic surveying. J Prosthet Dent. 2004;91(1):85–8.
Vandenbroucke B, Kruth JP. Selective laser melting of biocompatible metals for rapid manufacturing of medical parts. Rapid Prototyp J. 2007;13(4):196–203.
Silva NRFA, Witek L, Coelho PG, Thompson VP, Rekow ED, Smay J. Additive CAD/CAM process for dental prostheses. J Prosthodont. 2011;20(2):93–6.
Kathuria P. Microstructuring by selective laser sintering of metallic powder. Surf Coat Technol. 1999;116–119:643–7.
Khaing MW, Fuh JYH, Lu L. Direct metal laser sintering for rapid tooling: processing and characterisation of EOS parts. J Mater Process Technol. 2001;113(1–3):269–72.
Van Assche N, van Steenberghe D, Quirynen M, Jacobs R. Accuracy assessment of computer-assisted flapless implant placement in partial edentulism. J Clin Periodontol. 2010;37:398–403.
Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2014;29(SUPPL):25–42.
Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health. 2017;17(1):150.
Wismeijer D, Joda T, Flügge T, Fokas G, Tahmaseb A, Bechelli D, et al. Group 5 ITI consensus report: digital technologies. Clin Oral Implants Res. 2018;29(Suppl 16):436–42.
Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C. The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):416–35.
Fokas G, Vaughn VM, Scarfe WC, Bornstein MM. Accuracy of linear measurements on CBCT images related to presurgical implant treatment planning: a systematic review. Clin Oral Implants Res. 2018;29(Suppl 16):393–415.
Numajiri T, Morita D, Nakamura H, Tsujiko S, Yamochi R, Sowa Y, Toyoda K, Tsujikawa T, Arai A, Yasuda M, Hirano S. Using an In-house approach to computer-assisted design and computer-aided manufacturing reconstruction of the maxilla. J Oral Maxillofac Surg. 2018;76:1361–9.
Acknowledgments
The authors thank the radiology centers CIRO and Doc Digital (Sao Paulo, Brazil), as well as Dr. Mauricio P.G. da Costa, for their support in this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cortes, A.R.G., Baptista, O.H.P., Zambrana, N.R.M. (2019). Digital Implant Surgery. In: Tamimi, F., Hirayama, H. (eds) Digital Restorative Dentistry . Springer, Cham. https://doi.org/10.1007/978-3-030-15974-0_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-15974-0_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15973-3
Online ISBN: 978-3-030-15974-0
eBook Packages: MedicineMedicine (R0)