Abstract
Obsessive-compulsive disorder (OCD) is a clinical syndrome characterised by recurrent intrusive thoughts (obsessions) and repetitive mental or behavioural acts (compulsions), typically performed in response to obsessions or related anxiety. OCD generally has a stable symptom pattern throughout life but nevertheless is well known for its heterogeneity, as symptomatic presentations and comorbidity patterns differ widely among patients. A number of other psychiatric and neurological disorders may share similar phenomenological characteristics with OCD or are sometimes conceptualised as atypical OCDs. These heterogeneous aspects of the disorder have led to a search for OCD subtypes that might be associated with different aetiologies or treatment responses.
In the past few decades, the predominant models of OCD pathophysiology have focused on cortico-striatal circuitry, but more recent neuroimaging studies implicate involvement of the lateral and medial orbitofrontal cortices, the dorsal anterior cingulate cortex, and the amygdalo-cortical circuitry, in addition to cortico-striatal circuitry, in the pathophysiology of this disorder.
In this chapter, we have highlighted how a dimensional approach can offer opportunities for better assessment and more effective treatment than categorical diagnosis. The usefulness of this approach is based on the fact that the obsessive psychopathological dimension can be found in a number of syndromes and that treatment can be provided for it independently of the baseline disorder. For this purpose, our patients have been assessed with the SVARAD and treated accordingly, taking into account the particulars of each individual case.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Obsessive-compulsive disorder (OCD) has been an ancient companion of humans. The tendency to seek psychopathological concordance between OCD and disorders that demonstrate peculiar affinity with it can be traced back to comments by classical authors. Janet described the obsessive character using a large number of psychopathological phenomena including the “obsession de la honte du corps” (obsession of the shame of their body), due to dysmorphophobia; motor symptoms, which he defined as “forced agitations” not unlike the expression of a Tourette disorder; and experiences of depersonalisation. Dysmorphophobia was described by Kraepelin [1] as “compulsive neurosis”, emphasising the iterative and ego-dystonic nature of the symptoms.
Jaspers [2] highlighted a continuity of obsessive-compulsive symptoms and “impulsive actions,” suggesting common psychopathological roots for OCD and impulse control disorders. Krafft-Ebing [3] in Germany used the term Zwangsvorstellung to define invasive and irresistible thoughts that are oppressive (Zwang) representations (Vorstellung). Westphal [4] introduced the concept of compulsions as secondary to obsessive ideas, and obsessive-compulsive suffering in France was described as folie lucide, because the patient was quite aware of the wrong and anomalous recurring ideas besieging his mind [5]. Falret [6] introduced the word obsession from the Latin obsidere. Early in the nineteenth century, the term appeared in British and American medical literature [7].
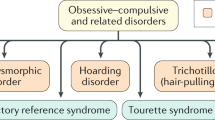
In more recent years, the renewed interest in OCD has led researchers to “drill down” in an attempt to define its subtypes and explore other psychiatric and neuropsychiatric disorders that might have clinical and/or aetiopathological links with OCD. Disorders that are posited to be linked to OCD, based on their similarities with OCD in a variety of domains, are referred to as “OC spectrum disorders” or “OC continuum” [8, 9]. On the other hand, OCD has undergone significant changes in its classification within categorical systems of mental disorders. The Diagnostic and Statistical Manual (DSM) III and DSM IV included OCD within the category of anxiety disorders, conceiving it as within the anxiety disorders group because of the often very high levels of anxiety in clinical OCD patients, along with the common symptoms of distressing obsessive thoughts and compulsive behaviours [10]. Growing evidence has finally led to a separation of OCD from the other anxiety disorders and to the decision by the DSM-5 task force to classify it within its own separate category: “obsessive-compulsive and related disorders” [11]. Today, the DSM-5 [11] recognises obsessive-compulsive and related disorders (OCRDs) as a new diagnostic category. The category includes OCD, body dysmorphic disorder (BDD), trichotillomania (TTM, hair-pulling disorder), excoriation disorder (skin picking), and hoarding disorder. OCD involves the experience of obsessions (recurrent, distressing intrusive thoughts, images, or urges) and compulsions (ritualised behaviours completed to reduce distress from obsessions). BDD involves an excessive, distressing, and time-consuming preoccupation with an imagined appearance flaw and repetitive rituals performed in response to this preoccupation. TTM is characterised by recurrent hair pulling, resulting in hair loss. Excoriation disorder involves recurrent skin picking, resulting in lesions. Finally, hoarding disorder involves persistent difficulty parting with possessions and a perception that items must be saved, resulting in clutter in one’s active living space that reduces the space’s usability [11].
The grouping of these conditions is based on their phenomenological similarities to OCD (i.e. obsessive thinking and/or compulsive behaviours), as well as similarity to OCD in course of illness, comorbidity, family history patterns, biological abnormalities, and treatment responses. The research planning agenda for DSM-5 examined possible similarities in phenomenology, comorbidity, familial and genetic features, brain circuitry, and treatment response between OCD and several related disorders that are characterised by repetitive thoughts or behaviours. Certain disorders, such as BDD, obsessive-compulsive personality disorder (OCPD), Tourette syndrome (TS), and TTM, share many commonalities with OCD in phenomenology, comorbidity, familial and genetic features, brain circuitry, and treatment response. Other disorders, such as the impulse control disorders (ICDs), share some common features with OCD but also differ in many ways as well.
According to most epidemiological studies, OCD is currently considered a relatively rare disorder, with a weighted 1-month prevalence of 1.1% in the British National Comorbidity Survey [12]. Similar results were reported by Crino et al. [13] who estimated the 12-month prevalence of DSM-IV OCD to be 0.6%.
Although many advances have been made with regard to the aetiopathogenesis and treatment of OCD, there are still no correct estimates of the prevalence of the disorder in the community. The variation in the different studies is mostly due to limitations in methodology and inconsistencies between lay and clinical diagnosis [14]. Further regarding prevalence in the general population, data obtained from a prospective longitudinal study of an unselected birth cohort has shown that 21–25% of individuals from the general population exhibit obsessions and/or compulsions, as defined in the DSM-IV, although only 2–3% meet full diagnostic criteria for the disorder [15].
The aim of this chapter is to disentangle obsessive-compulsive manifestations in psychiatric subjects not affected by OCD. In fact, obsessions and compulsions may range from physiologic/transient or normal presentation, to a pathological degree of suffering [16].
The continuum hypothesis, proposed by Clark and Rhyno [17], has been challenged by recent literature and regarded as an oversimplified interpretation of a more complex phenomenon of obsessions and compulsions, characterised not simply by quantitative but by qualitative differences as well, related in particular to the severity of the content of obsessions, triggers, appraisals, and responses. Berry and Laskey [18] argue for a revised continuum model of intrusive thoughts that incorporates the above-mentioned differences in obsessions, with particular reference to content and its severity, with clinically obsessive individuals reporting more bizarre and aggressive thoughts than individuals with symptoms too mild to be considered clinically obsessive.
Over the last 20 years, the concept of spectrum has received strong impetus in international psychiatry literature. The “spectrum” attributed to a psychopathological phenomenon may have various meanings. Strictly speaking, it should refer to a set of disturbances that, beyond possible heterogeneity of symptomatic manifestations, share the same aetiological determinants or similar pathogenic mechanisms. There are a number of reasons for this interest in “spectrum”. First, the identification of a psychopathological spectrum can guide the search for the common aetiopathogenic mechanisms underlying it. Second, this could be the first step in a common therapeutic approach. The finding of concordance between disorders, in various nosographic environments, does not relate only to psychopathological criteria but extends to common aetiopathogenic hypotheses, thus constituting a clinical picture with expected response to specific therapeutic treatments.
OCD is in a favourable position from this point of view. In fact, among psychopathological phenomena, obsessions and compulsions have a high level of consensus regarding their definition criteria. Moreover, this is one of the few cases in which the dominant presence of a single symptom allows the identification of a “syndrome” disorder. Despite this, the concept of the obsessive-compulsive (OC) spectrum has been discussed in the literature and increasingly studied, with contrasting evidence depending on the starting hypothesis (5HT system involvement and/or basal ganglia-thalamus-cortex-frontal circuitry).
Finally, the term “spectrum” has been used to mean many issues, as well as many disorders, that have a degree of similarity, at least in terms of symptoms, to OCD. The list includes BDD, hypochondriasis, trichotillomania, the eating disorders, autism spectrum disorders, and several other impulse control disorders, such as pathologic gambling and kleptomania. Other psychiatric disorders, such as depersonalisation disorder, borderline personality disorder, sexual compulsions, and paraphilias, and some neurological disorders such as Tourette’s syndrome, Sydenham’s chorea, and parkinsonism have been included in this spectrum.
8.2 Neurobiology of Obsessions and Compulsions
Initially, OCD was considered a primary psychiatric disorder. Subsequently, clinical observation increasingly showed that this disorder has a neurodevelopmental basis.
The first observation of the existence of brain alterations in obsessive patients resulted from the finding that patients with neurological dysfunctions, such as streptococcal infection, head trauma, or encephalitis, as well as comorbid tic disorders such as Tourette’s syndrome, often develop obsessive phenomena [19,20,21]. Several studies have reported an abnormally high prevalence of neurological soft signs (NSS) in patients with obsessive-compulsive disorder as compared to healthy people [8, 22].
The classical cortico-striato-thalamo-cortical (CSTC) model of OCD was established a few decades ago. Thanks to modern brain imaging methods, neurocircuitry models of OCD and related disorders have been refined to a higher level of complexity, with possible promising implications.
In addition to cortico-striatal circuitry, which is now regarded as interconnected rather than segregated, the lateral orbitofrontal cortex (OFC) might mediate obsessions, and the dorsal anterior cingulated cortex (dACC) might be implicated in fear expression and conditioning, as well as in aberrant error monitoring, in OCD. On the basis of such a conceptual framework, Milad and Rauch [23] proposed a testable hypothesis on how dysfunctions in these areas might be linked to fear inhibition and severity of symptoms. This information, in turn, could be used to predict treatment response.
Subsequent studies using functional magnetic resonance imaging (fMRI), positron emission tomography (PET), and single photon emission computed tomography (SPECT), as well as other more sophisticated techniques, such as voxel-based morphometry (VBM), diffusion tensor imaging (DTI), and proton magnetic resonance spectroscopy (1H-MRS), have compared OCD patients with healthy controls. These studies have tended to confirm the key role of the CSTC and its connections with the limbic system (amygdalo-cortical circuitry) in the pathogenesis of OCD [24, 25].
The above-mentioned functional imaging studies generally showed that patients with OCD have reduced grey matter density in the dorsolateral prefrontal cortex (DLPFC) and OFC and reduced volume of the anterior cingulate cortex (ACC) and OFC [26, 27]. Further, patients with OCD showed hyperactivity in the area of the OFC, caudate nucleus, and thalamus, compared with healthy controls [28,29,30]. PET studies of OCD patients have supported these findings, showing changes in brain metabolism, more or less in the same areas as previously described (head of the caudate nucleus and the orbital gyrus, OFC, and prefrontal cortex, which are a part of the CSTC circuit) [31]. Furthermore, the increased glucose metabolism along orbitofrontal-basal ganglia-thalamo-cortical circuits measured by PET generally decreases after treatment with antidepressants [32,33,34,35] and/or psychotherapy [36,37,38].
The empirical demonstration of the effectiveness of antidepressants (especially those blocking serotonin reuptake) for OCD dates back to more than 30 years ago. The new neuroimaging approaches, allowing the examination of regional cerebral neurochemistry and permitting in vivo quantification of specific neurochemicals in various brain regions, have allowed greater clarification of the role of serotonin in OCD.
Neurochemistry techniques have been used in the study of the transport of neurotransmitters, in order to better explain the role of serotonin in OCD. These studies have provided an increased understanding of the biology underlying the well-known empirical evidence that antidepressant drugs blocking serotonin reuptake improve obsessive symptoms over time. Also, they indicated not only the involvement of the serotonin system but also, albeit to a lesser extent, the involvement of dopamine [39].
These studies, mainly conducted using SPECT, allowed not only the confirmation of the role of serotonin and other neurotransmitters in OCD but also the examination of changes following treatment through cerebral metabolic monitoring [37, 38]. They also facilitated the development of hypotheses about both pharmacological and psychotherapeutic models that are potentially valid and useful in clinical practice [40].
As evidenced by early studies using PET and SPECT, hyperactivity of the head of the caudate nucleus and the orbital gyrus may be the source of complex obsessive symptomatology. Modern functional neuroimaging methods permit the establishment of a relationship between cerebral activity and a particular symptom. This allows comparison of cerebral activation in the presence of the symptoms of interest with corresponding activation in the same subject when these symptoms are resolved [41].
Several functional neuroimaging studies report that the cortico-striatal-thalamo-cortical (CSTC) circuit is dysfunctional in obsessive patients. This dysfunctional CSTC circuit consists mainly of altered communication between the lateral OFC and the ventral striatum [23, 42]. According to some authors, the “dysfunction” of this circuit would be hyperactivity during the resting or neutral state, which would increase during the onset of the symptoms, subsequently attenuating later pharmacological and behavioural treatment [32, 43, 44].
Studies by fMRI in OCD patients exploring brain metabolism alterations during a brain activation task report the involvement of the same areas that make up the CSTC circuit [30, 45, 46]. Most studies have examined these various areas, each of which, stimulated with specific tasks, produces a different result of increased, decreased, or stable glucose metabolism [47, 48].
Other studies have investigated possible changes in brain activation before and after drug therapy and/or psychotherapy [49, 50]. These neuroimaging studies have also, more sophisticatedly, sought to correlate the therapeutic response with neuropsychological tests, with the aim of finding predictive response indices. The resulting neuropsychological and treatment findings further support neuromorphological data, obtained through several different methods, implicating the role of CSTC circuitry in OCD pathophysiology. It has been mentioned several times before that OCD symptoms are manifested through a hyperactivity of the regions involved in the CSTC circuitry (coronary orbital cortex, cortical cortege, thalamus, and head of the caudate nucleus), causing a “malfunction” of this circuitry. Such a malfunction has been proposed to be the origin of the intrusive symptoms and neuropsychological dysfunctions [22, 49].
Regarding molecular imaging studies that have considered the role of neurotransmitters in brain sites involved in OCD obsessive phenomena, the results obtained, though encouraging, are limited due to small sample sizes and mixed diagnoses.
In approximately one third of patients with OCD, standard treatment with selective serotonin reuptake inhibitors (SSRIs) fails to bring satisfactory relief of obsessive-compulsive symptoms. Atypical antipsychotics can augment the effectiveness of SSRIs in such patients, but the mechanism underlying this synergetic effect still needs to be better clarified [51,52,53].
Another important aspect of OCD and related disorders, likely to be a common trait across specific diagnostic categories, has been recently considered and studied: deficits in goal-directed control. Deficits of this type have been observed across the spectrum of OCD and related disorders, for example, OCD [54,55,56], drug addiction [57, 58], and binge eating disorder [59]. These deficits are associated with dysfunction of the caudate and medial orbitofrontal cortex. Goal-directed control permits deliberate behaviour regulation. Its deficits lead to lack of flexibility; more rigid habits are induced; and repetition of thoughts and actions is enhanced. Gillan et al. looked at this trait as a clue to a transdiagnostic compulsivity dimension and, in two large general population samples, found it to be associated with (1) OCD symptoms and (2) symptoms of other DSM diagnostic categories. Exactly these kinds of studies reflect the concept of dimensional psychopathology as suggested by Pancheri [60].
Obsessive phenomena may appear in other psychiatric disorders, in comorbidity, and occasionally even in healthy subjects. Therefore, it is conceivable that these obsessive phenomena share at least part of the same pathogenic mechanism.
The empirical demonstration of the effectiveness of antidepressants, especially serotonin reuptake blockers, on OCD and, consequently, also on obsessive phenomena can be traced back to 30 years ago.
8.3 Dimensional Psychopathology of Obsessions
A psychopathological dimension is defined as an alteration of psychic function phenomenologically expressed by symptoms (referred to by the patient) or by signs (observed) that are indicative of and specific to the observed function [61].
Obsessions and compulsions, like any other psychiatric symptoms, can appear as psychopathologically dominant and exclusive elements, or they can be associated with a psychopathological framework in which one or more symptoms, and possibly a cluster of other symptoms, characterise a specific clinical picture. In the first case, “symptom” and “disorder” coincide and qualify as the OCD. In other conditions, obsessive symptoms occur in association with, or in the presence of, other symptoms within the main disorder (e.g. schizophrenic episode) or in comorbidity.
The dimensional model posits that obsession-compulsion may, however, manifest itself with a certain frequency in association with typical symptoms of a given syndrome (e.g. depressive episode). In this case, the obsessive phenomenon must be considered as a symptom, even if an atypical one, that takes on particular characteristics in relation to the disorder in which it is co-appearing. In other words, the basis of the obsessive symptom probably follows pathogenic mechanisms and has neurobiological, genetic, neuroanatomical, neurochemical, or psychophysiological correlates, stemming from the disturbance with which it is associated. This means that, rather than the obsessive symptom mechanisms being separate from the mechanisms underlying the main disorder, the different mechanisms can influence and trigger each other in the context of a particular clinical presentation. Obsession, therefore, understood as a symptom with a specific pathogenic mechanism with its own psychopathological manifestations, can appear in many psychiatric disorders with sometimes-different phenomenological characteristics. Taking this into account, in the next analysis, transnosographic aspects of this dimension will be fully explored.
8.4 Obsessions and Schizophrenia
The frequency of obsessive symptoms in schizophrenia seems to be higher than in the general population. The percentage of schizophrenic patients having “obsessive-compulsive symptoms” reported in the literature fluctuates between 30% and 59% [62], and the frequency of OCD comorbidity in patients affected by schizophrenia has been estimated to range from approximately 8 to 23% [63]. In contrast, the appearance of schizophrenic symptoms in the course of OCD seems to be relatively rare and only slightly higher than the incidence of schizophrenia in the general population [64]. These data indicate that the schizophrenic disorder could present a vulnerability to obsessions, but not vice-versa. It has even been proposed that the presence of obsessive-compulsive symptoms could be an extreme mechanism of defence that takes place during the initial phase of the psychotic disorder [65].
Data suggest that, because of the involvement of similar functional brain networks (e.g. frontal cortex, basal ganglia) and neurotransmission systems (serotonin and dopamine), in these two disorders, it may be possible to identify a subgroup, designated schizo-obsessive [66]. However, it is not yet clear whether the presence of obsessive symptoms in schizophrenic patients is an indicator of good prognosis [67, 68] or, as has been found in the latest literature, of poor prognosis (in terms of clinical and functional outcomes, including responsiveness to treatment) [69,70,71]. It should be emphasised that these studies are affected by certain limitations related to sample inequalities and methodologies used.
Some studies have investigated obsessive-compulsive symptoms induced or markedly aggravated by second-generation antipsychotic treatment, particularly with clozapine (most frequent), olanzapine, and risperidone [72]. These effects, however uncomfortable and poorly tolerated by patients, must always be evaluated in the context of the overall intervention. It should be remembered that, especially in the case of clozapine, this is a drug used in resistant schizophrenia and one that is also effective for suicidal ideation [73]. Further, it is often used in monotherapy. Therefore, before suspending treatment, all possible caution should be exercised. In this regard, various strategies for augmentation with anti-obsessive drugs have been proposed, before discontinuing clozapine, and have also been shown to be effective (aripiprazole and amisulpride) [74, 75]. Alternatively, CBT has also proved effective in some schizophrenic patients with obsessive-compulsive symptoms who did not respond well to the various pharmacological protocols [76].
8.5 Obsessions and Mood Disorders
The presence of obsessive-compulsive symptoms in mood disorders has been recognised especially in depression. Regarding bipolar disorder, obsessive-compulsive symptoms manifest themselves more often during depressive episodes and almost never during manic episodes. There is an apparent comorbidity between bipolar disorder and OCD: among OCD patients, 18.3% also have bipolar disorder, and among bipolar patients, 17% also have OCD. However, studies have shown that obsessive-compulsive symptoms occur frequently in depressive patients as well, with an approximate incidence of 20–40% [77].
This suggests that when there is a depressive disorder, obsessions can be, as in the case of schizophrenia, a defensive factor that appears to ease the suffering of the depressed patient. In the case of depression, an additional predisposing factor seems to be represented by a personality with traits or features of “obsessive” type. In contrast to what may happen in schizophrenic disorder, the obsessive-compulsive symptoms in depression keep their fundamental characteristics, especially with respect to awareness of illness.
8.6 Obsessions and Eating Disorders
In light of the new definition of eating disorders that emerged in the DSM-5 and new findings on their aetiopathogenesis, their relationship with OCD has also gained new significance. While earlier emphasis was placed on personality aspects, emphasising obsessive personality traits or comorbid OCD in patients with anorexia nervosa, the concept of spectrum in this group of diseases is currently spreading and becoming increasingly accepted. In line with this, eating disorders can be considered as a spectrum within which, in addition to the more classical anorexia and bulimia nervosa, there are a number of other new disorders or behavioural alterations, including anorexia, “reverse anorexia” or “bigorexia” (i.e. muscle dysmorphia, a phenomenon started among professional athletes and now rising in the general population) [78], “diabulimia” (an eating disorder specific to patients with diabetes, characterised by limiting insulin treatment to lose weight through sustained hyperglycaemia) [79], “drunkorexia” (restricting food intake prior to drinking alcohol to avoid weight) [80], and “pregorexia” (pregnant women who will reduce calories and exercise in excess in an effort to control pregnancy weight gain) [81]. Many of these eating disorders show strong affinity with OCD, in light of the well-known exercise of control. One condition in particular, which is not entirely pathological, is orthorexia nervosa. According to some authors, it appears that, aside from anorexia nervosa, obsessive phenomena seem to be most marked in this disorder [82]. The term orthorexia nervosa describes people whose extreme diets, intended for health reasons, end up leading to malnutrition and/or impairment of daily functioning. Although studies on this are still few and with different methodological limits, it turns out that these patients, apart from poor insight, share many features with OCD and obsessive personality disorder, as anorexia nervosa does [83, 84]. The phenomenological aspects these disorders share include perfectionism, rigid thinking, preoccupation with details and perceived rules, and high levels of anxiety [85]. However, it is important to remember that there is a significant difference between this continuum and OCD, represented by the ego-syntonic experience present in eating disorders and usually absent in OCD. Nevertheless, these data give rise to new questions and further insights [86].
8.7 Treatments
The available research indicates that evidence-based psychotherapy options targeting the Obsessiveness dimension include Exposure with Response Prevention (ERP) and cognitive behavioural therapy (CBT) [87]. An interesting study suggests that basolateral amygdala-ventromedial prefrontal cortex connectivity seems to predict CBT outcome in obsessive-compulsive patients. Although this is reported only by one study, this data suggests that this cerebral structure might be a target of CBT for Obsessiveness [88].
Third-wave cognitive-behavioural therapies for OCD have become more popular in the past few years. These are therapies such as ACT (acceptance and commitment therapy) and MBCT (mindfulness-based cognitive therapy), which encompass cultivating a different relationship with the symptoms, in which the patient is asked to observe the manifestation of the symptoms and accept them as they are. The hypothesised mechanism underlying these therapies is that the maintenance of the symptoms is curtailed as the patient assumes a decentralised perspective towards them. Currently, there is no neuroimaging evidence on the circuits or brain areas modulated by third-wave CBT targeting the Obsessiveness dimension, but it is reasonable to argue that these psychotherapeutic treatments target brain structures and circuits that are involved in the manifestation of obsessive and compulsive behaviour. Despite the good outcome of these therapies in targeting the Obsessiveness dimension, there is currently too little evidence in the literature to support their choice as a first-line therapy. However, they are good candidates for add-on therapies to complement classical CBT and exposure with response prevention [89].
As concerns other available treatments targeting the Obsessiveness dimension, novel neurostimulatory techniques are able to target the cortico-striato-thalamo-cortical loop, involved in obsessive and compulsive behaviour. In particular, these techniques include deep brain stimulation (DBS), repetitive transcranial magnetic stimulation (rTMS), and transcranial direct current stimulation (tDCS), which all can elicit changes in specific brain regions implicated in obsessive and compulsive symptoms. A growing body of literature is showing that brain stimulation techniques can improve symptoms by modulating cortico-striatal circuit activity [90, 91]. DBS targeting the nucleus accumbens (NAcc) reduced anxiety and obsessive symptoms in subjects with OCD and enhanced libido [92]. Even DBS of the ventral caudate led in some cases to an improvement of OCD symptoms [93]. Two studies have shown that the application of inhibitory rTMS to both the left and right lateral orbitofrontal cortex (lOFC) led to a significant improvement of obsessive and compulsive symptoms, and this improvement was associated with a decrease in local metabolism of lOFC [94, 95]. Only two studies investigated tDCS targeting the OFC: Mondino et al. [96] showed a decrease of OCD symptomatology that was maintained after a 1-month follow-up. The protocol consisted of ten twice-daily sessions of tDCS inhibitory stimulation of the left OFC. Bation et al. [97] used the same protocol as Mondino et al. and reported similar results. There is no evidence that electroconvulsive therapy (ECT) improves obsessive or compulsive symptoms [98].
These studies are still in their infancy, but the preliminary results and preclinical trials appear promising in their findings, mostly with regard to resistant symptoms that exist transdiagnostically across traditional categories of psychiatric suffering.
8.8 Findings
The SVARAD describes the Obsessiveness dimension as “Doubtfulness, rigidity, meticulousness, perfectionism; repetitive behaviours aimed at preventing, checking, controlling; presence of obsessions, compulsions”. As described in the previous chapters, each item of the SVARAD is scored on a 5-point rating scale (from 0 to 4), where the highest score represents a profound presence of “invasive obsessions and compulsions, present for the vast majority of the day, non-controllable, with impairment of the social and occupational activities”. Among the SVARAD dimensions, Obsessiveness is probably the one that is most closely linked to a specific diagnostic category. However, it was introduced into dimensional assessment because clinical experience has suggested that non-OCD disturbances often have an Obsessiveness component or manifestation: for example, body dysmorphic disorder (BDD), trichotillomania, and hoarding disorder. SVARAD studies reported Obsessiveness findings from both the inpatient and outpatient groups of our sample. We present here data concerning our diagnostic groups, exploring how the SVARAD Obsessiveness dimension is present as a transdiagnostic feature (Table 8.1).
This section reviews Obsessiveness findings from both the inpatient and outpatient groups of our sample.
The SVARAD Obsessiveness dimension shows low mean scores in the psychiatric inpatient group as a whole (Fig. 8.1), as well as in the outpatient sample (Fig. 8.2).
High scores on the SVARAD Obsessiveness dimension in the inpatient group were most highly correlated with OCD, followed by schizophrenia, bipolar disorder, depressive episode, major depressive disorder, and psychotic disorder NOS. Figure 8.3 shows the mean (±standard deviation) value of the SVARAD Obsessiveness dimension in the inpatient sample for several DSM-IV-TR diagnostic categories. The highest mean values were observed in OCD (2.72 ± 1.48), followed by schizophrenia (0.45 ± 0.95), bipolar disorder-depressive episode (0.38 ± 0.87), major depressive disorder (0.36 ± 0.71), and finally, psychotic disorder NOS (0.30 ± 0.86).
It’s interesting to point out that, although mean Obsessiveness scores were low throughout the inpatient group, 25.1% of depressive patients (Fig. 8.4), 20% of bipolar-depressive episode patients (Fig. 8.5), and 23.3% of schizophrenic patients (Fig. 8.6) have an Obsessiveness score greater than zero. From a clinical viewpoint, this suggests that taking this dimension into account could lead to better understanding and treatment of one out of four cases.
The mean SVARAD profile for OCD in the inpatient sample displayed a 4-1-2 code type and is shown in Fig. 8.7. Multiparametric analysis showed the highest peak for the Obsessiveness dimension (2.88 ± 1.35), two peaks for the Apprehension/Fear (2.25 ± 1.16) and Sadness/Demoralisation (2.25 ± 1.03) dimensions, and a final peak for the Apathy (2.13 ± 1.45) dimension, all with mean scores above 2. Four out of eight cases had a moderate grade of Apprehension/Fear, and one out of three had a severe/extreme value for this dimension. One patient out of three had a moderate degree of Sadness/Demoralisation, while one out of three had severe to extreme degrees of this dimension. One half of the group had severe to extreme degrees of Apathy.
Obsessiveness was negatively correlated with Impulsivity (0.636 ± 1.027, Rho = −0.71, p = 0.038) and Activation (0.545 ± 1.214, Rho = −0.629, p = 0.038). Significant positive correlations were also seen between Obsessiveness and Apprehension/Fear (Rho = 0.147, p < 0.001), Sadness/Demoralisation (Rho = 0.148, p < 0.001), and Apathy (Rho = 0.51, p < 0.001).
Regarding the Obsessiveness dimension, values were highest for the OCD DSM-IV diagnostic outpatient group, which displayed mean values just above a score of 2, which is lower than those in the OCD inpatient group, as expected, because of less severe psychopathology in the outpatient group (Fig. 8.8). The highest mean values were observed in OCD (2.68 ± 0.97), followed by eating disorders (0.62 ± 0.89), delusional disorder (0.58 ± 0.90), bipolar disorder-depressive episode (0.45 ± 0.73), and schizophrenia (0.39 ± 0.76).
One patient out of three in the following diagnostic categories had an Obsessiveness score between mild and severe: eating disorders (40%) (Fig. 8.9), bipolar disorder-depressive episode (36%) (Fig. 8.10), delusional disorder (33.8%) (Fig. 8.11), and schizophrenia (30%) (Fig. 8.12). One patient out of four in the following diagnostic categories had an Obsessiveness score between mild and severe: psychotic disorder NOS (27%), dysthymia (27%) (Fig. 8.13), somatoform disorders (26%) (Fig. 8.14), major depressive disorder (25%) (Fig. 8.15), anxiety disorder NOS (24%), and finally, borderline personality disorder (23%) (Fig. 8.16). Although the mean Obsessiveness scores seem low, one quarter to one third of patients of several diagnostic groups had a mild to severe degree of Obsessiveness, indicating that this dimension should be considered for better comprehension and treatment. Mild to moderate Obsessiveness probably predicts to some extent a more problematic relationship with rumination, compulsivity, and doubtfulness, while from a pharmacological perspective, it suggests the choice of 5-HT antidepressants rather than noradrenergic or dopaminergic antidepressants.
The SVARAD dimensional profile of the outpatient OCD group showed a 4-1-2 code type. The Obsessiveness dimension had the highest mean values (2.68 ± 0.98), followed by Apprehension/Fear (2.16 ± 0.86), Sadness/Demoralisation (1.48±0.96), Apathy (0.77 ± 0.92), and Aggressiveness (0.77 ± 0.92) (Fig. 8.17). As Fig. 8.17 shows, more than one half of the group displayed a moderate degree of Apprehension/Fear, while nearly one patient out of four displayed a severe degree of Apprehension/Fear. One half of the group had a moderate to severe degree of Sadness/Demoralisation. One patient out of four showed a moderate degree of Aggressiveness: that is, a clinically significant proportion.
8.9 Discussion
As expected, our findings showed low mean Obsessiveness dimension scores for several categories, with the exception of the OCD diagnostic category, both in the inpatient and outpatient groups. Regarding the OCD group, the SVARAD mean profiles for the inpatient and outpatient samples showed different clinically significant dimensional components for OCD. The OCD group consisted of 8 out of 867 inpatients and 31 out of 1124 outpatients. Given that seldom is OCD so severe as to require acute hospitalisation in Italian general hospital psychiatric wards, our OCD inpatient group represents patients with very severe symptoms, so that our findings may only be partially representative of the whole diagnostic category.
The first finding concerning low values of the Obsessiveness dimension in the whole inpatient and outpatient group reflects the fact that obsessiveness and iterativity are uncommon in psychiatric diagnoses other than OCD. This differs from Apprehension/Fear and Sadness/Demoralisation, which are widespread and present in various psychopathological disorders. In inpatients, after the OCD diagnostic category, the Obsessiveness dimension scores were the second and third most relevant dimensions in schizophrenia and bipolar disorder-depressive episode, respectively.
In the outpatient sample, Obsessiveness was the second and third most relevant dimension in eating disorders and delusional disorder, respectively (see Figs. 8.3 and 8.8). As concerns schizophrenia, our relatively high Obsessiveness SVARAD scores in some cases are not surprising: possible obsessive thoughts and iterative behaviours have often been described in the psychopathological literature for this diagnostic category, before and after the DSM-III [66, 68, 99]. Their presence, however, was not formally included in the DSM and ICD criteria for schizophrenia or delusional disorder. In light of this absence, SVARAD representation seems to be meaningful for psychopathological completeness and subsequent treatment. Two clinical cases might better illustrate this concept.
Case Vignette 1: Paranoid Schizophrenia
Mary is a 46-year-old woman with a DSM-IV-TR diagnosis of paranoid schizophrenia. She lives in a therapeutic community and has a middle-school diploma. She was hospitalised for 17 days. Her SVARAD dimensional profile shows the highest peak in the Obsessiveness dimension (score 4), followed by Apathy, Reality Distortion, and Thought Disorganisation (score 3), and finally Anger/Aggressiveness, Apprehension/Fear, and Activation (score 2) (Fig. 8.18). Psychopharmacological treatment was utilised to address the psychopathological needs of this patient, including the following treatments targeting the SVARAD dimensions: Reality Distortion (quetiapine RP 400 mg/day), Obsessiveness (sertraline 50 mg/day), Activation, Anger/Aggressiveness, and Apprehension/Fear (valproic acid CH 1000 mg/day, diazepam 20 mg/day, and clonazepam 6 mg/day).
Case Vignette 2: Psychotic Disorder Not Otherwise Specified
Michael is 29 years old, with a DSM-IV-TR diagnosis of Psychotic Disorder NOS. He lives with his parents, has a middle-school diploma, and is currently not working. He was hospitalised for 10 days. His SVARAD dimensional profile shows the highest peak in the Obsessiveness dimension (score 4) followed by Apprehension/Fear, Sadness/Demoralisation, Apathy, and Somatic Preoccupation/Somatisation (score 3). The Reality Distortion and Thought Disorganisation dimensions reached scores of 2. The patient did not fulfil DSM-IV-TR diagnostic criteria for obsessive-compulsive disorder or major depressive disorder. The patient was treated with olanzapine, a second-generation antipsychotic that may cause OCD symptoms OCDS (Fig. 8.19). Psychopharmacological treatment was utilised to address the psychopathological needs of this patient, including the following treatments targeting the SVARAD dimensions: Obsessiveness (fluoxetine 20 mg/day and aripiprazole 15 mg/day), Sadness/Demoralisation and Apathy (venlafaxine 150 mg/day), Reality Distortion (olanzapine 10 mg/day and aripiprazole 15 mg/day), and Apprehension/Fear (zolpidem 10 mg/day, gabapentin 900 mg/day, and clonazepam 5 mg/day).
It is also interesting to point out that the DSM-5 introduces three levels of insight concerning beliefs associated with OCD: good insight, poor insight, or no insight/delusional belief. A patient with an OCD diagnosis at this last level of insight should not be diagnosed—according to the DSM-5—as a psychotic disorder. The differential diagnosis suggested by the DSM-5 is to classify obsessions and compulsions without insight as schizophrenia or schizoaffective disorder only if the patients include in their clinical manifestation hallucinations or formal thought disorders (DSM-5, 2013, p. 241).
The issue of differential diagnosis between OCD and schizophrenia is, however, difficult in some clinical cases and has been under debate for many years and from several perspectives. Obsessions and compulsions in the past were seldom recognised by clinical psychiatry as a possible component in some clinical pictures of these disorders. As Fineberg [100] emphasises:
In the past OCD was thought to have more in common with psychotic disorders than we recognize today…Like OCD, schizophrenia develops in early adulthood, runs a chronic course, and shows roughly equal gender ratios in clinical cohorts. Co-occurrence of OCD, bizarre grooming, and hoarding in schizophrenia is well recognized… it remains unclear whether the observed overrepresentation of obsessive-compulsive symptoms in schizophrenia reflects true comorbidity, more severe illness, or distinct neuropsychological substrates unique to this group.
Obsessive-compulsive symptoms of a neurotic disorder were viewed, according to the psychodynamic perspective, as the “last” defence from a psychotic decompensation and the emergence of a schizophrenic disorder. Their appearance during the clinical course of schizophrenia, conversely, might suggest the beginning of an improvement of the psychotic state towards a “less severe” and better integrated neurotic functioning. Bahnson (1966), in his psychodynamic model of “psychophysiological complementarity”, for instance, proposes the hypothesis that the relationship between OCD and schizophrenia reflects a larger degree of behavioural regression under stress for the latter, as a consequence of external life events or severe internal intrapsychic conflicts [101]. It is interesting to point out that the SVARAD seems to be able to capture Obsessiveness components within non-OCD disorders, and this represents a relevant finding for complete psychopathological assessment and treatment of many patients. Of note, Bellodi [102] discusses the need for a fine cross-sectional psychopathological analysis but also the observation of the longitudinal course of the clinical picture of these cases for the differential diagnosis between OCD with poor insight and schizophrenia. With regard to our findings of mild mean Obsessiveness values in eating disorder outpatients, the issue of comorbidity between eating disorders and OCD has been widely discussed, as has been the presence of obsessive-compulsive symptoms in eating disorders. The DSM-5 considers obsessive-compulsive symptoms in the differential diagnosis of anorexia nervosa but not bulimia nervosa, suggesting that OCD comorbidity should only be considered if the individual shows obsessions and compulsions which are not related to food. Eating disorders have also been extensively discussed as belonging to the OCD spectrum [85, 86]. The following case vignette can better illustrate this concept.
Case Vignette 3: Anorexia Nervosa
Sara is a 30-year-old woman with a DSM-IV-TR diagnosis of anorexia nervosa. She lives with her parents and has a high school degree. She is currently studying at a university. She was hospitalised for a duration of 12 days. Her SVARAD dimensional profile showed the highest peak in the Obsessiveness dimension (score 4), followed by Sadness/Demoralisation, Apathy and Impulsivity (score 3), and Apprehension/Fear (score 2) (Fig. 8.20). The patient did not fulfil DSM-IV-TR diagnostic criteria for OCD or major depressive disorder. She was treated with clomipramine 150 mg/day (targeting Obsessiveness and Sadness/Demoralisation), topiramate 50 mg/day, and olanzapine 10 mg/day (targeting Impulsivity and Apprehension/Fear), together with medical treatment to support metabolic functions.
Considering the above discussion about psychotic disorders, eating disorders, and OCD symptoms and the formulation of clear-cut criteria and categorical distinction by the DSM-5, it is interesting to point out how the routine use of the SVARAD might be useful in the clinical setting. The SVARAD allows the recognition of Obsessiveness components in both disorders, even if they do not fully satisfy the criteria for classification of OCD as a comorbidity. Of some interest is the fact that the SVARAD Obsessiveness dimension displays a significant role in major depression. Although not relevant for this diagnostic group as a whole, the recognition of a major depression subgroup with significant Obsessiveness components is of peculiar interest because of its potential role for assessment of the intrapsychic functioning and the choice of psychopharmacological treatment, perhaps suggesting 5HT-ergic (such as clomipramine and SSRI) antidepressants as better than noradrenergic antidepressants [103]. In the OCD inpatients, we found that the Obsessiveness dimension displayed the highest score, followed by Apprehension/Fear, Sadness/Demoralisation, and Apathy (all with mean scores above 2). Furthermore, Obsessiveness was negatively correlated with Impulsivity (r = −0.71, p = 0.038) and Activation (r = −0.629, p = 0.038), and positively correlated with Apprehension/Fear (Rho = 0.147, p < 0.001), Sadness/Demoralisation (Rho = 0.148, p < 0.001), and Apathy (Rho = 0.51, p < 0.001). In the OCD outpatients, the SVARAD dimensional profile also showed the highest value for the Obsessiveness dimension, followed by Apprehension/Fear, Sadness/Demoralisation, Apathy, and Anger/Aggressiveness. Unlike in the inpatient OCD group, Apathy mean scores were below 1, suggesting lesser impairment of affective reactivity and more active involvement with life. One can argue that these results are a reflection of a less severe psychopathology than that of the inpatient group. In addition, the outpatient group showed, as the fourth peak, Anger/Aggressiveness: this finding could confirm the association of anger with symptom subtypes in severe OCD outpatients [104]. The two SVARAD dimensional mean profiles for OCD inpatients and outpatients reflect the main different components of suffering that the clinician can observe in these patients. These components are not formally included in DSM-5 and ICD diagnostic criteria. The clinical picture of OCD patients—even when cases fulfil the DSM criteria—can significantly differ from individual to individual.
Case Vignette 4: Obsessive-Compulsive Disorder
Marc is 69 years old, with a DSM-IV-TR diagnosis of obsessive-compulsive disorder. He lives alone and is an unemployed university graduate. He was hospitalised for a duration of 16 days. His SVARAD profile shows two main peaks (score 4) in Obsessiveness and Sadness/Demoralisation, followed by a third peak in Apathy (score 3) and a fourth peak in Apprehension/Fear (score 2). The patient does not fulfil the DSM criteria for a depressive episode or major depressive disorder (Fig. 8.21).
The psychopharmacological treatment addressed the psychopathological needs of this patient, including the following treatments targeting the profile’s dimensions: Obsessiveness (sertraline 50 mg/day, aripiprazole 10 mg/day), Sadness/Demoralisation and Apathy (venlafaxine 150 mg/day), and Apprehension/Fear (diazepam 20 mg/day and quetiapine SR 100 mg/day).
Case Vignette 5: Obsessive-Compulsive Disorder with Comorbid Diagnosis of Psychotic Disorder NOS
Colette is 37 years old, with a DSM-IV-TR diagnosis of OCD with comorbid psychotic disorder NOS. She currently lives with her parents and is unemployed. She was hospitalised for a duration of 18 days. The patient also takes a full dose of clozapine, and this may induce the onset of obsessive symptoms. Her SVARAD profile shows two main peaks (score 4) in Obsessiveness and Apathy, followed by Apprehension/Fear, Sadness/Demoralisation, Reality Distortion, and Thought Disorganisation (score 2) (Fig. 8.22). The psychopathological needs of this patient were addressed through psychopharmacological treatment, including the following drug treatments targeting the profile’s dimensions: Reality Distortion (clozapine 500 mg/day), Sadness/Demoralisation and Apathy (lamotrigine 150 mg/day, as a mood stabiliser with mild antidepressant properties), Apprehension/Fear (zolpidem 7.5 mg/day and diazepam 4 mg/day), and Obsessiveness (clomipramine 150 mg/day).
Another issue resulting from our findings is the presence of the Obsessiveness dimension at mild (score 1) to moderate (score 2) levels in several DSM-IV diagnostic groups, as well as mild to severe (score 3) levels in other groups. As previously reported, in outpatients, one patient out of three shows an Obsessiveness score between mild and severe for the following disorders: eating disorders (40%), bipolar disorder and depressive episode (36%), delusional disorder (33.8%), and schizophrenia (30%). One outpatient out of four shows mild to severe Obsessiveness for the following disorders: psychotic NOS (27%), dysthymia (27%), somatoform disorders (26%), major depressive disorder (25%), anxiety disorder NOS (24%), and finally, borderline personality disorder (23%). In a similar way, although mean Obsessiveness scores were low in the whole inpatient group, 25.1% of major depression patients, 20% of bipolar patients-depressive episode, and 23.3% of schizophrenic patients have an Obsessiveness SVARAD score between 1 (mild) and 4 (very severe).
In both inpatient and outpatient groups, some degree of Obsessiveness is present in a small but significant proportion of cases, providing suggestions for clinical attention and more precise psychopharmacological targeting and related interventions. The construction of the therapeutic alliance should take into account the possible presence of patient characteristics like doubtfulness, inflexibility, preciseness, checking or preventing behaviours, presence of obsessions or compulsions, rumination, and some tendency towards slowness, ranging from mild to severe. Although mean Obsessiveness scores seemed low, in one third to one quarter of patients from several diagnostic groups, Obsessiveness played a role, from mild to severe, that could be considered as helpful for better comprehension and treatment.
Finally, our studies of the Obsessiveness SVARAD dimension have several limitations. The first is that the assessment of the Obsessiveness dimension does not allow distinguishing between obsessions and compulsions. This was a methodological choice in the construction of the SVARAD, for the sake of simplicity, because obsessions, iterative manifestations, and compulsions are clinically often—although not always—presented as concomitants in the same patient. This represents a limitation of the studies with regard to the obsessive compulsive spectrum of these disorders, which may manifest more strongly in iterative/compulsive behaviour than in the obsessive component. In all of these cases, further psychopathological assessment with specific instruments should be added, even if they require more complex designs, personnel, and time.
A second limitation is the fact that the cases discussed in this chapter are limited to a cross-sectional observation. Further analyses are needed, taking into account longitudinal course and, particularly, response to treatment, via pre- and post-discharge assessments.
References
Kraepelin E. Psychiatrie. Ein Lehrbuch für Studierende und Ärzte Klinische Psychiatrie. Leipzig: Barth; 1915.
Jaspers K. Allgemeine Psychopathologie. 5th ed. Berlin: Springer; 1948.
Krafft-Ebing R. Űber Geisterstörungen durch Zwangsvorstellung. Allg Z Psychiatr. 1879;35:303–28.
Westphal C. Űber Zwangsvorstellung. Arch Psychiatr Nervenkr. 1872;3:138–61.
Janet P. Les Obsessions et la Psychasthenié. Paris: Alcan; 1919.
Falret JP. Obsession intellectuelles et emotives. Arch Neurolog. 1889;2:274–93.
Berrios GE. The history of mental symptoms. Cambridge: Cambridge Univeristy Press; 1996.
Hollander E, Schiffman E, Cohen B, Rivera-Stein MA, Rosen W, Gorman JM, Fyer AJ, Papp L, Liebowitz MR. Signs of central nervous system dysfunction in obsessive-compulsive disorder. Arch Gen Psychiatry. 1990;47(1):27–32.
Hollander E. Obsessive-compulsive spectrum disorders: an overview. Psychiatr Ann. 1993;23(7):355–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 3rd edition, revised. Washington, DC: American Psychiatric Association; 1987.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Torres AR, Prince MJ, Bebbington PE, Bhugra D, Brugha TS, Farrell M, Jenkins R, Lewis G, Meltzer H, Singleton N. Obsessive-compulsive disorder: prevalence, comorbidity, impact, and help-seeking in the British National Psychiatric Morbidity Survey of 2000. Am J Psychiatry. 2006;163(11):1978–85.
Crino R, Slade T, Andrews G. The changing prevalence and severity of obsessive-compulsive disorder criteria from DSM-III to DSM-IV. Am J Psychiatry. 2005;162(5):876–82.
Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53–63.
Castle DJ, Phillips KA. Obsessive–compulsive spectrum of disorders: a defensible. Aust N Z J Psychiatry. 2006;40(2):114–20.
Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, Poulton R. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166(3):329–36.
Clark DA. Innovation in obsessive compulsive disorder: A commentary. J Behav Ther Exp Psychiatry. 2015;49(Pt B):129–32.
Berry LM, Laskey B. A review of obsessive-compulsive thoughts in the general population. J Obsessive Compulsive Relat Disord. 2012;1:125–32.
Berthier ML, Kulisevsky J, Gironell A, Heras JA. Obsessive-compulsive disorder associated with brain lesions: clinical phenomenology, cognitive function, and anatomic correlates. Neurology. 1996;47:353–61.
Carmin CN, Wiegartz PS, Yunus U, Gillock KL. Treatment of late-onset OCD following basal ganglia infarct. Depress Anxiety. 2002;15:87–90.
Murphy DL, Timpano KR, Wheaton MG, Greenberg BD, Miguel EC. Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts. Dialogues Clin Neurosci. 2010;12:131–48.
Bolton D, Gibb W, Lees A, Raven P, Gray JA, Chen E, et al. Neurological soft signs in obsessive compulsive disorder: standardised assessment and comparison with schizophrenia. Behav Neurol. 1998;11:197–204.
Milad MR, Rauch SL. Obsessive compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16(1):43–51.
Breiter HC, Rauch SL. Functional MRI and the study of OCD: From symptom provocation to cognitive-behavioral probes of cortico-striatal systems and the amygdala. NeuroImage. 1996;4(3 Pt 3):127–38.
Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, López-Solà M, Hernández-Ribas R, Deus J, Alonso P, Yücel M, Pantelis C, Menchon JM, Cardoner N. Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch Gen Psychiatry. 2009;66(11):1189–200.
Szeszko PR, Robinson D, Alvir JM, Bilder RM, Lencz T, Ashtari M, et al. Orbital frontal and amygdala volume reductions in obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56:913–9.
Rotge J-Y, Guehl D, Dilharreguy B, Tignol J, Bioulac B, Allard M, et al. Meta-analysis of brain volume changes in obsessive-compulsive disorder. Biol Psychiatry. 2009;65(1):75–83.
Saxena S, Rauch SL. Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:563–86.
Saxena S, Bota RG, Brody AL. Brain-behavior relationships in obsessive-compulsive disorder. Semin Clin Neuropsychiatry. 2001;6(2):82–101.
Whiteside SP, Port JD, Abramowitz JS. A meta-analysis of functional neuroimaging in obsessive-compulsive disorder. Psychiatry Res. 2004;132(1):69–79.
Nordahl TE, Benkelfat C, Semple WE, Gross M, King AC, Cohen RM. Cerebral glucose metabolic rates in obsessive compulsive disorder. Neuropsychopharmacology. 1989;2:23–8.
Benkelfat C, Nordahl TE, Semple WE, King AC, Murphy DL, Cohen RM. Local cerebral glucose metabolic rates in obsessive-compulsive disorder. Patients treated with clomipramine. Arch Gen Psychiatry. 1990;47:840–8.
Perani D, Colombo C, Bressi S, Bonfanti A, Grassi F, Scarone S, et al. [18F] FDG PET study in obsessive-compulsive disorder A clinical/metabolic correlation study after treatment. Br J Psychiatry. 1995;166:244–50.
Hoehn-Saric R, Schlaepfer TE, Greenberg BD, McLeod DR, Pearlson GD, Wong SH. Cerebral blood flow in obsessive-compulsive patients with major depression: effect of treatment with sertraline or desipramine on treatment responders and non-responders. Psychiatry Res. 2001;108:89–100.
Hansen ES, Hasselbalch S, Law I, Bolwig TG. The caudate nucleus in obsessive-compulsive disorder. Reduced metabolism following treatment with paroxetine: a PET study. Int J Neuropsychopharmacol. 2002;5:1–10.
Baxter LR Jr, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC, et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry. 1992;49:681–9.
Brody AL, Saxena S, Schwartz JM. FDG-PET predictors of response to behaviour therapy and pharmacotherapy in obsessive compulsive disorder. Psychiatry Res. 1998;84:1–6.
Kang DH, Kwon JS, Kim JJ, Youn T, Park HJ, Kim MS, et al. Brain glucose metabolic changes associated with neuropsychological improvements after 4 months of treatment in patients with obsessive-compulsive disorder. Acta Psychiatr Scand. 2003;107:291–7.
Arnsten Amy FT. Catecholamine influences on dorsolateral prefrontal cortical networks. Biol Psychiatry. 2011;69(12):89–99.
Apostolova I, Block S, Buchert R, Osen B, Conradi M, Tabrizian S, et al. Effects of behavioral therapy or pharmacotherapy on brain glucose metabolism in subjects with obsessive-compulsive disorder as assessed by brain FDG PET. Psychiatry Res. 2010;184:105–16.
Ho Pian KL, van Megen HJ, Ramsey NF, Mandl R, van Rijk PP, Wynne HJ, et al. Decreased thalamic blood flow in obsessive-compulsive disorder patients responding to fluvoxamine. Psychiatry Res. 2005;138:89–97.
Yücel M, Wood SJ, Wellard RM, Harrison BJ, Fornito A, Pujol J, et al. Anterior cingulate glutamate-glutamine levels predict symptom severity in women with obsessive-compulsive disorder. Aust N Z J Psychiatry. 2008;42:467–77.
Brennan BP, Rauch SL, Jensen JE, Pope HG Jr. A critical review of magnetic resonance spectroscopy studies of obsessive-compulsive disorder. Biol Psychiatry. 2013;73(1):24–31.
Adler CM, McDonough-Ryan P, Sax KW, Holland SK, Arndt S, Strakowski SM. fMRI of neuronal activation with symptom provocation in unmedicated patients with obsessive compulsive disorder. J Psychiatr Res. 2000;34:317–24.
Nakao T, Nakagawa A, Yoshiura T, Nakatani E, Nabeyama M, Yoshizato C, et al. Brain activation of patients with obsessive-compulsive disorder during neuropsychological and symptom provocation tasks before and after symptom improvement: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57:901–10.
Kang DH, Jang JH, Han JY, Kim JH, Jung WH, Choi JS, et al. Neural correlates of altered response inhibition and dysfunctional connectivity at rest in obsessive-compulsive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2013;40:340–6.
Tian L, Meng C, Jiang Y, Tang Q, Wang S, Xie X, et al. Abnormal functional connectivity of brain network hubs associated with symptom severity in treatment-naive patients with obsessive compulsive disorder: a resting-state functional MRI study. Prog Neuropsychopharmacol Biol Psychiatry. 2016;66:104–11.
Bernstein GA, Mueller BA, Schreiner MW, Campbell SM, Regan EK, Nelson PM, et al. Abnormal striatal resting-state functional connectivity in adolescents with obsessive-compulsive disorder. Psychiatry Res. 2016;247:49–56.
Nakatani E, Nakgawa A, Ohara Y, Goto S, Uozumi N, Iwakiri M, et al. Effects of behavior therapy on regional cerebral blood flow in obsessive-compulsive disorder. Psychiatry Res. 2003;124:113–20.
Freyer T, Klöppel S, Tüscher O, Kordon A, Zurowski B, Kuelz AK, et al. Frontostriatal activation in patients with obsessive-compulsive disorder before and after cognitive behavioral therapy. Psychol Med. 2011;41:207–16.
Rauch SL, Savage CR. Neuroimaging and neuropsychology of the striatum. Bridging basic science and clinical practice. Psychiatr Clin North Am. 1997;20:741–68.
Fineberg NA, Sivakumaran T, Roberts A, Gale T. Adding quetiapine to SRI in treatment-resistant obsessive-compulsive disorder: a randomized controlled treatment study. Int Clin Psychopharmacol. 2005;20(4):223–6.
Fineberg NA, Gale TM, Sivakumaran T. A review of antipsychotics in the treatment of obsessive compulsive disorder. J Psychopharmacol. 2006;20(1):97–103.
Gillan CM, Fineberg NA, Robbins TW. A trans-diagnostic perspective on obsessive-compulsive disorder. Psychol Med. 2017;47(9):1528–48.
Gillan CM, Papmeyer M, Morein-Zamir S, Sahakian BJ, Fineberg NA, Robbins TW, et al. Disruption in the balance between goal-directed behavior and habit learning in obsessive-compulsive disorder. Am J Psychiatry. 2011;168:718–26.
Voon V, Reiter A, Sebold M, Groman S. Model-based control in dimensional psychiatry. Biol Psychiatry. 2017;82(6):391–400.
Fontenelle LF, Oostermeijer S, Harrison BJ, Pantelis C, Yucel M. Obsessive-compulsive disorder, impulse control disorders and drug addiction: common features and potential treatments. Drugs. 2011;71:827–40.
Sjoerds Z, de Wit S, van den Brink W, Robbins TW, Beekman AT, Penninx BW, Veltman DJ. Behavioral and neuroimaging evidence for overreliance on habit learning in alcohol-dependent patients. Transl Psychiatry. 2013;3(12):e33.
Voon V, Derbyshire K, Rück C, Irvine MA, Worbe Y, Enander J, Schreiber LR, Gillan C, Fineberg NA, Sahakian BJ, Robbins TW, Harrison NA, Wood J, Daw ND, Dayan P, Grant JE, Bullmore ET. Disorders of compulsivity: a common bias towards learning habits. Mol Psychiatry. 2015;20(3):345–52.
Pancheri P, et al. Validazione della scala per la valutazione rapida dimensionale “SVARAD”. Riv Psichiatr. 1999;34:84–93.
Bellodi L. Diagnosi differenziale e casi clinici. In: Smeraldi E, editor. Il disturbo Ossessivo-Compulsivo e il suo spettro, vol. 2003. Milano: Masson; 2003. p. 303–26.
Berman I, Merson A, Viegner B, Losonczy MF, Pappas D, Green AI. Obsessions and compulsions as a distinct cluster of symptoms in schizophrenia: a neuropsychological study. J Nerv Ment Dis. 1998;186:150–6.
Bland RC, Newman SC, Orn H. Schizophrenia: lifetime comorbidity in a community sample. Acta Psychiatr Scand. 1987;75:383–91.
de Haan L, Dudek-Hodge C, Verhoeven Y, Denys D. Prevalence of psychotic disorders in patients with obsessive-compulsive disorder. CNS Spectr. 2009;14(8):415–7.
Porto L, Bermanzohn PC, Pollack S, Morrissey R, Siris SG. A profile of obsessive-compulsive symptoms in schizophrenia. CNS Spectr. 1997;2:21–5.
Bottas A, Cooke RG, Richter MA. Comorbidity and pathophysiology of obsessive-compulsive disorder in schizophrenia: is there evidence for a schizo-obsessive subtype of schizophrenia? J Psychiatry Neurosci. 2005;30(3):187–93.
Poyurovsky M, Koran LM. Obsessive-compulsive disorder (OCD) with schizotypy vs. schizophrenia with OCD: diagnostic dilemmas and therapeutic implications. J Psychiatr Res. 2005;39:399–408.
Rosen I. The clinical significance of obsessions in schizophrenia. J Ment Sci. 1957;103:773–85.
Hwang MY, Morgan JE, Losconzcy MF. Clinical and neuropsychological profiles of obsessive–compulsive schizophrenia: a pilot study. J Neuropsychiatry Clin Neurosci. 2000;12:91–4.
Niendam TA, Berzaka J, Cannon TD, Bearden CE. Obsessive compulsive symptoms in the psychosis prodrome: correlates of clinical and functional outcome. Schizophr Res. 2009;108(1–3):170–5.
Öngür D, Goff DC. Obsessive-compulsive symptoms in schizophrenia: associated clinical features, cognitive function and medication status. Schizophr Res. 2005;75:349–62.
Lim M, Park DY, Kwon JS, Joo YH, Hong KS. Prevalence and clinical characteristics of obsessive-compulsive symptoms associated with atypical antipsychotics. J Clin Psychopharmacol. 2007;27(6):712–3.
Tiihonen J, Lonnqvist J, Wahlbeck K, Klaukka T, Niskanen L, Tanskanen A, Haukka J. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009;374(9690):620–7.
Englisch S, Esslinger C, Inta D, et al. Clozapine-induced obsessive-compulsive syndromes improve in combination with aripiprazole. Clin Neuropharmacol. 2009;32:4,227–9.
Kim SW, Shin IS, Kim JM, Yang SJ, Hwang MY, Yoon JS. Amisulpride improves obsessive-compulsive symptoms in schizophrenia patients taking atypical antipsychotics: an open-label switch study. J Clin Psychopharmacol. 2008;28(3):349–52.
Tundo A, Necci R. Cognitive-behavioural therapy for obsessive-compulsive disorder co-occurring with psychosis systematic review of evidence. World J Psychiatry. 2016;6(4):449–55.
Adam Y, Meinlschmidt G, Gloster AT, Lieb R. Obsessive-compulsive disorder in the community: 12-month prevalence, comorbidity and impairment. Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):339–49.
Leone JE, Sedory EJ, Gray KA. Recognition and treatment of muscle dysmorphia and related body image disorders. J Athl Train. 2005;40(4):352–9.
Davidson J. Diabulimia: how eating disorders can affect adolescents with diabetes. Nurs Stand. 2014;29(2):44–9.
Roosen KM, Mills JS. Exploring the motives and mental health correlates of intentional food restriction prior to alcohol use in university students. J Health Psychol. 2015;20(6):875–86.
Mathieu J. What is pregorexia? J Am Diet Assoc. 2009;109(6):976–9.
Mathieu J. What is orthorexia? J Am Diet Assoc. 2005;105(10):1510–2.
Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C. Orthorexia nervosa: a preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat Weight Disord. 2004;9(2):151–7.
Dunn TM, Bratman S. On orthorexia nervosa: a review of the literature and proposed diagnostic criteria. Eat Behav. 2015;21:11–7.
Halmi KA, Tozzi F, Thornton LM, et al. The relation among perfectionism, obsessive-compulsive personality disorder and obsessive-compulsive disorder in individuals with eating disorders. Int J Eat Disord. 2005;38(4):371–4.
Dell'Osso L, Abelli M, Carpita B, Pini S, Castellini G, Carmassi C, Ricca V. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr Dis Treat. 2016;12:1651–60.
McKay D, Sookman D, Neziroglu F, Wilhelm S, Stein DJ, Kyrios M, Matthews K, Veale D. Accreditation task force of the Canadian Institute for Obsessive Compulsive Disorders. Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Res. 2015;227(1):104–13.
Fullana MA, Zhu X, Alonso P, Cardoner N, Real E, López-Solà C, Segalàs C, Subirà M, Galfalvy H, Menchón JM, Simpson HB, Marsh R, Soriano-Mas C. Basolateral amygdala-ventromedial prefrontal cortex connectivity predicts cognitive behavioural therapy outcome in adults with obsessive-compulsive disorder. J Psychiatry Neurosci. 2017;42(5):160215.
Külz A, Barton B, Voderholzer U. Third wave therapies of cognitive behavioral therapy for obsessive compulsive disorder: a reasonable add-on therapy for CBT? State of the art. Psychother Psychosom Med Psychol. 2016;66(3–4):106–11.
Downar J, Geraci J, Salomons TV, Dunlop K, Wheeler S, McAndrews MP, et al. Anhedonia and reward-circuit connectivity distinguish nonresponders from responders to dorsomedial prefrontal repetitive transcranial magnetic stimulation in major depression. Biol Psychiatry. 2014;76:176–85.
Dunlop K, Woodside B, Olmsted M, Colton P, Giacobbe P, Downar J. Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive-compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology. 2016;41:1395–403.
Denys D, Mantione M, Figee M, van den Munckhof P, Koerselman F, Westenberg H, et al. Deep brain stimulation of the nucleus accumbens for treatment-refractory obsessive-compulsive disorder. Arch Gen Psychiatry. 2010;67:1061–8.
Aouizerate B, Cuny E, Martin-Guehl C, Guehl D, Amieva H, Benazzouz A, et al. Deep brain stimulation of the ventral caudate nucleus in the treatment of obsessive—compulsive disorder and major depression. J Neurosurg. 2004;101:682–6.
Ruffini C, Locatelli M, Lucca A, Benedetti F, Insacco C, Smeraldi E. Augmentation effect of repetitive transcranial magnetic stimulation over the orbitofrontal cortex in drug-resistant obsessive-compulsive disorder patients: a controlled investigation. Prim Care Companion J Clin Psychiatry. 2009;11:226–30.
Nauczyciel C, Le Jeune F, Naudet F, Douabin S, Esquevin A, Vérin M, et al. Repetitive transcranial magnetic stimulation over the orbitofrontal cortex for obsessive-compulsive disorder: a double-blind, crossover study. Transl Psychiatry. 2014;4:e436.
Mondino M, Haesebaert F, Poulet E, Saoud M, Brunelin J. Efficacy of cathodal transcranial direct current stimulation over the left orbitofrontal cortex in a patient with treatment-resistant obsessive-compulsive disorder. J ECT. 2015;31:271–2.
Bation R, Poulet E, Haesebaert F, Saoud M, Brunelin J. Transcranial direct current stimulation in treatment-resistant obsessive compulsive disorder: an open-label pilot study. Prog Neuro-Psychopharmacol Biol Psychiatry. 2016;65:153–7.
Fettes P, Schulze L, Downar J. Cortico-striatal-thalamic loop circuits of the orbitofrontal cortex: promising therapeutic targets in psychiatric illness. Front Syst Neurosci. 2017;11:25.
Cunill R, Castells X, Simeon D. Relationships between obsessive-compulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry. 2009;70(1):70–82.
Fineberg NA, Saxena S, Zohar J, Craig KJ. Obsessive-compulsive disorder. In: Hollander E, Zohar J, Sirovatka PJ, Regier DA, editors. Obsessive-compulsive spectrum disorders. Arlington: American Psychiatric Publishing; 2011. p. 9–10.
Bahnson CB, Kissen DM. Psychophysiological aspects of cancer. Ann N Y Acad Sci. 1966;125:775–1055.
Bellodi L, Erzegovesi S. Disturbi dell’alimentazione. In: Smeraldi E, editor. Il disturbo Ossessivo-Compulsivo e il suo spettro. Milano: Masson; 2003. p. 489–544.
Hirschtritt ME, Bloch MH, Mathews CA. Obsessive-compulsive disorder: advances in diagnosis and treatment. JAMA. 2017;317(13):1358–67.
Piacentino D, Pasquini M, Tarsitani L, Berardelli I, Roselli V, Maraone A, Biondi M. The Association of Anger with symptom subtypes in severe obsessive-compulsive disorder outpatients. Psychopathology. 2016;49(1):40–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Taddei, I., Valentini, M., Pasquini, M. (2018). The Obsessive-Compulsive Dimension. In: Biondi, M., Pasquini, M., Picardi, A. (eds) Dimensional Psychopathology. Springer, Cham. https://doi.org/10.1007/978-3-319-78202-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-78202-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-78201-0
Online ISBN: 978-3-319-78202-7
eBook Packages: MedicineMedicine (R0)