Abstract
Robust and sustainable development of poultry industry requires prevention of deadly infectious diseases. Vigorous vaccination of the birds is a routine practice; however, the live and inactivated vaccines that are used have inherent disadvantages. New-generation vaccines such as DNA vaccines offer several advantages over conventional vaccines. DNA vaccines, which encode an antigen of interest or multiple antigens in the target host, are stable, easy to produce and administer, do not require cold chain maintenance, and are not affected by the maternal antibodies. In addition, DNA vaccines can also be administered in ovo, and thus, mass vaccination and early induction of immune response can effectively be achieved. In this chapter, we focus on the development of DNA vaccines against important infectious viral as well as parasitic diseases of poultry.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Keywords
1 Introduction
Proper health management of birds is very crucial for successful development of the poultry sector. A number of infectious diseases affect birds and cause a potential threat to the industry in the form of huge economic losses. Vaccination of the birds against the infectious diseases is widely followed; however, conventional vaccines have certain disadvantages [1]. With the advancement in the recombinant DNA technology, new-generation vaccines have emerged as a safer replacement to the conventional vaccines. DNA vaccines, which contain gene(s) encoding for one or more than one antigenic proteins, offer many advantages over conventional vaccines. In DNA vaccine, the expression of antigens in the target host resembles native pathogen epitopes more closely, and thus preserves the protein structure and antigenicity than the conventional vaccines [2–4]. Further, DNA vaccines are able to efficiently stimulate both humoral and cellular immune responses to protein antigens, and thus effective against a wide range of pathogens [5]. However, success of DNA vaccination in birds depends on many factors apart from their efficacy. They have to be relatively less expensive, easy to administer, and stable under field conditions. Moreover, as poultry are food animals as well, it is undesirable to have vaccine residues in the relevant tissues. This has been avoided by the use of subcutaneous or intradermal routes instead of intramuscular route [6].
The plasmid vectors are easy to construct and can be produced in large quantities quickly and affordably than conventional vaccines. In addition, only a small quantity (micrograms) of plasmid vector can deliver several antigens in a single shot, which provide immunity against many pathogens at once. All these factors significantly reduce the expenses incurred by vaccination [7, 8]. The effectiveness of DNA vaccines can be further enhanced by the inclusion of the molecular adjuvants such as TLR (Toll-like receptor) ligands and cytokines. Notable examples of TLR ligands include CpG (TLR21) and flagellin (TLR5) and cytokines such as IL-12 and IFN-γ. A number of studies have reported upregulation of the immune response when TLR ligands and cytokines were given along with a DNA vaccine [3, 9–13].
1.1 Advantages of DNA Vaccines
-
1.
The production of DNA vaccine is easy, rapid, and economical as compared to conventional vaccines.
-
2.
The DNA vaccine is more thermostable than traditional vaccines; hence, maintenance of a cold chain is not required.
-
3.
It eliminates the risk of reversion of pathogenic phenotypes.
-
4.
DNA vaccines present antigen to both MHC-I and MHC-II molecules.
-
5.
The immune response elicited by DNA vaccine is directed against only the antigen of interest.
-
6.
Cost-effectiveness and ease of development.
-
7.
DNA vaccines mimic a natural infection. Antigenic protein closely resembles the normal eukaryotic structure and undergoes post translational modifications.
1.2 Important Poultry Infectious Diseases and DNA Vaccine Antigens
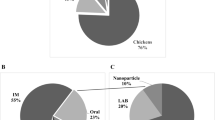
Poultry suffers from a number of infectious diseases, including Newcastle disease (ND), Infectious bursal disease (IBD), Infectious bronchitis (IB), Avian Influenza (AI), and Eimeria sp. Both inactivated and live vaccines are widely used against these diseases, but these vaccines are associated with their inherent disadvantages [1, 3, 4]. A number of studies have shown that DNA vaccines are efficacious in conferring protection against infectious diseases in chickens. Further, as a DNA vaccine encodes antigenic protein(s) in the absence of the live pathogen, it helps in avoiding the occurrence of problems associated with reverted virulence, divergent mutants and reduces environmental contamination [13]. The antigenic protein encoding pathogen genes which have been used in the chicken DNA vaccines are given in Table 1 along with molecular adjuvants that were used to enhance the efficacy of the vaccines.
1.3 Points to Consider before Selecting a Vaccine Antigen
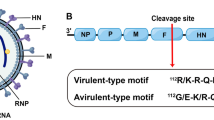
The selection of a gene of interest (vaccine gene) is a crucial aspect before construction of a DNA vaccine as it affects the type of immune response (humoral or cell mediated) induced. In case, where neutralizing antibodies are needed to prevent the occurrence of an infection, most appropriately, a surface antigen is selected. DNA vaccines designed to treat an established infection need to have an antigen that induce a potent cell mediated immune (CMI) response. In such cases, infecting pathogens have intracellular life cycle and, hence, humoral immune response will not be effective to eliminate the infection. The antigens selected for this purpose are the ones which are expressed intracellularly during infection. Such antigens are processed inside the cell and presented to major histocompatibility molecules for the generation of CMI response. For example, cellular immunity is essential in Newcastle disease virus (NDV) infection as viral pathogenesis includes an intracellular stage [13, 44].
1.4 Strategies to Enhance the Protein Expression from a DNA Vector
This can be achieved by the following methods:
-
1.
Placing Kozak sequence (GCCRCCATGG) upstream to the gene in such a way that, if possible, it includes start codon of the gene [45].
-
2.
Check if 5′ untranslated (UTR) region contains ATG codons, they can be removed [46].
-
3.
Placing an intron in front of the gene further enhances the rate of transcription.
-
4.
Codon optimization without altering the protein sequence can enhance the rate of translation [46].
-
5.
The efficiency of the DNA uptake following DNA vaccination is not very efficient; hence, to enhance the DNA uptake various formulations have been used. Formulating DNA vaccine in microparticles or liposomes has been reported to increase the uptake of plasmid DNA by cells in animal models [47].
1.5 Enhancing Immunogenicity of the DNA Vaccine
-
1.
Immunogenicity of the DNA vaccine can be augmented by incorporating coding sequences for the peptide epitopes as opposed to the full coding sequence.
-
2.
Inclusion of sequence coding for cytokines such IL-12 and granulocyte–macrophage colony-stimulating factor (GM-CSF) which can enhance CTL responses [48].
-
3.
Plasmid encoding IL-2 improves overall efficacy while interferon (IFN)-γ enhances Th1 type responses.
-
4.
Humoral responses are enhanced by including coding sequences of IL-4, IL-5 and IL-10.
-
5.
Inclusion of TLR (Toll-like receptor) ligands such flagellin (TLR5), Poly I:C (TLR3) and CpG (TLR21) can substantially enhance the immune responses [13].
2 Materials Required
2.1 For Cloning
-
1.
DNA or plasmid containing the gene of interest.
-
2.
RNA isolation and cDNA synthesis kit.
-
3.
Gene specific primers for amplification by polymerase chain reaction (PCR).
-
4.
PCR cloning kit.
-
5.
A cloning vector (pTZ 57R/T) for cloning and sequencing of the vaccine gene.
-
6.
Restriction enzymes, T4 DNA ligase, 10× buffers.
-
7.
Suitable eukaryotic expression vector (e.g., pcDNA3.1, pCI).
-
8.
Agarose, loading dye, and nucleic acid stain (ethidium bromide) suitable for gel electrophoresis.
-
9.
Agarose gel electrophoresis system.
-
10.
UV spectrophotometer.
-
11.
Gel extraction kit (Qiagen).
-
12.
Competent E.coli(DH5α) cells for the propagation of the plasmid vector. Competent E. coli cells can be made following standard Sambrook protocol.
-
13.
SOC media.
To prepare 1000 ml SOC—add the following to 900 ml of distilled H2O: 20 g Bacto tryptone, 5 g Bacto yeast extract, 2 ml of 5 M NaCl, 2.5 ml of 1 M KCl, 10 ml of 1 M MgCl2, 10 ml of 1 M MgSO4, 20 ml of 1 M glucose. Adjust to 1 l with distilled H2O (dH2O) and sterilize by autoclaving.
-
14.
LB agar plate with appropriate antibiotic for selection of transformed colonies.
To make 1000 ml of LB agar—add the following to 800 ml dH2O: 10 g Bacto tryptone, 5 g yeast extract, 10 g NaCl. Adjust pH to 7.5 with NaOH. Add 15 g agar, melt agar into solution in a microwave oven. Adjust volume to 1 l with dH2O and sterilize by autoclaving.
-
15.
Incubator for the growth of plates.
2.2 Recombinant Clone Selection
-
1.
LB medium—add the following to 800 ml dH2O: 10 g Bacto tryptone, 5 g yeast extract, 10 g NaCl. Adjust pH to 7.5 with NaOH. Make final volume to 1 l with dH2O and sterilize by autoclaving.
-
2.
Sterile inoculation loop.
-
3.
Sterile tubes.
-
4.
Shaker incubator.
-
5.
Plasmid isolation kit (Qiagen).
-
6.
Restriction enzymes to confirm the clone.
-
7.
Agarose, loading dye, DNA molecular ladder, and ethidium bromide stain.
-
8.
Agarose gel electrophoresis system, UV spectrophotometer.
2.3 Confirmation of Protein Expression
-
1.
Cell line for transfection of the expression vector (CHO, HEK).
-
2.
Appropriate growth medium (e.g., DMEM) with serum or growth factors or both.
-
3.
Opti-MEM media, transfection agent (Lipofectamine 2000), fetal bovine serum (FBS), PBS, 6-well plates.
-
4.
A positive control (GFP cloned into the expression vector).
-
5.
Specific primary antibody to the antigenic protein.
-
6.
Secondary conjugated antibody against the primary antibody.
-
7.
Materials for Western blotting and/or immunofluorescence.
-
8.
Molecular adjuvants
2.4 Inoculation of Plasmid
-
1.
High quality endotoxin free plasmid DNA.
-
2.
Needles (18- and 27-Gauge) and tuberculin syringes.
-
3.
Phosphate-buffered saline (PBS): 0.01 M Na2HPO4/KH2PO4, 0.15 M NaCl/KCl, pH 7.3 (8 g NaCl, 0.2 g KCl, 1.15 g Na2HPO4, 0.2 g KH2PO4 per liter).
2.5 Evaluation of Humoral Immunity
-
1.
An enzyme-linked immunosorbent assay (ELISA) reader.
-
2.
Coating buffer: 100 mM Na2CO3/NaHCO3, pH 9.5 for ELISA.
-
3.
PBST (PBS with 0.05 % Tween 20).
-
4.
HRP conjugated secondary antibody, substrate [100 mM citrate phosphate solution containing 1 mg/ml o-phenylenediamine (OPD) and 1 μl H2O2].
-
5.
Reaction stop solution (50 μl of 8 N H2SO4).
2.6 Evaluation of Cellular Immunity (Lymphocyte Proliferation Test and ELISPOT)
-
1.
Vacutainer tubes with anticoagulant.
-
2.
Hemocytometer, 96-well microtiter plate.
-
3.
Trypan blue dye.
-
4.
Ficoll-Hypaque solution.
-
5.
RPMI-1640, PBS, pen-strep, FBS, Con A.
-
6.
MTT dye (3-4,5-dimethylthiazol-2-yl-2,5-diphenyl-tetrazoliumbromide).
-
7.
DMSO (dimethyl sulfoxide).
-
8.
ELISA reader.
-
9.
96-well nitrocellulose plates.
-
10.
RBC lysis buffer. 10× RBC Lysis Buffer: 90 g NH4Cl (0.155 M), 10 g KHCO3 (0.01 M), 370 mg EDTA (0.1 mM). Dissolve in 1 l of ddH2O and filter through a 0.22 μm filter.
-
11.
Chicken IFN-γ specific antibody.
-
12.
Bovine serum albumin (BSA).
-
13.
Appropriate secondary conjugated antibody (Biotinylated).
-
14.
Streptavidin-alkaline phosphatase, substrates nitro-blue tetrazolium (NBT) and 5-bromo-4-chloro-3′-indolyl phosphate.
3 Procedure
3.1 Construction, Production, and Purification of the Plasmid Vector
Plasmid vector for expression of the gene of interest mostly contain human cytomegalovirus virus promoter (HCMV), like pcDNA3.1 and pCI; however, other promoters such as Rou sarcoma virus long terminal repeat (LTR) is also being used though it drives a weaker expression than HCMV promoter. Vaccine gene having start and stop codon is being inserted downstream to the promoter sequence followed by a polyadenylation sequence at its 3′ end (Fig. 1).
-
1.
Obtain vaccine gene either from other cloned plasmid or from DNA sequence by PCR amplification. When the vaccine gene is not available, but its sequence is known, cDNA is generated from the virus infected tissue that expresses high levels of the gene. Primers used for this purpose should have suitable restriction sites (directional cloning). Use proofreading polymerases to eliminate the chances of sequence modifications.
-
2.
Purify the amplicon and digest it with the specific restriction enzymes. Cut the plasmid vector with the same restriction enzymes.
-
3.
Load the restriction digested vector and insert on an agarose gel.
-
4.
Resolve and gel purify the insert and vector fragments using the Qiagen gel purification kit. Measure the concentration of the vector and insert elutes.
-
5.
Set up ligation reaction. Usually a molar ratio of 1:3 (vector to insert) is chosen.
For a typical 10 μl reaction (containing equimolar concentrations of vector and insert):
Vector:
2 μl
Insert:
6 μl
10× ligase buffer:
1 μl
T4 DNA ligase:
0.5 μl
DW:
0.5 μl
-
6.
Incubate the ligation mixture overnight at 16 °C.
-
7.
Take out the competent Escherichia coli(DH5α) cells from deep freezer and thaw it on ice.
-
8.
Add 1–5 μl of the ligation mixture to the 50 μl of the competent cells. Gently mix by flicking the bottom of the tube with finger. Keep for 30 min on ice.
-
9.
Transform the cells. Give a brief heat shock by placing the bottom 1/2 to 2/3 of the tube into a 42 °C water bath for 30–60 s (45 s is usually ideal, but this varies depending on the competent cells).
-
10.
Place the tube back on ice for 2 min.
-
11.
Add 500 μl of SOC media (without antibiotic) and grow in a 37 °C shaking incubator for 60 min.
-
12.
Spread 50–100 μl of transformation growth onto an agar plate containing the appropriate antibiotic.
-
13.
Grow the transformed culture overnight at 37 °C in an incubator.
3.2 Recombinant Clone Selection
-
1.
Using sterile inoculation loops, pick each colony and aseptically inoculate each into a 6 ml culture of Luria–Bertani (LB) medium with appropriate antibiotic in a 15 ml tube.
-
2.
Grow overnight in LB medium at 37 °C in a shaking incubator for 12–15 h.
-
3.
Plasmid is isolated from the culture with a plasmid isolation kit (Qiagen).
-
4.
Check for the presence of gene of interest by restriction digestion and by sequencing of the plasmid DNA region having the gene of interest.
-
5.
Asses the purity and concentration of the plasmid DNA by determining the ratio of absorbance at 260 nm over 280 nm (~1.8).
-
6.
Grow a culture of the confirmed clone to isolate plasmid for in vitro and in vivo testing.
-
7.
High quality plasmid (low endotoxin) DNA may be bulk purified by using a purification kit (Qiagen).
3.3 In Vitro Confirmation of Protein Expression
The expression of the DNA vaccine construct is verified in vitro before it could be used in vivo by transient transfection studies in a suitable cell line. The most commonly used cell lines for this purpose include HEK (Human embryonic kidney) and COS-7 (Monkey kidney fibroblasts) cell lines which offer high transfection efficiencies and, hence, greater protein expression.
-
1.
Cells are grown in a suitable medium supplemented with 10 % fetal bovine serum (FBS).
-
2.
When cells reach 50–70 % confluency, transfect the DNA.
-
3.
For a 6-well plate, add 4 μg of plasmid in 150 μl of Opti-MEM. In another vial, dilute 10 μl of Lipofectamine™ 2000 (Invitrogen) reagent and keep at room temperature for 5 min (seeNote 1).
-
4.
Mix the contents of both the vials and allow to stand at room temperature for 25–30 min.
-
5.
After the incubation period, add the complex drop by drop to the cells. Media can be changed after 5–6 h.
-
6.
Use a positive control such as GFP cloned downstream to the promoter to monitor its activity in the cells.
-
7.
Harvest the cells and supernatant after a stipulated period of time (1–3 days).
-
8.
Presence of expressed foreign protein either in cells or in supernatant may be determined by the following methods (seeNote 2):
-
(a)
Western blotting.
-
(b)
Immunofluorescence.
-
(c)
Immunoprecipitation after radiolabeling the cells.
-
(d)
Enzyme-linked immunosorbent assay (ELISA).
-
(e)
Fluorescence-activated cell sorting (FACS) analysis.
-
(a)
3.4 In Vivo Immunization
-
1.
Procure specific pathogen free chickens (SPF).
-
2.
Divide birds at 14 days of age into different groups depending on the study including suitable controls.
-
3.
Birds are immunized with about 100 μg of plasmid either by subcutaneous or intramuscular route twice at 2 weeks interval with the help of 1 ml tuberculin syringes with attached 27 G 3/4″ needle.
3.5 Evaluation of Humoral and Cellular Response
3.5.1 Humoral Response
Humoral immune response can be evaluated in many ways including ELISA, B-cellELISPOT assay, and Neutralization assay. The most frequent and convenient way of measuring specific antibody immune response is ELISA which can also be used to quantitate the response [49, 50].
Antibody levels in pre- and post-immunization serum sample are quantified by ELISA as follows:
-
1.
The serum samples from immunized and control groups are collected at different intervals (0, 7, 21, and 28 days) post immunization and tested for the vaccine antigen specific antibodies.
-
2.
Coat the 96-well microtiter plate with vaccine antigen in the coating buffer (100 mM bicarbonate buffer, pH 9.5) at 4 °C overnight.
-
3.
Wash the plate next day and block with 2 % bovine serum albumin (BSA).
-
4.
Collect sera at different intervals and add in the respective wells (1:100).
-
5.
Incubate the plate at 37 °C for 1 h.
-
6.
After incubation, wash the plate with PBS-T thrice and incubate with HRP conjugated secondary antibody (1:3000) at 37 °C for 1 h (seeNote 3).
-
7.
Wash the plate and add substrate solution [100 mM citrate phosphate solution containing 1 mg/ml o-phenylenediamine (OPD) and 1 μl H2O2].
-
8.
Stop the reaction after 30 min with 50 μl of 8 N H2SO4.
-
9.
Measure the absorbance at 490 nm in an ELISA reader.
3.5.2 Evaluation of Cell Mediated Immune Response
Cell mediated immune response can be measured by Lymphocyte transformation assay (LTT) and cytokine ELISPOT assay. In response to specific antigen, lymphocytes proliferate which indicates the specificity of the lymphocytes to the particular antigen. Cytokine ELISPOT assay detects the cytokines secreted by the lymphocytes in response to the specific antigen [51, 52].
3.5.2.1 Lymphocyte Transformation Test (LTT)
-
1.
Collect the blood from chicken in sterile syringe having an anticoagulant (EDTA) and layer it over Ficoll-Hypaque with density 1.077 g/ml.
-
2.
After centrifugation at 1000 × g for 45 min, collect the interface containing the PBMCs and wash twice with PBS.
-
3.
Resuspend PBMCs in RPMI-1640 media containing 10 % FBS and 1 % pen-strep.
-
4.
Determine the cell viability by trypan blue dye exclusion method.
-
5.
Adjust the cell concentration to 1 × 107 cells/ml.
-
6.
Plate 100 μl of the cell suspension in triplicate into 96-well plates.
-
7.
Add 100 μl of the media containing either vaccine antigen (50 μg/ml) or ConA (10 μg/ml) into wells.
-
8.
Incubate the plate at 37 °C in 5 % CO2 for 2 days.
-
9.
After 2 days of incubation, add 20 μl of 5 mg/ml MTT dye (3-4,5-dimethylthiazol-2-yl-2,5-diphenyl-tetrazoliumbromide) to each well.
-
10.
Incubate the plate for another 4 h.
-
11.
Dissolve the formazan crystal formed in 100 μl of DMSO.
-
12.
Take the optical density (OD) readings on microplate ELISA reader at an absorbance of 495 nm.
-
13.
The proliferative response for the assay is expressed as stimulation index (SI), calculated by dividing the mean OD of the stimulated cultures by the mean OD of unstimulated control cultures.
3.5.2.2 ELISPOT Assay
-
1.
Spleen tissue is collected from the immunized chickens and placed in Hank’s balanced salt solution (HBSS) (140 mM NaCl, 5 mM KCl, 2.5 mM CaCl2, 1.1 mM MgCl2, 5.6 mM glucose, and 10 mM HEPES, pH 7.4).
-
2.
Make single cell suspension by squeezing it through 70 μm mesh or 5-ml syringe plunger in RPMI-1640 media supplemented with FBS.
-
3.
Centrifuge and resuspend in RBC lysis buffer at room temperature for 5 min (seeNote 4).
-
4.
Wash twice with HBSS and resuspend in RPMI-1640 with 5 % FBS, 2 mM GlutaMAX-I, 50 mM β-mercaptoethanol, 100 U/ml penicillin, and 100 μg/ml streptomycin sulfate.
-
5.
Determine the cell viability by trypan blue method and adjust the cell concentration to 1 × 106/ml.
-
6.
Coat plate with anti-chicken IFN-γ antibody (5 μg/ml) in coating buffer (sodium bicarbonate, 50 mM, pH 9.6) and incubate overnight at 4 °C.
-
7.
Wash the plate thrice with PBS-T (140 mM NaCl, 5 mM KCl, 10 mM Na2HPO4, 1 mM KH2PO4, and 0.05 % (v/v) Tween 20, pH 7.2).
-
8.
Block the plates with blocking solution (1 % BSA) for 1 h at 41 °C in 5 % CO2.
-
9.
Discard the blocking buffer and seed splenocytes at a cell density of 2 × 105 to 3 × 105/100 μl to triplicate wells.
-
10.
Cells are incubated with either in the presence of media alone or with recombinant vaccine antigen to a final volume of 200 μl per well for 24 h at 41 °C in 5 % CO2 incubator.
-
11.
After incubation, wash the plate twice with dH2O and thrice with PBS-T.
-
12.
Dilute biotinylated secondary antibody (1 μg/ml) specific to chicken IFN-γ in PBS-T and 1 % BSA (blocking buffer) and add 100 μl/well for 1–2 h at room temperature.
-
13.
Incubate plate with streptavidin-alkaline phosphatase (2 μg/ml) (in blocking buffer for 1 h at room temperature).
-
14.
Wash the plate three to five times and develop the color by adding substrate NDB/BCIP and wait for the spots to appear.
-
15.
Let the plate dry and count the spots with a stereoscope.
-
Humoral and cell mediated immune response may also be estimated at transcription level by quantifying cytokines mRNA levels by real-time PCR (seeNote 5).
-
3.6 Challenge Study (Determination of Protection from Challenge)
-
1.
To further test the efficacy of the DNA vaccine, immunized birds may be challenged with a virulent strain of the pathogen.
-
2.
After booster dose (second immunization), birds are intra-ocularly challenged with the virulent pathogen.
-
3.
Monitor the birds for the next few days (10 days) for clinical signs and symptoms.
-
4.
Protection against challenge is assessed by studying the occurrence of mortality in susceptible birds, presence of pathogen in the tissue, gross lesions, and bursa–body weight ratio.
-
5.
Histological examinations are also done to confirm the protection status.
4 Notes
-
1.
The optimal Lipofectamine–DNA ratio for transfection varies from one cell type to another, and should be determined beforehand to enhance the transfection efficiency. Also, use of other transfection agents may enhance the transfection efficiency.
-
2.
Expression of vaccine gene can also be analyzed at the transcription level through quantifying mRNA levels by Real-time PCR.
-
3.
The optimal dilutions of the antibody for the use in experiments are provided by the manufacturers, but may have to be determined in some cases depending on the type of experiment.
-
4.
Splenocytes may also be separated by density gradient centrifugation omitting the need of a RBCs lysis step. Spleen tissue is passed through a 70 μm mesh and cells are suspended in the media. Layer the cell suspension over Ficoll and centrifuge. Wash the interface twice with PBS and resuspend the cells in media [52].
-
5.
Both humoral and cellular immune responses may also be analyzed at the transcription level by quantifying mRNA levels of cytokines. The mRNA levels of Th1 and Th2 cytokines such as IFN-γ, IL-12, and IL-4 are quantified by real-time PCR.
References
Bowersock TL (2002) Evolving importance of biologics and novel delivery systems in the face of microbial resistance. AAPS PharmSci 4:1–7
O’Hagan DT, MacKichan ML, Singh M (2001) Recent developments in adjuvants for vaccines against infectious diseases. Biomol Eng 18:69–85
Min W et al (2001) Adjuvant effects of IL-1beta, IL-2, IL-8, IL-15, IFN-alpha, IFN-gamma TGFbeta4 and lymphotactin on DNA vaccination against Eimeria acervulina. Vaccine 20:267–274
Li K et al (2013) Adjuvant effects of interleukin-18 in DNA vaccination against infectious bursal disease virus in chickens. Vaccine 31:1799–1805
Donnelly JJ, Ulmer JB, Shiver JW, Liu MA (1997) DNA vaccines. Annu Rev Immunol 15:617–648
Dhama K, Mahendran M, Gupta PK, Rai A (2008) DNA vaccines and their applications in veterinary practice: current perspectives. Vet Res Commun 32:341–356
Rao SS et al (2009) A gene-based avian influenza vaccine in poultry. Poultry Sci 88:860–866
Beard CW, Mason PW (1998) Out on the farm with DNA vaccines. Nat Biotechnol 16:1325–1328
Van Duin D, Medzhitov R, Shaw AC (2006) Triggering TLR signaling in vaccination. Trends Immunol 27:49–55
Coban C et al (2011) Novel strategies to improve DNA vaccine immunogenicity. Curr Gene Ther 11:479–484
Gupta SK et al (2013) Recombinant flagellin and its cross-talk with lipopolysaccharide—effect on pooled chicken peripheral blood mononuclear cells. Res Vet Sci 95:930–935
Gupta SK, Bajwa P, Deb R, Chellappa MM, Dey S (2014) Flagellin a toll-like receptor 5 agonist as an adjuvant in chicken vaccines. Clin Vaccine Immunol 21:261–270
Gupta SK, Deb R, Dey S, Chellappa MM (2014) Toll-like receptor-based adjuvants: enhancing the immune response to vaccines against infectious diseases of chicken. Exp Rev Vaccine 13:909–925
Loke CF, Omar AR, Raha AR, Yusoff K (2005) Improved protection from velogenic Newcastle disease virus challenge following multiple immunizations with plasmid DNA encoding for F and HN genes. Vet Immunol Immunopathol 106:259–267
Sawant PM et al (2011) Immunomodulation of bivalent Newcastle disease DNA vaccine induced immune response by co-delivery of chicken IFN-γ and IL-4 genes. Vet Immunol Immunopathol 144:36–44
Zhao K et al (2013) Preparation and efficacy of Newcastle disease virus DNA vaccine encapsulated in PLGA nanoparticles. PLoS One 8(12):e82648
Chang HC, Lin TL, Wu CC (2001) DNA-mediated vaccination against infectious bursal disease in chickens. Vaccine 20:328–335
Hulse DJ, Romero CH (2004) Partial protection against infectious bursal disease virus through DNA-mediated vaccination with the VP2 capsid protein and chicken IL-2 genes. Vaccine 22:1249–1259
Mahmood MS, Siddique M, Hussain I, Khan A, Mansoor MK (2006) Protection capability of recombinant plasmid DNA vaccine containing VP2 gene of very virulent infectious bursal disease virus in chickens adjuvanted with CpG oligodeoxynucleotide. Vaccine 24:4838–4846
Park JH, Sung HW, Yoon BI, Kwon HM (2009) Protection of chicken against very virulent IBDV provided by in ovo priming with DNA vaccine and boosting with killed vaccine and the adjuvant effects of plasmid-encoded chicken interleukin-2 and interferon-γ. J Vet Sci 10:131–139
Kumar S et al (2009) Effective protection by high efficiency bicistronic DNA vaccine against infectious bursal disease virus expressing VP2 protein and chicken IL-2. Vaccine 27:864–869
Sun JH, Yan YX, Jiang J, Lu P (2005) DNA immunization against very virulent infectious bursal disease virus with VP2‐4‐3 gene and chicken IL‐6 gene. J Vet Med B 52:1–7
Maity HK, Dey S, Mohan CM, Khulape SA, Pathak DC, Vakharia VN (2015) Protective efficacy of a DNA vaccine construct encoding the VP2 gene of infectious bursal disease and a truncated HSP70 of Mycobacterium tuberculosis in chickens. Vaccine 33:1033–1039
Kapczynski DR, Hilt DA, Shapiro D, Sellers HS, Jackwood MW (2003) Protection of chickens from infectious bronchitis by in ovo and intramuscular vaccination with a DNA vaccine expressing the S1 glycoprotein. Avian Dis 47:272–285
Tang M, Wang H, Zhou S, Tian G (2008) Enhancement of the immunogenicity of an infectious bronchitis virus DNA vaccine by a bicistronic plasmid encoding nucleocapsid protein and interleukin-2. J Virol Methods 149:42–48
Tan B, Wang H, Shang L, Yang T (2009) Coadministration of chicken GM-CSF with a DNA vaccine expressing infectious bronchitis virus (IBV) S1 glycoprotein enhances the specific immune response and protects against IBV infection. Arch Virol 154:1117–1124
Yang T et al (2009) Multivalent DNA vaccine enhanced protection efficacy against infectious bronchitis virus in chickens. J Vet Med Sci 71:1585–1590
Fynan EF, Robinson HL, Webster RG (1993) Use of DNA encoding influenza hemagglutinin as an avian influenza vaccine. DNA Cell Biol 12:785–789
Qiu M et al (2006) Protection against avian influenza H9N2 virus challenge by immunization with hemagglutinin-or neuraminidase-expressing DNA in BALB/c mice. Biochim Biophy Res Commun 343:1124–1131
Jiang Y (2007) Enhanced protective efficacy of H5 subtype avian influenza DNA vaccine with codon optimized HA gene in a pCAGGS plasmid vector. Antiviral Res 75:234–241
Rao S et al (2008) Multivalent HA DNA vaccination protects against highly pathogenic H5N1 avian influenza infection in chickens and mice. PLoS One 3(6):e2432
Jalilian B et al (2010) Research development of avian influenza virus H5 DNA vaccine and MDP-1 gene of Mycobacterium bovis as genetic adjuvant. Genet Vaccine Ther 8:4
Cherbonnel M, Rousset J, Jestin V (2003) Strategies to improve protection against low-pathogenicity H7 avian influenza virus infection using DNA vaccines. Avian Dis 47:1181–1186
Oveissi S, Omar AR, Yusoff K, Jahanshiri F, Hassan SS (2010) DNA vaccine encoding avian influenza virus H5 and Esat-6 of Mycobacterium tuberculosis improved antibody responses against AIV in chickens. Comp Immunol Microbiol Infect Dis 33:491–503
Sawant PM et al (2015) Development of a DNA vaccine for chicken infectious anemia and its immunogenicity studies using high mobility group box 1 protein as a novel immunoadjuvant indicated induction of promising protective immune responses. Vaccine 33:333–340
Senthil K et al (2004) Development of DNA vaccine against chicken anemia virus simultaneously using its VP1 and VP2 proteins. Paper presented in XII Conference of IPSA and National Symposium, Himachal Pradesh Krishi Vishwavidalya, Palampur, p 152
Song KD et al (2000) A DNA vaccine encoding a conserved Eimeria protein induces protective immunity against live Eimeria acervulina challenge. Vaccine 19:243–252
Ma D et al (2011) Vaccination of chickens with DNA vaccine encoding Eimeria acervulina 3-1E and chicken IL-15 offers protection against homologous challenge. Exp Parasitol 127:208–214
Shah MAA, Song X, Xu L, Yan R, Li X (2011) Construction of DNA vaccines encoding Eimeria acervulina cSZ-2 with chicken IL-2 and IFN-γ and their efficacy against poultry coccidiosis. Res Vet Sci 90:72–77
Ding X et al (2005) In ovo vaccination with the Eimeria tenella EtMIC2 gene induces protective immunity against coccidiosis. Vaccine 23:3733–3740
Du A, Wang S (2005) Efficacy of a DNA vaccine delivered in attenuated Salmonella typhimurium against Eimeria tenella infection in chickens. Int J Parasitol 35:777–785
Xu Q et al (2008) Vaccination of chickens with a chimeric DNA vaccine encoding Eimeria tenella TA4 and chicken IL-2 induces protective immunity against coccidiosis. Vet Parasitol 156:319–323
Cho SH, Loewen PC, Marquardt RR (2004) A plasmid DNA encoding chicken interleukin-6 and Escherichia coli K88 fimbrial protein FaeG stimulates the production of anti-K88 fimbrial antibodies in chickens. Poultry Sci 83:1973–1978
Brandsma JL (2006) DNA vaccine design. In: Saltzman MW, Shen H, Brandsma JL (eds) DNA vaccines. Humana, Totowa, NJ, pp 3–10
Kozak M (1986) Point mutations define a sequence flanking the AUG initiator codon that modulates translation by eukaryotic ribosomes. Cell 44:283–292
Nagata T, Uchijima M, Yoshida A, Kawashima M, Koide Y (1999) Codon optimization effect on translational efficiency of DNA vaccine in mammalian cells: analysis of plasmid DNA encoding a CTL epitope derived from microorganisms. Biochim Biophys Res Commun 261:445–451
Ferraro B et al (2011) Clinical applications of DNA vaccines: current progress. Clin Infect Dis 53:296–302
Chang DZ, Lomazow W, Somberg CJ, Stan R, Perales MA (2004) Granulocyte-macrophage colony stimulating factor: an adjuvant for cancer vaccines. Hematology 9:207–215
Mohan CM, Dey S, Rai A, Kataria JM (2006) Recombinant haemagglutinin neuraminidase antigen-based single serum dilution ELISA for rapid serological profiling of Newcastle disease virus. J Virol Methods 138:117–122
Dey S et al (2004) Recombinant LipL32 antigen-based single serum dilution ELISA for detection of canine leptospirosis. Vet Microbiol 103:99–106
Ruiz-Hernandez R et al (2014) An infected chicken kidney cell co-culture ELISpot for enhanced detection of T cell responses to avian influenza and vaccination. J Immunol Methods 416:40–48
Ariaans MP (2008) ELISPOT and intracellular cytokine staining: novel assays for quantifying T cell responses in the chicken. Dev Comp Immunol 32:1398–1404
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Gupta, S.K., Dey, S., Chellappa, M.M. (2016). DNA Vaccination in Chickens. In: Thomas, S. (eds) Vaccine Design. Methods in Molecular Biology, vol 1404. Humana, New York, NY. https://doi.org/10.1007/978-1-4939-3389-1_11
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3389-1_11
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-4939-3388-4
Online ISBN: 978-1-4939-3389-1
eBook Packages: Springer Protocols