Abstract
Human epidermal growth factor receptor-2 (HER2) is a well-studied member of epidermal growth factor receptor (EGFR) family. HER2 gene amplification and/or protein overexpression can be observed in many cancers of epithelial origin, including breast carcinoma. In breast carcinomas, HER2 gene amplification serves as a negative prognostic factor and its presence is usually associated with a more aggressive clinical behavior. Currently, there are several medications, including monoclonal antibodies or small molecules that target this receptor on the surface of tumoral cells. Targeted therapy improves patients’ response rates and survival and increase time to progression when used alone or in combination with other therapeutic modalities. As the accurate determination of HER2 gene status is very important for proper selection of treatment, this can be achieved by several methods, such as immunohistochemistry and/or in situ hybridization.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Background
Currently, there are four different members in the epidermal growth factor receptor (EGFR) family. These consist of the erbB lineage of proteins and include erbB1 (EGFR), erbB2 (HER2), erbB3, and erbB4. Each of these molecules consists of an extracellular domain, a single hydrophobic transmembrane segment, an intracellular portion with a juxtamembrane segment, a protein kinase domain, and a carboxy terminal tail [1–3].
The human epidermal growth factor receptor-2 (HER2 or ERBB2) gene product is a transmembrane growth factor receptor, which is normally expressed in secretory epithelia. It is involved in the cellular signaling that regulates growth and development [3–5]. Other HER (ErbB) proteins can preferentially heterodimerize with HER2, which leads to phosphorylation of the tyrosine residues and activation of downstream effectors such as mitogen activating protein kinase (MAPK), phosphatidylinositol-3 kinase (PI3K), and signal transducer and activator of transcription (STAT). Depending on the particular signal cascades triggered, HER2 can be involved in different biological processes, including cell survival, proliferation, differentiation, invasion, adhesion, migration, and angiogenesis, as well as malignant transformation (Fig. 9.1) [6–8].
Signaling by ErbB homodimers in comparison with ErbB2-containing heterodimers. Receptors are shown as two lobes connected by a transmembrane stretch. Binding of a ligand (EGF-like or NRG) to the extracellular lobe of ErbB1, ErbB3 (note inactive kinase, marked by a cross), or ErbB4 induces homodimer formation. Unlike homodimers, which are either inactive (ErbB3 homodimers) or signal only weakly, ErbB2-containing heterodimers have attributes that prolong and enhance downstream signaling (green box) and their outputs (yellow box). NRG Neuregulin, EGF Epidermal Growth Factor. With permission from [4]. Copyright Nature Publishing Group 2001
Biology of HER2
HER2 protein is expressed at low levels in normal epithelial cells [9]. HER2 amplification and/or overexpression, however, is often observed in several cancers of epithelial origin, such as breast, colorectal, ovarian, pancreatic, and renal cell carcinomas [9, 10]. Studies using erbB2-deficient mouse models have shown lethal neural and cardiac defects during embryonic development [3, 11]. Over the past 20 years many mouse models have been developed to study the role of HER2 gene expression in breast cancer. These studies have shown that the erbB2 receptor can have a causal role in the development of breast carcinoma [12, 13].
The erbB-receptor family plays a crucial role in cell lineage differentiation into many tissue types, including the epithelial–mesenchymal transformation in epithelial tissues [14]. Although no ligand has been identified for erbB2, the receptor is recruited into heterodimers with other erbB receptors and this process increases ligand binding affinity of other erbB-receptor family members. Among erbB-family members, HER2 is the favored receptor for heterodimerization [6, 15].
Several mechanisms have been proposed to explain the role of erbB2 in oncogenesis. For instance, overexpression of erbB2 on the cell membrane may lead to increased heterodimerization with the kinase-defective erbB3 (HER3). These heterodimers may undergo a conformational change into the ligand-active state leading to weak, but prolonged activation of the receptor. Alternatively, spontaneous erbB2 homodimers may be formed upon overexpression of the protein with subsequent activation of the receptor tyrosine kinase [4, 16–18].
HER2 in Clinical Setting
HER2 overexpression can be seen in a number of tumors, including, but not limited to, breast, gastroesophageal, endometrial, lung, ovarian, bladder, and pancreatic carcinomas [17, 19–27]. HER2 gene amplification is the most common mechanism driving HER2 protein overexpression. This mechanism is observed in 15−20 % of breast and gastroesophageal carcinomas and at lower rates in other carcinomas [21, 24, 26]. In normal breast tissue, the ductal epithelial cells display an average of 80,000–100,000 HER2 receptors on the cell surface, whereas breast carcinoma cells can show 500,000 to 1,000,000 receptors on their surface [28–31].
Overexpression of HER2 receptor in breast cancer leads to increased homodimerization (HER2:HER2) and heterodimerization (e.g., HER2:HER3) of the receptors, which initiates a strong pro-tumorigenic signaling cascade [4].
HER2 gene amplification has been associated with a more aggressive clinical course.
In addition, HER2 gene amplification in breast carcinoma correlates with lymph node metastasis, negative hormone receptor status, high nuclear grade, and high proliferation index, such as high Ki67 positivity or increased mitotic activity [31–37].
Current evidence suggests that HER2 receptor overexpression can serve as a negative prognostic indicator [38]. HER2 protein overexpression has consistently been shown to act as an independent marker of poor prognosis in patients with lymph node-positive disease. Interestingly, this feature is often found in concert with other poor prognostic factors, such as large tumor size, higher histologic grade, or positive nodal status [29, 32, 38, 39].
Therapies Targeting HER2
HER2 gene amplification represents the underlying molecular event for the vast majority of HER2-driven breast cancers [40–44]. Since HER2 receptor plays a role in biological and clinical behavior of breast cancers, targeting this receptor in breast carcinomas with HER2 overexpression has been an attractive therapeutic approach. HER2 was the first molecule to be targeted with a novel humanized monoclonal antibody [45].
In 1998, the U.S. Food and Drug Administration (FDA) approved trastuzumab (Genentech, Inc., San Francisco, California), a humanized monoclonal antibody that targets the extracellular portion of the HER2 receptor. Clinical trials with trastuzumab showed that this treatment improves survival, response rates, and time to progression when used alone or in combination with chemotherapy [46–49]. Although approved for use in metastatic cancer, several prospective randomized clinical trials have also shown therapeutic benefit of trastuzumab in early stage breast cancers, by reducing the mortality rate by one-third and recurrence rate by one-half [50–55]. This therapy has been shown to be effective as a single agent or in combination with more traditional chemotherapy [56–59]. However, both clinical and in vitro studies have demonstrated that trastuzumab is only active against HER2-overexpressing (HER2 positive) tumors [49, 56, 58, 60]. There are also several reports showing that patients with relatively lower expression of HER2 protein on the cell surface derive some benefit from anti-HER2 therapy [61, 62].
Lapatinib (GlaxoSmithKline, King of Prussia, Pennsylvania), a tyrosine kinase inhibitor of HER2 and EGFR was the next therapeutic agent approved by the FDA for the treatment of HER2 positive breast cancers. Lapatinib is an ATP competitor that blocks phosphorylation of the HER2/EGFR1 tyrosine kinase domains inhibiting activation of AKT/PIK3CA and MAP kinase pathways. Lapatinib provided a significant improvement in disease-free survival of breast cancer patients after progression on trastuzumab [45, 63–65].
More recently, additional monoclonal antibody therapies have been approved for the treatment of HER2 positive metastatic breast cancer. In one instance, the original trastuzumab antibody has been conjugated to the cytotoxic agent mertansine. In one study, this antibody-drug conjugate, ado-trastuzumab emtansine (T-DM1), offered a better tolerance and improved both progression-free and overall survival when compared with the standard drug combination lapatinib–capecitabine [66]. A meta-analysis indicates that this antibody-drug conjugate is effective for HER2-positive metastatic breast cancer in patients previously treated with a variety of therapeutic agents, including trastuzumab, lapatinib, and a taxane [67, 68].
Another recently approved frontline therapy for HER2 positive metastatic breast cancer is the monoclonal antibody pertuzumab (Genentech, Inc) [69–73]. This represents a new class of monoclonal antibody that targets a different site on the HER2 molecule. Unlike trastuzumab, which binds to extracellular domain IV [74], a region that does not contribute to receptor dimerization, pertuzumab binds to domain II and blocks dimerization of the HER2 receptor. In vitro studies have shown that pertuzumab is more effective than trastuzumab in disrupting the HER1–HER2 and HER3–HER2 dimers [75, 76]. Several clinical trials are currently underway to show efficacy and potential side effects of these therapeutic agents (NCT01966471, NCT01855828, NCT02003209). These new HER2-targeting agents have been tested in the adjuvant setting, including trials with single agent or dual antibody regimens without concomitant or sequential chemotherapy [72, 77–82]. So far, pertuzumab therapy is associated with increased progression-free survival and a strong trend toward improved overall survival [73]. All of these ongoing efforts point to the fact that accurate HER2 testing is now more critical than ever to ensure that the patients receive the correct treatment.
Resistance to HER2 Targeted Therapy
The fact that still a fraction of HER2 positive breast carcinomas treated with these targeted therapies ultimately relapse or develop a more progressive disease, suggests that there are some de novo or acquired intrinsic mechanisms of resistance to these drugs [83]. Resistance may be innate or develop during the course of HER2-targeted therapy. Some of these mechanisms include mutations in HER2 gene itself, the use of compensatory signaling pathways and other resistance mutations affecting response to therapy (e.g., apoptosis). Mechanisms involving HER2 receptor alter the antibody binding site through alternative transcription and splicing. Compensatory signaling through other receptor or intracellular signaling pathways, such as insulin-like growth factor 1 receptor (IGF-1R), which widely bypass the HER2 receptor signaling, may also occur (Fig. 9.2). In addition, acquired mutations in PIK3CA or PTEN genes have been shown to confer resistance to trastuzumab. Finally, defects in cell cycle regulation or apoptosis, such as elevated levels of the apoptosis inhibitor survivin, as well as host factors that affect the immunomodulatory function of these drugs, may contribute to resistance [83–95].
Schematic depicting resistance to EGFR and HER2 inhibitors due to activation of bypass track signaling. a model of a sensitive EGFR or HER2-addicted cancer treated with an erbB small-molecule inhibitor or antibody resulting in suppression of downstream signaling. EGFR or HER2 homodimers and heterodimers are shown. b Model of an EGFR-mutant or HER2-amplified cancer with resistance due to maintenance of downstream signaling in the presence of the EGFR or HER2 inhibitors. Activation of signaling can be caused by activation of other receptor tyrosine kinases (RTKs) or mutational activation of downstream signaling. With permission from [83]. Copyright Elsevier 2014
Methods of HER2 Testing
Accurate determination of HER2 status is essential, given the significant therapeutic benefit derived from targeted therapy in HER2 positive tumors. This is underscored by the most recent American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) recommendations, which require HER2 testing of all newly diagnosed invasive breast cancers [95]. In addition, these therapeutic agents are not without complications or even serious side effects, necessitating the proper selection of patients who really benefit from them [96–98].
There are several methods that can be used to assess routine formalin-fixed paraffin-embedded (FFPE) clinical breast samples for HER2 status. These include the evaluation for HER2 protein overexpression at the tumor cell membrane by immunohistochemistry (IHC), the assessment of HER2 gene amplification by in situ hybridization [fluorescence in situ hybridization (FISH), chromogenic in situ hybridization (CISH), silver in situ hybridization (SISH)], by multiplex ligation-dependent probe amplification or reverse transcription polymerase chain reaction (RT-PCR) [99–103].
Two of these methods, namely IHC and FISH, have been studied more thoroughly and gained popularity for assessing HER2 status in breast carcinomas in routine clinical practice. These methods offer several advantages. Both of these assays allow correlation between HER2 protein expression or HER2 gene status and the morphologic features in tissue sections. Both methodologies have received FDA approval for HER2 evaluation [104, 105].
Assessment of HER2 Status by IHC
There are two FDA-approved antibodies, namely Herceptest (Dako, Carpinteria, California) and Pathway (Ventana, Tucson, Arizona), which may be used to assess HER2 protein status by IHC. These IHC systems have been reviewed in more detail elsewhere [95, 106]. A standardized scoring system for IHC studies has been developed and was most recently updated in 2013 (Fig. 9.3) [95, 104, 105].
Algorithm for evaluation of HER2 protein expression by IHC assay of the invasive component of a breast cancer specimen. ISH in situ hybridization. (Asterisk) Readily appreciated using a low-power objective and observed within a homogeneous and contiguous invasive tumor cell population. With permission from [95]. Copyright American Society of Clinical Oncology 2014
Briefly, a positive HER2 IHC is defined by intense, complete circumferential membrane staining in >10 % of invasive tumor cells (score 3+). HER2 IHC result is negative if weak and incomplete pattern of staining is seen in ≤10 % of tumor cells (score 0/1+). In approximately 20 % of cases, an equivocal result is observed showing incomplete and/or weak to moderate circumferential staining in >10 % of the invasive tumor cells or complete and intense circumferential membrane staining is present in ≤10 % of the invasive tumor cells. All equivocal HER2 results should be reflexed to an alternative testing (i.e., FISH or CISH) on the same or another specimen, if available (Fig. 9.4) [95].
Assessment of HER2 Status by FISH
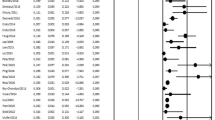
FISH is a molecular cytogenetic technique designed to detect specific chromosomal DNA sequences using fluorescent-labeled complementary DNA probes [106, 107]. There are three FDA-approved FISH probes manufactured by Abbott (PathVysion, Des Plaines, Illinois), Dako (HER2 FISH pharmaDx), and Ventana (INFORM, Tucson, Arizona) to assess HER2 gene status. These FISH systems have been reviewed in more detail elsewhere [95, 106]. A standardized scoring system for FISH has been developed and was most recently updated in 2013 (Figs. 9.5 and 9.6) [95, 104, 105].
Algorithm for evaluation of HER2 gene amplification by ISH assay of the invasive component of a breast cancer specimen using a single-signal (HER2 gene) assay (single-probe ISH). Amplification in a single-probe ISH assay is defined by examining the average HER2 gene copy number. If there is a second contiguous population of cells with increased HER2 signals per cell, and this cell population consists of more than 10 % of tumor cells on the slide, a separate counting of at least 20 nonoverlapping tumor cells must also be performed within this cell population and also reported. (Asterisk) Observed in a homogeneous and contiguous population. With permission from [95]. Copyright American Society of Clinical Oncology 2014
Algorithm for evaluation of HER2 gene amplification by ISH assay of the invasive component of a breast cancer specimen using a dual-signal (HER2 gene) assay (dual-probe ISH). Amplification in a dual-probe ISH assay is defined by examining first the HER2/CEP17 ratio followed by the average HER2 gene copy number. If there is a second contiguous population of cells with increased HER2 signals per cell, and this cell population consists of more than 10 % of tumor cells on the slide, a separate counting of at least 20 nonoverlapping tumor cells must also be performed within this cell population and also reported. CEP17, chromosome enumeration probe 17 (Asterisk) Observed in a homogeneous and contiguous population. With permission from [95]. Copyright American Society of Clinical Oncology 2014
Probe sets for HER2 may include a single-color HER2 probe or dual-color probes with one sequence labeled for the HER2 gene and the other for the centromere of chromosome 17 (CEP17). To determine amplification, an absolute HER2 gene copy number or a ratio of HER2 gene to CEP17 can be used. Since FISH studies have shown superior results in predicting a benefit from monoclonal antibody therapy, this approach has gained acceptance as a primary mode for HER2 testing in breast cancer [49, 56, 59, 100, 108–112]. As HER2 gene amplification almost always results in HER2 protein overexpression, it generally translates to 90−95 % concordance between these two methods [105]. However, 3−15 % of breast cancers may show protein overexpression without HER2 gene amplification [63, 105, 106, 113, 114]. Recent addition of copy number to the scoring guidelines may help to identify cases with polysomy (greater than 2 copies) of chromosome 17 with HER2 protein overexpression. FISH result should be reported as positive, if dual-probe HER2/CEP17 ratio is ≥2.0 or an average HER2 gene copy number ≥6.0 signals/cell. An equivocal result is defined as an average HER2 gene copy number ≥4.0 and <6.0 signals/cell and HER2/CEP17 ratio <2.0. Negative result is defined as HER2/CEP17 ratio <2.0 and an average HER2 gene copy number <4.0 signals/cell (Fig. 9.7) [95, 104, 108].
Although true polysomy 17 is not a common finding in breast carcinoma [115–117], in the presence of simultaneous increase in CEP17 and HER2 gene copy number, the ratio of HER2/CEP17 may remain less than 2.0 and mask the true amplification of the HER2 gene [118, 119]. In this regard, several other genes on chromosome 17, such as RARA, SMS, or TP53, have been tested as alternative probes in determining the true HER2 gene amplification and used successfully in different studies [120].
Brightfield In Situ Hybridization (ISH)
FISH has some disadvantages, such as the need for a dark field (fluorescence) microscope, which limits the ability to assess the conventional morphological details.
Brightfield ISH, which allows the user to assess HER2 gene status using light microscopy, has recently been introduced as an alternative to FISH testing for the detection of HER2 gene amplification. The current ASCO/CAP guidelines also endorse brightfield ISH methods due to high concordance with FISH and comparable clinical utility [95, 106]. Of these, chromogenic in situ hybridization (CISH) has recently been approved by the FDA. In contrast to FISH, the signals from these techniques do not fade. Therefore, the slides may be archived. Since CISH uses the brightfield microscopy, the viewer is able to easily locate the invasive tumor component to evaluate the gene status [121–124]. This method can be used to enumerate gene copy number (amplification, deletion) and chromosome translocation [125–128]. CISH similar to IHC uses enzyme-linked antibodies and chromogens to detect a hapten-labeled probe specific for the target DNA that can be applied to formalin-fixed paraffin-embedded (FFPE) tissues. Under the light microscopy the brown and red signals are visualized with better preservation of morphologic details. The interpretation of the signals may be difficult due to limitation in discriminating between discrete and overlapping signals on light microscopy [129]. However, the advantage of CISH over FISH in routine practice is that simultaneous verification of brightfield histology can be performed using CISH [130]. Although, CISH does not permit the actual determination of gene copy number, it has been shown to correlate with FISH [131]. Silver in situ hybridization (SISH) is a novel brightfield ISH technique [130]. It is a fully automated system which uses an enzyme-linked probe to deposit silver ions on the target site that improves the efficacy and consistency of ISH and reduces the risk of error. Automated detection of chromogenic signals also allows HER2 and CEP17 assays to be performed on consecutive tissue slides [130], making interpretation easier and resulting in a readily identifiable signals [129, 130, 132, 133]. This strategy allows HER2 gene status to be determined in reference to chromosome 17, so that a HER2/CEP17 ratio can be determined using the same reported ranges as those recommended by ASCO/CAP guidelines for FISH [129, 134]. The main disadvantage of these assays is an inherent risk of sectioning through the smaller tumors, when biopsy material is used for analysis [129, 135].
Correlation of Immunohistochemistry (IHC) with Fluorescence in Situ Hybridization (FISH)
In most studies, only cases with uniform intense circumferential membrane staining (score 3+) show a good concordance with HER2 gene amplification detected by FISH assay. This group of patients will be the most likely to benefit from HER2 monoclonal antibody therapies [49, 56, 58, 111, 136–142]. On the contrary, when there is no HER2 membrane staining or only faint and barely perceptible incomplete staining is observed (scores 0 or 1+), gene amplification studies typically demonstrate a normal HER2 gene status and these cases are regarded as negative [137, 138, 141, 143–145]. Cases with incomplete and/or weak to moderate circumferential membranous staining (score 2+) show poor agreement with FISH results and are considered inconclusive [66, 138, 143]. In this regard, an accurate and quantitative assessment of hormone receptor (HR) results is critical, when using IHC studies to determine therapeutic targets [95, 146, 147]. It should be emphasized that a number of pre-analytical (such as tissue handling and fixation), analytical (such as reagents, antibodies, protocols), and post-analytical (reporting, quality analysis, interpretation) factors can adversely affect immune reactivity of HER2 protein [108, 148]. These are discussed in more detail in chap. 19.
Key Points
-
Currently, there are four members in EGFR family of molecules. They include erbB1 (EGFR), erbB2 (HER2), erbB3 and erbB4.
-
In normal states, HER2 is expressed at low levels on the surface of epithelial cells.
-
HER2 protein overexpression can be seen in a number of epithelial tumors, including breast, gastroesophageal, endometrial, ovarian and lung carcinomas.
-
HER2 gene amplification as the most common mechanism for HER2 protein overexpression is seen in 15 % to 20 % of breast carcinomas.
-
HER2 protein overexpression can serve as a negative prognostic factor.
-
HER2 overexpression can be determined at the protein or gene levels by IHC or ISH assays.
-
HER2 overexpressing breast carcinomas can be targeted by several therapeutics, including monoclonal anti-HER2 antibodies or small molecules.
-
Currently trastuzumab, pertuzumab and lapatinib have been approved by FDA as targeted therapies for breast carcinomas with HER2 protein overexpression.
References
Roskoski R Jr. The ErbB/HER receptor protein-tyrosine kinases and cancer. Biochem Biophys Res Commun. 2004;319(1):1–11.
Roskoski R Jr. ErbB/HER protein-tyrosine kinases: structures and small molecule inhibitors. Pharmacol Res. 2014;87C:42–59.
Burgess AW. EGFR family: structure physiology signalling and therapeutic targets. Growth Factors. 2008;26(5):263–74.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2(2):127–37.
Waterman H, et al. The C-terminus of the kinase-defective neuregulin receptor ErbB-3 confers mitogenic superiority and dictates endocytic routing. EMBO J. 1999;18(12):3348–58.
Citri A, Skaria KB, Yarden Y. The deaf and the dumb: the biology of ErbB-2 and ErbB-3. Exp Cell Res. 2003;284(1):54–65.
Wallasch C, et al. Heregulin-dependent regulation of HER2/neu oncogenic signaling by heterodimerization with HER3. EMBO J. 1995;14(17):4267–75.
Seliger B, Kiessling R. The two sides of HER2/neu: immune escape versus surveillance. Trends Mol Med. 2013;19(11):677–84.
Press MF, Cordon-Cardo C, Slamon DJ. Expression of the HER-2/neu proto-oncogene in normal human adult and fetal tissues. Oncogene. 1990;5(7):953–62.
Seidman JD, Frisman DM, Norris HJ. Expression of the HER-2/neu proto-oncogene in serous ovarian neoplasms. Cancer. 1992;70(12):2857–60.
Negro A, Brar BK, Lee KF. Essential roles of Her2/erbB2 in cardiac development and function. Recent Prog Horm Res. 2004;59:1–12.
Suda Y, et al. Induction of a variety of tumors by c-erbB2 and clonal nature of lymphomas even with the mutated gene (Val659—Glu659). EMBO J. 1990;9(1):181–90.
Ursini-Siegel J, et al. Insights from transgenic mouse models of ERBB2-induced breast cancer. Nat Rev Cancer. 2007;7(5):389–97.
Burden S, Yarden Y. Neuregulins and their receptors: a versatile signaling module in organogenesis and oncogenesis. Neuron. 1997;18(6):847–55.
Citri A, Yarden Y. EGF-ERBB signalling: towards the systems level. Nat Rev Mol Cell Biol. 2006;7(7):505–16.
Di Fiore PP, et al. erbB-2 is a potent oncogene when overexpressed in NIH/3T3 cells. Science. 1987;237(4811):178–82.
Hudziak RM, Schlessinger J, Ullrich A. Increased expression of the putative growth factor receptor p185HER2 causes transformation and tumorigenesis of NIH 3T3 cells. Proc Natl Acad Sci USA. 1987;84(20):7159–63.
Kokai Y, et al. Synergistic interaction of p185c-neu and the EGF receptor leads to transformation of rodent fibroblasts. Cell. 1989;58(2):287–92.
Gonzaga IM, et al. Alterations in epidermal growth factor receptors 1 and 2 in esophageal squamous cell carcinomas. BMC Cancer. 2012;12:569.
Cappuzzo F, Bemis L, Varella-Garcia M. HER2 mutation and response to trastuzumab therapy in non-small-cell lung cancer. N Engl J Med. 2006;354(24):2619–21.
Boku N. HER2-positive gastric cancer. Gastric Cancer. 2014;17(1):1–12.
Boku N. Molecular target for Her2 positive gastric cancer. Nihon Shokakibyo Gakkai Zasshi. 2012;109(12):2014–20.
Bang YJ, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376(9742):687–97.
Yan M, et al. HER2 aberrations in cancer: implications for therapy. Cancer Treat Rev. 2014;40(6):770–80.
Zhang HT, et al. New perspectives on anti-HER2/neu therapeutics. Drug News Perspect. 2000;13(6):325–9.
Koeppen HK, et al. Overexpression of HER2/neu in solid tumours: an immunohistochemical survey. Histopathology. 2001;38(2):96–104.
Chan DS, Twine CP, Lewis WG. Systematic review and meta-analysis of the influence of HER2 expression and amplification in operable oesophageal cancer. J Gastrointest Surg. 2012;16(10):1821–9.
Ross JS, et al. The Her-2/neu gene and protein in breast cancer 2003: biomarker and target of therapy. Oncologist. 2003;8(4):307–25.
Slamon DJ, et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177–82.
Stefano R, et al. Expression levels and clinical-pathological correlations of HER2/neu in primary and metastatic human breast cancer. Ann NY Acad Sci. 2004;1028:463–72.
Yaziji H, Gown AM. Accuracy and precision in HER2/neu testing in breast cancer: are we there yet? Hum Pathol. 2004;35(2):143–6.
Yu D, Hung MC. Overexpression of ErbB2 in cancer and ErbB2-targeting strategies. Oncogene. 2000;19(53):6115–21.
Penault-Llorca F, Cayre A. Assessment of HER2 status in breast cancer. Bull Cancer. 2004;91(Suppl 4):S211–5.
Varga Z, et al. Assessment of HER2 status in breast cancer: overall positivity rate and accuracy by fluorescence in situ hybridization and immunohistochemistry in a single institution over 12 years: a quality control study. BMC Cancer. 2013;13:615.
Dowsett M, et al. Assessment of HER2 status in breast cancer: why, when and how? Eur J Cancer. 2000;36(2):170–6.
Yarden Y. Biology of HER2 and its importance in breast cancer. Oncology. 2001;61(Suppl 2):1–13.
Eccles SA. The role of c-erbB-2/HER2/neu in breast cancer progression and metastasis. J Mammary Gland Biol Neoplasia. 2001;6(4):393–406.
Pegram MD. Treating the HER2 pathway in early and advanced breast cancer. Hematol Oncol Clin North Am. 2013;27(4):751–65.
Slamon DJ, et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244(4905):707–12.
Gown AM. Current issues in ER and HER2 testing by IHC in breast cancer. Mod Pathol. 2008;21(Suppl 2):S8–15.
Garcia-Caballero T, et al. Determination of HER2 amplification in primary breast cancer using dual-colour chromogenic in situ hybridization is comparable to fluorescence in situ hybridization: a European multicentre study involving 168 specimens. Histopathology. 2010;56(4):472–80.
Owens MA, Horten BC, Da Silva MM. HER2 amplification ratios by fluorescence in situ hybridization and correlation with immunohistochemistry in a cohort of 6556 breast cancer tissues. Clin Breast Cancer. 2004;5(1):63–9.
Peintinger F, et al. Hormone receptor status and pathologic response of HER2-positive breast cancer treated with neoadjuvant chemotherapy and trastuzumab. Ann Oncol. 2008;19(12):2020–5.
Paik S, Kim C, Wolmark N. HER2 status and benefit from adjuvant trastuzumab in breast cancer. N Engl J Med. 2008;358(13):1409–11.
Robidoux A, et al. Lapatinib as a component of neoadjuvant therapy for HER2-positive operable breast cancer (NSABP protocol B-41): an open-label, randomised phase 3 trial. Lancet Oncol. 2013;14(12):1183–92.
Slamon D, Pegram M. Rationale for trastuzumab (Herceptin) in adjuvant breast cancer trials. Semin Oncol. 2001;28(1 Suppl 3):13–9.
Horton J. Trastuzumab use in breast cancer: clinical issues. Cancer Control. 2002;9(6):499–507.
Tan-Chiu E, Piccart M. Moving forward: herceptin in the adjuvant setting. Oncology. 2002;63(Suppl 1):57–63.
Vogel CL, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20(3):719–26.
Ferretti G, et al. Adjuvant trastuzumab with docetaxel or vinorelbine for HER-2-positive breast cancer. Oncologist. 2006;11(7):853–4.
Joensuu H, et al. Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med. 2006;354(8):809–20.
Piccart-Gebhart MJ, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353(16):1659–72.
Untch M, et al. Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol. 2010;28(12):2024–31.
Romond EH, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353(16):1673–84.
Smith I, et al. 2-year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007;369(9555):29–36.
Slamon DJ, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Pegram MD, et al. Rational combinations of trastuzumab with chemotherapeutic drugs used in the treatment of breast cancer. J Natl Cancer Inst. 2004;96(10):739–49.
Tedesco KL, et al. Docetaxel combined with trastuzumab is an active regimen in HER-2 3+ overexpressing and fluorescent in situ hybridization-positive metastatic breast cancer: a multi-institutional phase II trial. J Clin Oncol. 2004;22(6):1071–7.
Cobleigh MA, et al. Multinational study of the efficacy and safety of humanized anti-HER2 monoclonal antibody in women who have HER2-overexpressing metastatic breast cancer that has progressed after chemotherapy for metastatic disease. J Clin Oncol. 1999;17(9):2639–48.
Pegram M, Slamon D. Biological rationale for HER2/neu (c-erbB2) as a target for monoclonal antibody therapy. Semin Oncol. 2000;27(5 Suppl 9):13–9.
Borley A, et al. Impact of HER2 copy number in IHC2+/FISH-amplified breast cancer on outcome of adjuvant trastuzumab treatment in a large UK cancer network. Br J Cancer. 2014;110(8):2139–43.
Dowsett M, et al. Disease-free survival according to degree of HER2 amplification for patients treated with adjuvant chemotherapy with or without 1 year of trastuzumab: the HERA Trial. J Clin Oncol. 2009;27(18):2962–9.
Sauter G, et al. Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. J Clin Oncol. 2009;27(8):1323–33.
Inoue T, et al. Clinical evaluation of lapatinib therapy in metastatic breast cancer using the Bayes meta-analysis. Gan Kagaku Ryoho. 2014;41(3):347–52.
Garcia-Munoz C, et al. Lapatinib plus transtuzumab for HER-2 positiva metastatic breast cancer: experience of use. Farm Hosp. 2014;38(2):130–4.
Verma S, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91.
Krop IE, et al. Trastuzumab emtansine versus treatment of physician’s choice for pretreated HER2-positive advanced breast cancer (TH3RESA): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15(7):689–99.
Corrigan PA, et al. Ado-trastuzumab Emtansine: A HER2-positive targeted antibody-drug conjugate. Ann Pharmacother. 2014;48:1484–93.
Lynce F, Swain SM. Pertuzumab for the treatment of breast cancer. Cancer Invest. 2014;32:430–8.
McCormack PL. Pertuzumab: a review of its use for first-line combination treatment of HER2-positive metastatic breast cancer. Drugs. 2013;73(13):1491–502.
O’Sullivan CC, Connolly RM. Pertuzumab and its accelerated approval: evolving treatment paradigms and new challenges in the management of HER2-positive breast cancer. Oncology (Williston Park). 2014;28(3):186–94 196.
Gianni L, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(1):25–32.
Schneeweiss A, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol. 2013;24(9):2278–84.
Cho HS, et al. Structure of the extracellular region of HER2 alone and in complex with the Herceptin Fab. Nature. 2003;421(6924):756–60.
Jhaveri K, Esteva FJ. Pertuzumab in the treatment of HER2+ breast cancer. J Natl Compr Canc Netw. 2014;12(4):591–8.
Franklin MC, et al. Insights into ErbB signaling from the structure of the ErbB2-pertuzumab complex. Cancer Cell. 2004;5(4):317–28.
Swain SM, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2013;14(6):461–71.
Baselga J, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–19.
de Azambuja E, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol. 2014;15(10):1137–46.
Baselga J, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379(9816):633–40.
Baselga J, Swain SM. CLEOPATRA: a phase III evaluation of pertuzumab and trastuzumab for HER2-positive metastatic breast cancer. Clin Breast Cancer. 2010;10(6):489–91.
Blackwell KL, et al. Randomized study of Lapatinib alone or in combination with trastuzumab in women with ErbB2-positive, trastuzumab-refractory metastatic breast cancer. J Clin Oncol. 2010;28(7):1124–30.
Arteaga CL, Engelman JA. ERBB receptors: from oncogene discovery to basic science to mechanism-based cancer therapeutics. Cancer Cell. 2014;25(3):282–303.
Engelman JA, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316(5827):1039–43.
Nahta R, et al. Insulin-like growth factor-I receptor/human epidermal growth factor receptor 2 heterodimerization contributes to trastuzumab resistance of breast cancer cells. Cancer Res. 2005;65(23):11118–28.
Lu Y, et al. Insulin-like growth factor-I receptor signaling and resistance to trastuzumab (Herceptin). J Natl Cancer Inst. 2001;93(24):1852–7.
Berns K, et al. A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell. 2007;12(4):395–402.
Nagata Y, et al. PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell. 2004;6(2):117–27.
Esteva FJ, et al. PTEN, PIK3CA, p-AKT, and p-p70S6 K status: association with trastuzumab response and survival in patients with HER2-positive metastatic breast cancer. Am J Pathol. 2010;177(4):1647–56.
Xia W, et al. A model of acquired autoresistance to a potent ErbB2 tyrosine kinase inhibitor and a therapeutic strategy to prevent its onset in breast cancer. Proc Natl Acad Sci USA. 2006;103(20):7795–800.
Valabrega G, et al. HER2-positive breast cancer cells resistant to trastuzumab and lapatinib lose reliance upon HER2 and are sensitive to the multitargeted kinase inhibitor sorafenib. Breast Cancer Res Treat. 2011;130(1):29–40.
Oliveras-Ferraros C, et al. Inhibitor of Apoptosis (IAP) survivin is indispensable for survival of HER2 gene-amplified breast cancer cells with primary resistance to HER1/2-targeted therapies. Biochem Biophys Res Commun. 2011;407(2):412–9.
Musolino A, et al. Immunoglobulin G fragment C receptor polymorphisms and clinical efficacy of trastuzumab-based therapy in patients with HER-2/neu-positive metastatic breast cancer. J Clin Oncol. 2008;26(11):1789–96.
Gennari R, et al. Pilot study of the mechanism of action of preoperative trastuzumab in patients with primary operable breast tumors overexpressing HER2. Clin Cancer Res. 2004;10(17):5650–5.
Wolff AC, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of clinical oncology/college of American pathologists clinical practice guideline update. J Clin Oncol. 2013;31(31):3997–4013.
Keefe DL. Trastuzumab-associated cardiotoxicity. Cancer. 2002;95(7):1592–600.
Ewer SM, Ewer MS. Cardiotoxicity profile of trastuzumab. Drug Saf. 2008;31(6):459–67.
Babar T, et al. Anti-HER2 cancer therapy and cardiotoxicity. Curr Pharm Des. 2014;20(30):4911–9.
Moelans CB, et al. Current technologies for HER2 testing in breast cancer. Crit Rev Oncol Hematol. 2011;80(3):380–92.
Pauletti G, et al. Assessment of methods for tissue-based detection of the HER-2/neu alteration in human breast cancer: a direct comparison of fluorescence in situ hybridization and immunohistochemistry. J Clin Oncol. 2000;18(21):3651–64.
Xing WR, et al. FISH detection of HER-2/neu oncogene amplification in early onset breast cancer. Breast Cancer Res Treat. 1996;39(2):203–12.
Persons DL, et al. Fluorescence in situ hybridization (FISH) for detection of HER-2/neu amplification in breast cancer: a multicenter portability study. Ann Clin Lab Sci. 2000;30(1):41–8.
Susini T, et al. Preoperative assessment of HER-2/neu status in breast carcinoma: the role of quantitative real-time PCR on core-biopsy specimens. Gynecol Oncol. 2010;116(2):234–9.
Wolff AC, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of clinical oncology/college of American pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138(2):241–56.
Wolff AC, et al. American Society of clinical oncology/college of American pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med. 2007;131(1):18–43.
Wolff AC, et al. American Society of clinical oncology/college of American pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25(1):118–45.
Bartlett J, Mallon E, Cooke T. The clinical evaluation of HER-2 status: which test to use? J Pathol. 2003;199(4):411–7.
Cornejo KM, et al. Theranostic and molecular classification of breast cancer. Arch Pathol Lab Med. 2014;138(1):44–56.
Shak S. Overview of the trastuzumab (Herceptin) anti-HER2 monoclonal antibody clinical program in HER2-overexpressing metastatic breast cancer. Herceptin multinational investigator study group. Semin Oncol. 1999;26((4 Suppl 12)):71–7.
Ross JS, et al. HER-2/neu testing in breast cancer. Am J Clin Pathol. 2003;120(Suppl):S53–71.
Press MF, et al. Evaluation of HER-2/neu gene amplification and overexpression: comparison of frequently used assay methods in a molecularly characterized cohort of breast cancer specimens. J Clin Oncol. 2002;20(14):3095–105.
Addition of trastuzumab to chemotherapy produces 50 % increase in survival in patients selected by FISH. Oncology (Williston Park), 2001; 15(10): 1345, 1364.
Dyhdalo KS, et al. Laboratory compliance with the american society of clinical oncology/college of american pathologists human epidermal growth factor receptor 2 testing guidelines: a 3-year comparison of validation procedures. Arch Pathol Lab Med. 2014;138(7):876–84.
Grimm EE, et al. Achieving 95 % cross-methodological concordance in HER2 testing: causes and implications of discordant cases. Am J Clin Pathol. 2010;134(2):284–92.
Moelans CB, de Weger RA, van Diest PJ. Absence of chromosome 17 polysomy in breast cancer: analysis by CEP17 chromogenic in situ hybridization and multiplex ligation-dependent probe amplification. Breast Cancer Res Treat. 2010;120(1):1–7.
Yeh IT, et al. Clinical validation of an array CGH test for HER2 status in breast cancer reveals that polysomy 17 is a rare event. Mod Pathol. 2009;22(9):1169–75.
Viale G. Be precise! The need to consider the mechanisms for CEP17 copy number changes in breast cancer. J Pathol. 2009;219(1):1–2.
Vranic S, et al. Assessment of HER2 gene status in breast carcinomas with polysomy of chromosome 17. Cancer. 2011;117(1):48–53.
Perez EA, et al. HER2 and chromosome 17 effect on patient outcome in the N9831 adjuvant trastuzumab trial. J Clin Oncol. 2010;28(28):4307–15.
Tse CH, et al. Determining true HER2 gene status in breast cancers with polysomy by using alternative chromosome 17 reference genes: implications for anti-HER2 targeted therapy. J Clin Oncol. 2011;29(31):4168–74.
Clark BZ, Bhargava R. Bright-field microscopy for HER2 gene assessment: not just DISH-ful thinking? Am J Clin Pathol. 2013;139(2):137–9.
Bhargava R, Lal P, Chen B. Chromogenic in situ hybridization for the detection of HER-2/neu gene amplification in breast cancer with an emphasis on tumors with borderline and low-level amplification: does it measure up to fluorescence in situ hybridization? Am J Clin Pathol. 2005;123(2):237–43.
Isola J, et al. Interlaboratory comparison of HER-2 oncogene amplification as detected by chromogenic and fluorescence in situ hybridization. Clin Cancer Res. 2004;10(14):4793–8.
Mayr D, et al. Chromogenic in situ hybridization for Her-2/neu-oncogene in breast cancer: comparison of a new dual-colour chromogenic in situ hybridization with immunohistochemistry and fluorescence in situ hybridization. Histopathology. 2009;55(6):716–23.
Kato N, et al. Evaluation of HER2 gene amplification in invasive breast cancer using a dual-color chromogenic in situ hybridization (dual CISH). Pathol Int. 2010;60(7):510–5.
Todorovic-Rakovic N, et al. Prognostic value of HER2 gene amplification detected by chromogenic in situ hybridization (CISH) in metastatic breast cancer. Exp Mol Pathol. 2007;82(3):262–8.
Di Palma S, et al. Chromogenic in situ hybridisation (CISH) should be an accepted method in the routine diagnostic evaluation of HER2 status in breast cancer. J Clin Pathol. 2007;60(9):1067–8.
Arnould L, et al. Agreement between chromogenic in situ hybridisation (CISH) and FISH in the determination of HER2 status in breast cancer. Br J Cancer. 2003;88(10):1587–91.
Francis GD, et al. Bright-field in situ hybridization for HER2 gene amplification in breast cancer using tissue microarrays: correlation between chromogenic (CISH) and automated silver-enhanced (SISH) methods with patient outcome. Diagn Mol Pathol. 2009;18(2):88–95.
Park K, et al. Silver-enhanced in situ hybridization as an alternative to fluorescence in situ hybridization for assaying HER2 amplification in clinical breast cancer. J Breast Cancer. 2011;14(4):276–82.
Schnitt SJ, Jacobs TW. Current status of HER2 testing: caught between a rock and a hard place. Am J Clin Pathol. 2001;116(6):806–10.
Bae YK, et al. HER2 status by standardized immunohistochemistry and silver-enhanced in situ hybridization in Korean breast cancer. J Breast Cancer. 2012;15(4):381–7.
Koh YW, et al. Dual-color silver-enhanced in situ hybridization for assessing HER2 gene amplification in breast cancer. Mod Pathol. 2011;24(6):794–800.
Unal B, et al. Determination of HER2 gene amplification in breast cancer using dual-color silver enhanced in situ hybridization (dc- SISH) and comparison with fluorescence ISH (FISH). Asian Pac J Cancer Prev. 2013;14(10):6131–4.
Jacquemier J, et al. SISH/CISH or qPCR as alternative techniques to FISH for determination of HER2 amplification status on breast tumors core needle biopsies: a multicenter experience based on 840 cases. BMC Cancer. 2013;13:351.
Dowsett M, et al. Correlation between immunohistochemistry (HercepTest) and fluorescence in situ hybridization (FISH) for HER-2 in 426 breast carcinomas from 37 centres. J Pathol. 2003;199(4):418–23.
Bilous M, et al. Current perspectives on HER2 testing: a review of national testing guidelines. Mod Pathol. 2003;16(2):173–82.
Ridolfi RL, Jamehdor MR, Arber JM. HER-2/neu testing in breast carcinoma: a combined immunohistochemical and fluorescence in situ hybridization approach. Mod Pathol. 2000;13(8):866–73.
Tubbs RR, Hicks DG. HER-2 testing in breast cancer. JAMA. 2004; 292(15): p 1817-8 (author reply 1818).
Lal P, et al. HER-2 testing in breast cancer using immunohistochemical analysis and fluorescence in situ hybridization: a single-institution experience of 2,279 cases and comparison of dual-color and single-color scoring. Am J Clin Pathol. 2004;121(5):631–6.
Yaziji H, et al. HER-2 testing in breast cancer using parallel tissue-based methods. JAMA. 2004;291(16):1972–7.
Elkin EB, et al. HER-2 testing and trastuzumab therapy for metastatic breast cancer: a cost-effectiveness analysis. J Clin Oncol. 2004;22(5):854–63.
Zhang H, et al. HER-2 gene amplification by fluorescence in situ hybridization (FISH) compared with immunohistochemistry (IHC) in breast cancer: a study of 528 equivocal cases. Breast Cancer Res Treat. 2012;134(2):743–9.
Goud KI, et al. Evaluation of HER-2/neu status in breast cancer specimens using immunohistochemistry (IHC) & fluorescence in-situ hybridization (FISH) assay. Indian J Med Res. 2012;135:312–7.
Kemp JD, Royer MC. 2+ HER-2/neu IHC results: positively equivocal. J Cutan Pathol. 2010; 37(8): p. 915; author reply 916.
Hammond ME, et al. American Society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med. 2010;134(7):e48–72.
Hammond ME, et al. American Society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28(16):2784–95.
Penault-Llorca F, et al. Optimization of immunohistochemical detection of ERBB2 in human breast cancer: impact of fixation. J Pathol. 1994;173(1):65–75.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Sakhdari, A., Hutchinson, L., Cosar, E.F. (2015). Molecular Pathology of HER Family of Oncogenes in Breast Cancer: HER-2 Evaluation and Role in Targeted Therapy. In: Khan, A., Ellis, I., Hanby, A., Cosar, E., Rakha, E., Kandil, D. (eds) Precision Molecular Pathology of Breast Cancer. Molecular Pathology Library, vol 10. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2886-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2886-6_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2885-9
Online ISBN: 978-1-4939-2886-6
eBook Packages: MedicineMedicine (R0)