Abstract
Tissue engineering (TE) technology combines different aspects of medicine, biology, and engineering to generate, repair, or replace human tissues. In particular, the bone TE approach may be used to induce new functional bone regeneration via the synergistic combination of implanted porous ceramic scaffold with bone marrow stromal cells (BMSC) in vivo. The efficiency of an artificially implanted construct depends on the timely delivery and exchange of nutrients from blood vessels to the BMSC and the contemporary removal of the metabolism waste products. Therefore, the control of the angiogenesis of the microvascular network with proper spatial organization is a key step to obtain tissue regeneration and repair (Carano and Filvaroff, Drug Discov Today 8:980–989, 2003). In this review, we discuss the fundamentals of bone tissue engineering, highlighting the most recent advances in the understanding of the relation between bone formation and vascularization.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Biomineralization (BM) is the widespread and fascinating process by which living organisms form mineral materials, in organized crystals. In the BM process, ions in solution are converted in solid composites (biominerals) thanks to chemical-physical transformations performed by the cellular activity. The process creates sophisticated composite materials, composed of organic and inorganic compounds, with a wide range of properties depending on the many different functions they have to carry out. These include the mechanical functions of exo- and endoskeletons and free-ion regulation or sensing. The research goals in BM are to understand the underlying mechanisms that organisms use to control mineral formation. Only the full comprehension of the morphology and functionality of the biomineralized tissue (i.e., shell, bone, and teeth) will provide the opportunity to mimic nature for the development of bio-inspired materials. Bone provides an important and intriguing model system to investigate the mechanisms involved in BM.
In particular, a deeper comprehension of the BM process is at the basis of tissue engineering (TE) and regenerative medicine developments. Several in vivo and in vitro studies were dedicated to this purpose via the application of 2D and 3D diagnostic techniques. However, due to the complexity of the process, a complete and exhaustive explanation, still far to be reached, requires the synergy of different advanced experimental techniques.
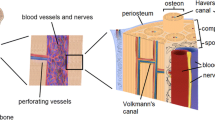
The scaffold plays a crucial role in tissue regeneration since it acts as a guide and it stimulates the bone growth creating living biocomposites [2, 3]. The physical characteristics of the scaffold are represented by a high porosity, maximal surface area for bone growth, and an interconnected pore space, with pores having a sufficiently large size to allow the penetration and diffusion of the blood vessels [4]. In addition, the efficiency of an artificially implanted construct (scaffold) depends on several factors, such as the rate of exchange and removal of substances (as nutrients and metabolism waste, respectively) from the surrounding blood vessels to the bone marrow stromal cell (BMSC, see Fig. 9.1) loaded in the scaffold. The control of the angiogenesis of the vascular network by providing an appropriate template for its spatial organization is a key step to obtain tissue regeneration and repair [1]. In this framework, the formation of vascular networks with tissue-appropriate structure is crucial to tissue engineering (TE) [5, 6]. Thus, a quantitative analysis of the 3D vasculature arrangements in TE is essential to the evaluation of the success of a given strategy. However, to image blood vessels using conventional high-resolution techniques based on X-ray absorption is challenging and often requires the introduction of contrast agents or corrosion casts that generate absorption contrast. In turn, this can result in a nonuniform filling of the vessels and possibly in the need to destroy the rest of the tissue. Complete reliance on absorption contrast thus leads to significant challenges when attempting to simultaneously identify multiple tissue features in a single sample (e.g., microvascular and soft tissue structure).
Recent works [7, 8] demonstrated the capability of synchrotron X-ray phase-contrast micro-tomography (SXPCmT) to visualize the 3D neuronal network architecture and vascular network in the central nervous system at scales spanning from millimeters to hundreds of nanometers, without contrast agent and without a destructive sample preparation, which could lead to data misinterpretation.
The potential of SXPCmT was also confirmed in recent works [9], where it was applied to the visualization and analysis of the 3D microvascular networks in bone-engineered constructs, made of porous ceramic scaffolds loaded with BMSC, in an ectopic bone formation mouse model. Samples seeded and not seeded with BMSC were compared, with or without the use of contrast agents. Thanks to the high quality of the images, it was possible to simultaneously investigate the 3D distribution of both vessels and organic collagen matrix. This approach represents a valuable tool for quantitative studies of angiogenesis in TE and for any other preclinical investigations wherein a quantitative analysis of the vascular network has an important role. In this framework, in the following paragraph, we present the most recent advances in the understanding of the relation between bone formation and vascularization using high-resolution imaging techniques.
2 Vascularization
An active blood vessel network is an essential prerequisite for the development of TE bone and for its integration with the existing host tissue. Various scaffold constructs have thus been developed with the specific goal of promoting angiogenesis, in turn stimulating bone regeneration [10, 11].
Indeed, the greatest amount of new bone formation occurs in the most vascularized areas, whereas an inadequate vascularization at bone defect sites is associated with decreased bone tissue repair and regeneration and has been identified as the main hindrance to successful bone TE (BTE) [11]. Specifically, until the timely onset of construct vascularization (typically on the order of hours to days), seeded cells in an implanted bone TE construct rely on diffusion for the uptake of nutrients (i.e., oxygen, glucose, etc.) and the clearing of metabolic by-products. However this transport mechanism is only efficient over short distances (i.e., less than 200 μm) [12]. These diffusional constraints result in viable cells being located only superficially (i.e., at the periphery of the constructs) and thus limit the success of BTE throughout the entire thickness of the defect. To remedy this obstacle, scientists have proposed several methods to accelerate the onset of neovascularization for survival and integration of BTE with host tissue including (1) scaffold design, (2) inclusion of angiogenic growth factors, (3) in vitro pre-vascularization (i.e., co-culture of endothelial and osteogenic cells), and (4) in vivo pre-vascularization. Although it is still unclear which method is the best for successful in vivo application, a combination of these methods may prove to be most effective.
The achievement of a full understanding of the processes of angiogenesis, osteogenesis, and tissue engineering strategies would offer exciting future therapeutic opportunities for skeletal repair and regeneration in orthopedics.
In this framework, the ability to quantitatively analyze, in three dimensions, the vascular structure in TE is essential for the evaluation of the success of a given strategy. In the following, we will present the imaging techniques most used to evaluate the vascularization in the scaffold.
3 Assessment of BTE Microvessel Detection by Imaging Approaches
Different imaging methods are available to monitor the vascularization. In particular, it is possible to classify the vascular imaging approaches into three main groups: nonoptical techniques (X-ray, magnetic resonance, ultrasound, and positron emission imaging), optical techniques (optical coherence, fluorescence, multiphoton, and laser speckle imaging), and hybrid techniques (photoacoustic imaging) [13]. In the first group, great interest is focused on X-ray imaging methods, which are based on X-ray attenuation by the different tissues and have been successfully used to visualize large blood vessels.
In addition, micro-tomography [14] is able to provide higher-resolution imaging (about 1 μm) than ultrasound (about 30 μm) and MRI (about 100 μm), enabling the visualization and quantification of microvasculature. However, this level of performance can normally be obtained only with the use of contrast agents [15]. A recently emerging method, synchrotron phase-contrast micro-tomography, could help overcome this limitation. This method permits to combine 3D imaging with the analysis of microvascularization and bone microstructure [16], enabling the simultaneous identification of multiple tissue features without using contrast agents. This is due to the increased sensitivity of phase-sensitive X-ray imaging techniques. Indeed, this technique also overcomes the intrinsic limitations of conventional tomographic approaches, often unable to reliably reconstruct the full vascularization network in case of an incomplete filling of microvessels by contrast agents [17]. In addition, conventional characterization techniques have other limitations: 2D imaging, such as histology, yields incomplete spatial coverage with possible data misinterpretation, whereas conventional micro-CT does not achieve sufficient resolution and contrast.
4 X-Ray Phase-Contrast Tomography
The advent of synchrotron radiation supported the development of advanced 3D imaging techniques, such as X-ray phase-contrast tomography. Classical radiography and tomography are based on absorption, and they are well-known tools for imaging objects with hard X-rays. For studies of weakly absorbing materials, such as biological samples, the attenuation in the sample becomes often too small to give detectable contrast. In these cases, a better contrast can be achieved by imaging the phase modulation induced by an object in a coherent beam, which makes phase-based methods attractive for studies of weakly absorbing samples, both in materials and life sciences.
Various techniques have been developed to exploit phase contrast in the X-ray range. They can be classified into five main categories: propagation-based imaging (PBI) methods, analyzer-based imaging (ABI) methods, interferometric methods based on the use of crystals, and grating interferometric and grating non-interferometric methods [18]. These methods differ not only for their experimental setup and for their requirements in terms of the X-ray beam spatial and temporal coherence but also for the nature and amplitude of the provided image signal and for the amount of radiation dose that is delivered to the sample.
A simple yet effective phase-contrast method for hard X-rays is based upon in-line imaging after free-space propagation. When synchrotron X-rays illuminate the sample, variations in the optical path length produce slight local deviations (refraction) of the X-ray beam from its original path (Fig. 9.2).
In absorption radiography, the detector is generally placed close enough to the sample that these variations are unnoticed. On the contrary, when a larger free-space propagation distance is allowed between the sample and detector, the recorded image contains the refraction information in the form of interference fringes appearing at the interfaces between different materials within the sample (edge-enhancement effect) [19]. The fringes thus enhance the visibility of low-absorbing features. Nevertheless, the image captured by in-line propagation always contains mixed absorption and phase effects. Therefore, specific algorithms have to be used to recover the morphological distribution of absorption and phase within the object [20, 21]. Strictly speaking, the quantitative estimation of the object-projected thickness is possible only for mono-elemental samples under monochromatic illumination [20]. On the other hand, although the refractive indices of different soft tissues are very similar for hard X-rays, a semiquantitative phase imaging is still possible taking into account the specific interfaces between tissues [21].
The phase retrieval algorithm is applied to all projections of the tomographic measurements, using the code ANKAphase [20], based on Paganin algorithm (see Chap. 5). The algorithm produces the projected thickness of the object which is proportional to the refractive index decrement if the object is homogeneous. When applied to all tomographic projections, the retrieved phase maps can be fed to a standard filtered back-projection algorithm to obtain phase tomograms.
5 Experience in Bone Tissue Using X-Ray Phase-Contrast Tomography
Conventional X-ray micro-CT is a technique that enables a good visualization of the structure of mineralized bone and of biomaterials, but it fails when attempting to discern soft tissues at high resolutions. On the contrary, SXPCmT, based on propagation-based settings, presents a better soft tissue contrast than conventional CT, clearly discriminating neural and vascular structures [7]. These results enable the investigation of the 3D vascularization of BTE. Detailed imaging and a quantitative description of the complete vascular network in such constructs are indeed crucial for monitoring the relation between bone formation and vascularization, and phase tomography was shown to efficiently discriminate between tissues with similar absorption coefficients (like collagen fibrils and blood vessels) [22,23,24,25]. In addition, the high quality achieved for the 3D images obtained by SXPCmT enabled the extraction of quantitative pieces of information (number, section, and distribution of the vessels crossing each section) for all the different sample preparations. In this framework, we have investigated by SXPCmT the 3D imaging of a vascular network in samples that underwent different preparations. Details on the sample preparation and animal treatment can be found in [9]. In particular, samples seeded with BMSC and perfused by the radiopaque medium MICROFIL were compared with samples seeded with BMSC and unstained, thus obtaining evidence that a high-resolution imaging of the vascular network is also possible without any previous staining treatment (Fig. 9.3a, b).
The scale bar corresponds to 30 μm. (a) Sample A was prepared with MICROFIL®, and it was pre-seeded with BMSCs. The vessels in sample A are rendered in red, the scaffold in blue, and the soft tissue in yellow and green. (b) The 3D volume of sample B is reported. The segmentation renders the vessels in red and the scaffold in blue. The soft tissues were computationally removed from the 3D rendering to highlight the vessel distribution inside the scaffold. Sample B was also pre-seeded with BMSCs, but it was left unstained after the recovery of the scaffold from the animal. (c) Sample C was not BMSC seeded, but it was perfused with MICROFIL. The vessels are rendered in red and the soft tissue in yellow and green (Figure adapted from Bukrreva et al. [9])
In addition, we also investigated samples not seeded with BMSC to study how such seeding affects vascularization process (Fig. 9.3c).
In particular, we have explored a central cube volume of 1.4 mm side, for all the samples. The precision of the selected volume was assured by the precision of the experimental setup, which allowed to illuminate equal portions of the samples. Exploiting the 3D character of the tomographic approach, we systematically analyzed the virtually selected sections (each 640 nm thick) of the samples, perpendicular to any chosen direction, studying the number, diameter, and distribution of the vessels crossing each section. To get insights on the structure of the vascular trees in the recovered implants, we first plotted the number of vessels of the vascular network reaching the system at different depths, and then we investigated the depth distribution of vessels with different sizes.
We observed that the major difference lies in the average number of branches forming the vascular trees. The sample not seeded with BMSC was poorly ramified, while the other three samples displayed thriving trees with many branches. It is important to emphasize that the histological studies performed on samples unseeded with cells also show a poor vascularization (Fig. 9.4).
Histological studies of (right side) scaffold skelite without cells; (left side) scaffold with cells. The arrows indicate vessels marked by MICROFIL. Acquisition by Zeiss Axiovert 200 M. sk skelite, ft fibrous tissue, b bone tissue, m MICROFIL; 40×, scale bar 100 μ micron. (Figure adapted from Bukrreva et al. [9])
Even though SXPCmT was able to visualize the 3D vascularization network inside the scaffold without any sample sectioning and preparation, the use of a coherent, highly brilliant X-ray synchrotron source was mandatory in order to achieve a high image quality with sub-micrometer spatial resolution.
This could certainly limit a possible future use of this technique in the clinical routine; however, this remains a highly valuable experimental approach in preclinical researches such as those involving the investigation of the vascularization process in different scaffolds.
6 Imaging Vascular Segmentation Method
SXPCmT provides an excellent investigation tool for soft tissues, in particular the mapping of the cellular and vascular distribution in biological samples without any casting preparation and with resolution in the 1–10 μm range [7]. Moreover, the capability to distinguish the vascular network without contrast agents has already been demonstrated [7, 26, 27], for example, in the case of the liver or for tumors and for the central nervous system [7, 27, 28]. Even in the visual inspection of tomography data, image segmentation is a crucial step for obtaining quantitative information. In particular, the purpose of any segmentation method is to classify the voxels of a particular feature in order to further assess significant parameters, thus providing a better visualization of the region of interest. Several approaches exist in order to reach this goal, including intensity- and model-based algorithms [28,29,31].
A simple intensity-based segmentation method, which can be employed, for example, to detect the vascular network, is based on the gray levels of the image, by considering the result of different threshold values in the image histogram. In intensity-based segmentation, indeed, the extraction of the voxels to be assigned to the different features (e.g., to the vessels) is based on the analysis of the image histogram. In particular, the image histogram is characterized by a multimodal distribution with slightly asymmetric tails on both sides of the modal value. It is easy to recognize that the main peak is to be assigned to the scaffold, so that it should not to be included in the segmented volume if we want to isolate only the vessels. On the other hand, voxels compatible with vessel lumen or walls and connective tissues have to be included and are located on gray levels identified by two small peaks at both sides of the main one, respectively. The result of the threshold application to the whole tomographic volume is shown in Fig. 9.5. Segmentation is able to reproduce the spatial arrangement of the different features in the vascular network, and it is possible to skeletonize and quantify the different features.
Unfortunately, the usage of a simple intensity approach presents several drawbacks.
Since no assumption on the continuity of the detected structure is considered, voxels with a local contrast decrease will not be included even though they represent part of the vessel.
In order to overcome this limitation, “undecided” voxels can be attached to segmented ones using different approaches [32]. Overall, intensity-based segmentation provides a good starting point to obtain fast and quantitative results.
7 Conclusions
SXPCmT is able to visualize the 3D vascularization network inside the scaffold without any sample sectioning and preparation. However, in order to achieve a higher image quality with sub-micrometer spatial resolution, the use of a coherent, highly brilliant X-ray synchrotron source was mandatory. While this could certainly limit a possible future use of this technique in the clinical routine, PCmT remains a highly valuable experimental approach in preclinical researches such as those involving the investigation of different scaffold vascularizations. We therefore propose our approach as a tool for angiogenesis studies in TE and for any other preclinical investigations where the quantitative analysis of the vascular network is required.
References
Carano RA, Filvaroff EH (2003) Angiogenesis and bone repair. Drug Discov Today 8:980–989
Hench LL, Polak JM (2002) Third-generation biomedical materials. Science 295:1014–1017
Cancedda R, Dozin B, Giannoni P, Quarto R (2003) Tissue engineering and cell therapy of cartilage and bone. Matrix Biol 22:81–91
Quarto R et al (2001) Repair of large bone defects with the use of autologous bone marrow stromal cells. NEJM 344:385–386
Francis ME, Uriel S, Brey EM (2008) Endothelial cell–matrix interactions in neovascularization. Tissue Eng Part B Rev 14(1):19–32
Francis-Sedlak ME, Moya ML, Huang JJ, Lucas SA, Chandrasekharan N, Larson JC, Cheng MH, Brey EM (2010) Collagen glycation alters neovascularization in vitro and in vivo. Microvasc Res 80(1):3–9
Fratini M, Bukreeva I, Campi G, Brun F, Tromba G, Modregger P et al (2015) Simultaneous submicrometric 3D imaging of the micro-vascular network and the neuronal system in a mouse spinal cord. Sci Rep 5:8514
Cedola A, Bravin A, Bukreeva I, Fratini M, Pacureanu A, Mittone A, Massimi L, Cloetens P, Coan P, Campi G, Spanò R, Brun F, Grigoryev V, Petrosino V, Venturi C, Mastrogiacomo M, Kerlero De Rosbo N, Uccelli A (2017) X-ray phase contrast tomography reveals early vascular alterations and neuronal loss in a multiple sclerosis model. Sci Rep 7:5890
Bukrreva I et al (2015) High-resolution X-ray techniques as new tool to investigate the 3D vascularization of engineered-bone tissue. Front Bioeng Biotechnol 3:133
Kanczler JM, Oreffo RO (2008) Osteogenesis and angiogenesis: the potential for engineering bone. Eur Cell Mater 15:100–114
Das A, Botchwey E (2011) Evaluation of angiogenesis and osteogenesis. Tissue Eng Part B Rev 17(6):403–414
Muschler GF, Nakamoto C, Griffith LG (2004) Engineering principles of clinical cell-based tissue engineering. J Bone Joint Surg Am 86-A(7):1541–1558
Upputuri PK et al (2015) Recent developments in vascular imaging techniques in tissue engineering and regenerative medicine. Biomed Res Int 2015:783983
Barbetta A, Bedini R, Pecci R, Dentini M (2012) Role of X-ray microtomography in tissue engineering. Ann Ist Super Sanita 48:10–18
Langer M, Prisby R, Peter Z, Guignandon A, Lafage-Proust MH, Peyrin F (2011) Simultaneous 3D imaging of bone and microstructure in a rat model. IEEE Trans Nucl Sci 58:139–145
Giuliani A, Mazzoni S, Mele L, Liccardo D, Tromba G, Langer M (2017) Synchrotron phase tomography: an emerging imaging method for microvessel detection in engineered bone of craniofacial districts. Front Physiol 8:769
Fei J, Peyrin F, Malaval L, Vico L, Lafage-Proust MH (2010) Imaging and quantitative assessment of long bone vascularization in the adult rat using microcomputed tomography. Anat Rec 293:215–224
Bravin A, Coan P, Suortti P (2013) X-ray phase-contrast imaging: from pre clinical applications towards clinics. Phys Med Biol 58:R1–R35
Wilkins SW, Gureyev TE, Gao D, Pogany A, Stevenson AW (1996) Phase-contrast imaging using polychromatic hard X-rays. Nature 384(6607):335
Paganin D, Mayo SC, Gureyev TE, Miller PR, Wilkins SW (2002) Simultaneous phase and amplitude extraction from a single defocused image of a homogeneous object. J Microsc 206(1):33–40
Beltran MA, Paganin DM, Uesugi K, Kitchen MJ (2010) 2D and 3D X-ray phase retrieval of multi-material objects using a single defocus distance. Opt Express 18(7):6423–6436
Campi G, Fratini M, Bukreeva I, Ciasca G, Burghammer M, Brun F, Tromba G, Mastrogiacomo M, Cedola A (2015) Imaging collagen packing dynamics during mineralization of engineered bone tissue. Acta Biomater 23:309–316
Albertini G, Giuliani A, Komlev V, Moroncini F, Pugnaloni A, Pennesi G et al (2009) Organization of extracellular matrix fibers within polyglycolic acid-polylactic acid scaffolds analyzed using X-ray synchrotron-radiation phase-contrast micro computed tomography. Tissue Eng C Methods 15:403–411
Giuliani A, Manescu A, Langer M, Rustichelli F, Desiderio V, Paino F et al (2013) Three years after transplants in human mandibles, histological and in-line HT revealed that stem cells regenerated a compact rather than a spongy bone: biological and clinical implications. Stem Cells Trans Med 2:316–324
Cedola A, Campi G, Pelliccia D, Bukreeva I, Fratini M, Burghammer M, ... & Sodini N (2013). Three dimensional visualization of engineered bone and soft tissue by combined x-ray micro-diffraction and phase contrast tomography. Phys Med Biol 59(1):189
Mittone A, Ivanishko Y, Kovalev S, Lisutina P, Lotoshnikov M, Tkachev S, Tkacheva M, Crippa L, Dmitriev V, Bravin A (2018) High resolution hard X-ray 3D mapping of a Macaca fascicularis eye: a feasibility study without contrast agents. Phys Med 51:7–12
Lang S, Müller B, Dominietto MD, Cattin PC, Zanette I, Weitkamp T et al (2012) Three-dimensional quantification of capillary networks in healthy and cancerous tissues of two mice. Microvasc Res 84(3):314–322
Ciasca G, Sassun TE, Minelli E, Antonelli M, Papi M, Santoro A, Giangaspero F, Delfini R, De Spirito M (2016) Nano-mechanical signature of brain tumours. Nanoscale 8(47):19629–19643
Müller B, Beckmann F, Huser M, Maspero F, Szekely G, Ruffieux K et al (2002) Nondestructive three-dimensional evaluation of a polymer sponge by microtomography using synchrotron radiation. Biomol Eng 19(2):73–78
Pham DL, Xu C, Prince JL (2000) Current methods in medical image segmentation. Annu Rev Biomol Eng 2(1):315–337
Massimi L et al (2016) Characterization of mouse spinal cord vascular network by means of synchrotron radiation X-ray phase contrast tomography. Phys Med 32:1779–1784
Atwood RC, Lee PD, Konerding MA, Rockett P, Mitchell CA (2010) Quantitation of microcomputed tomography-imaged ocular microvasculature. Microcirculation 17(1):59–68
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fratini, M. (2018). The Challenge of the Vascularization of Regenerated Tissues. In: Giuliani, A., Cedola, A. (eds) Advanced High-Resolution Tomography in Regenerative Medicine. Fundamental Biomedical Technologies. Springer, Cham. https://doi.org/10.1007/978-3-030-00368-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-00368-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00367-8
Online ISBN: 978-3-030-00368-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)