Abstract
This chapter reviews, in detail, all Parent-Child Interaction Therapy (PCIT) studies for children diagnosed with autism spectrum disorder (ASD) and provides information to improve clinical expertise and inform effective practice. Even though PCIT was originally developed to treat children with externalizing behaviors, there has been increased interest in using this evidence-based treatment (EBT) with children on the spectrum. Two theoretical articles, seven nonexperimental studies, and four quasi-experimental and experimental studies comprise the entire literature of PCIT for children with ASD (PCIT-ASD). These studies lay the groundwork necessary to inform future researchers and clinicians interested in PCIT-ASD.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Parent-Child Interaction Therapy (PCIT)
- Autism spectrum disorder (ASD)
- Adaptations
- Evidence-based treatments
- Disruptive behaviors
This chapter reviews, in detail, all Parent-Child Interaction Therapy (PCIT) studies for children diagnosed with autism spectrum disorder (ASD) and provides information to improve clinical expertise and inform effective practice. Even though PCIT was originally developed to treat children with externalizing behaviors, there has been increased interest in using this evidence-based treatment (EBT) with children on the spectrum. Two theoretical articles, seven nonexperimental studies, and four quasi-experimental and experimental studies comprise the entire literature of PCIT for children with ASD (PCIT-ASD). These studies lay the groundwork necessary to inform future researchers and clinicians interested in PCIT-ASD.
1 Prevalence Rates
In the past 10 years, ASD has emerged as a recognizable and dire public health concern (Baio, 2012). The overall prevalence of ASD is approximately 60 individuals per 10,000 (Newschaffer et al., 2007). However, current prevalence estimates for child populations indicate that between 1 in 88 and 1 in 110 children have ASD (Baio, 2012; Lord & Bishop, 2010). This statistic is particularly jarring as preliminary estimates of healthcare costs for children on the spectrum are nine times higher than other Medicaid-eligible children, with a lifetime societal cost estimate of $3.2 million for each person diagnosed with ASD (Ganz, 2007; Newschaffer et al., 2007).
The current rates of ASD are expected to rise as disparities in diagnosis decrease (Baio, 2012; Lord & Bishop, 2010) yet, even with this increased need, the heterogeneous symptomatology of ASD will continue to present treatment issues for clinicians (e.g., variability in functioning across the spectrum, comorbidities). For example, a single ASD resource classroom serving an entire school is likely to fall short of meeting their students’ diverse needs (Lord & Bishop, 2010). That is, a school district with 10,000 children would expect to serve around 100 children on the spectrum; one elementary school would have about 5 children with ASD who range in age (5–12), language skill (nonverbal to verbal), IQ (severely impaired to superior), and disruptive behavior (none to highly disruptive). Researchers and service providers must understand both the prevalence and heterogeneity of ASD to inform successful intervention implementation efforts and effective clinical practice.
1.1 Disruptive Behaviors
Disruptive behaviors in children on the spectrum are particularly important when conceptualizing ASD-PCIT as many children experience comorbid oppositional behaviors (Kaat & Lecavalier, 2013). Disruptive behaviors encompass a range of externalizing problems ranging from whining and hyperactivity to aggression and defiance. In a large national sample, Mandell, Walrath, Manteuffel, Sgro, and Pinto-Martin (2005) noted that a sizeable number of children were referred for psychological treatment due to disruptive behaviors, of which as many as 40% had a diagnosis of ASD. Specifically, children diagnosed with autism and Asperger’s syndrome most often exhibited physical aggression (19.0% and 20.0% of the sample, respectively). Consistent with disruptive behavior referral rates, Kanne and Mazurek (2011) found that 56% of children and adolescents with ASD in a large sample (N = 1380) were exhibiting mild-to-severe levels of aggressive behaviors. However other researchers have found that 27% of children with autism demonstrated clinically significant externalizing problems (Hartley, Sikora, & McCoy, 2008). As shown above, several studies highlight a subsample of children with ASD present with comorbid disruptive behaviors; with that in mind, we must understand what system provides effective and timely treatment to these children.
1.1.1 Treatment of Disruptive Behaviors in ASD Children
Community-based mental health (CMH) clinics provide a range of comprehensive mental health services to support and treat people within their communities (e.g., outpatient, wraparound, and support groups; Mandell et al., 2005). Many children on the spectrum may receive support for social and academic issues through the education system ; however, they turn to the mental health system for issues related to behavioral problems and comorbid psychiatric conditions (Brookman-Frazee et al., 2009). For instance, the CMH system serves the same percentage of children with ASD as the special education system in the United States (Mandell et al., 2005). Many parents report participating in CMH services with their children prior to the child receiving an ASD diagnosis. In one of the first studies characterizing CMH for children with ASD, Brookman-Frazee, Taylor, and Garland (2010) found that children on the spectrum represent almost 10% of children referred for services due to disruptive behaviors. Additional studies exploring CMH services also reported disruptive behaviors as the most common presenting problem for children with ASD, based on both therapist (84.6%) and parent report (100%; Brookman-Frazee, Baker-Ericzén, Stadnick, & Taylor, 2012; Brookman-Frazee, Drahota, Stadnick, & Palinkas, 2012). CMH clinics are therefore particularly important in identifying children on the spectrum to provide them with effective and timely early interventions (Brookman-Frazee, Baker-Ericzén, et al., 2012).
2 Motivation for Application
The application of PCIT with children with ASD is both practical and theoretically driven. With disruptive behaviors causing significant additional impairments beyond ASD, Kaat and Lecavalier’s (2013) literature review pointed to a dearth of EBTs for ASD that focus on comorbid disruptive behaviors. These children, who sometimes appear at CMH clinics prior to receiving an ASD diagnosis, need quality, time-limited EBTs targeting disruptive behaviors (Brookman-Frazee, Baker-Ericzén, et al., 2012; Kaat & Lecavalier, 2013). In recent years, more and more clinicians have expressed interest in ways to apply PCIT to children on the spectrum. Since 2009, researchers have also shown interest in this topic as PCIT with children on the autism spectrum has been explored at nearly all regional, national, and international PCIT conferences (see references for an extensive list). Adding PCIT-ASD to the set of services available to children on the spectrum would provide parents a unique treatment option directly targeting disruptive behavior problems.
Social contingencies—verbal reinforcement, ignoring, and time-out—constitute a major component of PCIT . Prior assumptions on the salience of social contingencies resulted in the historical exclusion of children on the autism spectrum from participating in PCIT. Awareness that social reinforcement does work with children on the spectrum has allowed for research to investigate the efficacy and effectiveness of PCIT-ASD. Over 40 years of PCIT research supports the effectiveness of PCIT in decreasing disruptive behavior and increasing compliance among typically developing children (see Chap. 14 in this handbook for a review; Brestan & Eyberg, 1998). The current PCIT-ASD literature provides a case for conducting PCIT-ASD with children who display co-occurring disruptive behaviors.
3 PCIT-ASD Research Overview
The goals of this literature review are to survey the current state of knowledge, provide a historical account of the development of PCIT-ASD, and identify limitations in the existing literature. Research will be discussed chronologically within three categories of study design—theoretical, nonexperimental, and quasi-experimental and experimental. The following study overviews integrate the research clearly within a historical context to inform effective clinical practice and guide future research.
3.1 Theoretical
Theoretical research provides a conceptual framework for understanding, analyzing, and designing ways to investigate relationships. It also establishes a foundation on which to build future studies. In the case of PCIT-ASD, theoretical research informs planned changes, otherwise known as adaptations , to effectively apply this intervention with this unique population (Eyberg, 2005). The first two articles discuss the theoretical reasoning and conceptualization to effectively apply PCIT for use with children on the autism spectrum.
3.1.1 Developmental Disabilities
Similar to children on the spectrum, children with developmental disabilities (DD) are at greater risk for exhibiting disruptive behaviors , which greatly impact their social relationships and adaptive functioning. McDiarmid and Bagner (2005) set the stage for the expansion of PCIT to ASD populations through their theoretical discussion of PCIT for children with DD. Specifically, they drew parallels between the primary components of current treatments for children with DD and those used in PCIT (i.e., behavioral approaches, incidental teaching, errorless compliance training, and parent training). For example, the Child-Directed Interaction (CDI) phase of PCIT includes ample incidental teaching and reinforcement of children’s positive behaviors. The Parent-Directed Interaction (PDI) phase of PCIT utilizes an increasingly challenging continuum of commands. PCIT also teaches caregivers contingency management, an important aspect of parent-training programs implemented for children with DD.
McDiarmid and Bagner (2005) noted that standard PCIT requires minimal modifications to elicit behavioral change in children with DD. This approach is successful because PCIT was developed for implementation with children who display varied levels of cognitive and language development. Children do not need to be verbal to participate in PCIT , but they need to understand simple commands. Therefore, the authors recommended that potential developmentally delayed candidates for PCIT have receptive language skills at or above 24 months.
However, children with cognitive delays may receive additional benefit from PCIT when parent-child interactions are used to increase children’s vocabulary and emphasis is placed on ensuring that children comprehend parent verbalizations (McDiarmid & Bagner, 2005). The authors identified three specific caregiver skills developed in the traditional PCIT model that could be adapted to increase beneficial treatment outcomes for individuals with DD—praise, behavioral descriptions, and providing effective commands. Specifically, it was suggested that praise be modified to match the child’s language and/or cognitive abilities to guarantee that the child comprehends the praise. For example, if the child had limited language abilities and could not understand verbal praise, a hug or pat on the back might be a more effective method than verbal praise. Secondly, it was recommended that behavioral descriptions were concise and focused on correct word usage when being used with a child who has a DD. Parents were coached to describe what the child was doing without any speculation, therefore giving the child the ability to understand his or her behaviors in a verbal way. Such behavioral descriptions might also provide the child with the opportunity to learn new vocabulary. Lastly, commands were instructed to be consistent and direct, as these types of commands helped a child with DD more clearly understand behavioral expectations.
To demonstrate the effectiveness of PCIT for children with DD, McDiarmid and Bagner (2005) discussed a case study of a 3-year-old male with moderate intellectual disability and limited language. He was referred for behavior problems that met diagnostic criteria for oppositional defiant disorder and his mother reported significant levels of parenting stress. Standard PCIT protocol was implemented over the course of 14 sessions (5 CDI sessions and 9 PDI sessions). Notably, the child required more repetitions of the PDI procedures than are typically provided in order to fully understand the time-out process. At the end of the treatment, the child’s behavior was rated in the normal range and he no longer met the criteria for oppositional defiant disorder. Additionally, his mother reported significantly lower levels of parenting stress and high satisfaction with treatment.
3.1.2 Conceptualizing PCIT-ASD
Masse, McNeil, Wagner, and Chorney (2007) were the first authors to publish theoretical justification and a conceptual model for the use of PCIT with children on the autism spectrum. Their pioneering study suggested that PCIT could be used as a supplement to other interventions to decrease destructive behaviors and increase functional behaviors in children with autism.
Similar to McDiarmid and Bagner (2005), Masse et al. (2007) explored the theoretical parallels between PCIT and well-known treatments for children diagnosed with ASD. The authors focused on six established ASD treatments (i.e., applied behavior analysis (ABA), the UCLA Young Autism Project, pivotal response training, positive behavior support, TEACCH, and DIR/Floortime). The primary similarity found across many of these ASD interventions was the role of the parent as an agent of change—which is also a hallmark of PCIT (Masse et al., 2007). Enhancing the parent-child bond , promoting generalization, and utilizing intensive compliance training are three major components found in both PCIT and well-known ASD interventions. As emphasized in PCIT, Floortime and TEACCH focus on the importance of the parent-child bond to support child behavior and verbalizations. Both PCIT and pivotal response training promote generalization by using familiar play objects in a comfortable environment. Lastly, like discrete trials seen in ABA, PCIT contains an intensive compliance training component (i.e., PDI). Masse et al. (2007) advocated that this blend of therapeutic techniques found in PCIT may best serve to prime families for more intensive ASD treatments by enhancing the parent-child relationship and increasing child compliance. The authors proposed that because PCIT is so similar to existing treatments for ASD , it could be paired with one or more established ASD interventions to maximize the effectiveness of therapy, especially if PCIT is used as a precursor to exposure to other treatments or environments.
Another important issue that Masse et al. (2007) addressed was the existence of self-stimulatory behaviors in the ASD population and how it could become an important theoretical issue in the CDI phase of PCIT. During this phase, parents address inappropriate or undesirable behaviors by using selective attention. However, it can be unclear if self-stimulatory behaviors should be conceptualized as appropriate or inappropriate, as attempting to use parental attention to modify these frequently occurring behaviors can impede the strengthening of the parent-child relationship—the goal of CDI. Therefore, it was determined that as long as repetitive, self-stimulatory activities were not dangerous, they could be considered appropriate behaviors during CDI. However, addressing self-stimulatory behaviors is still necessary to expand a child’s behavioral repertoire, a crucial component for success in future educational environments. The authors noted that in their clinical experience, parents eventually were able to elicit changes in self-stimulatory behavior through redirection during the PDI phase of PCIT.
3.2 Nonexperimental
Nonexperimental research provides rich and detailed information through the use of case reports. Detailed descriptions of client characteristics, interventions, and treatment outcomes can inform clinical practice and provide a basis for future experimental studies. Conversely, results must be interpreted with caution due to the inherent lack of experimental control. Seven nonexperimental articles explored the use of PCIT-ASD and provided valuable information to guide clinical practice. These varying accounts all yield helpful information considering the heterogeneity of the ASD population.
3.2.1 Cross-Cultural Support
Hatamzadeh, Pouretemad, and Hassanabadi (2010) demonstrated cross-cultural support for the effectiveness of PCIT with children on the autism spectrum using a convenience sample of four males with high-functioning autism ranging in age from 3 to 7. Participants in this sample from Iran met the diagnostic criteria for autism as defined in the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000), exhibited clinically significant disruptive behaviors as measured by the Eyberg Child Behavior Inventory (ECBI; Eyberg & Pincus, 1999), and demonstrated IQ scores above 70. Utilizing an A-B single-case experimental design, Hatamzadeh et al. (2010) treated participants with PCIT in weekly 1-h sessions over an undisclosed period of time. The ECBI was given to participants at six different times: 2 weeks prior to treatment, at the first treatment session, after CDI mastery, after PDI mastery, and during 2- and 4-week follow-ups.
Results suggested that child disruptive behavior decreased significantly following completion of PCIT in high-functioning children with autism (Hatamzadeh et al., 2010). From the initial assessment to follow-up, ECBI problem scores dropped 34%, 53%, 70%, and 54% in the four participants. There were similar decreases in ECBI intensity scores (19–39%) across the same period. Two limitations of these findings included the lack of a stable baseline for disruptive behavior and the reliance on maternal report for all outcome measures. Additionally, the authors’ description of participants lacked sufficient detail to assist clinicians in determining which symptom presentations of ASD are most ideal for PCIT. Thus, the study’s clinical utility was therefore limited.
3.2.2 Community-Based Mental Health Clinic Case Study
To demonstrate the diverse populations within which PCIT is effective, Budd, Hella, Bae, Meyerson, and Watkin (2011) compiled a collection of four case studies delivering PCIT in a CMH clinic. One of these case studies focused on a 5-year-old male with ASD and aggressive behavior who was referred to PCIT by his mother. Although this child was described as high functioning , he experienced speech and motor delays.
The participant and his mother successfully completed both phases of PCIT within 13 sessions. Standard PCIT was tailored to the participant based on recommendations made by McDiarmid and Bagner (2005) and Masse et al. (2007) with some adjustments; for example, therapists instructed the child’s mother to ignore his stereotyped and repetitive behaviors by avoiding any reflections or descriptions while these behaviors occurred. The child also presented with some food aversions. To address the child’s sensory sensitivities to some foods, therapists provided the dyad with play food to practice engaging in appropriate eating behaviors, with his mother providing subsequent positive reinforcement. During treatment, researchers measured child behavior problems using the ECBI, parenting stress using the Parenting Stress Index-Short Form (Abidin, 1995), and caregiver-child interactions and child compliance using the Dyadic Parent-Child Interaction Coding System (DPICS; Eyberg, Chase, Fernandez, & Nelson, 2014).
Following the completion of PCIT, the participant no longer met the criteria for a disruptive behavior disorder. His behaviors had come within normal limits as measured by his ECBI problem score (decreased from 15 to 7) and his ECBI intensity score (decreased from 131 to 84). There were significant decreases in some aspects of his mother’s stress—particularly in her perception of her child and her total stress levels (to within normal limits). In this case example, Budd et al. (2011) illustrated the effective application of PCIT within a CMH setting for a child diagnosed with ASD and presenting with severe disruptive behaviors. They highlighted the complexity of successfully implementing PCIT in real-world service settings. It should be noted, however, that the CMH center in this study was located on a university campus, and therefore possessed additional resources that supported treatment fidelity (e.g., practicum training clinic and research-oriented supervisor) and flexibility (e.g., flexible admission criteria and adjustable attendance policy). Study limitations included a lack of experimental control and insufficient discussion of the contribution of extraneous family stressors during treatment.
3.2.3 Asperger’s Case Study
Given the heterogeneity in clinical presentations of ASD, it is necessary to explore the efficacy of PCIT with children who fall across the breadth of the autism spectrum. Armstrong and Kimonis (2013) conducted a case study examining the efficacy of PCIT for a child diagnosed with Asperger’s disorder , formerly a separate subcategory in prior diagnostic manuals (DSM-IV-TR) that was folded into the broader ASD diagnostic criteria in the DSM-5 (5th ed.; American Psychiatric Association, 2013). Children diagnosed with Asperger’s disorder prior to the DSM-5 (2013) typically displayed higher verbal IQ scores and no delays in early language development (Armstrong & Kimonis, 2013). Motivated by previous findings supporting the application of PCIT in children with ASD (Solomon, Ono, Timmer, & Goodlin-Jones, 2008), Armstrong and Kimonis (2013) examined the efficacy of PCIT with a 5-year-old male experiencing comorbid Asperger’s disorder and disruptive behaviors.
The participant began displaying severe and long-lasting temper tantrums at the age of 2. The participant’s numerous disruptive behaviors (e.g., disobedience, running away, and destroying property) occurred at home, school, and in the community. After multiple diagnoses and numerous medications (i.e., stimulants and antipsychotics), he was referred to a university clinic with the diagnoses of Asperger’s disorder, attention-deficit/hyperactivity disorder (ADHD) , oppositional defiant disorder, and obsessive compulsive disorder. His caregivers and the researchers sought to decrease his disruptive behavior with alternative methods to medication. Therefore, treatment goals consisted of increasing his ability to obtain attention with appropriate behavior, follow directions, and use appropriate communication when upset.
PCIT sessions were conducted with the participant and his mother once per week for 1 h, lasting a total of 16 weeks. Two weeks before treatment, the participant was evaluated for his IQ, behavior, and Asperger’s symptoms. His mother and teacher completed behavior rating scales pretreatment, posttreatment, and at a 3-month follow-up.
From pretreatment to posttreatment, there were clinically significant decreases in the participant’s intensity and problem scores from both parent and teacher reports. His ECBI intensity scores remained relatively stable over time, except for large dips in the first two CDI sessions (i.e., sessions 1–2) and the final two PDI sessions (i.e., sessions 15–16). Alternatively, his ECBI problem scores showed a steady decline across treatment. Three months posttreatment, the participant’s mother reported that his behavior improved at home. His teacher reported that he still had difficulties with inattentive and disruptive behaviors at school, but he had improved over the year. Subsequently, he successfully attended an all-day summer camp and was able to transition into a mainstream first-grade class. A limitation of this case study was that many of the outcome measures were based on parent and teacher report . Additionally, it should be noted that the child experienced multiple atypical environmental stressors over the course of treatment that may have impacted his progress (e.g., deployment of a parent, transition to a new classroom).
3.2.4 Complex Comorbidity Case Study
Agazzi, Tan, and Tan (2013) provided a case example highlighting clinical challenges, adaptations , and recommendations for a 7-year-old male diagnosed with ASD and a variety of comorbidities, including severe behavior problems, sleep problems, developmental delays, hearing impairment, premature birth, and in utero substance exposure. Following assessments by a psychiatrist, developmental pediatrician, neurologist, and pediatric psychologist, the child was found to exhibit clinically significant anxiety issues, ADHD, and conduct problems. He displayed tantrums with verbal and physical aggression toward family members, teachers, and peers , impacting both social and academic activities. Desperate for a strategy to reduce aggression and noncompliance, local physicians and psychologists referred him for PCIT. Treatment consisted of an hour-long session per week for 15 weeks. Standard PCIT was used, and the family completed eight CDI sessions and seven PDI sessions. Notably, therapists prematurely discontinued two consecutive CDI sessions due to the intensity of the child’s aggressive behavior.
There were clinically significant decreases in ECBI intensity scores from the child’s mother and father following the completion of PCIT, but only his father’s scores were maintained at a 3-month follow-up. The ECBI’s problem scores increased, perhaps due to a beginning high tolerance for his disruptive behavior. Three months after treatment, his parents requested three follow-up coaching sessions because they reported that the participant’s disruptive behavior was escalating in the school setting . However, they reported that his behavioral gains remained stable in the home environment. Limitations of this study included a reliance on parent and teacher report, many complications with the participant’s medications , and difficultly implementing time-out at home. First, many assessment measures were used in a multidisciplinary evaluation prior to therapy, but these were not readministered at posttreatment. Inclusion of these measures at follow-up may have complemented the ECBI scores and helped evaluate the effect of treatment. Second, the child was taking several medications that were changed three times over the course of treatment, which may have confounded any behavioral improvements. Third, his parents had significant difficulty executing time-out at home due to the severity of the child’s aggression; this may have provided the child with reinforcing attention for inappropriate behaviors.
3.2.5 Limited Communication Case Study
Lesack, Bearss, Celano, and Sharp (2014) investigated the salience of social reinforcement by applying PCIT to a child with ASD and more severe developmental delays. They adapted components of CDI and PDI to accommodate the 5-year-old male with ASD , severe developmental delay, and significant disruptive behaviors. The child was unable to produce any words with intended meaning. His parents referred him to PCIT due to elevated rates of problem behavior including running away in public, climbing on furniture, tantrums, and self-injurious behaviors. He also displayed self-stimulatory behaviors and lack of eye contact.
Twenty-two treatment sessions were conducted once per week for 45 min each. During CDI, two adaptations were made coinciding with recommendations for PCIT with developmental delays and typically developing children (Lesack et al., 2014). First, the participant regularly engaged in solitary and self-stimulatory play; therefore toys that facilitated this type of play (e.g., eliciting sound and/or lights) were excluded in favor of other PCIT-appropriate toys (i.e., blocks, Mr. Potato Head, and wooden puzzles). Second, his vocal communication was primarily made up of single-syllable vocalizations (e.g., “ba, ba, ba,” “ah”) and stereotypic verbalizations without communicative intent. This impacted his mother’s ability to reflect during CDI and warranted the following guidelines: his mother only reflected vocalizations with communicative intent, she ignored stereotypic vocalizations, and her reflections included both the uttered vocalization (e.g., child says, “ah,” while point to a ball) and the word(s) referencing the accompanying item or action (e.g., his mother reflects, “Ah, you said ball”). These deliberate modifications still offered high-quality attention contingent on appropriate vocalizations while also promoting functional communication.
For PDI, five adaptations were made while carefully considering PCIT’s protocol recommendations (McNeil & Hembree-Kigin, 2010). There was a concern regarding whether the participant could discriminate commands from other types of communication because he did not respond to most vocal communication directed at him. The first two adaptations were made to decrease the likelihood that noncompliance was due to receptive language difficulties, while the final three PDI adaptations were made regarding time-out procedures. First, his name was used to prompt a command (e.g., “Kevin, sit here”) to help him identify the command. Second, a teaching phase including a three-step sequence (i.e., tell, show, do) was implemented to teach the child the appropriate response to specific commands. The participant was given a verbal command with a gestural cue, a verbal command with the request modeled, and a verbal command with a physical prompt. He was required to demonstrate mastery with the target command (i.e., compliance three consecutive times after a verbal or gestural prompt) before time-out was added to PDI. Third, the time-out consequence was limited to certain commands selected to address situations involving task disengagement eliciting aggression (i.e., give his mother a specified item) and safety concerns (i.e., sit in a specific spot next to mother). Fourth, time-out was decreased from 3 min plus 5 s of quiet to a developmentally appropriate 60 s plus 2 s of quiet. Fifth, a holding chair procedure was selected in place of a time-out room due to safety concerns related to the child’s tendency to engage in dangerous behaviors if left alone (Hembree-Kigin & McNeil, 1995).
Researchers relied heavily on the ECBI to track the participant’s progress throughout treatment. His mother filled out the ECBI once during pretreatment, every 2–3 sessions, and once during the last session. The DPICS was also used by researchers to code parent-child interactions and child compliance during sessions.
There were clinically significant decreases in the participant’s ECBI problem and intensity scores from 160 at pretreatment to 106 at the last PDI coaching session. His mother also reported overall decreases in self-stimulatory behavior and dangerous activities (e.g., climbing on furniture and unscrewing light bulbs). A limitation of this study was the lack of collected data regarding the participant’s vocalizations throughout treatment, although his mother reported that his overall number of vocalizations increased. Additionally, because this study only included one child, researchers were limited in their ability to make conclusions about the efficacy of adapted PCIT with an ASD population.
3.2.6 Intellectual Disability Case Study
Because half of the individuals with ASD have a comorbid intellectual disability, Armstrong, DeLoatche, Preece, and Agazzi (2015) conducted a case study using PCIT with a 5-year-old female diagnosed with ASD, intellectual disability, ADHD, and epilepsy. She developed typically until age 2; she then began to experience seizures which caused her motor and verbal development to regress. Her expressive language consisted of five words and she was able to follow simple instructions with gestures. Her problem behaviors included biting, pinching, hitting, and screaming. Armstrong et al. (2015) believed that these were attention-seeking behaviors, making PCIT a suitable treatment option.
PCIT treatment lasted for ten weekly sessions. The standard PCIT protocol was followed, with the addition of visual supports (e.g., visual schedules and social stories) to help the child better understand what was expected of her during treatment. Researchers created a social story to help her comprehend the discipline sequence in PDI. A visual schedule was also utilized to assist with completion of her bedtime routine. Caregiver and teacher reports of child behaviors were collected before initiating treatment, at the final PCIT session, and at 5-month follow-up. Multiple scores on parent and teacher report of child behavior decreased from the clinical to the normal ranges from pretreatment to 5-month follow-up including reductions in child intensity, problems, anxiety, oppositional defiance, and ADHD symptomology. During the follow-up assessment, researchers found that problem behavior had increased since the final PCIT session, perhaps due to the new school year beginning. Her mother reported that the family still utilized PCIT skills and their ECBI problem scores remained in the normal range at follow-up.
The first limitation of note in this study was a change in the families’ insurance, causing an abrupt end to sessions. Second, because the child was simultaneously followed by a psychiatrist throughout the study, the influence of additional therapies and changes in her medications may have impacted her PCIT treatment outcomes.
3.2.7 PCIT and Vocalizations
The previously discussed case studies have primarily focused on the effect of PCIT on disruptive behavior. Hansen and Shillingsburg (2016) introduced a novel outcome measure in their examination of the impact of PCIT-ASD on children’s production of vocalizations. They presented case studies of two males between the ages of 2 and 4 years with ASD diagnoses. Both children demonstrated considerable language impairment on either the Receptive-Expressive Emergent Language Test-Third Edition (REEL-3; Bzoch, League, & Brown, 2003) or the Mullen Scales of Early Learning (MSEL; Mullen, 1995). The first participant was diagnosed with mixed receptive-expressive language disorder at 46 months old. On the REEL-3, he demonstrated severe language impairment (scores ranked within the first percentile or below) in overall language ability and receptive and expressive language skills. The second participant demonstrated very low range scores (first percentile) on the MSEL for both receptive and expressive language.
The participants completed 1- to 2-h weekly PCIT sessions over 12 to 16 weeks. During pretreatment and posttreatment, parent-child interactions were observed and coded using the DPICS. The researchers made modifications in both phases of PCIT to accommodate the children’s language abilities. In the CDI phase, mastery criteria was modified such that caregivers only needed to meet two of the three criteria for positive caregiver behaviors (i.e., ten reflections, ten label praises, ten behavior descriptions) because children with language delays often present fewer opportunities for caregivers to display reflections . Caregivers also were trained to encourage vocalizations and appropriate requests. They were given request training and taught to use stimulus-stimulus pairing strategies to reinforce child vocalizations (e.g., when a child says “mama” the mother responses by saying “mama” and then providing the child with reinforcing stimulus, such as attention). In the PDI phase, three adaptations were made to the standard PCIT protocol. First, PDI sessions did not include time-out. Second, caregivers used a three-step sequence (i.e., tell, show, do) when giving verbal commands. Third, caregivers utilized instructional fading by reinforcing compliance following a verbal or model prompt with either social praise or preferred items/activities (e.g., a snack).
At the conclusion of treatment, there was an increase in the number of positive parenting behaviors exhibited by the children’s caregivers. Additionally, one caregiver displayed decreased engagement in negative parenting behaviors, while the other caregiver showed no change in this area. However, the unique result obtained in this study was the change in child vocalizations from pre- to posttreatment. The first participant was observed vocalizing 48 words following PCIT compared to his 18 vocalizations prior to treatment aggregated across three 5-min activities (i.e., child-led play, parent-led play, and a cleanup activity). The second participant vocalized 50 words at posttreatment as compared to 5 vocalizations at pretreatment aggregated across the three 5-min activities . The authors noted that they did not control for maturation effects or the effect of outside therapies on the children’s development, which limits the conclusions that can be drawn for this study. Even so, the results suggested that modified PCIT can address both behavior and language abilities in children with ASD.
3.3 Quasi-Experimental and Experimental
Quasi-experimental and experimental research uses more rigorous study designs (e.g., single-subject, randomized controlled trials) to empirically establish the efficacy and effectiveness of an intervention. Experimental study designs contain strong internal validity through methods such as random assignment that add necessary support to the establishment of an evidence-based treatment . Nonetheless, as designs become more tightly controlled, internal validity often increases at the expense of external validity, making results less generalizable. Therefore, single-subject designs are experimental designs that can be ideal for the development of an EBT in highly heterogeneous populations (Byiers, Reichle, & Symons, 2012). Four quasi-experimental and experimental articles follow and provide the most rigorous support currently available for PCIT-ASD.
3.3.1 High-Functioning Autism Efficacy
Solomon et al. (2008) provided the first study with a strong experimental design, paving the way for PCIT-ASD research. This study piloted the use of PCIT in children with high-functioning autism using a matched waitlist case-control design. The authors examined the efficacy of PCIT in reducing child disruptive behavior, improving child adaptive and social functioning, reducing parental stress, and increasing shared positive affect between children and their caregivers. Specifically, a positive relationship between shared positive affect and improvements in child and parent functioning was expected.
The sample included 19 males, ranging from 5 to 12 years old, who met the diagnostic criteria for autism (using DSM-IV-TR criteria, the Autism Diagnostic Observation Schedule-Generic [Lord et al., 2000], and the Autism Diagnostic Interview-Revised [Lord, Rutter, & Le Couteur, 1994]) and demonstrated clinically significant externalizing behavior on the Behavioral Assessment System for Children (BASC; Reynolds & Kamphaus, 1992) Parent Rating Scale, BASC Externalizing Scale, or the ECBI Intensity Scale. Additionally, study exclusion criteria included IQ eligibility scores below 70 as well as insufficient receptive and expressive language skills, since insufficient language skills impact treatment (e.g., meeting CDI mastery criteria). Participants were assigned to matched pairs based on age, cognitive level, and severity of behavioral symptoms. After matching, a single subject from each matched pair was randomly selected to receive treatment first, while the other subject served as a control participant.
Treatment participants received an average of 12.5 PCIT sessions. Pretreatment and posttreatment assessments took place 2 weeks before and after treatment and consisted of measures of child behaviors, parenting stress, and the Shared Positive Affect Coding Adapted from Kochanska and Aksan (1995). Parent-child shared affect, measured via behavioral coding, was obtained for the first intervention group only.
Overall, results showed a significant improvement in child adaptability, parent positive affect, and shared positive affect. At posttreatment, there was no significant reduction in parent report of child disruptive behavior in the treatment group, as evidenced by scores on the Conduct Problems, Aggression , and Attention Problems scales of the BASC. However, parent ratings in the intervention group indicated a significant decline on the ECBI problem scale, indicating that parents viewed their children’s behavior as less problematic and more “typical” following treatment even if actual behaviors did not lessen. Additionally, both groups demonstrated decreases in their ECBI intensity scores over the course of the study, suggesting an overall reduction in problem behavior. Children in the treatment group displayed increased flexibility following PCIT, as measured by the BASC Adaptability scale. PCIT was associated with improvements in parent positive affect and shared positive affect, with shared positive affect scores increasing significantly from baseline to mid-treatment and throughout PDI (despite the compliance training component of this phase). Notably, over the course of treatment, there was a fourfold increase in occurrences of parent positive affect being followed by child positive affect. However, in spite of improvements in parent positive affect, parents did not report significant reductions in stress. Finally, results were mixed regarding the relationship between shared positive affect and improvements in child and parent functioning.
Limitations of this study included the small sample size and reliance on parent report for most outcome measures. The participants also represented a limited sample of children (i.e., “high-functioning”) on the autism spectrum, thus preventing wide generalizability of the findings. Although Solomon et al. (2008) noted that treatment fidelity was maintained throughout the study in regular team coding meetings , no formal measure was used. In addition to a measure of treatment fidelity, authors stated that including a control group would improve the reliability of the shared positive affect measure and associated analyses.
3.3.2 Standard Home-Based PCIT Efficacy
Although PCIT has primarily been implemented in clinical settings, emergent research is exploring the use of this treatment in families’ homes (Lieneman, Brabson, Highlander, Wallace, & McNeil, 2017). Masse, McNeil, Wagner, and Quetsch (2016) examined the use of home-based PCIT with children on the autism spectrum. A nonconcurrent multiple baseline design was utilized to demonstrate the efficacy of standard PCIT protocol (both CDI and PDI phases) with this population.
Participants included three 3- to 4-year-old males recruited from local health centers. Inclusion criteria for this study consisted of receptive language skills at a minimum 24-month developmental level on the Peabody Picture Vocabulary Test-III (Dunn & Dunn, 1997), the ability to speak English, a score of 44 or higher on the Autism Behavior Checklist (Krug, Arick, & Almond, 1980), a score of 30 or higher on the Childhood Autism Rating Scale (Schopler, Reichler, & Renner, 1988), and clinically significant disruptive behavior scored within clinical range on the ECBI. The Peabody Picture Vocabulary Test-III, an interviewer-based vocabulary test, assessed receptive language skills. The Autism Behavior Checklist measured parent-reported behaviors indicative of ASD, while the Childhood Autism Rating Scale measured child behavior indicative of ASD via direct behavior observation.
The first participant (age 3) was referred for behavioral concerns comorbid with ASD. The second participant (age 4) was referred for his disruptive behavior; this child received speech, physical, and occupational therapy before participating in PCIT services. The third participant (age 4) was referred by his school because he displayed severe self-stimulatory behaviors, language delays, and aggression. Each dyad was randomly assigned a number of baseline sessions to establish stability.
Researchers followed standard PCIT protocol, but implemented therapy in the home rather than an outpatient clinic. Therapists coached parents via an in-room format due to limitations with technology and other environmental factors. This technique includes sitting behind the caregiver and quietly providing feedback, presenting written coaching statements, and actively ignoring the child’s advances. Researchers hypothesized that there would be improvements in caregiver-child interactions (as measured using the DPICS), decreases in the severity of the presentation of autistic behaviors, reductions in child problem behavior (as measured on the ECBI), increases in child compliance, and a high rate of treatment satisfaction.
Results indicated that child compliance rates increased for two of the three participants from pretreatment to posttreatment and for all three participants from pretreatment to 3-month follow-up. Positive parenting behaviors increased from pretreatment to posttreatment for all participants and also maintained at follow-up assessments. Child behavior problems as measured using the ECBI intensity and problem scores showed significant decreases from pretreatment to posttreatment across all participants. Caregivers also reported a moderate to high level of satisfaction with treatment. Regarding the effect of PCIT on autism-related behaviors, participants generally displayed downward trends across treatment but often remained in the clinical range. The results of this study demonstrated that standard PCIT implemented in-home can be effective in increasing compliance and decreasing behavior intensity for children on the spectrum. It was also suggested that treatment may lead to reduction in the severity of some autism-related behaviors. Limitations of this study include the possible influence of history effects on treatment outcomes (an inherent limitation for nonconcurrent multiple baseline designs) and possible bias due to the raters’ knowledge of study hypotheses.
3.3.3 Randomized Controlled Trial
Ginn, Clionsky, Eyberg, Warner-Metzger, and Abner (2017) conducted the first and only published RCT to date examining the efficacy of PCIT for children with ASD. This experiment utilized only the CDI phase of PCIT to strengthen the relationship between the child and the caregiver. The authors asserted that if the CDI phase was found to be sufficiently effective in improving outcomes for children on the spectrum, it could be a more economic intervention as compared to completing the full PCIT protocol (i.e., CDI, PDI, and additional graduation criteria). Therefore, this initial RCT did not examine the efficacy of the full PCIT model, but provided valuable information regarding the effect of CDI on children with ASD.
The sample consisted of 30 caregiver-child dyads with children between 3 and 7 years old. Inclusion criteria involved a prior ASD diagnosis, cognitive functioning estimated to be at 24 months or higher, and the ability to speak three or more words. Caregivers were also required to meet cutoffs for minimal cognitive functioning. However, children were not required to display disruptive behavior for study inclusion. Of note, children were excluded from participation if they were receiving any additional behavioral therapies or treatments to ensure that outcomes could be attributed to the experimental intervention.
Participants in this study were assigned to either an immediate treatment group or a waitlist group. Each dyad received eight sessions of PCIT, with each session lasting 60–75 min, over a period of 10 weeks. Families on the waitlist received treatment following the immediate treatment group. Sessions followed standard PCIT protocol for the CDI phase, and content of the sessions was matched to the children’s cognitive abilities. Researchers measured children’s receptive language ability, behavior problems, social responsiveness, as well as child and parent behaviors during the DPICS , and parent stress at pretreatment, posttreatment, and 6-week follow-up.
At posttreatment, participants in the immediate treatment group demonstrated significantly more positive parent-following behaviors, fewer negative parent-leading behaviors, and fewer child disruptive behaviors compared to those on the waitlist. Group differences in overall maternal stress were not significant, but parents receiving immediate treatment reported less distress associated with child disruptive behaviors at posttreatment. This finding may suggest greater parental self-efficacy in their behavior management skills following CDI. Children in the two groups did not display significant differences in language ability at posttreatment; this unexpected result may have been due to the majority of the sample (86%) displaying adequate language skills prior to treatment. Similarly, there were no significant group differences in social responsiveness at posttreatment, but children in the immediate treatment group displayed improved levels of social awareness. All treatment gains were maintained at a 6-week follow-up. It should be noted that growth in parenting skills (specifically, reduction in negative “leading” behaviors) significantly mediated improvements in child behavior problems, aligning with previous research on PCIT in typically developing populations (Bagner & Eyberg, 2007).
Although this study provides the most rigorous experimental design in the current PCIT-ASD literature, some limitations can be recognized to inform future research. The sample size used is the largest among all available PCIT-ASD studies but is still relatively small for an experimental treatment study. While the exclusion of participants receiving other behavioral treatments (i.e., ABA) increased internal validity, it conversely limited the generalizability of these findings, as many children with ASD receive multiple behavioral therapies. Furthermore, the measures utilized in this study may not have fully depicted the type of behavior change found in this unique population. For example, future research may benefit from including direct observation of child social behaviors.
3.3.4 Standard PCIT Efficacy
Zlomke, Jeter, and Murphy (2017) examined the efficacy of standard PCIT for children on the autism spectrum. This study included a sample of 17 caregiver-child dyads with children between the ages of 2 and 8 years who demonstrated clinically significant behavior problems and a prior ASD diagnosis. Researchers examined the impact of PCIT on child disruptive behavior, effective parenting skills, and social-emotional symptoms associated with ASD (e.g., social skills and adaptability).
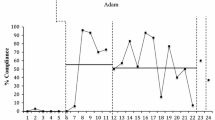
Participating families received treatment weekly for approximately 60–90 min per session, with an average of 19 sessions per dyad. PCIT mastery criteria for some families were modified (as suggested in the PCIT Protocol Manual; McNeil & Hembree-Kigin, 2010) due to limited child verbalizations. The ECBI and DPICS were administered throughout treatment. Measures of general child behaviors, autism symptoms, and attitude toward therapy were administered at pretreatment, mid-treatment, and posttreatment.
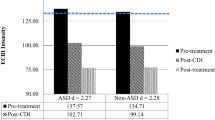
Results indicated statistically significant decreases in ECBI problem and intensity scores as well as measures of externalizing problems and other behavioral symptoms. A significant improvement in child compliance was observed from pre- to posttreatment. Caregivers also displayed significantly more positive following behaviors and fewer negative leading behaviors over the course of treatment, as measured by the DPICS. Notably, decreases were also observed in parent report of children’s hyperactivity, aggression, and atypicality levels. Additional analyses showed improvements in child adaptive functioning, including a significant increase on measures of children’s social skills.
Significant changes on many of the aforementioned outcome measures were observed from pretreatment to mid-treatment, suggesting that the CDI phase of PCIT may be particularly effective in addressing symptoms in children with ASD. This provides support for a strong emphasis on CDI in PCIT-ASD. Additional decreases in caregiver-reported problem behavior intensity and frequency were observed during PDI, highlighting that the PDI phase is still an essential aspect of the intervention when implemented with an ASD population. Limitations to this study include the lack of a control group, absence of coding for some dyads during certain sessions due to a technological error, a relatively small sample size, and uncertain generalizability to children with various levels of functioning on the autism spectrum.
4 Discussion
There has been a proliferation of research into the application of PCIT-ASD within the past decade (for a summary, see Table 16.1), mainly because social contingencies were recognized as reinforcing for children on the autism spectrum (McNeil & Hembree-Kigin, 2010). Additionally, clinicians encounter many children on the spectrum with disruptive behaviors as the primary treatment concern and require an effective and timely treatment option (Mandell et al., 2005); commonly, disruptive behaviors detrimentally impact family functioning as well as impede readiness and success in other comprehensive ASD treatments. Although gaps still exist in the literature, current research supports the application of PCIT for children on the autism spectrum in reducing disruptive behavior. To inform effective PCIT-ASD practice, a discussion on what child is most likely to benefit from PCIT-ASD (e.g., ASD subpopulations and presenting problems) and suggestions for future research is outlined below.
4.1 Inclusion Criteria
4.1.1 Age Range
Most children participating in PCIT-ASD studies ranged in age from 2 to 6 years, the recommended age range for standard PCIT (McNeil & Hembree-Kigin, 2010). A few studies slightly extended the age range of participants to 7-year-olds (Agazzi et al., 2013; Ginn et al., 2017; Hatamzadeh et al., 2010) and 8-year-olds (Zlomke et al., 2017). However, Solomon et al. (2008) sampled children ranging in age from 5 to 12 years, as they viewed the mental age of participants as more relevant to treatment fit than their chronological age. Successfully adapting PCIT to older children requires careful consideration and review of the literature to make appropriate modifications because the size of the child, not just mental age, becomes an issue in the application of PCIT in older populations (Stokes, Scudder, Costello, & McNeil, 2017).
4.1.2 Behavioral Problems
Across most of the PCIT-ASD studies, participants presented with clinically significant behavioral problems . Screening for the presence of disruptive behaviors is the first step in determining if PCIT-ASD is an appropriate treatment option, because not all children on the spectrum exhibit disruptive behavior. Eight of eleven PCIT-ASD studies reported clinically significant ECBI intensity scores at pretreatment, whereas only one study reported scores that did not reach clinical significance for all participants (Hatamzadeh et al., 2010). Although nearly all studies noted the severity of disruptive behavior, future PCIT-ASD research would benefit from routine reporting of pretreatment and posttreatment ECBI scores to examine changes in child behavior. Additionally, future studies should incorporate multiple measures of disruptive behavior to capture a wider array of externalizing behaviors in the ASD population.
4.1.3 Language Impairment
Although children on the spectrum often experience language delays that may contribute to their disruptive behavior, only four studies measured language impairment. Two studies excluded children with receptive language skills below 24 months (Ginn et al., 2017; Masse et al., 2016), while another two studies included children with these lower levels (Hansen & Shillingsburg, 2016; Lesack et al., 2014). Solomon et al. (2008) excluded participants that did not demonstrate sufficient receptive and expressive language to participate in treatment. Lesack et al. (2014), however, looked at the effect of PCIT on increasing children’s vocalizations and found vocalizations to be sporadic and highly variable across treatment. Hansen and Shillingsburg (2016) found increases in the number of child vocalizations from pre- to posttreatment aggregated across three 5-min activities (i.e., 18–48 and 5–50). Overall, language level impacts many areas of treatment, and practitioners should assess language ability in deciding the appropriateness of PCIT for a child with ASD. The more controlled studies examining the effect of PCIT-ASD on disruptive behavior focused only on children with receptive and expressive language ability at or above the level of 24 months. Future research should build upon the work of Hansen and Shillingsburg (2016) and Ginn et al. (2017) by looking at changes in child vocalizations from pretreatment to posttreatment.
4.1.4 Cognitive Functioning
The literature does not provide clear guidance on whether a child with ASD is appropriate for PCIT based on cognitive functioning . Some studies did not specify or exclude participants based upon IQ requirements. For example, Masse et al. (2016) recruited participants with IQ scores both above and below 70. Two studies even included participants with very complex diagnoses (e.g., Armstrong et al., 2015; Armstrong & Kimonis, 2013). It may be easiest for practitioners to apply PCIT-ASD to children with IQ scores above 70 and language skills at 24 months or higher because this population would be expected to require the least amount of adaption from standard PCIT implementation. For example, parents of children with lower language abilities may significantly benefit from PCIT-ASD, but treatment may require more adaptations for use with those experiencing serious language delays . This does not exclude PCIT from use with other ASD subpopulations, as the PCIT-ASD literature provides helpful adaptations for children with limited language skills as well as rich case reports to help guide complex and unique ASD presentations (e.g., Budd et al., 2011). Additional training in implementing these adaptations safely and effectively may be required for clinicians however looking to use PCIT with more severe ASD cases.
4.2 Future Directions
4.2.1 Strengthening the PCIT-ASD Evidence Base
Evidence-based practice (EBP) constitutes an integration of empirical evidence, clinical judgement, and client values (American Psychological Association Presidential Task Force on Evidence-Based Practice, 2006). Guidelines for establishing EBPs help ensure that patients receive the best interventions; however, the definitions of EBPs vary across, even within, divisions of professions (Reichow & Volkmar, 2011). For instance, Reichow and Volkmar (2011) note that the medical community often rates randomized controlled trails (RCTs) as the gold standard of empirical evidence. While RCTs provide strong support for the efficacy of an EBP, Lord et al. (2005) emphasize the difficultly of conducting a highly controlled RCT with the autism community due to treatment switching, contamination (e.g., parents seeking out the most useful treatments), and funding constraints. Future research should add more methodological diversity to the PCIT-ASD literature by adopting more creative and tactful experimental designs such as cross-site replication and partial factorial designs, including underrepresented populations (e.g., geographic location, ethnicity), and examining relationships between child characteristics and treatment outcomes (Lord et al., 2005).
4.2.2 Social Interactions and Child Functioning
The literature provides some support that PCIT improves social interactions for children with ASD, although additional research should include measures to assess these child outcomes (see Chap. 31 in this handbook for more information about assessments for ASD). Four studies evaluated children’s social skills using observational and parent-report measures (Ginn et al., 2017; Masse et al., 2016; Solomon et al., 2008; Zlomke et al., 2017). These procedures should be incorporated in future research to effectively describe sample characteristics and determine any changes that occur in the research sample. Solomon et al. (2008) and Zlomke et al. (2017) used the general measure of child behavior, the BASC which broadly examines a variety of internalizing and externalizing behaviors and symptoms but also includes potentially useful subscales. For example, Zlomke et al. (2017) explored changes in social, emotional, and adaptive functioning on the BASC. Ginn et al. (2017) used the Social Responsiveness Scale (Constantino & Gruber, 2005) to obtain a more in-depth examination of social awareness and other ASD-specific symptoms. Other ASD-specific measures may provide similar benefits to the Social Responsiveness Scale. For instance, Masse et al. (2016) included the Autistic Behavior Checklist to study the impact of PCIT on ASD-related behaviors. The Autism Diagnostic Observation Schedule (Lord et al., 2012), although a diagnostic measure, is a structured, observational measure that researchers may consider using to indicate change over treatment. Furthermore, teacher-report measures complement parent-report measures to depict a fuller picture of children’s functioning in multiple settings, as shown in two studies (Armstrong et al., 2015; Armstrong & Kimonis, 2013).
4.2.3 Adaptations
Adaptations serve an extremely important role in the application of PCIT with children on the autism spectrum. Due to the heterogeneous symptomology of ASD, adapting and tailoring (Eyberg, 2005) the standard PCIT protocol may be necessary to obtain successful treatment outcomes. However, whimsical or unplanned adaptations can undermine treatment integrity and compromise client outcomes. Whether adaptations are minor or significant, they should be made only when necessary and with careful concern for maintaining treatment fidelity. To assist with the development of appropriate adaptations for future PCIT-ASD studies, Table 16.2 outlines changes made in the existing PCIT-ASD research, mapped onto a framework of 12 previously identified content adaptations (Stirman, Miller, Toder, & Calloway, 2013). Forthcoming PCIT-ASD research would benefit from using an adaptation classification system to help identify which adaptations are most salient for specific ASD subpopulations.
5 Conclusion
In summary, PCIT is an emerging and promising treatment for disruptive behavior in children with ASD. Children with ASD may also make improvements in social awareness (Ginn et al., 2017), adaptability (Zlomke et al., 2017), and positive affect (Solomon et al., 2008) after receiving PCIT. The literature has focused on applying PCIT to children with a mental or chronological age of 3–7 years and language ability consistent with a typically developing 24-month-old. However, some clinicians have found improvements in disruptive behavior for lower functioning children when they have made necessary and appropriate adaptations (e.g., Lesack et al., 2014). Future research should add methodological diversity to the PCIT-ASD literature by conducting creative and thoughtful experimental designs, adding evidence to the efficacy and effectiveness of PCIT-ASD, while simultaneously identifying interactions between subgroups of ASD children and PCIT-ASD treatment components to guide timely, effective treatment practice.
References
Abidin, R. (1995). Parenting stress index (3rd ed.). Odessa, FL: Psychological Assessment Resources.
Abner, J. P., Bonney, E., Dugger, J., Lingerfelt, A., Michalk, E., & Suggs, J. (2008, October). CDI: An effective brief intervention for children with autism spectrum disorders? Paper presented at the National Parent-Child Interaction Therapy Conference, Sacramento, CA.
Abner, J. P., Masse, J., & Warner-Metzger, C. (2013). Parent-child interaction therapy with children on the autism spectrum. Expert panel presented at the PCIT International Convention, Boston, MA.
Agazzi, H., Tan, R., & Tan, S. Y. (2013). A case study of parent-child interaction therapy for the treatment of autism spectrum disorder. Clinical Case Studies, 12(6), 428–442. https://doi.org/10.1177/1534650113500067
Allen, K., Harrington, J., & Cooke, C. (2011, September). PCIT for children with autism spectrum disorder and behavior problems. Paper presented at the 2011 Biennial International PCIT Convention, Gainesville, FL.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revised). Washington DC: American Psychiatric Association.
American Psychiatric Association. (2013). diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
American Psychological Association Presidential Task Force on Evidence-Based Practice. (2006). Evidence-based practice in psychology. The American Psychologist, 61, 271–228.
Armstrong, K., DeLoatche, K. J., Preece, K. K., & Agazzi, H. (2015). Combining parent-child interaction therapy and visual supports for the treatment of challenging behavior in a child with autism and intellectual disabilities and comorbid epilepsy. Clinical Case Studies, 14(1), 3–14. https://doi.org/10.1177/1534650114531451
Armstrong, K., & Kimonis, E. R. (2013). Parent-child interaction therapy for the treatment of Asperger’s disorder in early childhood: A case study. Clinical Case Studies, 12(1), 60–72. https://doi.org/10.1177/1534650112463429
Bagner, D., & Eyberg, S. M. (2007). Parent-child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child & Adolescent Psychology, 36(3), 418–429.
Baio, J. (2012). Prevalence of autism spectrum disorders: Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. Morbidity and Mortality Weekly Report. Surveillance Summaries. Volume 61, Number 3. Centers for Disease Control and Prevention.
Brestan, E. V., & Eyberg, S. M. (1998). Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. Journal of Clinical Child Psychology, 27(2), 180–189. https://doi.org/10.1207/s15374424jccp2702_5
Brookman-Frazee, L., Baker-Ericzén, M., Stadnick, N., & Taylor, R. (2012). Parent perspectives on community mental health services for children with autism spectrum disorders. Journal of Child and Family Studies, 21(4), 533–544. https://doi.org/10.1007/s10826-011-9506-8
Brookman-Frazee, L., Baker-Ericzén, M., Stahmer, A., Mandell, D., Haine, R. A., & Hough, R. L. (2009). Involvement of youths with autism spectrum disorders or intellectual disabilities in multiple public service systems. Journal of Mental Health Research in Intellectual Disabilities, 2(3), 201–219. https://doi.org/10.1080/19315860902741542
Brookman-Frazee, L., Drahota, A., Stadnick, N., & Palinkas, L. A. (2012). Therapist perspectives on community mental health services for children with autism spectrum disorders. Administration and Policy in Mental Health and Mental Health Services Research, 39(5), 365–373. https://doi.org/10.1007/s10488-011-0355-y
Brookman-Frazee, L. I., Taylor, R., & Garland, A. F. (2010). Characterizing community-based mental health services for children with autism spectrum disorders and disruptive behavior problems. Journal of Autism and Developmental Disorders, 40(10), 1188–1201. https://doi.org/10.1007/s10803-010-0976-0
Budd, K. S., Hella, B., Bae, H., Meyerson, D. A., & Watkin, S. C. (2011). Delivering Parent-child interaction therapy in an urban community clinic. Cognitive and Behavioral Practice, 18(4), 502–514.
Burrows, C. A., Parlade, M. V., Weinstein, A., Saint-Facile, J. J., & Jent, J. F. (2017, September). Moderators of parent-child interaction therapy for children with autism spectrum disorder and disruptive behavior. Poster session presented at the Parent-Child Interaction Therapy International Biennial Convention, Traverse City, Michigan.
Byiers, B. J., Reichle, J., & Symons, F. J. (2012). Single-subject experimental design for evidence-based practice. American Journal of Speech-Language Pathology, 21(4), 397–414. https://doi.org/10.1044/1058-0360(2012/11-0036
Bzoch, K. R., League, R., & Brown, V. L. (2003). Receptive-expressive emergent language test: examiner’s manual. Austin, TX: Pro-ed.
Chengappa, K., Anderson, R., & McNeil, C. B. (2011, September). PCIT with autism spectrum disorders: A case study. Poster presented at the Parent-Child Interaction Therapy Conference, Gainesville, FL.
Clionsky, L. N. (2012). Child directed interaction training for young children with autism spectrum disorders: The impact on child language, social skills, adaptive skills, and problematic behaviors (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses.
Constantino, J. N., & Gruber, C. P. (2005). The social responsiveness scale (SRS). Los Angeles, CA: Western Psychological Services.
Dunn, L. M., & Dunn, L. M. (1997). Peabody picture vocabulary test (3rd ed.). Circle Pines, MN: American Guidance Service.
Eyberg, S. M. (2005). Tailoring and adapting Parent-Child Interaction Therapy to new populations. Education and Treatment of Children, 28(2), 197–201.
Eyberg, S., Chase, R., Fernandez, M., & Nelson, M. (2014). Dyadic Parent-Child Interaction Coding System (DPICS) Clinical Manual, 4th Edition. PCIT International. Retrieved from https://books.google.com/books?id=A8I5jgEACAAJ.
Eyberg, S. M., & Pincus, D. (1999). Eyberg child behavior inventory and Sutter-Eyberg behavior inventory: Revised professional manual. Odessa, FL: Psychological Assessment Resources.
Ganz, M. L. (2007). The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics & Adolescent Medicine, 161(4), 343. https://doi.org/10.1001/archpedi.161.4.343
Ginn, N. C., Clionsky, L. N., Eyberg, S. M., Warner-Metzger, C., & Abner, J. P. (2017). Child-directed interaction training for young children with autism spectrum disorders: Parent and child outcomes. Journal of Clinical Child and Adolescent Psychology, 46(1), 101–109. https://doi.org/10.1080/15374416.2015.1015135
Hansen, B., & Shillingsburg, M. A. (2016). Using a modified parent-child interaction therapy to increase vocalizations in children with autism. Child and Family Behavior Therapy, 38(4), 318–330. https://doi.org/10.1080/07317107.2016.1238692
Hartley, S. L., Sikora, D. M., & McCoy, R. (2008). Prevalence and risk factors of maladaptive behaviour in young children with autistic disorder. Journal of Intellectual Disability Research, 52(10), 819–829. https://doi.org/10.1111/j.1365-2788.2008.01065.x
Hatamzadeh, A., Pouretemad, H., & Hassanabadi, H. (2010). The effectiveness of parent-child interaction therapy for children with high functioning autism. Procedia Social and Behavioral Sciences, 5(2), 994–997. https://doi.org/10.1016/j.sbspro.2010.07.224
Hembree-Kigin, T., & McNeil, C. B. (1995). Parent-child interaction therapy. New York: Plenum Press.
Kaat, A. J., & Lecavalier, L. (2013). Disruptive behavior disorders in children and adolescents with autism spectrum disorders: A review of the prevalence, presentation, and treatment. Research in Autism Spectrum Disorders, 7(12), 1579–1594. https://doi.org/10.1016/j.rasd.2013.08.012
Kanne, S. M., & Mazurek, M. O. (2011). Aggression in children and adolescents with ASD: Prevalence and risk factors. Journal of Autism and Developmental Disorders, 41(7), 926–937. https://doi.org/10.1007/s10803-010-1118-4
Kochanska, G., & Aksan, N. (1995). Mother-child mutually positive affect, the quality of child compliance to requests and prohibitions, and maternal control as correlates of early internalization. Child Development, 66(1), 236–254. https://doi.org/10.1111/j.1467-8624.1995.tb00868.x
Krug, D. A., Arick, J. R., & Almond, P. J. (1980). Autism behavior checklist. Austin, TX: Pro-Ed.
Lehman C., Wong C., Mendoz-Burcham M., Allen K., & Handen B. (2015, October). PCIT with autism spectrum disorder. Presented at the PCIT International Convention, Pittsburgh PA.
Lesack, R., Bearss, K., Celano, M., & Sharp, W. G. (2014). Parent-child interaction therapy and autism spectrum disorder: Adaptations with a child with severe developmental delays. Clinical Practice in Pediatric Psychology, 2(1), 68–82. https://doi.org/10.1037/cpp0000047
Lieneman, C., Brabson, L., Highlander, A., Wallace, N., & McNeil, C. (2017). Parent-child interaction therapy: Current perspectives. Psychology Research and Behavior Management, 10, 239–256.
Lord, C., & Bishop, S. L. (2010). Autism spectrum disorders: Diagnosis, prevalence, and services for children and families. Social Policy Report. Volume 24, Number 2. Society for Research in Child Development.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Jr., Leventhal, B. L., & DiLavore, P. C. (2000). The autism diagnostic observation schedule – generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule: ADOS-2. Los Angeles, CA: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism diagnostic interview – revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive develop- mental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685.
Lord, C., Wagner, A., Rogers, S., Szatmari, P., Aman, M., Charman, T., … Yoder, P. (2005). Challenges in evaluating psychosocial interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders, (6), 35, 695–708. https://doi.org/10.1007/s10803-005-0017-6
Mandell, D. S., Walrath, C. M., Manteuffel, B., Sgro, G., & Pinto-Martin, J. (2005). Characteristics of children with autistic spectrum disorders served in comprehensive community-based mental health settings. Journal of Autism and Developmental Disorders, 35(3), 313–321. https://doi.org/10.1007/s10803-005-3296-z
Masse, J. (Invited Clinical Workshop, 2015, September). Parent-child interaction therapy with autism spectrum disorders and sensory disorders. Presented at the Parent-Child Interaction Therapy International Biennial Convention, Pittsburgh, PA.
Masse, J. (Invited Keynote Speaker, 2016a, September). Parent-child interaction therapy with autism spectrum disorders. Presented at the 16th Annual Conference on Parent-Child Interaction Therapy (PCIT) for Traumatized Children, University of California, Los Angeles, CA.
Masse, J. (Invited Speaker, 2016b, May). Parent-child interaction therapy with autism spectrum disorders workshop. Presented at the Parent-Child Interaction Therapy Regional Conference, University of California, Irvine, CA.
Masse, J. (Invited Speaker, 2017a, March). Parent-child interaction therapy with autism spectrum disorders workshop. Presented at the 7th Annual Parent-Child Interaction Therapy (PCIT) Conference, Seattle, WA.
Masse, J. (Invited Speaker, 2015, December; 2017b, April). PCIT and autism. Presented on the Oregon state-wide PCIT training call series (~100 participants).
Masse, J., & Abner, J.P. (2011). Views from the frontline of autism spectrum disorders. Paper presented as part of a symposium entitled Tailoring PCIT with Children on the Autism Spectrum (Clionsky, Chair) at the Parent-Child Interaction Therapy Conference, Gainesville, FL.
Masse, J., McNeil, C., Wagner, S., & Chorney, D. (2007). Parent-child interaction therapy and high functioning autism: A conceptual overview. Journal of Early and Intensive Behavior Intervention, 4(4), 714–735. https://doi.org/10.1037/h0100402
Masse, J. J., McNeil, C. B., Wagner, S., & Quetsch, L. B. (2016). Examining the efficacy of Parent-child interaction therapy with children on the autism spectrum. Journal of Child and Family Studies, 25(8), 2508–2525. https://doi.org/10.1007/s10826-016-0424-7
McDiarmid, M., & Bagner, D. (2005). Parent-child interaction therapy for children with disruptive behavior and developmental disabilities. Education and Treatment of Children, 28, 130–141.
McNeil, C. B., & Hembree-Kigin, T. L. (2010). Parent-child interaction therapy (2nd ed.). Boston, MA: Springer. https://doi.org/10.1007/978-0-387-88639-8
Mullen, E. M. (1995). Mullen scales of early learning (pp. 58–64). Circle Pines, MN: AGS.
Newschaffer, C. J., Croen, L. A., Daniels, J., Giarelli, E., Grether, J. K., Levy, S. E., …, Windham, G. C. (2007). The epidemiology of autism spectrum disorders. Annual Review of Public Health, 28(1), 235–258. doi:https://doi.org/10.1146/annurev.publhealth.28.021406.144007
Reichow, B., & Volkmar, F. R. (2011). Evidence-based practices in autism: Where we started. In B. Reichow, P. Doehring, D. V. Cicchetti, & F. R. Volkmar (Eds.), Evidence-based practices and treatments for children with autism (pp. 3–24). Boston, MA: Springer US. https://doi.org/10.1007/978-1-4419-6975-0_1
Reynolds, C. R., & Kamphaus, W. (1992). Behavior assessment system for children (BASC): Manual. Circle Pines: American Guidance Services.
Schopler, E., Reichler, R. J., & Renner, B. R. (1988). Child autism rating scale. Los Angeles, CA: Western Psychological Services.
Solomon, M., Ono, M., Timmer, S., & Goodlin-Jones, B. (2008). The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. Journal of Autism and Developmental Disorders, 38(9), 1767–1776. https://doi.org/10.1007/s10803-008-0567-5
Stirman, S. W., Miller, C. J., Toder, K., & Calloway, A. (2013). Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Science, 8(1), 65. https://doi.org/10.1186/1748-5908-8-65
Stokes, J. O., Scudder, A., Costello, A. H., & McNeil, C. B. (2017). Parent-child interaction therapy with an eight-year-old child: A case study. Evidence-Based Practice in Child and Adolescent Mental Health, 2(1), 1–11.
Zlomke, K., & Greathouse, D. (2017, September). Parents of children with autism spectrum disorder and their readiness for change with PCIT. Poster session presented at the Parent-Child Interaction Therapy International Biennial Convention, Traverse City, Michigan.
Zlomke, K. R., Jeter, K., & Murphy, J. (2017). Open-trial pilot of parent-child interaction therapy for children with autism spectrum disorder. Child and Family Behavior Therapy, 39(1), 1–18. https://doi.org/10.1080/07317107.2016.1267999
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Owen, C.K., Stokes, J., Travers, R., Ruckle, M.M., Lieneman, C. (2018). Parent-Child Interaction Therapy with Children on the Autism Spectrum: A Narrative Review. In: McNeil, C., Quetsch, L., Anderson, C. (eds) Handbook of Parent-Child Interaction Therapy for Children on the Autism Spectrum. Springer, Cham. https://doi.org/10.1007/978-3-030-03213-5_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-03213-5_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03212-8
Online ISBN: 978-3-030-03213-5
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)