Abstract
Obsessive-compulsive disorder (OCD) is a common and debilitating psychiatric condition. Relatively little, however, is understood about the etiology and brain basis of OCD despite decades of research. Although neuroimaging findings in OCD frequently report abnormalities of the orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus, new insights into the disorder are urgently needed. In this chapter, we review the current state of this evidence, including neuroimaging studies, genetics, neurochemical investigations, and insights from animal models.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Dopamine
- Glutamate
- Hypothalamic-pituitary-adrenal (HPA) axis
- Obsessive-compulsive disorder (OCD)
- Animal models
- Genome wide association studies
- History
- HPA axis
- Immune system
- Neuroanatomical circuits
- Neurocognition
- Neurotransmitter systems
- Pediatric autoimmune neuropsychiatric disorders associated with Streptococcus (PANDAS)
- Serotonin
Brief History
Obsessive-compulsive disorder (OCD) appears to be an ancient illness with descriptions of people’s behavior in the Bible and ancient Greek texts resembling the symptoms of modern day OCD. Starting in the seventeenth century, the medical literature began describing clinical cases of obsessional doubts and of scrupulosity which mirror today’s cases of OCD. In the nineteenth century, modern concepts of OCD began to emerge with the differentiation of obsessions, in which insight was preserved, from delusions, in which it was not. In addition, obsessions and compulsions were included with conditions we now identify as phobias and panic disorder, as OCD was often accompanied by anxiety. Various terms for modern day OCD emerged during the late nineteenth century: “grubelsucht,” a ruminatory or questioning illness (from the Old German for racking one’s brains), and “zwangsvorstellung” (compelled presentation or idea) were two early terms for the illness. “Zwangsvorstellung” was translated in the United Kingdom as “obsession,” and in the USA as “compulsion.” In the twentieth century, Sigmund Freud conceptualized OCD as a maladaptive response to conflicts between unacceptable, unconscious sexual or aggressive impulses and the demands of conscience and reality. Compulsions were used as defense to neutralize the offending ideas and impulses.
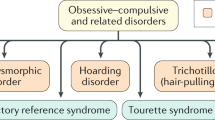
By the end of the twentieth century, however, theories of OCD gave way to advances in neuroimaging, neurocognition, animal models, and immunology, resulting in a deeper neurobiological understanding of the illness. Although the etiology of OCD is still unknown, we have a wealth of information regarding the neuroscience of the illness. Our present day clinical definition of OCD is characterized by obsessions and compulsions (or both) that are distressing, time-consuming, or impairing. In addition to OCD, a number of other psychiatric disorders also have obsessions or compulsions as prominent features, and these include autism spectrum disorders, Tourette’s syndrome, hypochondriasis, eating disorders, trichotillomania (hair pulling) and skin picking disorder, and schizophrenia.
OCD is a disorder characterized by a symptom constellation suggestive of dysregulation of fronto-striatal brain circuitry that results in a failure to update behavioral responses on the basis of new environmental information. In addition to disrupted functioning of the central nervous system, other organ systems of the body such as the immune system may also be dysregulated in patients with OCD and implicated in its manifestation – at least in some cases. In this chapter, we will provide a brief and selected overview of biological research into the etiology of OCD.
OCD Is a Common and Disabling Psychiatric Disorder
OCD is the fourth most common psychiatric illness with a lifetime prevalence of 1–3 %. Among adults with OCD, the sex ratio is approximately equal for men and women. Although onset of illness is possible across the lifespan, the age at the onset of OCD generally appears to be bimodal with onset either during childhood (approximately 10 years of age) or during adolescence/young adulthood (approximately 21 years of age). If untreated, OCD is a chronic illness, resulting in a poor overall quality of life and high social costs due to the high rates of unemployment and disability associated with OCD. The World Health Organization has identified OCD as a leading global cause of nonfatal illness.
Causes and Pathogenesis of OCD
Neurocognition
The thoughts and behaviors that characterize OCD (e.g., doubting, repetitive checking) are repetitive and intrusive and undertaken in a rigid fashion. Neuropsychological studies involving patients with OCD have shown deficits in cognitive abilities that are linked to the functioning of the frontal lobe and its related fronto-subcortical structures, such as executive functioning, response inhibition, cognitive flexibility (i.e., the ability to adapt behavior on the basis of new information), working memory, and implicit learning. In addition, unaffected first-degree relatives of OCD patients also exhibit deficits on tasks of response inhibition and flexible responding, compared with unrelated healthy controls, suggesting that these measures may be endophenotypes (or intermediate phenotypes) for OCD. These studies, however, do not enable a clear characterization of the temporal association between the manifestation of cognitive deficits and clinically significant OCD symptoms. In addition, the cognitive findings raise issues regarding the classic orbitofronto-striatal theory of OCD as patients show deficits on a broad array of tasks, not just those dependent on this circuitry. This has led to a model emphasizing involvement of the orbitofrontal but also dorsolateral prefrontal sectors and the parietal cortex.
Neurobiology
Neurotransmitter Systems Implicated in OCD
A large body of research investigating the role of monoamine neurotransmitter systems in the pathogenesis of OCD has been ongoing since the 1980s. The monoamine hypothesis of OCD suggested that OCD was caused by a deficiency in concentration or receptor function of several catecholamine/indoleamine neurotransmitters, including serotonin and dopamine. These hypotheses about the specific roles of catecholamines/indoleamines in the pathophysiology of OCD arose in part from pharmacological interventions in humans
Serotonin
Serotonin is a neurotransmitter synthesized from the amino acid, tryptophan, within the neurons of the rostral and caudal raphe nuclei of the brainstem. One of the main hypotheses regarding the pathophysiology of OCD is that it results from some abnormality in the serotonin system. Several lines of evidence suggest a role for serotonin deficiencies in OCD. Serotonin reuptake inhibitors demonstrate better clinical efficacy than other pharmacological agents in treating OCD and represent a current first-line treatment option. Drugs which lack serotonergic mechanism (e.g., desipramine) are widely held to be ineffective in OCD. Studies examining the risk for OCD with polymorphisms in the serotonin transporter, however, have produced mixed results. Pharmacological and genetic evidence implicates the serotonin receptor type 2A, and possibly type 2C and type 1Dbeta receptors as well, in the pathophysiology of OCD. Increased serotonin in peripheral blood has also been reported in people with OCD, as compared to controls.
Dopamine
Dopamine is a catecholamine neurotransmitter synthesized from tyrosine and is the direct precursor to norepinephrine. Dopaminergic neurons are organized into three major systems: nigrostriatal system, which in part regulates movement; mesolimbic/mesocortical system, which regulates limbic and cortical activity; and the tuberoinfundibular system (prolactin regulation). The effects of dopamine are mediated by several subtypes of receptors, and its action is terminated through synaptic reuptake by the dopamine (or norepinephrine) transporter and/or degradation by the catechol-o-methyl transferase (COMT) enzyme.
Animal (see later) and human data suggest that dopaminergic dysregulation may also contribute to the pathophysiology of OCD. Several lines of evidence implicate dopamine in the mediation of certain types of repetitive behavior. Recent trials of combined SRI medication with typical and atypical antipsychotic treatments suggest that dopamine receptor antagonism may further reduce OC symptom severity at least in some forms of OCD. Dopamine receptors 2, 3, and 4 and the dopamine transporter gene have all been implicated in OCD based on human genetic studies, animal research, and neuroimaging research. None of the research, however, has been successfully replicated across research laboratories to date.
Glutamate
Glutamate is the primary excitatory neurotransmitter in the cortico-striato-thalamic circuit and as such has been examined in the neurobiology of OCD. Reports from neuroimaging and genetic studies suggest that glutamate plays some role in the pathophysiology of OCD. Neuroimaging studies have demonstrated increased glutamate levels in caudate and frontal cortex of humans with OCD. In addition, several glutamate-related genes have been associated with OCD risk. In particular, the glutamate transporter gene Slc1A1 has been implicated in association studies with OCD. A total of nine genetic studies support the association between a region of the genome on chromosome 9p that contains the Slc1A1 gene and OCD. In fact, none of the genes implicated in serotonin or dopamine transmission have attained significant value in genetic studies but glutamate genes have. Cerebrospinal fluid studies of unmedicated adults with OCD have found statistically significant higher glutamate in OCD patients, with no significant effect of age, gender, disease severity, or other covariates. The majority of magnetic resonance spectroscopy studies examining glutamate in various brain regions have suggested some abnormality in glutamate regulation within the CSTC circuit, but the results have not been unequivocal. In addition, a recent placebo-controlled study using the glutamate antagonist, Riluzole, failed to show efficacy in treating OCD.
Hypothalamic-Pituitary-Adrenal Axis
In addition to the findings of neurotransmitter disturbances in OCD, some data suggest disturbances in hypothalamic-pituitary-adrenal (HPA) axis function in individuals with OCD. Physical and psychological stress activates the HPA axis through the secretion of corticotropin releasing hormone (CRH) and arginine vasopressin (AVP) by the parvocellular neurons of the hypothalamus. These neuropeptides activate the synthesis and the release of adrenocorticotropin hormone (ACTH) from the anterior pituitary, which successively stimulates the adrenal cortex to synthesize cortisol in humans.
OCD onset is often preceded by stressful events, such as job loss, birth of a child, death of a family member, or from trauma. Additionally, OCD symptoms worsen under stressful situations and that patients with OCD suffer more from daily life stress compared to controls. Studies suggest that plasma cortisol and ACTH levels are elevated in patients with OCD and that cortisol levels are somewhat proportional to the severity of OCD symptoms. Cerebrospinal spinal fluid studies have also found that CRH and AVP levels are elevated in people with OCD.
The Immune System in OCD
In addition to the above systems, the immune system may play an important role in the etiology of OCD in some individuals. The influence of the immune system in OCD was actually first hinted at in the 1920s with the finding that some cases of Tourette’s syndrome were associated with sinus infections. The association between Group A Strep (GAS) infection and OCD was not presented however until the early 1990s and was then referred to as pediatric autoimmune neuropsychiatric disorders associated with Streptococcus (PANDAS) in which GAS was seen as the trigger for OCD (other infectious agents have also been considered as possible etiological agents). Over time-specific criteria for PANDAS was developed and included prepubertal onset, OCD symptoms occurring intermittently or following a sawtooth course, a temporal relationship of OCD symptoms to GAS infection, and the presence of other neurological findings such as choreiform movements. PANDAS is usually diagnosed in children who can be carriers of the infection but do not show symptoms. It happens in about 1 in 1,000 children, and three times as often in boys than girls. PANDAS is defined as a prepubertal condition, since most children, by the time they enter adolescence, have developed immunity to strep, so onset after childhood is unlikely. Although several lines of evidence appear to link GAS infection and OCD onset in some individuals, proof of infectious etiology has been difficult. Plasmapheresis (the exchange of blood plasma) or IVIG (intravenous immunoglobin), which gives children antibodies from donors, however, have both been successful in treating OCD associated with PANDAS in some cases.
Multiple theories underlying PANDAS include molecular mimicry whereby antibodies intended GAS target brain proteins instead because of the similarities to human cells. In the case of OCD, the antibodies likely attack the basal ganglia, and antibodies to basal ganglia are found in the sera of most OCD PANDAS subjects. Other possible mechanisms by which autoantibodies cause OCD include direct stimulation or blockade of receptors in the basal ganglia or immune complexes promoting inflammation of these brain regions. Antineuronal antibody binding in the basal ganglia tissue has been found in OCD patients, and the increased antineuronal antibody binding correlates with OCD symptom severity. In addition, the anticarbohydrate A antibody measures the immune response to N-acetyl-beta-d-glucosamine (the dominant epitope of GAS carbohydrate), and this antibody has been shown to fluctuate with OCD symptom changes. Finally, antibodies against dopamine D1 and D2 receptors have also been detected in PANDAS.
Neuroanatomical Circuits in OCD
Several brain structures and functions have been implicated in OCD. Studies have consistently shown hyperactivity in the orbitofrontal cortex and caudate. Other key implicated regions (suggested by structural or functional abnormalities, and/or connective abnormalities) include the dorsolateral prefrontal cortex, anterior cingulate cortex, thalamus, amygdala, and parietal cortex.
Structural brain abnormalities, examining the “whole brain” using magnetic resonance imaging (MRI), have reported structural abnormalities involving fronto-striatal circuits. Functional imaging studies have identified abnormalities in the basal ganglia, cingulate cortex, and orbitofrontal cortex in OCD when compared to healthy controls. In addition, functional brain imaging has been used when provoking OCD symptoms in individuals and has found increased activation in the right caudate, left anterior cingulate, and bilateral orbitofrontal cortex. Additionally, there is some suggestion that different subtypes of OCD may have distinct neural correlates. For example, research has found that OCD patients with washing compulsions exhibit increased activation compared to controls in bilateral ventromedial prefrontal regions and the right caudate nucleus, whereas those with checking compulsions exhibit activation in the putamen/globus pallidus, thalamus, and dorsal cortical areas.
Some OCD research also suggests that functional abnormalities in the orbitofrontal cortex, anterior cingulate cortex, and caudate can be ameliorated by behavior therapy or pharmacological interventions such as the SRIs. Whether the reported metabolic changes occurring over the course of successful treatment are simply a reflection of symptom reduction or of correction of underlying brain pathology is still unclear.
An understanding of the neural circuitry of OCD contributed to the development of successful surgical options for patients with severe refractory OCD, including deep-brain stimulation (specifically, of the ventral capsule or ventral striatum) or ablative neurosurgery (e.g., capsulotomy and cingulotomy).
Genetic Factors
Although relatively little is known about the etiology of OCD, it has been consistently reported for decades that OCD is transmitted within families. In addition, in cases of childhood-onset OCD, rates of OCD among first-degree relatives are higher than in relatives of adult-onset OCD patients. In fact, childhood-onset OCD is estimated to be 45–65 % heritable, and OCD with an onset during adolescence or adulthood 27–47 % heritable.
Familiality, however, does not necessarily mean an illness is genetic. Twin studies, however, can provide evidence of the extent to which a condition is influenced by genetic factors compared to environmental variables. Levels of monozygotic twin concordance have been reported to be between 63 % and 87 %, and first-degree relatives showing increased rates of OCD of 10–22.5 % compared with the normal population risk of 2–3 %.
As considered previously, genome-wide association studies and candidate gene studies have suggested that several genes may contribute to the increased risk of OCD such as genes in the glutamatergic, serotonergic, and dopaminergic systems. The genome-wide association studies, however, have produced inconsistent findings, and many have not been replicated or withstood rigid statistical analysis. Much of this research has led investigators to speculate that OCD may instead be due to dysregulation of genes in a functional brain network rather than single genes that cumulatively increase risk of OCD.
Animal Models of OCD
Animal models capable of capturing, or modeling, aspects of OCD could be useful to help explain treatment mechanisms and the neurobiological basis of human OCD and could even help to identify novel treatment directions for patients. Many animal models relating to OCD have been developed. However, because thought processes in animals are inaccessible, such models can only ever capture “compulsive” behaviors rather than the “obsessional” component of the disorder. Initial animal models of OCD focused on anxiety and conditioning. For example, electric shocks were paired with a light in dogs, leading to anxiety behaviors that persisted when a light was later triggered in the absence of shock – thus demonstrating persistence of behavior. In later genetic models, compulsive behaviors were found to arise from specific genetic manipulations. In mice with mutation of the “Hoxb8” gene, involved in brain development, repetitive grooming behaviors are observed, which have been argued to relate to OCD. Pharmacological models of OCD have also been developed. Checking behaviors are triggered in rodents by repeated administration of quinpirole, a dopamine D2/3 receptor agonist; these checking behaviors are reduced by clomipramine, a medication with efficacy in the treatment of human OCD. Another type of OCD animal model is the “ethological” type model, which refers to excessive compulsive behaviors observed “naturally” in a subpopulation of a given animal species. Examples include acral lick dermatitis in dogs, hair pulling in cats, feather picking in birds, or excess grooming of cage mates in mice. Some of these ethological models can occur sporadically (tail-chasing in dogs), while others (listed above) are more likely to develop in response to stressful circumstances. Finally, animal cognitive models of OCD have been studied. In this approach, animals show cognitive deficits (such as in relation to flexible responding, or control over inhibiting behavior) that are argued to be similar to aspects of cognitive dysfunction seen in OCD patients. A key example is the signal attenuation model, in which surplus lever-pressing by rats is reduced by many of the drugs that are useful in human OCD, but is not reduced by medications with no established efficacy in human OCD. In all, there are numerous intriguing animal models purporting to capture aspects of OCD. Each model has pros and cons, and none can ever capture all aspects of the human disorder. It remains to be seen whether such models can be used to successfully identify new drug treatments for OCD that translate into success in human OCD drug trials.
Outlook
In this chapter, we have provided a brief overview of biological findings in patients with OCD with respect to the integrated involvement of the central nervous system, the immune systems, and the contribution of genetic factors. We have also considered the role of animal models. Key neural circuitry involved in OCD includes orbitofrontal and dorsolateral prefrontal cortex, caudate nucleus, anterior cingulate cortex, parietal cortex, thalamus, and amygdala. Implicated neurotransmitters (in terms of pathology but also treatment mechanisms) include the serotonin, dopamine, and glutamatergic systems. Patients with OCD show cognitive problems especially on tests of flexible responding and the ability to suppress repetitive behaviors, but so too do asymptomatic people at heightened risk of developing OCD (clinically unaffected first-degree relatives of patients). Despite these advances in knowledge, up to 60 % of OCD patients do not get better in response to currently available pharmacological and psychological treatments. We hope that with time, these advances in knowledge will translate into the clinic.
Further Reading
Burguière E, Monteiro P, Mallet L, Feng G, Graybiel AM (2015) Striatal circuits, habits, and implications for obsessive-compulsive disorder. Curr Opin Neurobiol 30:59–65
Camilla d’Angelo LS, Eagle DM, Grant JE, Fineberg NA, Robbins TW, Chamberlain SR (2014) Animal models of obsessive-compulsive spectrum disorders. CNS Spectr 19(1):28–49
Chamberlain SR, Menzies L (2009) Endophenotypes of obsessive-compulsive disorder: rationale, evidence and future potential. Expert Rev Neurother 9(8):1133–1146
Grant JE (2014) Clinical practice: obsessive-compulsive disorder. N Engl J Med 371(7):646–653
Grant JE, Chamberlain SR, Odlaug BL (2014) Clinical guide to obsessive compulsive and related disorders. Oxford University Press, Oxford. ISBN 9780199977758
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this entry
Cite this entry
Grant, J., Chamberlain, S. (2016). Obsessive Compulsive Disorders. In: Pfaff, D., Volkow, N. (eds) Neuroscience in the 21st Century. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3474-4_160
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3474-4_160
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3473-7
Online ISBN: 978-1-4939-3474-4
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences