Abstract
The growing prevalence of various forms of dementia as well as awareness related to their associated prodromes has increased demand for assessment and interventions directed at behavioral issues in dementia, as well as the psychological issues presenting in dementia prodromes. The nature of such interventions must also evolve across disease course. Although pharmacological intervention may be effective in managing some of the cognitive, psychological, and behavioral symptoms of dementias and their prodromes, greater focus on non-pharmacological interventions (i.e., psychological and behavioral interventions) is required in order to minimize the limitations and negative side effects of pharmacological treatments alone (Oliveira et al., Biomed Res Int, 2015). Thus, this chapter will focus upon non-pharmacological interventions across the course of dementia from prodromes to late-stage illness.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The worldwide prevalence of dementia has exceeded historical predictions, having reached 46.8 million affected individuals in 2015 with these numbers expected to double in the subsequent 20 years to come. Furthermore, incidence rates of dementia significantly increase with advancing age. Approximately 2% of those affected are under the age of 65, with prevalence rates doubling every 5 years thereafter (Prince, Wimo, Guerchet, Ali, & Wu, 2015). There is also well-documented financial and social costs for the burgeoning population of Alzheimer’s disease and other forms of dementia, with predicted estimates reaching $1 trillion in US dollars in 2018 (Wimo et al., 2017).
These neurodegenerative diseases are defined by their varying cognitive, psychological, and behavioral symptoms. The complexity in management of such issues is further confounded by the evolution of dementia symptoms inherent over the course of illness. Further challenges to effective management of the behavioral and psychological symptoms of dementia (BPSD) include the heterogeneity of these factors that span the course of illness. The psychological issues inherent in the prodromal phases, including preclinical dementia (PCD) and mild cognitive impairment (MCI), can encompass symptoms of depression as well as variants of anxiety (Caselli et al., 2018), which may evolve to grief. There are also challenges of adjusting to cognitive change in early-stage dementia. These issues are distinct from those faced in mid- to late-stage dementia (Cerejeira, Lagarto, & Mukaetova-Ladinska, 2012; Muller-Spahn, 2003), where behavioral issues such as agitation and noncompliance with care or increased risk of falls increases with the evolution of cognitive decline. Consequently, the form of assessment and the interventions required for BPSD must evolve across the disease course. Although pharmacological interventions may be effective in managing some of the cognitive, psychological, and behavioral symptoms of dementias and their prodromes, greater focus upon non-pharmacological interventions including psychological and behavioral is important in order to minimize the limitations and negative side effects experienced by utilizing only pharmacological treatments (Oliveira et al., 2015). This chapter will focus upon non-pharmacological interventions across the course of dementia from prodromes to late-stage illness.
Psychological Factors of Dementia Prodromes
The prodromes of various forms of dementia, including preclinical dementia (PCD – prior to the presence of objective evidence for cognitive impairment) and mild cognitive impairment (MCI – objective evidence for cognitive impairment is present without meeting full diagnostic criteria for dementia) may present with distinct psychological issues that need to be distinguished from future disease progression. For example, symptoms of depressed mood and anxiety may be in response to emerging cognitive issues. A recent study of personality factors in PCD and MCI suggests an increase in neuroticism and decreasing openness along with subclinical indices of psychological factors including somatization, depression, anxiety, irritability, and aggression which were opined to be intrinsic to emerging disease as these issues were identified prior to the communication of change from PCD to MCI status (Caselli et al., 2018). These authors conclude that there may be a relationship between such psychological factors and prior findings of preclinical memory decline which precluded predicted diagnosis by 15–20 years.
Such findings affirm the need for comprehensive non-pharmacological approaches of care for this prodromal population. There is a growing public access to information about dementia and their risk factors, and although such information can certainly be of benefit, lack of regulation (e.g., online information) may place consumers accessing the information at risk for increased anxiety and/or misinterpretation of risk factors (Lawless, Augoustinos, & LeCouteur, 2017). Thus, it is important for clinicians addressing PCD and/or MCI populations to query perceptions of cognitive status and risk, as well as to provide evidenced-based psychoeducation in order to mitigate the emergence of anxiety or depression in anticipation of future dementia.
Regardless, in clinical practice, depression and anxiety are significant confounds to the clinical presentation of MCI populations. Although, historically, depression has been the focus of preclinical dementia care (McAllister, 1983), an emerging literature (Rozzini et al., 2009) supports the predominance of anxiety in this heterogeneous group. Anxiety is certainly known to be prevalent in aging populations with estimates of up to 15% of adults aged 60 and over experiencing symptoms meeting the criteria for anxiety disorder (Tampi & Tampi, 2014), with subclinical anxiety symptoms presenting in an additional 15–20%. Thus, it will also be important for clinicians to provide undiagnosed populations such as those with PCD or MCI who are presenting with concerns for cognitive change with information about the other possible contributing factors, including anxiety that may impact cognition, apart from the neurodegenerative process. Discussion of the cognitive impact of mood factors, as well as the normal course of aging upon cognition, must become a component of clinical care within the prodromes of dementia, along with any discussion of dementia risk factors.
Complicating diagnostic specificity within the prodromal phases of dementia is the relationship of anxiety in later life, which can be associated with some degree of cognitive impairment (Beaudreau & O’Hara, 2008). As the profile of cognitive performance is the criteria upon which diagnosis of most forms of dementia depends, it is critical to formally evaluate these psychological factors in conjunction with the formal assessment of cognitive function, which is more standard in the diagnostic process of dementia care. Ideally, this would take the form of a comprehensive neuropsychological evaluation including objective measurement of all aspects of cognition (e.g., overall intellect, attention, visual/verbal memory, visual-spatial skills, executive functions), as well as a full objective evaluation of mood and personality (e.g., symptoms of depression, anxiety, somatization, mood stability, personality traits). Such an objective assessment, in conjunction with a semi-structured clinical interview, provides greater specificity of cognitive deficits in the context of psychological factors.
One of the most clinically relevant distinctions in the evaluation of mood issues within prodromal populations is the differentiation of reactive anxiety from primary form of anxiety. Reactive anxiety is anxiety in response to or in anticipation of the consequence of measurable cognitive decline, whereas primary form of anxiety is anxiety that may be casually related to cognitive change. However, the paucity of formal research on anxiety within the PCD and MCI groups, as well as in dementia in general, remains a barrier to further understanding. Some studies suggest anxiety as a risk factor for conversion to dementia (Gulpers et al., 2016) and may represent the reactive anxiety group cited above, with anxiety emerging most often in response to specific cognitive change experienced by the affected individual. Other studies have not replicated this finding (Devier et al., 2009), suggesting a possible primary anxiety group contained within MCI populations, where the anxiety is contributing to perception of cognitive change rather than in reaction to objective cognitive decline. Such equivocal findings in the area of anxiety in PCD and MCI reflect the complexity of this psychological factor within this population, which may simply reflect a diversity of factors contributing to the presenting anxiety, such as intolerance of uncertainty (i.e., as experienced within the often prolonged diagnostic process), intolerance for change (i.e., as experienced with any change in cognition for MCI), or anticipatory worry (i.e., related to expected consequence of cognitive change and/or in anticipation of future disability related to dementia).
Appropriate identification and treatment of anxiety are required to improve diagnostic specificity in MCI, which may facilitate prediction of conversion to dementia. Cognitive behavioral therapy (CBT) has proven to be one of the most effective means of managing anxiety both for general and MCI populations. However, modifications to standard protocol approaches for such treatment may be required to accommodate objective cognitive compromise present in MCI groups. Such modifications would include the need for increased repetition of information and exercises conducted within this form of psychotherapy. Such treatment modifications would ideally be informed by the aforementioned comprehensive neuropsychological evaluation of cognitive strengths and weaknesses to ensure accurate compensatory strategies embedded within any form of psychological treatment are provided.
With such support, individuals within the MCI group may be better able to cope with the uncertainty of future diagnosis. In addition, stabilization of anxiety symptoms would aid more accurate cognitive evaluation for diagnostic purposes. Unfortunately, formalized anxiety treatment is not a common component in outpatient dementia clinics. However, integration of psychological treatment such as CBT interventions into the standard practice of dementia care would be more likely with further research into the efficacy of such forms of treatment with focus upon the potential for increased diagnostic specificity and perhaps prediction of conversion.
It is important to note that increased use of health-care resources and functional disability are inherent in anxiety populations, in general (Roy-Byrne, 1996). This would be no different for those in the prodromes of dementia, which only serve to increase health costs further in this area. In the dementia field where diagnostic uncertainty can remain for several years prior to meeting formal criteria, it is essential that health resources be more effectively utilized with individuals presenting with primary anxiety being treated through different care pathways such as via psychiatry or psychology resources rather than through neurology.
In addition to addressing the psychological issues noted above, the role of neurorehabilitation in mitigating cognitive issues has been a significant focus within the public domain for aging populations, including dementia and their prodromes. For PCD and MCI populations, computer “brain games” based upon theories of neuroplasticity are primarily involved. Neuroplasticity is a theory of generation of neural pathways through cognitive activities, thought to improve neurological resilience. Although there is evidence of the benefit of such programs on targeted cognitive skills, there is no consistent evidence of such skills being generalized to daily function (Sherman, Mauser, Nuno, & Sherzai, 2017). Therefore, in discussing these neurorehabilitation programs, which often have associated costs such as through websites or clinicians providing such programs, it is important to emphasize the lack of evidence for reversal of cognitive symptoms or disease. This informed approach to such intervention is critical to ensuring the engagement in such programs does not become predatory or misleading for this vulnerable population. Further research about the use of online tests and quality of online articles about Alzheimer’s disease is warranted as there are ethical issues in the unregulated industry of neurorehabilitation of dementia (Robillard & Feng, 2016; Robillard et al., 2015). Ongoing formal review and psychoeducation are arranged within clinical populations.
Behavioral and Psychological Symptoms in Early-Stage Dementia
The psychological factors of early-stage dementia may include continuation of anxiety symptoms present within the PCD and MCI groups. However, following formal diagnosis, additional psychological factors such as grief, frustration, and anger may emerge and require distinct intervention and/or support. These resulting psychological factors are often in response to greater awareness of cognitive change and the consequent challenges of functional capacities during early-stage illness. In addition, for some individuals, fear regarding anticipated future decline (e.g., cognitive, functional) can result in excessive preoccupation and/or rumination, which in turn results in emotional discord or anxiety. Such issues frequently respond well to direct discussion regarding the nature of the fears and frustration within the context of an established clinical relationship. It is critical for health-care providers to have sufficient evidenced-based education and emotional support in addressing such concerns early and directly, should the affected individual express such forms of distress. This has been somewhat formalized in the concept of dementia care pathways, which provide frequent review and involvement of psychosocial interventions to mitigate distress inherent in the uncertainty of future care for affected individuals and their families (Samsi & Manthorpe, 2014).
Clearly then, it is critical for these early-stage dementia populations to have access to sufficient and individualized psychoeducation and support during the period of adjustment to diagnosis. Standard care for this stage of illness includes various forms of support groups for the individuals with early-stage dementia and their families (Logsdon, McCurry, & Teri, 2007), with literature reflecting evidence of improved quality of life and decreased family conflicts as a result of interventions. In many areas, such support groups are available through the Alzheimer Society which appear to be an effective means for provision of necessary psychoeducation and support required at this stage of illness. However, a proportion of this early-stage dementia group experience psychological distress of a degree that requires more directed treatment than can be provided in support group formats alone. Recent review of psychotherapeutic interventions in this group by Cheston and Ivanecka (2017) suggests the most effective is short-term group psychotherapy following diagnosis of dementia which affirms benefit for group psychological intervention formats for these early-stage dementia populations.
Nevertheless, there are certain affected individuals who are uncomfortable or unwilling to engage in the group format of psychosocial interventions, and this may place such individuals at risk for mood symptoms due to avoidance of support groups or group therapy formats. One recent Norwegian study of adapted CBT for individuals with early-stage dementia reflected benefit to everyday living and life satisfaction (Saubo, Misvaer, Tonga, Kvigne, & Ulsetin, 2017). Also, there is evidence of efficacy for CBT in early-stage dementia for such issues, which can be combined with cognitive rehabilitation techniques. Although the latter has not demonstrated significant impact on everyday activities of the participants, positive impact on life satisfaction was evident in one study (Kurz et al., 2012). Other forms of psychotherapeutic intervention, including validation therapy, reminiscence therapy, and supportive psychotherapy, have also demonstrated positive benefits although formal studies tend to be based upon small sample groups to date (Birtwell & Dubrow-Marshall, 2017; Gatz et al., 1998). Certainly, the area of efficacy of a variety of psychotherapeutic interventions with early-stage dementia requires further investigation.
In addition to various formats for intervention for psychological factors in early-stage dementia, this phase of dementia can result in behavioral issues consequent to evolving cognitive change. Consequently, it is critical for behavioral modification and cognitive adaptation techniques to be implemented with an understanding of the individual’s cognitive profile including cognitive strengths and weaknesses which can be identified through formal neuropsychological assessment, as discussed earlier. These behavioral interventions may be further supported through the use of assistive devices for symptom management, which may be provided through occupational therapy service, with evidence in literature of demonstrated benefit for both patients and families (Gitlin et al., 2010).
Evolving Behavioral Issues in Mid- to Late-Stage Dementia
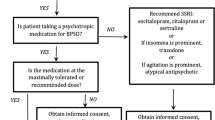
As dementia progresses, the affected individual’s capacity for insight regarding the nature of their condition tends to fade, which often results in decreased identifiable psychological distress in response to disease symptoms. Less demand for psychotherapeutic interventions to address anxiety or grief responses is created, requiring a shift to management of the cognitive and behavioral issues, which are directly impacting the provision of care. However, the increase in objective cognitive impairment, in turn, increases risk for behavioral disturbance (see Fig. 22.1).
During these stages of dementia, psychoeducation for caregivers regarding cognitive factors that may be contributing to problem behaviors is critical in formulating specific behavioral interventions. For example, it would be helpful for caregivers to understand behaviors typical of the type of dementia experienced by the affected individuals. Behavioral observation of the affected individuals and of caregiver responses in conjunction with administration of cognitive screening measures (e.g., MMSE, 3MS, MoCA, Severe Impairment Battery) to those that remain accessible for such formalized testing may be explored. Such an approach allows for understanding of the context of behavioral challenges, including environmental triggers, which may be contributing to behavioral issues. In this context, it is critical to educate caregivers to distinguish affected individuals’ behavioral responses to environment triggers and how they differ from the psychological issues that were previously present in response to grief, anxiety, or depression for earlier-stage illness. Examples of possible behavioral responses triggered by cognitive changes are provided below (see Table 22.1). With greater understanding of these triggers, individualized and appropriate behavioral interventions may be provided in nursing or caregiver settings.
At this stage of illness, there has also been demonstrated positive benefit on behavior in SOMC dementia populations from alternative non-pharmacological treatments including interventions such as art or music therapies (Svansdottir & Snaedal, 2006; Tucknott-Cohen & Ehresman, 2016). It is important to recognize, however, that once again, studies have been limited in this area. Also, for some forms of dementia such as some variants of frontal-temporal dementia, exposure to such interventions may result in increased behavioral disturbances due to overstimulation. Individualized review and treatment planning are essential in determining the outcome of such interventions.
Family Issues in Dementia Care
There is well-documented evidence of increased risk for psychological issues in caregivers, which, in turn, can have negative impacts on care provided to the affected individuals. Meta-analysis of psychological interventions such as CBT with unpaid caregivers has found to have significant benefit for caregiver groups (Brodaty, Green, & Koschera, 2003; Kwon, Ahn, Kim, & Park, 2017). Furthermore, support groups for families and caregivers have demonstrated benefit as well although the benefit for these various psychological interventions tends to be domain specific, addressing only components of psychological needs inherent in caregiving (Sörensen & Conwell, 2011). The research identified a need to find at-risk caregivers with greater specificity, as well as a need for understanding biological and social contributors to the caregiving experience.
Clinicians must recognize the heterogeneity of caregiver responses to those affected by dementia in mid- to late-stage illness. The heterogeneity of responses results in additional challenges for the provision of appropriate and effective interventions. Of considerable importance is the provision of psychoeducation regarding the nature of symptoms experienced by their loved ones. An individualized approach based upon objective evidence of cognitive and/or behavioral issues reflected in objective testing, such as neuropsychological evaluation, cognitive screening, and behavioral measurement, would be most effective in increasing families’ understanding of dementia symptoms, associated interventions, and their functional limitations. Providing evidenced-based education regarding dementia and behavioral challenges and clinician understanding of any misperceptions are essential.
Future Research and Practice Directions
Although this chapter certainly does not represent a comprehensive review of all non-pharmacological interventions for behavioral and psychological issues in dementia, the primary theme of this review suggests the need for coordinated plans for psychological care to be integrated into standard care practices for those with varying stages of dementias and their prodromes. Formal objective cognitive evaluation throughout the course of the disease, as long as accessibility for such testing remains, can take the form of comprehensive neuropsychological assessment in the prodromal and early stages of illness. As dementia progresses, formalized cognitive evaluation may be limited to screening tasks and/or behavioral observation. Regardless, information from mapping cognitive skills for affected individuals can inform non-pharmacological interventions such as CBT and support-based therapies. These therapies are aimed at decreasing emotional distress within the prodromal and early phases of dementia and providing the required behavioral interventions and cognitive compensatory strategies as the disease progresses.
To support such integration of services, there is a need for further exploration of the impact of anxiety or other mood/personality factors within the prodromal phases of dementia (PCD & MCI) to determine the relationship with future conversion to dementia. Greater specificity of subtypes of anxiety symptoms is also required in these groups. Additional research, including longitudinal methodologies into the efficacy of neuro- or cognitive rehabilitation programming for dementia and its prodromes, is required to ensure their appropriate use with this vulnerable population. Furthermore, ongoing investigation of ethical issues within this unregulated industry is required. Finally, longitudinal intervention studies to determine the impact of psychotherapeutic treatments (e.g., CBT, behavioral interventions, cognitive compensatory coaching) are required, both independent of and in combination with pharmacological treatments.
References
Beaudreau, S., & O’hara, R. (2008). Late-life anxiety and cognitive impairment: A review. American Journal of Geriatric Psychiatry, 16(10), 790–803.
Birtwell, K., & Dubrow-Marshall, L. (2017). Psychological support for people with dementia: A preliminary study. Counseling & Psychotherapy Research, 18(1), 79–88.
Brodaty, H., Green, A., & Koschera, A. (2003). Meta-analysis of psychological interventions for care-givers of people with dementia. Journal of American Geriatrics Society, 51(5), 657–664.
Caselli, R., Langlais, B., Dueck, A., Henslin, B., Johnson, T., Woodruff, B., … Locke, D. (2018). Personality changes during the transition from cognitive health to mild cognitive impairment. Journal of the American Geriatrics Society, 66(4), 671–678.
Cerejeira, J., Lagarto, L., & Mukaetova-Ladinska, E. (2012). Behavioral and psychological symptoms of dementia. Frontiers in Neurology, 3(73). https://doi.org/10.3389/fneur.2012.00073
Cheston, R., & Ivanecka, A. (2017). Individual and group psychotherapy with people diagnosed with dementia: A systematic review of the literature. International Journal of Geriatric Psychiatry, 32(1), 3–31.
Devier, D., Pelton, G., Tabert, M., Liu, X., Cuasay, K., Eisenstadt, R., … Devanand, D. (2009). The impact of anxiety on conversion from mild cognitive impairment to Alzheimer’s disease. International Journal of Geriatric Psychiatry, 24(12), 1335–1342.
Gatz, M., Fiske, A., Fox, L. S., Kaskie, B., Kasl-Godley, J. E., McCallum, T. J., & Wetherell, J. L. (1998). Empirically validated psychological treatments for older adults. Journal of Mental Health and Aging, 4(1), 9–46.
Gitlin, L., Winter, L., & Dennis, M. (2010). Assistive devices caregivers use and find helpful to manage problem behaviors of dementia. Geron, 9(3), 408–414.
Gulpers, B., Ramakers, I., Hamel, R., Köhler, S., Oude Voshaar, R., & Verhey, F. (2016). Anxiety as a predictor for cognitive decline and dementia: A systematic review and meta-analysis. American Journal of Geriatric Psychiatry, 24(10), 823–842.
Kurz, A., Thöne-Otto, A., Cramer, B., Egert, S., Frölich, L., Gertz, H. J., … Werheid, K. (2012). CORDIAL: Cognitive rehabilitation and cognitive-behavioral treatment for early dementia in Alzheimer disease: A multicenter, randomized, controlled trial. Alzheimer Disease & Associated Disorders, 26(3), 246–253.
Kwon, O., Ahn, H., Kim, H., & Park, K. (2017). Effectiveness of cognitive behavioral therapy for caregivers of people with dementia: A systematic review and meta-analysis. Journal of Clinical Neurology, 13(4), 394–404.
Lawless, M., Augoustinos, M., & LeCouteur, A. (2017). “Your brain matters”: Issues of risk and responsibility in online dementia prevention information. Qualitative Health Research.
Logsdon, R., McCurry, S., & Teri, L. (2007). Time-limited support groups for individuals with early stage dementia and their care partners. Clinical Gerontologist, 30(2), 5–19.
McAllister, T. W. (1983, May). Overview: Pseudodementia. American Journal of Psychiatry, 140(5), 528–533.
Muller-Spahn, F. (2003). Behavioral disturbances in dementia. Dialogues Clinical Neuroscience, 5(1), 49–59.
Oliveira, A., Radanovic, M., Cotting, P., de Mello, H., Cardoso Buchain, P., Vizzotto, A., … Forlenza, O. (2015). Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: A systematic review. Biomed Research International.
Prince, M., Wimo, A., Guerchet, M., Ali, G., & Wu, Y. (2015). The global impact of dementia: An analysis of prevalence, incidence, cost and trends. Alzheimer’s Disease International.
Robillard, J. M., & Feng, T. L. (2016). Digital health advice: Quality of online articles about the prevention of Alzheimer disease. Journal of Alzheimer’s Disease, 55, 219–229.
Robillard, J. M., Illes, J., Arcand, M., Beattie, B. L., Hayden, S., Lawrence, P., … Jacova, C. (2015). Scientific validity and ethics of online tests for Alzheimer disease. Alzheimer’s Disease and Dementia: Diagnosis, Assessment and Disease Monitoring, 1(3), 281–288.
Roy-Byrne, P. (1996). Generalized anxiety and mixed anxiety-depression: Association with disability and health care utilization. The Journal of Clinical Psychiatry, 57(Suppl 7), 86–96.
Rozzini, L., Chilovi, B. V., Peli, M., Conti, M., Rozzini, R., Trabucchi, M., & Padovani, A. (2009). Anxiety symptoms in mild cognitive impairment. Journal of Geriatric Psychiatry, 24(3), 300–305.
Samsi, K., & Manthorpe, J. (2014). Care pathways for dementia: Current perspectives. Clinical Interventions in Aging, 27(9), 2055–2063.
Saubo, H., Misvaer, N., Tonga, J., Kvigne, K., & Ulsetin, I. (2017). People with dementia may benefit from adapted cognitive behavioural therapy. Forskning, 10–42. https://sykepleien.no/en/forskning/2017/12/people-dementia-may-benefit-adapted-cognitive-behavioural-therapy.
Sherman, D., Mauser, J., Nuno, M., & Sherzai, D. (2017). The efficacy of cognitive intervention in mild cognitive impairment (MCI): A meta-analysis of outcomes on neuropsychological measures. Neuropsychological Review, 27(4), 440–484.
Sörensen, S., & Conwell, Y. (2011). Issues in dementia caregiving: Effects on mental and physical health, intervention strategies, and research needs. American Journal of Geriatric Psychiatry, 19(6), 491–496.
Svansdottir, H. B., & Snaedal, J. (2006). Music therapy in moderate and severe dementia of Alzheimer’s type: A case–control study. International Psychogeriatrics, 18(4), 613–621.
Tampi, R., & Tampi, D. (2014). Anxiety disorders in late life: A comprehensive review. Healthy Aging Research, (14), 3, 1–8.
Tucknott-Cohen, T., & Ehresman, C. (2016). Art therapy for an individual with late stage dementia: A clinical case description. Art Therapy, 33(1), 41–45.
Wimo, A., Guerchet, M., Ali, G., Prina, A., Winblad, B., Jonsson, L., … Prince, M. (2017). The worldwide costs for dementia 2015 and comparisons with 2010. Alzheimers & Dementia, 13(10), 1–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hayden, S. (2018). Non-pharmacological Management of Symptoms of Dementias and Their Prodromes. In: Gatchel, R., Schultz, I., Ray, C. (eds) Handbook of Rehabilitation in Older Adults. Handbooks in Health, Work, and Disability. Springer, Cham. https://doi.org/10.1007/978-3-030-03916-5_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-03916-5_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03915-8
Online ISBN: 978-3-030-03916-5
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)