Abstract
Sevoflurane and propofol are widely used for induction and maintenance of general anesthesia. Although the effects of sevoflurane and propofol on cerebral hemodynamics during maintenance of general anesthesia have been demonstrated, the effects during induction of general anesthesia have still not been clarified. We therefore compared changes in cerebral blood flow (CBF) and oxygenation (CBO) during induction of anesthesia using sevoflurane (group S: n = 9) or propofol (group P: n = 9). CBF and CBO were evaluated using the following variables: oxy-, deoxy-, and total-hemoglobin (Hb) concentrations and tissue oxygen index (TOI), measured on the forehead by near-infrared spectroscopy. The variables were recorded immediately before administration of sevoflurane or propofol and at every 10 s for 4 min after administration of the induction agent. Patients received 8 % sevoflurane in 100 % oxygen via an anesthesia mask in group S, and an IV bolus of 2 mg/kg of propofol during oxygenation in group P. We found that oxy-Hb, total-Hb, and TOI were significantly higher in group S than in group P (P > 0.05). Changes in deoxy-Hb, MBP, and HR did not differ between the groups. The results of the present study demonstrated that sevoflurane increases CBF and CBO during induction of general anesthesia.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Sevoflurane and propofol are widely used for induction and maintenance of general anesthesia. The effects of sevoflurane and propofol on cerebral hemodynamics during maintenance of general anesthesia have been previously demonstrated [1, 2]. However, the effects during induction of general anesthesia, when hemodynamic changes are usually greater than during maintenance of anesthesia, have still not been clarified. We therefore compared changes in cerebral blood flow (CBF) and oxygenation (CBO) during induction of general anesthesia with sevoflurane or propofol using near infrared spectroscopy (NIRS).
2 Methods
After obtaining approval from our hospital ethics committee, we recruited and obtained written informed consent from 18 American Society of Anesthesiologists (ASA) I patients scheduled for elective surgical procedures under general anesthesia. The patients were divided into two groups according to whether they were anesthetized with sevoflurane (Group S) or propofol (Group P).
2.1 Monitoring
Intraoperative monitoring included automatic non-invasive blood pressure (NIBP) on the right arm, pulse oximetry, and electrocardiography. We evaluated the changes in CBF and CBO on the forehead using NIRS (NIRO-200NX®, Hamamatsu Photonics, Hamamatsu City, Japan). The NIR light from three laser diodes (735, 810, and 850 nm) was directed at the forehead, and the reflected light was transmitted to a multisegment photodiode detector array. The source-detector distance of the optode is 4 cm. With this, we continuously measured the changes in oxy-Hb, deoxy-Hb, total-Hb concentrations, and TOI (tissue oxygen index). Baseline data were recorded using NIRS immediately before administration of sevoflurane or propofol, and the time course of the variables was evaluated every 10 s for 4 min after administration of sevoflurane or propofol. Mean blood pressure (MBP) and heart rate (HR) were recorded every 1 min for 4 min after administration of sevoflurane or propofol.
2.2 Anesthetic Procedure
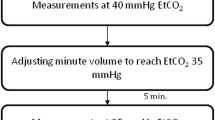
Eighteen patients were randomly allocated to group S (age, 40.0 ± 16.2 years) or group P (age, 44.6 ± 10.4 years). None of the patients received premedication. An intravenous line was inserted while the patient was still in the ward. In the operating room, the patients were placed in the supine position and received 6 l/min of oxygen through a face mask. After oxygenation for 3 min, patients were given 2 μg/kg fentanyl IV. One minute later, the patients who were assigned to group S received 8 % sevoflurane in 100 % oxygen via an anesthesia mask, while those in group P received an IV bolus of 2 mg/kg of propofol during oxygenation. All patients were administered 1 mg/kg rocuronium for muscle relaxation after loss of consciousness and were mechanically ventilated via an anesthesia mask, with maintenance of end-tidal CO2 within 35–40 mmHg for 4 min after administration of sevoflurane or propofol. Tracheal intubation was performed after the study measurements.
2.3 Data Analysis
All results are expressed as mean ± SD. Patient characteristics were compared between the groups using the unpaired Student’s t-test. Changes in MBP, HR, and NIRS variables during induction of anesthesia were analyzed using repeated-measures ANOVA and the Tukey-Kramer multiple comparison test for post-hoc analysis. P < 0.05 was considered to represent a statistically significant difference.
3 Results
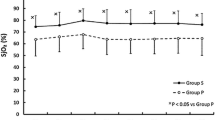
There were no significant differences in patient characteristics between the groups (Table 60.1). Figure 60.1 shows that there were no significant decreases in MBP and HR in both groups. As shown in Fig. 60.2, oxy-Hb (1.93 μmol/l), total-Hb (1.73 μmol/l), and TOI (2.93 %) increased from the baseline values and reached plateau within about 2 min in group S. When compared with the values observed in group P, the increases showed statistically significant differences. Changes in deoxy-Hb, MBP, and HR did not differ between the groups. In group P, oxy-Hb and TOI transiently decreased within 1 min after an injection of propofol, however there were no statistically significant changes from the baseline and shortly thereafter recovered to baseline level (Fig. 60.2).
4 Discussion
This is the first study to use NIRS to evaluate the changes in CBF and CBO during induction of general anesthesia with sevoflurane or propofol.
The present study demonstrated that oxy-Hb, total-Hb, and TOI increased during induction of general anesthesia with sevoflurane, while no time course change was observed after a bolus of propofol. It is well known that changes in total-Hb on NIRS reflect changes in cerebral blood volume (CBV) and correlate with changes in CBF [3, 4], while TOI reflects CBO [5]. Based on these facts, the results of the present study suggest that sevoflurane inhalation during induction of general anesthesia increases CBF and CBO, while propofol does not influence these variables.
It has been suggested that 1.0 minimum alveolar concentration (MAC) sevoflurane decreased CBF due to reduction in cerebral metabolism, whereas more than 1.5 MAC of sevoflurane dose-dependently increased CBF caused by its cerebral vasodilating effect [6–9]. Thus, 8 % (4.6 MAC) sevoflurane used in the present study may give rise to luxury perfusion secondary to uncoupling of flow and metabolism, and cause an impairment of cerebral autoregulation [1]. Therefore, a high concentration of sevoflurane may be unsuitable for patients with increased intracranial pressure, as occurs with intracranial space-occupying lesions, although it may be suitable for patients with carotid artery stenosis and cerebral ischemia.
The present study showed that oxy-Hb and TOI in group P transiently decreased within 1 min after an injection of propofol. It has been demonstrated that reduction in cerebral metabolism caused by propofol decreases CBF [1]. However, no concomitant change in total-Hb and deoxy-Hb suggests that CBF and cerebral metabolism remained stable. A further study to explain the phenomenon will be needed.
NIRS has the advantage of enabling evaluation of CBO using the ratio between oxy-Hb and total-Hb. When both cerebral metabolism and hemodynamics reduce concurrently during induction of general anesthesia, NIRS is specifically useful in evaluating both CBO and CBF.
5 Conclusion
Sevoflurane increases CBO and CBF during induction of general anesthesia, while propofol has no effect on these variables during anesthesia induction.
References
Conti A, Iacopino DG, Fodale V et al (2006) Cerebral haemodynamic changes during propofol-remifentanil or sevoflurane anaesthesia: transcranial Doppler study under bispectral index monitoring. Br J Anaesth 97:333–339
Kaisti KK, Metsahonkala L, Teras M et al (2002) Effects of surgical levels of propofol and sevoflurane anesthesia on cerebral blood flow in healthy subjects studied with positron emission tomography. Anesthesiology 96:1358–1370
Ferrari M, Wilson DA, Hanley DF et al (1992) Effects of graded hypotension on cerebral blood flow, blood volume, and mean transit time in dogs. Am J Physiol 262:1908–1914
Pryds O, Greisen G, Skov LL et al (1990) Carbon dioxide-related changes in cerebral blood volume and cerebral blood flow in mechanically ventilated preterm neonates: comparison of near infrared spectrophotometry and 133 Xenon clearance. Pediatr Res 27:445–449
Yagi T, Nagao K, Sakatani K et al (2013) Changes of oxygen metabolism and hemodynamics during ECPR with hypothermia measured by near-infrared spectroscopy: a pilot study. Adv Exp Med Biol 789:121–128
Matta BF, Hearth KJ, Tipping K et al (1999) Direct cerebral vasodilatory effects of sevoflurane and isoflurane. Anesthesiology 91:677–680
Bundgaard H, von Oettingen G, Larsen KM et al (1998) Effects of sevoflurane on intracranial pressure, cerebral blood flow and cerebral metabolism. A dose-response study in patients subjected to craniotomy for cerebral tumours. Acta Anaesthesiol Scand 42:621–627
Berkowitz RA, Hoffman WE, Cunningham F et al (1996) Changes in cerebral blood flow velocity in children during sevoflurane and halothane anesthesia. J Neurosurg Anesthesiol 8:194–198
Rhodali O, Juhel S, Mathew S et al (2014) Impact of sevoflurane anesthesia on brain oxygenation in children younger than 2 years. Paediatr Anaesth 24:734–740
Acknowledgments
The authors thank Kaoru Sakatani MD, PhD, (NEWCAT Institute, Department of Electronic Engineering, Nihon University College of Engineering, Koriyama, Japan) for assistance with data analysis.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media, New York
About this paper
Cite this paper
Kondo, Y., Hirose, N., Maeda, T., Suzuki, T., Yoshino, A., Katayama, Y. (2016). Changes in Cerebral Blood Flow and Oxygenation During Induction of General Anesthesia with Sevoflurane Versus Propofol. In: Elwell, C.E., Leung, T.S., Harrison, D.K. (eds) Oxygen Transport to Tissue XXXVII. Advances in Experimental Medicine and Biology, vol 876. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3023-4_60
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3023-4_60
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3022-7
Online ISBN: 978-1-4939-3023-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)