Abstract
The suprachiasmatic nucleus (SCN) is the master clock of the mammalian brain. Lesions in the human SCN region due to suprasellar pituitary tumors or metastasis result in a decreased expression of a major SCN peptide, arginine vasopressin (AVP), and in disturbed circadian rhythms. In Nissl-stained paraffin sections, the human SCN cannot be recognized without immunocytochemistry for AVP, vasoactive intestinal polypeptide (VIP), or neurotensin. Gamma-aminobutyric acid is co-localized with one or more peptides in SCN neurons. Compared to monkeys and other animals, the human SCN has very large populations of neurotensin cells and of neuropeptide Y neurons, which obscure a geniculo-hypothalamic tract containing the same peptide. In postmortem human SCN, distinct day–night and seasonal fluctuations were found for the AVP- and VIP-expressing neurons in subjects up to 50 years of age. Moreover, structural and functional differences in SCN are attributed to gender, sexual orientation, and sex differences in aging. The SCN drives circadian and circannual rhythms in the pineal gland production of melatonin that affects many brain functions mediated by the melatonin receptors (MT1 and MT2). Like the SCN, the pineal system also shows strong changes with aging. The retino-hypothalamic tract (RHT) directly innervates the VIP and neurotensin neurons in the SCN and mediates the entraining effects of light on the SCN. The RHT is made up of retinal ganglion cells, which contain pituitary adenylate cyclase-activating polypeptide (PACAP) and co-store glutamate. Light activates these cells via the photopigment melanopsin in the PACAP cells. In addition, serotonin and histamine innervate the SCN, while melatonin acting on the SCN is mediated by MT receptors. Immunocytochemical observations show that AVP and VIP fibers innervate the SCN itself, including the contralateral SCN and a number of other hypothalamic areas, including the sub-paraventricular zone and the dorsomedial nucleus. These observations match very well with the results of postmortem tracing following an injection into the human SCN. The strong projection from the SCN to the supraoptic nucleus seen in rodents was not found in human.
The SCN of Alzheimer (AD) patients—who tend to suffer from circadian rhythm disturbances—exhibits a dramatic loss of AVP-, neurotensin-, and MT1-expressing neurons. AVP-mRNA levels decrease in the SCN as early as the preclinical stages (Braak stages I–II), while day–night fluctuations in pineal melatonin production are already disrupted in the preclinical AD stages (Braak II–III). A combination of light and melatonin treatment was found to increase sleep efficiency and improve nocturnal restlessness, mood, performance, daytime energy, and quality of life.
In Huntington’s disease patients, the SCN contains 85 % less VIP-expressing neurons and 33 % less AVP-expressing neurons. However, the total amount of VIP- or AVP-mRNA was unchanged. In depression an increased number of AVP-expressing neurons were observed, together with a decreased amount and a diminished circadian fluctuation of AVP-mRNA in the SCN. The number of MT1 was also increased in the SCN in depression, while the number of MT2-expressing cells did not change. In primary hypertension the number of AVP-, VIP-, and neurotensin-containing neurons was reduced by more than 50 %. The amount of AVP-mRNA expression in the SCN in glucocorticoid-exposed patients was found to be two times lower. In addition, there was a 53 % decrease in the total number of profiles in the SCN that expressed AVP-mRNA.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Suprachiasmatic nucleus
- Biology rhythms
- Aging
- Sexual differentiation
- Depression
- Alzheimer’s disease
- Huntington’s disease
- Hypertension
- Glucocorticoids
4.1 Human Suprachiasmatic Nucleus in Health
The suprachiasmatic nucleus (SCN) , a structure of only 0.25 mm3, is located in the hypothalamus, on both sides of the midline on top of the optic nerve, and borders the third ventricle (for microscopic anatomy , see Fig. 4.1). The SCN is the master clock of the mammalian brain and coordinates all hormonal and behavioral circadian and circannual rhythms (Swaab 2003). Lesions in the SCN region, e.g., as a result of suprasellar pituitary tumors or metastasis (Fig. 4.2), were found to result in a decreased expression of one of the major SCN peptides, arginine vasopressin (AVP), and in disturbed circadian rhythms (Swaab 2003; Borgers et al. 2011, 2013).
Schematic representation of the nuclei of the human hypothalamus . Ox optic chiasm, NBM nucleus basalis of Meynert, hDBB horizontal limb of the diagonal band of Broca, SDN sexually dimorphic nucleus of the preoptic area, SCN suprachiasmatic nucleus, BST bed nucleus of the stria terminalis (c centralis, m medialis, l lateralis, p posterior), PVN paraventricular nucleus, SON supraoptic nucleus, DPe periventricular nucleus dorsal zone, VPe periventricular nucleus ventral zone, fx fornix, 3V third ventricle, ac anterior commissure [From Swaab (2003); Fig. 4.0, with permission]
Metastasis affecting function of the suprachiasmatic nucleus. Scully et al. (1983) and Schwartz et al. (1986) have described a 55-year-old postmenopausal female patient with a discrete metastasis of an adenocarcinoma of the rectum in the ventral hypothalamus, optic chiasm, and neurohypophysis (a, thionine staining) who, while she was admitted to hospital for the final time, developed an abnormal daily rhythm of oral temperature. She had hypothalamic diabetes insipidus, low FSH, blurring of vision in the periphery of the right temporal field, and required more sleep at night. The metastasis was located between the infundibulum, carotid artery, and optic nerve. The infundibulum was pushed into the hypothalamus. The mass also infiltrated downward along the pituitary stalk. The white granular mass extended into the supraoptic recess. The fornices were pushed laterally by the tumor. We determined 1964 vasopressin-expressing neurons in the SCN, which was only 23 % of the control values for the group of 50- to 80-year-old women (8370 ± 950 vasopressin neurons, n = 8). This observation supports the importance of the activity of vasopressin neurons for the expression of circadian rhythms in the human (Bar = 1 mm) [From Swaab (2003); Fig. 4.2, with permission]
4.1.1 Chemoarchitecture
The human SCN cannot be recognized with certainty in the conventional 6–10 μm Nissl-stained paraffin sections (Mai et al. 1991), and immunocytochemical labeling of this structure (i.e., with anti-AVP, anti-vasoactive intestinal polypeptide (VIP) or anti-neurotensin) is thus necessary (for references, see Swaab (2003); Fig. 4.3). By means of immunocytochemistry Mai et al. distinguished five major subdivisions in the human SCN (Mai et al. 1991). The region of the SCN that receives retinohypothalamic tract (RHT) input—and is therefore considered to be important for entrainment—is characterized by VIP neurons (Moore 1992). AVP is found in the remainder of the SCN and neurotensin is found throughout the entire SCN (Moore 1992). In addition, somatostatin, thyrotropin-releasing hormone, galanin preproenkephalin, delta-sleep-inducing peptide, leptin receptor, and hypocretin fibers are present in the SCN (Couce et al. 1997; Swaab 2003; Garcia-Falgueras et al. 2011). Furthermore, VIP binding sites, estrogen receptor (ER) α and β, the progesterone receptor (Kruijver and Swaab 2002) (Fig. 4.4), and melatonin receptors (MT) (Wu et al. 2013) were found in the human SCN . Because VIP is present in the SCN, it is not surprising that peptide methionine amide (a peptide with histidine and methionine, PHM) is also present in the human SCN. PHM and VIP are encoded on two adjacent exons of a common prepro-VIP gene. Using confocal laser scanning microscopy , Romijn et al. (1999) found that a small percentage of the neurons in the human SCN co-localized with AVP and VIP.
Diagram showing the organization of the human SCN . The distribution of vasopressin (VP), vasoactive intestinal polypeptide (VIP), neuropeptide-Y (NPY), neurotensin (NT), neurons (large black dots), fibers (small gray points) is shown at three levels, from rostral to caudal [From Moore (1992); Fig. 6, with permission]
(a) Estrogen receptor (ER) α, (b) ERβ, and (c) progesterone receptor (PR) immunoreactivity in SCN neurons . The asterisk points to nuclear ERβ immunoreactivity in smooth muscles and endothelial cells of a small blood vessel. Note the positive and negative nuclear ERα, ERβ, and PR staining in adjacent SCN neurons, as indicated by the arrows in (a), (b), and (c). Scale bar represents 8 mm [From Kruijver and Swaab (2002); Fig. 3, with permission]
Following antigen retrieval by microwave treatment of sections, the staining of AVP and VIP becomes more sensitive. Due to this treatment, the volume of the AVP-SCN subnucleus increased 2.4 times and that of the VIP-SCN subnucleus by 4 times; the number of AVP-stained neurons increased by 70 % and the number of VIP-stained neurons increased by 280 %. The neurons that were visible without microwave treatment were localized mainly in the central part of the SCN, whereas the neurons that became visible only after microwave treatment were localized in the peripheral area of the SCN. This suggests that the AVP and VIP neurons in the central part of the SCN contain more peptide, possibly because they are more active than the peripheral ones (Zhou et al. 1996). Could this be a general characteristic of hypothalamic nuclei?
Many neurons in the human SCN contain the two isoforms of glutamic acid decarboxylase (GAD) , GAD65 and GAD67. Gamma-aminobutyric acid (GABA) is co-localized with one or more peptides in SCN neurons (Swaab 2003). GABA is generally known as an inhibitory neurotransmitter in the brain, but its action may depend on the circadian time. SCN neurons can be excited by GABA through a GABAA-dependent mechanism. An intermediate density of benzodiazepine binding sites is already present in the SCN of the human fetus and neonate . A dense catecholaminergic network is found in the SCN of the human fetus from as early as the third and fourth months of pregnancy (Swaab 2003).
4.1.2 Day/Night Rhythm
Much of the variability observed in the human SCN is related to its function as the biological clock. In postmortem tissue of a group of young subjects (6–47 years of age), a distinct day–night fluctuation with an asymmetrical, bimodal waveform was found for the AVP- and VIP-expressing neurons in the human SCN (Fig. 4.5) (Hofman and Swaab 1993; Hofman 2000, 2003). The AVP cycle has a peak in the early morning, a lower plateau during the day, a second peak in the late afternoon, and a decline beginning in the early evening, leading to a nadir around midnight. The VIP cycle shows a peak in the middle of the night, a lower plateau beginning in the late night and lasting for about 12 h, and a second peak in the late afternoon, followed by a sharp decline in the early evening (Hofman 2003). Time series analysis showed that the circadian cycles in the human SCN can be adequately described by a model consisting of nonlinear periodic functions, which could be decomposed into monophasic and diphasic cycles, with periods of 24 and 12 h, respectively (Hofman 2003). The demonstration of these two significantly different, but temporally linked, output profiles suggests that the SCN contains more than one oscillator. Circadian rhythms are also present in the human retina (Tuunainen et al. 2001), which may be the consequence of circadian rhythms in the SCN, or it could be based upon intrinsic circadian oscillations, and, through the RHT, influence the rhythms in the SCN.
Circadian rhythm in the number of vasopressin-containing neurons in the human suprachiasmatic nucleus (SCN) of (a) young subjects (<50 years of age) and (b) elderly subjects (>50 years of age). The black bars indicate the night period (22:00–06:00 h). The general trend in the data is enhanced by using a smoothed double-plotted curve and is represented by mean ± S.E.M. values. Note the circadian rhythm in the SCN of young people with low values during the night period and peak values during the early morning [From Hofman and Swaab (1994); Fig. 1, with permission]
Interestingly, since the biological clock stops at the time of death, it is possible to read the time of death in forensic tissues by measuring gene expression levels of various clock genes and their ratios (Kimura et al. 2011).
4.1.3 Seasonal Rhythm
Strong seasonal fluctuations were also observed in postmortem human SCN tissue. The number of AVP- and VIP-containing neurons in the SCN was found to change in the course of a year, with August–September values being two times higher than April–May values (Fig. 4.6) (Hofman and Swaab 1992b; Hofman 2004). Photoperiod seems to be the major Zeitgeber (German for “time-giver” or pacemaker) for the observed annual variations in the SCN (Hofman and Swaab 1993).
Annual rhythm in the number of vasopressin-containing neurons in the human suprachiasmatic nucleus (SCN) of (a) young subjects (<50 years of age) and (b) elderly subjects (>50 years of age). The general trend in the data is enhanced by using a smoothed, double-plotted curve and is represented by mean ± S.E.M. Note the circannual rhythm in the SCN of young people with low values during the summer and peak values in the autumn period [From Hofman and Swaab (1995); Fig. 1, with permission]
The hypothalamic levels of serotonin and dopamine, neurotransmitters known to innervate the SCN, show diurnal rhythms and seasonal rhythms as well (Carlsson et al. 1980). In addition, reduced thalamus/hypothalamus serotonin transporter availability was observed in living patients by single-photon emission computed tomography in winter compared with summer, at least for female subjects (Neumeister et al. 2000). It remains to be determined exactly how these seasonal fluctuations causally relate to the SCN circannual rhythms. However, the fact that both serotonin and dopamine circadian and seasonal rhythms are observed in the hypothalamus suggests that the SCN drives the monoaminergic systems instead of the other way around. Furthermore, a notable seasonal variation in the volume of the hypothalamic paraventricular nucleus (PVN) was observed in postmortem human brain material. The PVN volume reached its peak during the spring (Hofman and Swaab 1992a).
4.1.4 Pineal Gland
An important component in the circadian and circannual timing system is the pineal gland. Melatonin production varies with age, time of the day, and season. The nocturnal excretion of the major melatonin metabolite, 6-sulfatoxymelatonin, was three times higher in healthy full-term infants of 8 weeks of age, born in summer, than that of those born in winter. When exposed to long nights, the duration of melatonin and prolactin secretion and the rise in cortisol are longer than the duration of secretion found during short nights. The seasonal variations were no longer present at 16 weeks of postnatal age, suggesting a prenatal influence of the photoperiod on the ontogeny of melatonin (Sivan et al. 2001). There is a relationship between diurnal and seasonal pineal rhythms . The diurnal rhythms in pineal melatonin content of autopsy material are evident only in the long photoperiod (i.e., April–September), with melatonin concentrations being four times higher at night (22.00–10.00 h) than during the day (10.00–22.00 h) (Hofman et al. 1995). This seasonal effect was confirmed by Luboshitzky et al. (1998). In contrast, diurnal variations in the pineal 5-methoxytryptophol contents are only observed in the short photoperiod (i.e., October–March) with high concentrations during the day and low concentrations at night (Hofman et al. 1995). This shows that the synthesis of indolamines in the human pineal exhibits a diurnal rhythm that is affected by seasonal changes in day length (Hofman et al. 1995). Seasonal rhythms are also found in gonadotropin receptors in the pineal gland, with higher values in the winter than in the summer (Luboshitzky et al. 1997).
Melatonin is implicated in numerous physiological processes, including circadian rhythms, stress, and reproduction, many of which are mediated by the MTs. Immunocytochemistry was used to study the distribution of the MT1 in the postmortem human hypothalamus and pituitary. In addition to its localization in the SCN, a number of novel sites, including the PVN, periventricular nucleus, supraoptic nucleus (SON), sexually dimorphic nucleus, the diagonal band of Broca, the nucleus basalis of Meynert, infundibular nucleus, ventromedial and dorsomedial nucleus, tuberomamillary nucleus, mamillary body, and paraventricular thalamic nucleus, were observed to have neuronal MT1 receptor expression. Moreover, the MT1 receptor was co-localized with some AVP neurons in the SCN, co-localized with some parvocellular and magnocellular AVP and oxytocin neurons in the PVN and SON, and co-localized with some parvocellular corticotropin-releasing hormone (CRH) neurons in the PVN. In the pituitary, strong MT1 expression was observed in the pars tuberalis, while a weak staining was found in the posterior and anterior pituitary. The co-localization of MT1 and CRH suggests that melatonin might directly modulate the hypothalamic–pituitary–adrenal (HPA) axis in the PVN, which may have implications for stress conditions such as depression (Wu et al. 2006b, 2013).
4.1.5 Sexual Differentiation in the SCN
Structural and functional sex differences are present in the SCN [for a review, see Bailey and Silver (2013)]. Staining with anti-AVP showed that the shape of the human SCN is sexually dimorphic, i.e., more elongated in women and more spherical in men, but the AVP cell number and the volume of the SCN-AVP subnucleus are similar in both sexes (Swaab et al. 1985). These gender differences and the presence of sex hormone receptors (ER and PR; see Fig. 4.4) (Kruijver and Swaab 2002) in the SCN indicated the possible involvement of this nucleus in sexual behavior and reproduction (Swaab 2003; Bailey and Silver 2013). In addition, sex differences are present in sleep, i.e., a shorter average intrinsic circadian period was observed in women, which may have implications for understanding the sex differences in habitual sleep duration and insomnia prevalence (Duffy et al. 2011).
Moreover, SCN structure has a link with sexual orientation. Morphometric analysis of the human hypothalamus revealed that the volume of the SCN in homosexual men is 1.7 times larger as that of a reference group of male subjects and contains 2.1 times as many cells, while another hypothalamic nucleus, located in the immediate vicinity of the SCN, the sexually dimorphic nucleus (SDN), showed no such differences in either volume or cell number (Fig. 4.7) (Swaab and Hofman 1990). The SDN data indicate the selectivity of the enlarged SCN in homosexual men, but do not support the hypothesis that homosexual men simply have a “female hypothalamus” (Swaab and Hofman 1990, 1995).
(a) Volume of the human suprachiasmatic nucleus (SCN) and sexually dimorphic nucleus of the preoptic area (SDN) as measured in three groups of adult subjects : (1) a male reference group (n = 18); (2) male homosexuals who died of AIDS (n = 10); (3) heterosexuals who died of AIDS (n = 6; 4 males and 2 females). The values indicate medians and the standard deviation of the median. The differences in the volume of the SCN between homosexuals and the subjects from both other groups are statistically significant (Kruskal–Wallis multiple comparison test, *p < 0.05; **p < 0.01; ***p < 0.001). Note that none of the parameters measured in the SDN (A, B) showed significant differences among the three groups (p always > 0.4). (b) Total number of cells in the human SCN and SDN. The SCN in homosexual men contains 2.1 times as many cells as the SCN in the reference group of male subjects and 2.4 times as many cells as the SCN in heterosexual AIDS patients. (c) The number of vasopressin neurons in the human SCN (the SDN does not contain vasopressin-producing cells). The SCN in homosexual men contains, on average, 1.9 times as many vasopressin neurons as the SCN in heterosexual AIDS patients. Note that the SCN of heterosexual individuals who died of AIDS contains fewer vasopressin cells than the SCN of the subjects from the reference group [From Swaab and Hofman (1990); Fig. 2, with permission]
In humans, during normal aging , the number of peptidergic neurons in the SCN deteriorates in a sexually dimorphic way. The number of VIP-expressing neurons in the SCN of women does not change during aging, whereas in men a complex pattern of changes is observed. Between 10 and 40 years of age, the male SCN contains twice as many VIP neurons as the female SCN, but a subsequent decrease in the number of male VIP neurons between 40 and 65 years of age results in fewer VIP neurons in men than in women. After 65 years of age, the sex difference remained just short of significance (Fig. 4.8) (Zhou et al. 1995).
Lifespan changes in the number of vasoactive intestinal polypeptide (VIP)-immunoreactive neurons of the human SCN in control subjects. The blank bar indicates the males and the hatched bar indicates the females. The SCN of young males (10–40 years) contains twice as many neurons as that of young females (**p < 0.02). This sex difference reverses in middle-aged subjects (*p < 0.04). Note that the decrease in the number of VIP cells in males already begins in middle age and there is a significant reduction in the elderly males compared with young males (#p < 0.02) [From Zhou et al. (1995); Fig. 2, with permission]
4.1.6 Aging
With advancing age, the circadian timing system in humans is progressively disturbed as is clearly demonstrated by a reduced amplitude and period length of circadian rhythms and an increased tendency toward internal desynchronization [for reviews, see Van Someren (2000)].
There are indeed signs of neuronal degeneration of the SCN during aging. In the human SCN, the number of AVP-expressing neurons exhibits a marked diurnal oscillation in young (up to 50 years of age), but not in elderly people (over 50 years of age) (Hofman and Swaab 1994). Whereas in young subjects, low AVP-expressing neuron numbers were observed during the night and peak values during the early morning, a disrupted cycle with reduced amplitude was found in the SCN of elderly people. Similar age-related decrements have been reported for the seasonal timing system (see Fig. 4.6) (Hofman and Swaab 1995). As the fluctuating number of AVP-expressing neurons probably reflects the peptidergic activity state of the cells, these findings suggest that the temporal organization of these neuronal rhythms becomes progressively disturbed in senescence. It is of interest to notice that more frequent and prolonged awakenings and shorter sleep periods have already been observed in subjects aged 50–60 (Wu and Swaab 2007), whereas a reduction in SCN volume and number of AVP-expressing neurons is only present from the age of 80 years onward (Fig. 4.9) (Swaab et al. 1985, 1993; Hofman 1997). The observed AVP-expressing neurons loss in the SCN at later ages may, therefore, only be a relatively late correlate of functional changes in the biological clock that appear much earlier.
Number of vasopressin (AVP)-expressing neurons in the SCN. Note the low values in the 81- to 100-year-old group and the very low numbers in the AD patients (DEM) that were 78 ± 5 years of age. The decreased number of cells expressing VP is considered to be an indication of low metabolic activity of the SCN in old people and AD patients and the changes in the SCN in AD are held responsible for sleep disturbances and nightly restlessness [Based upon Swaab et al. (1987) Fig. 1, with permission]. The variability is largely due to circadian and circannual changes (see Figs. 4.5, 4.6, and 4.7)
The pineal hormone melatonin is involved in the regulation of circadian rhythms and feeds back to the central biological clock, the hypothalamic SCN, via MTs. Supplementary melatonin is considered to be a potential treatment for age-related circadian disorders. Alterations of the MT1 receptor in the SCN during aging were investigated by immunocytochemistry in postmortem human brain material; the number and density of AVP- and VIP-expressing neurons in the SCN did not change, but the number and density of MT1-expressing neurons in the SCN were decreased in aged versus young controls (Fig. 4.10) (Wu et al. 2007).
(a) MT1-immunoreactive (MT1-ir) neuron number per central SCN section and (b) MT1-ir neuron density in the central SCN section in young controls, aged controls (Braak stage 0), subjects in early AD stages (Braak stages I–II; preclinical AD), and late stage AD patients (Braak stages V–VI). Note that both MT1-ir neuron density and number are decreased in the old controls and preclinical “AD” subjects and are more dramatically decreased in the late stage clinical AD patients [From Wu et al. (2006b); Fig. 2, with permission]
It has been demonstrated in aged rats (up to 37 months old) that both overt sleep–wake rhythms (Witting et al. 1993) and AVP-expressing neurons in the SCN (Lucassen et al. 1995) can be restored by enhancing the amount of environmental light. A similar degree of plasticity was also observed in the human circadian timing system. Improvement of the sleep–wake rhythm of older people and patients with dementia was demonstrated by application of a variety of potent modulators of the circadian timing system such as bright light, melatonin, and physical activity (Van Someren et al. 2002) (see also below).
4.2 Input SCN
The RHT is the principal pathway mediating the entraining effects of light on the circadian pacemaker, the SCN. Indeed, suprasellar tumors with compression of the optic chiasm leading to permanent visual field defects are associated with reduced AVP but not with reduced VIP immunoreactivity in the SCN, which raises the possibility that selective impairment of the SCN contributes to the sleep–wake disturbances these patients experience (Borgers et al. 2011, 2013).
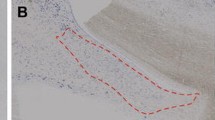
The RHT is made up of retinal ganglion cells, which contain pituitary adenylate cyclase-activating polypeptide (PACAP) and co-store glutamate . Light activates these cells, which directly innervate the SCN via the photopigment melanopsin in the PACAP cells. PACAP interacts with glutamate signaling during the light-induced phase shift. At the same time, the retina itself possesses intrinsic circadian oscillations, exemplified by diurnal fluctuations in visual sensitivity, neurotransmitter levels, and outer segment turnover rates (Hannibal 2006). The human RHT was studied by means of postmortem tracing. Remarkably, up to 6–8 h after the death of the patients, the individual neurons are still capable of actively taking up tracer molecules and transporting them over relatively large distances. The RHT appeared to leave the optic chiasm and enter the hypothalamus both medially and laterally of the SCN. The density of the RHT fibers decreases from rostral to caudal (Fig. 4.11) (Dai et al. 1998b). The RHT terminates predominantly in a zone of the SCN that contains VIP neurons (Moore 1992) but does not only contact VIP but also neurotensin cells in the SCN. In addition, some AVP-expressing neurons are innervated by the RHT in the ventral part of the SCN. Only few projections to the dorsal part of the SCN and the ventral part of the anterior hypothalamus were found (Dai et al. 1998b). Lateral RHT projections reach the ventral part of the ventromedial SON. These fibers may take part in diurnal fluctuations of AVP release. Lateral RHT projections also innervate the area lateral to the SCN. No projections to other hypothalamic areas were observed (Dai et al. 1998b). These data generally confirmed Sadun et al.’s observations with paraphenylenediamine, which stains remnants of degenerated axons in patients with a lesion of the optic nerve (Sadun et al. 1983), and confirmed Friedman et al.’s observations following DiI staining of the RHT in intact human brains (Friedman et al. 1991). Dai et al. (1998b) could, however, not confirm the innervation of the hypothalamic PVN by human RHT that was described by the degeneration technique (Schaechter and Sadun 1985). This technique may, however, have been confounded by lesions that were not restricted to the optic nerve.
Postmortem tracing of the retinohypothalamic tract . Anterior level of the suprachiasmatic nucleus (SCN) showing the injection spot (asterisk, b) in the optic nerve. Many labeled fibers (a) can be seen to course along the wall of the third ventricle (3V) and project to the SCN (arrows). Many fibers (b) also extend to the optic tract (arrows). (a) shows the high magnification of the area in (b) (arrowheads) and shows more clearly labeled fibers in the optic nerve and ventral part of the SCN. The morphology of labeled fibers is clearly visible. Dashed lines in (a) and (b) represent the lateral border of the SCN. Scale bar = 40 mm for (a), 150 mm for (b) [From Dai et al. (1998a, b, c); Fig. 5, with permission]
Compared to monkeys and other animals, the human SCN has a very large population of neurotensin cells and a large population of neuropeptide Y neurons, which obscure a geniculo-hypothalamic tract that contains the same peptide, provided this tract is present in all humans (Moore 1992). In addition, serotonin innervates the SCN, and histamine, the neurotransmitter produced in the tuberomamillary nucleus, is necessary for the circadian rhythmicity of adrenocorticotropic hormone (ACTH) release, food intake, drinking, and the sleep–wakefulness cycle. In fact, histamine can phase-shift circadian rhythms and some authors even consider it to be the final neurotransmitter in the entrainment of the SCN (Eaton et al. 1995; Hannibal 2002).
Another important input to the SCN which influences circadian and circannual functions is melatonin , produced by the pineal gland and acting on the SCN through MT receptors (Wu et al. 2006b, 2013).
Finally, it should be noted that the rest–activity cycle and meals influence rhythmic endocrine changes as well (Swaab 2003). Circadian rhythms in the endocrine system are covered in detail in Chap. 2.
4.3 Output SCN
Many, if not all, brain areas are directly or indirectly functionally affected by the diurnal fluctuations of the nervous output of the SCN and by melatonin fluctuations from the pineal gland. Immunocytochemical observations show that AVP and VIP fibers innervate the SCN itself as well as a number of other hypothalamic areas, including the contralateral SCN, and these observations match very well with postmortem tracing following an injection in the human SCN (Dai et al. 1998a). The densest projections from the human SCN first reach the area between the SCN and the anteroventral part of the hypothalamic PVN, the anteroventral hypothalamic area (Dai et al. 1998a). Immunocytochemical staining showed AVP and VIP fibers in these areas, some of which run anteriorly and enter the anteroventral part of the periventricular nucleus and of the PVN (Fig. 4.12) (Dai et al. 1997). Many SCN fibers continue in the posterior direction and innervate the zone below the PVN, or they reach the ventral PVN (Dai et al. 1998a). The dense network of AVP- and VIP-positive fibers in the sub-PVN zone (Dai et al. 1997) is in agreement with this observation. The SCN fibers in the ventral PVN innervate AVP and corticotropin-releasing hormone (CRH) neurons. This mainly concerns AVP fibers (Dai et al. 1997). The SCN fibers innervating the PVN may directly or indirectly (see below) provide an anatomical basis for the strong influence of the SCN on hormone secretion. Another extensive projection courses posteriorly and passes close to the third ventricle to reach the dorsomedial nucleus (DMN) of the hypothalamus. Most fibers innervating the DMN are concentrated in its ventral part (Dai et al. 1998a) and VIP fibers were more abundant than AVP fibers (Dai et al. 1997). Also in the human brain, the DMN projects to the PVN (Dai et al. 1998c). The SCN thus also influences PVN functions in an indirect way, via the DMN. Injections in the dorsal part of the SCN showed more extensive projections to the PVN than those placed in the ventral part of the SCN. Tracing or immunocytochemistry showed the presence of only a few fibers in the ventromedial nucleus (VMN) (Dai et al. 1997, 1998a).
A series of line drawings arranged from rostral to caudal (a–v) to illustrate schematically the location of vasoactive intestinal polypeptide (VIP) and vasopressin (VP) cell bodies and fibers in a human hypothalamus (case no. 96-010). The dots correspond to the position and density of the cell bodies. Short lines (in j, l, n) illustrate the area through which the fibers of VP magnocellular cell bodies pass. AVH anteroventral hypothalamic area, BST bed nucleus of the stria terminalis, DMH dorsomedial nucleus of the hypothalamus, FO fornix, INF infundibular nucleus, MB mamillary body, NBM nucleus basalis of Meynert, NTL lateral tuberal nucleus, OC optic chiasm, POA preoptic area, PVN paraventricular nucleus, PH posterior hypothalamic nucleus, PEN periventricular nucleus, SCN suprachiasmatic nucleus, SDN sexually dimorphic nucleus of preoptic area (=INAH-1), SON supraoptic nucleus, sub-PVN area below paraventricular nucleus, TMN tuberomamillary nucleus, VMN ventromedial nucleus, VP vasopressin, VIP vasoactive intestinal polypeptide [From Dai et al. (1997); Fig. 2, with permission]
In rodents there is a strong projection from the SCN to the SON with both inhibitory (GABAergic) and excitatory (glutaminergic) components that may also be responsible for the circadian rhythmicity in the SON . Such connections have, however, not been shown in the human brain, although SCN fibers come very close to the SON (Dai et al. 1997) and possibly even contact SON dendrites or interneurons. In addition, the lateral RTH tract projections that innervate the ventral part of the SON (Dai et al. 1998b) may impose a diurnal rhythm on AVP release. Transcriptome-wide analysis of the human brain demonstrated a rhythmic rise and fall of gene expression in regions outside of the SCN, including the dorsolateral prefrontal cortex, the anterior cingulate cortex, the hippocampus, the amygdala, the nucleus accumbens, and the cerebellum. Some 700 transcripts in each region showed 24-h cyclic patterns in controls, and more than 100 transcripts exhibited consistent rhythmicity and phase synchrony across regions. Among the top-ranked “rhythmic” genes were the canonical clock genes BMAL1 (ARNTL), PER1-2-3, NR1D1 (REV-ERBa), DBP, BHLHE40 (DEC1), and BHLHE41 (DEC2) (Li et al. 2013).
The diurnal fluctuations in central functions are not only caused by the neuronal output of the SCN, but also by the action of melatonin on the brain. The pineal gland is innervated by sympathetic noradrenergic fibers. This polysynaptic pathway starts in the SCN and passes the cervical spinal cord. This explains the prevalence of decreased sleep quality in individuals with tetraplegia that is due to a cervical spinal cord lesion between C4 and C7 and the complete absence of the evening increase in melatonin concentration in this group of patients (Verheggen et al. 2012).
4.4 SCN in Neuropsychiatric Diseases
4.4.1 Alzheimer’s Disease
The disruption of circadian rhythms and the increased incidence of disturbed sleep in humans during aging (Van Someren et al. 2002) are accompanied by age-related alterations in the neural organization of the SCN, a decreased photic input to the clock, and a dramatic decrease in peptide synthesis in the SCN of Alzheimer’s Disease (AD) (Liu et al. 2000; Swaab 2004b). In addition, the presence of pretangles (Swaab et al. 1992; van de Nes et al. 1998) and tangles (Stopa et al. 1999) in the SCN of AD patients shows that this structure is affected by the disease process. However, diffuse amyloid plaques are only seldom found in this nucleus (van de Nes et al. 1998; Stopa et al. 1999). Stopa et al. (1999), for example, reported that the SCN of AD patients, who tend to suffer from sleep disruption and other circadian rhythm disturbances, is severely damaged and exhibits a dramatic loss of AVP- and neurotensin-expressing neurons and a corresponding increase in the glial fibrillary acidic protein (GFAP)-stained astrocytes. Harper et al. (2008) have observed, in postmortem material, in relation to antemortem clinical data, that specific loss of SCN neurotensin neurons was associated with loss of activity and temperature amplitude without increase in activity fragmentation. In addition, the loss of SCN AVP-expressing neurons was associated with increased activity fragmentation but not with loss of amplitude. Harper et al.’s data provide information on the role of neuronal subpopulations in subserving the SCN function and the utility of AD.
The immunocytochemical data showing decreased activity of the SCN in AD (Figs. 4.9 and 4.13) have been confirmed by in situ hybridization . The total amount of AVP-mRNA in the SCN of AD patients was three times lower than in age- and gender-matched controls. In addition, the AVP-mRNA-expressing neurons in the SCN showed a marked day–night difference in controls under the age of 80 years. The amount of AVP-mRNA was more than three times higher during the day than at night, whereas no clear diurnal rhythm of AVP-mRNA was observed in AD patients (Fig. 4.14) (Liu et al. 2000). Only in female presenile Alzheimer patients was a significant decrease in the number of VIP-expressing neurons in the SCN found (Zhou et al. 1995). The AVP and VIP data support the idea that damage to the SCN is the underlying anatomical substrate for the clinically often observed disturbances in circadian rhythmicity in AD.
In both presenile (n = 7) and senile (n = 8) Alzheimer patients the volume of the vasopressin subnucleus of the SCN (a) and the number of vasopressin-expressing neurons (b) are significantly decreased when compared to young (n = 14) or old (n = 9) age-matched controls. In presenile Alzheimer patients only 10 % of the number of neurons expressing vasopressin in controls is found. ***p > 0.001; *p > 0.02 (Mann–Whitney-U-test) [From Swaab (2004a); Fig. 29.7, with permission]
Day–night fluctuations in vasopressin (AVP)-mRNA in the suprachiasmatic nucleus (SCN) expressed as masked area of silver grains in controls and in Alzheimer patients (AD). Note that at any moment of the day the values for AD patients are lower than those for controls [From Liu et al. (2000); Fig. 3, with permission]
It was found that the number and density of AVP- or VIP-expressing neurons in the SCN did not change in aged control subjects compared to young control subjects, but the number and density of MT1-expressing neurons in the SCN were decreased. In addition, both MT1-expressing neurons and AVP- or VIP-expressing neurons were strongly diminished in the final neuropathological stages of AD (Braak stages V–VI), but not in the earliest stages (Braak stages I–II), compared to aged control subjects (Braak stage 0) (see Fig. 4.10). These data suggest that the MT1-mediated effects of melatonin on the SCN are disturbed during aging and even more so in late stage AD, which may contribute to the clinical circadian disorders and to the efficacy of therapeutic melatonin administration under these conditions (Wu et al. 2007).
Day–night fluctuations in pineal melatonin production are already disrupted in the preclinical AD stages (Braak stages II–III) (Fig. 4.15) (Wu et al. 2003), which was proposed to be due to a disruption of the SCN functions. The diurnal fluctuation in the pineal gland in the expression of the clock genes hBmal1, hCry1, hPer1 and in the expression of the β-adrenergic receptor is lost in the pineal gland, and AVP-mRNA levels decrease in the SCN of both preclinical (Braak stages I–II) and clinical (Braak stages V–VI) AD subjects, indicating that the activity of the SCN and of the pineal gland is reduced very early on in AD pathogenesis (Wu et al. 2006a).
The day–night difference in pineal melatonin content is present in Braak stage 0 controls, but disappears in Braak stage I–II and is also absent in Braak stage VI [From Wu et al. (2003); Fig. 3, with permission]
In a long-term, double-blind, placebo-controlled, randomized trial performed with 189 residents in the Netherlands, 87 % of whom had dementia , a combined treatment of light and melatonin was found to increase sleep efficiency and to improve nocturnal restlessness (Riemersma-van der Lek et al. 2008). Contrary to treatment with hypnotics, the improvement of sleep following these treatments is without adverse effects and even results in the improvement of mood, performance, daytime energy, and quality of life. All these data support the hypothesis that increased stimulation of the brain can improve or even restore the decreased neuronal activity (Swaab et al. 2002).
Concluding, there is a loss of function in both the SCN and the pineal gland in aging and in the earliest presymptomatic stages of AD, while these alterations in the circadian system become more pronounced in the later stages of AD. The SCN can functionally be stimulated in AD by enhanced environmental light,
4.4.2 Other Neurodegenerative Disorders
Huntington’s disease ( HD) has a number of features that suggest dysfunction of the SCN, such as a disturbed circadian secretion patterns of cortisol and melatonin, the frequent occurrence of sleeping disorders and the presence of huntingtin-positive cytoplasmic inclusion bodies in the SCN of some patients (Aziz et al. 2008). Studies in HD patients yielded the information that the SCN contained 85 % less VIP-expressing neurons and 33 % less AVP-expressing neurons. However, the total amount of VIP- or AVP-mRNA was unchanged. No significant changes were observed in the number of MT-1- or MT-2 receptor-expressing neurons. These findings suggest that the disorders in sleep and other circadian rhythms in HD patients may at least partly arise from SCN dysfunction (van Wamelen et al. 2013a) and that there are post-transcriptional neuropeptide changes in the SCN of HD patients. However, the expression of the prohormone convertases PC1/3 and PC2 expressions were not different between HD and control cases (van Wamelen et al. 2013b).
In the SCN of one of two patients with hippocampal sclerosis, Stopa et al. (1999) found an increased ratio of astrocyte to neuron. In both these patients the density of AVP- and neurotensin-expressing neurons seemed to be below average, although more subjects are required to be able to draw a proper conclusion. In addition, there are indications that the seizures seen in hippocampal sclerosis affect circadian rhythms (Quigg et al. 1999).
Ozawa et al. (1993) described a patient with Shy–Drager syndrome (multisystem atrophy), who exhibited nocturnal polyuria associated with decreased urinary-specific gravity and a reversed circadian rhythm of AVP, suggesting that the SCN was affected. Subsequently, postmortem evidence indeed provided a disorder in the SCN of this disease. The patient had a decreased number of AVP-expressing neurons, together with gliosis, in the SCN. In addition, the AVP-expressing neurons in the SCN of this patient were smaller than those of the control subjects. Moreover, there was an observation that patients with multisystem atrophy have decreased early morning cortisol levels, which indicates a functional alteration of the SCN (Ozawa et al. 2001). Furthermore, a decrease in the nightly plasma AVP levels has been confirmed in a sample of 13 patients with multisystem atrophy (Ozawa et al. 1998), and the physiological nocturnal fall of body core temperature is blunted in multisystem atrophy patients. The lack of a decrease in body temperature in these patients—possibly caused by a defect in the SCN—distinguishes them from Parkinson patients (Pierangeli et al. 2001).
In the SCN of three Pick Disease patients, Stopa et al. (1999) have found a decreased density of AVP- and neurotensin-expressing neurons, which are changes similar to those observed in AD. In a 1-year-old boy with X-linked lissencephaly with abnormal genitalia, who had absent circadian variation in rhythms of sleep and core temperature, the SCN was not identified, in spite of the use of anti-AVP (Miyata et al. 2009).
4.5 Depression
The human SCN not only shows circadian but also circannual variations in neuronal activity (see above, Fig. 4.6), which is supposed to be related to circadian and circannual fluctuations in mood and to sleeping disturbances in depression (van Londen et al. 2001). The symptoms of depression fluctuate over the day, and the stress response, too, is strongly influenced by the time of the day. The activity of the SCN is directly influenced by light and light therapy is found to be affected in depression. Seasonal affective disorder (SAD) is more prevalent in the northern states of the USA than in the southern states (Miller 2005). So there is a close relationship between light, the SCN, and mood. Since polymorphisms in the clock genes and in lithium target GCK3 are associated with dysfunctional circadian rhythm and susceptibility to mood disorders, in particular in SAD and bipolar disorder (BD) (Lamont et al. 2007), the SCN may also play a causal role in depression at least in subgroups of patients.
Zhou et al. found a disorder of SCN function that is characterized by an increased number of AVP-expressing neurons, a decreased amount of AVP-mRNA in this nucleus, and diminished circadian fluctuation of AVP-mRNA in the postmortem brain of depressed patients (Fig. 4.16) (Zhou et al. 2001). Decreased activity of the SCN in depression is presumed to be, at least partly, due to the increased circulating plasma cortisol levels observed in depression patients, since corticosteroids inhibit the mRNA expression of AVP in the SCN (Figs. 4.17 and 4.18) (Liu et al. 2006). In a transcriptome-wide analysis of the human brain it was also found that the day–night fluctuations were much weaker in the brains of major depression disorder patients due to shifted peak timing and potentially disrupted phase relationships between individual circadian genes (Li et al. 2013).
The number of arginine vasopressin-immunoreactive (AVP-IR) neurons (a) and the mask area of silver grains of the AVP-messenger RNA (b) in the suprachiasmatic nucleus (SCN) in control subjects (n = 11) and depressed subjects (n = 11). The error bars indicate the SD. Note the change in the balance between the presence of more AVP and less AVP-messenger RNA in depression. There is probably a disorder of the transport of AVP that leads to accumulation of the peptide, in spite of the decreased production rate [From Zhou et al. (2001); Fig. 2, with permission]
Estimated total amount of AVP-mRNA in the suprachiasmatic nucleus (SCN) (expressed as masked area of silver grains) of the controls and the corticosteroid-exposed subjects (CST). The bars and error lines represent the mean and standard error of the mean (SEM) [From Liu et al. (2006); Fig. 2, with permission]
Day–night fluctuation in the total amount of AVP-mRNA of the SCN in controls and in the glucocorticoid-exposed subjects (CST). Note that at any moment of the day the values for CST are lower than those of controls [From Liu et al. (2006); Fig. 3, with permission]
The number of MT1-immunoreactive (ir) cells and AVP- and/or VIP-ir cells were found to be increased in the central SCN in depression, while the number of MT2-ir cells was not altered (Wu et al. 2013). In addition, the number of MT1-ir cells, but not MT2-ir cells, was negatively correlated with age at onset of depression, while positively correlated with disease duration. MT1 receptors appeared to be specifically increased in the SCN of depressed patients and may increase during the course of the disease. These changes may be involved in circadian disorders and may contribute to the efficacy of MT receptor agonists or melatonin in depression. Moreover, these data suggest that MT receptor agonists for depression should be selectively targeted toward the MT1 receptor (Wu et al. 2013).
A major question is how light therapy may work in depression. Animal data have shown that AVP neurons of the SCN exert an inhibitory influence on CRH neurons in the PVN (Kalsbeek et al. 1992). Depressed patients have a deficient SCN (Zhou et al. 2001), which may subsequently fail to inhibit sufficiently the CRH neurons in the PVN of depressed patients. Such an impaired negative feedback mechanism may lead to a further increase in the activity of the HPA axis in depression. Both the resulting higher CRH and cortisol levels may contribute to the symptoms of depression. Light therapy may activate the SCN, directly inducing an increased synthesis and release of AVP that will inhibit the CRH neurons. However, it should be noted that human beings are diurnal creatures, whose mode of interaction between SCN-AVP neurons and the PVN-CRH neurons might be different from that of the nocturnal rat, especially because of the fact that opposite actions of hypothalamic AVP have recently been observed on the circadian corticosterone rhythm in nocturnal versus diurnal species (Kalsbeek et al. 2008). The exact mechanism of the action of light in depressed patients thus deserves further study.
4.6 Hypertension
In a postmortem study of the SCN of primary hypertension patients who had died due to myocardial infarction or brain hemorrhage, and in comparison with controls who had normal blood pressure, it was found that the immunoreactivity staining for the three major neuronal populations of the SCN, i.e., AVP, VIP, and neurotensin, was reduced by more than 50 % in hypertension compared with controls (Fig. 4.19) (Goncharuk et al. 2001).
Coronal sections of the human hypothalamus stained for vasopressin (VP) (upper images) [area of the suprachiasmatic nuclei (SCN)], or for corticotropin-releasing hormone (CRH) (lower images) [area of the paraventricular nuclei (PVN)]. Sections on the left side of the figure are from the same control person, and those on the right from the same hypertensive person. It is evident that, although the vasopressin staining in the SCN of the hypertensive person is diminished compared to the control, CRH staining is enhanced [From Kalsbeek et al. (2010); Fig. 5, with permission]
In hypertensive patients an extremely high expression of CRH was also observed in all parts of the hypothalamic PVN (Fig. 4.19) . In addition, in contrast to the controls, the hypertensive patients had a very high number of CRH fibers running from the most rostral part of the PVN to the median eminence and innervating the caudal part of the SCN. A quantitative evaluation showed that the area covered by CRH fibers in the SCN of hypertensive patients was about three times larger than that in the SCN of controls. Moreover, a clear negative correlation was found between the area of CRH fibers and the number of AVP- or neurotensin-expressing neurons within the SCN (Goncharuk et al. 2007). These data indicate a serious dysregulation of the SCN in hypertensive patients. Such a disturbance may cause a harmful hemodynamic imbalance with a negative effect on circulation, especially in the morning, which is when the inactivity–activity balance changes. The difficulty in adjusting from inactivity to activity might be involved in the morning clustering of cardiovascular events. Interestingly, a transgenic hypertensive mouse strain (TGR(mRen2)27) showed an altered light-entrainment response, accompanied by suppressed c-fos-mRNA expression in the SCN (Lemmer et al. 2000), indicating a possible primary involvement of the SCN in hypertension.
4.7 Corticosteroids
Impaired sleep and mood disorder are the major side effects of glucocorticoid therapy . The mechanism responsible for the circadian disorder is unknown, but alterations in the SCN are presumed to play a major role. Liu et al. studied the amount of AVP-mRNA expression in the SCN in 10 glucocorticoid-exposed patients and 10 glucocorticoid-free controls, all well matched for age and clock time of death (Liu et al. 2006). The total amount of AVP-mRNA in the SCN was found to be two times lower in the glucocorticoid-exposed patients than in the control subjects. In addition, there was a 53 % decrease in the total number of profiles in the SCN that expressed AVP-mRNA in glucocorticoid-exposed patients compared with controls (Figs. 4.17 and 4.18). In conclusion, glucocorticoids have an inhibitory effect on AVP-mRNA expression in the human SCN, which may be the biological basis of the circadian rhythm disturbances during glucocorticoid therapy (Liu et al. 2006).
4.8 Conclusion
The human SCN shows functional alterations in relation to day–night, season, age, gender, sexual orientation, tumors compressing the SCN, AD, HD, depression, hypertension, and glucocorticoid exposure. In AD treatment, light and melatonin were found to increase sleep efficiency and to improve nocturnal restlessness, mood, performance, daytime energy, and quality of life.
These data show that functional immunocytochemistry, in situ hybridization, tracing, and morphometrics studies on clinically and neuropathologically well-characterized human postmortem material are not only possible but also meaningful in relation to health and disease.
References
Aziz A et al (2008) Hypocretin and melanin-concentrating hormone in patients with Huntington disease. Brain Pathol 18(4):474–483
Bailey M, Silver R (2013) Sex differences in circadian timing systems: implications for disease. Front Neuroendocrinol 35:111–139
Borgers AJ et al (2011) Compression of the optic chiasm is associated with permanent shorter sleep duration in patients with pituitary insufficiency. Clin Endocrinol (Oxf) 75(3):347–353
Borgers AJ et al (2013) Arginine vasopressin immunoreactivity is decreased in the hypothalamic suprachiasmatic nucleus of subjects with suprasellar tumors. Brain Pathol 23(4):440–444
Carlsson A et al (1980) Seasonal and circadian monoamine variations in human brains examined post mortem. Acta Psychiatr Scand Suppl 280:75–85
Couce ME et al (1997) Localization of leptin receptor in the human brain. Neuroendocrinology 66(3):145–150
Dai J et al (1997) Distribution of vasopressin and vasoactive intestinal polypeptide (VIP) fibers in the human hypothalamus with special emphasis on suprachiasmatic nucleus efferent projections. J Comp Neurol 383(4):397–414
Dai J et al (1998a) Postmortem tracing reveals the organization of hypothalamic projections of the suprachiasmatic nucleus in the human brain. J Comp Neurol 400(1):87–102
Dai J et al (1998b) Human retinohypothalamic tract as revealed by in vitro postmortem tracing. J Comp Neurol 397(3):357–370
Dai J et al (1998c) Postmortem anterograde tracing of intrahypothalamic projections of the human dorsomedial nucleus of the hypothalamus. J Comp Neurol 401(1):16–33
Duffy JF et al (2011) Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Natl Acad Sci USA 108(Suppl 3):15602–15608
Eaton SJ et al (1995) Histamine synthesis inhibition reduces light-induced phase shifts of circadian rhythms. Brain Res 695(2):227–230
Friedman DI et al (1991) Labeling of human retinohypothalamic tract with the carbocyanine dye, DiI. Brain Res 560(1–2):297–302
Garcia-Falgueras A et al (2011) Galanin neurons in the intermediate nucleus (InM) of the human hypothalamus in relation to sex, age, and gender identity. J Comp Neurol 519(15):3061–3084
Goncharuk VD et al (2001) Neuropeptide changes in the suprachiasmatic nucleus in primary hypertension indicate functional impairment of the biological clock. J Comp Neurol 431(3):320–330
Goncharuk VD et al (2007) Corticotropin-releasing hormone neurons in hypertensive patients are activated in the hypothalamus but not in the brainstem. J Comp Neurol 503(1):148–168
Hannibal J (2002) Neurotransmitters of the retino-hypothalamic tract. Cell Tissue Res 309(1):73–88
Hannibal J (2006) Roles of PACAP-containing retinal ganglion cells in circadian timing. Int Rev Cytol 251:1–39
Harper DG et al (2008) Dorsomedial SCN neuronal subpopulations subserve different functions in human dementia. Brain 131(Pt 6):1609–1617
Hofman MA (1997) Lifespan changes in the human hypothalamus. Exp Gerontol 32(4–5):559–575
Hofman MA (2000) The human circadian clock and aging. Chronobiol Int 17(3):245–259
Hofman MA (2003) Circadian oscillations of neuropeptide expression in the human biological clock. J Comp Physiol A Neuroethol Sens Neural Behav Physiol 189(11):823–831
Hofman MA (2004) The brain’s calendar: neural mechanisms of seasonal timing. Biol Rev Camb Philos Soc 79(1):61–77
Hofman MA, Swaab DF (1992a) The human hypothalamus: comparative morphometry and photoperiodic influences. Prog Brain Res 93:133–147, discussion 148–139
Hofman MA, Swaab DF (1992b) Seasonal changes in the suprachiasmatic nucleus of man. Neurosci Lett 139(2):257–260
Hofman MA, Swaab DF (1993) Diurnal and seasonal rhythms of neuronal activity in the suprachiasmatic nucleus of humans. J Biol Rhythms 8(4):283–295
Hofman MA, Swaab DF (1994) Alterations in circadian rhythmicity of the vasopressin-producing neurons of the human suprachiasmatic nucleus (SCN) with aging. Brain Res 651(1–2):134–142
Hofman MA, Swaab DF (1995) Influence of aging on the seasonal rhythm of the vasopressin-expressing neurons in the human suprachiasmatic nucleus. Neurobiol Aging 16(6):965–971
Hofman MA et al (1995) Effect of photoperiod on the diurnal melatonin and 5-methoxytryptophol rhythms in the human pineal gland. Brain Res 671(2):254–260
Kalsbeek A et al (1992) Vasopressin-containing neurons of the suprachiasmatic nuclei inhibit corticosterone release. Brain Res 580(1–2):62–67
Kalsbeek A et al (2008) Opposite actions of hypothalamic vasopressin on circadian corticosterone rhythm in nocturnal versus diurnal species. Eur J Neurosci 27(4):818–827
Kalsbeek A et al (2010) Vasopressin and the output of the hypothalamic biological clock. J Neuroendocrinol 22(5):362–372
Kimura A et al (2011) Estimating time of death based on the biological clock. Int J Legal Med 125(3):385–391
Kruijver FP, Swaab DF (2002) Sex hormone receptors are present in the human suprachiasmatic nucleus. Neuroendocrinology 75(5):296–305
Lamont EW et al (2007) The role of circadian clock genes in mental disorders. Dialogues Clin Neurosci 9(3):333–342
Lemmer B et al (2000) Loss of 24 h rhythm and light-induced c-fos mRNA expression in the suprachiasmatic nucleus of the transgenic hypertensive TGR(mRen2)27 rat and effects on cardiovascular rhythms. Brain Res 883(2):250–257
Li JZ et al (2013) Circadian patterns of gene expression in the human brain and disruption in major depressive disorder. Proc Natl Acad Sci USA 110(24):9950–9955
Liu RY et al (2000) Decreased vasopressin gene expression in the biological clock of Alzheimer disease patients with and without depression. J Neuropathol Exp Neurol 59(4):314–322
Liu RY et al (2006) Glucocorticoids suppress vasopressin gene expression in human suprachiasmatic nucleus. J Steroid Biochem Mol Biol 98(4–5):248–253
Luboshitzky R et al (1997) Seasonal variation of gonadotropins and gonadal steroids receptors in the human pineal gland. Brain Res Bull 44(6):665–670
Luboshitzky R et al (1998) Daily and seasonal variations in the concentration of melatonin in the human pineal gland. Brain Res Bull 47(3):271–276
Lucassen PJ et al (1995) Increased light intensity prevents the age related loss of vasopressin-expressing neurons in the rat suprachiasmatic nucleus. Brain Res 693(1–2):261–266
Mai JK et al (1991) Evidence for subdivisions in the human suprachiasmatic nucleus. J Comp Neurol 305(3):508–525
Miller AL (2005) Epidemiology, etiology, and natural treatment of seasonal affective disorder. Altern Med Rev 10(1):5–13
Miyata R et al (2009) Analysis of the hypothalamus in a case of X-linked lissencephaly with abnormal genitalia (XLAG). Brain Dev 31(6):456–460
Moore RY (1992) The fourth C.U. Ariens Kappers lecture. The organization of the human circadian timing system. Prog Brain Res 93:99–115, discussion 115–117
Neumeister A et al (2000) Seasonal variation of availability of serotonin transporter binding sites in healthy female subjects as measured by [123I]-2 beta-carbomethoxy-3 beta-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry 47(2):158–160
Ozawa T et al (1993) Shy-Drager syndrome with abnormal circadian rhythm of plasma antidiuretic hormone secretion and urinary excretion. Intern Med 32(3):225–227
Ozawa T et al (1998) Suprachiasmatic nucleus in a patient with multiple system atrophy with abnormal circadian rhythm of arginine-vasopressin secretion into plasma. J Neurol Sci 154(1):116–121
Ozawa T et al (2001) Reduced morning cortisol secretion in patients with multiple system atrophy. Clin Auton Res 11(4):271–272
Pierangeli G et al (2001) Nocturnal body core temperature falls in Parkinson’s disease but not in Multiple-System Atrophy. Mov Disord 16(2):226–232
Quigg M et al (1999) Hypothalamic neuronal loss and altered circadian rhythm of temperature in a rat model of mesial temporal lobe epilepsy. Epilepsia 40(12):1688–1696
Riemersma-van der Lek RF et al (2008) Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 299(22):2642–2655
Romijn HJ et al (1999) Colocalization of VIP with AVP in neurons of the human paraventricular, supraoptic and suprachiasmatic nucleus. Brain Res 832(1–2):47–53
Sadun AA et al (1983) Paraphenylenediamine: a new method for tracing human visual pathways. J Neuropathol Exp Neurol 42(2):200–206
Schaechter JD, Sadun AA (1985) A second hypothalamic nucleus receiving retinal input in man: the paraventricular nucleus. Brain Res 340(2):243–250
Schwartz WJ et al (1986) A discrete lesion of ventral hypothalamus and optic chiasm that disturbed the daily temperature rhythm. J Neurol 233(1):1–4
Scully RE et al (1983) A 55-year-old woman with diabetes insipidus. N Engl J Med 309:418–425
Sivan Y et al (2001) Melatonin production in healthy infants: evidence for seasonal variations. Pediatr Res 49(1):63–68
Stopa EG et al (1999) Pathologic evaluation of the human suprachiasmatic nucleus in severe dementia. J Neuropathol Exp Neurol 58(1):29–39
Swaab DF (2003) The human hypothalamus. Basic and clinical aspects. Part I: Nuclei of the hypothalamus. In: Aminoff MJ, Boller F, Swaab DF (eds) Handbook of clinical neurology, vol 79. Elsevier, Amsterdam
Swaab DF (2004a) The human hypothalamus. Basic and clinical aspects. Part II: Neuropathology of the hypothalamus and adjacent brain structures. In: Aminoff MJ, Boller F, Swaab DF (eds) Handbook of Clinical Neurology, vol 80. Elsevier, Amsterdam
Swaab DF (2004b) Neuropeptides in hypothalamic neuronal disorders. Int Rev Cytol 240:305–375
Swaab DF, Hofman MA (1990) An enlarged suprachiasmatic nucleus in homosexual men. Brain Res 537(1–2):141–148
Swaab DF, Hofman MA (1995) Sexual differentiation of the human hypothalamus in relation to gender and sexual orientation. Trends Neurosci 18(6):264–270
Swaab DF et al (1985) The suprachiasmatic nucleus of the human brain in relation to sex, age and senile dementia. Brain Res 342(1):37–44
Swaab DF et al (1987) Suprachiasmatic nucleus in aging, Alzheimer’s disease, transsexuality and Prader-Willi syndrome. Prog Brain Res 72:301–310
Swaab DF et al (1992) Tau and ubiquitin in the human hypothalamus in aging and Alzheimer’s disease. Brain Res 590(1–2):239–249
Swaab DF et al (1993) Functional neuroanatomy and neuropathology of the human hypothalamus. Anat Embryol (Berl) 187(4):317–330
Swaab DF et al (2002) Brain aging and Alzheimer’s disease; use it or lose it. Prog Brain Res 138:343–373
Tuunainen A et al (2001) Retinal circadian rhythms in humans. Chronobiol Int 18(6):957–971
van de Nes JA et al (1998) Comparison of beta-protein/A4 deposits and Alz-50-stained cytoskeletal changes in the hypothalamus and adjoining areas of Alzheimer’s disease patients: amorphic plaques and cytoskeletal changes occur independently. Acta Neuropathol 96(2):129–138
van Londen L et al (2001) Weak 24-h periodicity of body temperature and increased plasma vasopressin in melancholic depression. Eur Neuropsychopharmacol 11(1):7–14
Van Someren EJ (2000) Circadian rhythms and sleep in human aging. Chronobiol Int 17(3):233–243
Van Someren EJ et al (2002) Functional plasticity of the circadian timing system in old age: light exposure. Prog Brain Res 138:205–231
van Wamelen DJ et al (2013a) Suprachiasmatic nucleus neuropeptide expression in patients with Huntington’s disease. Sleep 36(1):117–125
van Wamelen DJ et al (2013b) Decreased hypothalamic prohormone convertase expression in Huntington disease patients. J Neuropathol Exp Neurol 72(12):1126–1134
Verheggen RJ et al (2012) Complete absence of evening melatonin increase in tetraplegics. FASEB J 26(7):3059–3064
Witting W et al (1993) Effect of light intensity on diurnal sleep-wake distribution in young and old rats. Brain Res Bull 30(1–2):157–162
Wu YH, Swaab DF (2007) Disturbance and strategies for reactivation of the circadian rhythm system in aging and Alzheimer’s disease. Sleep Med 8(6):623–636
Wu YH et al (2003) Molecular changes underlying reduced pineal melatonin levels in Alzheimer disease: alterations in preclinical and clinical stages. J Clin Endocrinol Metab 88(12):5898–5906
Wu YH et al (2006a) Pineal clock gene oscillation is disturbed in Alzheimer’s disease, due to functional disconnection from the “master clock”. FASEB J 20(11):1874–1876
Wu YH et al (2006b) Distribution of MT1 melatonin receptor immunoreactivity in the human hypothalamus and pituitary gland: co-localization of MT1 with vasopressin, oxytocin, and corticotropin-releasing hormone. J Comp Neurol 499(6):897–910
Wu YH et al (2007) Decreased MT1 melatonin receptor expression in the suprachiasmatic nucleus in aging and Alzheimer’s disease. Neurobiol Aging 28(8):1239–1247
Wu YH et al (2013) Alterations of melatonin receptors MT1 and MT2 in the hypothalamic suprachiasmatic nucleus during depression. J Affect Disord 148(2–3):357–367
Zhou JN et al (1995) VIP neurons in the human SCN in relation to sex, age, and Alzheimer’s disease. Neurobiol Aging 16(4):571–576
Zhou JN et al (1996) Morphometric analysis of vasopressin and vasoactive intestinal polypeptide neurons in the human suprachiasmatic nucleus: influence of microwave treatment. Brain Res 742(1–2):334–338
Zhou JN et al (2001) Alterations in arginine vasopressin neurons in the suprachiasmatic nucleus in depression. Arch Gen Psychiatry 58(7):655–662
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 The American Physiological Society
About this chapter
Cite this chapter
Bao, AM., Swaab, D.F. (2016). The Human SCN in Health and Neuropsychiatric Disorders: Postmortem Observations. In: Gumz, M. (eds) Circadian Clocks: Role in Health and Disease. Physiology in Health and Disease. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3450-8_4
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3450-8_4
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3448-5
Online ISBN: 978-1-4939-3450-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)