Abstract
Despite marked improvements in perinatal care, the smallest premature infant remains at high risk for the development of intraventricular hemorrhage. The pathogenesis of the hemorrhage includes vulnerable poorly supported capillary beds within the germinal matrix, with the propensity for rupture of these vessels under conditions where there are perturbations in systemic blood/venous pressures that maybe reflected in the cerebral circulation, particularly with a pressure passive state. Blood filling the ventricles, particularly when followed by hydrocephalus, and/or associated involvement of the periventricular white matter markedly increases the risk for neurologic deficits. The extent of hemorrhage can be minimized if the mother receives a course of antenatal steroids shortly prior to delivery, in the postnatal period with the early administration of indomethacin and by avoiding vascular perturbations. The management of post hemorrhagic hydrocephalus will depend on the size of the infant, the amount of blood in the ventricles and the intracranial pressure.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Intraventricular hemorrhage
- Prematurity
- Germinal matrix
- Cerebral autoregulation
- Periventricular white matter
- Post-hemorrhagic hydrocephalus
BE, a 1080 g, 26 weeks appropriate for gestational age, white male was born to a 27-year-old primigravida mother following an uncomplicated pregnancy except for premature onset of labor. Upon arrival in Labor and Delivery, the mother was fully dilated with the infant in the breech position. An immediate Cesarean section was performed. The infant was delivered flaccid with a heart rate of 70 beats per minute. Resuscitation included bag and mask ventilation followed by intubation. The Apgar scores were 4 at 1 min and 7 at 5 min, respectively. The infant was transferred to the neonatal intensive care unit where his clinical course was consistent with moderate-to-severe hyaline membrane disease and he received a dose of surfactant replacement therapy within the first 60 min of life. The ventilator support and oxygen requirements were lowered in response to improved pulmonary compliance, Over the initial 24 h, the infant continued to exhibit moderate costal retractions, and the FiO2 requirement gradually increased. A second dose of surfactant was administered at 18 h of age. Over the course of the day, the infant was noted to exhibit increasing irritability; however, he received no medication for sedation. Additional ancillary information revealed the following: the weight was now 970 g; the urine output for the initial 24 h was 0.9 ml/kg/h; a serum K+ was 6.3 meq/l with a serum bicarbonate of 20 meq/l. The hematocrit had fallen from 45 to 35 %. A cranial ultrasound scan was obtained at 30 h of age, because of the irritability and fall in hematocrit. The scan revealed a large amount of blood in the germinal matrix region that had extended into the left lateral ventricle, which was dilated and filled with blood—consistent with a grade 3 IVH. In addition there were increased echogenicity within the left fronto-parietal white matter (Fig. 11.1).
This case raises several important questions:
-
1.
Why did this premature infant develop a significant hemorrhage?
-
2.
Could the bleeding have been prevented?
-
3.
How should the infant be managed and evaluated over the next several days to weeks?
Background
The overall incidence of PV-IVH has declined over the past three decades; however the occurrence of severe hemorrhage remains substantial, particularly in the tiniest of the very-low-birth-weight population [1–3] (Table 11.1). Thus, approximately 26 % of infants of a gestational age between 23 and 25 weeks and 12 % between 26 and 27 weeks still develop the most severe forms of hemorrhage [3]. This is highly relevant because as survival of infants born at the cutting edge of viability continues to increase, severe hemorrhage rates are likely to increase, and with them long-term neurodevelopmental deficits.
Neuropathology
The primary lesion is bleeding from vessels within the periventricular subependymal germinal matrix located between the caudate nucleus and thalamus at the level of the foramen of Monro [2] (Fig. 11.2). The matrix is a transient gelatinous region that provides poor support for a large, immature network of blood vessels primarily supplied by Heubner’s artery, a branch of the anterior cerebral artery [4]. The venous drainage also appears to be important with regard to the risk for bleeding. Thus the drainage includes the terminal, choroidal, and thalamo-striate veins that lead to the internal cerebral vein. The blood flow then makes a “U-turn” in the subependymal region at the level of the foramen of Monro, where most of hemorrhage originates [2]. This creates the potential for obstruction of the venous drainage resulting in venous distention with obstruction of the terminal and medullary veins, with subsequent rupture. The primary vascular source of PV-IVH has not been clearly established. Thus the initial descriptions suggested a venous origin of hemorrhage [2] while subsequent pathologic studies described it as emanating from capillary or arterial vessels [4]. Based on studies conducted over the years it is most likely, that PV-IVH results from forces acting upon both the arterial and venous circulations [1, 2].
Importance of the Germinal Matrix
The germinal matrix is an active site of active cellular proliferation, and is a source of both neuronal precursors early in gestation as well as glial elements that become oligodendroglia and astrocytes in the third trimester [2]. The matrix involutes after approximately 32 weeks and by term gestation, this region is essentially absent. Destruction of the matrix as a result of hemorrhage may result in impairment of myelination, brain growth, and subsequent cortical development [2].
Grading the Hemorrhage
The hemorrhage may be confined to the germinal matrix region (grade 1 IVH) or it may extend and rupture into the adjacent ventricular system (grade II or III IVH) depending on the extent of blood, or may extend into the adjacent white matter (termed a grade IV IVH or intraparenchymal echogenicity (IPE)) [2, 5, 6] (Fig. 11.1). The latter lesion, which is often unilateral, represents an area of hemorrhagic necrosis of varying size within periventricular white matter, dorsal and lateral to the external angle of the lateral ventricle [2, 6, 7].
Pathogenesis of IVH
In general terms, three factors appear to be central to the genesis of hemorrhage. The first relates to inherent vulnerability of the germinal matrix, with immature vessels and poorly supportive gelatinous matrix as described above [2]. The second relates to the concept of a pressure passive circulation often referred to as loss of autoregulation, and the third relates to perturbations in cerebral blood which are common in the sick premature infant.
Cerebral Autoregulation and Pressure-Passive Circulation
Autoregulation is defined as a state whereby CBF remains constant as cerebral perfusion pressure varies over a certain range [8]. The mean arterial pressure at which CBF decreases during hypotension is termed the lower limit, and the arterial pressure at which CBF increases is called the upper limit of autoregulation. In newborn animals, the range of blood pressures at which CBF remains constant is lower than in adult animals [9, 10]. More importantly, in fetal lambs, the resting blood pressure is only slightly higher than the lower limit of the autoregulatory curve [10]. If a similar situation exists in newborn infants, moderate hypotension could result in reduced CBF and create the potential for ischemic brain injury. Evidence has indicated that the autoregulatory response remains intact in human neonates with mild asphyxiation or who have minimal respiratory distress [2]. By contrast seminal data of Lou and colleagues [11] derived from 19 newborn infants with varying degrees of respiratory distress studied in the first hours of life were the first to indicate that CBF varied considerably with spontaneous variations in blood pressure, suggesting that autoregulation was, in fact, lacking. Subsequent studies over the subsequent years utilizing different methods to assess CBF or cerebral blood flow velocity including Doppler, near-infrared spectroscopy, and xenon have supported the concept of a pressure passive cerebral circulation in the sick infant; that is, CBF varies directly with changes in systemic blood pressure [12–15].
To summarize, although intact cerebral autoregulation has been documented in the premature infant, it appears to function within a limited blood pressure range, and is likely to be absent particularly in the sick hypotensive preterm infant [12–15]. This clinical state places the developing brain at great risk for injury during times of hypotension and or elevated blood pressures .
Intravascular Perturbations
Evidence has pointed to a critical role for intravascular factors and specifically perturbations in ABP as a major mechanism of capillary rupture and hemorrhage. First, the cerebral circulation of the sick infant was considered pressure passive (see above) [12–15]. Second, experimental studies indicated that germinal matrix hemorrhage could be produced by systemic hypertension with or without prior hypotension [16, 17]. Third, infants with lower mean ABP in the first postnatal days and infants who received rapid volume expansion to correct hypotension were more likely to develop IVH [18–20].
In the original pathologic description of IVH, elevations in venous pressure were proposed as an important source of hemorrhage, based in part on the previously described venous drainage of germinal matrix and white matter [2]. Indeed simultaneous increases in venous pressure were observed in infants who exhibit variability in ABP, such as with respiratory distress syndrome (RDS) and associated complications, e.g., pneumothorax or pulmonary interstitial emphysema, or with mechanical or high-frequency ventilation [21–23].
To summarize, the cumulative data suggested that there is a significant contribution from both arterial and venous perturbations to the development of IVH. Over the years, studies have indicated that these intravascular responses can be modulated by additional factors, i.e., inflammation associated with chorioamnionitis (negative influence) [24] or the administration of glucocorticoids to the mother (positive influence) [25, 26].
Periventricular White Matter Injury (WMI) Associated with IVH
The cause of the WMI associated with hemorrhage still remains unclear. The original hypothesis was that the intraparenchymal lesion represented an “extension” of hemorrhage from the germinal matrix or lateral ventricle into previously normal periventricular white matter. However subsequent neuropathologic data indicate that the intraparenchymal lesion represents an area of hemorrhagic necrosis [2, 5, 7]. The WMI appears to be closely linked to the adjacent hemorrhage and two potential pathways have been proposed to explain this intricate relationship. The first suggests a direct relationship to the hemorrhage based on several clinical observations. First, the WMI is always noted concurrent with or following a large GM and/or IVH, and is rarely if ever observed prior to the hemorrhage, and second the WMI is always observed ipsilateral to the side of the larger hemorrhage with bilateral bleeding [1, 2]. This consistent relationship between the GM and WMI may in part be explained by the venous drainage of the deep white matter as described previously. A second explanation is that the WMI evolves de novo and the IVH and WMI occur concurrently. Since both the GM and the periventricular white matter are border zone regions, the risk for ischemic injury increases during periods of systemic hypotension, particularly in the face of a pressure passive cerebral circulation [1, 2]. Hemorrhage in these regions may then occur as a secondary phenomenon i.e. reperfusion injury. In support of this theory is the fairly consistent observation of the simultaneous detection of PV-IVH and WMI by cranial ultrasound imaging. Moreover elevated hypoxanthine and uric acid levels, perhaps as markers of reperfusion injury, have been observed on the first postnatal day in infants who subsequently developed WMI [27, 28].
Case Continued
The infant continued to exhibit moderate respiratory distress and developed a left sided pneumothorax requiring chest tube placement. The arterial blood gases showed moderate hypercarbia (pCO2 55 to 58 mmHg and mild acidosis—pH 7.20–7.26). The hematocrit continued to fall to 22 % on DOL 4. A repeat cranial sonogram revealed more prominent “echoes” within the left fronto-parietal white matter, and the lateral ventricles were more distended as a result of increased hemorrhage. Serial sonograms over the first 6 weeks demonstrated progressive enlargement of the lateral, third, and fourth ventricles (Fig. 11.3).
Question
-
1.
Why did the hemorrhage progress?
-
2.
What is the cause of the progressive ventriculomegaly?
Linking Systemic and Cerebral Vascular Perturbations in Infants with Respiratory Distress Syndrome (RDS) to PV-IVH
Perturbations on the Arterial Side
Numerous studies established an association between RDS its complications, i.e., pneumothorax and IVH [22, 23]. The mechanisms linking the two conditions appear to be mediated via systemic perturbations including fluctuations or rapid increases in blood pressure in large part related to respiratory mechanics often precipitated by the infant breathing out of synchrony with the ventilator and/or in associations with complications such as a pneumothorax [23, 29]. Simultaneous perturbations on the venous side were noted with resultant increases in venous pressure [21]. In a series of studies conducted in sick intubated and ventilated premature infants, these striking systemic changes with parallel changes in the cerebral circulation were associated with the subsequent development of IVH, and could be prevented by eliminating the fluctuations [23, 30]. Importantly over time, the advent of newer ventilators that work in tandem with the infants own respiratory efforts coupled with the antenatal use of steroids perhaps by stabilizing the germinal matrix vessels has made this association less prominent [25, 26]. However in a susceptible infant (no exposure to antenatal steroids) close attention to fluctuations in blood pressure should be a priority, and when present should be minimized .
Perturbations in Venous Pressure
Fluctuations in venous pressure simultaneous with the ABP perturbations in preterm infants with RDS who developed PV-IVH have also been observed [21]. The fluctuations or increases in venous pressure can be exacerbated by the use of higher mean airway pressures such as may be observed with high-frequency oscillatory ventilation, or pneumothorax. The potential importance of these venous fluctuations in the genesis of hemorrhage is intertwined with the venous drainage of the deep white matter and in particular the peculiar U-shaped turn ending at the terminal vein in the region of the germinal matrix. Increases in venous pressure in this region raise the likelihood of venous distension and resultant obstruction of the terminal and medullary veins resulting in a venous infarction.
Hypercarbia and Intraventricular Hemorrhage
The potential contribution of hypercarbia has only in recent years been clearly delineated in premature infants [31]. Thus in a study undertaken in the first week of life in VLBW infants, increasing PaCO2 resulted in an increase in CBF and progressive impairment of cerebral autoregulation [31]. Hypercapnia defined by a maximum PaCO2 recorded during the first 3 days of life has also been associated with severe IVH. In a retrospective cohort study of 574 VLBW infants, as the maximum PaCO2 increased from 40 to 100 mmHg, the probability of severe IVH increased from 8 to 21 % [32]. In a single-center retrospective review of 849 infants weighing <1250 g extremes in PaCO2, both low and high, as well as fluctuations in PaCO2 during the first 4 days of life increased the risk of severe IVH [33]. These cumulative observations indicate that extremes in PaCO2 should be avoided during the period in which infants are at high risk of IVH. This is highly relevant since permissive hypercapnia has been advocated as a ventilator strategy to minimize barotrauma to the lungs of preterm infants, and thus prevent the evolution to chronic lung disease [34] (Fig. 11.4).
Surfactant Administration and PV-IVH
The introduction of surfactant administration to reduce the severity of RDS in the late 1980s was the most important development in the management of sick premature infants. Since surfactant reduced the severity of RDS as well as the rate of pneumothorax, it was postulated that it would also lead to a decrease in the rates of IVH. However, this was not borne out in the many surfactant trials [35]. This lack of effect has been attributed to the impact of surfactant administration on fluctuations of CBF in sick preterm infants who have pressure passive circulation and the rapid changes of PaCO2 and PaO2 that may subsequently lead to brain injury [36, 37].
Post-hemorrhagic Hydrocephalus (PHH)
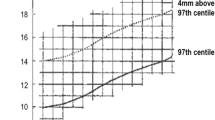
PHH complicates approximately 40–50 % of severe IVH [2]. The progression of PHH may be rapid, i.e., days, and in such cases, it is usually associated with raised intracranial pressure . The obstruction under such circumstances appears to be secondary to an impairment of cerebrospinal fluid absorption caused by particulate clot usually demonstrated by ultrasound scan. This may be at the foramen of Monroe or the aqueduct of Sylvius. Treatment is usually immediate, via external drainage above the site of obstruction. More commonly, a communicating hydrocephalus evolves from 1 to 4 weeks following the diagnosis of hemorrhage. The hydrocephalus is commonly secondary to an obliterative arachnoiditis distal to the outflow of the fourth ventricle. The clinical criteria of evolving hydrocephalus, i.e., full anterior fontanel and rapid head growth, do not appear for days or weeks after ventricular dilation has already been present. Possible explanations for this discrepancy include the relative excess of water in the centrum semiovale and the relatively large subarachnoid space. Thus, serial scans are critical to follow for the evolution of PHH.
Understanding the natural history of PHH is important to consider when deciding upon management strategy. The natural tendency is to immediately intervene. However, in most cases, the ventricular dilation is under normal pressure and slowly progresses [38]. In approximately half the cases, the progression ceases usually within the first month without intervention. In the remaining 50 % the hydrocephalus is progressive and under increased pressure, and intervention becomes mandatory [38].
The management of PHH will depend on the size of the infant, the amount of blood in the ventricles, and the intracranial pressure. Many neurosurgeons prefer not to place a ventriculoperitoneal shunt until the infant’s weight is at least >1500 g. In the smallest premature infants, temporizing diversion techniques to control ventricular size have evolved and include the placement of an external ventricular drain or subgaleal shunt, serial lumbar punctures, and/or the use of drugs, namely acetazolamide [38–40].
Clinical Manifestations of Hemorrhage
The time to initial diagnosis hemorrhage has shifted to a later onset in recent years [41]. Thus, in the initial descriptions of PV-IVH, the majority of cases, i.e., 90 %, evolved within the first 72 h of postnatal life [42]. However, in a subsequent report, the onset of IVH was delayed beyond the first week of life in a substantial number of cases [41]. Thus, for neonates <28 weeks or less than 1000 g, IVH was diagnosed by days 3–5 in approximately 80 % of infants, with the remaining cases noted beyond the tenth postnatal day. This changing pattern likely reflects the complexity of disease in the tiniest infants and the extent of supportive medical care, i.e., prolonged use of high-frequency ventilation. Most cases (up to 70 %) continue to remain clinically occult, and are only detected by screening cranial ultrasound imaging [2]. Those infants with severe IVH frequently exhibit clinical signs including a bulging fontanel, seizures, fall in hematocrit, hyperglycemia, metabolic acidosis, and pulmonary hemorrhage.
Strategies to Prevent Severe IVH
General Considerations
Based on accumulating data over the years, several fundamental factors should be considered when assessing the risk for IVH. The development of IVH appears to be strongly influenced in part by the administration of antenatal glucocorticoids [25, 42–44] and/or the presence of histologic chorioamnionitis/fetal vasculitis [45] (Table 11.2). Postnatal markers of infants at high risk for IVH include extreme prematurity , i.e., <1000 g, male gender, and intubated with RDS [1–3, 38]. For infants with RDS, the risk for IVH is even greater when there are associated perturbations in arterial and venous pressures [29, 30]. The perturbations can be minimized with careful ventilator management including the use of synchronized mechanical or assist control ventilation, sedation, or in more difficult cases with paralysis [30]. By contrast the risk for severe IVH in the non-intubated infant is low, i.e., <10 % [38].
Perinatal Glucocorticoid Administration
The single most important “intervention” shown to significantly reduce the development of IVH has been a short course of antenatal glucocorticoid steroids administered to augment pulmonary maturation [25, 42, 43]. An effect that is dose dependent (Table 11.3). The relative risk (RR) for severe IVH following any antenatal glucocorticoid exposure 0.54 (95 % CI 0.43–0.69) [25]. In a recent review the number of mothers needed to treat with antenatal steroids to prevent one case of IVH was 9 (95 % confidence interval 6–19) [46]. The mechanisms whereby glucocorticoids reduce severe IVH remain unclear, but may relate to less severe RDS, or higher resting ABP [25, 47]. The type of glucocorticoid also appears be important with antenatal exposure of dexamethasone, but not betamethasone associated with an increased risk of WMI in premature infants [48].
Postnatal Strategies
Postnatal medications used to prevent hemorrhage have included phenobarbital [49, 50], vitamin E [51], and indomethacin [52, 53]. While there was initial enthusiasm for the use of the first two medications, significantly different outcomes have not been described. Noteworthy, in one large randomized study, infants who received phenobarbital exhibited a higher incidence of severe IVH when compared to controls [50]. The early postnatal administration of indomethacin has been associated with a significant reduction in severe IVH; however the neurocognitive deficits were comparable between groups [53] (Table 11.3).
Outcomes
The infant with severe IVH is at highest risk for adverse motor and cognitive deficits. This is related in part to the extent of the white matter involvement noted by cranial ultrasound imaging or MRI [54]. Thus with a large IPE (>1 cm in diameter) the outcome is invariably poor with major motor and cognitive defects consistently noted at follow-up [1, 2, 5, 6]. With smaller lesions (<1 cm in diameter), the outcome is less precise and a small percentage (approximately 20 %) may even have a normal outcome [2, 5]. However, as noted previously, the issue is more complicated and even infants with a normal ultrasound scan as well as those with lesser grades of hemorrhage are at risk for motor as well as cognitive deficits. Thus major neurologic disability was noted in 5–10 % of infants and a MDI < 70 and in 25 % of cases infants with a normal cranial sonograms and major neurologic disability noted in 13 %, and a mental developmental index < 70 noted in 45 % of infants with lesser grades of hemorrhage (grade 1 and 2) [55, 56]. However, the comparable neurodevelopmental outcome for infants with and without IVH in the indomethacin study (Table 11.3) clearly indicates that the genesis of brain injury in the sick premature infant is much more complex than can be deduced from the neonatal neurosonographic appearance.
Future Directions
In recent years, white matter injury often in the absence of IVH is the predominant finding observed on MRI in very-low-birth-weight infants [1, 2]. Since antenatal glucocorticoids significantly reduce IVH, the target population should be those VLBW who deliver rapidly or emergently with minimum intrapartum care. In addition close attention to blood pressure should be a priority so as to avoid hypotension and/or perturbations. It is this group of infants who may derive benefit from early indomethacin administration. Understanding the mechanisms of white matter injury remains an important avenue for future research.
Pediatrician’s Perspective
-
1.
The management of children with very low birth weights and resultant intraventricular hemorrhage is almost entirely within the domain of neonatal intensivists. However, delayed appearance of hydrocephalus may occur within the general pediatrician’s window of post-PICU surveillance.
-
2.
Close surveillance of head circumference and assessment of sutures and fontanel’s remain as the single most important feature of the clinical examination when concerned about IVH and its immediate consequences.
-
3.
Delayed consequences of IVH are quite varied. Development of cerebral palsy for example, can occur many years after the child has been discharged from NICU follow-up clinics and becomes the responsibility of the pediatrician to recognize and help triage.
-
4.
Referrals to neurosurgical care should occur with divergent macrocephaly, splayed sutures, bulging fontanels, irritability of uncertain etiology, increased tone/spasticity, and asymmetric neurologic examination. Often head ultrasound is a simple and accessible route of imaging these children to begin the process of establishing an urgency to the referral.
References
Shalak L, Perlman M. Hemorrhagic-ischemic cerebral injury in the preterm infant: current concepts. Clin Perinatol. 2002;29:745–63.
Volpe J. Neurology of the newborn. 5th ed. Philadelphia, PA: Saunders/Elsevier; 2008.
Stoll BJ, Hansen NE, Bell EF, et al. Neonatal outcomes of extremely premature infants from the NICHD neonatal research network. Pediatrics. 2010;126:443–56.
Hambleton G, Wiggelsworth JS. Origin of intraventricular hemorrhage in the preterm infant. Arch Dis Child. 1976;57:651–5.
Guzzetta F, Schackelford GD, Volpe S, et al. Periventricular intraparenchymal echodensities in the premature newborn: critical determinant of neurologic outcome. Pediatrics. 1986;78:945–1006.
Perlman JM, Rollins N, Burns D, et al. Relationship between periventricular intraparenchymal echodensities and germinal matrix-intraventricular hemorrhage in the very low birth weight neonate. Pediatrics. 1993;91:474–80.
Gould SJ, Howard S, Hope PL, Reynold EO. Periventricular intraparenchymal cerebral hemorrhage in preterm infants: the role of venous infarction. J Pathol. 1987;151:197–202.
Harper AM. Autoregulation of cerebral blood flow influence of the arterial blood pressure on the blood flow through the cerebral cortex. J Neurol Neurosurg Psychiatry. 1966;29:398.
Hernandez MJ, et al. Autoregulation of cerebral blood flow in the newborn dog. Brain Res. 1980;184:199.
Papile LA, et al. Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res. 1985;19:159.
Lou HC, et al. Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr. 1979;94:118–25.
Pryds O, et al. Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr. 1989;115:638–45.
Pryds O, et al. Cerebral blood flow reactivity in spontaneously breathing preterm infants shortly after birth. Acta Paediatr Scand. 1990;79:391.
Tsuji M, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 2000;106:625.
Kaiser JR, Gauss CH, Williams DK. Surfactant acutely affects cerebral and systemic hemodynamics and gas exchange in very low birth weight infants. J Pediatr. 2005;144:809–14.
Goddard-Finegold J, Armstrong D, Zeller RS. Intraventricular hemorrhage following volume expansion after hypovolemic hypotension in the newborn beagle. J Pediatr. 1982;100:796–9.
Ment LR, Stewart WB, Duncan CC, et al. Beagle puppy model of intraventricular hemorrhage. J Neurosurg. 1982;57:219–23.
Bada HS, Korones SB, Perry EH, et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr. 1990;117:607–14.
Goldberg RN, Chung D, Goldman SL, et al. The associations of rapid volume expansion and intraventricular hemorrhage in the preterm infant. J Pediatr. 1980;96:1060–3.
Miall-Allen VM, De Vries LS, Whitelaw AG. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987;62:1068–9.
Perlman JM, Volpe JJ. Are venous circulatory changes important in the pathogenesis of hemorrhagic and/or ischemic cerebral injury? Pediatrics. 1987;80:705–11.
Hill A, Perlman JM, Volpe JJ. Relationship of pneumothorax to the occurrence of intraventricular hemorrhage in the premature newborn. Pediatrics. 1982;69:144–9.
Perlman JM, McMenamin JB, Volpe JJ. Fluctuating cerebral blood flow velocity in respiratory distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med. 1983;309:204–9.
Yanowitz TD, Potter DM, Bowen A, Baker RW, Roberts JM. Variability in cerebral oxygen delivery is reduced in premature neonates exposed to chorioamnionitis. Pediatr Res. 2006;59:299–304.
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006; (3): CD004454.
Salhab W, Hyman L, Perlman JM. Partial or complete antenatal steroids treatment and neonatal outcome in extremely low birth weight infants less than or equal to 1000 grams: is there a dose dependent effect? J Perinatol. 2004;23:668–72.
Russell GAB, Jeffers G, Cook RWI. Plasma hypoxanthine: a marker for hypoxic-ischemic induced periventricular leukomalacia? Arch Dis Child. 1992;67:388–92.
Perlman JM, Risser R. Relationship of uric acid concentrations and severe intraventricular hemorrhage/leukomalacia in the premature infant. J Pediatr. 1998;132:436–9.
Perlman JM, Thach BT. Respiratory origin of fluctuations in arterial blood pressure in premature infants with respiratory distress syndrome. Pediatrics. 1988;81:399–403.
Perlman JM, Goodman S, Kreusser KL, et al. Reduction of intraventricular hemorrhage by elimination of fluctuating cerebral blood flow velocity in preterm infants with respiratory distress syndrome. N Engl J Med. 1985;312:1253–7.
Kaiser JR, Gauss CH, Williams DK. The effects of hypercapnia on cerebral autoregulation in ventilated very low birth weight infants. Pediatr Res. 2005;58(5):931–5.
Kaiser JR, Gauss CH, Pont MM, Williams DK. Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol. 2006;26(5):279–85.
Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N. Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics. 2007;119(2):299–305.
Woodgate P. G., Davies M. W. Permissive hypercapnia for the prevention of morbidity and mortality in mechanically ventilated newborn infants. Cochrane Database Syst Rev 2001; (2): CD002061.
Jobe AH. Pulmonary surfactant therapy. N Engl J Med. 1993;328:861–8.
Nuntnarumit P, Bada HS, Yang W, Korones SB. Cerebral blood flow velocity changes after bovine natural surfactant instillation. J Perinatol. 2000;20(4):240–3.
Kaiser JR, Gauss CH, Williams DK. Surfactant administration acutely affects cerebral and systemic hemodynamics and gas exchange in very-low-birth-weight infants. J Pediatr. 2004;144(6):809–14.
Hill A, Volpe JJ. Normal pressure hydrocephalus in the newborn. Pediatrics. 1981;68:623–9.
Ventriculomegaly Trial Group. Randomized trial of early tapping in neonatal post-hemorrhagic ventricular dilation. Arch Dis Child. 1990;114:611.
Shinnar S, Gammar K, Bergman EW, et al. Management of hydrocephalus, use of acetazolamide and furosemide to avoid cerebrospinal fluid shunts. J Pediatr. 1985;107:31–5.
Perlman JM, Rollins N. Surveillance protocol for the detection of intracranial abnormalities in premature neonates. Arch Pediatr Adolesc Med. 2000;154(8):822–6.
Perlman JM, Volpe JJ. Intraventricular hemorrhage in the extremely small premature infant. Am J Dis Child. 1986;140:1122–4.
Kari MA, Eronen M, Virtanen M, Hallman M, Teramo K, Koivisto M, et al. Prenatal dexamethasone treatment in conjunction with rescue therapy of human surfactant: a randomized placebo-controlled multicenter study. Pediatrics. 1994;93:730–6.
Leviton A, Dammann O, Allred EN, Kuban K, Pagano M, Van Marter L, et al. Antenatal corticosteroids and cranial ultrasonographic abnormalities. Am J Obstet Gynecol. 1999;181(4):1007–17.
Hansen A, Leviton A. Labor and delivery characteristics and risks of cranial ultrasonographic abnormalities among very-low-birth-weight infants. The Developmental Epidemiology Network Investigators. Am J Obstet Gynecol. 1999;181(4):997–1006.
Halliday H. Use of steroids in the perinatal period. Paediatr Respir Rev. 2004;5:s321–7.
Garland JS, Buck R, Leviton A. Effect of maternal glucocorticoid exposure on risk of severe intraventricular hemorrhage in surfactant-treated preterm infants. J Pediatr. 1995;126:272–9.
Baud O, Foix-L’Helias L, Kaminski M, Audibert F, Jarreau P, Papiernik E, et al. Antenatal glucocorticoid treatment and cystic periventricular leukomalacia in very premature infants. N Engl J Med. 1999;341(16):1190–6.
Donn S, Roloff DW, Goldstein GW. Prevention of intraventricular hemorrhage in preterm infants by phenobarbitone: a controlled trial. Lancet. 1981;2:215–7.
Kuban KC, Leviton A, Krishnamoorthy KS, Brown E, Littlewood-Teele R, Baglivo JA, et al. Neonatal intracranial hemorrhage and phenobarbital. Pediatrics. 1986;77:443–50.
Sinha S, Davis J, Toner N, Bogle S, Chiswick M. Vitamin E supplementation reduces frequency of periventricular hemorrhage in very preterm infants. Lancet. 1987;11:466–71.
Ment LR, Ehrenkranz RA, Duncan CC, Scot DT, Taylor KJW, Katz K, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. 1994;94:543–50.
Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, et al. Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N Engl J Med. 2001;344(26):1966–72.
Woodward LJ, Anderson PJ, Austin NC, et al. Neonatal MRI to predict neurodevelopment outcome in preterm infants. N Engl J Med. 2006;355:685–94.
Laptook AR, O’Shea TM, Shankaran S, Bhaskar B. Adverse neurodevelopmental outcomes among extremely low birth weight infants with a normal head ultrasound: prevalence and antecedents. Pediatrics. 2005;115:673–80.
Patra K, Wilson-Costello D, Taylor HG. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: effects on neurodevelopment. J Pediatr. 2006;149:169–73.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media New York
About this chapter
Cite this chapter
Perlman, J.M. (2017). Intraventricular Hemorrhage in the Premature Infant. In: Greenfield, J., Long, C. (eds) Common Neurosurgical Conditions in the Pediatric Practice. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3807-0_11
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3807-0_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3805-6
Online ISBN: 978-1-4939-3807-0
eBook Packages: MedicineMedicine (R0)