Abstract
Information technology (IT) becomes crucial part of the healthcare system and it is getting more attention worldwide. Health IT includes well-known systems that have transformed the health sector, such as electronic health records (EHRs), electronic medical records (EMRs), and electronic personal health records (ePHRs). ePHR aims at enabling patients to take more active role in their care by providing them with a tool to access their health records in a secure and safe environment. The ePHR allows greater patient-provider engagement. The provider’s adoption rate of the ePHR as a tool to connect with patients and to enable them to have access to their records is increasing at an accelerated rate. However, the patient’s ePHR adoption rate remains low. In the United States, the number of office-based physicians adopting EHR increased from 17% in 2008 to 58% as of 2015. Similarly, the non-federal acute care hospitals with certified EHR rate increased from 9% in 2008 to 84% as of 2015 [1]. Despite the efforts to encourage the health care provider’s adoption of certified EHR and ePHR, the adoption rate by patients remains below expectations [2]. The goal of this report is to investigate the key factors influencing the adoption and use of the ePHR in order to understand the patients’ intentions of the adoption and use of such a technology. More attention is needed to improve the patient’s adoption of ePHR. The factors influencing the adoption and use of the ePHR for health management are grouped into six themes. These themes include performance factors, effort factors, social factors, facilitating conditions, perceived credibility, health factors, and computer factors. The themes involve essential factors that influence the adoption and use, such as perceived usefulness, perceived ease of use, portal features, subjective norms, computer and internet availability, computer literacy, computer anxiety, privacy and security, health literacy, satisfaction with medical care, and provider’s support.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others

1 Introduction
Information technology (IT) becomes crucial part of the healthcare system and it is getting more attention worldwide. Health IT includes well-known systems that have transformed the health sector, such as electronic health records (EHRs), electronic medical records (EMRs), and electronic personal health records (ePHRs). ePHR aims at enabling patients to take more active role in their care by providing them with a tool to access their health records in a secure and safe environment. The ePHR allows greater patient-provider engagement. The provider’s adoption rate of the ePHR as a tool to connect with patients and to enable them to have access to their records is increasing at an accelerated rate. However, the patient’s ePHR adoption rate remains low. In the United States, the number of office-based physicians adopting EHR increased from 17% in 2008 to 58% as of 2015. Similarly, the non-federal acute care hospitals with certified EHR rate increased from 9% in 2008 to 84% as of 2015 [1]. Despite the efforts to encourage the health care provider’s adoption of certified EHR and ePHR, the adoption rate by patients remains below expectations [2]. The goal of this report is to investigate the key factors influencing the adoption and use of the ePHR in order to understand the patients’ intentions of the adoption and use of such a technology. More attention is needed to improve the patient’s adoption of ePHR. The factors influencing the adoption and use of the ePHR for health management are grouped into six themes. These themes include performance factors, effort factors, social factors, facilitating conditions, perceived credibility, health factors, and computer factors. The themes involve essential factors that influence the adoption and use, such as perceived usefulness, perceived ease of use, portal features, subjective norms, computer and internet availability, computer literacy, computer anxiety, privacy and security, health literacy, satisfaction with medical care, and provider’s support.
2 Factor Influencing the Patient’s Adoption of ePHR
There several key factors play an essential role in the ePHR adoption. This section will address the most key factors influencing patient’s adoption of ePHR such as health literacy, usability, computer literacy, health information exchange (HIE) and interoperability, health care provider’s support, ePHR features, patient characteristics, and health conditions. At the end of the report, a taxonomy of the factors is developed, and the essential factors are grouped in themes.
2.1 Health Literacy
The explosion of the internet and the massive amount of information available on the web have become a source for individuals to look up passively for health information. The available information on the web requires consumers to have the skills to search and evaluate the quality of the existing information related to their health in order to facilitate their health-related decisions.
Patient’s health literacy is another factor that may prevent patients from taking full advantage of the ePHR. Patients may not have the interest to adopt and use a system that they find difficult to understand the information it consists of. Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [3]. The low health literacy can add a financial burden on the healthcare systems. Vernon et al. [4] studied the health literacy implications on the national policy. They stated that low health literacy costs the U.S. health care system and economy between $106 billion and $238 billion annually. Studies show that about one-half of American adults are shown to have low health literacy which would negatively impact their interest in the health information technology (HIT) adoption [5]. Health literacy also can be defined in terms of information technology as “the ability to read, use computers, search for information, understand health information, and put it into context” [6]. These two definitions emphasize the combination of the health information understanding and the information technology associated commands.
Mackert et al. [5] conducted a study to investigate the relationship between the health literacy and the adoption and use of HIT tools like fitness and nutrition apps, activity trackers, and patient portals. The study investigated the ease of use and usefulness of these tools as well as the perceived privacy and trust. The results show a positive relationship between the health literacy and the adoption and use of HIT tools. Also, greater health literacy revealed greater perceived ease of use and usefulness of the HIT tools. In terms of privacy, a negative association is found between the health literacy and privacy perception toward HIT tools. The health literacy has a positive association with trust in healthcare but a negative association with trust in government [5].
Briones conducted a study [7] to examine how young adults evaluate the health information available on the web and how they ensure its credibility. Fifty face-to-face in-depth interviews were conducted to gather the views of the young adults, then, analyzed using techniques from the grounded theory approach. The findings suggest that young adults find online sources of health information to be an acceptable channel. Young adults perceive the social media sites as networking channels rather than a credible source of health information.
To measure the electronic health literacy, Norman and Skinner have developed a reliable tool called eHealth Literacy Scale (eHEALS) to assess the patients’ knowledge, comfort, and perceived skills in utilizing the information technology for the health issues [6]. The eHEALS tool has been widely adopted and used to measure the eHealth literacy.
A study utilized “eHEALS” tool found out that patient’s health literacy is a key factor in the patient willingness and interest to adopt ePHR [8]. It showed that 65% of the patients performed well in the health literacy scale which resulted in higher interest in the ePHR adoption [8]. Health literacy is influenced by various factors such as education level, income, and age [8]. It is found that people with less education and have a low income are shown to be less likely to look up health-related information online [9]. Heuristic evaluation and usability testing are two assessment tools that can be used with an added focus to detect health literacy issues from the patient portal [10]. Low health literacy influences the patient perceptions toward the value of the ePHR as well [11]. Oppositely, Cortelyou-Ward et al. [12] examined the patient engagement and patient-provider communication resulting from the use of ePHR to increase the patient health literacy which in return will improve the patient satisfaction and outcomes. They suggest the importance of considering the ePHR as a tool that improves the patient health literacy and education. The health literacy positively influences the adoption of ePHR. Health literacy plays a key role in the adoption of the ePHR. The level of health literacy demands on the patients and healthcare providers are deemed to be equally important in the ePHR adoption [13].
Validated translated into different languages versions of the eHEALS scale have been developed. These versions such as Dutch [14], Japanese [15], and Persian [16] versions developed to measure the health literacy of different nations and the tool has proved its reliability in measuring the eHealth literacy. A study [14] conducted in examine the validity of a Dutch translation of the eHEALS scales in two populations. The eHEALS was assessed and the results showed the high reliability as the internal consistency of the scale was high. Mitsutake et al. conducted a study [15] to test the validity and reliability of a Japanese version of the eHEALS (J-eHEALS) scales. The study as well aims at examining the relationship between the eHealth literacy and the demographic attributes. Internet-based cross-sectional survey was used to capture the responses of 3000 Japanese adults. The findings confirm the J-eHEALS as a highly validated and reliable scale. Dashti et al. conducted a study [17] to evaluate the level of e-Health literacy of Medicine and Health Sciences University students in Iran. The study utilized the e-Health literacy scale (eHEALS) but with a validated Persian translated version (P-EHEALS). The findings show that there is a low level of e-Health literacy among Medical and Health Sciences University students in Mashhad, Iran.
A study [18] used the eHealth Literacy Scale (eHEALS) to provide a better understanding of the eHealth literacy among college students and their health behaviors. It aims as well to understand their use of online resources to maintain their health. The results of surveying 422 college students revealed that eHealth Literacy Scale (eHEALS) showed a significant association for students’ current and future maintenance of health and use of online health resources.
Petrič et al. provided an extension of the eHealth Literacy Scale (eHEALS) to better understand the different types of online health communities (OHC) users [19]. The study was based on a cross-sectional web survey on a representative sample size of 644 users of the OHC. The extended eHEALS scale presented six dimensions: awareness of sources, recognizing quality and meaning, understanding information, perceived efficiency, validating information, and being smart on the net with the awareness of the various online sources being the most developed and the understanding information being the least developed dimension. The study identified four types of OHC users: active help-seekers, lurkers, core relational users, and low-engaged users. The findings showed statistically significant differences among the four user types across the six dimensions. The active help-seekers users are shown to have strong eHealth literacy skills and the ability to filter through online information [19].
Another method developed to explore health literacy is the Rapid Estimate of Adult Literacy in Medicine. A study was conducted in Mashhad, Iran [16] to examine women’s health literacy using cross-sectional approach. The study used a translated to Persian version of the Rapid Estimate of Adult Literacy in Medicine. The results of the study show that younger women have low health literacy than older women. The education level appeared to be a key determinant of the level of women’s health literacy. The study shows a positive correlation between health literacy and both age and education.
2.2 Usability
The ePHR portal usability is an essential factor in the adoption. The usability of the ePHR portal includes the ability of the patient to navigate through the website smoothly, learn and use the portal easily, find information easily and quickly, spend short time completing the task, make minimal errors, and prefer the portal to search for health-related information over other websites [20]. There are some barriers of use that have been noted such as the ability to use and access to computers and internet for some people especially [21] older adults.
Ease of use has been an essential construct of many models that examine technology acceptance and use such as technology acceptance model (TAM) and unified theory of acceptance and use of technology (UTAUT). A study used protection motivation theory (PMT) & UTAUT models to examine the patients’ intentions to adopt ePHR showed the factor perceived ease-of-use as significant factors in influencing the use of PHR [22]. A study of the physicians “acceptance of PHR using UTAUT model suggested that Performance Expectancy is the most significant factor affecting physicians‘ acceptance of PHR [23]. The Diffusion of Innovation Model was applied to test the patients” perceptions of the ePHR found that ease of use, relative advantage, and trialability best predictors of the ePHR value [24]. Another study examined the patient’s adoption of the ePHR using UTAUT revealed that performance expectancy and effort expectancy are the drivers of the ePHR adoption [25].
Usability evaluation on the health IT context can be a complex and costly process and depends on various factors such as number end-users or patients in the case ePHR, the patient portal, and the process of the evaluation itself [26]. Usability of the patient portal or ePHR can be measured through heuristic evaluation or usability testing [10]. Heuristic evaluation is one assessment tool for ePHR that is conducted at low-cost and has proved its success in identifying the challenges to use of such a system [26]. Heuristic evaluation depends on the specialists who evaluate and examine the portal to detect and note any usability issues that may influence the usability of it [10]. On the other hand, usability testing depends on the patients interacting with portal while the specialists observe the patients interaction, and analyze and record any issues that the patients face [10]. Human-centered design method evolves around the patients and allows them to shape the design of the end version of the portal and improve its usability [20]. In this method, participant patients are asked to perform certain scenarios in the patient portal and think aloud as they proceed. They also complete surveys and conduct interviews thereafter. The results then analyzed to present design improvements [20].
A study conducted to evaluate usability and usefulness of ePHR for older adults analyzed four components of the ePHR which are tasks, users, representations, and functions [27]. It found out that the tasks were easy for the patients to learn and apply even though the performance time appeared to be slow [27]. University of Victoria’s eHealth Observatory has evaluated the Personal Health Portal (PHP) of Alberta Health facility in Canada focusing on the pre-design, design, and adoption assessment using persona-based usability inspection combined with usability testing sessions. The study focused on the early usability assessment of the PHR application and found out that there is a great opportunity for improvement that can add tremendous value to users in different areas of the PHR information architecture, content, and presentation [28]. Overall, it is important to consider the patients in the process of designing the ePHR. Failure to do so may lead to human errors and difficulty to use which would lead to unsatisfied patients that may result in abandoning the system and slow rate of adoption.
2.3 Health Information Exchange (HIE) and Interoperability
Both health information exchange (HIE) and interoperability involve the transfer of information either from one health care provider or system to another. They pose a crucial role in the adoption and acceptance of the ePHR since they help in providing a full picture of the patient health record. It is important to mention and understand the difference between the HIE and interoperability as they involve the transfer of patient health information.
2.3.1 Health Information Exchange (HIE)
The HIE is perceived to have two definitions: one as a verb and a second as a noun. Healthcare Information and Management Systems Society (HIMSS) defines the verb HIE as “the sharing action between two or more non-affiliated organizations with an executed business/legal arrangement that have deployed commonly agreed-upon technology with applied standards for the purpose of electronically exchanging health-related data between the organizations” and the noun form of the HIE as “a catch-all phrase for the health information exchange organizations (HIOs) providing data exchange under the legal arrangements” [29]. It is important to mention the regional health information organization (RHIO) as an important element in the health information exchange process which is defined as “a type of health information exchange organization (HIO) that brings together health care stakeholders within a defined geographic area and governs health information exchange among them for the purpose of improving health and care in that community” [30]. Based on the HealthIT.gov, HIE “allows doctors, nurses, pharmacists, other health care providers and patients to appropriately access and securely share a patient’s vital medical information electronically—improving the speed, quality, safety and cost of patient care” [31]. The HIE aims at achieving the goals of improving healthcare quality, enhanced workflow efficiency, and reduced cost [32]. Efficiency improvement includes being able to access test/lab results from other providers and improve the efficiency of the office administration workload regarding handling referrals and claims processing [32]. The concerns related to HIE may include technical and organizational ability of the health provider, privacy and security, and cost concern [32]. There are three forms of HIE: direct exchange, query-based exchange, and consumer-mediated exchange [31]. The Office of National Coordinator (ONC) works toward supporting governance initiatives of nationwide HIE to: enhance interoperability, reduce the cost of information exchange, and increase trust among participant involved in the HIE process [33]. There have been many studies that have examined the ePHR and HIE. Patients and health providers express an interest in using ePHR for the purpose of accessing, sharing, and exchanging vital health information such as medical history and medication list which would not be possible without the HIE existence [34]. Another study examined the patient’s perceptions and attitudes toward PHR and HIE use by their health provides [35]. The study showed a great patient’s interest in ePHR and to access their health information and concluded by emphasizing the importance of addressing the issues related to privacy and security as part of HIE process. Patel et al. [36] examined the patient’s support for HIE and PHR and concluded that patients support the physicians’ use of HIE. It emphasized the importance of demonstrating the benefits of HIE to the underserved population in order to achieve a higher rate of HIE acceptance and support [36]. The HIE is an essential element of the ePHR success as it allows the exchange of patient health information across different health care providers for the purpose of supporting and providing better healthcare service.
2.3.2 Interoperability
The interoperability between the systems that deal with ePHR is an essential success factor for ePHR adoption. Healthcare Information and Management Systems Society (HIMSS) defines interoperability as “the extent to which systems and devices can exchange data, and interpret that shared data” [37]. Department of Health and Human Services (HHS) and ONC annual progress reports submitted to the U.S. Congress stated the importance of building interoperable health systems [38]. The tethered ePHR is built upon the successful interoperability between the EHR and the ePHR portal.
Archer et al. [39] conducted a literature review on the ePHR. They suggest that having a functional ePHR relies on the existence of unified technical standards for the system interoperability [39, 40]. Interoperability is considered as a key factor in the successful ePHR adoption [40]. The standards of building interoperable ePHR include security and privacy standards, adoption and use of certified HIT solutions, and data interchange standards [39].
In order to build interoperable health system, HHS highlights the key priorities to provide seamless and secure flow of health information that includes propose standards to enable the seamless and secure exchange of health information, build business case for interoperability, and change the culture around access to health information. The activities involved in building the business case for interoperability in order to better assist the smooth information flow include moving toward value-based care, supporting health care providers utilizing Health IT by providing technical assistance and sufficient guidance and resources, and CMS funding to foster the electronic health information flow [38]. The ONC aims at changing the culture around access to health information by supporting the rights of patients to access their health information, efforts to discourage information blocking, and encouraging transparency as indicated in the annual report. It also emphasizes the interoperability commitments to ensure proper consumer access, transparency, and electronic health information standards implementation [38].
HIMSS has formed a group of HIE and interoperability experts to prepare a comprehensive business case for the adoption of HIE and interoperability. The group has identified some challenges and barriers to HIE, and interoperability adoption [29]. The cost associated with having such systems may include hardware, software, implementation and ongoing training, maintenance, and staffing [29]. Also, barriers identified in the report include lab data transmission standards, privacy and security, long-term care/behavioral health, semantic and syntactic interoperability, and competing and conflicting document standards. The existence and success of HIE and interoperability in the health care system allow for the successful exchange of essential health information and in return improve the chance of other systems such as EHR and ePHR success. The document as well presents the benefits of successful implementation of HIE attained by hospitals, physicians, patients and health information organizations such as improved and efficient workflow, faster and easier access to various health information, better decision making by having necessary data in hand, more patient’s involvement in their care, and reduction in healthcare costs. The utilization of HIE and better interoperable systems resulted in, as per pilot study presented in the report 53% drop in non-urgent visits to ER, 68% an increase in primary care visits, and cost saving of between two and four million dollars over a period of 6 months.
2.4 Computer-Related Factors
Patient’s ability and knowledge to utilize computer have considerable influence on the adoption of health technologies. These factors include computer literacy, access to computer and internet, internet reliance required by certain technologies such as ePHR, computer self-efficacy, computer anxiety, and personal IT innovativeness. Computer literacy requires the ability to have access to the computer and use it to solve a problem or accomplish certain task [41]. Computer literacy contributes to the ability of the patients to effectively adopt and use the ePHR [42]. The technology related factors are essential in the adoption process of the ePHR.
The relationship between the patient’s computer knowledge and the adoption of the HIT has been investigated by many researchers. Saranto and Leino-Kilpi examined computer literacy in nursing [43]. They used a three-round Delphi survey to extract knowledge from experts. The results showed that nurses are required to have computer knowledge and skills especially in accessing and using the hospital information system as well as be aware of the computer security threats and implications [43].
Computer availability and literacy are among the top barriers facing the adoption of ePHR. Computer-related barriers that limit the utilization of the ePHR include the patient’s lack of computers and nurses’ negative attitudes regarding computer usage [44]. In a study examining the barriers to the use of ePHR by an elderly population, computer literacy, and computer anxiety were ranked as the top major barriers in using ePHR by elderly population [45].
Cocosila and Archer empirically investigated the patients’ perceptions on the adoption of ePHR [46]. The study examined factors to predict the intention to adopt ePHR that include: internet reliance, computer self-efficacy, personal IT innovativeness, security and privacy and trust, anxiety, and perceived usefulness. The findings showed that personal IT innovativeness and perceived usefulness are the top factors influencing ePHR adoption. The findings as well showed a positive impact on the adoption by the following factors: internet reliance, security and privacy, and trust constructs. The access to the internet and computer literacy are presenting the digital divide concept.
The term “Digital Divide” has emerged to describe the access to computer by people. The digital divide is defined as “the gap that exists among individuals and communities with regards to the ‘haves’ and ‘have-nots’ of information and modern communications technologies” [47]. Digital divide represents the “disparities among subgroups based on access to the Internet and computer literacy” [48]. Digital divide is shown to be a problem facing the ePHR adoption and use [49]. The Pew Research Center’s estimates an increase in the number of people accessing the internet. Eighty-nine percent of U.S. adults in 2018 are estimated to have accessed the internet in comparison with 74% a decade ago [50].
Different technology adoption models have considered the computer-related factors to measure and predict the ePHR adoption. The task-technology fit (TTF) model studies how technology support people accomplish tasks by examining the technology characteristics, task characteristic, task-technology fit, performance impact, and utilization [51]. One of the unified theory of acceptance and use of technology model four constructs, facilitating conditions examined the degree to which an individual believes that resources and technical infrastructure exists to support the use of the ePHR [52].
In the context of health IT, computer literacy has generated and new concept call eHealth literacy. Ehealth literacy is a concept that has been developed to combine the computer literacy and health literacy. It is defined with regards to the patients as “ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” [41]. It is also shown that there is a positive relationship between health literacy and use of internet-based technologies [9].
2.5 Health Care Provider’s Support
The support and encouragement of the health care providers, physicians, nurses, and hospital administrators to the patient’s adoption of the ePHR are crucial. A study about the patient portal and patient engagement showed the importance of the provider’s acceptance and promotion of the ePHR [48]. Studies show that there is an increasing attention from the clinical staff in educating and supporting patient to use and access the patient portals [53].
Nazi conducted a study using in-depth interviews with 30 VA health care professionals who are engaged in providing direct patient care to examine the health care professionals’ perspectives toward the ePHR in organizational and clinical settings [54]. The author believes that the current efforts focus on the patients’ adoption of ePHR as a tool for them to take more control over their health, and was designed as patient-oriented tools without taking into consideration the role of the social and organizational context of health care delivery. It is believed that the nature of the patient engagement is a reciprocal process. The study presented various factors such as adequate education and training opportunities that facilitate the health care professionals’ endorsement of the patient adoption and use of the ePHR as this endorsement has been limited. The provider’s endorsement is a continuous process that starts from influencing the patient’s decision to adopt ePHR to the engagement and continuous adoption to reach positive outcome. The study shows that health care professionals are shown to have a limited view of the patient adoption, and use of various ePHR functions such as access to the health education materials and track their health history reports. The health care professionals have the perceptions and concerns that the patients fear that their entered data in the ePHR could be viewed by the health care team. One of the main reasons of the insufficient endorsement by health care professionals is the lack of integration between the ePHR (My HealtheVet) and the Veterans Affair’s electronic health record (VA-EHR). The study highlights the importance of the health care professionals’ endorsement of ePHRs to patients and in the engagement along the way. Also, the study emphasizes the importance of the patients’ and physicians’ utilization of the ePHR tools together as partners.
Nurses play a key role in the ePHR introduction to the patients and as a promotion role model. A study examined the intentions of nurses to adopt patient’s ePHR [55] suggests that subjective norms had the most significant influence on the attitudes and intentions of nurses to use e PHRs as they are influenced by their peers. It emphasizes the importance of nurse’s contribution to the development and promotion of the ePHR as well. Nurses can add insight into the development and revisions of the ePHR [11].
On the other hand, patients trust their physicians and are willing to follow their advice to adopt and use ePHR if they recommend it to them [46]. Vydra et al. [56] emphasized the importance of the physician endorsement for the ePHR to gain widespread diffusion. They highlighted the significance of rewarding the employee using ePHR the most, providing financial reimbursement for workload resulted from the time spent on the ePHR communicating with the patients, and providing more ePHR educational materials. Satisfaction with healthcare provider and the current medical care improve the chances of the patient adopting and using their provider’s ePHR [46].
The ownership of the ePHR software appears to matter to the patients. A study conducted to investigate the patient’s and physician’s willingness and interest to adopt and use ePHR in the emergency department [57]. The study showed that patients prefer the hospitals as the source of the ePHR and to control their health information rather than any other entities such as the software companies, the government, and insurance company.
The healthcare entities should put more efforts in promoting the adoption and use of ePHR among patients. Wells et al. conducted a study to examine the organizational strategies of the health care providers who had implemented PHRs for at least 12 months to promote PHR adoption using semi-structured interviews and a web-based survey [58]. The study identified the health professional encouragement and endorsement as the most effective strategy to promote the ePHR and improve the patient acceptance. Also, raising patient awareness of the ePHR existence and benefits, and the provider acceptance are among the main organizational strategies to promote ePHR. The study summarizes the main providers’ strategies as the organizational vision actively communicated, clear governance and policies, enforce work process redesign, staff training, information technology (IT) support, and monitoring and incentives. Another study suggests that in order to promote the adoption of ePHR, policymakers should provide sufficient assistant in the forms of financial support, interoperability, and training of information technology support staff [59]. It is obvious that the role of health care providers, physicians, and nurses on promoting the ePHR adoption and use is an important success factor toward the widespread of the ePHR adoption.
One of the main goals of the “Meaningful Use” initiative released by the Office of National Coordinator (ONC) is to engage the patients and health care providers. For the health care providers to be eligible for the meaningful use incentives, they should meet certain criteria that influence the patient’s adoption and use of the ePHR. As part of the meaningful use Stage 1, the healthcare provider must provide the patients with the ability to view, download, and transmit their health information [60]. Also, the meaningful use Stage 2 requires that 5% of the healthcare providers patients’ population use secure e-messaging in order to qualify for the meaningful use Stage 2 incentives which require direct interaction between the patient and the health care provider [61]. Giving the patients the ability to access their information is measured as the following: more than 50% of the patients are to be given online access to their records which are mostly provided during the doctor visit for the first time [60].
Health care providers, physicians, and nurses may have positive and negative perceptions toward ePHR which may influence their endorsement of the ePHR adoption to the patients. Physicians are attracted to the features that empower patients to engage effectively in their care but are concerned regarding the data management, practice management problems, and changes to the patient–physician relationship [62]. Physicians are interested in having their patients enter their health data and update their medication list in the portal, so they can go over them with their physicians in the visits while the nurses interested in giving the patients the ability to access information that they may need later [54]. Pharmacists expect an increase in the workload and the prescription refills that have to fulfill due to the increase in the secure messages related to prescription refills [54]. Some physicians perceive that may patients may have low levels of computer and health literacy, and low levels of interest and motivation to use the ePHR which may hinder their effort to encourage their patients to adopt and use the ePHR [63]. Clinic personnel believe that patient portals can improve the patient-provider communication, increase efficiency, and enhance information sharing, while, their concerns are evolved around the potentiality for the workload to increase, health disparities increase, privacy issues, and to confuse the patients [64]. Clinic personnel expected an improvement in the patients’ satisfaction and trust with their healthcare providers [64]. The more experienced in the practice the physicians, the more they are willing to dedicate the time to interact with their patients through the ePHR, despite, the belief that the lack of reimbursement for the workload and time spent interacting with the patients through the ePHR as a major barrier in using and supporting the adoption of the ePHR [56].
It is important to understand the perceptions of the physicians before and after the adoption and implementation of the ePHR in their facilities. Physicians who perceived an increase in the workload due to the ePHR implementation, had an opposite respond after the implementation and expressing no change on the level of the workload [65]. Staff should receive appropriate training and education about the benefits of the ePHR to the practice as well as the patients themselves. Realization of the benefits of the ePHR should foster its adoption and encourage health care staff in promoting it to their patients. The perceptions of the health care providers, physicians, and nurses should be addressed in order to gain their support and endorsement toward the patients’ adoption of the ePHR.
2.6 Health Condition
The health condition and ePHR adoption appear to have a positive correlation. Many researchers have examined the adoption and use of ePHR for chronic condition management. Patients with chronic diseases tend to be more adopters to the ePHR than patients with less complex health condition [53, 66]. According to the connecting for health report which is part of the Markle Foundation’s [67], patients with chronic diseases tend to have a higher interest in the ePHR with a percentage of 65% compared to 58% of the patients without chronic diseases. Studies suggest the utilization of ePHR as a method to improve chronic disease self-management [2]. Irizarry et al. [48] showed that patients with chronic conditions and disabilities have a higher rate of adoption and use of the ePHR. The health condition may play a factor in the ePHR adoption.
Laugesen and Hassanein have developed a theoretical model for ePHR adoption by chronic disease patients as self-management tool [2]. The model intends to explain the health-related behaviors through the protection motivation theory (PMT) and information technology adoption through task-technology fit (TTF) theory in combination with the health self-management readiness concept of the patient activation measure (PAM). The new theoretical model was tested and validated vis statistical model by surveying diabetes patient. The results of the model indicated that all constructs used in the models showed significant influences on the patient’s intention to adopt an ePHR for the chronic condition management.
A systematic review conducted in 2015 on 27 selected articles investigating the patient and provider attitudes toward the use of patient portals for the management of chronic diseases [68]. The study revealed substantial improvements in the patient with chronic disease self-management and the quality of care provided by the providers has enhanced. Also, there were positive and negative attitudes toward the patient portal. Patient-provider improved communication represents the positive attitude and the security concerns and user-friendliness were the negative attitudes noted [68].
The ePHR has been used as a health management tool for various health conditions, such as diabetes, asthma, cancer, and for the children’s health care. The ePHR is used to help diabetes patients in better managing their health. A qualitative study is conducted to study the use of ePHR to improve diabetes management [69]. The study was intended to capture the perspective of the patients, general practitioners, nurses, diabetes educators, and clinical staff about the ePHR as an online diabetes management tool. The study identified four themes: disease management facilitators, challenges to ePHR use, the communication between the patients and providers, and ePHR system improvement recommendations. The results of the study showed that patients are more engaged in their care due to the ePHR as a management tool and emphasize the role of the healthcare providers as facilitators of disease management. The ePHR also has been used in the primary care settings to manage chronically ill children. The ePHR adoption is investigated in the primary care setting, as well, as a management tool of pediatric asthma [70]. The study aims at exploring the results of potential improvement in the patient–provider communication due to the ePHR adoption and use of the clinical outcomes. The findings suggest that patients with uncontrolled asthma appeared to have more medication changes and clinic visits after starting to use the ePHR compared to the year earlier. It noted that the adoption rate is unlikely to be achieved in the short-term and the more efforts are required in the ePHR implementation phase [70]. Pai et al. conducted a study to capture feedback from prostate cancer patients who were given access to an ePHR in order for them to view their medical records and use a set of support tools [71]. Information about usability, satisfaction, and concerns with the ePHR were gathered. The findings showed that the most used functions were test results and transcribed doctor’s notes. Prostate cancer patients in the study showed positive responses regarding the use of ePHR with high satisfaction rate, being able to find answers to their questions, and privacy was preserved. They as well agreed that the ePHR has improved their communication with their physicians and would continue to use it in the future.
Clark et al. have explored the current ePHR adoption by parents as caregivers to manage their children’s health care [72]. The study aimed at capturing the parents’ perspective and have found out that the main reason for the parents chose not to use ePHR to manage their children’s health care is the low perceived need to do so. It showed as well that the most used functions of the ePHR for the parent’s adopting ePHR are checking lab results and immunization records.
2.7 Portal’s Features
The ePHR features and functionalities have positive influences in the ePHR adoption. Patients want to have more control over their records and be able to explore a wide range of the portal’s features. In some cases, patients use the ePHR because they like certain features that they use frequently. The ePHR offers many features, such as patients access to their health information, summary of recent doctor visits, discharge reports, medications lists, immunizations records, secure messaging for patient-provider communication, prescription refills request, lab/tests results review, medical appointments scheduling, and educational materials access [73]. A study found that the features of the ePHR that patients use most frequently include: checking their lab results, being informed of health changes, and managing chronic disease [74].
Communication tools allow patients to take an active role in their health care and improve the relationship with their providers. Secure messaging feature facilitates the communication with the healthcare providers to better assist informed health decisions, and is considered one of the most used collaborative communication features by patients [53] alongside with medication reconciliation [48]. Secure messaging allows access to health care without, in many cases, the need for in-person visits as well as improving the quality of the doctor visits [66].
The Foundation for Accountability (FACCT), as part of the Markle Foundation’s Connecting for Health program, studied the ePHR functionalities and their usability by surveying 1246 online individuals between 2002 and 2003 [67]. The features of the ePHR that were tested are messaging doctors, checking immunizations, note mistakes in one’s record, transfer of information to new provider, and test results. The findings showed that over 70% of respondents have an interest in using one or more features of the ePHR, 35% would use 7 or more features if they were available, 75% use ePHR to communicate with doctors through email, 69% to track immunizations, 69% to track mistakes in their records, 65% to transfer information to new healthcare provider, and 63% to check the test results. The more features and functionalities offered to the patient through the ePHR, the more interested and engaged they are.
Meaningful use initiative requires providers to allow patients to have access to view, download, and transmit their health information [60], as well as, requires that 5% of the healthcare providers patients’ population use secure e-messaging to improve the communication between the provider and the patient [61]. The availability of the more practical features of the ePHR encourages the patient’s adoption and use of such an innovative health management tool.
2.8 Patients Characteristics
Patients have various characteristics that may influence their intention to adopt ePHR. Current research has demonstrated that patients’ interest and ability to use ePHR is strongly influenced by personal factors such as age, ethnicity, education level, health literacy, health status, and role as a caregiver [48]. Health care delivery factors, mainly provider endorsement, and patient portal usability, also contribute to patients’ ability to engage through and with the ePHR [48].
A study examining the digital divide in the adoption and use of ePHR investigated the characteristics of the ePHR adopters and non-adopters based on the activation of the ePHR online account given by their health providers and the frequent use [75]. The study showed that the percentage of patients adopting ePHR is 43% out of 75,056 patients representing the population of the patients in a certain health care facility. The study indicated that the adoption and use of ePHR among certain populations such as underserved, low-income, and elderly seem to be low due to factors like lack of access to computer or internet and fear of using such a computerized system. The study showed that White population have a higher rate of ePHR adoption in compared to Black and Hispanic population as the race could be used as a determinant factor of the adoption. Also, people with higher income appeared to have a higher adoption rate than people with lower income. This chapter concluded with the statement that the following factors increasing the number of chronic diseases, race/ethnicity, and insurance status are used to predict the intensity of the ePHR usage.
People with different race and ethnicity appear to have different perception toward the adoption and use of the ePHR. A study indicated that there is a low rate of adoption by the race and ethnicity. It is as well shown that it might be a result of either the lack of interest and motivation in such a system [53] or the availability of the computer and internet connection [76].
Elderly population as potential ePHR adopters are an important segment of the ePHR adoption and use. A study investigated the older adult’s perspective on the adoption and use of ePHR interviewed 74 elderlies to capture their perspective [77]. The finding showed that only 20% reported using ePHR. The interviewee cited the most valuable features of the ePHR as the ease of access to health records and direct messaging and communication with health providers. The study highlighted the lack of computer proficiency, internet costs, and security concerns as the barriers to adoption by the elderly. It indicates the importance of taking into consideration the elderly perspective when designing and implementing ePHR.
Sakaguchi-Tang et al. conducted a systematic review to study the ePHR use and experience among older adults [21]. The review identified two barriers: privacy and security concerns, and lack of competency to use technology. The study highlighted two facilitators: technical assistance availability and family and provider advice.
Czaja et al. studied the use of ePHR by underserved adult population to perform health management activities [78]. The results showed that older adults consider ePHR as a valuable tool despite not being able to complete certain tasks and needed assistance. It can be concluded that the race/ethnicity, income, and age factors influencing the adoption and use of ePHR. Barriers that should be considered in designing the ePHR and influence the adoption include the lack of computer and internet access, the fear to deal with technology or perform certain ePHR tasks, and the need for assistance.
2.9 Perceived Credibility (Privacy and Security)
Privacy and security of health information can pose a huge threat to the ePHR adoption. The patients’ health information is dispersed and distributed among various systems that are aggregated and then transferred to the ePHR for the patients to access. Through the data transmission process, security issues may occur. Furthermore, data governance and access rights determine who has the access right to what part of data which also may threaten the patient health information privacy. The importance of security and privacy of the patient health information are as equal as having interoperable system that allows the patient to access their information from various sources in a unified ePHR. Steele et al. identified three important security and privacy components of the patient health data in the ePHR [79]: who controls the access policy of the data, who is responsible for the physical security and policies, and the technical mechanism for achieving data security.
The security and privacy of the patient’s health information is a critical component of the health process as if the patients lose their trust in the system or feel their confidentiality is being compromised, they may not want to share the full details of their health information with their health providers [80]. There are a variety of privacy and security threats. These threats may include insider abuse; accidental disclosures, insider curiosity, and insider subornation; secondary users; and outsider intrusion [81].
A study found out that about 91% of the patients are very concerned regarding their health information being secure and safe despite their belief that ePHR systems are safe and their health information are protected [67]. In the case of the chronically ill patients, patients value some of ePHR features over the privacy and security and feel less concerned about their health information privacy [67]. Dontje et al. ranked the security issue as one of the barriers of ePHR adoption factors [11]. Ong et al. added a new construct to the TAM called perceived credibility to test the consumer’s acceptance of a certain technology [82]. Perceived credibility is defined with regards to the ePHR as the degree to which a person believes that using ePHR would be free of privacy and security threats [82]. A survey-based study was conducted to investigate the factors that motivate nurses to protect the privacy of electronic medical records (EMR) [83]. The findings suggest that the factors of attitude, subjective norm, and perceived behavioral control of the nurses significantly predicted the nurses’ intention to protect the privacy of EMR. The privacy and security of the ePHR are essential factors influencing the patient’s adoption of the ePHR.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) aims at developing regulations and policies to protect the privacy and security of the health information. The HIPAA standards aim at protecting health information and ensure secure transmission of the electronic transferred health information. These rules allow healthcare providers to adopt and implement new innovative technologies to improve the quality of provided care while ensuring the privacy and security of the patient’s health information [84]. The health care providers under the HIPAA privacy rule are committed to provide patients with a notice of privacy practices (NPP) and respond to patients’ requests that include: access to their protected health information (PHI), confidential communications, and restrictions on uses and disclosures of their health information [85]. HIPAA laws and regulations regarding the privacy and security of the patient health information have had a significant impact on the health care industry including the way, health care providers communicate with the patients and their families.
3 Taxonomy of Factors Related to the Adoption and Use of ePHR
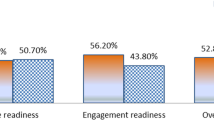
This section identifies the key factors retrieved from previous research on the adoption and use of the ePHR and the technology adoption and use theories and models. These factors are important as they are related to the adoption and use of the ePHR for health management. A taxonomy of the key factors related to the adoption and use of ePHR technology has been developed, and a classification of the related factors into six main variables is constructed as shown in Fig. 15.1. The six main variables are shown to have been determinants of the patient’s intention to adopt and use the ePHR for health management. The six main factors are performance factors, effort factors, social factors, facilitating conditions, perceived credibility, health factors, and computer factors. The factors included under performance are perceived usefulness [22, 23, 25, 46, 51, 55, 86,87,88,89], relative advantage [24], and portal features [67, 74, 77]. Effort factors include perceived ease of use [20, 22,23,24,25, 27, 28, 46, 51, 55, 86,87,88,89], and complexity. Social factors include subjective norms [22, 23, 25, 55, 83, 90] and self-perception [22, 25]. Facilitating conditions include perceived behavioral control [83, 90], facilitating conditions [23, 25], compatibility [24], computer and internet availability [21, 46, 91], and interoperability [31, 37, 39, 40, 59]. Perceived credibility includes two main factors privacy [11, 24, 46, 55, 67, 82, 83, 86, 91] and security [11, 24, 46, 55, 67, 82, 86]. Health factors covers consumer’s and provider’s health-related aspects, such as health literacy and eHealth literacy [6, 8, 11, 12, 41], satisfaction with medical care [46, 57, 92], self-perceived health [91], provider’s support [11, 46, 48, 53, 56,57,58,59, 69, 88], and health condition [48, 53, 66, 67, 69, 71]. Computer factors involve factors other than the ones dealing with the computer as infrastructure computer literacy [41,42,43, 45, 46] and computer anxiety [41, 45]. These factors are perceived to influence the adoption and use of the ePHR for health management. Further evaluation, validation, and selection of only the most crucial factors are required in order to construct the final model.
Table 15.1 shows the taxonomy of the factors related to the adoption and use of the ePHR.
4 Conclusion
Electronic personal health record (ePHR) helps support patient-centered healthcare by allowing patients to access their health information from their provider’s EHR. This report is intended to investigate the key factors impacting the adoption and use of the tethered electronic personal health records (ePHR). This report retrieved the key factors from previous research on the adoption and use of the ePHR and the technology adoption and use theories and models then the taxonomy was created. The key factors are grouped into themes. These themes include performance factors, effort factors, social factors, facilitating conditions, perceived credibility, health factors, and computer factors. The themes involve essential factors that influence the adoption and use of the ePHR, such as perceived usefulness, perceived ease of use, portal features, subjective norms, computer and internet availability, computer literacy, computer anxiety, privacy and security, health literacy, satisfaction with medical care, and provider’s support.
References
Office of National Coordinator for Health Information Technology. Justification of estimates for appropriations committee: Fiscal year 2018. Department of Health and Human Services: Office of the National Coordinator for Health Information Technology.
Laugesen, J., & Hassanein, K. (2017). Adoption of personal health records by chronic disease patients: A research model and an empirical study. Computers in Human Behavior, 66, 256–272.
Ratzan, S. C., & Parker, R. M. (2000). Health literacy. In National library of medicine current bibliographies in medicine. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services.
Vernon, J. A., Trujillo, A., Rosenbaum, S. J., & DeBuono, B. (2007). Low health literacy: Implications for national health policy. Washington, DC: Department of Health Policy, School of Public Health and Health Services, The George Washington University.
Mackert, M., Mabry-Flynn, A., Champlin, S., Donovan, E. E., & Pounders, K. (2016). Health literacy and health information technology adoption: The potential for a new digital divide. Journal of Medical Internet Research, 18(10), e264.
Norman, C. D., & Skinner, H. A. (2006). eHEALS: The eHealth literacy scale. Journal of Medical Internet Research, 8(4), e27.
Briones, R. (2015). Harnessing the web: How E-health and E-health literacy impact young adults’ perceptions of online health information. Medicine 2.0, 4(2), e5.
Noblin, A. M., Wan, T. T. H., & Fottler, M. (2012). The impact of health literacy on a patient’s decision to adopt a personal health record. Perspectives in Health Information Management, 9(Fall), 1e.
Jensen, J. D., King, A. J., Davis, L. S. A., & Guntzviller, L. M. (2010). Utilization of internet technology by low-income adults: The role of health literacy, health numeracy, and computer assistance. Journal of Aging and Health, 22(6), 804–826.
Monkman, H., & Kushniruk, A. (2013). Applying usability methods to identify health literacy issues: An example using a personal health record. Studies in Health Technology and Informatics, 183, 179–185.
Dontje, K., Corser, W. D., & Holzman, G. (2014). Understanding patient perceptions of the electronic personal health record. The Journal for Nurse Practitioners, 10(10), 824–828.
Cortelyou-Ward, K., Noblin, A., & Williams, C. (2012). Using the personal health record to improve health literacy: A social capital perspective. International Journal of Business, Humanities and Technology, 2(3), 7–15.
Hemsley, B., Rollo, M., Georgiou, A., Balandin, S., & Hill, S. (2018). The health literacy demands of electronic personal health records (e-PHRs): An integrative review to inform future inclusive research. Patient Education and Counseling, 101(1), 2–15.
van der Vaart, R., van Deursen, A. J., Drossaert, C. H., Taal, E., van Dijk, J. A., & van de Laar, M. A. (2011). Does the eHealth literacy scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. Journal of Medical Internet Research, 13(4), e86.
Mitsutake, S., Shibata, A., Ishii, K., Okazaki, K., & Oka, K. (2011). Developing Japanese version of the eHealth literacy scale (eHEALS). Nihon Koshu Eisei Zasshi, 58(5), 361–371.
Jarahi, L., Asadi, R., & Hakimi, H. R. (2017). General health literacy assessment of Iranian women in Mashhad. Electronic Physician, 9(11), 5764–5769.
Dashti, S., Peyman, N., Tajfard, M., & Esmaeeli, H. (2017). E-health literacy of medical and health sciences university students in Mashhad, Iran in 2016: A pilot study. Electronic Physician, 9(3), 3966–3973.
Britt, R. K., Collins, W. B., Wilson, K., Linnemeier, G., & Englebert, A. M. (2017). eHealth literacy and health behaviors affecting modern college students: A pilot study of issues identified by the American College Health Association. Journal of Medical Internet Research, 19(12), e392.
Petrič, G., Atanasova, S., & Kamin, T. (2017). Ill literates or illiterates? Investigating the eHealth literacy of users of online health communities. Journal of Medical Internet Research, 19(10), e331.
Segall, N., Saville, J. G., L’Engle, P., Carlson, B., Wright, M. C., Schulman, K., & Tcheng, J. E. (2011). Usability evaluation of a personal health record. American Medical Informatics Association Annual Symposium Proceedings, 2011, 1233–1242.
Sakaguchi-Tang, D. K., Bosold, A. L., Choi, Y. K., & Turner, A. M. (2017). Patient portal use and experience among older adults: Systematic review. JMIR Medical Informatics, 5(4), e38.
Hsieh, H.-L., Kuo, Y.-M., Wang, S.-R., Chuang, B.-K., & Tsai, C.-H. (2017). A study of personal health record user’s behavioral model based on the PMT and UTAUT integrative perspective. International Journal of Environmental Research and Public Health, 14(1), 8.
Agrawal, E. (2011). Acceptance and use of personal health record: Factors affecting physicians’perspective. PhD thesis.
Emani, S., Yamin, C. K., Peters, E., Karson, A. S., Lipsitz, S. R., Wald, J. S., Williams, D. H., & Bates, D. W. (2012). Patient perceptions of a personal health record: A test of the diffusion of innovation model. Journal of Medical Internet Research, 14(6), e150.
Tavares, J., & Oliveira, T. (2016). Electronic health record patient portal adoption by health care consumers: An acceptance model and survey. Journal of Medical Internet Research, 18(3), e49.
Liu, L. S., & Hayes, G. R. (2010). Heuristic evaluation of personal health records systems. In International workshop on interactive systems in healthcare (p. 101). New York, NY: ACM.
Sheehan, B., & Lucero, R. J. (2015). Initial usability and feasibility evaluation of a personal health record-based self-management system for older adults. EGEMS (Washington, DC), 3(2), 1152.
Price, M., Bellwood, P., & Davies, I. (2015). Using usability evaluation to inform Alberta’s personal health record design. Studies in Health Technology and Informatics, 208, 314–318.
HIMSS. (2014, September 01). The business case for interoperability and health information exchange [Online]. Retrieved December 08, 2017, from http://www.himss.org/business-case-interoperability-and-health-information-exchange
HIMSS. (2016, May 12). Introductory glossary and brochure: Health information exchange [Online]. Retrieved August 02, 2017, from http://www.himss.org/introductory-glossary-and-brochure-health-information-exchange
What is HIE (health information exchange)? Providers & professionals. HealthIT.gov [Online]. Retrieved December 08, 2017, from https://www.healthit.gov/providers-professionals/health-information-exchange/what-hie
Fontaine, P., Ross, S. E., Zink, T., & Schilling, L. M. (2010). Systematic review of health information exchange in primary care practices. Journal of American Board of Family Medicine, 23(5), 655–670.
Health information exchange governance. Providers & professionals. HealthIT.gov [Online]. Retrieved December 08, 2017, from https://www.healthit.gov/providers-professionals/hie-governance
Fricton, J. R., & Davies, D. (2008). Personal health records to improve health information exchange and patient safety. In K. Henriksen, J. B. Battles, M. A. Keyes, & M. L. Grady (Eds.), Advances in patient safety: New directions and alternative approaches (Vol. 4: Technology and medication safety). Rockville, MD: Agency for Healthcare Research and Quality.
Wen, K.-Y., Kreps, G., Zhu, F., & Miller, S. (2010). Consumers’ perceptions about and use of the internet for personal health records and health information exchange: Analysis of the 2007 health information national trends survey. Journal of Medical Internet Research, 12(4), e73.
Patel, V. N., Dhopeshwarkar, R. V., Edwards, A., Barrón, Y., Sparenborg, J., & Kaushal, R. (2012). Consumer support for health information exchange and personal health records: A regional health information organization survey. Journal of Medical Systems, 36(3), 1043–1052.
HIMSS. (2017, August 17). Interoperability and health information exchange [Online]. Retrieved December 08, 2017, from http://www.himss.org/library/interoperability-health-information-exchange
2016 report to congress on health information technology progress [Online]. Retrieved December 05, 2017, from https://dashboard.healthit.gov/report-to-congress/2016-report-congress-examining-hitech-era-future-health-information-technology.php
Archer, N., Fevrier-Thomas, U., Lokker, C., McKibbon, A., Willison, D., & Straus, S. (2010). Electronic Personal Health Records: An Environmental Scan. Working Paper No. 34. McMaster Business Research Centre (MeRC), McMaster University: Hamilton, Canada
Pagliari, C., Detmer, D., & Singleton, P. (2007). Electronic personal health records. In Emergence and implications for the UK. London, UK: The Nuffield Trust.
Norman, C. D., & Skinner, H. A. (2006). eHealth literacy: Essential skills for consumer health in a networked world. Journal of Medical Internet Research, 8(2), e9.
Day, K., & Gu, Y. (2012). Influencing factors for adopting personal health record (PHR). Studies in Health Technology and Informatics, 178, 39–44.
Saranto, K., & Leino-Kilpi, H. (1997). Computer literacy in nursing; developing the information technology syllabus in nursing education. Journal of Advanced Nursing, 25(2), 377–385.
Koivunen, M., Hätönen, H., & Välimäki, M. (2008). Barriers and facilitators influencing the implementation of an interactive internet-portal application for patient education in psychiatric hospitals. Patient Education and Counseling, 70(3), 412–419.
Lober, W. B., Zierler, B., Herbaugh, A., Shinstrom, S. E., Stolyar, A., Kim, E. H., & Kim, Y. (2006). Barriers to the use of a personal health record by an elderly population. American Medical Informatics Association Annual Symposium Proceedings, 2006, 514–518.
Cocosila, M., & Archer, N. (2012). Consumer perceptions of the adoption of electronic personal health records: an empirical investigation. Seattle, Washington: Americas Conference on Information Systems Proceedings; Americas Conference on Information Systems 2012 Proceedings. 10. https://aisel.aisnet.org/amcis2012/proceedings/ISHealthcare/10
Kim, E., Mayani, A., Modi, S., Kim, Y., & Soh, C. (2005). Evaluation of patient-centered electronic health record to overcome digital divide. Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 1, 593–596.
Irizarry, T., DeVito Dabbs, A., & Curran, C. R. (2015). Patient portals and patient engagement: A state of the science review. Journal of Medical Internet Research, 17(6), e148.
Kim, K., & Nahm, E. (2012). Benefits of and barriers to the use of personal health records (PHR) for health management among adults. Online Journal of Nursing Informatics, 16(3), 1–9.
Pew Research Center: Internet & Technology. (2018, Feb 05). Internet/broadband fact sheet. Pew Research Center: Internet, Science & Tech.
Goodhue, D. L., & Thompson, R. L. (1995). Task-technology fit and individual performance. MIS Quarterly, 19(2), 213–236.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D. (2003). User acceptance of information technology: Toward a unified view. MIS Quarterly, 27(3), 425–478.
Griffin, A., Skinner, A., Thornhill, J., & Weinberger, M. (2016). Patient Portals. Applied clinical informatics, 7(2), 489–501.
Nazi, K. M. (2013). The personal health record paradox: Health care professionals’ perspectives and the information ecology of personal health record systems in organizational and clinical settings. Journal of Medical Internet Research, 15(4), e70.
Chung, M.-H., Ho, C.-H., & Wen, H.-C. (2016). Predicting intentions of nurses to adopt patient personal health records: A structural equation modeling approach. Computer Methods and Programs in Biomedicine, 136, 45–53.
Vydra, T. P., Cuaresma, E., Kretovics, M., & Bose-Brill, S. (2015). Diffusion and use of tethered personal health records in primary care. Perspectives in Health Information Management, 12(Spring), 1c.
Menon, A. S., Greenwald, S., Ma, T. J., Kooshesh, S., & Duriseti, R. (2012). Patient and physician willingness to use personal health records in the emergency department. Western Journal of Emergency Medicine, 13(2), 172–175.
Wells, S., Rozenblum, R., Park, A., Dunn, M., & Bates, D. W. (2015). Organizational strategies for promoting patient and provider uptake of personal health records. Journal of the American Medical Informatics Association, 22(1), 213–222.
Jha, A. K., DesRoches, C. M., Campbell, E. G., Donelan, K., Rao, S. R., Ferris, T. G., Shields, A., Rosenbaum, S., & Blumenthal, D. (2009). Use of electronic health Records in U.S. hospitals. New England Journal of Medicine, 360(16), 1628–1638.
HIMSS. (2014, December 01). Using patient portals to achieve meaningful use (EP Edition) [Online]. Retrieved August 02, 2017, from http://www.himss.org/using-patient-portals-achieve-meaningful-use-ep-edition
Wright, A., Feblowitz, J., Samal, L., McCoy, A. B., & Sittig, D. F. (2014). The Medicare electronic health record incentive program: Provider performance on core and menu measures. Health Services Research, 49(1 Pt 2), 325–346.
Yau, G. L., Williams, A. S., & Brown, J. B. (2011). Family physicians’ perspectives on personal health records: Qualitative study. Canadian Family Physician, 57(5), e178–e184.
Witry, M. J., Doucette, W. R., Daly, J. M., Levy, B. T., & Chrischilles, E. A. (2010). Family physician perceptions of personal health records. Perspectives in Health Information Management, 7, 1d.
Miller, D. P., Jr., Latulipe, C., Melius, K. A., Quandt, S. A., & Arcury, T. A. (2016). Primary care providers’ views of patient portals: Interview study of perceived benefits and consequences. Journal of Medical Internet Research, 18(1), e8.
Keplinger, L. E., Koopman, R. J., Mehr, D. R., Kruse, R. L., Wakefield, D. S., Wakefield, B. J., & Canfield, S. M. (2013). Patient portal implementation: Resident and attending physician attitudes. Family Medicine, 45(5), 335–340.
Wade-Vuturo, A. E., Mayberry, L. S., & Osborn, C. Y. (2013). Secure messaging and diabetes management: Experiences and perspectives of patient portal users. Journal of the American Medical Informatics Association, 20(3), 519–525.
Connecting for Health. (2003, July 01). The personal health working group final report. Markle Foundation [Online]. Retrieved November 12, 2017, from http://www.providersedge.com/ehdocs/ehr_articles/The_Personal_Health_Working_Group_Final_Report.pdf
Kruse, C. S., Argueta, D. A., Lopez, L., & Nair, A. (2015). Patient and provider attitudes toward the use of patient portals for the management of chronic disease: A systematic review. Journal of Medical Internet Research, 17(2), e40.
Urowitz, S., Wiljer, D., Dupak, K., Kuehner, Z., Leonard, K., Lovrics, E., Picton, P., Seto, E., & Cafazzo, J. (2012). Improving diabetes management with a patient portal: Qualitative study of a diabetes self-management portal. Journal of Medical Internet Research, 14(6), e158.
Fiks, A. G., DuRivage, N., Mayne, S. L., Finch, S., Ross, M. E., Giacomini, K., Suh, A., McCarn, B., Brandt, E., Karavite, D., Staton, E. W., Shone, L. P., McGoldrick, V., Noonan, K., Miller, D., Lehmann, C. U., Pace, W. D., & Grundmeier, R. W. (2016). Adoption of a portal for the primary care management of pediatric asthma: A mixed-methods implementation study. Journal of Medical Internet Research, 18(6), e172.
Pai, H. H., Lau, F., Barnett, J., & Jones, S. (2013). Meeting the health information needs of prostate cancer patients using personal health records. Current Oncology, 20(6), e561–e569.
Clark, S. J., Costello, L. E., Gebremariam, A., & Dombkowski, K. J. (2015). A national survey of parent perspectives on use of patient portals for their children’s health care. Applied clinical informatics, 6(1), 110–119.
PatientEngagementHIT. (2017, February 17). How do patient portals and personal health records differ? [Online]. Retrieved December 20, 2017, from https://patientengagementhit.com/features/how-do-patient-portals-and-personal-health-records-differ
Zettel-Watson, L., & Tsukerman, D. (2016). Adoption of online health management tools among healthy older adults: An exploratory study. Health Informatics Journal, 22(2), 171–183.
Yamin, C. K., Emani, S., Williams, D. H., Lipsitz, S. R., Karson, A. S., Wald, J. S., & Bates, D. W. (2011). The digital divide in adoption and use of a personal health record. Archives of Internal Medicine, 171(6), 568–574.
Goel, M. S., Brown, T. L., Williams, A., Cooper, A. J., Hasnain-Wynia, R., & Baker, D. W. (2011). Patient reported barriers to enrolling in a patient portal. Journal of the American Medical Informatics Association, 18(Suppl 1), i8–i12.
Turner, A. M., Osterhage, K., Hartzler, A., Joe, J., Lin, L., Kanagat, N., & Demiris, G. (2015). Use of patient portals for personal health information management: The older adult perspective. American Medical Informatics Association Annual Symposium Proceedings, 2015, 1234–1241.
Czaja, S. J., Zarcadoolas, C., Vaughon, W. L., Lee, C. C., Rockoff, M. L., & Levy, J. (2015). The usability of electronic personal health record systems for an underserved adult population. Human Factors, 57(3), 491–506.
Steele, R., Min, K., & Lo, A. (2012). Personal health record architectures: Technology infrastructure implications and dependencies. Journal of the Association for Information Science and Technology, 63(6), 1079–1091.
HealthIT.gov. (2015, April). Guide to privacy and security of electronic health information. Office of the National Coordinator for Health Information Technology [Online]. Retrieved March 19, 2018, from https://www.healthit.gov/sites/default/files/pdf/privacy/privacy-and-security-guide.pdf
Rindfleisch, T. C. (1997). Privacy, information technology, and health care. Communications of the ACM, 40(8), 92–100.
Ong, C.-S., Lai, J.-Y., & Wang, Y.-S. (2004). Factors affecting engineers’ acceptance of asynchronous e-learning systems in high-tech companies. Information & Management, 41(6), 795–804.
Ma, C.-C., Kuo, K.-M., & Alexander, J. W. (2016). A survey-based study of factors that motivate nurses to protect the privacy of electronic medical records. BMC Medical Informatics and Decision Making, 16(1), 13.
HHS.gov. (2009, November 20). Summary of the HIPAA security rule [Online]. Retrieved November 15, 2017, from https://www.hhs.gov/hipaa/for-professionals/security/laws-regulations/index.html
HealthIT.gov. Guide to privacy and security of electronic health information [Online]. Retrieved March 25, 2018, from https://www.healthit.gov/providers-professionals/guide-privacy-and-security-electronic-health-information
Gartrell, K., Trinkoff, A. M., Storr, C. L., Wilson, M. L., & Gurses, A. P. (2015). Testing the electronic personal health record acceptance model by nurses for managing their own health. Applied clinical informatics, 6(2), 224–247.
Klein, R. (2007). An empirical examination of patient-physician portal acceptance. European Journal of Information Systems, 16(6), 751–760.
Goff, C. R. (2016). Predictors of patient portal use: Patient engagement through meaningful use. Ph.D., Capella University, Minneapolis, MN.
Razmak, J., & Bélanger, C. (2018). Using the technology acceptance model to predict patient attitude towards personal health records in regional communities. Information Technology & People, 31(2), 306–326.
Emani, S., Healey, M., Ting, D. Y., Lipsitz, S. R., Ramelson, H., Suric, V., & Bates, D. W. (2016). Awareness and use of the after-visit summary through a patient portal: Evaluation of patient characteristics and an application of the theory of planned behavior. Journal of Medical Internet Research, 18(4), e77.
Harrison, T. G., Wick, J., Ahmed, S. B., Jun, M., Manns, B. J., Quinn, R. R., Tonelli, M., & Hemmelgarn, B. R. (2015). Patients with chronic kidney disease and their intent to use electronic personal health records. Canadian Journal of Kidney Health and Disease, 2, 23.
Agarwal, R., Anderson, C., Zarate, J., & Ward, C. (2013). If we offer it, will they accept? Factors affecting patient use intentions of personal health records and secure messaging. Journal of Medical Internet Research, 15(2), e43.
Laugesen, D. J. (2013). Adoption of electronic personal health records by chronic disease patients: Integrating protection motivation theory and task-technology fit. PhD thesis, School of Graduate Studies, McMaster University, Hamilton, ON.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Alzahrani, S., Daim, T. (2019). Assessing the Key Factors Impacting the Adoption and Use of Tethered Electronic Personal Health Records for Health Management. In: Daim, T., Dabić, M., Başoğlu, N., Lavoie, J.R., Galli, B.J. (eds) R&D Management in the Knowledge Era. Innovation, Technology, and Knowledge Management. Springer, Cham. https://doi.org/10.1007/978-3-030-15409-7_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-15409-7_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15408-0
Online ISBN: 978-3-030-15409-7
eBook Packages: Business and ManagementBusiness and Management (R0)