Abstract
Hydrocephalus comprises a high proportion of children managed at neurosurgical centers. One of the leading causes of hydrocephalus in infants and children is prematurity-related IVH. Intraventricular hemorrhage is the commonest type of brain injury in premature infants and the most prevalent type of neonatal intracranial hemorrhage (Vasileiadis et al. 2004). The primary event in the production of posthemorrhagic hydrocephalus (PHH) consists of bleeding within the periventricular germinal matrix. The subependymal matrix is a highly cellular and richly vascular primitive tissue where neurons and glial precursor cells are formed, that afterwards migrate to the superficial cortical layers. The hemorrhage may destroy and cause loss of the precursor cells producing this particular type of brain injury. The incidence of IVH is directly related to the degree of prematurity. The initial intensity of the hemorrhage and its eventual extension account for the different degrees of the associated brain damage. Numerous factors are involved in the production of germinal matrix hemorrhage. Accordingly, preventive measures are to be directed toward the avoidance of these factors. In this chapter, we will discuss the current views on the pathophysiology, diagnosis, and management of both IVH and PHH.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Introduction
Hydrocephalus comprises a high proportion of children managed at neurosurgical centers. One of the leading causes of hydrocephalus in infants and children is prematurity-related IVH. Intraventricular hemorrhage is the commonest type of brain injury in premature infants and the most prevalent type of neonatal intracranial hemorrhage (Vasileiadis et al. 2004). The primary event in the production of posthemorrhagic hydrocephalus (PHH) consists of bleeding within the periventricular germinal matrix. The subependymal matrix is a highly cellular and richly vascular primitive tissue where neurons and glial precursor cells are formed, that afterwards migrate to the superficial cortical layers. The hemorrhage may destroy and cause loss of the precursor cells producing this particular type of brain injury. The incidence of IVH is directly related to the degree of prematurity. The initial intensity of the hemorrhage and its eventual extension account for the different degrees of the associated brain damage. Numerous factors are involved in the production of germinal matrix hemorrhage. Accordingly, preventive measures are to be directed toward the avoidance of these factors. In this chapter, we will discuss the current views on the pathophysiology, diagnosis, and management of both IVH and PHH.
Understanding Terms and Concepts
Commonly utilized terms referring to children’s age, gestation, and birth weight are summarized in Table 1 (Engle 2004) and those referring to IVH and associated lesions are shown in Table 2. Intraventricular hemorrhage refers to bleeding that typically originates in the subependymal germinal matrix and that extends to the ventricles. The germinal layer contains precursor cells of neurons and glia and is a highly vascular zone of the developing brain. The blood vessels of the subependymal germinal matrix are very fragile and susceptible to hemorrhage. If bleeding in the germinal matrix is large enough, the ependymal layer ruptures and the blood escapes from this zone to the ventricular cavities causing an IVH (Ballabh 2014). The terms intraventricular, subependymal, periventricular, and germinal matrix hemorrhage are often used interchangeably. An intraventricular extension of a germinal matrix hemorrhage occurs in approximately 80% of cases (Tsitouras and Sgouros 2011).
The term ventriculomegaly refers to an abnormal increase in the ventricular size and that of posthemorrhagic ventricular dilatation refers to the enlargement of the ventricles that follows the intraventricular irruption of blood from the germinal matrix. A part of neonates with IVH develop posthemorrhagic hydrocephalus either by obstruction of the normal CSF pathways or by impairment of the CSF absorption at the cerebral convexities.
The ventricular dilatation seen in cerebral atrophy is not synonymous of hydrocephalus. In atrophy, the ventricles are not rounded, they enlarge slowly, and the infants’ head enlargement is not exaggerated. Cerebral damage can be subtle and, even in cases of uncomplicated IVH, some authors find a reduction in brain volume (Vasileiadis et al. 2004). PHH refers to progressive ventriculomegaly that is accompanied by clinical manifestations of intracranial hypertension.
The most commonly used scale for reporting the severity of IVH by US is the Papile grading scale shown in Table 2 (Robinson 2012). IVH grade I refers to bleeding restricted to the subependymal layer or with minimal (<10%) ventricular irruption, IVH grade II designates occupation by blood of <50% of the ventricles without ventricular expansion, IVH grade III encloses occupation by blood of >50% of the ventricles, frequently associated with ventricular dilatation, and IVH grade IV refers to extensive intraventricular bleeding with parenchymal involvement (Figs. 1, 2, and 3a, b). Parenchymal injury is likely due to venous infarction with secondary hemorrhage (Fig. 3c). Another type of brain abnormality in IVH of prematurity consists of cystic periventricular leukomalacia , probably the result of hypoxic-ischemic insults (Fig. 3d). Common terms utilized for describing associated intracranial abnormalities are displayed in Table 2.
US studies illustrating Papile grading scale of IVH (a) coronal view of an IVH grade I showing subependymal hemorrhage, (b) axial slice of a case of a IVH grade III showing >50% intraventricular occupation by blood, (c) axial slice of a case of IVH grade II illustrating partial reabsorption of the intraventricular blood (<50%) and hydrocephalus, (d) axial view depicting a large (>50%) bilateral ventricular hemorrhage together with a frontal parenchymal lesion corresponding to IVH grade IV
Neuroimaging studies illustrating in four cases of IVH the value of MRI: (a) hemosiderin stain from a clot in the left choroid plexus; (b) dense blood clots, a blood fluid level on the right occipital horn, and ventricular enlargement; (c) images corresponding to a midline hemorrhage and bilateral hemorrhagic venous infarctions; (d) a case of severe cystic ventricular leukomalacia
Facts of “Born Too Soon” Babies
Preterm Birth Overview
Approximately 15 million infants are born prematurely every year worldwide, more than 1 in 10 babies. Almost one million children die each year due to complications of prematurity. In the majority of countries with reliable data, preterm birth rates have been reported to be rising (WHO 2012). Prematurity is the leading cause of death in children under age 5 years. In low-income countries, half of the babies born prematurely die due to lack of basic care, such as warmth, breastfeeding support, antibiotics for perinatal infection, and to breathing problems. Establishing viable and cost-effective measures could save many children (WHO 2012). In contrast, in high-income countries, the vast majority of premature infants survive. For reducing preterm birth, women need improved care before, between, and during pregnancies. Better access to contraceptives could also help in reducing preterm gestations. Most premature births occur spontaneously, without any identifiable cause. However, multiple pregnancies, infections, chronic diseases, such as diabetes, obesity, and high blood pressure, constitute common causes of preterm births. Genetic predisposition to preterm birth might also play a role.
Preterm births occur predominantly (>60%) in Africa and South Asia, but preterm birth remains a global problem. The incidence of premature birth ranges between 12% in low-income countries and 9% in higher-income countries, being poorer families at a higher risk. In the majority of countries, there has been an increase in preterm birth rates over the last 20 years (WHO 2015). Possible reasons for this include more dependable data, increases in maternal age and in underlying chronic conditions such as diabetes and arterial hypertension, wider use of assisted reproduction methods that favor multiple pregnancies, and also to changes in obstetric practices with more preterm cesarean births (WHO 2012).
Main comorbidities that may complicate IVH outcomes are listed in Table 3 (Christian et al. 2016a). Mortality related with premature births has been estimated to be higher than 90% of extremely preterm babies in underdeveloped regions in contrast with that of high-income countries that is lower than 10% (WHO 2012).
Germinal Matrix and Intraventricular Hemorrhage
About 12,000 premature infants in the United States develop germinal matrix hemorrhage/IVH (Robinson 2012). Approximately 50–75% of preterm survivors with IVH present neurological problems, as mental retardation, cerebral palsy, and/or hydrocephalus. Consequently, IVH and its sequelae constitute a relevant matter of public health worldwide.
After a period of increase, some authors report that the incidence of IVH seems to have plateaued (Robinson 2012). Advances in perinatal care and the development of neonatal intensive care units have decreased IVH-related morbidity and mortality. The high rate of preterm births may also be linked to the growing use of new methods of assisted human reproduction that increase the incidence of multiple pregnancies and of premature births.
Brain Atrophy, Ventriculomegaly, and Hydrocephalus
As stated by Warf et al. (2011), while postinfectious hydrocephalus is a disease of poverty, PHH is a disease of prosperity. The overall incidence of PHH requiring treatment in preterm infants with IVH has been reported to be 25–50% (Christian et al. 2016a). A recent study of 147,823 preterm neonates, that included data for the years 2000–2010, reports that 13,736 (9%) developed hydrocephalus during their initial admission (Christian et al. 2016a). Of these, 5,266 (38% of patients with IVH) underwent placement of a permanent CSF shunt . The remaining 8,470 infants either died or did not require shunting (Christian et al. 2016a). According to Papile ’s grading of IVH, the proportion of children requiring a shunt was 1% for grade I, 4% for grade II, 25% for grade III, and 28% for grade IV, respectively (Christian et al. 2016a). The prevalence of PHH seems also to be maintained reflecting the increased survival of low and very low preterm infants (Massimi et al. 2009).
How Intraventricular Hemorrhage Occurs?
Germinal matrix hemorrhage and IVH arise from bleeding in the periventricular germinal matrix. This brain region is also termed the ganglionic eminence and is mainly located on the head of the caudate nucleus. Typically the IVH occurs in the first 3 days of life. The germinal matrix consists of neuronal and glial precursor cells and of a rich vascular network. These precursor cells later mature and migrate to the cortex and white matter. The volume of the germinal matrix decreases after the 24th gestational week and it almost completely disappears by week 36–37. Three main factors account for bleeding in the germinal matrix and for IVH, namely (a) the fragility of the germinal matrix vessels, (b) the fluctuations of the cerebral blood flow, and (c) the coexistence of platelet and coagulation disorders (Ballabh 2014).
-
(a)
The fragility of germinal matrix vessels accounts for their vulnerability to hemorrhage. Delicate dilated endothelial channels mainly compose the germinal matrix vascular network. Vascular weakness is further increased by the scarcity of pericytes and by an immature basal lamina with a low content of fibronectin. In addition, there is a reduced content of glial fibrillary acidic protein (GFAP) in the astrocyte end-feet that wrap the blood vessels. Thus, the mechanical strength of the GFAP-containing filaments that form the cytoskeleton of the astrocytes is markedly debilitated, further contributing to the fragility of the germinal matrix vessels (Ballabh 2014). Risk factors for bleeding include inflammation, hypoxic-ischemic insults, and sepsis.
-
(b)
There is evidence that systemic arterial hypo- or hypertension can produce oscillations in the cerebral blood flow (CBF). Apparently, it is not the level of hypo- or hypertension what matters more but the fluctuations in the CBF (Ballabh 2014). Rises and falls in CBF velocity do occur during the first days of life, which actually correlate with the timing of IVH. Fluctuations in CBF may occur during suctioning and handling, infant fighting with the ventilator, respiratory distress syndrome, patent ductus arteriosus, closure of patent ductus arteriosus, and rapid infusion of sodium bicarbonate. High cerebral venous pressure may also contribute to disturbances in CBF, as occurs in prolonged labor, pneumothorax, or high ventilator pressure. Sepsis and dehydration can also cause abnormal blood pressure. Pressure passive circulation can also trigger CBF fluctuations as occurs in extreme prematurity and in severe low birth weight and in hemodynamic instability from respiratory compromise and sepsis. The role of impaired autoregulation in premature infants needs further evaluation.
-
(c)
Although more infrequently, platelet and coagulation disturbances with hemostatic failure may also contribute to the production of IVH, as happens with thrombocytopenia and disseminated intravascular coagulation.
Regarding spreading of the germinal matrix hemorrhage, in nearly 80% of cases there exists invasion of the lateral ventricles by blood (Miranda 2010). Blood can stream through the foramina of Monro to the third ventricle, the aqueduct, fourth ventricle, and basal cisterns (Figs. 1, 2, and 3). The hemorrhage may trigger an inflammatory response with arachnoiditis in the basal cisterns and in the arachnoidal granulations leading to communicating hydrocephalus. On the other hand, solid clots and aqueductal arachnoiditis can produce obstructive hydrocephalus (Miranda 2010). Most parenchymal lesions seen in the context of IVH are due to hemorrhagic venous infarction (Fig. 3c) while lesions denominated cystic periventricular leukomalacia (Fig. 3d) are thought to be the result of an anoxic-ischemic insult.
Clinical Scenarios
IVH occurs almost exclusively during the first 3 days of life, especially in the first day, while hemorrhagic venous infarction usually manifest after this period.
Debut of Intraventricular Hemorrhage
Robinson (2012) described three patterns of clinical presentation of IVH (Table 4).
-
(a)
A catastrophic pattern that develops over minutes to hours and closely resemble the evolution of adult intracranial hemorrhage.
-
(b)
The saltatory pattern that evolves from hours to days and manifest with decreased reactivity and alertness, hypo- or hypertonus, abnormal eye movements, bradycardia, apneic spells, or respiratory difficulties.
-
(c)
A clinically silent pattern, with few or no clinical signs of deterioration. An unexplained fall in the hematocrit may be the only indication of that an IVH has occurred (Robinson 2012). This pattern would justify the systematic use of US screening in this population performed in some centers. In a study of 240 preterm and term babies with intracranial hemorrhage studied by magnetic resonance imaging (MRI), 32 of 36 of them were asymptomatic (Sirgiovanni et al. 2014).
Interestingly, general neurologic deterioration without focalizing signs usually points toward the occurrence of IVH . On the contrary, the presence of lateralizing symptoms usually indicates the existence of an associated parenchymal lesion.
How Does PHH Manifest?
PHH may become evident by clinical symptoms and signs of raised intracranial pressure (ICP) as progressive macrocephaly, bulging fontanels, split sutures, sun-setting eyes, irritability, pupillary dilatation, ophthalmoplegia, vomiting, diminished activity, hypertonus, hyperreflexia, and seizures (Massimi and Di Rocco 2013; Robinson 2012; Wellons et al. 2013). Bradycardia, apnea, lethargy, and decreased activity are all signs of alarm that call for immediate attention (Table 4).
Diagnostic Workup
Antenatal Identification
The diagnosis of subependymal matrix hemorrhage and of IVH can be made prenatally and be confirmed by prenatal and postnatal MRI (Morioka et al. 2006). US detected ventriculomegaly, with or without associated lesions, of antenatal onset in 16 premature infants (Luciano et al. 2007). Criteria for the diagnosis of antenatal PHH in this series were ventricular dilatation, residual ventricular clots, unilateral porencephalic cysts, and/or periventricular venous infarction. The rapid evolution of the hydrocephalus in seven cases required CSF shunting (Luciano et al. 2007). Antenatal treatment of fetal hydrocephalus was reported in 85 instances that included 18 of 39 premature infants with IVH (Cavalheiro et al. 2003); 20 fetuses underwent cephalocentesis, 18 were given a ventriculo-amniotic shunt, and 1 was treated with an intrautero endoscopic third ventriculostomy (ETV).
Recognition After Birth
The existence of IVH in a preterm neonate must be suspected on clinical grounds. Confirmation of the diagnosis is habitually made by cranial US. Current indications at our hospital for the realization of US in preterm neonates include gestation of <32 weeks, birth weight <1,500 g, infants at special risks (seizures, sepsis, mechanical ventilation, coagulopathies, heart disease, etc.) and, in general in neonates admitted at the Neonatal Intensive Care Unit. These criteria are similar to the recommendations of the American Academy of Neurology and the Child Neurology Society (Ment et al. 2002).
-
(a)
Ultrasonography: preferred and safe tool for detection
Ultrasonography is the diagnostic method of choice in IVH. US studies are dependable, cheap, noninvasive, can be repeated as needed, can be performed at the crib-side, and require no sedation, and most importantly, US avoid the risks of radiation. US studies are performed either soon after birth if indicated or routinely between 7 and 14 days of life, and are repeated between 36 and 40 weeks of gestational age. This practice permits an accurate and timely diagnosis of IVH, an estimation of its extent, the detection of associated parenchymal lesions, and an estimate of ventriculomegaly (Fig. 1). In addition to the diagnostic value of IVH, serial US studies also provide information about the evolution (progression or regression) and prognosis of the hemorrhagic lesions and eventually of hydrocephalus (Davies et al. 2000; Ment et al. 2002).
US is performed through the anterior fontanel, in coronal, axial, and sagittal slices, and can be complemented with studies through the posterior or posterolateral fontanel, or even via the foramen magnum. Doppler studies can also be carried out for assessing intracranial hemodynamics and to make an estimation of the ICP. If the ICP is higher than the cerebral perfusion pressure a difficulty for CBF will result as indicated by an elevated resistance index (Bravo et al. 2011).
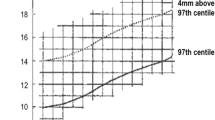
US are also utilized for differentiating PHH from cerebral atrophy. In hydrocephalus, the frontal horns are rounded, the temporal horns are easily identifiable, and there is ballooning of the third ventricle. US also detect signs of intraventricular bleeding, as are clots, fluid levels, and ependymal thickening. The progression of hydrocephalus needs serial measurements of the ventricular size. Several publications provide data on these calculations that can be used for reference (Davies et al. 2000). One of the most used measurements is the Levene ventricular index that calculates the distance from the falx to the external border of the lateral ventricle at the level of the foramina of Monro in coronal cuts.
-
(b)
Additional imaging studies
Noncontrast computerized tomography (CT) is recommended in term and late-preterm neonates (Fig. 2) with a history of birth trauma, coagulopathy, low hematocrit, and/or of hemorrhagic lesions (Ment et al. 2002). Regarding MRI (Figs. 3 and 4), there are insufficient data for recommending MRI studies in the standard preterm patient with IVH. An interesting case of syringomyelia prior to CSF shunting as initial presentation of PHH was diagnosed by MRI (Camacho et al. 2008). On the other hand, MRI can be performed when CT findings are inconclusive to assess the origin, extent, and localization of hemorrhagic lesions with uncommon features, for example, if there is the suspicion of a vascular malformation or a tumor (Counsell et al. 2003).
-
(c)
Miscellaneous diagnostic studies
Electroencephalography and evoked potential monitoring have also been used, especially to provide information on the evolution and in the assessment of the patients’ outcomes and sequels.
-
(d)
ICP monitoring
In certain cases, assessment of ICP before first shunt implantation is required and also in the evaluation of presumed shunt failure. Manometry can be performed at the time of performing a decompressive lumbar puncture although it has significant inaccuracies and is not devoid of risks. Continuous pressure recording can also be carried out via a subcutaneous reservoir, a method that is difficult to maintain for a significant time due to infants’ movements and to nursing necessities. In children given an external ventricular drain, the device can be used for recording the ventricular pressure. Transfontanelar ICP recording represents a safe noninvasive method that provides information in children with doubtful signs of progression of the ventriculomegaly. We used this technique for many years but it has the inconvenience of the difficulty for fixing the sensor to the fontanel and, in addition, transfontanelar ICP measurements are not regarded reliable, especially for research purposes. ICP sensors can also be placed in the subdural or epidural spaces. At present, the most used monitoring system is the intraparenchymal sensor that constitutes a minimally invasive procedure although its use may be complicated with brain damage, hemorrhage, or infection. However, continuous ICP recording is seldom utilized in this subset of patients.
(a) Sagittal MRI with FIESTA sequences in a case of communicating PHH, (b) coronal MRI view showing marked lateral ventricle asymmetry and absence of midline shifts, (c) MRI of a left frontal hemorrhagic venous infarction showing marked mass effect and midline displacement that required surgical treatment
Some Conditions Look Like IVH
In late preterm and term neonates, differential diagnosis is established against other types of hemorrhagic stroke associated to a variety of conditions (Bruno et al. 2014). In a study of 42 neonates with hemorrhagic stroke, a mixed intraparenchymal-IVH pattern was seen in 27 children, periventricular bleeding in 18, isolated IVH in 4, parenchymal bleeding in 11, subdural hematoma in 30, and subarachnoid hemorrhage in 25 (Bruno et al. 2014). In most of these patients, the stroke manifested during the first week of life and the main presentation was with seizures that were present in 64% of cases. Regarding the mechanism of the hemorrhagic stroke, there were 12 instances of hemorrhagic venous infarction (including five with cerebral venous sinus thrombosis and seven with medullary vein thrombosis), hemorrhagic arterial stroke in 10, germinal matrix bleeding in eight, hemorrhagic arterial watershed injury in two, and choroid plexus hemorrhage in eight. MRI-angiography was performed in 35 cases (Bruno et al. 2014). Hydrocephalus was present in 19 (45%) cases in the acute CT scan, although only 4 required a definitive CSF shunt .
Using the Data for Action: Management Options
Given the potential for complications of CSF shunting, there exists a reasonable reluctance to operate on small, especially preterm, children. On the other hand, delaying surgical treatment in the presence of progressive hydrocephalus might carry the risk of producing a progressive or even irreversible brain damage. To prevent the development of hydrocephalus and to avoid or to delay CSF shunt placement, several pharmacological and other nonsurgical therapies have been assayed both in experimental and clinical settings (Del Bigio and Di Curzio 2016). The goals of nonsurgical treatments are basically intended to: (a) reducing CSF production, (b) decreasing inflammatory and fibrotic responses due to the hemorrhage, and (c) protecting brain cells and axons of the damage caused by the hydrocephalus.
Medical Handling
-
(a)
Drug therapy with diuretics is aimed at reducing CSF production or at dehydrating the brain by diuresis. Several pharmacological agents have been utilized in clinical practice: theobromin (now of only historical interest), isosorbide that has been used for temporary control of ICP prior to shunting but not for replacement of surgery, glycerol that showed no effect in premature infants with PHH, and mannitol that is widely utilized for treatment of brain swelling but that is rarely used in PHH.
-
(b)
Some pharmacological therapies that act by interfering CSF formation have been tested with variable results. Acetazolamide, a carbonic-anhydrase inhibitor, directly reduces CSF production but has shown little therapeutic effect in hydrocephalic children. Furosemide/acetazolamide combination has demonstrated its utility in some infants with posthemorrhagic ventricular dilatation by the furosemide action on diuresis, but a randomized trial failed to show any benefit in these patients (Kennedy 1998).
-
(c)
Ion channel blockers, as digoxin or triamterene, provide a transient reduction in the ICP or in the CSF pressure although, at present, they are not used in clinical practice.
-
(d)
Glucocorticoids, as dexamethasone or methylprednisolone, reduce the production of CSF by binding to the choroid plexus epithelium. These agents are amply used by their well-known effects for decreasing the ICP in a variety of neurological conditions.
-
(e)
Pharmacological choroid plexus destruction with Gold-198, Rhenium-188, and Technetium-99 were tested in experimental animals. Intraventricular radioactive chromic phosphate-phosporus-32 was also used in four hydrocephalic children with relative success, but this therapy has not gained diffusion due to its high potential for side effects.
-
(f)
Thrombolytic agents in IVH. Intraventricular hemorrhage and bacterial meningitis in children are associated with secondary inflammation and meningeal fibrosis, especially in the subarachnoid space, producing CSF pathways blockage that impairs CSF absorption. Several approaches have been tested for the enzymatic lysis of blood, and therapies addressed at decreasing inflammation and at impairing the production of extracellular matrix molecules have also been utilized (Del Bigio and Di Curzio 2016). Common therapies include intraventricular streptokinase (Whitelaw et al. 1992), intraventricular urokinase, and intraventricular recombinant tissue plasminogen activator (rTPA) (Whitelaw et al. 1996).
-
(g)
“Brain wash.” Drainage, irrigation, and fibrinolytic therapy with rTPA (DRIFT) was tested in a multicenter randomized trial and showed a decrease in short-term deaths and in CSF shunting . The published studies on antifibrinolytic substances conclude that although there is insufficient evidence on the safety and efficacy of these therapies, there is also insufficient evidence for ruling out these treatments as unsafe or ineffective (Mazzola et al. 2014).
-
(h)
Brain protection. Progressive ventricular dilatation is known to interfere with cell genesis and myelination. This justifies the research on therapies that might protect the brain temporarily before shunting. These interventions include: anti-inflammatory agents (minocycline, ibuprofen or pioglitazone), antioxidants, neuronal and axonal protectors, cerebral stimulants, etc.
-
(i)
Cell transplantation and some of the abovementioned studies are anecdotal or are in the experimental phase, but many of these approaches seem open for further research (Del Bigio and Di Curzio 2016).
Briefly, nonsurgical temporizing measures are not recommended to reduce the need of CSF shunting (level I strength of recommendation that indicates a high clinical certainty) (Mazzola et al. 2014).
Wait-and-See Policy with Invasive Measures
A number of circumstances advise to adopt some form of transitory treatment of PHH. Basically, these measures are justified by diverse reasons: (a) absence of agreed protocols for shunting, (b) asymptomatic infants with progressive or severe ventriculomegaly or asymptomatic cases with mild or stable ventricular enlargement, (c) infants in poor clinical condition and/or with very low weight that disqualify them for shunt placement, (d) contraindications to definitive treatment (systemic infection, large amount of ventricular clots), (e) cases in which the ventriculomegaly is expected to be transitory (Massimi and Di Rocco 2013).
-
(a)
Lumbar puncture (LP)
Serial LPs are often utilized as the initial method for evacuation of CSF (Fig. 5). In addition to technical difficulties, as is the scanty amount of CSF retrieval in each tap, there always exists the possibility of infection. In addition, serial LPs do not avoid the final need for CSF shunting. The routine use of LP is not recommended in PHH with high clinical certainty and a level I strength of recommendation (Mazzola et al. 2014).
-
(b)
Ventricular taps
Serial ventricular taps are usually performed through the anterior fontanel. They can also produce temporary decompression by CSF removal (Fig. 6). Repeated ventricular taps are to be avoided due to risks of brain damage, bleeding, and infection. Its use should be restricted to achieving diagnosis or as a life-saving procedure.
-
(c)
Ventricular access reservoirs
Ventricular access devices consist of a ventricular catheter joined to a subcutaneously placed reservoir. These reservoirs allow performing serial taps for CSF removal. Their infection rate is low and they are recommended as a temporizing method for the relief of hydrocephalus (Fountain et al. 2016; Tröbs and Sander 2015; Wellons et al. 2009).
-
(d)
Ventriculo subgaleal shunts
A subgaleal shunt is a temporary procedure used in infants who are too small or premature to tolerate other shunt types. The shunt consists of creating a pocket in the subgaleal space that allows the drainage of CSF from the ventricles to the subcutaneous cavity via a low-pressure valve thus forming a fluid-filled pouch beneath the infant’s scalp where the fluid is absorbed. The large surface of the pericranial pocket permits collecting large amounts of fluid within the subgaleal space. The CSF collection can be punctured for fluid evacuation when it becomes tense. Main complications consist of obstruction, infection, fluid leaks, skin breakdown, intracranial bleeding from CSF hypotension, and skull deformation from pressure by the fluid collection. Ventriculosubgaleal shunts may be converted to VP shunt once the infant grows up (Fountain et al. 2016; Tubbs et al. 2005; Wellons et al. 2009).
-
(e)
External ventricular drainage
An external ventricular drain (EVD) consists of a ventricular catheter attached to a silastic tube that conducts the CSF from the ventricle to an externally placed collecting bag that permits the drainage of CSF to control ICP. It can be inserted either at the operating room or at the bedside. EVD is usually regarded as a safe and effective method but its use can be complicated with infection, blockage, or migration out of the ventricle.
-
(f)
Neuroendoscopic ventricular lavage
Schulz et al. (2014) have developed a variant for intraventricular clots lavage by using neuroendoscopic techniques.
In summary, ventricular access reservoirs, ventriculosubgaleal shunts, and external ventricular drains constitute treatment options for PHH with a moderate degree of clinical certainty (Mazzola et al. 2014).
Definitive Surgical Solutions
Two main surgical procedures are presently utilized in the treatment of established hydrocephalus, namely (a) ETV and (b) CSF shunting . Ventriculoperitoneal (VP) shunt still constitutes the main surgical option for treating PHH. Normally, definitive surgery is indicated after unsuccessful temporary use of medical and/or surgical treatments, once the neurosurgeon confirms the progression of the ventricular enlargement. At present, there is an increased neurosurgeon tolerance for moderate ventriculomegaly after IVH, given the potential for complications of CSF shunting, especially in preterm children. This expectant attitude must be counterbalanced against the fact of that delaying surgery in the presence of active hydrocephalus might cause progressive or even permanent brain damage.
ETV: A Promising Innovative Surgical Tool
Presently, ETV is increasingly performed to treat cases of hydrocephalus of diverse etiologies. ETV consists of performing a perforation in the floor of the third ventricle to divert the CSF toward the prepontine cisterns by endoscopic methods. The miniaturization of modern endoscopic tools permits the use of ETV even in small or premature infants (Fig. 7a). Findings of ETV include ependymal hemosiderin staining (Fig. 7b), intraventricular clots, scarring of the third ventricle floor (Fig. 7c), and/or aqueductal obstruction (Warf et al. 2011). Complications from ETV utilization of varying severity comprise brain damage, hemorrhage, CSF leaks, and infection. The chief drawback of ETV is by far its high percentage of failures in children younger than 1 year and a success rate of only ~30% in this age group. On the contrary, ETV seems to be more successful in the management of late CSF shunt failure.
(a) Endoscopic third ventriculostomy in a 1-month-old baby with PHH showing miniaturized tools, (b) endoscopic view of the ventricular walls illustrating hemosiderin deposits and some small floating blood clots, (c) endoscopic image showing cloudiness and scarring of the third ventricle floor in a case of failed ETV
A novel approach for PHH management consists of performing a combined ETV plus choroid plexus coagulation as primary treatment, which improved the success rate to 40% of cases (Warf et al. 2011; Zhu and Di Rocco 2013). In addition, the surgeon may add, in certain instances, opening of the lamina terminalis, septostomy, rupture of ventricular septations and of the membrane of Liliequist in the same procedure. In a recent series of 91 children submitted to this treatment, only 7 of 25 with PHH required further surgery (Stone and Warf 2014). Age 6 months or older, lack of prior CSF diversion, and presence of clean cisterns were good predictors of success. In this series, there was no mortality and no infections, and there were only two complications of lesser severity. The presence of clean prepontine cisterns can be ascertained by preoperative MRI FIESTA images (Warf et al. 2011; Stone and Warf 2014). In spite of the relative low rate of success of this procedure, the authors believe that the combined ETV-choroid plexus cauterization as a primary treatment in PHH is worthwhile as it avoids shunt complications and shunt dependence, improves the patients’ quality of life, and reduces the health care cost burden (Stone and Warf 2014). However, ETV lacks of sufficient evidence to recommend its use as a primary treatment in PHH (level III, unclear clinical certainty) (Mazzola et al. 2014).
CSF Valves: First-Line Treatment
In spite of all therapeutic efforts (medical or surgical) to avoid CSF shunt insertion, approximately 8–10% of children with IVH, especially those with IVH grade III and IV, develop progressive PHH and require placement of a CSF shunting device (Christian et al. 2016a). Despite recent advances in techniques and in valve fabrication, VP shunts are not well tolerated by small infants. Premature babies are hemodynamically instable, fragile to anesthetics, and prone to infection due to their intrinsic immature immunity (Massimi and Di Rocco 2013).
Although stringent recommendations for CSF shunting are lacking, several issues regarding placement of CSF shunts deserve attention (Table 5):
-
(a)
Timing for CSF shunt insertion. It depends on the babies’ weight, the children’s general status (presence of multisystem comorbidities and additional prematurity-related complications), skin condition, and on the characteristics of the CSF (presence of clots, high protein content, etc.). Most authors recommend a minimal weight of 1500 g and some recommend waiting until the baby weighs 2500 g (Robinson 2012). At our hospital we preferably insert a VP shunt when the infants’ reach at least a weight of 1300 g, although some babies were operated with a weight as low as 900 g (Martínez-Lage et al. 2008).
-
(b)
The type of valve. There are several types of CSF derivations, ranging from a valveless tube to differential pressure valves, flow-regulated systems, and valves with a siphoning-retarding device. Recently, manufacturers have also launched several models of programmable and gravity valves. An important issue regarding shunts is to choose the smallest, low-profile, system to prevent skin erosion.
-
(c)
Cavity for drainage of the CSF. At present shunts are almost exclusively implanted in the peritoneal cavity either by minilaparotomy or by laparoscopy. Alternatively, the valve can be placed in the right atrium in cases of problematic peritoneal conditions.
-
(d)
Prophylactic antibiotics. The mean shunt infection rate in this group of patients is 7%. Due to the children’s immature immunity system, most authors favor antibiotic prophylaxis for at least 24 h (Mazzola et al. 2014; Robinson 2012).
-
(e)
Technical details. Of utmost importance is paying attention to technical details, including meticulous preparation of the skin and surgical field, avoidance of intermediate skin incisions, avoidance of connections, cautious tunnelling, etc.
Although it is advisable to avoid or to delay shunt placement, some authors do not exclude inserting a CSF shunt as the primary surgical treatment for PHH, irrespective of the condition of the ventricular fluid, and report an acceptable rate of complications (Romero et al. 2014).
Hazards from CSF Derivations
The objectives of CSF shunting are: (a) to control the raised ICP, (b) to avoid mechanical and functional complications (c) to prevent infection, and (d) to delay as much as possible shunt replacement or revision. Probably, PHH and postinfectious hydrocephalus present the highest number of complications. In Reinprecht et al. (2001) series, 42 of 76 children with IVH and ventricular enlargement required permanent shunting and suffered a mean number of shunt revisions per patient of 1.57. The most frequent complications included infection (7.1%) and shunt obstruction (45.2%). They also had three instances of compartmentalization and two of overdrainage. In a series of 512 instances of hydrocephalus of all etiologies, 88 (17.8%) developed some type of CSF overdrainage syndrome (Martínez-Lage et al. 2005). This series included 103 children with PHH and of these 23 (22.33%) had clinical manifestations of overshunting. In another survey of 91 infants with PHH, 8% of patients had a valve infection, and 11 children developed loculated ventricles at a mean period of 2.5 years (Christian et al. 2016b). These authors reported a valve revision rate of 43% after a follow-up of 7 years. An ample review of shunt complications in postinfectious and PHH has been recently published (Wang and Ahn 2015).
Some children suffering a late shunt complication may become shunt free and this possibility should be explored in all cases. The probable explanation for this occurrence is that with time the subarachnoid adhesions clear up and the capability of spontaneous reabsorption of CSF restores. In a survey of 850 patients shunted for hydrocephalus, shunt independence could be demonstrated in 27 (3.2%) cases. In this subset of patients 11 of 27 (41%) had been operated of PHH (Iannelli et al. 2005). The authors remarked the prognostic value of the presence of normal or slightly enlarged ventricles for the success of CSF shunt removal and that no case showed slit ventricles.
In contrast with the low success rate of ETV as initial PHH treatment in infants younger than 1 year of age, this procedure produces better results in older children. Accordingly, the possibility of performing an ETV should be explored in older children undergoing a surgical shunt revision or lengthening of their shunt.
Outcome for IVH and PHH
Several mechanisms can account for the poor outcome in many children with PHH: (a) brain damage caused by the ventricular enlargement, (b) primary brain injury from the hemorrhage and the hypoxic-ischemic lesions, (c) comorbidities associated to prematurity, and (d) shunt-related complications (Murphy et al. 2002). Main comorbidities that may complicate IVH outcomes are summarized in Table 3 (Christian et al. 2016a). In this regard, information given to the parents should clearly state that placing a CSF valve can influence only the brain damage produced by the hydrocephalus but that, by no means, it does improve the lesions resulting from the hemorrhage or from the hypoxic-ischemic lesion.
Mortality related with prematurity was estimated to be higher than 90% of extremely preterm babies in underdeveloped regions in contrast with that of high-income countries that is lower than 10% (WHO 2015). IVH severity was the main determinant of cognitive and motor function and of epilepsy (Robinson 2012). At the long term, the main determinants of survival were IVH grade and multiple shunt revisions (Robinson 2012). The presence of hemorrhagic cerebral infarctions and of cystic periventricular lesions also influenced negatively the cognitive and motor functions. In regard to the role played by the PHH itself, functional outcomes were similar in patients who required surgery to those that did not.
Vinchon et al. (2012) reported the adult outcomes of 456 patients with hydrocephalus of all etiologies that were operated in pediatric age. The study included 57 (12.5%) subjects diagnosed with PHH. The actuarial mortality was 287 patients (18.1%) at 20 years. The shunt-related mortality rate was 4.2% before the age of 20 and 7.2% at age 30 years. The most common sequels in this series were cognitive in 217 (47.6%), motor in 212 (46.6%), behavioral in 69 (15.1%), and visual in 62 (13.6%) cases. For these authors, the worst outcome corresponded to hydrocephalus diagnosed at birth (PHH, malformative, postinfectious, and myelomeningocele) (Vinchon et al. 2012). Regarding specifically to the 57 individuals with PHH, their Karnofsky grade was 77.9, 14 (24.6%) had no sequels, 26 (45.6%) had motor sequels, 33 (57.9%) had cognitive problems, and 16 (28.1%) had epilepsy. Eighteen (31.65%) attended normal school and 10 (27% of evaluable cases) worked in a normal job (Vinchon et al. 2012). Early rehabilitation and social integration of the affected individuals seems to be of utmost importance to palliate the sequels that these individuals often present.
Actions to Improve the Outcome
Several guidelines and recommendations for improving survival and outcomes for problems derived from prematurity have been developed (WHO 2012). These guidelines include interventions made available to mothers, as are steroid injections before birth, and antibiotics for premature rupture of the amniotic membranes. They also contain interventions for the newborn baby including thermal care, safer oxygen use, and other measures addressed to dealing with babies’ breathing problems.
Available perinatal and neonatal measures have greatly improved mortality and morbidity in infants with IVH and hydrocephalus (Tortorolo et al. 1999). However, there still remains a relatively high rate of cognitive, sensorial, and motor sequels. Caffeine and erythropoietin are being assayed with promising perspectives. Another potential area of research consists of using human stem cells including the infant’s own umbilical cord stem cells to enhance neurorepair (Del Bigio and Di Curzio 2016; Robinson 2012; Williams et al. 2007).
Regarding hydrocephalus, a workshop outlined the priorities for hydrocephalus research (Williams et al. 2007). There is no proven medical or pharmacological alternative for hydrocephalus control and ETV can be used only in a minority of patients. Presently, CSF shunting remains the most effective and feasible way of hydrocephalus treatment. In the mentioned workshop, the need for developing new technologies for hydrocephalus treatment was stressed, including further research on biomaterials to prevent shunt infection and occlusion (Williams et al. 2007). Many aspects of hydrocephalus treatment also require the close collaboration between basic and clinical studies as well as the development of standardized methods to measure the health status of the patients (Kulkarni et al. 2004).
Conclusions
In spite of advances in obstetric and neonatal care, IVH and related PHH constitute an important problem in pediatric neurosurgery. Preventive measures addressed at reducing death and disability in preterm babies and at improving maternal and neonatal care need to be implemented both in underdeveloped and in high-income regions. The main diagnostic tool in IVH and PHH is ultrasonography. Several measures, medical or surgical (reservoir use, taps, EVD, and subgaleal shunts), can be utilized for delaying CSF shunt placement until the child arrives at a better condition. ETV, alone or combined with choroid plexus cauterization, is being tested for the management of PHH. However, VP shunting still remains the most practical treatment for this entity. There is a need for refining preventive measures and for improving materials and devices utilized in the construction of CSF shunts.
References
Ballabh P (2014) Pathogenesis and prevention of intraventricular hemorrhage. Clin Perinatol 41:47–67
Bravo C, Cano P, Conde R et al (2011) Posthemorrhagic hydrocephalus in the preterm infant: current evidence in diagnosis and treatment. Neurocirugia (Astur) 23:381–400 (Span)
Bruno CJ, Beslow LA, Witmer CM et al (2014) Hemorrhage stroke in term and late preterm neonates. Arch Dis Child Fetal Neonatal Ed 99:F48–F53
Camacho A, Simón R, Muñoz A et al (2008) Syringomyelia secondary to posthemorrhagic hydrocephalus in a preterm infant. Pediatr Neurol 38:211–214
Cavalheiro S, Fernandez Moron A, Zymberg ST, Dastoli P (2003) Fetal hydrocephalus- prenatal treatment. Childs Nerv Syst 19:561–573
Christian EA, Jin DL, Attenello F et al (2016a) Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. J Neurosurg Pediatr 17:260–269
Christian EA, Melamed EF, Peck E et al (2016b) Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J Neurosurg Pediatr 17:276–284
Counsell SJ, Rutherford MA, Cowan FM, Edwards AD (2003) Magnetic resonance imaging of preterm brain injury. Arch Dis Child Fetal Neonatal Ed 88:F269–F274
Davies MW, Swaminathan M, Chuang SL, Betheras FR (2000) Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch Dis Child Fetal Neonatal Ed 82:F218–F223
Del Bigio MR, Di Curzio DL (2016) Nonsurgical therapy for hydrocephalus: a comprehensive and critical review. Fluids Barriers CNS 13:3
Engle WA (2004) Policy statement: age terminology during the perinatal period. Pediatrics 114:1362–1364
Fountain DM, Chari A, Allen D, James G (2016) Comparison of the use of ventricular access devices and ventriculosubgaleal shunts in posthaemorrhagic hydrocephalus: systematic review and meta-analysis. Childs Nerv Syst 32:259–267
Iannelli A, Rea G, Di Rocco C (2005) CSF shunt removal in children with hydrocephalus. Acta Neurochir 47:503–507
Kennedy CR, International PHVD Drug Trial Group (1998) International randomised controlled trial of acetazolamide and furosemide in posthaemorrhagic ventricular dilatation in infancy. Lancet 352:433–440
Kulkarni A, Robin D, Drake JM (2004) An instrument to measure the health status in children with hydrocephalus: the Hydrocephalus Outcome Questionnaire. J Neurosurg Pediatr 101(2 Suppl):134–140
Luciano R, Baranello G, Masini L et al (2007) Antenatal post-hemorrhagic ventriculomegaly: a prospective follow-up study. Neuropediatrics 38:137–142
Martínez-Lage F, Pérez-Espejo MA, Almagro MJ et al (2005) Syndromes of overdrainage of ventricular shunting in childhood hydrocephalus. Neurocirugía/Astur 16:124–133 (Span)
Martínez-Lage JF, Almagro MJ, del Rincón IS et al (2008) Management of neonatal hydrocephalus: feasibility of use and safety of two programmable (Sophy and Polaris) valves. Childs Nerv Syst 24:549–556
Massimi L, Di Rocco C (2013) Surgical treatment of posthemorrhagic infantile hydrocephalus. Minerva Pediatr 65:417–425
Massimi L, Paternoster G, Fasano T, Di Rocco C (2009) On the changing epidemiology of hydrocephalus. Childs Nerv Syst 25:795–800
Mazzola CA, Choudhri AF, Auguste KI et al (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr (Suppl) 14:8–23
Ment LR, Bada HS, Barnes P et al (2002) Practice parameter: neuroimaging in the neonate. Report of the quality standards subcommittee of the American Academy of Neurology and the practice committee of the Child Neurology Society. Neurology 58:1726–1738
Miranda P (2010) Intraventricular hemorrhage and posthemorrhagic hydrocephalus in the preterm infant. Minerva Pediatr 62:79–89
Morioka T, Hashiguchi K, Nagata S et al (2006) Fetal germinal matrix and intraventricular hemorrhage. Pediatr Neurosurg 42:354–361
Murphy BP, Inder TE, Rooks V et al (2002) Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed 87:F37–F41
Reinprecht A, Dietrich W, Berger A et al (2001) Posthemorrhagic hydrocephalus in preterm infants: long–term follow-up and shunt-related complications. Childs Nerv Syst 17:663–669
Robinson S (2012) Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr 9:242–258
Romero L, Ros B, Rius F et al (2014) Ventriculoperitoneal shunt as a primary neurosurgical procedure in newborn posthemorrhagic hydrocephalus: report of a series of 47 shunted patients. Childs Nerv Syst 30:91–97
Schulz M, Bührer C, Pohl-Schickinger A et al (2014) Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates. J Neurosurg Pediatr 13:626–635
Sirgiovanni I, Avignone S, Groppo M et al (2014) Intracranial haemorrhage: an incidental finding at magnetic resonance imaging in a cohort of late preterm and term infants. Pediatr Radiol 44:289–296
Stone SSD, Warf BC (2014) Combined endoscopic third ventriculostomyand choroid plexus cauterization as primary treatment for infant hydrocephalus. A prospective North American series. J Neurosurg Pediatr 14:439–446
Tortorolo G, Luciano R, Papacci P, Tonelli T (1999) Intraventricular hemorrhage: past, present and future, focusing on classification, pathogenesis and prevention. Childs Nerv Syst 15:652–661
Tröbs RB, Sander V (2015) Posthemorrhagic hydrocephalus in extremely low birth weight infants: Ommaya reservoir vs. ventriculoperitoneal shunt. Childs Nerv Syst 31:1261–1266
Tsitouras V, Sgouros S (2011) Infantile posthemorrhagic hydrocephalus. Childs Nerv Syst 27:1595–1608
Tubbs RS, Banks JT, Soleau S et al (2005) Complications of ventriculosubgaleal shunts in infants and children. Childs Nerv Syst 21:48–51
Vasileiadis GT, Gelman N, Han VKM et al (2004) Uncomplicated intraventricular hemorrhage is followed by reduced cortical volume at near-term age. Pediatrics 114:e367–e372
Vinchon M, Baroncini M, Delestret I (2012) Adult outcome of pediatric hydrocephalus. Childs Nerv Syst 28:847–854
Wang JY, Ahn ES (2015) Posthemorrhagic and postinfectious complications. In: Di Rocco C, Turgut M, Jallo G, Martínez-Lage JF (eds) Complications of CSF shunting in hydrocephalus. Springer, Heidelberg/Dordrecht/London/New York, pp 149–158
Warf BC, Campbell JW, Riddle E (2011) Initial experience with combined endoscopic third ventriculostomy and choroid plexus cauterization for posthemorrhagic hydrocephalus of prematurity: the importance of prepontine cistern status and the predictive value of FIESTA MRI imaging. Childs Nerv Syst 27:1063–1071
Wellons JC III, Shannon CN, Kulkarni AV et al (2009) A multicenter retrospective comparison of conversion from temporary to permanent cerebrospinal fluid diversion in very low birth weight infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr 4:50–55
Wellons JC III, Holubkov R, Browd SR et al (2013) The assessment of bulging fontanel and splitting of sutures in premature infants: an interrater reliability study by the Hydrocephalus Clinical Research Network. J Neurosurg Pediatr 11:12–14
Whitelaw A, Rivers RPA, Creighton L, Gaffney P (1992) Low dose intraventricular fibrinolytic treatment to prevent posthaemorrhagic hydrocephalus. Arch Dis Child 67:12–14
Whitelaw A, Saliba E, Fellman V et al (1996) Phase I study of recombinant tissue plasminogen activator for treatment of posthaemorrhagic hydrocephalus. Arch Dis Child 75:F20–F26
WHO (2012) Born too soon: the global action report on preterm birth. http://www.who.int/pmnch/media/news/2012/201204_borntoosoon-report.pdf. Accessed 10 May 2016
WHO (2015) WHO recommentations on interventions to improve preterm birth outcomes http://apps.who.int/iris/bitstream/10665/183037/1/9789241508988_eng.pdf?ua=1. Accessed 27 June 2017
Williams MA, McAllister JP, Walker ML (2007) Priorities for hydrocephalus research: report from National Institutes of Health-sponsored workshop. J Neurosurg Pediatr 107(5 Suppl):345–357
Zhu X, Di Rocco C (2013) Choroid plexus coagulation for hydrocephalus not due to CSF overproduction: a review. Childs Nerv Syst 29:35–42
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry
Martínez-Lage, J.F., López-Guerrero, A.L., Almagro, MJ. (2020). Posthemorrhagic Hydrocephalus. In: Di Rocco, C., Pang, D., Rutka, J. (eds) Textbook of Pediatric Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-319-72168-2_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-72168-2_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72167-5
Online ISBN: 978-3-319-72168-2
eBook Packages: MedicineReference Module Medicine