Abstract
This chapter presents a new conceptual framework to characterize the interactions between modern environments and ancestral physiology that can influence health over the life course. Although the human body was not designed by natural selection to maximize health, it was nonetheless designed to function within certain environmental parameters. Physiology serves as the essential interface between genes and environment not only during life history transitions but also during short-term responses needed to regulate the impact of environmental variation on the internal state. Here, I argue that the contemporary habitat has become an “extreme environment” in the sense that, much like climbing Mount Everest, it requires the human body (and psyche) to function beyond the limits of its adaptive capacity, with potential dire consequences to health. Adaptive mechanisms that have become dysfunctional in an extreme environment show three distinct features: (1) gradient effects, often without overt signs of dysfunction, whereby (2) compensatory mechanisms themselves become the source of illness, and (3) involve systemic repercussions. I present an analysis of altitude hypoxia to illustrate an extreme environmental condition and then apply the same framework to a consideration of metabolic disorders. A conceptual framework that identifies lifestyle factors as being equivalent to entering an extreme environment conveys an immediate, intuitive sense of urgency and an implicit recognition that the human organism has strayed into a habitat for which it is ill equipped.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acclimatization
- Dysfunctional continuum
- Evolutionary mismatch
- Extreme environment
- Hypoxia
- Metabolic disorders,
- Physiologic dysregulation
11.1 Introduction
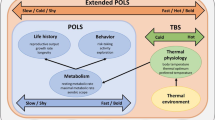
Evolutionary perspectives on health and medicine have given rise to two prominent conceptual models and messages (Stearns et al. 2010). The first emphasizes inherent design “flaws” in the human body arising from inevitable life history trade-offs involved in maximizing lifetime reproductive success. The second examines physiologic variation along dimensions of health in terms of a “functional continuum” composed of adaptive responses to environmental conditions. Both approaches recognize the growing evidence of widespread health risks associated with the dysregulation of major biological systems—metabolic, cardiovascular, and reproductive—under the influence of modern environments.
Typically, the modern environment has been characterized as a novel one, generating a “mismatch” between ancestral genes and contemporary Western lifestyles (Nesse and Williams 1994; Lieberman 2003; Pollard 2008; Trevathan et al. 2008). Although the term mismatch has been referred to as a hypothesis (Lieberman 2013) and a paradigm (Gluckman and Hanson 2006), it is clear that the term serves to describe the evolutionary basis for many of the contemporary trends in disease (Ewald 1994; Panter-Brick and Worthman 1999; Greaves 2000; Stearns and Koella 2008). Yet, as a heuristic and communication device, mismatch falls short for two reasons. First, the concept of mismatch connotes a relationship between two discrete entities (Willingham 2009), neglecting to capture or emphasize the important gradient effects that arise from the interaction between ancestral genes and modern environments. Second, as an emotionally neutral term, mismatch fails to convey the seriousness of health risks associated with the unraveling of biological systems (dysregulation) under contemporary conditions, especially those involving lifestyle factors.
The dysregulation of physiologic systems resulting from gene–environment interaction tends to fall along a graded continuum, whereby clinically recognized illness and pathology manifest after a period of relatively modest forms of dysregulation. This type of dysfunction resembles what happens to the human body when it enters an extreme environment. Although humans have occupied a broad range of habitats over the course of evolution, I argue that the contemporary habitat has become an “extreme environment” in the sense that, much like climbing Mount Everest, it requires the human body to function beyond the limits of its adaptive capacity, with potential dire consequences to health.
As Bateson (1987, p. 349) noted, a “lethal change in either environment or genotype is simply one which demands somatic modifications which the organism cannot achieve.” Under extreme conditions, not only do somatic modifications reach their limit in terms of effectiveness, but the compensatory mechanisms themselves begin to wreak havoc, although the body is performing exactly as designed by natural selection. Conversely, evidence of compensatory mechanisms as the source of illness signifies that the organism is attempting to operate under extreme conditions. Adaptive mechanisms that have become dysfunctional in an extreme environment show three distinct features: (1) gradient effects, often without overt signs of dysfunction, whereby (2) compensatory mechanisms themselves become the genesis of illness, and (3) involve systemic repercussions.
Bateson (1987) also pointed out in his essay first published in 1963 that somatic flexibility is built into the genotype as long as the benefits of flexibility outweigh the fitness costs. Evidence of a flexible functional continuum, such as the ovarian function response continuum (Ellison 1990; Ellison 2001), shifts the perception of pathology in relation to adaptive physiological mechanisms. Here, I propose that a “dysfunctional continuum” emerges whenever a departure from ancestral environmental conditions requires the human body (and psyche) to function in the equivalent of an extreme environment. I first consider the context of altitude hypoxia as an extreme environmental parameter and synthesize the research presented in West et al. (2013) to assemble the dysfunctional continuum en route to clinically recognized pathology. I then apply the same framework to a consideration of metabolic disorders, using standard textbook physiology to describe the foundational narratives of metabolism (Neal 2001; Dominiczak 2007).
From an evolutionary perspective, the current clinical view of functional physiology can mask potential dysfunction arising from adaptive responses to extreme conditions and thus requires a shift in perception. For example, altitude acclimatization is not a benign process and, for the most part, does not restore physiological systems to the sea level equivalent of functionality. Instead, acclimatization capitalizes on somatic flexibility by co-opting adaptive mechanisms designed to function at sea level (and roughly below 2000–2500 m). Although the body may not show overt signs of distress, systems are nonetheless strained and unraveling and, depending on the duration and magnitude of hypoxia, will continue to deteriorate along a continuum of dysfunction. Rather than a series of cost-free adjustments with little consequences to health, acclimatization represents the first line of defense against environmental assault.
11.2 Hypoxia
11.2.1 Adaptive Physiology at Sea Level
Two types of peripheral sensors monitor oxygen availability in the blood. The carotid body, located above the bifurcation in each carotid artery, acts as an immediate transducer if the arterial oxygen pressure drops, converting the hypoxic signal from the blood to a neural signal to the brain. Within seconds, the brain sends impulses to the respiratory muscles to increase the rate and depth of breathing (ventilation). Deep and rapid breathing opens up dormant alveoli and increases both the amount of air entering the lungs and the rate of oxygen diffusion across the capillary membranes. The hypoxic ventilatory response (HVR) is accompanied by a number of complementary responses, including an increase in heart rate and pulmonary artery pressure (caused by greater contraction and force of the right heart ventricle) and also an increase in cerebral blood flow to maintain a steady state of oxygen delivery to the brain.
Another rapid response stimulated by the carotid–neural pathway is a decrease in plasma volume orchestrated by the kidney (via shifts in sodium reabsorption), quickly boosting the supply of oxygen carried per unit volume of blood by increasing the concentration of red blood cells and hemoglobin. In addition, the enzyme that degrades the transcriptional factor HIF-1α (continuously formed and degraded in tissues throughout the body) is inhibited under conditions of hypoxia within minutes, facilitating the induction of certain genes and, in particular, the upregulation of vascular endothelial growth factor (VEGF) , known to play an important role in wound healing among other vascular tasks.
Oxygen-sensing chemoreceptors also exist in the kidney but serve a different purpose than the carotid bodies. Designed primarily to respond to hypoxic signals of injury and blood loss, the kidney monitors oxygen content (the quantity attached to hemoglobin) and stimulates the production of red blood cells in the bone marrow by releasing the hormone erythropoietin (EPO) . Although EPO levels rise in response to hypoxic conditions within hours, the full process of increasing red blood cell mass takes a period of weeks.
The lungs are also equipped with a means to defend against hypoxia resulting from injury or disease at sea level. Pulmonary vasoconstriction in response to local tissue hypoxia closes off the damaged section of the lung through the contraction of the smooth muscle in the small pulmonary arteries and effectively redirects blood flow to the undamaged regions of the lung.
While the peripheral sensors monitor the status of oxygen in the blood, a central mechanism located in the respiratory center of the brainstem uses the status of carbon dioxide (sensed primarily by changes in blood pH) to help regulate the processes of ventilation and cerebral blood flow . At sea level, the peripheral and central chemoreceptors provide complementary signals on the status of respiration. An increase in physical exertion, for example, typically requires both an increase in the supply of oxygen and a high rate of disposal of carbon dioxide, a by-product of the oxidative activity in tissues. An increase in carbon dioxide thus indicates that respiration rate needs to be ratcheted up along with cerebral vasodilation to meet the demands of increased physical activity or danger.
11.2.2 Acute Mountain Sickness
Altitude poses a potential threat to the human organism because the concentration of oxygen (roughly 21 %) in the atmosphere remains constant, although the barometric pressure decreases as altitude increases. The drop in barometric pressure translates into less oxygen per breath, referred to as a drop in the partial pressure of oxygen (PO2) because each gas exerts pressure based on its concentration independent of other gases present.
Acute exposure to moderate altitudes (above 2000–2500 m), such as flying from sea level to the Rocky Mountains for a ski vacation in Colorado, can cause acute mountain sickness (AMS ). The drop in PO2 registers with the peripheral chemoreceptors within a few minutes after ascent, initiating the hypoxic ventilatory response (HVR) . Yet, the onset of AMS can be delayed for another 6–24 h, indicating that when the HVR does not ameliorate the hypoxia, other responses give rise to the symptoms of illness. Common symptoms include headache, fatigue, gastrointestinal ailments (loss of appetite, nausea, vomiting), and a state of expanded extracellular fluid (evidence that the kidneys are responding by reducing plasma volume). AMS symptoms most likely reflect mild generalized brain swelling commensurate with increases in cerebral blood flow in an effort to oxygenate the brain. A swelling brain pressing against a rigid braincase likely leads to the headache and other AMS symptoms, although the precise physiologic pathways have not been fully determined. AMS does not pose a serious threat but can be prevented or mitigated by a gradual ascent, which allows time for other compensatory mechanisms to respond and maintain oxygen delivery to the brain.
11.2.3 Acclimatization as Deterioration
Ascending to higher elevations becomes possible through additional mechanisms designed to respond to hypoxic conditions at sea level. The series of physiologic changes that mitigate the drop in PO2 constitutes the process of acclimatization , a term that refers only to changes “seen as beneficial as opposed to changes which result in illness such as AMS (West et al. 2013, p. 57).” From an evolutionary perspective, altitude acclimatization falls outside the functional continuum and represents a state of physiologic dysfunction, progressing along a gradient of deterioration in response to the magnitude and duration of exposure to an extreme condition.
Further exposure to altitude continues to call upon the body’s repertoire of responses to signals of hypoxia as if operating at sea level. Stimulation of red blood cell production under the influence of EPO (erythropoietin) continues, increasing the hemoglobin concentration [Hb] per unit volume of blood. Plasma volume usually returns to sea level values after a few weeks. The increase in [Hb] tends to rise linearly with altitude (to about 5300 m) and generally restores the oxygen carrying content of the blood to near sea level values and also generates adjustments in blood flow so that oxygen delivery to the brain, in particular, remains constant over a range of [Hb]. At the same time, the rise in [Hb] thickens the blood, increasing vascular resistance throughout the circulation and contributing to the already raised pulmonary artery pressure. In addition, the rise in [Hb] does not translate into improvements in the work capacity of muscles, as it does at sea level, because oxygen diffusion at the tissue site rather than oxygen delivery becomes more limited at altitude.
Structural changes also begin to occur in the pulmonary vasculature in response to the rise in pulmonary artery pressure sensed in the vascular endothelium (lining of blood vessels). Referred to as remodeling, bands of smooth muscle develop fairly rapidly in the small pulmonary arteries under the influence of VEGF . Although vascular remodeling reduces stress on blood vessel walls, resistance is exacerbated by the narrowing of the vessel tube or lumen. Unlike vasoconstriction and the simple contraction of the vascular smooth muscle, pulmonary remodeling introduces structural changes with a substantial degree of irreversibility .
11.2.4 Corrupted Signals
As the human organism ascends along the altitude gradient, physiologic systems continue to be strained in an effort to respond to internal signals of distress that have lost their functional integrity. Key signals become corrupted in the sense that they no longer convey accurate information, as a consequence of both the shifting external parameters and the internal efforts to remedy the situation. In other words, in an extreme environment, the functional responses themselves become dysfunctional and also become the source of further damage that may or may not be reversible, depending on the degree and duration of exposure.
Two potentially fatal forms of AMS —high-altitude pulmonary edema (HAPE ) and high-altitude cerebral edema (HACE)—provide dramatic illustrations of the phenomenon of corrupted signals. HAPE, characterized by frothy sputum that may become blood tinged, can develop at relatively moderate altitude (as low as 2000 m). The genesis of HAPE lies in the main compensatory response by the lungs to the alarm signal of hypoxia. The pulmonary vasoconstriction mechanism, effective at sea level, becomes invoked more widely throughout the lungs yet unevenly at altitude, forcing total cardiac output through fewer sections of the lung as pulmonary arteries progressively close off. Given the high pulmonary artery pressure (PAP) at altitude, capillary walls can break or burst, leaking blood fluids into the alveolar space. A person literally begins to drown. Capillary walls are the most vulnerable structures in the pulmonary vasculature and must be thin enough to allow for gas exchange yet strong enough to withstand increases in pulmonary artery pressure during physical exertion. (Bleeding into the lungs has been found in racehorses in relation to very high PAP during physical exertion.) Although physical exertion at altitude can quickly increase the risk of developing HAPE, breaks in the capillary walls are readily repaired, and most individuals improve rapidly upon descent to lower altitude.
High-altitude cerebral edema (HACE ) also arises from breaks in the capillary walls under pressure but tends to occur at higher altitude (above 3500 m). Symptoms include loss of balance, hallucinations, and hostile or irrational behavior. HACE symptoms stem from the compensatory drive to increase blood flow to the brain in response to the unremitting signals of hypoxia, generating an inordinate amount of swelling and pressure, compounded further by damage to the capillary walls and the subsequent leak of blood fluids into the extravascular space. Descent to lower altitude becomes imperative as death can occur within a matter of days or hours.
Less dramatically, signals to the brain on the status of respiration also become corrupted at altitude. The prolonged HVR leads to a disproportional loss of carbon dioxide (CO2) because carbon dioxide diffuses through tissues about 20 times faster than oxygen due to its higher solubility. The different rates of diffusion for the two gases mean that CO2 is being eliminated through expiration faster than it is being produced by tissues, causing a shift in blood pH toward greater alkalinity. At sea level, alkaline blood pH signals the brain to lower the rate of ventilation and reduce cerebral blood flow through vasoconstriction. At altitude, the brain receives conflicting signals because low arterial PO2 simultaneously signals the brain to increase ventilation and cerebral vasodilation. Low PCO2 no longer conveys reliable complementary information at altitude, creating an unsteady state not encountered at sea level. Although the hypoxic drive to increase ventilation overrides the low PCO2 signal, the mixed signals to the brain may introduce some difficulty regulating cerebral blood flow. Irregular cerebral vasoconstriction, leading to diminished oxygen delivery to the brain, may contribute to the impairment of cognitive functions seen at altitude, including reaction time and hand–eye coordination as well as memory and speech.
Fluctuations in blood pH provide an index of PCO2 level because CO2 travels in the bloodstream attached to bicarbonate (an alkaloid) until expelled by the lungs. A drop in PCO2 leads to a rise in unattached bicarbonate, requiring a compensatory adjustment to ensure that body fluids maintain nearly neutral pH. The kidneys manage the correction fairly well at altitude by increasing the rate of bicarbonate excretion. However, at very high altitude (above 6500 m), the renal compensatory mechanism no longer functions effectively because the frequency of urination needed to maintain neutral pH would require the depletion of body fluids and lead to dehydration. Instead, the kidneys slow down the rate of bicarbonate excretion to preserve body fluids, and blood pH becomes severely alkaline —a disorder called respiratory alkalosis .
Skeletal muscles also initiate a suite of compensatory mechanisms at altitude to improve oxidative ability, as if undergoing greater demands for physical activity similar to endurance training over the course of several weeks at sea level. Under the stimulus of local tissue hypoxia, some responses improve oxygen delivery. For example, the proliferation of new capillaries facilitated by VEGF increases the surface area for oxygen diffusion and simultaneously decreases the diffusion distance to mitochondria, the primary sites of oxygen utilization. Oxidative capacity also improves due to increases in the total tissue volume of mitochondria and the augmented activity of key enzymes of the Krebs cycle and electron transport chain.
In spite of these local tissue changes, low tolerance for muscle activity, a prominent feature of exposure to altitude, persists. One contributing factor is that the muscles of locomotion receive less blood flow in deference to the muscles of respiration (primarily the diaphragm); the HVR requires a greater proportion of cardiac output for the activity of breathing than at sea level, thereby limiting the perfusion of blood to skeletal muscles and reducing the effectiveness of local tissue changes. Another contributing factor is that the anaerobic mechanism for supplying fuel and supporting muscle activity at sea level is not invoked at altitude. Known as the “lactate paradox” (in reference to the anaerobic by-product of lactic acid), the anaerobic pathway remains intact but not utilized, apparently held in check by the local tissue signals of enhanced oxidative ability. Notably, at relatively high altitude (above 5300–6000 m), local tissue changes wane, and muscle becomes preferentially lost over fat, in contrast to weight loss in the form of fat at moderate altitude. A reduction in the size and diameter of muscle fibers at high altitude increases capillary density (the number of capillaries per unit volume of tissue) as a way to improve oxygen diffusion at the tissue site.
11.2.5 Chronic Illness
For populations living at or commuting routinely to altitude above 2500 m, with the notable exception of Tibetans and some Andean populations, chronic exposure to hypoxic conditions over a period of months to years can manifest clinically as two types of illness: chronic mountain sickness (CMS) and high-altitude pulmonary hypertension (HAPH). CMS tends to occur in the high-altitude areas of South America and also has been found in Leadville, Colorado (3100 m), whereas HAPH tends to occur in the high-altitude regions of Asia. Although symptoms for both conditions show considerable overlap, CMS denotes an excessive number of red blood cells, while HAPH refers to the predominance of pulmonary hypertension.
In the early phase of CMS , red blood cell mass can increase by as much as 50 % of sea level values, although the benefits remain limited and both mental and physical deterioration ensue over time. Main symptoms include headache, loss of mental acuity, fatigue, and muscle weakness. The later stages of the illness involve hypertrophy of the right heart ventricle and moderate to severe pulmonary hypertension. Pulmonary hypertension develops not only because of the rise in blood viscosity but also due to the lung’s two compensatory mechanisms: arterial vasoconstriction and pulmonary remodeling. Ultimately, the compensatory mechanisms operating in both CMS and HAPH throw great strain on the right heart and can lead to congestive heart failure. Unfortunately, mild to moderate pulmonary hypertension does not give rise to symptoms. When signs do appear, including headache, labored breathing, sleeplessness, and irritability, the right heart has already begun to fail .
Tibetans, in particular, given their long history of residing at high altitude, appear to have undergone a degree of physiologic adaptation and tend to show very little rise in pulmonary artery pressure (similar to altitude-adapted animals such as the yak) under hypoxic conditions. The lack of pulmonary hypertension is likely related, in part, to the prominent upregulation of nitric oxide production compared to other populations (see Beall et al. 2012). Nitric oxide, a powerful vasodilator, presumably facilitates sufficient oxygen delivery to tissues.
Although constitutional factors, such as age and genetic polymorphisms, contribute to the likelihood of developing CMS and HAPH, chronic exposure to physiologic mechanisms designed as short-term remedies for hypoxia at sea level, and with limited effectiveness at altitude, generates dysfunction along a graded continuum that manifests as poor health only once the condition has become severe and potentially life-threatening.
11.3 Metabolic Dysfunction
The metabolic system was designed by natural selection to accomplish three main tasks: convert food into energy, convert surplus energy into storage, and mobilize energy from storage when needed. Because the body requires a continuous supply of energy, especially in the form of glucose (the only fuel the brain normally uses), the existence of energy storage pathways allows the body to function without a constant intake of food. Surplus glucose can be repackaged and stored in the liver and skeletal muscle as glycogen and as triglycerides in fat tissue. Managing the metabolic cycles of feeding and fasting falls primarily under the purview of the pancreas, orchestrated via changes in the production of the hormones insulin and glucagon by specialized beta cells and alpha cells, respectively. When food supply ceases, energy metabolism shifts direction within a few hours, reconfigured by a change in the ratio of insulin to glucagon circulating in the bloodstream. The adrenal glands also play a role in the signaling system.
11.3.1 Glycogen Stasis
The human body was also designed for relatively prolonged periods of physical activity followed by rest (e.g., Bramble and Lieberman 2004). The lack of physical activity, especially involving the use of major muscles such as the quadriceps, sets the stage for subsequent metabolic unraveling along a dysfunctional continuum. Muscle contractions depend upon the oxidation of the two major metabolic fuels, glucose and fatty acids, to generate ATP for energy. Initial physical activity draws upon the available ATP pool, but within minutes skeletal muscle begins to rely on glucose derived from its glycogen stores. Although glycogen can support muscle activity for about an hour, fatty acids become the main fuel for prolonged physical activity, mobilized after about 15–20 min by the low insulin-to-glucagon ratio. Skeletal muscle at rest also relies on fatty acid oxidation.
When major muscles are not being used for sustained activity, glycogen stores no longer need to be replenished to the degree required by a body experiencing states of high energy utilization or flux. When the cycles of utilization and replacement of glycogen, in particular, dampen or cease altogether, the physiologic mechanisms for metabolic regulation begin to operate in ways that depart from the ancestral state. Under conditions of chronic inactivity, “glycogen stasis ” ensues, prompting muscles to adjust accordingly. Recognized clinically as a state of insulin resistance, skeletal muscles downregulate their responsiveness to insulin in order to match the low levels of physical activity beyond baseline maintenance. Downregulation primarily involves reducing the number of insulin receptors on the cell surface, thereby interfering with insulin’s binding capacity and ability to command glucose uptake by the cell. Binding sets in motion a series of signaling cascades within the cell that recruit and direct the glucose transporter (GLUT) to move to the surface and usher glucose into the cell. Tissue-specific glucose transporters include GLUT4 for skeletal muscle and adipose tissue, GLUT5 for the intestines, and GLUT2 for the kidneys and pancreatic beta cells .
11.3.2 Glucose Overload
In addition to glycogen stasis, a second major metabolic departure from the formative ancestral past is the consumption of high glycemic foods and drinks on a consistent basis. After a meal containing carbohydrates, most (80 %) of the circulating glucose is absorbed by tissues that do not require insulin for glucose uptake, mainly the brain (and erythrocytes). Uptake of the remaining peripheral glucose occurs mostly in insulin-dependent tissues, primarily skeletal muscle (85 %) and adipose tissue (10 %).
Not surprisingly, given the strong selective pressure to safeguard a steady supply of glucose to the brain, the human body comes well equipped with an array of physiologic mechanisms designed to compensate for stints of mild hypoglycemia. Mild hypoglycemia was probably encountered regularly in the ancestral past, not only on a short-term scale of hours, such as between feeding bouts and during physical activity, but also on a longer-term scale in the case of injury or infection extending to days and weeks.
The two principle regulators of hypoglycemia are glucagon and epinephrine (also called adrenaline , produced by the adrenal glands). Both hormones activate the transformation of glycogen stores into available glucose, with glucagon acting specifically on the liver and epinephrine acting on muscle tissue. Glucose derived from liver glycogen can be released readily into the bloodstream to fuel the brain and other tissues. Notably, glucose derived from muscle glycogen remains designated for muscle use only; muscles do not possess the enzyme (glucose-6-phosphatase) required to release glucose from cells. Along with activating the degradation of glycogen, glucagon and epinephrine stimulate the production of lipase, a key enzyme that promotes lipolysis and the breakdown of stored triglycerides into free fatty acids and glycerol. Although fatty acids cannot be converted into glucose, the liver can transform glycerol into glucose for release into the general circulation. In addition, glucagon instructs the liver to produce more low density lipoproteins (LDLs) needed to transport free fatty acids to muscle tissue, thereby ensuring that muscles receive the requisite fuel for sustained activity .
In contrast, insulin is the only hormone responsible for removing glucose from the bloodstream. This fact indicates that the difficulty of eliminating excess glucose was probably not encountered sufficiently in the ancestral past to warrant selection for multiple regulators. Physiologic asymmetries such as this are not unusual and tend to reflect the relative strength of past selective pressures. The human body, for example, possesses multiple mechanisms to avoid overheating and relatively few in response to cold.
The consumption of high glycemic foods and drinks typically invokes a robust but imprecise insulin response, referred to as “overshooting” on the part of the pancreas. (Mild hypoglycemia often follows, experienced as being hungry again.) This imprecise insulin response to high glycemic loads suggests a domain of somatic flexibility: selective pressures were not strong enough to require a precise calibration. In this way, the human organism could take full advantage of sporadic, short-lived (acute) opportunities to consume high glycemic foods, such as during honey season, without altering the existing mechanism—as long as the costs of imprecision remained relatively low. However, physiologic mechanisms not highly canalized by natural selection are also highly vulnerable to dysfunction.
Where does a deluge of glucose go? When glycogen stores are full, surplus glucose will be directed to fat tissue for storage. Since skeletal muscle is the primary target tissue for most of the peripheral glucose disposal after a meal, glycogen stasis combined with chronic exposure to repeated bouts of glucose overload inevitably leads to steady weight gain. In a study based on imaging technology, Petersen et al. (2007) demonstrated that lean subjects with insulin resistance in skeletal muscle tended to convert excess glucose from high carbohydrate meals directly to triglycerides rather than glycogen, unlike the lean normal control group. Although periodic or seasonal fluctuations in body fat characterize the nutritional ecology of foragers (e.g., Sherry and Marlowe 2007), steady or chronic increases in fat stores represent an overt sign that the body has stepped onto the path of metabolic dysfunction.
When viewed as a symptom of metabolic dysfunction already underway rather than a cause, steady weight gain only compounds the complications. For example, as an active endocrine organ, adipose tissue secretes various products (adipokines), including tumor necrosis factor-α (TNF-α) . Notably, TNF-α acts to decrease the expression of GLUT4, the glucose transporter in muscle tissue. If seen as an adaptive mechanism, this pathway could allow the body to build or restore fat reserves during periods of energy abundance (Pond 1998; Wells 2010) by directing a greater proportion of peripheral glucose uptake to adipose tissue. Yet, this pathway also helps to explain how chronic weight gain can exacerbate insulin resistance in muscle tissue, thereby contributing to the further accumulation of fat stores. If left to continue unabated, this metabolic state of affairs sets in motion a number of far-reaching deleterious effects .
11.3.3 Compensatory Hazards
How does the body deal with chronic exposure to repeated bouts of glucose overload in the face of glycogen stasis? As the downregulation of glucose uptake by muscles begins to slow down the rate of clearance, excess glucose remains in the circulation for longer periods, triggering the pancreatic beta cells to ratchet up the production and dispatch of greater quantities of insulin—but to little avail. A cruel irony follows: circulating levels of glucose continue to creep higher and higher in the presence of ever-increasing outputs of insulin .
Over time, the ongoing frustrated effort to compensate for creeping hyperglycemia itself becomes the source of dysfunction, as the pancreas begins to fail. Although the precise pathways are not fully understood, beta cells lose their capacity to manufacture insulin, attributed to beta cell exhaustion or “burnout” and a sensitivity to oxidative damage (Hennige et al. 2003; Rashidi et al. 2009). (The phenomenon of organ exhaustion is not unique to the pancreas and can occur in the adrenal glands.) With the onset of incapacitated beta cells, the insulin-to-glucagon ratio becomes a corrupted signal, eliciting compensatory responses to a perceived shortage of glucose that doesn’t exist. Plenty of glucose remains in the bloodstream, yet a sham state of hypoglycemia signaled by the predominance of glucagon stimulates the hepatic release of glucose from glycogen stores, thereby contributing to the escalating hyperglycemia. Not surprisingly, LDLs and fatty acids also pour into the bloodstream under the influence of glucagon, further compounding the repercussions.
11.3.4 Clinical Manifestations and Systemic Effects
The unraveling of metabolic regulation described above along a dysfunctional continuum maps onto the typology of clinically recognized metabolic disorders as follows: The initial appearance of high levels of glucose due to slow clearance (insulin resistance) is classified as impaired glucose tolerance (IGT) . Extremely high levels of circulating glucose (hyperglycemia) coupled with high compensatory insulin levels (hyperinsulinemia) define the Metabolic Syndrome. Beta cell failure, the metabolic equivalent of entering “the death zone” on Everest (above 8000 m), becomes recognized as Type-2 Diabetes (T2D ), usually accompanied by disordered lipid metabolism (hyperlipidemia, one of the prevailing effects of the compensatory hypoglycemic response) and the risk of long-term vascular complications. The relationship between metabolic disorders and cardiovascular disease takes hold in the systemic effects of metabolic dysfunction well before any clinical manifestations.
11.3.4.1 Cardiovascular Health
Metabolism comes at a cost even under the best of circumstances. The oxidation or burning of metabolic fuels (glucose and fatty acids) to release energy as ATP yields a number of deleterious by-products classified into two main types: reactive oxygen species (R OS ) known to damage DNA and advanced glycation end products (AGEs ) known to damage tissues. Chronic glucose overload not only increases the rate of oxidation and the generation of its harmful by-products but also the rate of glycation, a process whereby circulating glucose reacts and attaches to various proteins, such as hemoglobin and collagen. (Glycated hemoglobin is often used as a diagnostic tool and likely also underlies the association between metabolic dysregulation and anemia.) Circulating glucose can also react with metals, such as copper, becoming oxidized in the process. All of these processes lead to the formation of AGEs, which can inflict tissue damage by binding haphazardly to cell receptors, disrupting signaling cascades and inciting inflammatory responses.
The vascular endothelium seems especially vulnerable to the negative effects of excess glucose and AGEs in the bloodstream, showing signs of damage to the vascular walls well before any clinical markers of glucose dysregulation appear (Tooke and Hannemann 2000). Healthy endothelium has a smooth surface. Damage to the vascular walls sets the conditions for a potential range of cardiovascular-related disease. Microvascular pathologies, in which the small arteries are affected, appear tightly coupled with hyperglycemia; retinopathy (eye disease), neuropathy (nerve disease), and nephropathy (kidney disease) are all strongly associated with T2D (Nakagawa 2007). Notably, nephropathy is rarely seen in the absence of T2D. (Kidney dialysis is one of the most common and expensive treatments for T2D.) By the time symptoms appear, hyperglycemia has overwhelmed the kidneys and glucose has entered the urine. Glucose traveling through the renal tubules attracts water by osmosis, causing an increase in the frequency and volume of urination, often accompanied by thirst—the telltale signs of T2D.
Damage to the macrovascular system becomes evident in Syndrome X, characterized by hyperglycemia, hyperlipidemia, creeping hypertension, and the eventual appearance of atherosclerosis. Hypertension develops as damaged endothelial cells stimulate vascular remodeling, leading to a loss of vasodilation in the large arteries. Damage to the integrity of the endothelium also allows circulating lipids and LDLs to penetrate the arterial walls, where oxidation and inflammatory responses can ultimately lead to the formation of arterial plaque. Because the plaque core is thrombogenic (can rupture and trigger a blood clot), atherosclerosis increases the risk of heart attack and stroke. In addition, the steady accumulation of fat stores, which often accompanies metabolic dysfunction, tends to promote through the independent activity of adipokines a state of low-grade inflammation seen, in particular, in the arterial walls.
11.3.4.2 Brain Health
The systemic effects of metabolic dysfunction also appear to extend to the brain. T2D, for example, is a known risk factor for Alzheimer’s Disease (AD) , and AD patients have a higher risk of developing T2D (Correia et al. 2011). Although this association has been attributed to particular features of metabolic dysfunction, especially hyperglycemia, hypertension, and systemic inflammation (Cotman et al. 2007), two main differences between central and peripheral regulation raise the possibility that features common to T2D and AD may represent physiologic correlates, rather than direct causal pathways to cognitive impairment. First, the brain is highly selective about which substances can cross the blood–brain barrier, making the circulatory milieu in the brain distinct from the periphery. Second, the brain utilizes a unique set of complex pathways to deliver a steady supply of glucose to match demand. The hypothalamus, for example, has the capacity to “pull” glucose from the periphery, if necessary (such as during periods of psychological stress), by activating the sympathoadrenal system; catecholamines released from strategically placed nerve endings can interfere with both insulin production by beta cells and GLUT4 translocation in muscle and fat tissue (Peters 2011).
In my view, the linchpin linking Type-2 diabetes and Alzheimer’s disease likely entails chronic physical inactivity. One of the essential mechanisms for maintaining brain function involves the interaction of three prominent growth factors: insulin-like growth factor-1 (IGF-1) produced by the liver, VEGF , and brain-derived neurotropic factor (BDNF) . Levels of IGF-1 and VEGF increase in the periphery in response to physical activity and cross the blood–brain barrier to enter the brain. In the brain, the interactive effects of IGF-1 and VEGF induce the formation of new neurons and blood vessels, while the interactive effects of IGF-1 and BDNF serve to strengthen synapses (Cotman et al. 2007).
From an evolutionary perspective, it is not surprising that mounting evidence indicates that physical activity not only enhances learning and memory in all age groups, but also provides protective benefits against depression, Alzheimer’s disease, and age-related cognitive decline (Ratey 2008; Brito 2009; Hwang and Kim 2015). Physical activity regulates the availability of key substrates necessary for brain function. Rather than emphasizing the clinical value of physical activity as an intervention strategy and remedy “uniquely positioned to improve brain health (Cotman et al. 2007, p. 469),” it may be worthwhile to see chronic inactivity as uniquely positioned to undermine brain health.
11.4 Conclusion
The field of evolutionary medicine posits that modern environments interact with ancestral physiology in ways that can promote disease. Here, I propose that a dysfunctional continuum emerges whenever a departure from ancestral conditions requires the human body (and psyche) to function in the equivalent of an extreme environment. Ascending to the highest point on Earth, the summit of Mount Everest (8848 m or 29,035 ft), becomes possible only because the human body utilizes mechanisms designed to respond to hypoxic conditions—honed over evolutionary time—encountered in the formative past at sea level, mainly in contexts involving physical exertion or injury and infection. The kidney, for example, shows a remarkable resilience to altitude hypoxia (maintains a high degree of functionality) because it was designed to withstand severe reductions in blood flow and, therefore, oxygen delivery during physical activity and exertion at sea level. At the same time, the brain is especially vulnerable to hypoxia because the brain’s consumption of oxygen remains constant. (Balloonists found this out the hard way during flights in the early 1860s.)
Evolutionary biologists have pointed out for decades that many diseases of modernization, including metabolic disorders such as Type-2 diabetes, are largely preventable because they arise from contemporary lifestyle factors (Boyd Eaton et al. 1988; Fries et al. 1993; Boyd Eaton et al. 2002; Lindeberg 2012). Public health research continues to emphasize the role of prevention, showing evidence that investment in prevention is more cost effective, for example, than improved diabetes management, and the “considerable adverse impact of diabetes in terms of costs to society, health care systems, individuals and employers… increase[s] with diabetes duration as well as with the severity of the disease (Seuring et al. 2015, p. 825).” Medical prevention efforts often remain focused on better screening and diagnostic criteria, including for youth (Mancini 2009; Halpern et al. 2010; Canadian Task Force on Preventive Health Care 2012), and better managed-care models (Lee et al. 2011; Baptista et al. 2016). Improving diagnostic recommendations for metabolic disorders in the future based on the implications of the dysfunctional continuum framework presented here is a topic of ongoing research by the author.
Lieberman (2013, p. 351) asked in his concluding chapter, “How can an evolutionary perspective help chart a better future for the human body?” After identifying four possible approaches and eliminating three as essentially ineffective, Lieberman suggested that a government-regulated system of soft coercion or “nudges” could provide a promising path to prevention in alignment with evolutionary biology by changing the environment (approach 4), especially for children. Although relying on natural selection to sort the problem out (approach 1) or continuing to invest disproportionally in biomedical research and treatment (approach 2) hold little practical value for prevention, dismissing the efficacy of education and empowerment (approach 3) in favor of soft coercion may be premature—precisely because little is known about the efficacy of evolutionary biology knowledge itself as a prevention strategy. A small study I conducted with high school biology students in Cambridge, MA (Sherry, in prep) showed unequivocally that students who received instruction on diet and glucose regulation coupled with evolutionary biology shifted their perceptions about healthy food choices, compared to the control group of students who received instruction on diet and glucose regulation alone. Knowledge of evolutionary biology also led to precise dietary changes students intended to implement immediately, although follow-up studies would be needed to determine the extent of lasting behavioral change.
Given that health psychology and communication is a rapidly growing subfield in applied evolutionary medicine (Elton and O’Higgins 2008; Roberts 2011; Gibson and Lawson 2014), a conceptual framework based on evolutionary biology that identifies lifestyle behaviors as equivalent to entering an extreme environment conveys an immediate, intuitive sense of urgency and an implicit recognition that the human organism has strayed into a habitat for which it is ill equipped both physiologically and psychologically. Health risks associated with certain lifestyle factors, especially physical inactivity and dietary choices, may be more accurately perceived from this standpoint and effectively communicated as a public health message. From an evolutionary perspective, it makes sense why there is no inherent alarm system for major lifestyle departures from the formative ancestral past. At the same time, knowledge of evolutionary biology itself may provide an untapped yet promising tool for rendering the invisible extreme visible.
References
Baptista DR, Wiens A, Pontarolo R et al (2016) The chronic care model for type 2 diabetes: a systematic review. Diabetol Metab Syndr 8:7–13
Bateson G (1987) Steps to an ecology of mind: collected essays in anthropology, psychiatry, evolution and epistemology. Jason Aronson, Northvale
Beall CM, Laskowski D, Erzurum SC (2012) Nitric oxide in adaptation to altitude. Free Radic Biol Med 52:1123–1134
Boyd Eaton S, Shostak M, Konner M (1988) The Paleolithic prescription: a program of diet & exercise and a design for living. Harper & Row, New York
Boyd Eaton S, Strassman BI, Nesse RM et al (2002) Evolutionary health promotion. Prev Med 34:109–118
Bramble DM, Lieberman DE (2004) Endurance running and the evolution of Homo. Nature 432:345–352
Brito GNO (2009) Exercise and cognitive function: a hypothesis for the association of type II diabetes mellitus and Alzheimer’s disease from an evolutionary perspective. Diabetol Metab Syndr 1:1–7
Canadian Task Force on Preventive Health Care (2012) Recommendations on screening for type 2 diabetes in adults. Can Med Assoc J 184(15):1687–1696
Correia SC, Santos RX, Perry G et al (2011) Insulin-resistant brain state: the culprit in sporadic Alzheimer’s disease? Ageing Res Rev 10:264–273
Cotman CW, Berchtold NC, Christie L-A (2007) Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci 30:464–472
Dominiczak M (2007) Flesh and bones of metabolism. Elsevier, Philadelphia
Ellison PT (1990) Human ovarian function and reproductive ecology: new hypotheses. Am Anthropol 92:933–952
Ellison PT (2001) On fertile ground: a natural history of human reproduction. Harvard University Press, Cambridge
Elton S, O’Higgins P (eds) (2008) Medicine and evolution: current applications, future prospects. CRC Press, Boca Raton
Ewald PW (1994) Evolution and infectious disease. Oxford University Press, New York
Fries JF, Koop CE, Beadle CE et al (1993) Reducing health care costs by reducing the need and demand for medical services. N Engl J Med 329(5):321–325
Gibson MA, Lawson DW (eds) (2014) Applied evolutionary anthropology: Darwinian approaches to contemporary world issues. Springer, New York
Gluckman P, Hanson M (2006) Mismatch: the lifestyle diseases timebomb. Oxford University Press, Oxford
Greaves MF (2000) Cancer: the evolutionary legacy. Oxford University Press, New York
Halpern A, Mancini MC, Magalhães MEC et al (2010) Metabolic syndrome, dyslipidemia, hypertension and type 2 diabetes in youth: from diagnosis to treatment. Diabetol Metab Syndr 2:55–75
Hennige AM, Burks DJ, Ozcan U et al (2003) Upregulation of insulin receptor substrate-2 in pancreatic β cells prevents diabetes. J Clin Invest 112:1521–1532
Hwang HJ, Kim SH (2015) The association among three aspects of physical fitness and metabolic syndrome in a Korean elderly population. Diabetol Metab Syndr 7:112–117
Lee A, Siu CF, Leung KT et al (2011) General practice and social service partnership for better clinical outcomes, patient self efficacy and lifestyle behaviours of diabetic care: randomized control trial of a chronic care model. Postgrad Med J 87:688–693
Lieberman LS (2003) Dietary, evolutionary, and modernizing influences on the prevalence of type 2 diabetes. Annu Rev Nutr 23:345–377
Lieberman DE (2013) The story of the human body: evolution, health, and disease. Pantheon Books, New York
Lindeberg S (2012) Paleolithic diets as a model for prevention and treatment of western disease. Am J Hum Biol 24:110–115
Mancini MC (2009) Metabolic syndrome in children and adolescents—criteria for diagnosis. Diabetol Metab Syndr 1:20–23
Nakagawa T (2007) Uncoupling of the VEGF-endothelial nitric oxide axis in diabetic nephropathy: an explanation for the paradoxical effects of VEGF in renal disease. Am J Physiol Renal Physiol 292:F1665–F1672
Neal JM (2001) How the endocrine system works. Blackwell, Malden
Nesse RM, Williams GC (1994) Why we get sick: The new science of Darwinian medicine. Times Books, New York
Panter-Brick C, Worthman CM (eds) (1999) Hormones, health, and behavior: a socio-ecological and lifespan perspective. Cambridge University Press, Cambridge
Peters A (2011) The selfish brain: competition for energy resources. Am J Hum Biol 23:29–34
Petersen KF et al (2007) The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci U S A 104:12587–12594
Pollard TM (2008) Western diseases: an evolutionary perspective. Cambridge University Press, Cambridge
Pond CM (1998) The fats of life. Cambridge University Press, Cambridge
Rashidi A, Kirkwood TBL, Shanley DP (2009) Metabolic evolution suggests an explanation for the weakness of antioxidant defenses in beta-cells. Mech Ageing Dev 130:216–221
Ratey JJ (2008) Spark: the revolutionary new science of exercise and the brain. Little, Brown and Company, New York
Roberts C (ed) (2011) Applied evolutionary psychology. Oxford University Press, Oxford
Seuring T, Archangelidi O, Suhrcke M (2015) The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics 33:811–831
Sherry DS, Marlowe FW (2007) Anthropometric data indicate nutritional homogeneity in Hadza foragers. Am J Hum Biol 19:107–116
Stearns SC, Koella JC (eds) (2008) Evolution in health and disease. Oxford University Press, New York
Stearns SC, Nesse RM, Govindaraju DR, Ellison PT (2010) Evolution in health and medicine Sackler colloquium: evolutionary perspectives on health and medicine. Proc Natl Acad Sci 107(l):1691–1695
Tooke JE, Hannemann MM (2000) Adverse endothelial function and the insulin resistance syndrome. J Intern Med 247:425–431
Trevathan WR, Smith EO, McKenna JJ (eds) (2008) Evolutionary medicine and health: new perspectives. Oxford University Press, New York
Wells JCK (2010) The evolutionary biology of human body fatness: thrift and control. Cambridge University Press, Cambridge
West JB, Schoene RB, Luks AM, Milledge JS (eds) (2013) High altitude medicine and physiology, 5th edn. CRC, Boca Raton
Willingham DT (2009) Why don’t students like school? A cognitive scientist answers questions about how the mind works and what it means for your classroom. Jossey-Bass, San Francisco
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media New York
About this chapter
Cite this chapter
Sherry, D.S. (2017). From Novel to Extreme: Contemporary Environments and Physiologic Dysfunction. In: Jasienska, G., Sherry, D., Holmes, D. (eds) The Arc of Life. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-4038-7_11
Download citation
DOI: https://doi.org/10.1007/978-1-4939-4038-7_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-4036-3
Online ISBN: 978-1-4939-4038-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)