Abstract
Modern TRUS technology has significantly evolved and is absolutely not at the same level as it was a decade ago. Nowadays, since prostate biopsy continues to rely on real-time TRUS image guidance and TRUS is the most effective imaging modality in the outpatient clinic in the urological field, we must re-think the contemporary role and techniques of TRUS to improve the management of prostate cancer.
Especially, new technology, such as the multi-parametric functions of TRUS, real-time three-dimensional imagery, simultaneous bi-plane TRUS, US contrast enhancer, image-fusion technology, various ablative energy techniques available using TRUS guidance, multi-planar display, and device tracking systems, would support the several specific aims of focal therapy for prostate cancer.
Real-time TRUS remains an essential technology to support the diagnosis and characterization of cancer, intra-operative targeting and monitoring, and follow-up surveillance after focal therapy. For developing protocol for meaningful focal therapy of prostate cancer in urological field, era of TRUS renaissance may come.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Introduction
Prostate cancer death rates in the United States declined in the early 1990s [1]. Many physicians have pointed out that the introduction of prostate-specific antigen (PSA)-based prostate cancer screening was followed by subsequent dramatic reductions in prostate cancer mortality. Although few have mentioned the role of transrectal ultrasound (TRUS) in contributing to this phenomenon, it is noteworthy that systematic prostate biopsy guided by TRUS, reported by Hodge in 1989 [2], spreads simultaneously with the widespread use of PSA. Unfortunately, however, current routine practitioners (mainly urologists) may not use TRUS as an important tool for image-targeted biopsy and intervention but only for simple delivery of the prostate biopsy needle toward the sextant portion of the prostate, even though TRUS-guided targeted biopsy from TRUS suspicious lesions is highly recommended in the guidelines of multiple organizations worldwide [3]. Modern TRUS technology has significantly evolved and is absolutely not at the same level as it was a decade ago. Nowadays, since prostate biopsy continues to rely on real-time TRUS image guidance and TRUS is the most effective imaging modality in the outpatient clinic in the urological field, we must rethink the contemporary role and techniques of TRUS to improve the management of prostate cancer. Especially, new technology related with modern TRUS, such as the multiparametric functions of TRUS, real-time three-dimensional imagery, simultaneous biplane TRUS, US contrast enhancer, image fusion technology, various ablative energy techniques available using TRUS guidance, multi-planar display, and device tracking systems, would support the several specific aims of focal therapy for prostate cancer.
The diagnostic and staging process of prostate cancer has multiple steps. In addition to both digital rectal examination (DRE) and PSA, improved quality of imaging to visualize suspicious lesions is vital to enhance detection as well as to better characterize the cancer. Evolving functions of TRUS have significantly contributed to this. Modern imaging can improve the process of prostate cancer diagnosis and staging, through the ability to localize and characterize lesions and to guide precise targeting [4]. Every effort to decrease sampling error has been critical for the precise characterization of prostate cancer, as routine prostate biopsy in current practice may be called “image-blinded” prostate biopsy [3]. Also, importantly, although some criticize that imaging is operator dependent, it has to be said that any interventional procedure or surgery is operator dependent. Especially, in image-guided surgery such as the focal therapy of prostate cancer, imaging technique is in fact an essential part of the surgical technique. Preoperative accurate localization of the cancer and intraoperative precise targeting of it are vital for establishing an effective focal therapy of the prostate cancer [5, 6]. Intraoperative TRUS guidance remains the most effective imaging modality to guide intraprostatic targeting and has been most familiar in urological outpatient practice as well as in the urological operation room.
This chapter focuses on the contemporary role of TRUS for the effective management of prostate cancer with focal therapy.
5.2 Technical Aspects of TRUS
5.2.1 Cancer Diagnosis, Characterization, and Staging
TRUS has improved knowledge of prostate zonal anatomy and internal prostate architecture. The technique is operator dependent, as the quality of this modality is related to the operator’s knowledge and experience. The majority of prostate cancers originate from the peripheral zone [7], in which typical clinically significant nodules can be characterized as a hypoechoic appearance in comparison to the homogeneous echotexture of normal glandular tissue in the peripheral zone. Ultrasonographers define brighter ultrasound images from a stronger ultrasound reflector (due to its heterogeneous structure) as hyperechoic, while darker ultrasound images from a weaker ultrasound reflector (due to its homogeneous structure) are known as hypoechoic; and lesions with an ultrasound appearance similar to the adjacent tissue are referred to as isoechoic. As a higher Gleason score cancer has less normal glandular structure, the ultrasound image of the lesion is likely to be more hypoechoic from benign glands, although the issue is that the prostate has several benign structures with a hypoechoic appearance which mimic hypoechoic cancer.
Biopsies taken from TRUS suspicious lesions are almost twice as likely to show cancer as when no lesion is visible [8]. These cancers in targeted biopsy from TRUS-visible lesions have a significantly higher grade (Gleason score 7 or greater) when compared to those from TRUS-invisible lesions (69 % vs. 28 %, p < 0.001). Similarly, biopsies from TRUS-visible lesions had a greater median percent of the core involved with the cancer in comparison to TRUS-invisible lesions (50 % vs. 10 %, p < 0.001). Therefore, the cancers in targeted biopsy from TRUS-visible lesions are more clinically significant. In a Canadian clinical setting study (n = 982), logistic regression analysis revealed that a TRUS-visible lesion is the most important independent predictor of prostate cancer detection (odds ratio [OR], 2.47; 95 % confidence interval [CI], 1.91–3.2), followed by DRE (OR, 2.29; 95 % CI, 1.72–3.06; p < 0.01), as well as of high-grade cancer detection [9].
On the other hand, diffuse tumors and clinically insignificant small tumors may obscure the normal glandular tissue or appear isoechoic because of the lack of contrast with adjacent normal glandular tissue. The difference of the echotexture of a lesion in ultrasound is dependent on how much different the anatomical structure of the lesion is from that of the adjacent tissue. The transition zone of the prostate is the origin of benign prostatic hyperplasia (BPH) and approximately 15–20 % of prostate cancers [10]. Fibromuscular tissue in the anterior fibromuscular stroma and BPH nodules in the transition zone are also likely to be characterized as hypoechoic. Therefore, the challenge is to diagnose the transition zone cancer with a single use of conventional grayscale TRUS. When there is ultrasound interference such as prostatic calculi or calcified corpora amylacea, the anterior part of the interface has poor image resolution due to the acoustic shadow from the interface.
The hypoechoic appearance of an area is often multiple in a prostate and is not a specific sign of cancer. Various benign prostate tissues of age-related physiological changes and zone-dependent biological differences mimic the cancerous hypoechoic lesion. These include BPH nodules, prostatic inflammation, glandular ectasia, cystic lesions, and so on. Importantly, the operator must be careful about the anisotropic effect (mimicking hypoechoic, but being an artifact), which is often seen in the posterior-lateral edge of the prostate. When an ultrasound beam hits the prostate lateral border in a tangential direction near the neurovascular bundle, a significant part of the ultrasound beam may be reflected in other directions, resulting in the attenuation of the ultrasound beam reflected back to the probe; this causes the posterior-lateral edge of the prostate to mimic the hypoechoic area as an artifact.
Taken together, the obvious limitation of conventional grayscale TRUS in identifying the hypoechoic lesion is that it is highly dependent on operator experience and ultrasound technology. However, in the hands of an expert in TRUS, the higher-grade and larger cancer can be more often visualized by grayscale TRUS, to better characterize clinically significant cancer [4, 5, 11]. As such, cooperation with the uroradiologist or expert ultrasonographer in TRUS imaging would be essential for establishing a meaningful clinical team for a focal therapy program [12].
The higher the frequency of the ultrasound beam, the higher the resolution is in the image but with less penetration in ultrasound wave delivery. For prostate imaging, an ultrasound frequency of 8–12 MHz is typically used for TRUS in consideration of the balance between ultrasound penetration depth (to allow visualization of the entire prostate) and to achieve a reasonable resolution of the image. In order to improve the image resolution with an additional signal, the introduction of a novel US technique using the nonlinear acoustic effects of US interaction either within the prostate or with the use of microbubble contrast agents has opened new prospects for grayscale US in native tissue and also for contrast imaging [13]. In physics, the ultrasound wave becomes distorted through the tissue, and additional frequencies that did not exist in the original wave form are generated. The multiples of the fundamental frequency are called harmonics, and the second harmonic frequency is used for construction of harmonic imaging. Tissue harmonic imaging uses higher frequencies generated on propagation of the US beam through the prostate to improve image visibility of the hypoechoic structure. Nowadays, the use of harmonic grayscale imagery has become routine practice during grayscale TRUS for the experienced ultrasonographer. On the other hand, using contrast harmonic imaging in addition to grayscale harmonic US, Halpern et al. reported that contrast-enhanced TRUS with intermittent harmonic imaging provides a statistically significant improvement in discrimination between benign and malignant biopsy sites (p < 0.05) [14].
Integration of the different functions of imaging potentially enhances diagnostic accuracy. Based on the concept that cancerous tissue has more neovascular supply to feed the cancer cells than normal tissue, the use of color or power Doppler TRUS has become a routine TRUS procedure to enhance the diagnostic accuracy of TRUS with the visualization of increased blood flow in the suspicious lesion [4, 15]. Sauvain et al. reported that targeted biopsy from increased blood flow in any part of the prostate was useful to detect isoechoic areas or lesions in patients with first negative biopsy results, as 57 % (41/72) of patients who had first negative biopsies and power Doppler TRUS-guided targeted biopsy were revealed as having a cancer by targeted biopsy [15]. Nelson et al. [16] also reported that a linear trend of increasing Gleason score was demonstrated with abnormal lesions on grayscale (P < 0.001) and Doppler (P < 0.005) images, where flow signs were strongly associated with Gleason 8–10 lesions. Furthermore, use of contrast agents enhances the Doppler function to identify a suspicious lesion, due to the increased ultrasound reflectors in the vasculature in the lesion. Mitterberger reported in 690 men who underwent contrast-enhanced color Doppler targeted biopsy that contrast-enhanced color Doppler targeted biopsy detected cancers with higher Gleason scores (6.8 vs. 5.4, P < 0.003) and had a better cancer detection rate (11 %, 379/3,417 vs. 5.7 %, 400/6,900, p < 0.001) than systematic biopsy [17]. Interestingly, Morelli et al. reported that vardenafil-enhanced power Doppler ultrasound enables excellent visualization of the microvasculature associated with cancer and can improve the detection rate compared to contrast-enhanced power Doppler ultrasound and the random systematic technique [18]. Analysis of the three methods including (a) vardenafil-enhanced power Doppler ultrasound-guided biopsy, (b) contrast-enhanced power Doppler ultrasound-guided biopsy, and (c) conventional random systematic biopsy showed significantly higher detection in the use of vardenafil (41.2 % vs. 22.7 % and 8.1 %, p < 0.005 and <0.001, respectively). These new techniques suggest that the expanded vasculature or increased ultrasound reflector in the lesion can enhance the diagnostic accuracy of Doppler TRUS. When comparing the Doppler study before and after targeted focal therapy, Ukimura et al. reported that the preoperatively documented signs of increased blood flow in the biopsy-proven cancer decreased or disappeared (and were likely accompanied with shrinking or the disappearance of hypoechoic appearance) suggesting the technical success of targeted focal therapy [4]. When the recent emerging TRUS technologies including Doppler, contrast, harmonic, elastography, computer analysis (such as HistoScanning), or image fusion with other imaging modalities could be integrated in a platform, the so-called multiparametric TRUS would have a key role for prostate imaging to facilitate the focal therapy of prostate cancer [5].
TRUS is also able to visualize the nodule with macroscopic signs of clinical T3 disease, which are associated with the ultrasound signs of bulging mass, discontinuity of capsular echo, disappearance of fat layer in the Denonvilliers space, and involvement of adjacent neurovascular bundles or seminal vesicles by the hypoechoic nodule [19]. Quantitative measurement of the TRUS-measured contact length of the biopsy-proven cancer has the ability to predict microscopic extraprostatic disease [20, 21]. Ukimura et al. reported that in 189 prostatectomy specimens, the contact length, maximum length (mm.) of the portion of the peripheral zone cancer that was in contact with the fibromuscular rim (prostate capsule), was more significantly related to extraprostatic extension than tumor volume, PSA level, and tumor grade. For men who are clinically candidates for radical prostatectomy and have peripheral zone hypoechoic cancers, the combination of ultrasound contact length and PSA value is the best predictor of microscopic extraprostatic extension [20].
TRUS can be used to direct the biopsy sampling from the suspicious area of the extraprostatic disease. Lee et al. reported that among 100 men with systematic biopsy-proven clinically T1–T2 prostate cancer who presented for an opinion for prognosis and treatment options, 27 % were upstaged to pathological T3–T4 disease by TRUS-directed staging biopsy [22]. Okihara et al. reported that among 244 possible candidates of prostatectomy who had a diagnostic biopsy Gleason score of 8 or higher and/or indications of extraprostatic extension (including the seminal vesicles and neurovascular bundles) by DRE or TRUS and underwent staging biopsies using an 18-gauge needle, 31 % (75/244) had positive staging biopsies to provide histological confirmation of locally advanced disease [23].
TRUS-directed staging biopsy has the ability to diagnose histological extracapsular extension and objectifies prognosis and choice of treatment [4, 22, 23].
5.2.2 Novel Techniques of TRUS for Cancer Mapping and Image Fusion
The major challenge for both active surveillance and focal therapy is precise mapping of baseline cancer location and extent. A significant debate continues over the optimal screening biopsy template as well as staging biopsy strategy prior to focal therapy. It is our belief that the key to refining optimal biopsy protocols is not to simply increase the number of cores taken, but rather to improve the quality of each biopsy by real-time image-guided targeting and to document each individual biopsy location to revisit the exact location of the known cancer during possible future interventions [24].
Conventional systematic random biopsies of the prostate are delivered randomly with estimation toward the prostatic sextant template. Current practice with conventional systematic random biopsy, even when extended, does not confidently map out all existing cancers [25, 26].
As the landmark report by Stamey et al. suggested, it is generally accepted that tumors less than 0.5 ml do not contain high-grade cancer and thus could be deemed as clinically insignificant [27]. In order to achieve potential diagnosis of all clinically significant cancer, several groups have proposed transperineal template 5-mm grid-based three-dimensional (3D) mapping (“saturation” biopsy) and introduced this strategy to avoid missing any clinically significant cancer in the prostate prior to focal therapy [28–30]. However, concerns have been raised with this grid-based saturation biopsy method, including the cost, potential biopsy-related complications, and further overdiagnosis of indolent cancer. Furthermore, since a grid-based delivery technique simply relies on the mathematical documentation of points on a grid outside the prostate, there are potential errors between the extraprostatic grid-based documentation and intraprostatic reality of the sampled 3D volume, due to prostatic swelling, needle bending, and/or deformation and shift of the prostate during multiple insertions of the needle. As such, a comprehensive but maximally invasive saturation biopsy method may yield maximum cancer detection but illustrates the limitations of grid-based mathematical 3D mapping biopsy when one simply increases the numbers of biopsies to increase detection [27].
Importantly, more sophisticated 3D cancer mapping strategies require computer-assisted technology including the image capture of real-time TRUS for the 3D volume of the prostate and its reconstruction into a 3D computer model, which can be supported by using either the tracking technology of a 2D TRUS probe or 3D TRUS image-based tracking of the prostate [24]. These emerging technologies also allow the novel and promising opportunity for image fusion-guided prostate biopsy between real-time TRUS and any other imaging modality such as multiparametric MRI that is acquired prior to the time of biopsy.
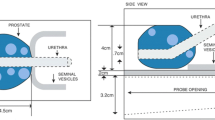
There are several technologies for tracking the TRUS probe in order to reconstruct a 3D computer model of the prostate, including the use of a magnetic tracker, an optical tracker, or robotic mechanical tracking. Generally, these intend to track the location of a 2D end-fire TRUS probe to image and then to reconstruct 3D prostate volume data, in order to register the 3D volume data of a preoperatively acquired prostate (such as by MRI) onto the real location of the prostate at the time of biopsy. This is because the image fusion of the preoperatively acquired MRI data with TRUS requires reliable registration between preoperative and intraoperative conditions. However, there are various challenges to achieve precise registration between the preoperative and the intraoperative reality of the prostate. The intraoperative reality of the prostate may change once the patient moves or when the prostate is deformed or shifted on needle insertion. Real-time monitoring and adjustment of such intraoperative change in location or shape of the prostate with the preoperative condition are essential to achieve reliable image fusion. For this, the most reliable approach is to track the prostate using real-time 3D TRUS and, second, using simultaneous biplane TRUS, since these new TRUS technologies can determine a specific point with coordinates of (x1, y1, z1) in the space of the prostate by documentation of either real-time 3D volume data or cross-sectional two plane (axial and sagittal) data, respectively. In order to achieve precise image fusion, the capability of determining the spatial location of intraprostatic specific points with coordinates of (x, y, z) between preoperative data and intraoperative data is necessary. In contrast, the use of a single end-fire TRUS probe cannot determine an intraprostatic specific point with coordinates of (x, y, z) [31–33]. As long as it uses the tracking system of a single plane TRUS probe, it may have significant error in image fusion once the patient moves or the prostate deforms or shifts at the time of biopsy, since such a tracking system can track the TRUS probe itself but is unlikely to track the prostate. Using a real-time 3D TRUS probe or a simultaneous biplane TRUS probe can track the prostate itself; therefore, these likely achieve a more precise image fusion. Taken together, the use of an image-based tracking system with a 3D TRUS probe or a simultaneous biplane TRUS probe is likely to achieve more precise monitoring and registration of reality of the prostate than the use of a single end-fire TRUS probe with any tracking system. Furthermore, since the prostate is a mobile organ and prostate shape is deformable between preoperative and intraoperative conditions, the use of image fusion with a nonrigid, i.e., elastic, image fusion technique is vital to achieve precise image fusion between them. An image-based tracking system using real-time 3D TRUS with elastic image fusion seems the most reliable registration and localizing system to document biopsy trajectory overlaid onto the image suspicious lesion [31–33].
On the other hand, in order to achieve precise real-time targeting into the suspected lesion, real-time simultaneous parallel display of the real-time TRUS and virtual MRI target is attractive [34, 35]. Since at the time of needle insertion through the prostate it is deformable, real-time 2D TRUS monitoring of such deformation is vital. In the display with both real-time TRUS and virtual fused MRI image, the operator must rely on the real-time TRUS image, but must not look at the virtual, i.e., image-fused image of the MRI, which is not real. The real-time TRUS is more important, since the TRUS image is real and the fused MRI target is virtual. In the authors’ experience, an MRI highly suspicious lesion (categorized as “Score 5” = clinically significant disease) is highly likely to be present and, in the scoring systems of MRI [36], is almost always visible in routine grayscale TRUS. However, when the MR suspected lesion is completely invisible (isoechoic) on TRUS or when a concerted effort has not been made to interpret the real-time US image, biopsy accuracy becomes challenging because real-time guidance then relies exclusively on a virtual image [37, 38]. The operator of MR/US fusion should make every effort to minimize the potential error at each step of the process.
5.2.3 Intraoperative and Postoperative TRUS Monitoring for Focal Therapy When the Cancer Is Visible or Even When It Is Invisible
Contemporary multiparametric TRUS with high-frequency, grayscale, harmonic, Doppler, contrast-enhanced, elastography, and/or computer-assisted analysis ultrasound can display a substantial percentage of biopsy-proven cancers due to a change in the intensity of the returning echoes. Furthermore, in addition to the use of a single 2D image, the use of simultaneous biplane TRUS or 3D TRUS with multi-planar functions improves the acquisition of the 3D volume data of the prostate to retrospectively review any angled tomography and also enables quantitative measurement of the anatomical details in the 3D view to improve reproducibility in measurement and 3D localization of the target without confusion based on possible differences between preoperative and intraoperative conditions.
Image visibility enhanced the precision of targeting and accurate spatial mapping of cancer to help identify more appropriate candidates for focal therapy [4]. When comparing TRUS-visible and TRUS-invisible index lesions using grayscale plus power Doppler study, the cancer-involved core length was 6.1 vs. 1.5 mm (P < 0.001), respectively; furthermore, the percent of core with involved cancer was 48 vs. 16 % (P < 0.001), and the mean Gleason score was 7.0 vs. 6.2 (P < 0.001).
Image visibility of a cancer lesion opens up exciting possibilities including (1) precise biopsy with recorded trajectory, (2) precise therapeutic targeting of the lesion plus margin, and (3) “per-lesion” follow-up after focal therapy [37]. For focal therapy to be successful, we must know where the cancer is. Even if a random biopsy-diagnosed cancer is invisible on imaging (using multiparametric TRUS or even using multiparametric MRI), if that biopsy trajectory is digitally recorded in computerized data, we can now compute the 3D intraprostatic location of the cancer lesion. However, if biopsy trajectories were not recorded, accurately “revisiting” a biopsy-proven cancer lesion would not be feasible. As such, for tissue-preserving targeted focal therapy, sophisticated imaging and/or precise geographically recorded biopsies are necessary, if we want to treat both visible and invisible lesions. When the biopsy-proven cancer lesion was visible with imaging, retargeting of the lesion could be achieved with image guidance. The real challenge is retargeting the cancer-proven lesion that is not identifiable by available imaging. In this situation, we must rely on the (x, y, z) coordinates recorded from the previous biopsy session by computerized techniques to guide the delivery of the retargeting biopsy or ablative probe toward the intended target plus a potential safety margin around the target.
Use of multiparametric TRUS as well as multiparametric MRI data with the aid of MRI/ultrasonography fusion would probably contribute to more sophisticated diagnosis and appropriate treatment of prostate cancer [31–35]; however, given that an imaged lesion is likely to be underestimated or overestimated compared with the true lesion [20, 39, 40], lesion-targeted therapy (instead of hemi-ablative therapy) needs to account for an additional safety margin by calculating the prediction error in imaging studies to ensure that the focal therapeutic zones cover the entire cancer lesion.
To preserve the accuracy of a planned intervention, any image-guided intervention system would require the capture of real-time imaging to constantly update the 3D planning model. The critical importance of real-time TRUS monitoring and corresponding real-time 3D planning model is supported by the successful practices in some of the most investigated real-time TRUS-guided therapeutic modalities, including TRUS-guided cryosurgery, brachytherapy, HIFU (high-intensity focused ultrasound), and photodynamic therapy.
The initial 3D planning models for these technologies have been developed to be adjustable during any time of the intervention, based on the comparison of initially referenced reconstructed 3D images and real-time TRUS imaging. This capability is considered a key feature in achieving the precision and efficacy necessary for focal therapy. In fact, the prostate is a mobile deformable organ and can be swollen or shift from within during the intervention. During therapy guided by real-time TRUS, the real-time image becomes the actual eyes through which the surgeon looks at the surgical field within the prostate. Due to needle insertion or energy delivery into the prostate, the prostate potentially swells and shifts [41]. If at least multiple treatment secession is necessary, without real-time modification of the 3D targeting plan according to the intraoperative swelling and shift during treatment, targeted focal therapy may potentially leave untreated gaps between two adjacent treatment zones. Based on the real-time TRUS monitoring of possible changes in 3D shape of the prostate, intraoperative adjustment of the treatment plan has an impact on achieving precise therapeutic targeting.
Techniques of postoperative follow-up are still evolving in focal therapy. TRUS can document the shrink of the prostate in size in the treated area as well as the disappearance of the biopsy-proven lesion after focal therapy [4]. Documentation of the evidence of the decreased blood flow or change from enhanced to unenhanced signatures between pre- and post-focal therapy could be important evidence for suggesting technical success or possible cancer cell death. Since TRUS is the main imaging technique to visualize and monitor the postoperative change in the urological outpatient clinic allowing surveillance of prostate biopsy to target the preoperatively confirmed cancer lesion as well as the possible multifocal unknown disease in the untreated area, TRUS continues to be of significant importance in the follow-up.
5.3 Conclusion
In conclusion, real-time TRUS remains an essential technology to support the diagnosis and characterization of cancer, intraoperative targeting and monitoring, and follow-up surveillance after focal therapy. For developing protocol for meaningful focal therapy of prostate cancer in urological field, the era of TRUS renaissance may come (Figs. 5.1, 5.2, 5.3, and 5.4).
Case 1: A 66-year-old man having PSA value of 7.47 ng/ml and TRUS-measured prostate volume of 51 g. TRUS with Doppler study identified hypoechoic suspicious lesion in right posterior-lateral aspects with suspicious focal increased blood flow. TRUS-guided targeted biopsy revealed Gleason 3 + 4 = 7 cancer in the TRUS-visible lesion with 9 mm cancer core length
Case 2: A 68-year-old man having PSA value of 3.5 ng/ml and TRUS-measured prostate volume of 53 g. TRUS with Doppler study identified hypoechoic suspicious lesion in left posterior-lateral aspects with suspicious focal increased blood flow. TRUS-guided targeted biopsy revealed Gleason 3 + 3 = 6 cancer in the TRUS-visible lesion with 4 mm cancer core length
Case 3: A 58-year-old man having PSA value of 4.2 ng/ml and TRUS-measured prostate volume of 38 g. Pre-biopsy multiparametric MRI suggested moderate suspicious lesion in the left transition zone in the ADC map and contrast-enhanced i-CAD color-coded image. This lesion corresponded with remarkable focal increased flow in TRUS Doppler study. Targeted biopsy from the TRUS Doppler-visible and ADC/contrast MR-visible lesion revealed Gleason 3 + 3 = 6 cancer with 12 mm cancer core length. Digitally documented 3D TRUS-based mapping biopsy could indicate the precise location of biopsy-proven cancer in the 3D space of the prostate
Case 4: A 59-year-old man having PSA value of 4.1 ng/ml and TRUS-measured prostate volume of 28 g. Pre-biopsy multiparametric MRI suggested highly suspicious lesion in the left peripheral zone in all three functions of MRI including T2-weighted, ADC map, and contrast-enhanced i-CAD color-coded image. This lesion corresponded with remarkable hypoechoic lesion with highly suspicious focal increased flow in TRUS Doppler study. MR/US fusion targeted biopsy from the TRUS-visible and MR-visible lesion revealed Gleason 4 + 3 = 7 cancer with 11 mm cancer length
References
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2009 (Vintage 2009 populations). http://seer.cancer.gov/csr/1975_2009_pops09/. Accessed 20 Aug 2012.
Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142(1):71–4.
Ukimura O, Coleman J, de la Taille A, Emberton M, Epstein J, Freedland S, Giannarini G, Kibel A, Montironi R, Ploussard G, Roobol M, Scattoni V, Jones S. Contemporary role of systematic prostate biopsies: indications, technique, implications on patient care. Eur Urol. 2013;63(2):214–30.
Ukimura O, Abreu AL, Gill IS, Shoji S, Hung AJ, Bahn D. Image-visibility of cancer to enhance targeting precision and spatial mapping biopsy for focal therapy of prostate cancer. BJU Int. 2013;111(8):E354–64.
Bahn D, de Castro Abreu AL, Gill IS, Hung AJ, Silverman P, Gross ME, Lieskovsky G, Ukimura O. Focal cryotherapy for clinically unilateral, low-intermediate risk prostate cancer in 73 men with a median follow-up of 3.7 years. Eur Urol. 2012;62(1):55–63.
Ahmed HU, Hindley RG, Dickinson L, Freeman A, Kirkham AP, Sahu M, Scott R, Allen C, Van der Meulen J, Emberton M. Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol. 2012;13(6):622–32.
McNeal JE. The zonal anatomy of the prostate. Prostate. 1981;2(1):35–49.
Toi A, Neill MG, Lockwood GA, Sweet JM, Tammsalu LA, Fleshner NE. The continuing importance of transrectal ultrasound identification of prostatic lesions. J Urol. 2007;177:516–20.
Trottier G, Roobol MJ, Lawrentschuk N, et al. Comparison of risk calculators from the prostate cancer prevention trial and the European randomized study of screening for prostate cancer in a contemporary Canadian cohort. BJU Int. 2011;108:E237–44.
McNeal JE, Redwine EA, Freiha FS, Stamey TA. Zonal distribution of prostatic adenocarcinoma. Correlation with histologic pattern and direction of spread. Am J Surg Pathol. 1988;12(12):897–906.
Shinohara K, Scardino CSS, Wheeler TM. Pathologic basis of the sonographic appearance of the normal and malignant prostate. Urol Clin North Am. 1989;16(4):675–91.
Ukimura O, Gill IS, Reply from Authors re: Mark Emberton. Tissue preservation may offer a harm-reduction strategy for men with early prostate cancer. Eur Urol. 2012;62:64–6. Eur Urol. 62:66–7.
Lencioni R, Cioni D, Bartolozzi C. Tissue harmonic and contrast-specific imaging: back to gray scale in ultrasound. Eur Radiol. 2002;12(1):151–65.
Halpern EJ, Ramey JR, Strup SE, Frauscher F, McCue P, Gomella LG. Detection of prostate carcinoma with contrast-enhanced sonography using intermittent harmonic imaging. Cancer. 2005;104(11):2373–83.
Sauvain JL, Palascak P, Bourscheid D, Chabi C, Atassi A, Bremon JM, Palascak R. Value of power doppler and 3D vascular sonography as a method for diagnosis and staging of prostate cancer. Eur Urol. 2003;44(1):21–30.
Nelson ED, Slotoroff CB, Gomella LG, Halpern EJ. Targeted biopsy of the prostate: the impact of color Doppler imaging and elastography on prostate cancer detection and Gleason score. Urology. 2007;70:1136–40.
Mitterberger M, Pinggera GM, Horninger W, Bartsch G, Strasser H, Schäfer G, Brunner A, Halpern EJ, Gradl J, Pallwein L, Frauscher F. Comparison of contrast enhanced color Doppler targeted biopsy to conventional systematic biopsy: impact on Gleason score. J Urol. 2007;178(2):464–8.
Morelli G, Pagni R, Mariani C, Minervini R, Morelli A, Gori F, Ferdeghini EM, Paterni M, Mauro E, Guidi E, Armillotta N, Canale D, Vitti P, Caramella D, Minervini A. Results of vardenafil mediated power Doppler ultrasound, contrast enhanced ultrasound and systematic random biopsies to detect prostate cancer. J Urol. 2011;185(6):2126–31.
Lee F, Torp-Pedersen ST, Siders DB, Littrup PJ, McLeary RD. Transrectal ultrasound in the diagnosis and staging of prostatic carcinoma. Radiology. 1989;170:609–15.
Ukimura O, Troncoso P, Ramirez EI, Babaian RJ. Prostate cancer staging: correlation between ultrasound determined tumor contact length and pathologically confirmed extraprostatic extension. J Urol. 1998;159(4):1251–9.
Ukimura O, Magi-Galluzzi C, Gill IS. Real-time transrectal ultrasound guidance during laparoscopic radical prostatectomy: impact on surgical margins. J Urol. 2006;175(4):1304–10.
Lee F, Bahn DK, Siders DB, Greene C. The role of TRUS-guided biopsies for determination of internal and external spread of prostate cancer. Semin Urol Oncol. 1998;16(3):129–36.
Okihara K, Kamoi K, Lane RB, Evans RB, Troncoso P, Babaian RJ. Role of systematic ultrasound-guided staging biopsies in predicting extraprostatic extension and seminal vesicle invasion in men with prostate cancer. J Clin Ultrasound. 2002;30:123–31.
Ukimura O, Hung A, Gill IS. Innovations in prostate biopsy strategies for active surveillance and focal therapy. Curr Opin Urol. 2011;21(2):115–20.
Tareen B, Godoy G, Sankin A, et al. Can contemporary transrectal prostate biopsy accurately select candidates for hemi-ablative focal therapy of prostate cancer? BJU Int. 2009;104:195–9.
Falzarano SM, Zhou M, Hernandez AV, et al. Can saturation biopsy predict prostate cancer localization in radical prostatectomy specimens: a correlative study and implications for focal therapy. Urology. 2010;76:682–7.
Stamey TA, Freiha FS, McNeal JE, et al. Localized prostate cancer. Relationship of tumor volume to clinical significance for treatment of prostate cancer. Cancer. 1993;71(3 Suppl):933–8.
Crawford ED, Wilson SS, Torkko KC, et al. Clinical staging of prostate cancer: a computer-simulated study of transperineal prostate biopsy. BJU Int. 2005;96:999–1004.
Barzell WE, Melamed MR. Appropriate patient selection in the focal treatment of prostate cancer: the role of transperineal 3-dimensional pathologic mapping of the prostate: a 4-year experience. Urology. 2007;70(6 Suppl):27–35.
Onik G, Miessau M, Bostwick DG. Three-dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. J Clin Oncol. 2009;27:4321–6.
Ukimura O, Desai M, Palmer S, Valencerina S, Gross M, Abreu A, Aron M, Gill IS. Three-dimensional elastic registration system of prostate biopsy location by real-time 3-dimensional transrectal ultrasound guidance with magnetic resonance/transrectal ultrasound image fusion. J Urol. 2012;187:1080–6.
Delongchamps NB, Peyromaure M, Schull A, Beuvon F, Bouazza N, Flam T, Zerbib M, Muradyan N, Legman P, Cornud F. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol. 2013;189(2):493–9.
Cornud F, Brolis L, Delongchamps NB, Portalez D, Malavaud B, Renard-Penna R, Mozer P. TRUS-MRI image registration: a paradigm shift in the diagnosis of significant prostate cancer. Abdom Imaging. 2013;38:1447–63.
Ukimura O, Hirahara N, Fujihara A, Yamada T, Iwata T, Kamoi K, Okihara K, Ito H, Nishimura T, Miki T. Technique for a hybrid system of real-time transrectal ultrasound with preoperative magnetic resonance imaging in the guidance of targeted prostate biopsy. Int J Urol. 2010;17(10):890–3.
Pinto PA, Chung PH, Ratinehad AR, et al. Magnetic resonance imaging/ultrasound fusion guided prostate biopsy improves cancer detection following transrectal ultrasound biopsy and correlates with multiparametric magnetic resonance imaging. J Urol. 2011;186:1281–5.
Dickinson L, Ahmed HU, Allen C, Barentsz JO, Carey B, Futterer JJ, Heijmink SW, Hoskin P, Kirkham AP, Padhani AR, Persad R, Puech P, Punwani S, Sohaib A, Tombal B, Villers A, Emberton M. Scoring systems used for the interpretation and reporting of multiparametric MRI for prostate cancer detection, localization, and characterization: could standardization lead to improved utilization of imaging within the diagnostic pathway? J Magn Reson Imaging. 2013;37(1):48–58.
Ukimura O, Gill IS. Reply from authors re: Mark Emberton. Tissue preservation may offer a harm-reduction strategy for men with early prostate cancer. Eur Urol. 2012;62:64–6. Eur Urol. 62:66–7.
Ukimura O. Editorial comment. J Urol. 2013;189(1):91–2.
Mazaheri Y, Hricak H, Fine SW, et al. Prostate tumor volume measurement with combined T2-weighted imaging and diffusion-weighted MR: correlation with pathologic tumor volume. Radiology. 2009;252:449–57.
Dudea SM, Giurgiu CR, Dumitriu D, et al. Value of ultrasound elastography in the diagnosis and management of prostate carcinoma. Med Ultrason. 2011;13:45–53.
Shoji S, Uchida T, Nakamoto M, Kim H, de Castro Abreu AL, Leslie S, Sato Y, Gill IS, Ukimura O. Prostate swelling and shift during high intensity focused ultrasound: implication for targeted focal therapy. J Urol. 2013;190(4):1224–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag France
About this chapter
Cite this chapter
Ukimura, O., Matsugasumi, T. (2015). Role and Technique of Transrectal Ultrasound for Focal Therapy. In: Barret, E., Durand, M. (eds) Technical Aspects of Focal Therapy in Localized Prostate Cancer. Springer, Paris. https://doi.org/10.1007/978-2-8178-0484-2_5
Download citation
DOI: https://doi.org/10.1007/978-2-8178-0484-2_5
Published:
Publisher Name: Springer, Paris
Print ISBN: 978-2-8178-0483-5
Online ISBN: 978-2-8178-0484-2
eBook Packages: MedicineMedicine (R0)