Abstract
The abuse of children can take many forms, although physical and sexual abuses are the forms that are most likely to result in cutaneous abnormalities. In order to effectively and reliably document changes in the skin, the examination must be carefully planned and should be conducted under optimum conditions. Such an examination may include photography as well as the detection of trace evidence by swabbing. This chapter describes these examination methods.
The most commonly observed cutaneous injuries are bruises, but these may have various features that allow the investigator to distinguish between abusive and non abusive causes. Such features may include location, pattern, number, appearance, and variations in apparent age. Occasionally natural medical conditions may cause or contribute to bruising, and these must be recognized as such to allow reliable identification of those unnatural situations. Bite marks are specific injuries that may carry serious connotations of abuse, and they are discussed in some detail especially in respect of the ability to classify them and to apply the examination to the identification of a perpetrator.
Burns and scalds represent a common form of child abuse, and these injuries should necessarily be recognized and adequately recorded and interpreted. They are discussed in detail especially in respect of their value in the investigation of mistreatment. The recognition of scarring as evidence of injury is also described. Finally, it is necessary to recognize the many natural and non abusive conditions and situations that may mimic or be misinterpreted as representing non accidental injury. These are described and documented.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The abuse of children can take many forms (Ellis 1997). Of these, physical and sexual abuse and even neglect can all be reflected in changes appearing in some form in the skin. While emotional abuse does not directly cause cutaneous injury, the secondary effects may be manifested by abnormalities that can be observed in the skin. For example, trichotillomania, possibly associated with emotional abuse, can produce areas of alopecia that may be misinterpreted as abusive hair pulling (Scales et al. 1999). Physical abuse can take many forms and can result in bruising, burns and scalds, patchy alopecia, and ultimately scarring and deformity if prolonged. These will be discussed in detail below. Sexual abuse will be described elsewhere in this text (see Chap. 23, “Pediatric Sexual Abuse”) but can be associated with cutaneous changes around the genitalia as well as bite marks which should be carefully identified and recorded. Neglect, by virtue of increasing the opportunity for skin infections and causing reduced cutaneous integrity, may also produce changes in the skin that need to be recognized for what they are. Severe dermatitis or cutaneous scaly rashes caused by nutritional deficiencies may occasionally represent forms of abuse, although this may not be readily recognized (Swerdlin et al. 2007).
Examination of the Skin
It is self-evident that the examination of the skin must be thorough and reproducible before attempting to attribute any cutaneous appearances to non accidental or unnatural causes. While the examination of the live child presents its own challenges, including medicolegal issues of consent as well as the general health and nutritional and even social settings of the child and its family grouping, the circumstantial data that is available to the forensic pathologist may be limited. It is, therefore, imperative that the examining pathologist be acquainted with as much information surrounding the child’s situation as is available. It is likewise essential that the examination is conducted under optimum conditions so as to maximize the value of any observations that are made. There is little point in attempting to interpret a detailed description of external pathological findings if the lighting is poor, all surfaces have not been cleaned and visualized, or the presence or availability of relevant physical evidence, such as wounding objects, has not been recognized. As injury of the skin can be the result of many different physical agents, it is appropriate to be familiar with possible injuring agents, such as belts, straps, and heated objects such as irons, cigarettes, hot plates, and scalding water (see below).
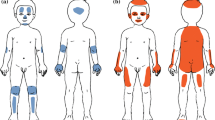
The examination of the skin requires recognition of all the various possible abnormalities that can be seen including bruises, bite marks, abrasions, lacerations, sharp injuries, burns and scalds, scars, and keloids, as well as natural conditions that may be misinterpreted as injuries. These include Mongolian spots, various congenital hemangiomata, as well as a number of rashes and erythemata. These are discussed in more detail below. If abnormalities are identified, it is appropriate that they should be photographed and possibly also recorded on a body outline (see Fig. 11.1). In this way, it is possible to relate a pattern of abnormalities that may of itself impart more information than is available just from consideration of the isolated skin mark.
Infant body outline (From http://www.afmes.mil/assets/docs/SUIDIform.pdf)
Photography of injuries and other abnormalities should not be undertaken without consideration of all the technological issues that can maximize the value of this essential procedure (Oliver 2011). When recording injuries, correct lighting is essential. This lighting must ensure that the injury is evenly illuminated and clearly visible even if it is located on a curved or protected part of the body surface. Photographing injuries in body crevices or folds may present significant challenges. It is often appropriate to consider the use of both color and black-and-white photography as these may highlight different features. It has been considered that the variation of color within any individual injury (especially bruises) may provide information relating to the age of that injury. While that is the subject of further discussion elsewhere in this text, it is important to recognize that if it is intended that the color of an injury is to be used to aid in its interpretation, then it is appropriate that color scales are also used in the photograph. Of course, in any photograph that may be used in a forensic setting, an accurate scale must be incorporated into the image to facilitate the assessment of size and dimension.
Different lighting techniques can be utilized to illustrate different aspects of an injury especially in association with digital technology (Tetley 2005). Simple light photography using the visible spectrum is widely available and will provide an accurate and convenient method of recording injuries. Photography using specific wavelengths especially those that are red free may facilitate observation of areas that are normally predominantly red. Infrared photography may demonstrate tissues beneath the epidermis particularly in areas that have differential absorption characteristics. It is said to be useful in detecting early bruising. Ultraviolet photography can be useful in observing old lesions, scars, bruises, and bite marks as there is good surface detailing (Tetley 2005). The application of alternative light sources to outline skin lesions is well known in forensic pathology, and the use of a Wood’s lamp may be considered in the documentation of both new and healing bruises (Vogeley et al. 2002).
Special procedures may need to be undertaken when there are suspected bite marks on the skin surface. As these marks are made by the dentition and it is recognized that this area may have some unique identifying characteristics (see below), it is necessary to ensure that any examination can capture those features that may allow identification of a perpetrator. Therefore, the physical examination must be especially thorough including breasts, genitalia, thighs, arms, and the back. Bite marks are often multiple so it is necessary to record these separately as well as jointly. The very fact that the marks may show evidence of differing ages (insofar as that is possible to determine) is in itself a positive observation that supports an abusive origin. Photography is an essential adjunct to the recording of bite marks, and it must be undertaken using special L-shaped rulers that allow the reliable comparison of sizes and shapes. The camera must be positioned at 90° angle to the bite to minimize any perspective effect that may render comparison unreliable (Bell 2000; Oliver 2011). It is advisable to take an initial localizing photograph to record the position of the bite and then to record a close-up with a properly aligned and orientated scale. It may be appropriate to take a black-and-white photograph as the better contrast may enhance study of the dimensions, although current digital technology allows for image manipulation to facilitate that process.
Finally, DNA evidence should be obtained by swabbing of the wound and its surrounding skin. The exact technique used will vary according to the procedures adopted by the local forensic laboratory, although it is often recommended that a double-swab (“wet and dry”) technique be used (Sweet et al. 1997). In this method, the initial swab is taken by wiping the area with a swab that has been moistened with sterile water. This loosens the surface epithelial cells which will then adhere to the second, dry swab that is wiped across the wound. This technique of swabbing the skin to retrieve nuclear material can be applied to any skin wound and is useful in detecting the presence of an assailant’s DNA. Another method that can be used to recover DNA on human skin is minitaping, in which adhesive tape is applied to lift foreign DNA that has been transferred from the assailant (Kenna et al. 2011). When using both of these techniques, it is appropriate that a control sample be taken from an uninvolved location on the body of the victim. Given that assailants in child abuse are often close contacts of the victim (and therefore likely to have deposited DNA on the skin anyway), this testing has limited value in the examination of much pediatric blunt trauma, but since bite marks are infrequently part of natural activity, this may be a useful adjunct to the forensic examination of the skin.
Bruises
Given that any application of external blunt force can cause bruising, it is obvious that the examination, description, and recording of bruises are an important part of the forensic examination of children. Bruises characteristically occur without surface damage. Of course they may be found in conjunction with other more disruptive injuries of the surface such as abrasions or lacerations, but these are then regarded as compound injuries. As up to 90 % of victims of child physical abuse show skin injuries, it is incumbent on the forensic examiner to attempt to identify those bruises and bruise patterns that are likely to be non accidental (Stephenson 1995). They are documented in Table 11.1.
A bruise follows damage to cutaneous blood vessels and the escape of blood into the surrounding connective tissue. The ensuing appearance is then the result of a number of factors. These include the extent of vessel injury leading to differing quantities of free blood as well as the density of connective tissue in the surrounding support structures and the presence of nearby hard tissue such as bone that may increase the likelihood that trauma applied to small capillaries results in damage to the wall and leakage of red cells. As a corollary, the presence of soft tissue such as fat beneath the skin may have the reverse effect. In that situation, a given degree of trauma may not distort the cutaneous capillaries sufficiently to result in damage and leakage of blood. The effect of this differential support offered by hard versus soft tissues is ably illustrated by the ease with which blunt force trauma applied to the skin of the head produces bruising (due to the hard bone beneath the skin), whereas even strong trauma applied to the front of the abdominal wall in a child may cause catastrophic internal damage leading to fatal gastrointestinal injury and hemorrhage but leave little or no evidence of bruising in the skin of the front of the abdomen.
The presence of diseases or medical therapies that affect the coagulation of blood or the integrity of blood vessels may significantly alter the propensity of a child to bruise and by inference the size and extent of bruising in a child exposed to any type of trauma. As mentioned elsewhere, diseases such as Henoch-Schönlein purpura, idiopathic thrombocytopenic purpura, or other coagulopathies may cause a child to appear well but to have unexplained bruising (Stephenson 1995).
Of more importance is the fact that bruises are more common among children as they become more mobile. Skin injuries are a normal feature of growing up and increasing mobility, and this pattern must be recognized by the forensic examiner in the assessment of a child who has bruises (Labbe and Caouette 2001; Sugar et al. 1999). The majority of children who are becoming mobile (greater than 9 months old) have one or more bruises. Alternatively, if a child is not mobile, then the presence of bruising should at least raise the specter of a non accidental cause (Maguire et al. 2005). There is an oft-quoted aphorism that states “children who don’t cruise rarely bruise” (Sugar et al. 1999). The pattern of bruising seen in mobile infants and young children reflects the increased exposure of the body to blunt force contact especially during times of increased mobility (such as during warmer weather in temperate regions) (Labbe and Caouette 2001). Accidental bruises are observed on bony surfaces such as the anterior aspects of the lower limbs or the dorsal surfaces of the forearms. Bruises on the forehead may be accidental. Bruises caused by abuse are much more common on other parts of the head, the neck and face, the anterior chest, as well as the back and buttocks (Dunstan et al. 2002) (Fig. 11.2). Other characteristics that are suggestive of physical abuse include multiple bruises in clusters, multiple bruises of uniform size or shape, and bruises that have a defined pattern or that suggest the imprint of a used implement.
Among the patterns of bruising commonly seen in abuse is the grouping of small round or oval bruises that raise the suspicion of contact with the fingertips of the striker (Figs. 11.3 and 11.4). This pattern may be seen over the face where it suggests that a hand has been placed firmly over the mouth to quieten a cry. This proposed scenario carries the implication that fingers have been placed with sufficient force to cause bruising. It is tempting to try to match the bruises to a hand pattern, but this should not be over-interpreted. The use of the hand to slap the face hard may also leave fingertip bruises as it is those parts of the hand that are most likely to impact the skin with the greatest force. However, this may also produce multiple parallel bruises reflecting contact with several fingers (Figs. 11.5 and 11.6). The pattern of fingertip bruising may also be seen on the upper arms or legs where the abuser is gripping the limbs either as enforced restraint or while holding the child during the act of throwing the body around or against a surface. In this situation, the bruises are often seen on the inner surfaces of the limbs, and this is highly suggestive of non accidental injury. Additionally, repeated blows with a closed fist may produce multiple bruises that each carry rounded features suggestive of fingertips or knuckles (Fig. 11.7).
The forcible application of an object may produce a bruise that carries the pattern of that object. Commonly seen are marks made by belts and belt buckles, various hard articles such as bats and wooden paddles, wide flat surfaces such as books, and narrow cylindrical articles such as cords, canes, branches, and other rods. Tubular structures characteristically produce bruises that carry a “tram track” configuration of two parallel lines often separated by a pale or non bruised strip (Fig. 11.8).
While bruises are the most common external signs of physical abuse, they are rarely severe enough to be fatal of themselves. However, occasionally bleeding in the skin is so extensive that there may be major clinical consequences such as anemia or even death. Unless there is a coexisting coagulation defect, this extensive bruising should be considered to be abusive until proved otherwise (Fig. 11.9).
As indicated above, one of the cardinal signs of abusive bruising is the presence of multiple injuries especially when those injuries have been inflicted over a prolonged period. To make such an observation implies the ability to distinguish differing ages of observed bruises. The combination of recent and older bruises especially in areas not prone to accidental trauma is highly suggestive of inflicted injury. This implies an ability to determine the age of individual bruises with sufficient accuracy to allow the distinction of different times of infliction. The subject of the aging of injuries in children is discussed in detail elsewhere in this text, but in any examination of the bruised child, consideration of whether multiple lesions were inflicted at the same or different times should be part of the process. It has been traditional to consider the differences in the coloring of various injuries as reflective of different ages, but there are many reasons why bruises have varying colors (Table 11.2).
The aging of bruises may involve more than the assessment of the color. The histological examination to assess any inflammatory and repair response may be part of the formal forensic examination of abusive bruising, although it should not be over-interpreted as there have been few reliable studies to support its efficacy (Langlois 2007).
Bite Marks
A bite mark is a mark made in a substrate by teeth, although the structures responsible may also involve other oral or perioral structures. The first phase in examination of a bite mark is the determination that the mark has indeed been caused by biting. As skin and subcutaneous tissue are elastic, they may be movable and may not record impressions reliably. They may stretch or compress according to the position of the body, and therefore distortions may be introduced. Bruising may occur or frank laceration may be present. This complicates the determination of tissue injury caused by teeth. It is necessary to consider other objects that may cause skin injury that resembles bite marks. For example, shoe heels, some belt buckles, and even the corners of a hot iron may inflict injuries that look similar to bites.
Assuming that a determination has been made that the tissue injury is consistent with a bite, it is necessary to determine whether it is an animal or human bite and if human, whether it is caused by a juvenile or by an adult mouth. Initially class characteristics should be determined (Table 11.3). These are the characteristics that determine if an injury is likely to be a bite mark or not. There may also be individual characteristics that may facilitate specific identification (Table 11.4) (Fig. 11.10).
Problems may arise when attempting to relate bite mark injuries to individual perpetrators using only anatomical or topographical evidence. It is inappropriate to use bite marks to identify offenders purely on the basis of the physical appearance of the injuries. There are too many uncontrolled variables. For example, as mentioned above, tissue is elastic and may stretch, and this is compounded by the fact that not all teeth will necessarily impact the bitten surface at the same time. So there may already be some distortion by the time that later teeth impact the surface (Sheasby and MacDonald 2001). Additionally, the child may pull away from the biter and this may introduce further distortions. Multiple bites may be inflicted in a small area, making it difficult to separate all the components of each individual bite. Therefore, in the absence of forensic biological analysis and DNA matching (see above), it is appropriate to confine anatomical bite mark analysis to being an exclusionary technique. Notwithstanding that rider, it may be possible to state that “a particular individual cannot be excluded as the perpetrator of this bite mark.”
In considering the resulting skin injury, it is worth describing how a bite mark is inflicted. The most common scenario has the mouth fairly wide open when the bite is begun. The lower anterior teeth impact the skin being bitten with the incisal edges holding that material steady (rather like the spikes on a meat tray holding the meat still for carving). These teeth are fairly small and narrow and tend not to move a great deal. They therefore leave similar small well-defined marks. The upper teeth tend to have a larger profile. When they first hit the skin, it is the inside, or palatal, surfaces of the teeth that contact the area being bitten, and as the jaws move closer together and the mouth closes, a wave of tissue (skin and subcutaneous soft tissues) is pushed up against the palatal surfaces. If the dental arches close together to a greater degree, then the upper teeth drag more than the lower teeth because of the greater surface area and lesser friction. In a bruised injury, this means that the mark left by upper teeth will generally be more diffuse than that left by lower teeth. This dragging may leave distinctive marks that have been compared to a “bar code.” It is not sure how distinctive this is for a given set of teeth. Not all teeth will touch the skin being bitten at the same time, either because there is a relative difference in heights of individual teeth relative to the bite plane or because there may be an angle between the bite plane and the skin surface being bitten.
Certain elements in a bite mark case are susceptible to comparison (Table 11.5). This is properly the field of the forensic odontologist, and such expertise should be sought when a bite mark injury is suspected.
There is probably no good relationship between the estimated force applied by individual teeth and the extent of resulting bruising. Therefore, examination of bite marks on the skin of a child tends to be an exercise in pattern matching, and the proper use of swabbing for DNA detection becomes an essential part of the forensic examination (Liston et al. 2001; Pretty and Hall 2002).
Burns and Scalds
Child abuse by burning constitutes from 6 % to 20 % of child abuse cases (Peck and Priolo-Kapel 2002). It is therefore essential that forensic investigators can recognize those lesions that have been caused by the application of heat and also that they can recognize those situations that may be confused with thermal injury. Burns occur when the skin and the subcutaneous tissues are damaged by thermal energy. For this to occur, a number of criteria must be satisfied, and the injury that results will depend on which of those criteria occur and for how long that injury is inflicted. These criteria include the temperature that is applied to the skin, whether the skin is wet or dry, whether the heat is wet or dry, the thickness of the keratin covering the area over which that heat is maintained, and the duration of that contact. These can be summarized in considering the coefficient of thermal conductivity. The resulting skin lesion and any systemic sequelae are dependent on the summation of these different components (Faller-Marquardt et al. 2008).
Young children constitute a high proportion of burn victims, and up to 25 % of pediatric burns may have had an abusive cause (McLoughlin and McGuire 1990).
Dry burning results when the heat that is absorbed by the skin results in local tissue damage. If this damage is extensive enough, it may be associated with systemic responses which may be fatal if severe or untreated. Similar results may follow scalding, and given that liquids may, by their very nature, spread this contact effect over extensive areas of skin, scalding is a more common cause for hospital admission than injury inflicted by dry heat. The damage that occurs after thermal contact will initially be observed as reddening of the surface as cutaneous erythema occurs. If the temperature is high enough, the contact long enough, or the heat transfer deep enough, there will be damage to the dermal and subcutaneous tissues resulting in blistering and even ulceration. It is possible in extreme cases to have charring of the skin if the heat is so high that the organic material combusts, such as when fireworks explode (Al-Qattan and Al-Tamimi 2009) or cigarette ends are applied to the skin for a prolonged time (Faller-Marquardt et al. 2008).
Thermal damage is traditionally classified according to whether the injury is inflicted by dry heat (burning) or by hot liquids (scalding), although the principles of damage are the same and it is not necessarily helpful to maintain this distinction. There are patterns of burn injury that are suggestive of an abusive origin. Many of these relate to the depth of the wound. Second- or third-degree burns, especially if they are multiple or symmetrical, should raise the index of suspicion. Skin is an effective insulator of heat, and most damage is confined to the epidermis due to the usually brief duration of contact. It is a normal reflex to rapidly withdraw an exposed area from applied heat, and if the damage is observed to be deep, then it implies that the time of contact may have been prolonged. This is strongly supportive of a non accidental cause. Burn injury patterns have been variously categorized, but one of the most useful classifications depends on the method of heat application rather than the resulting appearance. In this classification (Lenoski and Hunter 1977), burns are associated with splash, immersion, and contact. A flexion pattern may also be seen as a subset of immersion burns.
Splash burns result when the scalding liquid is thrown or poured onto the skin. This is more likely to be the result of an accidental event in children, and the burns that are produced may have a very heterogeneous range of appearances (Drago 2005; Fracasso et al. 2009; Shoufani and Golan 2003; Wallis et al. 2008). The liquid may drip or flow after contact and therefore the heat damage may spread locally. However, the temperature of the liquid may also fall rapidly after contact so the duration of the damaging heat may be short-lived and the injury is limited. If the hot liquid flows after impact, the burn may be directional in a way that demonstrates the position of the child when the liquid struck the skin. There is nothing in splash burns that is probative for abuse, although accidental splashes are frequently seen on the front and upper half of the body and face. The typical “spill” burn occurs on the anterior surfaces of the face, lower neck (the upper neck is often protected by the chin), chest, shoulders, and extended arms. Splash burns occurring in other areas should be regarded as suspicious for a non accidental origin.
Immersion burns are more frequently abusive than splash burns. They tend to be of even depth and have a uniform distribution over those areas in contact with the hot liquid. They are caused when the child is dropped or dipped into a hot liquid. A typical situation is bath water that is either accidentally or deliberately too hot for safety. The injuries tend to have a sharp line of demarcation between burnt and normal skin and are often of uniform depth. If an area of skin contacts the container, it may be protected from the heat, and this results in an uninjured zone in the middle of the large burn (Fig. 11.11). This “target” effect is typically seen on the buttocks. If the immersion burn is the result of accidental contact, it may be complicated by the presence of drip or splash marks as the child has the ability to move and to attempt to withdraw the affected body part from the hot liquid. Such an ability is often lacking in abuse, and such irregularities of the edge are less common.
Flexion sparing is seen when limbs are held in flexed positions during immersion. This results in the skin within creases being spared burn injury. These shielded areas include the hip flexion creases, the anterior elbow creases, and the posterior knee popliteal fossae. Shielded skin creases may also be seen on the anterior lower abdomen if the lower trunk is forced into flexion during immersion with the child in a seated position.
Distinguishing intentional from unintentional scalds may be difficult, but intentional injuries are often immersive, involving the extremities and buttocks or both. Additionally they are frequently symmetrical with clear upper margins (Maguire et al. 2008). Unintentional scalds are more commonly due to splash or spill and tend to affect the upper body with irregular margins and depth. Additionally, accidental scalds, burns, or splashes are more frequently referred for immediate medical attention.
Contact burns are usually caused by dry objects and characteristically reflect the size and shape of the applied burning object. These may be accidental or abusive. However, burns caused by contact with certain objects, such as those not normally associated with children, are more likely to be non accidental. Of course, contact with some heated household objects may be accidental, especially if the child is newly mobile and explorative. These injuries usually occur on the hands and are unilateral and shallow, being restricted by the rapid withdrawal of the burnt hand on contact with the hot surface (Wilson Jones et al. 2008). Prolonged contact or repeated contact with one object is probably abusive (Faller-Marquardt et al. 2008).
Cigarette burns are common findings in physical child abuse and present a characteristic appearance. They are of a similar size to the tip of a cigarette and are usually rounded and clearly defined. It is important to note that there may be some variation in the shape of wounds created by contact with a lighted cigarette as the nature of that contact is so variable. The contact may be intentional and well defined, in which case the wound is often discrete and rounded (Fig. 11.12). This is a feature of non accidental injury. If however there is a glancing touch, then the shape of the wound may be oval or poorly defined. Cigarette burns are frequently multiple, and their significant depth often produces scars that are easily recognized. However, as with most burns, the depth varies and the appearance depends on the degree of penetration (Faller-Marquardt et al. 2008). First-degree burns tend to be erythematous and may show local edema. As they may heal with no sequelae or just with mild hyperpigmentation, they may be difficult to identify forensically. Second-degree burns involving the superficial dermis may blister, and this should be recognizable by the forensic examiner. The full-thickness third-degree burn may show necrosis, blistering, or even a dry leathery appearance due to local thermal coagulation. It is these deeper wounds that readily scar.
Other forms of contact burn are not infrequent, and some may strongly suggest an abusive origin. Burns from contact or close proximity to household objects such as hair dryers and other cosmetic appliances may frequently be accidental (Prescott 1990; Wilson Jones et al. 2008). In this case, they are usually isolated, and any multiplicity of such injuries should raise the specter of a deliberate abusive origin. In some communities, electric water heaters may present a dangerous hot surface and can cause localized burning if the child places his/her hand onto the outside surface (Chuang et al. 2003; Drago 2005). Of course this pattern of injury whereby the child’s hand is deliberately held against a hot surface is a fairly frequent form of abuse. The most commonly available surface is a cooking hotplate/stove top and if burns of the palms of the hands or feet are seen, and especially if they are large, deep, or bilateral (implying prolonged or repeated application), then non accidental injury should be considered likely. Burns following the application of an object such as a hot iron are not uncommon and must be considered to be abusive until proved otherwise. As the surface is fairly broad, the resulting injury is naturally fairly large.
Microwave ovens are occasionally a source of childhood burns. While accidental injuries occur after contact with fluids or other food heated in such devices, abusive injuries have been reported following the placement of the child within the ovens (Alexander et al. 1987). Sharply defined burns have appeared in areas closest to the microwave-emitting devices, although there is nothing specific about the burns that indicate microwave radiation as the causative agent. The penetration depth of microwaves is small, and the heating takes place near the surface at the skin (Ozen et al. 2011). The temperature cannot be accurately predicted as there are so many variables (e.g., strength of radiation, duration of exposure, and moisture content of surface tissues), but temperatures of over 100 °C can be achieved in foods placed in microwave ovens.
Scarring
If an injury is deep or severe enough and if the child survives long enough, then a scar may form at the site of the original injury. Whether a scar forms depends on a number of factors including the size of the original injury, the age of the victim, the depth of the injury, and the tissues damaged by the original trauma. Infection at the site of the original injury or the presence of foreign material may predispose to scar development. Pediatric burns may develop into hypertrophic scars if they are particularly deep and if the healing time is prolonged (Cubison et al. 2006). The use of electrical cords to inflict injuries can lead to characteristic curved scars (Showers and Bandman 1986). Additionally some racial groups are more prone to develop post-injury scars, and some of those scars can be very prominent. Keloids are hypertrophic scars that are more common in persons of African ancestry.
Scars and keloids may therefore be a useful indicator of a history of injury. If such lesions are numerous or are observed in areas not normally susceptible to accidental trauma, then the very presence of scarring may support a suspicion of abusive trauma. In some groups, this scarring may be symbolic and can reflect local customs (Johnson 1994).
Skin Lesions That Mimic Child Abuse
As cutaneous lesions are recognized as the most common manifestation of child abuse, it must be remembered that there are some abnormalities of the skin that may be misinterpreted as evidence of mistreatment. This misreading of physical signs can have serious consequences for the child, the family, caregivers, the falsely accused, and even for investigators so the range of conditions that may give rise to misdiagnosis should be familiar to forensic examiners.
The first step in ensuring that observed abnormalities are definitely representative of abuse, both physical and sexual, is a full and accurate medical history of the child. This may include knowledge of the social and racial circumstances of the family. In this way, changes that may represent certain ethnic and cultural practices can be recognized for what they are. Of course, when those practices result in physical changes in the skin, some authorities may still interpret that as evidence of abuse. That is a matter for legal opinion and is outside the scope of this chapter. It merely needs to be recognized that some “folk remedies” may result in physical damage to the skin. Additionally, the knowledge of the racial background of the child may alert the examiner to recognize that some cutaneous abnormalities may be more common in certain racial groups. A history of congenital onset obviously excludes an abusive origin even in a lesion that otherwise may be interpreted as an injury. There are several reviews that outline the most common lesions that have the potential for misinterpretation as abuse (AlJasser and Al-Khenaizan 2008; Hansen 1998; Mudd and Findlay 2004; Scales et al. 1999).
Folk Remedies
Folk remedies and cultural practices present a significant potential source of misunderstanding with child abuse (Mudd and Findlay 2004). There are several practices that can result in hyperpigmentation and unusual bruises. The remedies known as coin rubbing (Vietnamese) or spoon rubbing (Chinese) can result in quite dramatic marks in the skin that mimic abuse. In coin rubbing, or cao gio (“scratch the wind”), the skin is rubbed with a coin, often after the application of medicated oil or ointment. This rubbing occurs along the spine, neck, or down intercostal spaces until petechiae or bruises appear. The Chinese variant termed spoon rubbing, or quat sha, is similar except that the back or side of a spoon is used. This process is believed to rid the body of “bad winds” that can cause many symptoms. However, it appears as one or more often parallel lines of reddening or bruising. These may even be bilateral and symmetrical (Fig. 11.13). Indeed this symmetry is a useful clue to the nature and origin of the lesion. If the rubbing was performed sometime before the examination, there may be hyperpigmentation following the same pattern. Occasionally, the skin may be pinched at the same time, and this can complicate the observations.
Cupping, dry or wet is an ancient remedy that is still seen in many cultures, including Russian immigrant families and Asian groupings (Hansen 1998). In the former, a vacuum must be created in the cup for it to be effective. This can be done in a number of ways, but most commonly a cotton wool ball soaked in alcohol is burnt to consume oxygen and thereby reduce pressure. On removing the ball, the cup is placed on the skin and the reduced pressure draws the skin upward. This produces a red circular mark with varying bruising in the center. Wet cupping differs in that small cuts are made on the skin surface prior to the application of the cup. This causes local bleeding. Both forms of cupping leave erythema, bruising, and sometimes burns. They may be confused with child abuse although, as mentioned above, it may itself be regarded as an abusive procedure.
Other “burns” can be produced by the practice of moxibustion, in which a piece of moxa herb (mugwort) or yarn is rolled into a ball, placed onto the body surface, and then ignited. This produces circular burns that will scar and may be confused with intentional abuse, especially by cigarette burns. Occasionally this may be combined with acupuncture, and it is a practice that is observed in several Asian countries including China, Japan, Cambodia, and Laos (Faller-Marquardt et al. 2008). Small deep burns can also result from some therapeutic cautery seen in some Arabic cultures (“maquas”) and some parts of Africa (Feldman 1984, 1995). Even the therapeutic use of garlic may produce burns after prolonged contact with the skin, and the use of common rue, an evergreen shrub found in the Mediterranean region and applied to treat various ailments, may cause phytophotodermatitis (Risser and Mazur 1995). This may also occur after the application of plants such as lemons, limes, celery, and many herbs (Scales et al. 1999).
Conditions Confused with Bruising
As indicated above, there are a number of appearances and conditions that may be mistaken for bruises (Table 11.6). In the forensic examination of a deceased child, the most common source of confusion is the misinterpretation of postmortem lividity as cutaneous bruising. All pathologists will be familiar with the great variation in the distribution of lividity. Characteristically, the pattern reflects the position in which the body has been lying in the period since circulation ceased (death). Therefore, the most dependent parts of the body contain cutaneous blood vessels that are suffused with blood, imparting a darker color than those skin areas either less dependent or under some compression due to contact with a surface or some other object, such as clothing. This dependent congestion may be very patchy, and not infrequently there may be areas of cutaneous darkening that are easy to misinterpret as bruising. It is not always clear why there are irregular areas of lividity on less-dependent parts of the body. What is important during the forensic examination is that each suspect area is examined carefully for the presence of extravasated blood. Fortunately this is usually quite straightforward as a small incision into the discolored area will quickly demonstrate the presence of extravascular red cells if there is genuine bruising. In the event of confusion or doubt, histological examination will establish the presence or absence of bruising in a suspect area. The performance of iron stains will identify those areas in which the presence of hemosiderin confirms earlier bleeding.
Bruises may be real but they are not necessarily the result of abuse. This is discussed above in the section on bruising. Several medical conditions produce cutaneous changes that either may be confused with bruising or may produce hemorrhage in the skin that is not abusive in origin.
Mongolian spots are variable patches or macules of blue/gray cutaneous pigmentation. They are usually present at birth and often fade gradually over weeks or months, although occasionally they may persist (Fig. 11.14). As the name suggests, they are more common in children of East Asian origin although they can be seen in many ethnic groups. Mongolian spots are most frequently observed over the lower back, above the natal cleft, but can be found in many other parts of the body including the shoulders and the extremities. In those situations, they can be easily mistaken for bruises, and their atypical location (including sites not normally associated with normal activity-based pediatric bruising) may compound this misinterpretation. Unlike bruises, their color does not change (although they usually fade over time), and the presence of several marks of varying colors such as blue, gray, green, and yellow strongly supports a diagnosis of bruising and mitigates against Mongolian spots. Histologically, there is an increase in pigmented melanocytes in the deep dermis with no extravasation of red cells.
Hemangiomas are congenital lesions that are commonly found in childhood. If they are deep lesions, they may be blue and may be misinterpreted as deep bruises. If superficial, especially in vascular areas such as the perineal area or in perioral tissues, they may be mistaken for injuries. Other lesions that may mislead include Henoch-Schönlein purpura, various hypersensitivity reactions (such as erythema multiforme and erythema nodosum), phytophotodermatitis, Ehlers-Danlos syndrome, and some lymphangiomas. Even the dyes that can elute from some clothing may color the skin in such a way as to confuse. Knowledge of the history, including the familial story and the circumstantial situation, should allow these conditions to be recognized (Scales et al. 1999).
Diagnostic errors may occur in children who have a bleeding disorder as well as bruising, and it is imperative that this situation is considered in the forensic examination. While it is relatively simple to perform coagulation studies and other laboratory investigations in the living child, this may be problematic after death. Retrieving a thorough clinical and family history is essential. The absence of any history that suggests a bleeding diathesis may support a diagnosis of inflicted injury, although the presence of such a history does not necessarily exclude it. Children with bleeding disorders do get abused (Lee 2008).
Conditions Confused with Burns
Many of the folk remedies mentioned above may produce lesions that are burns but are considered to be non abusive because of the circumstances. There may also be lesions that physically resemble burns but are in fact natural conditions, such as bullous impetigo or staphylococcal scalded skin syndrome (Table 11.7) (Porzionato and Aprile 2007). The latter may be so extensive that it is mistaken for extensive scalding. There are other disorders that resemble burns including epidermolysis bullosa, dermatitis herpetiformis, urticarial pigmentosa, and fixed drug eruptions (AlJasser and Al-Khenaizan 2008). Even severe nappy rash may be misread as scalding affecting the perianal area, and the possibility of burns caused by dipping the child in hot water needs to be considered. Laxative-induced dermatitis has been incorrectly diagnosed as abusive burns (Leventhal et al. 2001).
Lesions that can be confused with cigarette burns are many and include acne vulgaris, insect bites, focal pyoderma, healed infected chicken pox, and even smallpox vaccination scars. Indeed any irritated lesion, especially if scratched, could potentially be misinterpreted as a burn. Burns with other hot objects with similar profiles may be mistaken for cigarette burns (Faller-Marquardt et al. 2008).
Bibliography
Alexander RC, Surrell JA, Cohle SD. Microwave oven burns to children: an unusual manifestation of child abuse. Pediatrics. 1987;79(2):255–60.
AlJasser M, Al-Khenaizan S. Cutaneous mimickers of child abuse: a primer for pediatricians. Eur J Pediatr. 2008;167(11):1221–30.
Al-Qattan MM, Al-Tamimi AS. Localized hand burns with or without concurrent blast injuries from fireworks. Burns. 2009;35(3):425–9.
Bell K. Identification and documentation of bite marks. J Emerg Nurs. 2000;26(6):628–30.
Chuang SS, Yang JY, Tsai FC. Electric water heaters: a new hazard for pediatric burns. Burns. 2003;29(6):589–91.
Cubison TC, Pape SA, Parkhouse N. Evidence for the link between healing time and the development of hypertrophic scars (HTS) in paediatric burns due to scald injury. Burns. 2006;32(8):992–9.
Drago DA. Kitchen scalds and thermal burns in children five years and younger. Pediatrics. 2005;115(1):10–6.
Dunstan FD, Guildea ZE, Kontos K, Kemp AM, Sibert JR. A scoring system for bruise patterns: a tool for identifying abuse. Arch Dis Child. 2002;86(5):330–3.
Ellis PS. The pathology of fatal child abuse. Pathology. 1997;29(2):113–21.
Faller-Marquardt M, Pollak S, Schmidt U. Cigarette burns in forensic medicine. Forensic Sci Int. 2008;176(2–3):200–8.
Feldman KW. Pseudoabusive burns in Asian refugees. Am J Dis Child. 1984;138(8):768–9.
Feldman KW. Pseudoabusive burns in Asian refugees. Child Abuse Negl. 1995;19(5):657–8.
Fracasso T, Pfeiffer H, Pellerin P, Karger B. The morphology of cutaneous burn injuries and the type of heat application. Forensic Sci Int. 2009;187:81–6.
Hansen KK. Folk remedies and child abuse: a review with emphasis on caida de mollera and its relationship to shaken baby syndrome. Child Abuse Negl. 1998;22(2):117–27.
Johnson CF. Symbolic scarring and tattooing. Unusual manifestations of child abuse. Clin Pediatr (Phila). 1994;33(1):46–9.
Kenna J, Smyth M, McKenna L, Dockery C, McDermott SD. The recovery and persistence of salivary DNA on human skin. J Forensic Sci. 2011;56(1):170–5.
Labbe J, Caouette G. Recent skin injuries in normal children. Pediatrics. 2001;108(2):271–6.
Langlois N. The science behind the quest to determine the age of bruises – a review of the English language literature. Forensic Sci Med Pathol. 2007;3(4):241–51.
Lee AC. Bruises, blood coagulation tests and the battered child syndrome. Singapore Med J. 2008;49(6):445–9.
Lenoski EF, Hunter KA. Specific patterns of inflicted burn injuries. J Trauma. 1977;17(11):842–6.
Leventhal JM, Griffin D, Duncan KO, Starling S, Christian CW, Kutz T. Laxative-induced dermatitis of the buttocks incorrectly suspected to be abusive burns. Pediatrics. 2001;107(1):178–9.
Liston PN, Tong DC, Firth NA, Kieser JA. Bite injuries: pathophysiology, forensic analysis, and management. [Review]. N Z Dent J. 2001;97(428):58–63.
Maguire S, Mann MK, Sibert J, Kemp A. Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child. 2005;90(2):182–6.
Maguire S, Moynihan S, Mann M, Potokar T, Kemp AM. A systematic review of the features that indicate intentional scalds in children. Burns. 2008;34(8):1072–81.
McLoughlin E, McGuire A. The causes, cost, and prevention of childhood burn injuries. Am J Dis Child. 1990;144(6):677–83.
Mudd SS, Findlay JS. The cutaneous manifestations and common mimickers of physical child abuse. J Pediatr Health Care. 2004;18(3):123–9.
Oliver W. Considerations for gross autopsy photography. Acad Path. 2011;1(1):52–81.
Ozen S, Helhel S, Bilgin S. Temperature and burn injury prediction of human skin exposed to microwaves: a model analysis. Radiat Environ Biophys. 2011;50(3):483–9.
Peck MD, Priolo-Kapel D. Child abuse by burning: a review of the literature and an algorithm for medical investigations. J Trauma. 2002;53(5):1013–22.
Porzionato A, Aprile A. Staphylococcal scalded skin syndrome mimicking child abuse by burning. Forensic Sci Int. 2007;168(1):e1–4.
Prescott PR. Hair dryer burns in children. Pediatrics. 1990;86(5):692–7.
Pretty IA, Hall RC. Forensic dentistry and human bite marks: issues for doctors. [Review]. Hosp Med. 2002;63(8):476–82.
Risser AL, Mazur LJ. Use of folk remedies in a Hispanic population. Arch Pediatr Adolesc Med. 1995;149(9):978–81.
Scales JW, Fleischer AB, Sinai SH, Krowchuk DP. Skin lesions that mimic abuse. Cont Pediatrics. 1999;16(1):137–45.
Sheasby DR, MacDonald DG. A forensic classification of distortion in human bite marks. Forensic Sci Int. 2001;122(1):75–8.
Shoufani A, Golan J. Shabbes burn, a burn that occurs solely among Jewish orthodox children; due to accidental shower from overhead water heaters. Burns. 2003;29(1):61–4.
Showers J, Bandman RL. Scarring for life: abuse with electric cords. Child Abuse Negl. 1986;10(1):25–31.
Stephenson T. Bruising in children. Curr Pediatr. 1995;5:225–9.
Stephenson T. Ageing of bruising in children. J R Soc Med. 1997;90(6):312–4.
Sugar NF, Taylor JA, Feldman KW. Bruises in infants and toddlers: those who don’t cruise rarely bruise. Puget Sound Pediatric Research Network. Arch Pediatr Adolesc Med. 1999;153(4):399–403.
Sweet D, Lorente M, Lorente JA, Valenzuela A, Villanueva E. An improved method to recover saliva from human skin: the double swab technique. J Forensic Sci. 1997;42(2):320–2.
Swerdlin A, Berkowitz C, Craft N. Cutaneous signs of child abuse. J Am Acad Dermatol. 2007;57(3):371–92.
Tetley C. The photography of bruises. J Vis Commun Med. 2005;28(2):72–7.
Vogeley E, Pierce MC, Bertocci G. Experience with wood lamp illumination and digital photography in the documentation of bruises on human skin. Arch Pediatr Adolesc Med. 2002;156(3):265–8.
Wallis BA, Turner J, Pearn J, Kimble RM. Scalds as a result of vapour inhalation therapy in children. Burns. 2008;34(4):560–4.
Wilson Jones N, Wong P, Potokar T. Electric hair straightener burns an epidemiological and thermodynamic study. Burns. 2008;34(4):521–4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this entry
Cite this entry
Ellis, P. (2014). Cutaneous Findings in Children. In: Collins, K., Byard, R. (eds) Forensic Pathology of Infancy and Childhood. Springer, New York, NY. https://doi.org/10.1007/978-1-61779-403-2_45
Download citation
DOI: https://doi.org/10.1007/978-1-61779-403-2_45
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-61779-402-5
Online ISBN: 978-1-61779-403-2
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences